Abstract
Objective
The aims of this study were to follow up the monitoring, health and anxiety from women who became pregnant after an embryo transfer or a intrauterine insemination during the COVID-19 epidemic in France
Study Design
This is a single centre, retrospective study from December 2019 to March 2020 based on a phone call interview using a specific questionnaire sheet specially developed for this study. Questionnaires from 104 pregnant women were completed and descriptive data are then analyzed.
Results
Women with ongoing pregnancies (n = 88) did not change their physician visits. The COVID-19 outbreak has created no or few additional stresses for 77 % of pregnant women since the lockdown started. We report a miscarriage rate of 14.4 % (n = 15) and documented 10 patients (11.3 %) who had symptoms related to COVID-19. No severe symptoms and no hospitalization in intensive care unit were identified.
Conclusion
The epidemic context did not disrupt the medical monitoring of pregnancies and we did not recover an increased rate of miscarriage after ART. None of the patients who had COVID-related symptoms presented with severe clinical manifestations. Surprisingly, pregnant women were psychologically able to experience the lockdown.
Keywords: SARS-CoV-2, COVID-19, Follow-up, ART Pregnancies
1 Introduction
The COVID-19 pandemic is an emerging infectious disease caused by the coronavirus SARS-CoV-2 (Severe Acute Respiratory Syndrome Coronavirus 2). It appeared on 17 November 2019 in the city of Wuhan, central China, and then spread worldwide and declared on January 30, 2020, as a public health emergency of international concern by the World Health Organization (WHO). In France, on December 2, 2020, the first case was identified in eastern France but it cannot be excluded that there may be other previous undetected cases. From March 17 (8 days after Italy), to reduce contact and travel to the strictest minimum, the entire French population with 67 million citizens was placed in lockdown to stop the exponential spread of the COVID-19 and, in so doing, to reduce to a minimum the number of people affected, the number of patients admitted in intensive care unit (ICU) and therefore the number of deaths. At that time, 7730 cases and 175 deaths were related to the COVID-19 disease in France. Then rapidly, our country became the fourth most affected European countries and our Assisted Reproduction Technologies (ART) Center located in Paris has been in one of the most affected regions. On 22 March 2020, after the regional health agency and the French biomedicine agency recommendations, our ART Center had to stop its activities in all fields as In Vitro Fertilization (IVF) for infertile couples, Fertility Preservation (FP) and Preimplantation Genetic Testing (PGT). We had to organize ourselves in a stressful environment for both patients and health care staff. We also have to suspend initiation of new cycles aimed at achieving pregnancy [1]. For those who had started treatment, after making sure they were no flu-like symptoms we gave them a choice. After understanding the potential adverse event related to COVID-19 in case of infection during pregnancy [2], patients could therefore choose between cryopreserve their embryos or receive a fresh embryo transfer. Hence, many patients were transferred before or immediately after knowledge of the COVID-19 outbreak on French territory. While the literature review on pregnancy and COVID-19 related maternal and perinatal outcomes [[3], [4], [5]], no publication has yet been published on the monitoring and follow up of patients recommended by ESHRE three weeks after embryo transfer in the context of the COVID-19 outbreak (Eshre guidance and recommencing ART treatments, 2020).
The objectives of this study were i) to evaluate the impact of the lockdown on ongoing pregnancies monitoring ii) to describe the anxiety felt by ongoing pregnant women during a period characterized at increased risk for them and during lockdown iii) to evaluate the incidence of COVID 19 infection for women who became pregnant after embryo transfer before closing our IVF center.
2 Materials and methods
2.1 Population studied
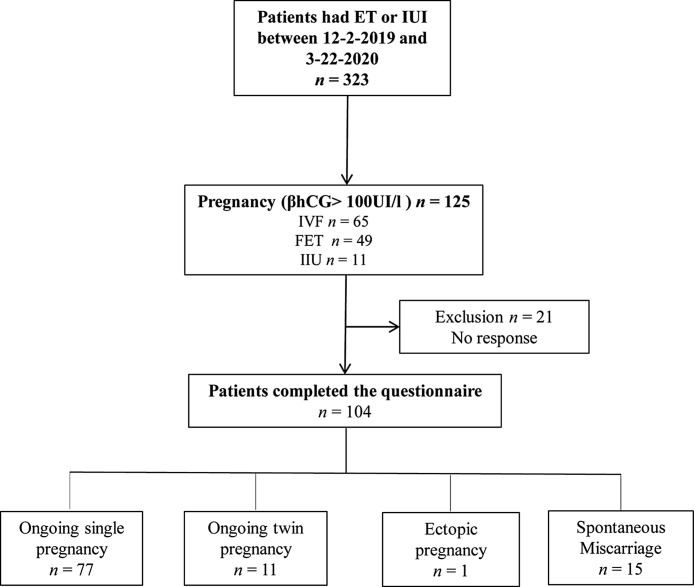
From December 2019 to 22 March 2020, 174 female-patients who became pregnant after either an IVF cycle for infertility (n = 65), an Intra Uterine Insemination (IUI) cycle (n = 11) or a frozen embryo transfer (FET) (n = 49) were retrospectively contacted according to ESHRE’s recommendations (Eshre guidance and recommencing ART treatments, 2020) by telephone to respond to a follow-up questionnaire. Twenty-one patients were excluded because they opposed to the research or underwent a miscarriage before the started date of COVID-19 outbreak in France. Finally, 104 couples were included in the study (Fig. 1 ). All couples included agreed to participate in this study and signed a written informed consent for the use of their medical data for publication. The database received authorization by the appropriate French authority (Commission Nationale de l’Informatique et des Libertés, CNIL no. 1,217,921) on February 21, 2007.
Fig. 1.
Flowchart of the study.
The study period was determined since the first case of COVID-19 had been confirmed in France (12−2-2019) until the suspension of new cycles initiation aimed at achieving pregnancy (3−22-2020). One hundred and twenty-five women who became pregnant during this study period were enrolled. Pregnancy was defined by a blood level of βhCG higher than 100 ng/mL measured three times at 48 -h intervals from the 10th day after embryo transfer.
2.2 Methods to patients’ follow-up
Our evaluation was based on a phone call interview using a specific questionnaire sheet specially developed for this study and consisted of a total of 28 items. The phone calls were performed during one week by 12 gynecologists and embryologists of our ART Centre. Questions concerning the follow-up of pregnancies focused on the following: number, place (hospital, personal physician or both) and reasons of medical consultations that occurred during lockdown, number and reasons of telemedicine medical consultations, number and place of ultrasounds examination performed, number of medical visits avoiding because of COVID-19 outbreak. To evaluate the number of women affected by COVID-19 during pregnancy, questions consisted of the following: presence of clinical manifestations of COVID-19 (cough, unusual headaches, fever, myalgia, anosmia, loss of taste), result of women tested for COVID-19 and knowledge of contact with potentially or confirmed infected individuals. To evaluate the anxiety felt by our specific pregnant population during lockdown we focused on a declarative scale with 4 levels of anxiety. With the same scale, we've been trying to determine whether the end of the lockdown could be a source of anxiety. We also evaluated the number and reasons for going out during lockdown.
2.3 Statistical analysis
Descriptive Data are presented as the mean ± standard deviations [minimum-maximum] for continuous variable and as absolute numbers (percentages) for categorical variables as appropriate. Pregnancy was defined by a blood level of βhCG higher than 100 ng/mL measured three times at 48 -h intervals from the 10th day after embryo transfer
3 Results
One hundred and twenty-five pregnant women were contacted within the study period. The response rate was of 83 % with 104 questionnaires completed. The mean age of the study population was 33.6 ± 4.1 years and the mean BMI was 24.8 ± 4.4 kg/m2. In line with our objectives data were presented only for ongoing pregnancy (n = 88) in Table 1 .
Table 1.
xxx.
| Women characteristic (n = 88) | |
|---|---|
| Age | 33.6 ± 4.1 |
| BMI (Kg/m2) | 24.8 ± 4.4 |
| Pregnancy follow-up | |
| Term of pregnancy on the day of women enrollment (WG) | 16.9 ± 4.6 [7.9−30.7] |
| Term of pregnancy at the time of lockdown (WG) | 9.9 ± 4.6 [1.7−24.1] |
| Ultrasound examination performed | 2.5 ± 1.4 [0.0−8.0] |
| Women benefited from a telemedicine consultation (%) | 35 (39.7) |
| Patients avoided a medicine consultation because of COVID-19 outbreak (%) | 10 (11.3) |
| COVID-19 infection | |
| Ongoing pregnancy with COVID-19 symptoms (%) | 10 (11.3) |
| Tested for COVID-19 | 5 |
| Positive for COVID-19 | 2 |
| Lockdown experiences | |
| Anxiety felt by lockdown (%) | |
| Any anxiety | 40 (45.5) |
| Few anxiety | 25 (28.4) |
| Mild anxiety | 11 (12.5) |
| Severe anxiety | 12 (13.6) |
| No. exits per week from home during lockdown (%) | |
| 0 | 19 (21.6) |
| 1−2 | 56 (63.6) |
| 3−4 | 8 (9.1) |
| >4 | 5 (5.7) |
| Anxiety felt by the end of lockdown (%) | |
| Any anxiety | 22 (25.0.) |
| Few anxiety | 23 (26.1) |
| Mild anxiety | 25 (28.4) |
| Severe anxiety | 28 (20.5) |
Data are expressed as mean ± SD [min-max] ; WG: weeks of gestation.
3.1 Pregnancy follow-up
The evaluation of the ongoing pregnancies (n = 88) follow-up was carried out in the first trimester of pregnancy for half of the patients and half in the second trimester with a mean pregnancy term of 16.9 ± 4.6 weeks of gestational age. Only two embryo transfers (ET) were performed between the beginning of the lockdown and the closure of our IVF centre (1 IVF-ET and 1 FET-ET). Ultrasound assessment of gestational age was performed for 87 patients either in hospital (63 patients, 72.4 %) or by a personal physician 24 patients, 27.8 %). One patient, working as a nurse, had her ultrasound canceled because she tested positive for COVID-19. More than one third of female-patients (39.7 %) benefited from medicine teleconsultation for pregnancy follow-up, written off sick renewal or for suspicion of COVID-19 related symptoms. Only ten pregnant women (11.3 %) avoided a medical visit because of the pandemic situation.
3.2 COVID-19 infection
We've documented 10 patients (11.3 %) who had symptoms related to COVID-19 after ET. Six of them report having been in contact with someone who had symptoms or tested positive. Fever and cough were the most frequent clinical manifestation recorded by pregnant women (5/10) prior to unusual headache and myalgia (4/10) and agueusie/anosmia (3/10). No severe symptoms were identified. No patient have been admitted to hospital. COVID PCR test was performed on 5 out of the 10 female-patients with symptoms. Two of them were positive (40 %) and three negative (60 %).
3.3 Lockdown experience
Most patients (85.2 %) left their homes less than twice a week. The main reasons for going out (excepting for medical appointments) were the need to go for a walk, to walk the dog or to grocery shopping. Among the 82 patients who were employed at the time of lockdown, twenty-eight patients (43.3 %) continued to work. Thirty of them teleworking (78.9 %), four patients were in health or childcare professions and continued to go to the office (7.9 %) and four (10.5 %) were teleworking and going to the office. Most of the 88 pregnant patients (73.9 %) experienced little (45.5 %) or no anxiety at all (28.4 %) by the situation related to lockdown in an epidemic context. The dispersion of patients regarding their anxiety related to the end of lockdown is more evenly distributed with about a quarter of patients in each category of feeling (any, few, mild, and severe).
3.4 Miscarriages
Among the 104 female-patients who respond to the questionnaire, 15 underwent a spontaneous miscarriage representing 14.4 % of our study population. Two of them underwent a late spontaneous miscarriage. The first one was caused by a large subchorionic hematoma with a miscarriage at 19 weeks of gestational age. The second one occurred at 18 weeks of gestational age in a context of cervical insufficiency and chorioamniotisis. This patient has also presented COVID-19 related symptoms with unusual headache, myalgia, dyspnea and diary. Her husband also had COVID-19 symptoms as diary and chills. Both have not been tested for COVID-19. No other patients have presented with COVID-19 related symptoms.
4 Discussion
As recommended by the ESHRE guidance, our study is the first to investigate the follow-up and stress for 88 pregnant women after ART during COVID-19 outbreak. This follow up shows that pregnant women did not change their physician visits for fear of being contaminated by the SARS CoV-2. Furthermore, it appears that Coronavirus epidemic has created no or few additional stresses for 77 % of pregnant women since the lockdown started and for which the patients have been compliant with less than 2 exits per week for most of them. We report a miscarriage rate of 14.4 % (n = 15) with a single miscarriage, related to the symptoms of COVID 19 but not tested.
France, like many other countries, saw the threat of the COVID 19 epidemic move closer to lockdown on March 17, 2020. The population has therefore had access to a large amount of information through television, radio, written and web media coverage. Every day the population could follow the number of new COVID 19 cases and the number of deaths increasing exponentially until the epidemic peak on at the beginning of May 2020. This situation can be potentially very stressful. In this context one can wonder if the obstetrical follow-up is indeed the one recommended. Many pregnant women do not go visit their physician due to the concerns that they may be exposed to the SARS CoV-2 in the hospital environment or and the way to the hospital. We report that the follow-up of pregnant patients was not disrupted by the pandemic context and that only 11.3 % of patients avoided a consultation. The context made it possible to develop teleconsultations with more than one out of three patients (39.7 %) having benefited from this new system.
Few published information are known on the psychological impact and mental health of the general population during the COVID 19 epidemic. Wang et al. related for the general public in China a psychological impact of the outbreak as moderate or severe for 53.8 % of respondents, 16.5 % reported moderate to severe depressive symptoms, 28.8 % reported moderate to severe anxiety symptoms and 8.1 % reported moderate to severe stress levels [6]. Our study population is distinct because it included pregnancies obtained after IVF. Ordinarily, both criterions taken separately can be an element of stress. In fact, pregnancy is a time of significant change which can elevate stress levels and increase response to external sensor [7]. This stress can lead to adverse perinatal outcomes such as perinatal depression, pregnancy induced hypertension and pre-eclampsia with prolonged maternal stress associated with both preterm birth and low birth weight [8]. Secondarily, pregnancies obtained in our study resulting from fresh or frozen ET after IVF cycles. It is well known that IVF procedure can be physically rigorous and emotionally difficult and consequently adds stress to an already complicated situation [9,10]. In our study we report that the majority of patients (77.3 %) have little or no anxiety about the lockdown and the outcome of their pregnancy. Indeed, they were aware of the outbreak and took their precaution by respecting the rules of lockdown with less than 2 exits per week for the majority of them (86.4 %). However, they felt more anxious about the perspective of the end of lockdown with half of them reporting being moderately or very anxious. It could be interesting to study the number of postnatal depression in our population in order to confirm the anxiety caused by the outbreak and the reduction in physical activity related to it [11].
Physiological changes during pregnancy, such as reduced functional residual volumes, diaphragm elevation, and altered cell immunity lead to increased susceptibility to viral infection and worse outcomes (Weinberger et al., 1980; Zhao et al., 2020). Pregnant women would therefore represent a high-risk population during infectious disease outbreaks. However, there is no yet evidence from other severe coronavirus infections such as SARS Cov and MERS Cov that pregnant women are more susceptible to infection with SARS CoV-2. In our study, we found that 11.3 % of pregnant women presented symptoms related to COVID-19. However, only one had been tested positive for. Whereas the virus nucleic acid RT‐PCR test has become the current standard diagnostic method for the diagnosis of COVID‐19 it has been shown that there are some numbers of false negatives [14]. A larger study with the results of serological tests could corroborate the rate of infection in pregnant women.
Although data are limited and constantly being updated, the clinical characteristics reported in pregnant women with confirmed COVID-19 infection are like those reported for non-pregnant adult’s patients with confirmed COVID-19 infection with fewer, cough, and dyspnea. However, pregnant women with COVID-19 infection can also had adverse maternal complications as such pneumonia and severe respiratory complications known in others at risk population [15,16]. In our study, women were infected with flu like syndrome and none presented more severe symptoms or were hospitalized in ICU.
When analyzing the data on first trimester recovered for SARS or MERS infection caused by two others Coronavirus (SARS Cov and MERS Cov), there were some cases of miscarriages. However series were very limited with four of the 7 patients had spontaneous miscarriage for SARS infection [17] and a single case of a woman with MERS in the first trimester has been reported [18]. Di mascio et al. in his systematic review and metanalysis, found in the overall population of pregnancies infected with CoV infections (including COVID-19) a rate of miscarriages around 39.1 % [3]. This rate appears to be a slightly higher than the ∼20 % rate of spontaneous abortion affecting pregnant women in the general population [19]. In the present study for our specific ART population we found a miscarriage rate of 14.4 % and just one of them related to COVID-19 symptoms without being tested for.
5 Conclusion
We focused on embryo transfer performed since the first two cases diagnosed in France on December 2, 2020. We wanted to carry out an initial follow-up assessment of pregnant women in the peak of COVID 19 outbreak. The epidemic context did not disrupt the medical monitoring of pregnancies and we did not recover an increased rate of miscarriage after ART. None of the patients who had COVID-related symptoms presented with a severe clinical manifestations. Surprisingly, pregnant women were psychologically able to experience the lockdown. This first data have help to inform and reassure both patients and the health care team. Due to the short duration of the investigation period, a more follow up study should be done to evaluate the psychological and physical health of pregnant women after delivery and his newborn babies.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
The authors thank the staff members at the Reproductive Biology and Clinical Units of the Antoine Béclère Hospital (Clamart, France). We are grateful to couples-patients who consent to the use of their medical data.
References
- 1.ASRM; 2020. Patient management and clinical recommendations during the coronavirus (COVID-19) pandemic - updated March 30.https://www.asrm.org/news-and-publications/covid-19/statements/patient-management-and-clinical-recommendations-during-the-coronavirus-covid-19-pandemic/ [Internet]. Available from: [Google Scholar]
- 2.Breslin N., Baptiste C., Gyamfi-Bannerman C., Miller R., Martinez R., Bernstein K., et al. COVID-19 infection among asymptomatic and symptomatic pregnant women: two weeks of confirmed presentations to an affiliated pair of New York City hospitals. Am J Obstet Gynecol MFM. 2020 doi: 10.1016/j.ajogmf.2020.100118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Di Mascio D., Khalil A., Saccone G., Rizzo G., Buca D., Liberati M., et al. Outcome of Coronavirus spectrum infections (SARS, MERS, COVID 1 -19) during pregnancy: a systematic review and meta-analysis. Am J Obstet Gynecol MFM. 2020 doi: 10.1016/j.ajogmf.2020.100107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mullins E., Evans D., Viner R.M., O’Brien P., Morris E. Coronavirus in pregnancy and delivery: rapid review. Ultrasound Obstet Gynecol. 2020;55:586–592. doi: 10.1002/uog.22014. [DOI] [PubMed] [Google Scholar]
- 5.Zaigham M., Andersson O. Maternal and perinatal outcomes with COVID-19: a systematic review of 108 pregnancies. Acta Obstet Gynecol Scand. 2020 doi: 10.1111/aogs.13867. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S., et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health. 2020;17(5) doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Littleton H.L., Bye K., Buck K., Amacker A. Psychosocial stress during pregnancy and perinatal outcomes: a meta-analytic review. J Psychosom Obstet Gynaecol. 2010;31(4):219–228. doi: 10.3109/0167482X.2010.518776. [DOI] [PubMed] [Google Scholar]
- 8.Baibazarova E., van de Beek C., Cohen-Kettenis P.T., Buitelaar J., Shelton K.H., van Goozen S.H.M. Influence of prenatal maternal stress, maternal plasma cortisol and cortisol in the amniotic fluid on birth outcomes and child temperament at 3 months. Psychoneuroendocrinology. 2013;38(6):907–915. doi: 10.1016/j.psyneuen.2012.09.015. [DOI] [PubMed] [Google Scholar]
- 9.Geisler M., Meaney S., Waterstone J., O’Donoghue K. Stress and the impact on the outcome of medically assisted reproduction. Eur J Obstet Gynecol Reprod Biol. 2020;248:187–192. doi: 10.1016/j.ejogrb.2020.03.006. [DOI] [PubMed] [Google Scholar]
- 10.Tuncay G., Yıldız S., Karaer A., Reyhani I., Özgöcer T., Ucar C., et al. Stress in couples undergoing assisted reproductive technology. Arch Gynecol Obstet. 2020;301:1561–1567. doi: 10.1007/s00404-020-05549-8. (2020) [DOI] [PubMed] [Google Scholar]
- 11.Haßdenteufel K., Feißt M., Brusniak K., Lingenfelder K., Matthies L.M., Wallwiener M., et al. Reduction in physical activity significantly increases depression and anxiety in the perinatal period: a longitudinal study based on a self-report digital assessment tool. Arch Gynecol Obstet. 2020;302:53–64. doi: 10.1007/s00404-020-05570-x. (2020) [DOI] [PubMed] [Google Scholar]
- 14.Corman V.M., Landt O., Kaiser M., Molenkamp R., Meijer A., Chu D.K., et al. Detection of 2019 novel coronavirus (2019-nCoV) by real-time RT-PCR. Euro Surveill. 2020;25(3) doi: 10.2807/1560-7917.ES.2020.25.3.2000045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chen H., Guo J., Wang C., Luo F., Yu X., Zhang W., et al. Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: a retrospective review of medical records. Lancet. 2020;395(10226):809–815. doi: 10.1016/S0140-6736(20)30360-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Liu Y., Chen H., Tang K., Guo Y. Clinical manifestations and outcome of SARS-CoV-2 infection during pregnancy. J Infect. 2020 doi: 10.1016/j.jinf.2020.02.028. Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wong S.F., Chow K.M., Leung T.N., Ng W.F., Ng T.K., Shek C.C., et al. Pregnancy and perinatal outcomes of women with severe acute respiratory syndrome. Am J Obstet Gynecol. 2004;191(1):292–297. doi: 10.1016/j.ajog.2003.11.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Alfaraj S.H., Al-Tawfiq J.A., Memish Z.A. Middle East Respiratory Syndrome Coronavirus (MERS-CoV) infection during pregnancy: report of two cases & review of the literature. J Microbiol Immunol Infect. 2019;52(3):501–503. doi: 10.1016/j.jmii.2018.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sedgh G., Bearak J., Singh S., Bankole A., Popinchalk A., Ganatra B., et al. Abortion incidence between 1990 and 2014: global, regional, and subregional levels and trends. Lancet. 2016;388(10041):258–267. doi: 10.1016/S0140-6736(16)30380-4. [DOI] [PMC free article] [PubMed] [Google Scholar]