Abstract
Objectives
Green House and other small nursing home (NH) models are considered “nontraditional” due to their size (10–12 beds), universal caregivers, and other home-like features. They have garnered great interest regarding their potential benefit to limit Coronavirus Disease 2019 (COVID-19) infections due to fewer people living, working, visiting, and being admitted to Green House/small NHs, and private rooms and bathrooms, but this assumption has not been tested. If they prove advantageous compared with other NHs, they may constitute an especially promising model as policy makers and providers reinvent NHs post-COVID.
Design
This cohort study compared rates of COVID-19 infections, COVID-19 admissions/readmissions, and COVID-19 mortality, among Green House/small NHs with rates in other NHs between January 20, 2020 and July 31, 2020.
Setting and Participants
All Green House homes that held a skilled nursing license and received Medicaid or Medicare payment were invited to participate; other small NHs that replicate Green House physical design and operational practices were eligible if they had the same licensure and payer sources. Of 57 organizations, 43 (75%) provided complete data, which included 219 NHs. Comparison NHs (referred to as “traditional NHs”) were up to 5 most geographically proximate NHs within 100 miles that had <50 beds and ≥50 beds for which data were available from the Centers for Medicare and Medicaid Services (CMS). Because Department of Veterans Affairs organizations are not required to report to CMS, they were not included.
Methods
Rates per 1000 resident days were derived for COVID-19 cases and admissions, and per 100 COVID-19 positive cases for mortality. A log-rank test compared rates between Green House/small NHs and traditional NHs with <50 beds and ≥50 beds.
Results
Rates of all outcomes were significantly lower in Green House/small NHs than in traditional NHs that had <50 beds and ≥50 beds (log-rank test P < .025 for all comparisons). The median (middle value) rates of COVID-19 cases per 1000 resident days were 0 in both Green House/small NHs and NHs <50 beds, while they were 0.06 in NHs ≥50 beds; in terms of COVID-19 mortality, the median rates per 100 positive residents were 0 (Green House/small NHs), 10 (<50 beds), and 12.5 (≥50 beds). Differences were most marked in the highest quartile: 25% of Green House/small NHs had COVID-19 case rates per 1000 resident days higher than 0.08, with the corresponding figures for other NHs being 0.15 (<50 beds) and 0.74 (≥50 beds).
Conclusions and Implications
COVID-19 incidence and mortality rates are less in Green House/small NHs than rates in traditional NHs with <50 and ≥50 beds, especially among the higher and extreme values. Green House/small NHs are a promising model of care as NHs are reinvented post-COVID.
Keywords: COVID-19, nursing homes
Since the onset of the Severe Acute Respiratory Syndrome Coronavirus 2 pandemic (COVID-19) in the United States, long-term care rsesidents have represented a disproportionate share of cases and deaths. As of January 8, 2021, 6% of COVID-19 cases, and 38% of COVID-19 deaths, have been attributed to long-term care.1 These rates reflect the medical conditions of this population that put them at risk, as well as the congregate nature of long-term care that increases the spread of infection.2
Short-term remedies related to the congregate nature of long-term care include using personal protective equipment, restricting visitors, and instituting screening.3 Longer-term remedies may ward off threats when the next pandemic arises, centered on nursing home (NH) quality,4 staffing,5 and physical design.6 , 7 Presumably, smaller NHs reduce risk because there are fewer residents (including new admissions), staff, and visitors who may spread infection.
Nontraditional small house NHs have garnered great interest in the wake of COVID-19.8 The most well-known model of this type, the Green House model, has 300 NHs across 32 states.9 Components of Green House homes that may be critical for infection prevention and control are that they house only 10 to 12 residents, and have consistent and universal staff assignment (thereby limiting ancillary staff), private rooms and bathrooms, smaller overall space, and a central entry. Research on Green House NHs has found their benefits include better resident quality of life, fewer hospital readmissions, better quality indicators, reduced Medicare spending, and perhaps less staff turnover.10
Given the potentially advantageous components of Green House/small NHs for infection prevention and control, this project collected data related to the number of COVID-19 cases and deaths among residents in Green House/small NHs, and examined them in comparison to larger NHs (<50 beds and ≥50 beds). Both categorizations “<50 beds” and “≥50 beds” omitted Green House/small NHs, and so refer to traditional model NHs. It also compared rates of COVID-19 admissions/readmissions. Data specific to COVID-19 in Green House/small NHs are not publicly available and have not been previously analyzed, meaning results provide novel findings and implications.
Methods
Sample
All operating Green House homes that held a skilled nursing license and received Medicaid or Medicare payment were invited to participate, as was one additional small house organization (with 10 NHs) that may be joining the Green House network because its operation mirrors that of Green House homes. Given that COVID-19 rates vary by location and relate to community prevalence,5 analyses compared rates of Green House/small NHs to other NHs that were selected through matching each Green House/small NH to up to the 5 nearest traditional NHs in the Centers for Medicare and Medicaid Services (CMS) database with <50 beds and with ≥50 beds and that were located within 100 miles. Because some Green House and other small NHs are colocated/colicensed with a larger NH, all such organizations were omitted from the CMS data. Distances for matching were calculated based on latitude and longitude information obtained from the “geosphere” package available in R.
Data
Green House/small NH administrators were asked to provide data related to their census (occupied beds), number of residents with incident COVID-19 (new laboratory positive COVID-19 cases), COVID-19 admissions/readmissions (persons admitted or readmitted who were previously hospitalized for COVID-19), and resident deaths from COVID-19 (suspected or laboratory positive who died in the NH or another location), from January 20, 2020 to July 31, 2020; data were reported for each week after May 31, 2020, and reported in aggregate for a single large period before that date. Data for other (traditional) NHs were obtained for the same time period from the online CMS COVID-19 Nursing Home DataSet11; they were reported weekly after an initial period where data were aggregated through May 24, 2020. Notably, the data items obtained from the Green House/small NH homes were worded exactly as the CMS data.
Analyses
COVID-19 cases and admission/readmission rates were calculated per 1000 resident days, and COVID-19 mortality was calculated as per 100 COVID-19 cases. Specifically, for each NH, COVID-19 case counts during the study period were summed over the reporting periods (usually weeks), and case rates were then calculated by dividing total case counts by days of exposure (ie, resident days = sum over reporting periods of occupied beds timess the number of days in the reporting period) and multiplying by 1000. COVID-19 admission/readmission rates were calculated in the same manner. The COVID-19 mortality rate per 100 COVID-19–positive cases was calculated by dividing the sum of COVID-19 death counts by the sum of COVID-19 confirmed cases and multiplying by 100. For each COVID-19 outcome, a log-rank test, which is a nonparametric test that emphasizes detection of group differences among higher values, was applied to compare rates among the 3 NH types. Multiple comparisons between 2 groups (Green House/small NHs vs traditional NHs <50 beds; Green House/small NHs vs traditional NHs ≥50 beds) were subsequently performed using log-rank tests if the omnibus test was statistically significant at P < .05. Statistical significance for the pairwise comparisons was set at P < .025, per Bonferroni adjustment. Analyses were conducted in R version 4.0.
Results
Of 57 eligible Green House/small NH organizations, 43 organizations (75%) across 20 states, representing 219 NHs, provided complete data for analyses. Comparison data were available for 177 traditional NHs <50 beds, and 215 traditional NHs ≥50 beds (Table 1 ).
Table 1.
Numbers of Green House/Small NH Organizations (and NHs) by State, and Comparison NHs Within 100 Miles, by Bed Size
| States (N = 20) | Number of Green House/Small NH Organizations (Number of NHs)∗ | Nearest 5 Comparison NHs to Each Organization (Within 100 Miles)† |
|
|---|---|---|---|
| <50 Beds | ≥50 Beds | ||
| AL | 1 (9) | 2 | 5 |
| AR | 4 (33) | 0‡ | 20 |
| CO | 3 (12) | 15 | 15 |
| Fl | 1 (12) | 5 | 5 |
| IL | 1 (1) | 5 | 5 |
| KS | 2 (8) | 10 | 10 |
| KY | 1 (2) | 5 | 5 |
| MI | 2 (4) | 10 | 10 |
| MN | 1 (6) | 5 | 5 |
| MO | 2 (8) | 10 | 10 |
| MS | 1 (6) | 4 | 5 |
| NY | 4 (29) | 17 | 20 |
| OH | 12 (51) | 59 | 60 |
| PA | 1 (6) | 5 | 5 |
| RI | 1 (4) | 5 | 5 |
| TN | 2 (12) | 6 | 10 |
| TX | 1 (2) | 2 | 5 |
| VA | 1 (8) | 5 | 5 |
| WI | 1 (2) | 5 | 5 |
| WY | 1 (4) | 2 | 5 |
| Total | 43 (219) | 177§ | 215|| |
All NHs within an organization share the same address. Small house NHs are typically clustered into organizations that also include the original founding NH (referred to as the “legacy” NH); together, these NHs hold a single license. All such organizations were omitted from the comparison NHs.
Data from CMS, excluding Green House/small NH organizations.
All nursing homes in Arkansas (AR) have ≥ 50 beds.
Mean size 36 beds (SD 9, range 12–49); mean distance to Green House/small NH organization 26.27 miles (SD 24.71, range 0.66–99.40).
Mean size 118 beds (SD 68, range 50–566); mean distance to Green House/small NH organization 8.05 miles (SD 11.67, range 0.17–72.84).
As shown in Table 2 , the median (middle value) rate of COVID-19 cases and COVID-19 admissions/readmissions per 1000 resident days is 0 in all NHs except in one instance. The only figure higher than 0 is COVID-19 cases per 1000 resident days for NHs ≥50 beds (0.06), meaning that half of NHs ≥50 beds had 6 or more COVID-19 cases for every 100,000 resident days. For NHs ≥50 beds, the median rate can also be expressed as 2.19 (= 0.06 × 365/10) cases per 100 resident years (eg, 100 residents each followed for 1 year) which exceeds the median rate of 0 for GH/small NHs and NHs <50 beds. In terms of COVID-19 mortality, the median rates per 100 COVID-positive residents are 0 (GH/small NHs), 10 (<50 beds), and 12.5 (≥50 beds).
Table 2.
Comparison of COVID-19 Rates Between Green House/Small NHs and Nearest 5 Comparison NHs, by NH Size
| Indicators | Green House/Small NH Organization (n = 43)† Median 75th Percentile 90th Percentile |
Nearest 5 Comparison NHs∗ |
||||
|---|---|---|---|---|---|---|
| NHs with <50 Beds (n = 177) Median 75th Percentile 90th Percentile |
NHs with ≥50 Beds (n = 215) Median 75th Percentile 90th Percentile |
P value‡ |
||||
| Omnibus Test(3 Groups) | Green House/Small NH Organizations Compared with Traditional NHs with <50 Beds | Green House/Small NH Organizations Compared with Traditional NHs with ≥50 Beds |
||||
| COVID-19 cases per 1000 resident days | 0 0.08 0.30 |
0 0.15 1.61 |
0.06 0.74 2.10 |
<.001 | .014 | <.001 |
| COVID-19 admissions/readmissions per 1000 resident days | 0 0 <0.01 |
0 0.13 0.74 |
0 0.11 0.49 |
<.001 | <.001 | <.001 |
| COVID-19 mortality per 100 positive cases§ | 0 <0.01 24.3 |
10.0 50.0 80.5 |
12.5 30.0 53.3 |
.016 | .007 | .007 |
Data from CMS, excluding Green House/small NH organizations.
Small house NHs are typically clustered into organizations which also include the original founding NH (referred to as the “legacy” NH); together, these NHs hold a single license. All such organizations were omitted from the comparison NHs.
P value calculated using log-rank test.
Number of suspected or laboratory positive resident deaths from COVID-19 divided by number of laboratory positive resident cases of COVID-19 times 100.
In light of the low rates overall, it is useful to look at rate summaries other than averages, specifically, rates at the 75th and 90th percentiles. In all comparisons, rates for Green House/small NHs are lower, with differences most marked in the higher and extreme values. For example, traditional NHs <50 beds and ≥50 beds have approximately twice and 9 times the 75th percentile rates of COVID-19 cases, respectively, than in Green House/small NHs, with omnibus log-rank test P < .001. Multiplying the figures in 2 by 36.5 (= 365/10), the corresponding 75th percentile figures translated into rates per 100 resident years are 2.92, 5.48, and 27.0, respectively, meaning that one-quarter of NHs of each type had rates higher than these.
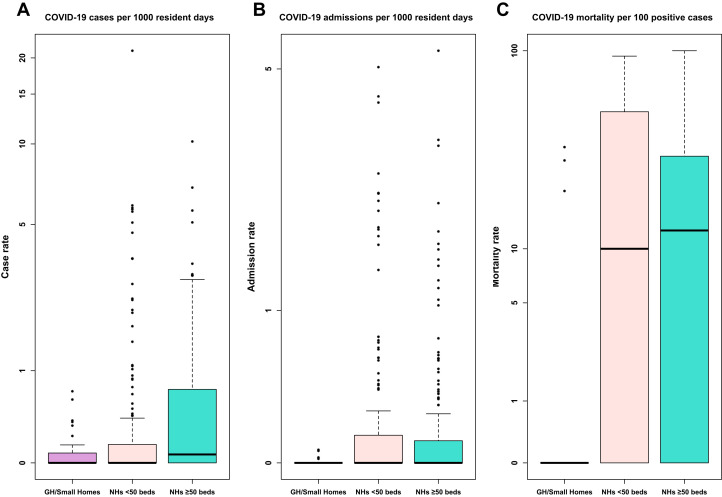
Figure 1 graphically displays the significantly lower rates of COVID-19 cases, COVID-19 admissions, and COVID-19 mortality in Green House/small NHs. The black line within the box indicates the median rate, the top of the box indicates the 75th percentile of rates, the line above the box indicates the majority of rates (the third quartile plus 1.5 × the interquartile range), and the asterisks indicate extreme values. In addition to demonstrating that even outlier rates for Green House/small NHs are markedly lower than those in other NHs, it appears that NHs <50 beds have generally lower COVID-19 case rates than NHs ≥50 beds, but such is not the case in relation to COVID-19 mortality rates or admissions.
Fig. 1.
Rates of COVID-19 cases, admissions, and mortality in Green House/small NHs (n = 43), traditional NHs with <50 beds (n = 177), and traditional NHs with ≥50 beds (n = 215). Each box represents rates between the 25th and 75th percentiles; the line within the box indicates the median. The line above the box indicates the majority of observations (up to the value representing the third quartile plus 1.5 times the interquartile range); asterisks indicate outliers. Data are presented on the log scale. One outlier among homes with ≥50 beds had an admissions rate of more than 50 per 1000 resident days and is not shown. GH, Green House.
Discussion
NH quality has been criticized for decades, and concern has increased markedly following the ravages of COVID-19. Stakeholders agree we must capitalize on the opportunity offered by COVID-19 to transform our system of long-term care, but the path to necessary changes (financing, accountability, workforce, regulation12) suggest an arduous and contentious road. Green House/small NHs, which already are widely in favor, may constitute a promising future. Their model already exists, and in addition to being advantageous in relation to COVID-19, they benefit resident quality of life, improve satisfaction, reduce hospital readmissions and Medicare spending, and result in better quality indicators.10 , 13
The median incidence of COVID-19 cases in Green House/small NHs was significantly less than that in NHs ≥50 beds: 0 versus 2.19 cases per 100 resident years (eg, 100 residents each followed for 1 year). Given the low rates overall, differences were even more notable among the higher and extreme values: while only one-quarter of Green House/small NHs had rates per 100 resident years higher than 2.92, the corresponding rates for traditional NHs <50 beds and ≥50 beds, respectively, were 5.48 and 27.0. Although small size is known to limit the proportion of COVID-19 cases,6 Green House/small NHs are beneficial above and beyond the mere benefit of size, perhaps due to their private bedrooms and bathrooms, limited ancillary staff, and fewer admissions; in fact, traditional NHs <50 beds were not as advantaged in terms of COVID-19 admissions as were Green House/small NHs.
In terms of COVID-19 mortality, the median rates per 100 COVID-positive residents were 0 (Green House/small NHs), 10 (<50 beds), and 12.5 (≥50 beds); thus, the benefit of Green House/small NHs remains in terms of mortality. In this regard, the potential advantage of small size may be to psychosocial well-being. Families may be more able to have socially distanced outdoor visits, and having consistent, universal staff may allow for the maintenance of social relationships. Notably, residents in Green House homes receive significantly more hours per day of care from certified nursing assistants than do residents in traditional nursing homes.14 Others have reported that visitor restrictions increase loneliness, depression, physical deterioration, and cognitive decline,15 and so Green House/small NHs may convey an important psychosocial advantage. However, NHs <50 beds were not advantaged in the higher and extreme values compared with NHs ≥50 beds (their mortality rates at 75% and 90% percentile were markedly higher), which may speak to other critical differences.
Differences exist between Green House/small NHs and other NHs that are less clearly related to infection prevention and psychosocial well-being, and which may in part relate to COVID-19 differences. One such driver may be for-profit status, which has repeatedly been found to relate to lower NH quality. Green House NHs are much less likely to be for-profit than are NHs across the country (18% compared with 69%),16, 17, 18 and tend to pay their certified nursing assistants more than do other NH14 (which may result in fewer staff working in more than one job). In addition, resident case-mix differs between Green House and other NHs which may partly explain COVID-19 differences, including that they have fewer African American residents who are at higher mortality risk, and fewer residents who are bedfast and catheterized.19, 20, 21 Such differences would be most consequential in terms of explaining differences in COVID-19 mortality rates.
Clearly, more research is needed on the model of Green House/small NHs, including consideration of components that could not be adjusted in analyses. Other limitations are that the accuracy of the CMS data cannot be affirmed, and analyses used data only through July 31, 2020. The decision to not extend analyses beyond that date was in part based on the fact that some Green House/small NHs and other NHs were changing their models of care such as becoming COVID-19–only NHs, which would have affected the results and their interpretation. On the other hand, the use of nonparametric descriptive and testing methods depended only on the rank order of the combined samples and so results are robust to extreme rates.
Green House NHs were established in 2003 and have been replicated across the country and widely researched (compared with other small NHs), largely with funding from The Robert Wood Johnson Foundation.22 AARP recently highlighted this model as an option to transform long-term care, while noting that its adoption has been limited, in part due to financing, regulatory, and workforce challenges.17 Hope may be on the horizon, however, given universal recognition that beyond the pandemic, we must transform how our nation provides and finances long-term care.23
Conclusions and Implications
COVID-19 incidence and mortality rates are less in Green House/small NHs than rates in traditional NHs with <50 and ≥50 beds, especially among the higher and extreme values. More than half of Americans who survive to age 65 will require long-term care,24 yet most would rather die than live in an NH.25 Nontraditional Green House/small NHs have better outcomes than traditional NHs in numerous areas; evidence now demonstrates they have lower rates of COVID-19 and COVID-19 mortality than other NHs as well. As such, they are an especially promising model as NHs are reinvented post-COVID.
Footnotes
CD-S, AH, and SR are employed by the Green House Project. No other authors have potential conflicts of interest.
References
- 1.Kaiser Family Foundation COVID-19: Long-term care facilities. https://www.kff.org/health-costs/issue-brief/state-data-and-policy-actions-to-address-coronavirus/ Available at:
- 2.Dosa D., Jump R.L.P., LaPlante K., Gravenstein S. Long-term care facilities and the coronavirus epidemic: practical guidelines for a population at highest risk. J Am Med Dir Assoc. 2020;21:569–571. doi: 10.1016/j.jamda.2020.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention Infection control for nursing homes. https://www.cdc.gov/coronavirus/2019-ncov/hcp/long-term-care.html Available at:
- 4.He M., Li Y., Fang F. Is there a link between nursing home reported quality and COVID-19 cases? Evidence from California skilled nursing facilities. J Am Med Dir Assoc. 2020;21:905–908. doi: 10.1016/j.jamda.2020.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gorges R.J., Konetzka R.T. Staffing levels and COVID-19 cases and outbreaks in U.S. nursing homes. J Am Geriatr Soc. 2020;68:2462–2466. doi: 10.1111/jgs.16787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Abrams H.R., Loomer L., Gandhi A., Grabowski D.C. Characteristics of U.S. nursing homes with COVID-19 cases. J Am Geriatr Soc. 2020;68:1653–1656. doi: 10.1111/jgs.16661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lynch R.M., Goring R. Practical steps to improve air flow in long-term care resident rooms to reduce COVID-19 infection risk. J Am Med Dir Assoc. 2020;21:893–894. doi: 10.1016/j.jamda.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Anderson D.C., Grey T., Kennelly S., O'Neill D. Nursing home design and COVID-19: balancing infection control, quality of life, and resilience. J Am Med Dir Assoc. 2020;21:1519–1524. doi: 10.1016/j.jamda.2020.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.The Green House Project. https://www.thegreenhouseproject.org/about/visionmission Available at:
- 10.Zimmerman S., Bowers B.J., Cohen L.W., THRIVE Research Collaborative New evidence on the Green House Model of nursing home care: synthesis of findings and implications for policy, practice, and research. Health Serv Res. 2016;51(Suppl 1):475–496. doi: 10.1111/1475-6773.12430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Centers for Medicare & Medicaid Services (CMS) COVID-19 Nursing Home DataSet. https://data.cms.gov/Special-Programs-Initiatives-COVID-19-Nursing-Home/COVID-19-Nursing-Home-Dataset/s2uc-8wxp Available at: [PubMed]
- 12.Coronavirus Commission for Safety and Quality in Nursing Homes: Commission Final Report. https://sites.mitre.org/nhcovidcomm/wp-content/uploads/sites/14/2020/09/FINAL-REPORT-of-NH-Commission-Public-Release-Case-20-2378.pdf Available at: [DOI] [PMC free article] [PubMed]
- 13.Ausserhofer D., Deschodt M., De Geest S. There's no place like home": A scoping review on the impact of homelike residential care models on resident-, family-, and staff-related outcomes. J Am Med Dir Assoc. 2016;17:685–693. doi: 10.1016/j.jamda.2016.03.009. [DOI] [PubMed] [Google Scholar]
- 14.Sharkey S.S., Hudak S., Horn S.D. Frontline caregiver daily practices: A comparison study of traditional nursing homes and the Green House project sites. J Am Geriatr Soc. 2011;59:126–131. doi: 10.1111/j.1532-5415.2010.03209.x. [DOI] [PubMed] [Google Scholar]
- 15.Sizoo E.M., Monnier A.A., Bloemen M. Dilemmas with restrictive visiting policies in Dutch nursing homes during the COVID-19 pandemic: A qualitative analysis of an open-ended questionnaire with elderly care physicians. J Am Med Dir Assoc. 2020;21:1774–1781. doi: 10.1016/j.jamda.2020.10.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bos A., Boselie P., Trappenburg M. Financial performance, employee well-being, and client well-being in for-profit and not-for-profit nursing homes: A systematic review. Health Care Manage Rev. 2017;42:352–368. doi: 10.1097/HMR.0000000000000121. [DOI] [PubMed] [Google Scholar]
- 17.Reinhard S.C., Hado E. AARP LTSS choices: Small-house nursing homes. https://www.aarp.org/content/dam/aarp/ppi/2021/small-house-nursing-homes.pdf Available at:
- 18.Harris-Kojetin L., Sengupta M., Lendon J.P. Long-term care providers and services users in the United States, 2015–2016. National Center for Health Statistics. Vital Health Stat. 2019;3 x-xii; 1-105. [PubMed] [Google Scholar]
- 19.Afendulis C.C., Caudry D.J., O'Malley A.J., THRIVE Research Collaborative Green House adoption and nursing home quality. Health Serv Res. 2016;51(Suppl 1):454–474. doi: 10.1111/1475-6773.12436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Izurieta H.S., Graham D.J., Jiao Y. Natural history of COVID-19: Risk factors for hospitalizations and deaths among >26 million U.S. Medicare beneficiaries. J Infect Dis. 2020:jiaa767. doi: 10.1093/infdis/jiaa767. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Reinhardt J.P., Cimarolli V.R., Burack O.R. The small house model of long-term care: Association with older adult functioning. J Am Med Dir Assoc. 2019;20:222–223. doi: 10.1016/j.jamda.2018.10.003. [DOI] [PubMed] [Google Scholar]
- 22.Fishman N.W., Lowe J.I., Ryan S.F. Promoting an alternative to traditional nursing home care: Evaluating the Green House small home model. Health Serv Res. 2016;51:344–351. doi: 10.1111/1475-6773.12429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Werner R.W., Hoffman A.K., Coe N.B. Long-term care policy after COVID-19 – Solving the nursing home crisis. N Engl J Med. 2020;383:903–905. doi: 10.1056/NEJMp2014811. [DOI] [PubMed] [Google Scholar]
- 24.Favreault M., Dey J. Long-term services and supports for older Americans: Risks and financing research brief. https://aspe.hhs.gov/basic-report/long-term-services-and-supports-older-americans-risks-and-financing-research-brief Available at:
- 25.Nationwide Retirement Institute Long-term care annual survey. https://nationwidefinancial.com/media/pdf/NFM-19975AO.pdf?_ga=2.134397489.1539286378.1607707700-1671690935.1607707700 Available at: