Remdesivir is the first antiviral drug fully licensed for the treatment of patients with COVID-19. The use of remdesivir in 2020, can be summarised in five stages. First, between May and July, several regulatory agencies issued the authorisation—under emergency or conditional schemes—to treat selected patients hospitalised with COVID-19.1 Second, the manufacturer, Gilead, set a price of US$2340 for a 5-day treatment course in late June.2 Third, in October, the US Food and Drug Administration (FDA)3 granted full approval for use of remdesivir in adults and adolescent patients (aged 12 years or older; >40 kg) with COVID-19; it should be given intravenously for 5 days (six vials) to patients who do not need invasive mechanical ventilation or extracorporeal membrane oxygenation, or both, and 10 days (11 vials) in those who require this type of support. Fourth, the European Commission4 signed a joint procurement contract in October for $1·2 billion of remdesivir vials to treat 500 000 patients in 36 European countries, although the full marketing authorisation has not been granted yet. And fifth, the negative interim results on mortality from the largest randomised controlled trial (RCT), WHO Solidarity,5 were reported.
The decision to grant temporary approvals was made on the basis of results from the ACTT-1 study,6 a placebo-controlled RCT, for which preliminary results were announced on April 29, 2020. ACTT-1 showed that the time to recovery for hospitalised patients receiving remdesivir (10 days) was significantly shorter than for patients receiving placebo (15 days); there was no significant survival benefit in the overall trial population, although a post-hoc analysis suggested a significant benefit in patients receiving oxygen. Supportive data were shown by two additional RCTs.7, 8
Based on ACTT-1 results,6 Gilead considered that the reduced length of hospital stays for patients receiving remdesivir would save approximately $12 000 per patient and established the value-based price of remdesivir at $3000 per day. To ensure broad and equitable access and remove any price negotiations, Gilead set a price for governments of $390 per vial.2 This high price prompted 11 US state treasurers to write a letter to Gilead asking for a substantial price reduction.9 The total cost to be recovered—which includes 2020 projected research and development costs—has been estimated at $101–160 per vial.10
The full licensing of remdesivir granted by the FDA was on the basis of results from the same trials6, 7, 8 used for issuing emergency use authorisation. An additional RCT11 done in China showed no clinical benefit of remdesivir versus placebo and was not included in the FDA assessment, although the study was published in April and was included in the European Medicines Agency (EMA) assessment of the conditional approval.
Amid a time of high incidence of COVID-19 cases in Europe, and with remdesivir in short supply, the European Commission4 signed a joint procurement contract with Gilead, with an agreed price of $2340 for a 5-day course. However, it seems that none of the 36 countries involved in the deal are obliged to purchase remdesivir.4
The Solidarity trial5 was done in 405 hospitals in 30 countries, assessing different drugs versus standard of care. The interim results from 5451 participants randomly allocated to a 10-day course of remdesivir or standard of care found no effect on mortality (rate ratio [RR] 0·95 [95% CI 0·81–1·11]), the need to initiate artificial ventilation, or time to discharge.5
Pooling the Solidarity trial results with RCTs that had a control group receiving placebo6, 11 or standard of care,7 resulted in RR of 0·91 (95%CI 0·79–1·05) of death from any cause. At best, remdesivir would prevent only a small proportion of all deaths. Further, the RR for death was 0·80 (0·63–1·01) in patients at low risk (not requiring ventilation) and 1·16 (0·85–1·60) in patients at higher risk (requiring ventilation),5 suggesting that remdesivir might provide a small benefit in mortality only when given to hospitalised patients not requiring ventilation. In this meta-analysis5 the absolute risk reduction in mortality in patients at low risk was 1·6% (8·6% in control group, 7·0% in remdesivir group), corresponding to a number needed to treat of 62·5; as a result the costs for public health systems would be $146 250 per life saved.
The WHO living guidance,12 based on a meta-analysis with data from the same four RCTs,5, 6, 7, 11 stated that remdesivir has possibly no effect on mortality (odds ratio [OR] 0·90 [95% CI 0·70–1·12]) and a conditional recommendation was given against the use of remdesivir in hospitalised patients with COVID-19.
The EMA recommends remdesivir in adults and adolescent patients (aged 12 years or older) with COVID-19 who require supplemental oxygen. If the European marketing authorisation limits its use to these patients, then remdesivir will be given with corticosteroids, which is the standard of care in patients with COVID-19 requiring oxygen or mechanical ventilation.13 In the USA, remdesivir plus dexamethasone is also recommended in patients requiring oxygen using a high-flow device, or non-invasive ventilation.14 However, there are no RCTs assessing the clinical benefit of adding remdesivir to corticosteroids in these patients—and an adequately powered mega-trial would need thousands of participants. Nowadays, it should be acknowledged that it is uncertain whether adding remdesivir to corticosteroids provides any benefit on mortality, compared with corticosteroids alone.
Once remdesivir becomes available in Europe, governments should agree a substantially lower price with Gilead. Until the effectiveness of remdesivir in clinical practice is well defined in Europe, a payment-by-result agreement could also be considered. In this scheme, reimbursement is linked to the performance of the drug in each patient. Survival should be the endpoint to assess the response to receiving remdesivir plus corticosteroids.
The commitment from WHO and the International Coalition of Medicines Regulatory Authorities (to which EMA belong) to work together towards rapid approvals on the basis of robust and scientifically sound evidence15 suggests that results from all RCTs (including the Solidarity trial) will be considered in the benefit and risk assessment of remdesivir by the EMA. The EMA and health technology assessment bodies should define the efficacy and cost-effectiveness of COVID-19 treatments at country level to help public health systems make the best clinical use of remdesivir.
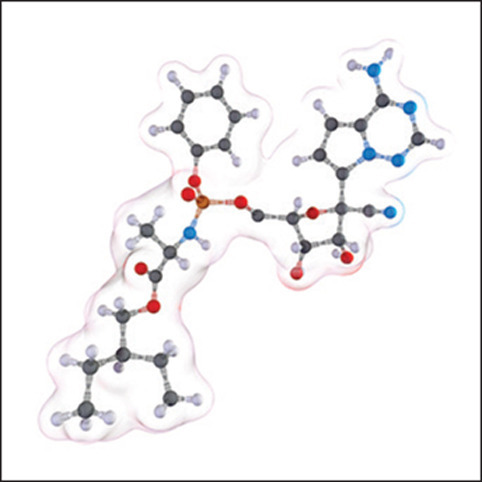
© 2021 Sci-Comm Studios/Science Photo Library
Acknowledgments
We thank Robin E Ferner (Birmingham, UK) for comments to an earlier version of this manuscript. RS is chair of the COVID-19 Therapeutics Advisory Group and a sub-committee of the Joint Specialist Committee for Infectious Disease at the Royal College of Physicians (London, UK). RD-R, RB, SG-L, RP, MZ, and FRR declare no competing interests. The views or opinions presented in this Comment are solely those of the authors and do not necessarily represent those of the institutions or organisations or advisory groups they work for.
References
- 1.Saint-Raymond A, Sato J, Kishioka Y, Teixeira T, Hasslboeck C, Kweder SL. Remdesivir emergency approvals: a comparison of the US, Japan and EU systems. Expert Rev Clin Pharmacol. 2020;13:1095–1101. doi: 10.1080/17512433.2020.1821650. [DOI] [PubMed] [Google Scholar]
- 2.Gilead Sciences An open letter from Daniel O'Day, chairman & CEO, Gilead Sciences. June 29, 2020. https://www.gilead.com/news-and-press/press-room/press-releases/2020/6/an-open-letter-from-daniel-oday-chairman-ceo-gilead-sciences
- 3.FDA Remdesivir. Highlights of prescribing information. October, 2020. https://www.accessdata.fda.gov/drugsatfda_docs/label/2020/214787Orig1s000lbl.pdf
- 4.Cohen J, Kupferschmidt K. The ‘very, very bad look’ of remdesivir, the first FDA-approved COVID-19 drug. Oct 28, 2020. https://www.sciencemag.org/news/2020/10/very-very-bad-look-remdesivir-first-fda-approved-covid-19-drug
- 5.WHO Solidarity Trial Consortium Repurposed antiviral drugs for COVID-19 —interim WHO Solidarity trial results. N Engl J Med. 2020 doi: 10.1056/NEJMoa2023184. published online Dec 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Beigel JH, Tomashek KM, Dodd LE, et al. Remdesivir for the treatment of COVID-19 - final report. N Engl J Med. 2020;383:1813–1826. doi: 10.1056/NEJMoa2007764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Spinner CD, Gottlieb RL, Criner GJ, et al. Effect of remdesivir vs standard care on clinical status at 11 days in patients with moderate COVID-19: a randomized clinical trial. JAMA. 2020;324:1048–1057. doi: 10.1001/jama.2020.16349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Goldman JD, Lye DCB, Hui DS, et al. Remdesivir for 5 or 10 days in patients with severe COVID-19. N Engl J Med. 2020;383:1827–1837. doi: 10.1056/NEJMoa2015301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Torsella JM. Treasury Department Commonwealth of Pennsylvania. Sept 16, 2020. https://patreasury.gov/pdf/newsroom/Gilead-Sciences-Letter_Redacted.pdf
- 10.Institute for Clinical and Economic Review Alternative pricing models for remdesivir and other potential treatments for COVID-19. Nov 10, 2020. https://icer-review.org/wp-content/uploads/2020/11/ICER-COVID_Updated_Report_11102020.pdf
- 11.Wang Y, Zhang D, Du G, et al. Remdesivir in adults with severe COVID-19: a randomised, double-blind, placebo-controlled, multicentre trial. Lancet. 2020;395:1569–1578. doi: 10.1016/S0140-6736(20)31022-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.WHO Therapeutics and COVID-19: living guideline, 20 November 2020. Nov 20, 2020. https://apps.who.int/iris/handle/10665/336729
- 13.Lamontagne F, Agoritsas T, Macdonald H, et al. A living WHO guideline on drugs for COVID-19. BMJ. 2020;370 doi: 10.1136/bmj.m3379. [DOI] [PubMed] [Google Scholar]
- 14.National Institutes of Health Coronavirus disease 2019 (COVID-19) treatment guidelines. Dec 3, 2020. https://www.covid19treatmentguidelines.nih.gov/ [PubMed]
- 15.WHO WHO-ICMRA joint statement on the need for improved global regulatory alignment on COVID-19 medicines and vaccines. Nov 6, 2020. https://www.who.int/news/item/06-11-2020-who-icmra-joint-statement-on-the-need-for-improved-global-regulatory-alignment-on-covid-19-medicines-and-vaccines


