Abstract
Introduction
There was a low level of pandemic preparedness in South Asia, but the region has done well in mounting an appropriate response to the coronavirus disease 2019 (COVID-19) pandemic. The rate and proportion of deaths attributed to COVID-19 are lower despite case surges similar to the rest of the world.
Results
The COVID-19 pandemic has revealed the glaring vulnerabilities of the health system. In addition, the high burden of non-communicable diseases in South Asia multiplies the complexities in combating present and future health crises. The advantage offered by the younger population demographics in South Asia may not be sustained with the rising burden of non-communicable diseases and lack of priority setting for improving health systems.
Conclusion
The COVID-19 pandemic has provided a window for introspection, scaling up preparedness for future pandemics, and improving the health of the population overall.
Keywords: South Asia, COVID-19, SARS-CoV-2
Introduction
South Asia comprises eight countries – Afghanistan, Bangladesh, Bhutan, India, Maldives, Nepal, Pakistan and Sri Lanka – and is home to one-fifth of the world’s population. This region accounts for 21% of the reported total number of cases of coronavirus disease 2019 (COVID-19) and 11% of COVID-19 deaths worldwide (Menon, 2020). Initial projections placed South Asia at even higher risk than observed for deaths and catastrophe due to the high population density, high burden of comorbidities, vast socio-economic vulnerabilities and poor health system infrastructure. The concern that South Asians may be at higher risk of poor outcomes of COVID-19 was supported by data from the UK Intensive Care National Audit and Research Centre, showing that one-third of patients with COVID-19 admitted to critical care units were from Black, Asian and Minority Ethnic groups (Holman et al., 2020). A prospective cohort study reported that South Asians had a higher mortality rate compared with people of White ethnicity, and this enhanced risk was mediated substantially by diabetes (18% of the increased relative risk of mortality was attributed to diabetes) (Harrison et al., 2020). The age, sex and multi-variable-adjusted hazard ratio for COVID-19-related mortality by risk factors in people with type 1 and type 2 diabetes was found to be 2.29 for people of Asian origin in a study performed in England (Samaranayake, 2020).
A dual burden of non-communicable and communicable diseases confronts the region and is exemplified by diabetes and COVID-19. The poor public health infrastructure, coupled with a lack of trained human resources to deal with non-communicable diseases (e.g. diabetes), has exacerbated the inequities in health care in these countries (Samaranayake, 2020). For example, cardiovascular diseases (CVDs) affect South Asians at a younger age than other ethnicities (UNICEF Regional Office for South Asia, 2020). There has been an increase in the disability-adjusted life years from CVDs by nearly two- to three-fold in the last 25 years. As a result, South Asia is struggling to meet the sustainable development goals (Counahan et al., 2020).
Search strategy and selection criteria
Databases: Google Scholar, Google
Free-text search terms: South Asia, COVID, pandemic, SARS-CoV
Filters: Year 2020
Pandemic preparedness in South Asia
South Asian countries generally had inadequate pandemic preparedness as measured by the Global Health Security Index (Figures S1 and S2, see online supplementary material) (Global Health Security Index, n.d.). The Global Health Security Index scores (highest possible score is 100) for South Asian countries were: 46.5 for India, 40.3 for Bhutan, 35.5 for Pakistan, 35.1 for Nepal, 35.0 for Banglasdesh, 33.9 for Sri Lanka, 33.8 for the Maldives and 32.3 for Afghanistan. Each country in the region had different preparedness levels to tackle a pandemic, with India being best prepared and Afghanistan being least prepared. Details regarding the components of pandemic preparedness are provided in the online supplementary material.
There are some unique attributes related to pandemic preparedness in South Asia (Table 1, Table 2). First, the South Asian nations do not have robust national plans, guidelines or laws that account for the surveillance and control of multiple zoonotic pathogens of concern for public health. Antibiotics are easily available in most of these nations without prescription and can contribute to antimicrobial resistance. Second, most nations in the region have a poor allocation of resources to health security (4.4% of Gross Domestic Product) (Counahan et al., 2018). Third, although laboratory systems test some pathogens of importance, they cannot test them all. Fourth, following a meeting of the South Asian leaders, several cooperative activities have commenced, including a US$ 22 million COVID-19 Emergency Fund. Fifth, all of the South Asian countries have a shortage of health workers and have less than one field epidemiologist per 200,000 people (Haidar, 2020). Finally, urban migration and forced displacement have a long history in South Asia, and this escalated in the postcolonial decades (Global Fund, 2020).
Table 1.
Indicators of Global Health Security Index of South Asian countries.entheses)
| Countries | Prevention of the emergence or release of pathogens | Early detection and reporting of epidemics of potential international concern | Rapid response to, and mitigation of, the spread of an epidemic | Sufficient and robust health sector to treat the sick and protect health workers | Commitments to improving national capacity, financing and adherence to norms | Overall risk environment and national vulnerability to biological threats | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Rank | Score | Rank | Score | Rank | Score | Rank | Score | Rank | Score | Rank | Score | Rank | Score | |
| Afghanistan | 130 | 32.3 | 140 | 23.5 | 77 | 44.8 | 161 | 23.6 | 102 | 21 | 52 | 56.3 | 191 | 23.3 |
| Bangladesh | 113 | 35 | 116 | 27.3 | 59 | 50.9 | 165 | 23.1 | 132 | 14.7 | 74 | 52.5 | 142 | 44 |
| Bhutan | 85 | 40.3 | 83 | 35.5 | 85 | 42.8 | 78 | 42 | 78 | 27.9 | 145 | 39.7 | 90 | 56.9 |
| India | 57 | 46.5 | 87 | 34.9 | 67 | 47.4 | 32 | 52.4 | 36 | 42.7 | 100 | 47.7 | 103 | 54.4 |
| The Maldives | 121 | 33.8 | 154 | 21.8 | 138 | 25.5 | 83 | 40.2 | 117 | 18.1 | 117 | 45.5 | 79 | 58.3 |
| Nepal | 111 | 35.1 | 58 | 43.7 | 150 | 22 | 79 | 41.9 | 76 | 28.1 | 167 | 33.5 | 137 | 44.7 |
| Pakistan | 105 | 35.5 | 136 | 24.1 | 91 | 41.7 | 88 | 38.7 | 107 | 19.9 | 86 | 49.7 | 160 | 38.7 |
| Sri Lanka | 120 | 33.9 | 135 | 24.2 | 82 | 43 | 145 | 26.4 | 122 | 16.9 | 137 | 41.7 | 91 | 56.7 |
Table 2.
Indicators influencing pandemic preparedness in South Asian countries.
| Surveillance | Resource allocation | Emergency preparedness and response act | Focus on vulnerable groups | Engagement with the private sector | |
|---|---|---|---|---|---|
| India | Integrated Disease Surveillance Program; Electronic reporting at both national and international level | Poor allocation to surveillance and preparedness | India has a national public health emergency preparedness and response plan | India’s national disaster management guidelines do not focus on vulnerable groups | Public–private partnership for comprehensive patient care as well as the development of a vaccine |
| Bhutan | Royal Centre for Disease Control has a national early warning, alert and response surveillance system | Bhutan has a health emergency and disaster contingency plan | Plan includes the vulnerable population | No mention of private partnerships for an emergency outbreak | |
| Pakistan | Pakistan has event-based surveillance | Pakistan does not have a prompt system for emergency preparedness and response | Either direct cash or postal services were utilized to maintain social distancing | Private transport companies supply necessities during a national disaster | |
| Nepal | The surveillance system developed is for insect-borne diseases, which can be tailor-made for COVID-19 surveillance | Rapid Response Teams(RRT) are functional | Establishment of information desks, camps and social mobilization networks | The private sector is not usually involved | |
| Afghanistan | Afghanistan does not have an event-based surveillance system | Public health emergency response plan | To reduce poverty-related implications, the World Bank approved approximately 300 million grants (Cancho and Pradhan, 2020) | The strategic framework (2018–2028) developed prioritizes engagement with the private sector | |
| The Maldives | The Maldives does not have event-based surveillance and analysis for infectious disease | The Maldives does not have a national public health emergency response plan | Provided relief on payment of utility bills either by deferring payments or through subsidies (Haidar, 2020) | Coordination of multiple sectors; no specific engagement mechanisms | |
| Sri Lanka | Routine disease surveillance system | Comprehensive disaster management programme (SAARC Disaster Management Centre, n.d.) | Government provided support to private sector businesses to cover the wage payments of their employees | No mechanisms for engagement with the private sector |
COVID-19, coronavirus disease 2019.
This table shows pandemic preparedness in South Asian countries with respect to surveillance, resource allocation, emergency preparedness and response act, focus on vulnerable groups, and engagement with the private sector.
South Asian countries initiated interventions as early as February and March 2020 to tackle the COVID-19 pandemic. All countries put measures in place to restrict incoming foreigners, did not permit foreign travel, air travel was suspended, and those who travelled to other countries were expected to quarantine for the number of days specified by the country. The details of the timeline and extent of early response in the region are provided in Table 3 .
Table 3.
Timeline and extent of early response against the coronavirus disease 2019 (COVID-19) pandemic in South Asian countries.
| Country | Airport screening initiated | Quarantine initiation | Lockdown initiation | Duration of lockdown |
|---|---|---|---|---|
| India | 31 January 2020 | 26 January 2020 | 25 March 2020 | 75 days |
| Pakistan | 24 January 2020 | 28 March 2020 | No national lockdown | – |
| Bhutan | 6 March 2020 | 16 March 2020 | 24 March 2020 | 21 days |
| The Maldives | 26 January 2020 | 10 March 2020 | 16 April 2020 | – |
| Bangladesh | 22 January 2020 | 9 March 2020 | 26 March 2020 | 50 days |
| Sri Lanka | 27 January 2020 | 13 March 2020 | 18 March 2020 | 52 days |
| Nepal | End of February 2020 | Mid-February 2020 | 19 March 2020 | – |
| Afghanistan | 25 January 2020 | – | 28 March 2020 | – |
This table shows the timeline of when various interventions were adopted in each country as a measure to reduce the number of people contracting COVID-19, nationally and internationally.
Despite poor pandemic preparedness, South Asian countries mounted a reasonably good response against the COVID-19 crisis (Figures S3–S5, see online supplementary material).
On 15 March 2020, leaders of the region met and proposed plans to combat severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) through the South Asian Association for Regional Cooperation (SAARC) during a video press conference arranged by the Indian Prime Minister Narendra Modi. India took the lead and created a ‘COVID-19 Emergency Fund’ that would be funded by voluntary contributions from the region, and offered US$ 10 million as an initial offering from India. With a corpus fund of US$ 21 million donated by the nations in the first round, work has started on a regional strategy to fight the pandemic (SAARC Disaster Management Centre, n.d.). The SAARC Disaster Management Centre has been set up in India to provide policy advice, technical support on system development, capacity-building services, and training for holistic management of disasters in the region.
Epidemiology of COVID-19 in South Asia
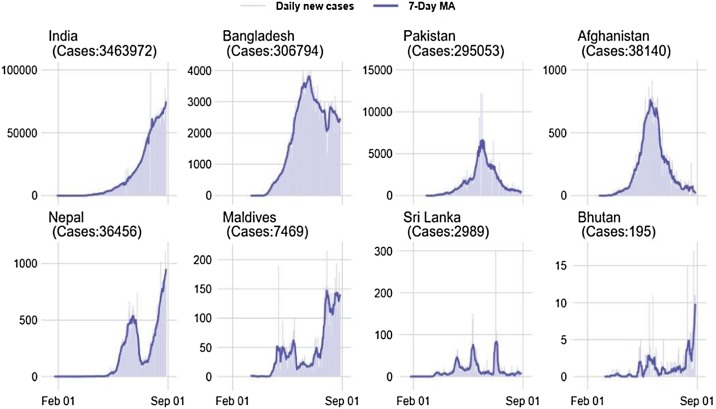
Currently, the total number of cases and deaths is increasing in South Asia, whereas countries that had earlier peaks currently have a lower number of cases (Johns Hopkins University of Medicine, n.d.). This is depicted in Fig. 1, Fig. 2 . In India, the highest number of cases to date occurred on 9 October 2020 with 387,973 cases. Overall, 17.9% of deaths have been among people with comorbidities (Roser, 2020), 90% were aged >40 years and 69% were males. The case fatality ratio (CFR) is higher among females, and the number of cases of COVID-19 is higher among males (HT Correspondent, 14 October 2020; Sharma, 2020). At the time of writing, there had been 812,345 active cases and 108,334 COVID-19-related deaths in India (Ministry of Health and Family Welfare, Government of India, 2020). There are 5111 cases per million population in India, the CFR is 1.5 (Kaul, 2020, 2020, Thakur, 2020) and approximately 6.3 million people have recovered (Zhang et al., 2020). The country is testing at the rate of 277,486 tests per million people (World Health Organization, 2020), which has increased from a few hundred in the beginning to the current rate; initially, the pace was slow due to political will, capacity issues and operational feasibility. Later, measures to improve testing rates were put in place by acquiring additional testing kits and approving a higher number of laboratories (Global Health Security Index, n.d.).
Fig. 1.
Coronavirus disease 2019: daily confirmed cases and 7-day average in South Asian countries from 1 February to 1 September 2020 (total confirmed cases in parentheses).
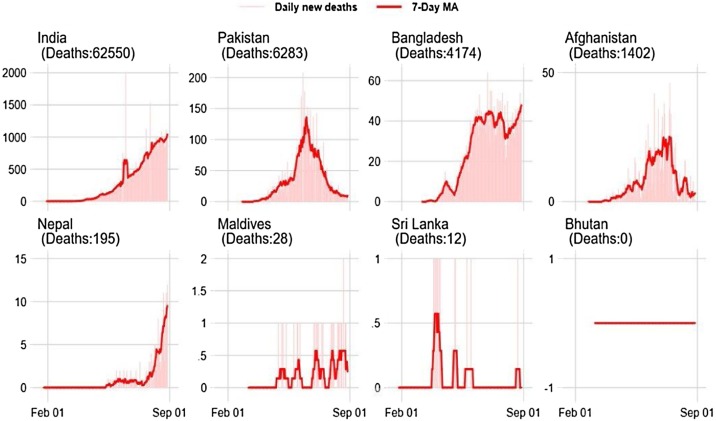
Fig. 2.
Coronavirus disease 2019: daily confirmed deaths and 7-day average in South Asian countries from 1 February to 1 September 2020 (total confirmed deaths in par
In Pakistan, there was a spike in the number of cases on 14 June 2020, with the majority of cases in Punjab and the highest mortality rate in Khyber Pakhtunkhwa (HT Correspondent, 13 October 2020). In the Maldives, the number of cases spiked on 3 August 2020 with 215 cases (HT Correspondent, 13 October 2020). The total number of cases per million population is highest in the Maldives (approximately 20,089 per million population) and lowest in Sri Lanka (approximately 216 cases per million population). The number of cases spiked at 4019 in Bangladesh on 3 July 2020, and at 519 cases in Sri Lanka on 7 October 2020. In Nepal, the highest number of cases was 5008 on 11 October 2020, and the peak in Afghanistan occurred on 16 May 2020 with 1063 cases (Roser et al., 2020) (Fig. 1, Fig. 2, and Figure S6, see online supplementary material).
Among the South Asian countries, the total number of cases is highest in India (705,3806 cases) and lowest in in Bhutan (316 cases). In almost all countries, more males have been affected compared with females, and the total number of deaths has been highest in the elderly.
As seen in Table 4 , Bhutan has the highest recovery rate of 96%, followed by Pakistan at 95%. Sri Lanka has the lowest recovery rate at 72%. Synchronous to the identification of cases, India has conducted the greatest number of tests per million population. The Maldives has the second-best test performance, with 107,335 tests performed per million ppulation. Afghanistan has performed the lowest number of tests per million population (2591 tests per million population) (Table 4).
Table 4.
Population, morbidity and mortality statistics related to coronavirus disease 2019 for South Asian countries.
| Country | Population in millions | Active cases | Total confirmed cases | Cases per million population | Deaths | Fatality rate | Death per million population | Recovered | Recovery rate | Total tests performed | Tests per million |
|---|---|---|---|---|---|---|---|---|---|---|---|
| India | 1347.1 | 812,345 | 7,053,806 | 5111.6 | 108,334 | 1.5 | 79 | 6,383,441.0 | 90.4 | 121,567,138 | 366,648 |
| Pakistan | 221.5 | 9209.0 | 318,932 | 1444 | 6570 | 2.06 | 30 | 305,395.0 | 95.7 | 3,975,596 | 17,900 |
| Bangladesh | 164.9 | 79917 | 377,073 | 2290 | 5500 | 1.4 | 33 | 297,449 | 78.8 | 2,112,448 | 12,790 |
| Nepal | 29.2 | 36,367 | 105,684 | 3627 | 614 | 0.5 | 21 | 80,954 | 76.6 | 1,221,038 | 41,694 |
| The Maldives | 0.5 | 1147 | 10,586 | 20,089 | 34 | 0.32 | 63 | 9880 | 93.3 | 150,743 | 277,486 |
| Afghanistan | 39.1 | 5159 | 39,799 | 1022 | 1477 | 3.7 | 38 | 33,354 | 83.8 | 115,720 | 2954 |
| Sri Lanka | 21.4 | 1800 | 4628 | 216.0 | 13 | 0.2 | 1 | 3357 | 72.5 | 348,909 | 16,274 |
| Bhutan | 0.8 | 316 | 306 | 397.0 | 0 | 0.0 | <1 | 294 | 96.0 | 154,864 | 200,071 |
| Average | 228.06 | 118,282.5 | 988,851.8 | 4274.5 | 14,699 | 1.21 | 33.125 | 889,265.5 | 85.8 | 16,205,807 | 116,977.1 |
Lower observed mortality in South Asian countries
In terms of mortality, India has seen the highest number of deaths due to COVID-19 (108,334 deaths), followed by Pakistan and Bangladesh (6570 and 5500 deaths, respectively). In terms of CFR, however, which is the total number of deaths from all causes, Pakistan has the highest rate (2.06) followed by India (1.5). Bhutan has recorded no deaths due to COVID-19 (Figure S7, see online supplementary material). Deaths per million population is a better indicator to assess the overall risk of death attributed to COVID-19. With the exception of the Maldives, the remaining South Asian nations have managed to keep deaths below one per million population (Figure S8, see online supplementary material).
Almost all of the South Asian countries are densely populated, but to date they seem to have avoided the high mortality rates seen in Europe and elsewhere. This may be explained as follows:
-
•
South Asian countries have a younger population compared with other countries, with an average age of people in South Asia of 24.4 years (Table S1, see online supplementary material). As the number of COVID-related deaths disproportionately affects older people, South Asian countries may have a unique advantage (Zhang et al., 2020).
-
•
The COVID pandemic arrived in South Asia at a much later stage compared with other countries. As such, the South Asian countries may have been able to learn from countries that had early peaks (Deepak, 2020), and therefore achieved better preparation in terms of the public health response. For example, this could have resulted in a lower viral load due to more people wearing masks.
-
•
Lack of prompt reporting of deaths may have resulted in underestimation of the number of deaths. However, the underestimation is unlikely to be substantial.
-
•
Early lockdown and timely intervention for prevention and response. Emerging evidence suggests that most of these countries implemented timely lockdowns and may have had an advantage in terms of an overall reduction in the number of deaths. Specifically, this lag time helped the South Asian countries to step up preparedness for any potential surge in cases beyond the routine capacity of the hospitals in these countries (Anonymous, 2020).
-
•
Potential role of cross-reactive immunity in reducing disease severity. Detailed scientific evaluations should be undertaken in these countries to determine if cross-reactive immunity plays a role in reducing severity and deaths. In particular, studies should be performed to examine if there is any role for the potential natural selection of SARS-CoV-2 by pre-existing cross-reactive T-cell immunity (Zhang et al., 2020). The presence of cross-reactive T cells, presumably from prior coronavirus infections, can attenuate disease severity. There are also other hypotheses which implicate some genetic advantage for South Asians (HT Correspondent, 14 October 2020). Emerging evidence suggests that asymptomatic and mildly symptomatic patients have high SARS-CoV-2-specific cytotoxic T-cell responses (Chen and Wherry, 2020).
South Asian countries are now easing lockdowns despite rising case numbers (Mondeaux, 2020). Healthcare facilities and hospitals are stretched due to the increase in the number of cases (Mangi and Devnath, 2020). It has been reported that testing levels in Pakistan and Bangladesh have fallen dramatically (Menon, 2020). Bangladesh did not act quickly during the early stages of the pandemic, which is thought to be one of the reasons why case numbers are now soaring. In addition, early interventions were not implemented very strictly (Mondeaux, 2020).
The lower mortality rate in South Asian countries may not be sustainable over the long term. First, more than half of deaths occur in people with non-communicable diseases. The spread of infection among people with comorbidities over the long term may increase mortality. A systematic literature review focusing on South Asian populations found that the mortality rate was higher in those with COVID-19 who also had type 1 or type 2 diabetes. This is another reason why the reported low mortality rate can only be an exaggerated way to show that the pandemic response is better (Deepak, 2020).
Conclusions and the way forward
The COVID-19 pandemic has exposed the vulnerabilities of the South Asian region. The region is fraught with the burgeoning double burden of communicable and non-communicable diseases (Bhatnagar et al., 2019), limited or low access to quality health care, widespread poverty and malnourishment. The South Asian countries have nevertheless shown much grit and determination to fight the pandemic with harsh but proactive lockdown measures in the early phase of the pandemic. These low-and-middle-income countries with large populations did not hesitate to lock down manufacturing units and other non-essential businesses, and prohibit religious and social gatherings (Haidar, 2020).
COVID-19 has had a devastating effect on the economies of the South Asian countries. It is speculated that they will shrink for the first time in four decades. This will affect the livelihoods and well-being of the people. This issue is compounded as international trade came close to a standstill during the pandemic. This could lead to an estimated 132 million people being pushed into extreme poverty, and will widen inequalities, including an increase in food insecurity and poor health. These hurdles reverse the gains made by these countries towards achievement of the sustainable development goals (World Health Organization, 2001). There is a demographic advantage of the younger population in South Asia, which has resulted in low overall mortality in the region. However, poor pandemic preparedness has exposed the weak health systems and broad disparities between these countries. In the long term, the burden of non-communicable diseases coupled with inadequate primary health systems may contribute to higher rates of mortality and morbidity as a result of the COVID-19 pandemic.
South Asian governments have achieved remarkable success during the pandemic despite the challenges. The lack of a substantial public health infrastructure and human resources was evident, and there is a need to strengthen the public health infrastructure. The region is already witnessing collateral damage of the weak health systems due to disruption of their routine functioning. A reduction in immunization rates, screening and treatment of other diseases (e.g. tuberculosis) has reversed the gains of many years (Global Fund, 2020). Even in countries that have developed strong systems, such as the Integrated Disease Surveillance Programme in India, several aspects of health security are missing. With the threat of future pandemics looming, there is a need for South Asia to invest heavily in building strong and resilient health systems. The region must develop a plan for health security with reasonable financial allocations (Haidar, 2020), and collaborate for emergency action. Regional cooperation in terms of medicines, healthcare equipment, and other essential goods and services can be strengthened by pooling resources and sharing acceptable practices in digital technologies. Regional collaboration can improve public health infrastructure and efficiency, including, but not limited to, international helplines; health portals; online disease surveillance systems; telemedicine; and the development and manufacture of affordable diagnostics, vaccines and drugs.
Overburdened or untrained healthcare staff in addition to the unregulated private sector warrant prioritization of the implementation of universal health coverage in the South Asian countries. Greater investment in educating, upskilling and employing healthcare staff will ensure better handling and management of future pandemics. The region must act on overwhelming evidence from the World Health Organization, 2001, World Health Organization, 2016) that investment in public health is a prerequisite for spurring economic growth. This should be initiated by evaluating the current capacities and priorities for pandemic preparedness, and planning and addressing them. There is a need for the development of national plans with timely revisions with the advice of the public and private sectors, and incorporation of best practices in pandemic planning.
While battling the COVID-19 crisis, there is a sense of urgency to prepare for future pandemics. This requires strong leadership and great political will to allocate substantial resources to prepare for future pandemics. Building a strong regional plan for universal health coverage can enhance social protection to secure livelihoods as well as mitigate potential deaths among the poor and vulnerable. The region needs to scale up the existing social ‘safety nets’ rapidly, such as cash transfers for food. The success of such programmes is demonstrated in Bangladesh (François et al., 2020), by the National Rural Employment Guarantee Act in India, and by the Benazir Income Support Programme–Ehsaan emergency cash programme in Pakistan (Kamran, 2020). Further, there should be inclusive, sustainable urban spaces and mobility. There is a need to improve international cooperation to recover from the COVID-19 crisis. At the same time, regional cooperation between the South Asian countries can help to alleviate the existing challenges. Efforts such as the SAARC Food Bank can be strengthened and reconfigured as these policy strategies promote food security. Similar cooperative strategies are required to fight climate change and prevent future pandemics. In fighting the COVID-19 pandemic, the South Asian countries have also resorted to the use of online portals, social media, working from home, online learning, direct benefit transfers, delivery of health services through ‘virtual doctors’, deploying facial recognition, and use of thermal scanners for identification of infected people (United Nations Economic and Social Commission for Asia and the Pacific, 2020). Investing in and strengthening the use of digital technology, information technology and data systems in South Asia can help to address public health challenges in the post-COVID-19 era.
Competing interests
None declared.
Funding
This work was supported by the Wellcome Trust/DBT India Alliance Fellowship (Grant No. IA/CPHI/14/1/501499) awarded to Dr Giridhara R. Babu.
Ethical approval
Not required.
Footnotes
Supplementary material related to this article can be found, in the online version, at doi:https://doi.org/10.1016/j.ijid.2020.12.048.
Appendix A. Supplementary data
The following is Supplementary data to this article:
References
- Anonymous . 2020. Under-reporting, young population: the mystery behind India’s low Covid-19 death rate, News 18, 11 October.https://www.news18.com/news/india/under-reporting-young-population-the-mystery-behind-indias-low-covid-19-death-rate-2951321.html Available at: [Google Scholar]
- Bhatnagar T., Kaur P., Kumaraswami V. Neglected tropical diseases – East Asia. Cham: Springer; 2019. Links between the epidemiology and control of noncommunicable diseases and neglected tropical diseases in Asia; pp. 149–173. [Google Scholar]
- Cancho C.A., Pradhan T. World Bank; Washington, DC: 2020. Mitigating the poverty implications of COVID-19 in Afghanistan.https://blogs.worldbank.org/endpovertyinsouthasia/mitigating-poverty-implications-covid-19-afghanistan Available at: [Google Scholar]
- Chen Z., Wherry E.J. T cell responses in patients with COVID-19. Nat Rev Immunol. 2020;20:529–536. doi: 10.1038/s41577-020-0402-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Counahan M., Khetrapal S., Parry J., Servais G., Roth S. Asian Development Bank; Mandaluyong: 2018. Investing in health security for sustainable development in Asia and the Pacific: managing health threats through regional and intersectoral cooperation.https://www.adb.org/sites/default/files/publication/446656/sdwp-056-regional-health-security.pdf Available at: [Google Scholar]
- Deepak N. 2020. The COVID-19 paradox in South Asia. The Hindu, 24 April.https://www.thehindu.com/opinion/lead/the-covid-19-paradox-in-south-asia/article31417806.ece Available at: [Google Scholar]
- François G., Imbert C., Orkin K. Social protection response to the COVID-19 crisis: options for developing countries. Oxford Rev Econ Pol. 2020;36(Suppl. 1):S281–96. [Google Scholar]
- Global Fund . Global Fund; Geneva: 2020. Mitigating The impact of COVID-19 on countries affected by HIV, tuberculosis and malaria.https://www.theglobalfund.org/media/9819/covid19_mitigatingimpact_report_en.pdf Available at: [Google Scholar]
- Haidar S. 2020. Coronavirus | South Asia remains an outlier in infections. The Hindu, 19 April.https://www.thehindu.com/news/national/coronavirus-south-asia-remains-an-outlier-in-infections/article31378180.ece Available at: [Google Scholar]
- Harrison E.M., Docherty A.B., Barr B., Buchan I., Carson G., Drake T.M. 2020. Ethnicity and outcomes from COVID-19: the ISARIC CCP-UK prospective observational cohort study of hospitalized patients.https://ssrn.com/abstract=3618215 Available at: [Google Scholar]
- Holman N., Knighton P., Kar P., O’Keefe J., Curley M., Weaver A. Risk factors for COVID-19-related mortality in people with type 1 and type 2 diabetes in England: a population-based cohort study. Lancet Diabetes Endocrinol. 2020;8:823–833. doi: 10.1016/S2213-8587(20)30271-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kamran S. Pakistan People’s Party; 2020. Response analysis, challenges & strategic vision for Pakistan amidst the COVID-19 crisis.https://en.baaghitv.com/wp-content/uploads/2020/07/PPP-Covid-19-Paper.pdf Available at: [Google Scholar]
- Kaul R. 2020. Covid-19: India inching closer to 1% death. Hindustan Times, 28 September.https://www.hindustantimes.com/india-news/covid-19-india-inching-closer-to-1-death-rate/story-CXFqVxOIIJaRaqK4WlsbdJ.html Available at: [Google Scholar]
- Mangi F., Devnath A. 2020. Covid cases in South Asia are rising at the fastest rate in the world. The Print, 9 June.https://theprint.in/health/covid-cases-in-south-asia-are-rising-at-the-fastest-rate-in-the-world/438708/ Available at: [Google Scholar]
- Menon S. 2020. Coronavirus in South Asia: is low testing hiding scale of the outbreak? BBC, 18 November.https://www.bbc.com/news/world-asia-53420537 Available at: [Google Scholar]
- Mondeaux C. 2020. South Asian countries ease coronavirus restrictions despite rising numbers. The Washington Diplomat, 9 June.https://washdiplomat.com/south-asian-countries-ease-coronavirus-restrictions-despite-rising-numbers/ Available at: [Google Scholar]
- Roser M. 2020. Our world in data. 5 August.https://ourworldindata.org/blog Available at: [Google Scholar]
- Samaranayake N. 2020. Covid-19 and competition for influence in South Asia.https://www.nbr.org/publication/covid-19-and-competition-for-influence-in-south-asia/ Available at: [Google Scholar]
- Sharma S. 2020. 90% of those killed by Covid in India are older than 40, 69% are men. Hindustan Times, 14 October.https://www.hindustantimes.com/india-news/90-of-those-killed-by-covid-in-india-are-older-than-40-69-are-men/story-glg0Ct4rHQ1YVvZgnckUcM.html Available at: [Google Scholar]
- Thakur P. 2020. Covid-19: at 3.3%, India’s fatality rate almost as low as South Korea’s. Times of India, 3 May.https://timesofindia.indiatimes.com/india/covid-19-at-3-3-indias-fatality-rate-almost-as-low-as-s-koreas/articleshow/75513184.cms Available at: [Google Scholar]
- UNICEF Regional Office for South Asia . UNICEF; 2020. COVID-19 Situation Report No. 3.https://reliefweb.int/report/afghanistan/unicef-regional-office-south-asia-covid-19-situation-report-no-3-march-18-24-2020 Available at: [Google Scholar]
- United Nations Economic and Social Commission for Asia and the Pacific . 2020. COVID-19 and South Asia: national strategies and subregional cooperation for accelerating inclusive, sustainable and resilient recovery. Bangkok; UN ESCAP.https://www.unescap.org/resources/covid-19-and-south-asia-national-strategies-and-subregional-cooperation-accelerating Available at: [Google Scholar]
- World Health Organization . WHO; Geneva: 2001. Macroeconomics and health: investing in health for economic development: report of the Commission on Macroeconomics and Health.https://apps.who.int/iris/handle/10665/42435 Available at: [Google Scholar]
- World Health Organization . WHO; Geneva: 2016. Working for health and growth: investing in the health workforce. Report of the High-Level Commission on Health Employment and Economic Growth.http://www.world-psi.org/sites/default/files/documents/research/en_comheegfinalreport.pdf Available at: [Google Scholar]
- World Health Organization . WHO; Geneva: 2020. Strengthening the health system response to COVID-19. Technical guidance #1: maintaining the delivery of essential health care services while mobilizing the health workforce for the COVID-19 response, 18 April 2020.https://apps.who.int/iris/handle/10665/332559 Available at: [Google Scholar]
- Zhang C., Jin X., Chen X., Leng Q., Qiu T. Antigenic evolution on global scale reveals potential natural selection of SARS-CoV-2 by pre-existing cross-reactive T cell immunity. bioRxiv. 2020 doi: 10.1101/2020.06.16.154591. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.