Abstract
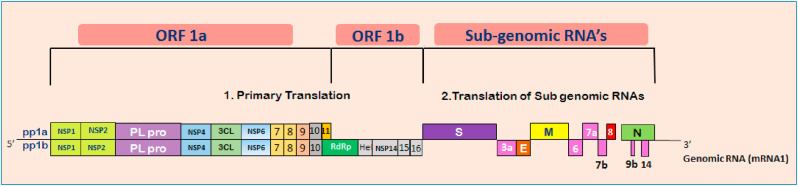
Recently, the COVID-19 disease spread has emerged as a worldwide pandemic and cause severe threats to humanity. The World Health Organisation (WHO) releases guidelines to help the countries to reduce the spread of this virus to the public, like wearing masks, hand hygiene, social distancing, shutting down all types of public transports, etc. These conditions led to a worldwide economic fall drastically, and on the other hand, indirect environmental benefits like global air quality improvement and decreased water pollution are also pictured. Currently, use of face masks is part of a comprehensive package of the prevention and control measures that can limit the spread of COVID-19 since there is no clinically proven drugs or vaccine available for COVID-19. Mostly, face masks are made of petroleum-based non-renewable polymers that are non-biodegradable, hazardous to the environment and create health issues. This study demonstrates the extensive use of the face mask and how it affects human health and the marine ecosystem. It has become a great challenge for the government sectors to impose strict regulations for the proper disposal of the masks as medical waste by the public. Neglecting the seriousness of this issue may lead to the release of large tonnes of micro-plastics to the landfill as well as to the marine environment where mostly end-up and thereby affecting their fauna and flora population vastly. Besides, this study highlights the COVID-19 spread, its evolutionary importance, taxonomy, genomic structure, transmission to humans, prevention, and treatment.
Keywords: COVID-19, Coronavirus, Face mask, Marine environment, Pollution
Graphical abstract
1. Introduction
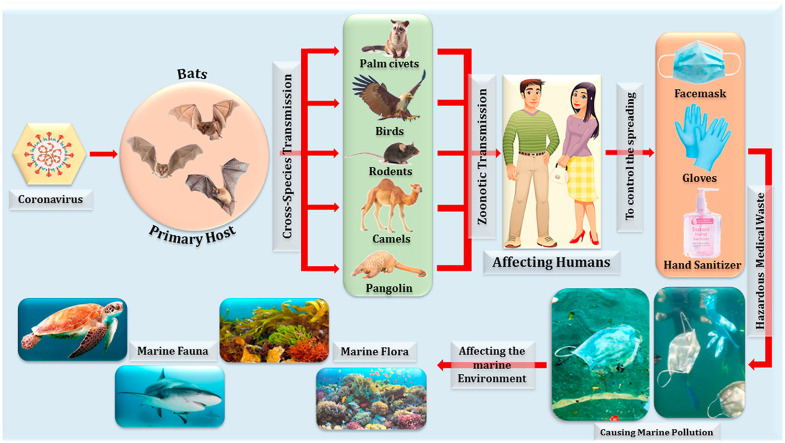
The world is facing a major crisis because of the coronavirus disease 19 (COVID-19) outbreak. It has made a great impact on the human population after severe acute respiratory syndrome coronavirus (SARS-CoV) in 2003 and the Middle East respiratory syndrome coronavirus (MERS-CoV) in 2012 (Shereen et al., 2020). COVID-19 is a type of virus that causes pneumonia by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). People prone to this viral infection get primarily infected in the lungs, resulting in inflammatory conditions causing severe damage to alveolar cells leading to high fluid accumulation. This causes gas exchange obstruction, which proceeds to symptoms like respiratory difficulties, dry cough, fever, chest pain, muscle aches, fatigue, chills, and later pneumonia-like symptoms, which leads to a severe condition termed acute respiratory distress syndrome (ARDS) (Yuki et al., 2020; Li et al., 2020). If the inflammation becomes severe, viral particles enter through the blood resulting in septic shock and multi-organ failure and the condition is called systemic inflammatory response syndrome (SIRS) (Fig. 1 ).
Fig. 1.
SARS-CoV-2 virus entry and infecting the lungs of humans causing the inflammation condition ARDS or SIRS (Alveolar cells reproduced from www.azuravesta.com).
COVID-19 has established an incredible impact around the world. At present, almost all the countries are focused on containing the spread of the COVID-19 disease by implementing certain public policies like the complete shutdown of public places (theatres, shopping malls, bars, hotels, and restaurants), travel restrictions, and stoppage of all public transport facilities (buses, trains, flights). These are being done, taking into consideration the health and welfare of the general public. Governments also ask the people to adopt social distancing among individuals, stay at home, and office-based employees are instructed to work from home. This pandemic situation has rendered numerous jobless, and most businesses are also struggling. Though these measures or regulations may significantly affect the economy of most of the countries but some positive or negative impacts have occurred to the environment like a sudden drop in greenhouse gas (GHG) emissions, which has not been witnessed after World War II, because many industries around the world halted their productions and usage of vehicles drastically decreased (Global Carbon Project, 2020). These factors led to a marked reduction in the concentrations of Nitrogen Dioxide (NO2) and Particulate Matter (diameter less than 2.5 μm) around the world. These conditions have prevailed because every countries government has adopted social distancing policies and ordered country citizens to stay in their homes to control the spread of the novel coronavirus disease. Noise pollution levels have also significantly reduced in most of the countries due to a decrease in the use of public or private transports and other commercial activities. Though COVID-19 has generated some positive effects on the environment there are still adverse effects. Few cities have stopped collecting the waste as well as suspended the recycling units in order to minimize the spreading of the virus at their recycling centers. More organic and inorganic wastes were generated due to online shopping and food ordering (Zambrano-Monserrate et al., 2020). A higher number of medical wastes also has been generated nowadays and this topic is separately detailed below.
Medical waste of COVID-19 a major threat to the environment: There has been a great threat even before the COVID-19 pandemic which is the waste management all over the world particularly plastics. This has become a major concern nowadays due to the pollution faced by both terrestrial and marine environments. Currently, during the COVID-19 epidemic, there is a sudden increase in the usage of gloves, face mask, hand sanitizer bottles and syringes, which are mostly made of plastic. If these products are not properly handled or disposed of it may still carry pathogen contaminants potentially considered hazardous waste. Many countries in the world are still struggling to manage plastic waste that threatens the environment. Recently, hazardous medical waste which is mostly made of plastics of COVID-19 origin, is emerging as a great threat to Earth’s ecosystems (Saadat et al., 2020).
Face mask usage during COVID-19: Generally, the main function of a face mask is to protect the individuals from contracting and transmitting the SARS-CoV- 2 viral infections. It is imperative to cover the mouth and nose because the SARS-CoV- 2 viruses are high level at the infected areas. Generally, this virus is transmitted through air droplets to other people when they cough, sneeze, breathe, and talk. During the mid of March 2020, when COVID-19 infection was at the peak, the World Health Organisation (WHO) and Centre for Disease Control and Prevention (CDC) instructed the healthcare workers and the infected patients to wear masks so that community spreading can be minimized. Currently, three types of masks are in circulation i) Respirator mask (N95, FFP2), ii) Surgical or medical mask and iii) Non-certified disposable mask (cloth mask) (Ho et al., 2020; Das et al., 2020).
The World Health Organisation (WHO) also initially instructed that it is necessary for healthy people to wear masks only if they are taking care of infected patients. Later, considering the advantages of using a mask, healthy people were also advised to wear masks to reduce the risk of getting exposed to infections from pre-symptomatic or asymptomatic people. This conflicting information caused worries among the public and led to panic buying, with people stocking up the masks, hand sanitizers, and even toilet paper (WHO, 2020a,b,c).
As the spread of disease worsened throughout the world, there was a rush to buy face masks, particularly of the surgical type, to protect from infection. This condition caused surgical mask shortage for those in need, such as infected people, because it can reduce the rate of transmission of respiratory droplets to others. Earlier reports suggested that the oral cavity was the source of respiratory droplets, ranging in size from 5 to 100 μm and transmitted via air, particularly during coughing and communicating. Wearing masks would significantly reduce the probability of airborne infections. On 3 April 2020, the Centre for Disease Control and Prevention (CDC) announced the public to wear a non-certified mask (cloth mask) where physical distancing is not possible. The spread can also be contained by hand washing or social distancing, but lacks evidence of preventing the disease. There has also been a report that cloth mask (70% cotton and 30% polyester), which contains three layers, exhibited nearly 40–60% filtration efficiency (Carlos Rubio-Romero et al., 2020).
Traces of SARS-CoV-2 virus have been detected for 6–8 h on plastics, 5–6 h on stainless steel, and up to 7 days on the face mask’s outer surface, but with a lower cell density of approximately 0.1 percent of the original inoculum (van Doremalen et al., 2020). It clearly shows that medical waste generated during COVID-19 such as needles and syringes used for blood tests, face masks, PPE, can have a longer SARS-CoV-2 persistence. Including the self-inoculation of mucous membranes of the eyes, nose and mouth, virus transmissions from infected dry surfaces have been postulated. By raising the reproductive number (R0) from its determined range between 2.2 and 3.58, exposure to medical waste may theoretically increase the virus’s spread (Li et al., 2020). A host carrier of SARS-CoV-2 may likely be the viral loads of saliva, cough, tears, and urine left with the medical waste of COVID-19. The main route of transmission of SARS-CoV-2 is splatters released during respiration and expelled by an infected individual’s sneezing. The common use of face mask and hand gloves during COVID-19 exhibited every possibility of these waste being disposed of along with solid waste due to its size and lightweight. So careful handling of such waste is recommended because it can be highly contagious for a sustained period of 7 days (Ilyas et al., 2020; Zhao et al., 2020).
Marine environment and its pollutants: The pollution entering the oceans are man-made or some natural causes which vastly affect the marine ecosystem. They all enter through the land to the sea, causing great danger to the marine fauna and flora and also affects humans. Marine pollutants exist in many forms like solid waste (plastics), nutrient enrichment (eutrophication), toxic chemicals (persistent organic pollutants [POP’s], pesticides, heavy metals from mine tailings, pharmaceutical waste, gases), untreated sewage discharge, radioactive substances, oil spills, and discarded fishing nets. These marine pollutants change the physical, chemical and biological characteristics of coastal and ocean zones vastly and threaten marine diversity, which ultimately affects their productivity (Li et al., 2016).
Marine debris consists of mostly solid materials that are discarded or transported to the oceans. These include numerous materials like metals, paper, wood, rubber, glass, clothes and plastics (Setyo and Muhammad, 2019). These are classified, under two groups, as biodegradable and non-biodegradable. One of the most significant concerns in the current world is the non-biodegradable plastics heavily polluting the marine environment. There are lightweight in nature and can be easily transported by wind and water. It has been estimated by world scientists that a minimum of 5.25 trillion plastic particles weighing nearly 269,000 tons are prevailing in the world’s oceans. Almost 280 million tons of plastic materials are produced in the world annually and these mostly end up in landfills or the oceans (Xuan-Thanh et al., 2020). Nowadays, they play a vital role in many applications like industrial, medical, municipal and commercial sectors. It has been estimated that nearly 267 species have been affected worldwide by plastics, of which 86% are sea turtles, 44% seabirds, and 43% marine mammals. Plastics affect or harm the marine species by ingestion (reduce the stomach capacity, hinder growth, internal injury, intestinal block), entanglement (through nets or other materials leads to drop in their feeding, drowning) and strangulation. The world is now dealing with one more emerging plastic pollutant named “Microplastics,” which has a particle size smaller than 5 mm. It has spread all over the world from land to the oceans. Owing to a smaller size, it affects the marine environment both physically and biologically and also their food chain drastically (Nirban and Upendra, 2019; Klemes et al., 2020). Microplastics can go up in the marine food chain has led to great concern for humans since they are the major consumers of seafood and still, its adverse effects on human health are currently difficult to assess.
This review highlights the spread of COVID-19 disease, its evolutionary link, taxonomy and structural characteristics, genome outlook, mode of transmission to humans, prevention, and treatment. Besides, the major objective of this study focuses on the usage of face masks during COVID-19: its primary benefits and drawbacks. This study also demonstrates the adverse effect of face mask medical waste (as plastic or microplastic) and its serious threat to the marine ecosystem. Lastly, its safe recycling process, energy conversions and alternatives are briefed as future applications.
2. Spreading of COVID-19 – mechanism
It has been a disastrous start for the year 2020 with the spread of pandemic COVID-19, which has already infected nearly 21.83 million people worldwide as of 15th August 2020 and causing a devastating death toll of about 7,73,122 people. This pandemic has its origin in the mid-December 2019 from the West District of Southern China Seafood Wholesale Market in Wuhan city of China and rapidly infected more than 50 patients (Lu et al., 2020). This seafood market has a history of selling live animals like bats, frogs, snakes, birds, marmots, and rabbits apart from fish and shellfish. It has been hypothesized that the cause of infection might be from either visiting the seafood market or by consumption of the animals or birds that are sold or by interaction with sellers who have infection history. Initially, the infected patients admitted to the hospitals had symptoms of cough, fever, dyspnoea with acute respiratory distress syndrome (ARDS). At the end of December 2019, the Chinese government informed WHO that several patients developed viral pneumonia with an unknown cause. By early January 2020, the National Health Commission of China provided the details of the disease spread and the viral isolates upon genome sequencing confirmed the presence of novel β-coronavirus genera (Gennaro et al., 2020). These strains exhibited more than 80% homology with severe acute respiratory syndrome coronavirus (SARS-CoV) and 50% similarity with that of the Middle East respiratory syndrome coronavirus. The earlier outbreak of this pneumonia-causing novel virus was referred to as Wuhan-Hu-1-CoV or 2019 novel coronavirus (2019-nCov) by the Chinese researchers named after its origin from Wuhan Seafood Wholesale Market. By February 11, 2020, due to its epidemic scale of spreading this novel coronavirus worldwide. TheWorld Health Organisation (WHO) Director-General, Dr. Tedros Adhanom Ghebreyesus, announced the global name of this virus as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and the disease was called COVID – 19 based on the recommendation from the International Committee on Taxonomy of Viruses (ICTV). World Health Organisation declared the status of the COVID-19 spread to be a pandemic on 11th March 2020 based on 114 countries affected with more than 118,000 cases with a death count of 4000 people (World Health Organization, 2020).
3. The evolutionary importance of SARS-CoV- 2 virus
It had been hypothesized that the SARS-CoV-2 virus, which is triggering COVID-19 disease, is not the first virus to cause such a respiratory disease outbreak. Earlier in 2003, a similar spread of coronavirus causing Severe Acute Respiratory Syndrome (SARS-CoV) in Guangdong province of China occurred, leading to more than 8000 infected and 776 deaths (Zheng et al., 2004). Similar to COVID-19 disease, the patients of SARS-CoV were also affected with pneumonia-like symptoms damaging the alveolar cells causing acute respiratory distress syndrome (ARDS) (Kan et al., 2005). Nearly after ten years of SARS-CoV outbreak, another epidemic disease caused by coronavirus emerged among the Saudi Arabian people in the year 2012. It was named Middle East Respiratory Syndrome Coronavirus (MERS-CoV), causing 2428 people infected and 838 deaths. Initially, MERS-CoV caused a slight respiratory injury, while its progression later led to severe respiratory disease (Paden et al., 2018). Like SARS-CoV, MERS-CoV affected patients suffer pneumonia, which further progresses, leading to ARDS condition and finally complete kidney failure. Genome sequencing analysis of the SARS-CoV- 2 virus revealed similar homology with SARS-CoV and MERS-CoV and even belongs to β-coronavirus genera (Shi and Hu, 2008).
Generally, to contain the infection caused by the viruses, its origin and mode of transmission have to be determined and appropriate measures or vaccines could be developed to prevent further spreading. Coronaviruses are pathogens of zoonotic origin. They are transmitted from animals to humans either directly or by the intermediate host, which can act as carriers of these viruses. In the year 1960, the first human coronavirus was detected in children causing many infections in the upper respiratory tract. Even the latest SARS-CoV-2 and other coronavirus epidemics might have originated from the zoonotic host bats. Bats have been found to be the key host in transmitting several human viruses like Nipah, Hendra, Rabies, Marburg and SARS-CoV. But it may also have some other animals as an intermediate host to get transmitted to humans (Annan et al., 2013).
Scientists initially believed that raccoon dogs and palm civets were the main suspected species responsible for the infections in the 2003 case of SARS-CoV, which originated from China’s Guangdong market. The samples of palm civets (Paguma larvata) exhibited positive on viral RNA detection and anti-SARS-CoV antibodies. But further research of the farmed and wild palm civets showed that the virus was transmitted to them by other animals suggesting that it may be the secondary hosts. Later by 2005, some researchers found that the SARS-CoV virus in horseshoe bats (genus Rhinolophus) and their findings suggest that bats might be the primary host or source of the SARS-CoV and palm civets were only intermediate hosts. The SARS-CoV isolated from palm civets arises from the recombination of two bat coronavirus strains, namely WIV16 and Rf4092 (Huynh et al., 2012). The bats, too, possessed anti-SARS-CoV antibodies. The recombination of strains occurred within the bats and later on transmitted to palm civets by fecal or oral mode. These then further underwent mutations before infecting humans.
Later by 2012, another pandemic - the Middle East respiratory syndrome coronavirus (MERS-CoV) spread in Saudi Arabia. This also comes under the classification of β-Coronavirus like SAR-CoV and dromedary camels have been the primary host of transmission to humans. MERS-CoV-specific antibodies are mostly present in camels of Middle Eastern, African and Asian countries. Like SARS-CoV, even MERS-CoV exhibited high genomic similarities with the bat β-coronavirus (Tylonycteris bat coronavirus HKU4, Pipistrellus bat coronavirus HKU5). They have matching genomic structures, highly conserved poly-proteins and structural proteins like the bat coronavirus. But they showed variability in their spike protein and some accessory proteins. Thus, all the genomic sequencing evidence suggested that bats may be the key host and through which it might be transmitted to other animals (Lau et al., 2013).
Phylogenetic analysis of the latest COVID-19 virus indicated nearly 88% sequence similarity with the two SARS-CoV, namely bat-SL-CoVZC45, bat-SL-CoVZXC21 and 50% sequence identity with MERS-CoV. Since the similarity is very close to SARS-CoV, it was termed as SARS-CoV-2. Scientific evidence is very clear that the novel β-coronavirus (SARS-CoV-2) might have originated in bats and later transmitted through intermediate species to humans (Chan et al., 2020a). Recent updates on novel coronavirus (SARS-CoV-2) indicated that rodents may also be a primary host or may act as an intermediate host. But till now, there is no substantial evidence which animal serves as primary or intermediary host. Thus there is an urgent need to know about the origin and transmission of viruses in order to develop preventive measures to contain the spreading (Chan et al., 2020b). One surprising fact is that no vaccine was developed during SARS-CoV or MERS-CoV, but the virus got vanished. Many factors were involved at the end of SARS-CoV or MERS-CoV, perhaps including summer weather and strict quarantine of all those who had contact with infected individuals, but exactly how the epidemic ended is unknown. Generally, viruses are like that, unpredictable!
4. SARS-CoV-2 taxonomy and their unique structural characteristics
Coronaviruses are most prevalent in animals as well as humans. Basically, in animals, they affect the gastrointestinal region and when considering humans, it causes mostly respiratory diseases. Earlier, before 2003, these coronaviruses were not as fatal to humans as what is seen nowadays. It caused mild symptoms such as running nose, headache, mild fever, cough, sore throat, which lasted only a few days. This virus rarely caused respiratory diseases like pneumonia and bronchitis to the patients with weaker immune systems. After the outbreak of SARS-CoV (Severe Acute Respiratory Syndrome Coronavirus) in 2003, in Guangdong, China, this coronavirus became a serious issue due to the large number of people it affected and fatalities (Alanagreh et al., 2020).
The current classification and taxonomy of the SARS-CoV- 2 viruses are mostly based on genome sequencing methods. The novel SARS-CoV- 2 belong to the realm of Riboviria under the order Nidovirales (Gorbalenya et al., 2019). It is classified in the family of Coronoviradae, subfamily Orthocoronavirinae, subgenera Betacoronavirus and sub-genra Sarbecovirus (Table 1 ). This taxonomical classification was brought out by the Coronaviridae Study Group (CSG), which falls under the organization of the International Committee on Taxonomy of Viruses (ICTV, 2018). Generally, coronaviruses belonging to the family Coronaviridae has four genera, namely α, β, γ and δ. Most of these genotypes infect bats and avian species while α and β alone affects humans. Previously several coronaviruses typeswere detected in humans of α type genera like HCoV-229E, NL63, and β type genera include MERS-CoV, SARS-CoV, HCoV-OC43, HCoV-HKU (Adams et al., 2017). This SARS-CoV-2 belongs to the novel β type genera, as mentioned above in the classification (Wu et al., 2020). Upon phylogenetic analysis of coronaviruses, it was thought to be of ancient origin, which initially infects the bats or birds. Later on, several mutations or recombinations occurring in the strains led to the cross-species transmission to the mammals and then to humans.
Table 1.
Taxonomy of SARS-CoV-2 virus.
| Category | Virus |
|---|---|
| Realm | Riboviria |
| Kingdom | Orthornavirae |
| Phylum | Pisuviricota |
| Class | Pisoniviricetes |
| Order | Nidovirales |
| Suborder | Cornidovirineae |
| Family | Coronaviridae |
| Subfamily | Orthocoronavirinae |
| Genus | Betacoronavirus |
| Subgenus | Sarbecovirus |
| Species | Severe acute respiratory syndrome-related coronavirus (SARS-CoV-2) |
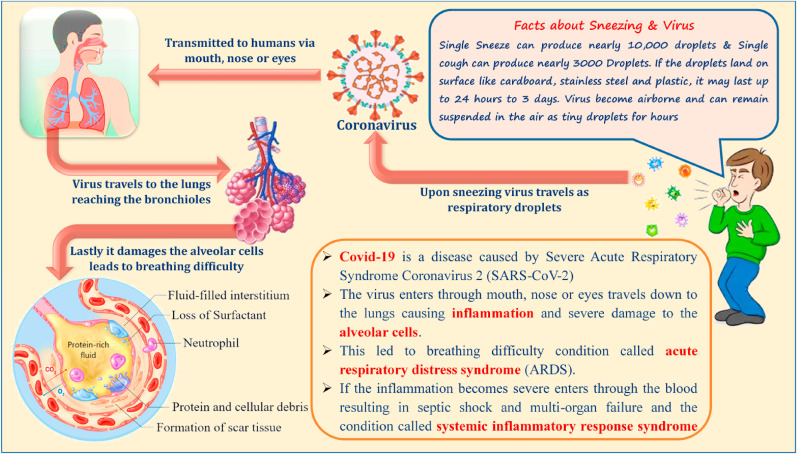
Typically, SARS-CoV- 2 are spherical or pleomorphic enveloped virus consisting of single-stranded positive RNA with a large genome in size ranging from 26.4 to 31.7 kb. They are in the size of 80–160 nm in diameter and have G + C contents in the range of 32%–43%. It was named coronavirus because of its crown-like appearance of large glycoprotein spikes or peplomers on its envelope when observed under an electron microscope (Czub et al., 2005, Woo et al., 2010; Van Boheemen et al., 2012). Like any other virus, its genome typically also possesses a 5′-cap structure and 3′ poly-A tail (Fig. 2 ) (Yang and Leibowitz, 2015). The structure SARS-CoV- 2 consists of five main parts i) Spike protein, ii) Membrane protein, iii) Envelope protein, iv) Nucleocapsid protein, and v) Hemagglutinin-esterase protein.
Fig. 2.
Structure of SARS-CoV-2 Virus (created using biorender.com).
Spike protein (S) – These are present at the outer surface of the virus and are type 1 membrane glycoprotein composed of peplomers. These spike proteins help in the binding of the virus to the host-specific cell surface receptors, thereby causing the attachment, which can lead to the viral genome entry inside the host. Sometimes the spike proteins can lead to the fusion of many cells resulting in the formation of giant multinucleated cells, which can directly damage the neutralizing antibodies causing viral spreading between the cells (Kirchdoerfer et al., 2016).
Membrane protein (M) - It is the structural glycoprotein that stretches the membrane lipid bilayer three times. It has a short amino-terminal domain projected externally in the virus and a long carboxy-terminal inside the virion’s cytoplasmic domain. Membrane proteins act as a central organizer for the virus formation and interact with all other structural proteins. Membrane proteins are a huge reserve of structural proteins and give proper shape to the viral envelope. It is necessary for spike proteins to interact with membrane proteins so that it is retained in the endoplasmic reticulum – Golgi intermediate compartment/Golgi complex and also for its integration in the new virions. Membrane protein binding causes nucleocapsid protein and the internal core of virions stabilization, which will lead to the viral assembly completion. The interaction of a membrane protein with envelope protein promotes the viral envelope formation and it is enough to produce and release virus-like particles (De Haan et al., 1998).
Envelope protein (E) – These are the smallest integral membrane protein that contains smaller spikes and has an important role in the life cycle of the virus, such as assembly, budding, envelope formation, and pathogenesis. Envelope protein has certain functions like ion-channeling viroporin, numerous interactions with other proteins of the virus as well as with the host cell proteins. Envelope proteins are highly expressed inside the host cell during the replication process, and only a very small part is assimilated in the virion envelope. Envelope proteins are mostly directed to a particular site of intracellular trafficking where it involves in virus assembly as well as its budding (Schoeman and Fielding, 2019).
Nucleocapsid protein (N) – These are phosphor-proteins present inside the virus, which are bounded with virion RNA and regulates the viral RNA synthesis. It is also involved in the functions of the replication cycle and host cell response to viral infections. Nucleocapsid protein has certain temporary expressions, such as helping in the gradual rise of virus-like particle production, which leads to the completion of virion formation (Siu et al., 2008).
Hemagglutinin-esterase protein (HE) – This protein interacts with envelope protein to help in the construction of the viral membrane. In most cases, it acts similarly to the influenza virus hemagglutinin, which binds to the sialic acid present in the cell surface glycoproteins of the host (Hussain et al., 2020).
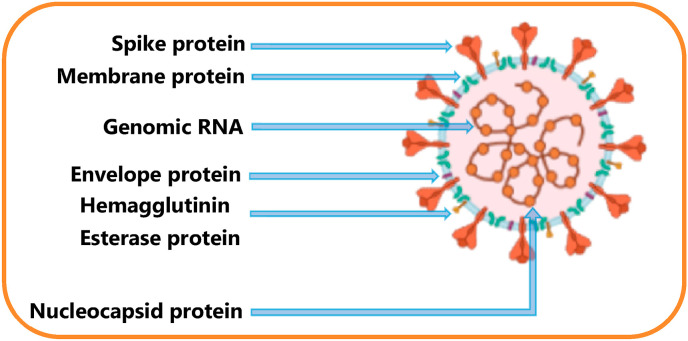
Genome Structure: Most commonly, Coronaviruses have the largest genomes among all other RNA viruses. They possess different numbers of small open reading frames (ORFs) on their genomic strand. In Coronaviruses, the genes required for the synthesis of all structural proteins occur in 5′-leader and 3′-terminal sequences, and they are in a certain order like S, E, M and N. One of the typical characteristics of coronaviruses is that they possess at least six ORFs within their genomes (Wu et al., 2020). The ORF cover more than two-thirds of the whole-genome length, which encodes for at least 16 non-structural proteins (NSP1 to NSP16). These NSPs on further processing forms the replication-transcription complex (RTC) that participate in viral genome replication and transcription. The ORF 1a and ORF 1b, which is present at the upstream 5′ end of genome upon −1 frame-shift, synthesize two polypeptides, namely pp1a and pp1b. NSP3 and NSP5 genes in ORF1a encode chymotrypsin-like protease (3CL-protease) and Papain-like protease (PLP) and helps in the processing of these polypeptides (pp1a, pp1b). Later the peptides help in cleaving and blocking the host’s innate immune response. Similarly, NSP12 genes in ORF1b helps in encoding RNA-dependent RNA polymerase (RdRp) and NSP15 encodes RNA helicase, which takes part in the transcription and translation process of the genome. As a result, a group of sub-genomic RNAs (sgRNAs) is synthesized by RTC in the form of discontinuous transcription. Other ORFs that are present on the 3′ terminus end mostly encodes for the four structural proteins synthesis like spike (S), membrane (M), envelope (E), and nucleocapsid (N) (Chen et al., 2020a, Chen et al., 2020b, Chen et al., 2020c; Hui et al., 2020). Each protein has its individual function like S protein, which is of glycoprotein in nature helps in recognizing the host cell surface receptors, M proteins involve in the proper folding or dimensions to the virions, E proteins assemble the virions as well as their release and N proteins are involved in the packaging of the RNA genome. They have roles in pathogenicity as an interferon (IFN) inhibitor. More structural and accessory proteins are still present, and they are mostly species-specific, like HE protein, 3a/b protein, 4a/b protein. These accessory proteins are highly unique among the coronaviruses in relation to numbers, genomic organizations, sequences, and functions. These structural and accessory proteins are mainly translated from the sub-genomic RNAs (Li et al., 2020; Gralinski and Menachery, 2020; Xu et al., 2020). These proteins are responsible for several essential functions in genome maintenance and virus replication (Fig. 3 ).
Fig. 3.
SARS-CoV-2 genome organization.
5. Mode of transmission among humans
The mode of transmission and spread of the SARS-CoV-2 virus among humans is mostly from symptomatic people. Another possibility of spreading would be from asymptomatic individuals who might have transmitted the virus before symptoms. SARS-CoV-2 viruses are respiratory pathogens that are transmitted through coughing or sneezing and are carried by tiny respiratory droplets (particles >5–10 μm in diameter), causing infection among humans. The infection of the SARS-CoV-2 virus would also be possible by aerosol transmission if there is an elevated concentration in closed spaces (Li et al., 2003; Bosch et al., 2003; Chen et al., 2020a,b,c). These respiratory droplets, which carry SARS-CoV- 2 virus enter through the mouth or nasal passage, then passes through the mucous membranes and then enters the lungs through the respiratory tract. Later, on entry, the virus targets the organs that express angiotensin-converting enzyme 2 (ACE2) like the lungs, heart, renal system, and gastrointestinal tract (Letko et al., 2020; Zou et al., 2020). Once the virus enters, it takes nearly 7–14 days to reach its second phase, where the infection aggravates, resulting in reduced B lymphocyte and ultimately affecting antibody production. Another inflammatory factor, interleukin 6 (IL-6), also gets increased and causing aggravation of the disease within 2–10 days (Belouzard et al., 2009).
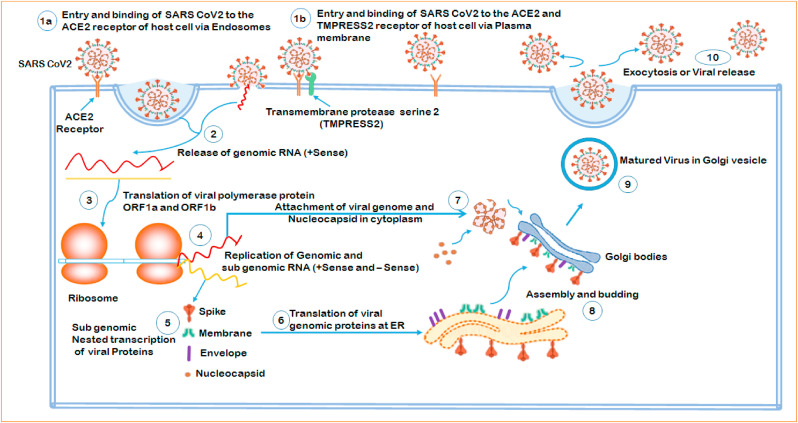
SARS-CoV-2 enters the alveolar cells (Type II) via two ways, namely the endosomal pathway (endocytosis) or plasma membrane fusion. Spike proteins or S-glycoproteins (S1, S2) that are present on the outer surface of SARS-CoV-2 virus through its receptor-binding domain (RBD) helps in the attachment to the host cell membrane and also binds to the angiotensin-converting enzyme 2 (ACE2) receptor (Millet and Whittaker, 2014; Walls et al., 2020). Spike proteins have two subunits, namely S1 and S2 in which S1, an ectodomain comprising the RBD, governs the host range, cellular response, and helps in attaching the virus to the target cell and S2 a trans-membrane endodomain that facilitates the fusion of virus and host membranes through endocytosis process. One of the critical moves in virus entry into the host is affinity chemistry between Spike proteins and ACE 2 receptors. Recent studies have shown that the binding capacity of spike protein and ACE 2 is nearly 10 to 20-fold higher than SARS-CoV and it clearly explains how pathogenic is the SARS-CoV-2 virus (Ou et al., 2020). More understanding of this binding mechanism would help in finding the drug targets. One of the unique characteristics of SARS-CoV-2 is that at the S1/S2 cleavage site without cleavage, the viral genome gets assembled and incorporated. This is due to the existence of a furin cleavage site [“Reverse phase protein array (RPPA)” sequence] at the S1/S2 cleavage site, which acts as another protease site. SARS-CoV-2 viruses possess unique pre-cleavage characteristics, which may be the reason for higher infections compared with other coronaviruses (Belouzard et al., 2012).
Once the spike protein of the virus and ACE2 of the host get engaged, it leads to the entry of the viral genome in the form of endosomes. Cathepsin L, a cysteine protease, cleaves the endosomal membrane and M proteins, thus releasing viral genes into the host cell’s cytoplasm. Alternatively, another protein called cell surface-associated transmembrane protease serine 2 (TMPRSS2) activates the spike protein to bind near the ACE2 receptor causing fusion with the plasma membrane of the host (2 Hoffmann et al., 2020). The plasma membrane fusion opens up the M protein to release the viral genome directly to the cytoplasm for its replication inside the host cell and this entry is less likely to trigger host cell antiviral immunity. Thus upon entry, the positive-sense ssRNA(+) viral genome in the cytoplasm of the host encodes for two large poly-cistronic open reading frames ORF1a and ORF1b at the 5′-leader end. These ORFs present in the most substantial part of the viral genome encodes nearly 16 non-structural proteins (NSP1– NSP16) and this gets involved in the formation of replication–transcription complex (RTC) (Guo et al., 2020).
Each NSP has specific roles in early translation, replication, transcription but some of their functions are still unknown. The ORF1a and ORF1b in the translation process produces two polyproteins (pp1a, pp1b). The synthesized polyproteins are processed into 16 non-structural proteins (NSPs) to form RTC, which is later involved in genome transcription and replication. Other ORFs present along with ORF1a and ORF1b in the genome help in the encoding of structural proteins, including the spike, membrane, envelope, nucleocapsid and accessory proteins. NSP1 and NSP2 are believed to show a role in host modulation to suppress an antiviral response. NSP3 and NSP5 present in the replication–transcription complex encodes for the protease enzymes: Papain-like protease (PLP), 3CL-protease, and they function in polypeptide cleaving as well as in stopping the host immune response. NSP3, NSP4, and NSP6 are trans-membrane proteins that induce the formation of double-membrane vesicles, which helps improve viral replication mediated by membrane-associated replication (Chen et al., 2020a, Chen et al., 2020b, Chen et al., 2020c). During replication, a full length (−) RNA genome is generated by replication–transcription complex and used as templates for full-length (+) RNA genomes. NSP12, which encodes for RNA-dependent RNA polymerase (RdRp) and NSP15 encodes for RNA helicase, help in the replication process. The replication complex formations are guided by NSP7, NSP8 and NSP9 that are believed to interact with NSP8 in the replication complex. These help in the release of primase, which generates short RNA primers for the primer dependent RdRp and thus increases its processivity. NSP13 and NSP16/NSP10 have helicase/triphosphatase and methyltransferase activity,and cap the nascent viral mRNA. NSP14 is an exonuclease with proofreading function in the replication machinery and helps in more SARS-CoV-2 RNA synthesis and NSP15 is uridine-specific endoribonuclease of replication complex (Masters, 2006). The genomic RNA directly synthesizes the RNA viral genome, and the fragments of sub-genomic RNAs (sgRNAs) helps in the production of structural proteins (N, S, M, E) in a manner of discontinuous transcription. Even though these sgRNAs may have several open reading frames (ORFs), only the closest ORF (to the 5′ end) will be translated. RNA-dependent RNA polymerase is mainly accountable for the replication of structural protein RNA. Except for the nucleocapsid, all other structural proteins (S, M, E) are translated by the ribosomes, which get bound in the endoplasmic reticulum (ER). They all assemble for the virion formation on the surface of the ER. The nucleocapsid is translated and released in the cytoplasm, where it gets connected with the viral genomic RNA. Later the nucleocapsid containing viral genome gets fused with the virion precursor and then assembled in the endoplasmic reticulum (ER)–Golgi intermediate compartment (ERGIC) (DeDiego et al., 2006; Neuman et al., 2010; Demogines et al., 2012; Fehr and Perlman, 2015; Cui et al., 2015). The so-formed mature virion containing Golgi vesicles are transported to the cell surface and released from the infected cell via exocytosis, which can search for another host to repeat its cycle (Fig. 4 ).
Fig. 4.
SARS-CoV-2 virus life cycle inside the host cell.
6. Preventions and treatment of COVID-19
Currently, there is no single or specific vaccine developed for COVID-19, and the people must prevent or reduce the intensity of infections among themselves. In order to avoid the spreading of COVID-19, all nations have been instructed by World Health Organisation (WHO) to follow certain guidelines, which include: i) Regular and thorough cleaning of hands with an alcohol-based hand sanitizer or with soap and water; ii) Maintaining at least 1 m (3 feet) distance between each other in order to avoid people who may cough, sneeze, or speak and are likely to spray small liquid droplets from their nose or mouth which may contain the virus. Even close contact with an infected person can lead to the transfer of droplets; iii) Avoid going to crowded places, where there is a higher chance of getting in contact with infected people as it is difficult to maintain the recommended physical distance of 1 m; iv) Avoid unnecessary touching of eyes, nose and mouth, which may lead to the entry of the virus inside the body and causing infections via contaminated hands; v) Maintenance of good respiratory hygiene such as covering the mouth and nose with bent elbow or tissue when during a cough or sneeze; vi) Proper disposal of the used tissues and immediate washing of hands with soap; vii) Strict warning given to people to stay home and self-isolate themselves when they possess minor symptoms such as cough, headache, mild fever until complete recovery; viii) If it is really necessary to leave the house, then a mask should be worn either to avoid getting infected or infecting others; ix) People, who have fever, cough and difficulty in breathing needs immediate medical attention; x) People should know updated information about the COVID-19 from the local or national health authorities (WHO, 2019; Wu, 2020; CDC, 2019).
Apart from the guidelines suggested by the World Health Organisation (WHO) certain other preventive measures can be followed for self-secure of individuals like a) When going out for office job or getting essential goods it can be a mandatory applied to wear face masks, b) Better to cover completely when coughs or sneezes with tissue paper and its immediate proper disposal, c) Regular hand wash with soap or hand sanitizer containing a proper proportion of alcohol in it, d) Social distancing from infected people, e) Unnecessarily touching the eyes, nose, and mouth with unwashed or contaminated hands has to be adopted, f) Any sign of symptoms pertaining to COVID 19 need immediate medical attention and self-isolation and medical advice from healthcare provider had to be strictly followed., The severity of the disease prognosis, warrants immediate hospital care with oxygen therapy. If all these measures are properly followed, then the spread of COVID-19 (Adhikari et al., 2020; Hopman et al., 2020).
Early or common signs that can be seen among COVID-19 patients would be coughing, sneezing, fever, shortness of breath, respiratory symptoms and other breathing difficulties. The advanced stage can affect the patients with pneumonia, severe respiratory failure requiring ventilation support in an intensive care unit (ICU), multi-organ affecting events like sepsis, septic shock, and multiple organ dysfunction syndromes (MODS) (Lupia et al., 2020). Pneumonia was found to be the most serious sort of infection that can be basically characterized by fever, cough, dyspnea, and bilateral infiltrates, which can be viewed on chest imaging using CT scan. Other most common symptoms include headaches, sore throat, and rhinorrhoea. Apart from respiratory infections, there are few reports on gastrointestinal symptoms like nausea and diarrhea (Yang et al., 2020).
Pneumonia condition occurring in COVID -19 infected patients was found to be a complex pathogenic mechanism. It has been sensed that SARS-CoV-2 viral infection will cause an enormous immune reaction inside the host. Several immune cells like T-lymphocytes, macrophages, dendritic cells secrete immersive amounts of cytokines and chemokines. This stage has been so popularly referred as “cytokine storm” which means excess and uncontrolled release of effector immune cells consisting of pro-inflammatory cytokines (IFNα, IFNγ, IL-1β, IL-6, IL-12, IL-18, IL-33, TNFα, TGFβ) and chemokines [low molecular weight proteins with a powerful chemo-attractant activity which play a role in the immune cell recruitment during inflammation] (CXCL10, CXCL8, CXCL9, CCL2, CCL3, CCL5) precipitate and sustain the abnormal systemic inflammatory response (Bennardo et al., 2020). This condition encourages the immediate attack on the immune system of the body, which leads to a drastic situation called Acute Respiratory Distress Syndrome (ARDS) followed by multiple organ failure, finally resulting in death. The main promoter of this storm is interleukin 6 (IL-6). This IL-6 is synthesized upon leukocyte activation, which acts on a large number of cells and tissues (Chen et al., 2020a, Chen et al., 2020b, Chen et al., 2020c). IL-6 mainly helps in the differentiation of B lymphocytes, growth of some types of cells, and in some other cells, they inhibit their growth. The main role played by IL-6 is pro-inflammatory activity but also possess anti-inflammatory effects. During certain conditions like inflammatory diseases, infections, heart diseases, autoimmune disorders, several cancer types, there will be an increase of IL-6 that results in cytokine release syndrome (CRS), which is an acute systemic inflammatory syndrome leading to fever and multiple organ dysfunctions (Pyle et al., 2017; Rose-John, 2018; Lei et al., 2018; Letko et al., 2020).
The treatments for COVID-19 have been delicately improving every day, but still, critical care support, antibiotic medication and good nourishment are the primary methods followed. There are different methods adopted for treating the COVID-19 patients and these depend upon their immune levels, other medical histories and medications provided. Currently, there are symptomatic treatments, oxygen therapy, and antiviral drugs that are used for COVID-19 patients. Most standing clinical and preclinical data on antiviral treatment is taken from other viruses, including SARS-CoV-1, Middle East Respiratory Syndrome virus, and non-coronaviruses (Ebola). The basic treatment given for COVID-19 patients is a complete rest with an excellent calorie diet, water intake to reduce the risk of dehydration, a random interval check of vitals and saturation of oxygen. In severe cases, blood count, C- reactive proteins, chest imaging, urine test, and other blood-related tests were carefully monitored. Antipyretic drug treatments are given to patients whose body temperature exceeds 100 °F. Common drugs include ibuprofen orally, 5–10 mg/kg every day and acetaminophen orally, 10–15 mg/kg every day. Oxygen therapy is needed when the patient is in a state of hypoxia when the lungs are severely infected with the virus. In emergency conditions, non-invasive or invasive mechanical ventilation is provided to the COVID-19 patients (Chhikara et al., 2020).
Generally, any anti-viral drug targets the viral replication process in the host cell. Prominently all strains of the virus have the same mode of action and infection. Some of the suggested antiviral drugs for the treatment of COVID-19 are Oseltamivir, peramivir, and zanamivir. These are neuraminidase inhibitors thathave been used for influenza treatments. α-interferon, lopinavir/ritonavir, chloroquine phosphate, ribavirin, and arbidol are therapeutically used to prevent, diagnose, and treat coronavirus-induced pneumonia patients by the National Health Commission (NHC) of the People’s Republic of China for tentative treatment of COVID-19. There has been a recent report from Shanghai Institute of Materia Medica and Shanghai Tech University, where drug screening by enzyme activity test and In Silico approach using nearly 30 agents like indinavir, saquinavir, lopinavir, carfilzomib, ritonavir, remdesivir, atazanavir, darunavir, tipranavir, fosamprenavir, enzaplatovir, presatovir, abacavir, bortezomib, elvitegravir, maribavir, raltegravir, montelukast, deoxyrhapontin, polydatin, chalcone, disulfiram, carmofur, shikonin, ebselen, tideglusib, PX-12, TDZD-8, cyclosporin A, and cinanserin was performed against the virus. Plasma therapy also helped certain percentages of people around the world to be cured completely of the COVID-19 disease. The polyclonal neutralizing antibodies carried by recovered patients are able to reduce the viral count drastically. Above all, the basic foundation is to prevent and fight against COVID-19 through strong immunity. This is the right time to focus on individuals’ health, get some adequate sleep, fresh air, and sunlight daily. People should stay hydrated, minimize the intake of overly processed foods and make sure to eat enough micronutrients (Lu, 2020; Gao et al., 2020; Martinez, 2020; Dong et al., 2020).
The World Health Organization’s (WHO) pandemic declaration of COVID-19 disease on 11th March 2020 and its subsequent genome sequence of SARS-CoV-2 publications have led the world’s research and development sectors to develop vaccines against the dreadful virus (Wu, 2020). Usually, any new vaccine production takes about 15 years, but the hunt for the SARS-CoV2 vaccine is going on rapidly, resulting in almost a breakthrough by many research institutions and vaccine manufacturers in the development of vaccines. However, in a pandemic case, the entire vaccine production process, including clinical trials, is shortened and can be quickly tracked for 15–18 months. The simultaneous promotion of many vaccines is expected to occur by the beginning of 2021 (Kaur and Gupta, 2020; Dutta, 2020).
Coronaviruses with a glycoprotein spike on the surface are enveloped, positive-sense single-stranded RNA viruses, mediating receptor binding and cell entry during infection. The functions of the spike protein make it an attractive vaccine antigen for receptor binding and membrane fusion. Apart from the full virion inactivated vaccine, almost all manufacturers target spike protein as antigen (Thanh et al., 2020; Fadda et al., 2020). For the production of this vaccine, there are numerous methods and platforms being tried. Vaccines are typically produced either as inactivated, live attenuated or sub-unit, but different organizations and manufacturers are trying next generation techniques. The world is likely to see several new platforms to develop the Covid-19 vaccine. Thus, the first RNA vaccine is expected to find a place in the history of vaccine production as an effective agent for Covid-19 prevention. In addition, in making of the SARS-CoV2 vaccine, DNA, vector-based RNA, subunits and several other variants of RNA technologies are being studied. The messenger RNA vaccine’s idea is relatively recent but quite basic, in which the spike protein mRNA coding is injected and the host produces the antibody and can be developed on an industrial scale (Wu, 2020).
As of 12th November 2020, according to WHO, there are 50 candidate vaccines that are in advanced stages of development and another 164 are in preclinical stages. All the following 50 candidate vaccines are either in Phase 1, 2, or 3 clinical trial stages and many have shown encouraging results after animal studies. Most of the countries are full-fledged involved in vaccine development, particularly in the USA, Europe, China, Russia, India, etc. The top 10 vaccine candidates which have entered phase 3 clinical trials are discussed in Table 2 . Currently, more than 100 candidates for COVID-19 vaccines are in the developmental stage, with a number of them in the human trial process. Through the Access to COVID-19 Tools (ACT) Accelerator, WHO works in partnership with scientists, industry, and global health organizations to speed up the pandemic response. COVAX (led by the WHO, the Global Alliance for Vaccines and Immunization [GAVI] and the Coalition for Disease Preparedness Innovations [CEPI]) will promote the equal access and distribution of these vaccines to protect citizens in all countries when a safe and efficient vaccine is developed and people who are most at risk will be given first priority on vaccination (Sharma et al., 2020; Rabaan et al., 2020).
Table 2.
Phase 3 clinical trials of COVID-19 Vaccines (www.raps.org).
| S. No. | Vaccine Developer | Candidate | Mechanism | Current Status |
|---|---|---|---|---|
| 1. | Moderna; Kaiser Permanente Washington Health Research Institute. | mRNA-1273 | mRNA-based vaccine | On 12 May, mRNA-1273 was granted Fast Track designation by the FDA. A Phase 3 vaccine trial is underway and is being funded by OWS. The Medicines and Healthcare Products Regulatory Agency (MHRA) of the United Kingdom has begun a real-time analysis of mRNA-1273, which will allow a faster vaccine approval process. |
| 2. | Sinovac; Sinovac Research and Development Co., Ltd. | CoronaVac | Inactivated vaccine (formalin with alum adjuvant) | Sinovac representatives told Reuters that the vaccine appeared to be effective for older participants in the trial and did not cause any significant side effects. Preliminary findings from the Instituto Butantan trial announced by the company suggest that CoronaVac has so far been safe and no significant adverse reactions have been identified. Owing to a patient death, the trial in Brazil was briefly suspended, but the trial has later resumed. |
| 3. | Bharat Biotech; National Institute of Virology | Covaxin | Inactivated vaccine | According to an ICMR scientist who spoke to Reuters, the vaccine could begin distribution as early as February 2021. |
| 4. | Pfizer; BioNTech | BNT162 | mRNA-based vaccine | For BNT162b1 and BNT162b2, Pfizer and BioNTech have secured the Fast Track designation from the FDA. Based on the totality of available evidence from our preclinical and clinical trials, including selected immune response and tolerability parameters, BNT162b2 was chosen to progress to a Phase 2/3 safety review. The companies also requested the FDA to consider an extended procedure to include up to 44,000 participants for the Phase 3 trial. European Medicines Agency (EMA) has launched a rolling review of BNT162b2, which may accelerate the candidate’s approval. According to the Wall Street Journal, Pfizer and BioNTech may be able to file for an Emergency Use Authorizations (EUA) in November and have the vaccine ready for use in December. In Australia, the Australian Therapeutic Goods Administration (TGA) provided BNT162b2 with a provisional determination, which is the first step on the path to approval of the vaccine in the region. Shanghai Fosun Pharmaceutical Company, BioNTech’s partner in China announced that it was seeking approval for BNT162b2 in China but would no longer conducting BNT162b1 clinical trials. |
| 5. | The University of Oxford; AstraZeneca; IQVIA; Serum Institute of India | AZD1222 | Replication-deficient viral vector vaccine (adenovirus from chimpanzees) | In part, the Biomedical Advanced Research and Development Authority (BARDA) and OWS are financing the AstraZeneca trials. IQVIA has announced that they are working with AstraZeneca to advance the vaccine’s clinical trials. In the United States and at study sites in India, phase 3 studies are being conducted, but have been put on hold following a serious adverse event. Trials have since resumed. The Human Medicines Committee (CHMP) of EMA has begun a rolling review of AZD1222 to decrease the amount of time before a safety and efficacy decision is taken, as has Health Canada. The Australian Therapeutic Good Administration (TGA) granted the provisional determination of AZD1222 in Australia, the first step in the approval process. An accelerated analysis of AZD1222 in Britain has also been initiated by the Medicines and Healthcare products Regulatory Agency (MHRA). |
| 6. | Johnson and Johnson | NJ-78436735 | Non-replicating viral vector | Johnson and Johnson announced on 10th June 2020, that it is accelerating Phase 1/2 trials and that human trials are underway. According to the firm, the Phase 3 study, estimated to enrol up to 60,000 individuals, is also under way. The ENSEMBLE research was on hold pending a review of an adverse condition developed by a participant in one of the study arms, but after the Independent Data Protection and Monitoring Board recommended the trial restart recruiting, Johnson and Johnson was cleared to resume the trial in the U.S. and Brazil. Johnson and Johnson said it expects as soon as possible to begin testing its vaccine in adolescents. |
| 7. | Wuhan Institute of Biological Products; China National Pharmaceutical Group (Sinopharm) | Not named | Inactivated vaccine | In Peru, Morocco, and the United Arab Emirates, a Phase 3 trial is underway. |
| 8. | Novavax | NVX-CoV2373 | Nanoparticle vaccine | Novavax has received the NVX-CoV2373Fast Track Designation from the FDA. The Coalition for Epidemic Preparedness Innovations (CEPI) announced on 11th May 2020, that it had provided Novavax with an additional $384 million to develop and produce NVX-CoV2373. As part of its recent acquisition of Praha Vaccines, Novavax plans to produce 1 billion doses of NVX-CoV2373 by 2021. According to a company press release, Novavax was awarded a $60 million by US Department of Defense contract to produce NVX-CoV2373, and another $1.6 billion from Operation Warp Speed if the candidate is successful in clinical trials. The candidate has formally initiated a Phase 3 trial in the United Kingdom to test the vaccine for up to 10,000 participants, the company said in a press release. Novavax updated its Phase 3 trial of NVX-CoV2373 in North America on 27th October 2020, announcing that the trial will begin at the end of November, approximately one month later than anticipated. |
| 9. | Gamaleya Research Institute; Acellena Contract Drug Research and Development. | Sputnik V | Non-replicating viral vector | The Russian Federation’s Health Ministry has approved Sputnik V as the first COVID-19 vaccine. To date, however no trial information has been released. Due to a lack of safety and efficacy evidence, the approval has drawn controversy in the medical community. In Brazil, the Institute has made a preliminary pre-submission of the vaccine appropriate for its use in the region. |
| 10. | CanSino Biologics; Tongji Hospital; Wuhan, China. | Ad5-nCoV | Recombinant vaccine (adenovirus type 5 vector) | As reported to Reuters on 25 June by the Central Military Commission of China announced that the military had been allowed to use Ad5-nCoV for a duration of one year. |
7. Effects of COVID-19 on the environment
The emergence of the COVID-19 pandemic has resulted in both positive and negative impacts on the environment. The positives include a decrease in air pollution, noise pollution, clean beaches, a reduction in emission of greenhouse gases, and traffic injuries. The negative impacts are increased waste, reduction in waste recycling, unemployment, economic crises and manufacturing demand. Before COVID-19, the world was facing many environmental issues like industrial pollution, noise pollution, water pollution, ozone layer depletion due to greenhouse gases from industry and vehicles, excessive use of chemicals in agricultural sectors, etc. (Saadat et al., 2020).
7.1. Positive impact of COVID-19 on environment
7.1.1. Air pollution
The major air pollutants include nitrogen dioxide (NO2), carbon monoxide (CO), Sulfur dioxide (SO2), Ozone (O3), fine particulate matter (PM2.5), and coarse particulate matter (PM10). The sources of these types of pollutants are mostly from industries and automobile exhaust. Carbon monoxide (CO) gases are emitted from fossil fuel burning and heavy machinery. Sulfur dioxides (SO2) are sourced from motor vehicles, domestic heating and power generation unit., The emission of these gases affects the respiratory system, lungs, and mucus secretions. Nitrogen dioxide (NO2) reacts with air to release ozone which is mainly emitted by vehicle or industry and cause severe damage to the lungs that leads to breathing problem and they are the source of early childhood asthma. Particulate matter (PM) was mainly found to be sourced from acid rain and cause cancer because it can easily penetrate inside the lung’s cells. Based on the size, it is of two forms, namely PM10 and PM2.5. PM10 with a size less than 10 μm includes the pollens, molds and dust. PM2.5 is even smaller than PM10, causing adverse health effects like chronic obstructive pulmonary disease and lower respiratory infection, which has led to the death of nearly three million people worldwide. Another important toxic pollutant includes the Ozone (O3), which is formed from harmful gases emitted by vehicles or industry, causing severe breathing problems, lung-function reduction, triggers asthma and lung diseases. The spread of COVID-19 disease has led to completely shut down most of the industries as well as automobile traffic reduction, which resulted in a drastic decrease in air pollution universally (ESA, 2020 a; b).
7.1.2. Clean beaches
Beaches are considered an important natural resource found in coastal areas. They are the source of land, sand, fishing grounds for the survival of coastal communities. As far as the government is concerned, beaches are a good source of revenue in the form of tourism. But currently, most of the beaches are highly polluted due to anthropogenic activities. The lockdown situation due to COVID-19 in many countries has caused decreased movement of people in and around the coastal areas, which has led to clean beaches and clear waters around the surrounding areas (Zambrano-Monserrate et al., 2020).
7.1.3. Reduction of environmental noise level
The major cities around the world are highly contaminated nowadays with noise pollution, which is mostly due to human activities like automobile traffic, high volume speakers in commercial spaces, and sounds from various industries. These cause lots of discomfort and health-related problems to humans. Noise pollution affects animals psychologically and especially birds, which are highly sensitive. Since the government imposed the lockdown due to COVID-19, the reduction in all modes of transport and commercial activities has caused a huge drop in noise level around the world’s major cities (Zambrano-Monserrate and Ruano, 2019).
7.2. Negative impact of COVID-19 on environment
7.2.1. Increased waste
Many of the countries have imposed strict quarantine to control the spread of COVID-19 disease, which caused a vast increase in organic and inorganic waste. Since most of the essentials are ordered online for home delivery, wastes like food packaging and household goods have led to the rise of organic as well as inorganic waste. Apart from that, a huge amount of medical waste has been generated by hospitals. In the present situation, the governments are in a critical state to handle the sudden rise of medical waste (gloves, masks, and disposable aprons) generated from the hospitals. Even the public is aware of its proper disposal in these times. If they are not properly disposed of, they still may carry traces of viral contaminants and that can lead to severe problems in the future (Calma, 2020).
7.2.2. Reduction in waste recycling
Another major problem currently rising is waste recycling. Waste recycling is done to prevent pollution, save energy and conserve natural resources. Currently, the recycling waste management operations of most countries have ceased as these a pose to risk to the workers in recycling centers who may get infected as the household or medical waste may carry trace amounts of this contaminant. Most countries are trying to find a solution for proper as well as safe disposal of COVID-19 waste. Till then, waste management will be difficult to process (Bir, 2020).
8. Face mask
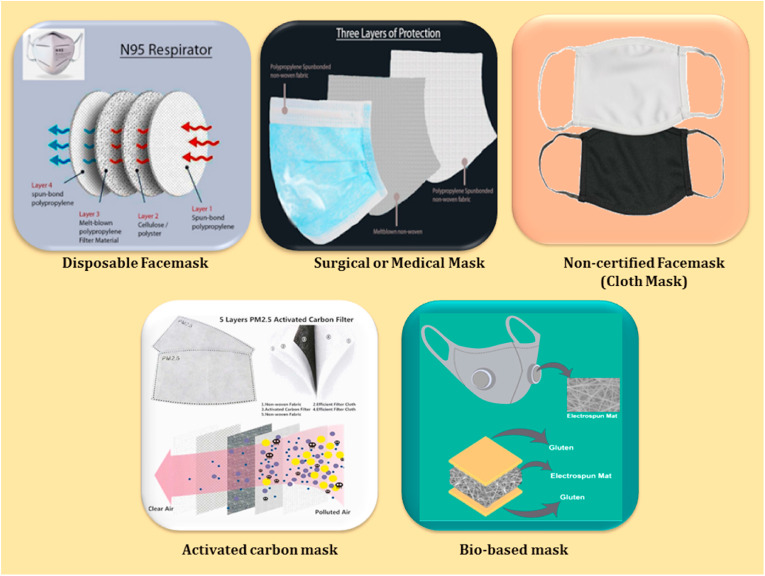
8.1. Types of face mask, its primary benefits and drawbacks
COVID-19 disease has emphasized the importance of global health care among people. The spread of the deadly virus can be optimally prevented or avoided by the effective usage of personal protective equipment (PPE) like gloves, face masks, air-purifying respirators, goggles, face shields and gowns among health care workers, the general public and infectious patients. One of the essential is the face mask, which has nowadays become a worldwide healthcare necessity. Though healthcare professionals are running many detection tests and other treatments, the main measures that have been focussed upon the general public by the world governments are the strict follow up of social distancing and certain other measures like safety protocols and good hygiene adoption. Previously these face masks (FFP2, FFP3, N95, KN95) are used only by occupational health and safety professionals, but now they have become common to everyone and have created a positive effect in the field of health and safety as well. This non-pharmacological face mask helps in the filtering of airborne particles, which are associated with health hazards and also prevent the rapid transmission of highly infectious diseases among each other. The main purpose of wearing a face mask is to ensure that the infected aerosols should not be expelled from them and transmitted to others. Currently, healthcare workers and the general public use this face mask daily, and it has become a universal requirement during this pandemic situation due to the lack of a vaccine or antiviral drugs (Carlos Rubio-Romero et al., 2020).
The quality of face mask has become a great obstacle among the public. Some metrics are followed to evaluate face mask performances, which include particle filtration efficiency (PFE), bacteria filtration efficiency (BFE), virus filtration efficiency (VFE), and filtering facepieces (FFP). Even the healthcare workers frequently in use of face mask would not be familiar with these types of metrics. Only limited official information has been provided to the public to select appropriate masks (Syed et al., 2003). Currently, three types of masks are in use by the health care workers as well as the public, namely i) Surgical or Medical mask, ii) Respirators (N95, FFP2) and iii) Non-certified mask (Cloth mask) (Fig. 5 ). Table 3 shows that the face mask types and its potential benefits.
-
i)
Surgical or Medical mask –The health care professionals use this type of mask. Generally, these consist of three layers, which can give protection as well as more air permeability. The inner layer is a standard non-woven fabric mainly used to absorb the moisture and release it by the wearer. The outer layer is a waterproof non-woven fabric used to isolate patient’s liquid sprayed. The filter layer in the middle is made from melt-blown material, which stops the microbes from entering and exiting the mask. The most common material which is used for making the mask is polypropylene. Other materials like polystyrene, polycarbonate, polyethylene, or polyester are also used to make masks of both 20 and 25 g per square meter (gsm) in density.
Fig. 5.
Different types of Masks that are currently in use as well as in research stage (Das et al., 2020, reproduced with permission).
Table 3.
Different types of Masks and its uses.
| TYPES OF MASKS | SURGICAL MASK | CLOTH MASKS | N95 RESPIRATORS | REFERENCES |
|---|---|---|---|---|
| Testing and Approval | European Standard EN 14683:2019 + AC: 2019, ASTM F2100- 11 in the United States, YY 0469 in China. | None | European Standard EN 149:2001 + A1: 2009, NIOSH-42CFR84 in the United States, GB2626-2006 in China. | AENOR, 2010; AFNOR 2020; Battelle, 2016; Bimedica, 2020a, b; Centers for Disease Control and Prevention, 2020a, Centers for Disease Control and Prevention, 2020b; ECDC, 2020a, b; FDA, 2020a, b; UNE, 2020. |
| Intended use and purpose | Fluid resistant and protects wearer from large droplets, splashes and bodily fluids | Helps protect others from you, not fluid resistant | Reduces wearer’s exposure to airborne particles including small particle aerosols and large fluid droplets. | |
| Breathability | Breathable | Breathable | Difficult | |
| Material | Non-Woven Fabric Polypropylene 3 Layers - Outer Layer-Hydrophobic Non-Woven layer, Middle layer - Melt blown filter, Inner layer -Soft absorbent Non-Woven layer | Cotton Filter paper, Nylon |
1st layer - Spun-bond polypropylene 2nd layer - Cellulose/Polyester 3rd layer -Melt-blown polypropylene Filter Material 4th layer – spun-bond polypropylene |
|
| Leakage | Leakage through mask edges | Leakage occurs throughout cloth | Minimal leakage. When [properly fitted and worn] | |
| Face Seal | Loose-fitted | Loose-fitted | Tight-fitted | |
| Filtration | Moderate level filtration | Low level filtration | High level filtration | |
| Limitation for usage | Disposable/Single use | Re-useable | Discard after each use, But can be used up to 5 times |
The filtering mechanism of medical masks is by Brownian diffusion, entrapment, inertial collision, gravity sedimentation and electrostatic adsorption. The first four are physical factors, that is, the characteristics of the non-woven fabric produced by the melt-blown method and the filterability rate is about 35%. A surgical mask is of loose-fitting type disposable device, but it does not filter or block very small particles in the air that may be transmitted by cough or sneeze. But they are effective barriers in retaining large droplets released from the mouth and nose by the wearer in public. It also helps in reducing exposure of the wearer’s saliva and respiratory secretions to others, which may travel up to 26 feet. The surgical mask protects the patients from contaminants, and it should not be worn for more than 3–8 h. The hypothetical part about the surgical mask is that it does not protect against “airborne” infectious agents. The advantages of using a surgical mask include its good filtering ability and disposable nature. The main disadvantage they possess includes the poor sealing ability and environmental pollution if not disposed of properly (Long et al., 2020).
-
ii)
Respirator (N95)– N95 respirators stop the contaminants, bacteria, and other matter from reaching the nose and mouth. They supply the user with clean air from a tank or other uncontaminated source. N95 respirators are one of the personal protective equipment that happens to be in high demand among healthcare workers while handling COVID-19 infected patients. This respirator filters out at least 95% of very small (0.3 microns) particles, including bacteria and viruses. They reduce the wearer’s exposure to airborne particles from small aerosol particles to large droplets. This type of mask has non-leakage proof around the edges of the respirator. N95 respirators are intended for single use in health care settings. CDC does not recommend the general public to wear N95 respirators to protect themselves from respiratory disease. Patients who possess chronic respiratory diseases or asthma should check with health care provider before using N95 respirators. The main advantages include the effective filtering of the surgical plume, bacteria, virus, fungi entering the mouth and allergens. N95 respirators generally have an excellent sealing effect. It may not feel comfortable to wear for long hours. The maximum time prescribed for wearing these types of respirators is 1–2 h and there is an increased chance of respiratory diseases among frequent users. It’s another polypropylene-based product that can act as pollutants to the environment (Radonovich et al., 2019).
-
iii)
Cloth Mask: There has been a high demand for medical masks or respirators during the COVID-19 spread. Due to shortage, many non-certified or home-made masks are in circulation among the public users. It has become popular among non-infected people as it tends to be more comfortable/breathable. These can be washed and reused. WHO recommended the fabric masks provided it consists of three layers, the outer layer of the mask should be water-resistant, the inner layer has to have water absorbent capacity and the middle layer should act as a filter. The cloth mask has less capacity in filtering the virus-containing droplets. It can still serve as an effective protective agent when the social distance is maintained among the infected and non-infected people. Wearing a cloth mask will not completely protect anyone from contracting the coronavirus, but it can reduce the possibility of spreading it. The main advantages of using a cloth mask are that these are easy to handle, cheap and reusable (Ho et al., 2020).
Many studies have exhibited that airborne particles cause respiratory, cardiovascular and pulmonary irregularities. Particles with a size of PM 2.5 will easily enter through the mouth or nose, reaching the alveolar cells of the lungs, causing asthma and cancer. A recent report suggested the nano-fiber-based filter can stop the inhalation of particles of size PM 2.5. Polysulfone-based nano-fibers are used to filter out the particles below PM 2.5 effectively. These nano-fibers can be used in the future to produce low-cost respirators and also will have longevity over other respirators that are currently available (Lim et al., 2004; Schlogl and Abd, 2009). Another study described the usage of carbon nanofibre and activated carbon as mask cartridges. These can effectively absorb and remove highly volatile organic vapors upon inhaling the air. These can act as a suitable substitute for normal respiratory cartridges because it has comparatively very low weight as well as acceptable absorption capacity (Jahangiri et al., 2012). A recent study, an update on the above observation with the same carbon nanofiber and activated carbon on impregnation with nickel nitrate catalyst exhibited still lesser weight and higher absorption capacities than previous findings. In the future, carbon nanofibers can be a suitable material for absorption and can be used with catalyst support for their unique properties, purity, mechanical strength and larger surface area (Jahangiri et al., 2013; Abbasinia et al., 2018).
Moreover, most of the currently available face masks are made from polypropylene, which is non-degradable, causing heavy environmental pollution. A sustainable way has to be adopted to develop face masks with excellent efficiency than the available ones. Recently researchers have designed a bio-based mask in which they used wheat gluten biopolymer that has been electrospun into nanofibre membranes and after that, they have carbonized them at over 700 °C to form a network structure. This mesh can act as the filter, and additionally, very low amounts of lanosol have been bonded and shaped by thermoforming to create the face masks. This type of bio-based mask that is completely biodegradable can effectively reduce the transmission of infectious diseases and also it will be an environmentally sustainable product (Das et al., 2020).
The Centre for Disease Control and Prevention (CDC) recommend that almost everyone wear a mask during the COVID-19 epidemic to control the spread of the infection (Centers for Disease Control and Prevention, 2020a, Centers for Disease Control and Prevention, 2020b). This situation has led to increased use of masks by people from the different sectors, which has caused a shortage of masks. It is estimated that approximately 89 million medical masks are needed each month to treat and take care of COVID-19 patients (WHO, 2020d). It is the prior responsibility of the government sectors, hospitals, pharmaceutical companies and researchers around the world to find a remedy on usage the mask vastly or to identify new personal protection equipment that has to be cost-effective as well as being reusable. In the coming days, most countries may lift the lockdown because continuous shutdown will affect their economy drastically, and also common people will get frustrated in staying home for a long time. During that time, there will be more requirements for masks.
8.2. Face masks - medical waste of COVID-19 a blooming threat to the marine ecosystem
During the COVID-19 pandemic, the demand for medical products and packaging has increased sharply. Due to this, the amount of hazardous medical waste generated is enormous when compared to normal conditions prevailing in any hospital around the world. Medical health sectors and waste management systems have already taken certain precautionary steps to control the contamination as well as disposal of the medical waste. But still, clearance of medical waste is increasing day by day and it is difficult for any government to find a solution very soon (Ho et al., 2020). Each individual must adopt certain measures for the safe disposal of face masks as well as other medical wastes. This is needed since whatever medical waste generated may carry a trace of infectious agents until a proper technology is acquired to destroy it completely. Some people may be more prone to medical waste exposure like cleaners, trash collectors and other people who spend much time in public places (Saadat et al., 2020).
Face masks are made mostly from plastic material, highly liquid-resistant and non-degradable and may carry traces even after being discarded. This kind of hazardous plastic waste either ends up in landfills or oceans, causing huge damage to that surrounding ecosystem. Health caretakers wearing surgical mask that cannot be worn more than a day and empty hand sanitizer bottles along with used tissue papers are disposed massively from each hospital which may end up as hazardous medical waste in future to the environment (Phan and Ching., 2020). The sudden usage of face mask, disposable gloves and hand sanitizers by billions of people will create an enormous amount of trash around the world. As a medical waste, its impact will be extended in the future and if these are not properly treated, it may cause deleterious effects to land and ocean ecosystem (Hellewell et al., 2020).
Medical waste like a disposable face mask, used gloves and gowns generated daily from hospitals has to be treated properly to destroy the remaining pathogens. The treatment technologies are based on thermal processes such as autoclaving, incineration and plasma or microwave treatment (Windfeld and Brooks, 2015; Liu et al., 2015). Most of the treatment facilities are designed to handle the average flow rate and composition of medical waste. Currently, the expected amount of medical waste generated during COVID-19 from hospitals exceeds the available capacity for the waste treatment of hazardous materials. In fact, compression or suppression of waste alone cannot effectively reduce the capacity. It also has to be ensured that pathogens contained in them are completely eradicated. After the pandemic subsides, it can be assumed that a large amount of treated waste will remain in the dump yard, which may or may not carry pathogens but still be left as a huge pollutant to the environment (Yu et al., 2020).
It has been estimated that nearly 90% of marine debris is composed of plastics, Styrofoam, food and packaging materials. Though the percentage of discarded fishing nets found in oceans is less, it still causes extensive trapping of marine organisms. They also cause the entangling of birds, turtles and other marine life forms. Currently, another growing concern is about microplastics that have been found in coastal as well as interior oceans. These are tiny bits of plastics with a size measuring less than 5 mm in diameter (Li et al., 2016). Microplastics are classified based on their origin into two types: 1) Primary and 2) Secondary microplastics (Avio et al., 2017). Micro-sized synthetic polymers are the primary microplastics that are utilized as exfoliates for several processes such as chemical preparations, sandblasting media, plastic goods maintenance, as well as synthetic clothing manufacturing. Another type of primary microplastic includes the microbeads (size < 2 mm) consisting of polyethylene (PE), polypropylene (PP), polystyrene (PS), which were used in cosmetic and health care products. Secondary microplastics are the disintegrated product of macro or meso plastics and are formed primarily by different environmental processes, such as hydrolysis, thermal degradation, photodegradation, biodegradation, and thermo-oxidative degradation (Sharma and Chatterjee, 2017). Plastic particles with a size of < 1 μm are referred as nanoplastics, and both of these microplastics and nanoplastics have possible consequences for the bioamplification and bioaccumulation of different chemicals and contaminants because of their large ratio of surface to volume (da Costa et al., 2016). These microplastics are easily washed down the drain and can enter the wastewater treatment plants or waste recycling facilities. But they don’t have filters fine enough to remove these microparticles and most likely, they are discharged into rivers along with the treated effluent or washed off as such, ending up in the oceans (Fig. 6 ).
Fig. 6.
Present and future plastic pollutants that exist in coastal and marine environment.
Because of their micron-sized particle existence, microplastics are persistent throughout the aquatic environment that is mistaken as food and eaten by various marine biota that includes phytoplankton’s, zooplanktons, corals, sea urchins, lobsters, fishes, etc. and are eventually gets transported to higher tropical levels. A problem of concern is the effect of microplastic on marine biota, as it contributes to entanglement and ingestion that can be lethal to marine life (Sharma and Chatterjee, 2017). Microplastics also have a detrimental impact on planktons, which play the most significant part in the marine ecosystem. The heterotrophic plankton undergoes the phagocytosis process when exposed to microplastics and holds these tiny plastic fragments in its tissues. Penetration of microplastics along the phytoplankton cell wall results in a decrease in chlorophyll absorption (Nerland et al., 2014). Zooplanktons have a crucial role in the marine environment, as these organisms are important primary consumers of the aquatic food chain. Zooplanktons have a variety of feeding pathways and they use the chemo-mechano receptor system for prey selection. The omnipresent presence of microplastics in marine environments results in interactions between microplastics and these zooplanktons, as both of them are of the same size (>333 μm), resulting in highly feasible interactions (Cole et al., 2013). Zooplankton appears to ingest beads of polystyrene with measurements between 1.7 and 30.6 μm. A well-known copepod, the Centropages typicus, was known to ingest microplastics of size 7.3 μm and gradually lost its feeding capacity, which had a negative impact on their health. In the benthic organism, Hyalella azteca, ingestion of polyethylene (PE) microplastics contributes to a decrease in the growth and reproduction process (Au et al., 2015). The uptake of microplastics in the Arenicola marina, a marine lugworm caused a decrease in their feeding capacity and weight loss (Besseling et al., 2013). By feeding on planktons, corals obtain energy to acquire important nutrients necessary for their growth, development and reproduction. In Australia, the Great Barrier Reef was firstly reported for the presence of microplastics in Scleractinian corals. The feeding coral experiment showed that corals eat these tiny fragments at a rate of ∼50 μg plastic cm−2 h−1 when exposed to microplastics. Microplastics’ exhibited an adverse effect on corals, including the accumulation of plastic particles in mesenterial tissue, leading to a decline in feeding potential and reduction in their energy reserves (Hankins et al., 2018).
Certain microplastic characteristics, such as microscopic size, attractive colors, and high buoyancy, make these tiny fragments readily accessible to fishes. By mistaking these particles as planktons or other natural prey, fishes eat microplastics. In a report, microplastic ingestion was observed in the Acanthochromis polyacanthus planktivorous fish where microplastics of < 300 μm size were present in the intestinal cavity of the individual fish (Critchell and Hoogenboom, 2018). Another study has shown that microplastic ingestion in fish induces metabolic changes, including up-regulation and down-regulation of fatty acids and amino acids (Lu et al., 2016). Particularly in the case of sea birds, the harmful effects of microplastic ingestion are a matter of concern as half of the species are endangered and the toxic impact of plastic particles has detrimental effects on their bodies that could cause changes in feeding behaviour, reproduction and mortality (Wilcox et al., 2015). Six species of sea birds, Phalacrocorax bougainvillii, Pelecanoides garnotii, Pelecanoides urinatrix, Pelecanus thagus, Spheniscus humboldti and Larus dominicanus were found to have plastic fragments in their stomach area, and maximum ingestion ability was detected in the case of Larus dominicanus, which typically feeds on fishing nets, waste disposal items and plastic containers (Thiel et al., 2018). Large marine biota species, including sharks, whales, dolphins, sea turtles and polar bears, are also prone to the ingestion of microplastics in oceans worldwide. In the stomach and intestine of the harbour seal, Phoca vitulina, the presence of microplastics was observed. This class of marine mammals were filter feeders and therefore ingests large quantities of microplastics either directly from ocean water or indirectly through the ingestion of the prey containing microplastics. The presence of microplastics in the intestine of sharks from Sea of Cortez and whales from the Mediterranean Sea showed that much of the world’s littered plastic waste inevitably ends up at sea and poses a significant threat to marine animals (Bravo Rebolledo et al., 2013; Gabbatiss, 2018).
8.3. Face masks - safe recycling and energy conversion
A higher volume of medical waste like masks, gloves and other protective equipment has been generated from infected and non-infected sources during the COVID-19 pandemic. In this situation, the most important aspect is the sound management of these medical wastes, which can reduce the unexpected health effects both on humans as well as the surroundings. For effective management of these medical wastes, it needs i) Proper identification (Infected or Non-infected), ii) Collection and separation, iii) Storage and transportation, iv) Treatment and disposal. It also requires certain associated factors for the waste management handlers like disinfection, personnel protection and training (Bourouiba, 2020).
The source of medical waste is generated from hospitals or advanced healthcare services and the patients infected by mild symptoms with self-quarantine facilities or the non-infected staying at home. Apart from the normal situation, it requires a specific protocol in the waste management system. It has to start with the sorting of the waste, its collection, treatment methodology and safety protocol for the waste handlers or workers. The countries of the world have taken numerous measures to handle the COVID-19 waste like double bagging with well-tied garbage bags for household waste as well as food containers, as these are now to be considered as hazardous because there may be a risk of pathogen contamination. In addition, suspected or positive cases are provided with separate waste collection systems. Though many precautionary steps are practiced, it still encourages the use of plastics as well as its generation as mixed waste. The COVID-19 pandemic has created a situation in which waste management systems, its associated economic and environmental issues, are of high concern and it must be carefully handled. But still, most countries have certain setbacks in tackling the current conditions (Association of cities and regions, 2020). Common techniques used for the COVID-19 waste treatment include the Incineration, Physical and Chemical methods. These techniques are applied at various stages in the Waste Management Systems (WMS) to handle the different types of waste that are carried by the COVID-19 Wastes (CW) (Ilyas et al., 2020). Incineration at a low or high temperature can be an efficient technology that can be adopted for handling the large some of CW and also, it would be sufficient investment for disinfecting pathological and pharmaceutical CW. Chemical disinfection combined with other technologies like Steam or autoclave disinfection techniques at later stages can be followed by the small investment hospitals for clearing the CW. Though incineration technology would efficiently degrade SARS-CoV-2 viruses at high temperatures still carries certain drawbacks like the release of toxins into the environment, which affects the immune system of humans and animals drastically (Ghodrat et al., 2017; Wang et al., 2020). Thermal technology is the latest technique that assist competently in degrading the CW and they are sub-classified into two types such as 1) Pyrolysis (operates at high temperatures), and 2) Microwave (operates at medium range temperatures) (Papari and Hawboldt, 2018).
Currently, plastic waste (mostly medical waste) generated during the pandemic has high calorific values when compared with other regular fuels. Plastics alone accounts for nearly 25% of calorific value in municipal solid waste. Pyrolysis and gasification were the techniques that have been adopted as additional sustainable waste treatment. The hidden energy in the plastics can be recovered through the recycling process like the usual mechanical or chemical methods, which are followed by the thermal processes. Most of this energy are lost when these are taken up to landfills as such or as a solid pollutant to the environment (Al-Salem, 2019).
Recycling plastics to be utilized as an energy source can be an alternative solution to overcome the current scenario, but there are some delays in executing it. Most recycling technologies are highly sensitive to purity (Lee et al., 2019; Cheng et al., 2020). The energy from recycled plastic or recycled waste can be utilized in the future as a replacement for fossil fuels. Currently, plastics have become an important application during COVID-19 management. But its usage can be minimized by providing awareness to the public and applying strict government regulations on its use. Often, plastics’ impact is not caused directly, but due to improper handling or disposal by the consumers. It then turns out as an environmentally hazardous pollutant (Zheng and Suh, 2019).
Few technologies can be applied for the recovery of energy from hazardous medical waste. Life cycle assessment and its associated methods can be a preferable alternative in treating hazardous medical waste. Burning of medical waste, which can release a high amount of energy as heat, can be recovered as well as the chemical content of plastics also can be recaptured by the process and utilized for useful purposes (Hong et al., 2018). Usage of life cycle assessment technology confirms that efficient heat energy has been recovered, causing minimal environmental impacts. However, the recovered heat energy usage still remains an obstacle and the emission of Products of Incomplete Combustion (PIC), dioxins and Furans in trace amount remains a problem. PIC’s are formed when the waste gets disintegrated during the treatment process and gets reorganized into small particles later on by post-combustion cooling. Dioxins are released unanimously on burning medical waste since most components are of plastics wastes. The metals which are carried by medical waste upon treatments are dispersed inside the reactor chamber and can act as a catalyst for the formation of dioxins. Furans coexist, along with the other toxins that are released during the treatment process. Toxins released during the process can store in fatty cells and run along the food chain. They are carcinogenic substances that can harm the immune system as well as causing an imbalance in hormonal secretions (Ilyas et al., 2020). The current concern is more on the safe disposal of medical waste rather than making energy recovery from it. Yet, the process of handling the huge amount of accelerating medical waste to energy recovery remains uncertain in a short period of time (Makarichi et al., 2018).
The occurrence and requirement of plastics in everyday life have led to the global presence of this hazardous material or pollutant in the environment (Klemes et al., 2020). Laws and regulations related to the discharge of plastics into the sea, implementation of biodegradable plastics, recycling and awareness campaigns can help in minimizing the problem of the use of plastics as well as its safe disposal. The other remedial measures that can be followed include enforcing strict environmental laws in the disposal of waste, wide knowledge on plastic waste management among the public and improvisation of recycled plastic product standards.
8.4. Challenges and future prospects
During COVID-19 outbreak, several types of medical and hazardous waste are generated, including used face masks, gloves, and other personal protective equipment. The coronavirus pandemic brings a new form of pollution as single-use personal protective equipment (PPE) floods our ocean. Plastic waste pollution was already considered as one of the major threats to our planet before the COVID-19 outbreak. The increased use of PPE to prevent the spread of the disease will now further contribute to this pollution. Millions of people are being advised to wear face masks to protect from the disease outbreak; however, little guidance has been given to the public about the safe disposal of the same and its recyclability. The lifting of lockdown restrictions in many countries translates to usage of billions of face masks every day globally.
Today, millions of used gloves and masks are being disposed every single day. The source of polluted medical waste is not limited to hospitals. Some advanced healthcare facilities have become insufficient for managing the rapidly increasing medical waste. To avoid the spread of COVID 19, wearing a face mask is considered a primary solution; on the other hand, this leads to an extraordinary increase in disposable mask production. Mostly, the face masks and other PPE are produced from long-lasting plastic materials. If not properly discarded, these can persist in the environment from decades to hundreds of years and create several problems for the people and the environment. In this context, special attention should be taken care to save our ecosystem. These pollutants must be treated as hazardous medical waste because they may carry the risk of contamination with pathogens (Klemes et al., 2020).
The patients with mild symptoms/suspected cases who self-isolate at home also contribute to this medical waste. They should be educated on the use of separate waste collection systems. The PPE, which is made from plastic materials, first breaks down into microplastic and then to nanoplastics. These nano plastic particles and fibers are long-lived polymers that can affect the food chains. Therefore, the governments worldwide should promote the environmentally friendly production of PPE, which are non-toxic, biodegradable, or easily recyclable alternatives that come from rice husk, a natural fiber obtained from plants, etc. Concerning the PPE pollution in the ocean, a single solution can’t solve this issue; however, it should be brought through by rapid and concerted action by which we can break the plastic pollution.
This constant increase in the quantity of wastes makes it imperative for new and better waste treatment methods to be created. Traditional methods of waste management, such as composting, landfilling and incineration, are obsolete and should be replaced by new solutions that are reliable and easy to run. As we look forward to a post-COVID-19 future, it will be of primary concern to counter fear-driven prejudices toward hygiene of reused and recycled goods. Investments in safety gear and physical facilities for sorting, collecting and recycling will restore the trust of sanitation workers in the safety of waste handling and can contribute to clear, homogeneous streams of plastic waste for recyclers. Automation and creativity in current as well as the emerging technologies into collection and segregation will help in effective waste management services.
9. Conclusion
The COVID-19 pandemic has been continuously causing heavy damage to the people around the world. Lots of life has been taken up by the virus and it still continues. For the control of the virus spreading, health care personnel, essential workers and the general public have to be completely reliant on personal protective equipment on this occasion. Nowadays, face mask has become an essential commodity and huge tons are manufactured every day to meet the world’s needs. They are mostly derived from petrochemicals as raw materials that are non-degradable and are considered as one of the hazardous medical waste now as well as in the future. There has been an alarming rise in face mask usage as well as other medical waste from hospitals and household garbage. It has become a huge task for the world countries to clear this particular waste, which may or may not carry a trace of infectious agents along with them. A constructive methodology or system has to be adopted by world countries for effective management of increasing medical waste. Adequate waste recycling or its conversion to other energy forms may be an excellent solution that can be implemented by any government to control the current situation. If the generated medical wastes are not properly treated now, its impact will be extended in the future and also may cause deleterious effects to the land and ocean ecosystem. An alternative to overcome the problem is improvised face mask production either made through nanotechnology or biomaterial, which should possess an equal or better efficiency than the conventional ones and should be completely biodegradable so that it may not harm the terrestrial as well as the marine ecosystem.
Credit authors statement
The authors: Selvakumar Dharmaraj, Sneha Hariharan, and Akila Manibharathi were involved in data collection and manuscript preparation.
Author Veeramuthu Ashokkumar was involved in the manuscript preparation and reviewing process.
The authors Pau Loke Show, Chong Cheng Tung, and Chawalit Ngamcharussrivichai helped in writing, reviewing, and editing the manuscript.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
The authors are grateful to the financial supports from Center of Excellence in Catalysis for Bioenergy and Renewable Chemicals (CBRC); Center of Excellence on Petrochemical and Materials Technology (PETROMAT), Chulalongkorn University, and Thailand Science Research Innovation (TSRI) under the International Research Network: Functional Porous Materials for Catalysis and Adsorption (Contract No. IRN61W0003)..
Handling Editor: Derek Muir
References
- Abbasinia M., Karimie S., Haghighat M., Mohammadfam I. Application of nanomaterials in personal respiratory protection equipment: a literature review. Saf. Now. 2018;4:47. [Google Scholar]
- Adams M.J., Lefkowitz E.J., King A.M.Q., Harrach B., Harrison R.L., Knowles N.J., Kropinski A.M., Krupovic M., Kuhn J.H., Mushegian A.R., Nibert M.L., Sabanadzovic S., Sanfaçon H., Siddell S.G., Simmonds P., Varsani A., Zerbini F.M., Orton R.J., Smith D.B., Gorbalenya A.E., Davison A.J. 50 years of the international committee on taxonomy of viruses: progress and prospects. Arch. Virol. 2017;162:1441–1446. doi: 10.1007/s00705-016-3215-y. [DOI] [PubMed] [Google Scholar]
- Adhikari S.P., Meng S., Wu Y.J., Mao Y.P., Ye R.X., Wang Q.Z., Sun C., Sylvia S., Rozelle S., Raat H., Zhou H. Epidemiology, causes, clinical manifestation and diagnosis, prevention and control of coronavirus disease (COVID-19) during the early outbreak period: a scoping review. Infect. Dis Poverty. 2020;9:29. doi: 10.1186/s40249-020-00646-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- AENOR UNE-EN 149:2001+A1:2010. Respiratory Protective Devices. Filtering half mask to protect against particles. 2010. https://www.aenor.com/normas-y-libros/buscador-de-normas/UNE?c=N0044643 Requirements, testing, marking. Available on 9th April 2020 at.
- AFNOR . Association française de Normalisation AFNOR; 2020. AFNOR SPEC S76-001 Barrier Masks. Guide to Minimum Requirements, Test Methods, Preparation and Use for Mass Manufactured and Homemade Masks.https://iv.revistalocal.es/wp-content/uploads/AFNORSpec-S76-001-MascarillasDeProteccion.pdf Available on 9th of April 2020 at. [Google Scholar]
- Alanagreh L., Alzoughool F., Atoum M. The Human Coronavirus Disease COVID-19: its origin, characteristics, and insights into potential drugs and its mechanisms. Pathogens. 2020;9(5):331. doi: 10.3390/pathogens9050331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Salem S.M. Plastics to Energy. William Andrew, Elsevier; Amsterdam, Netherlands: 2019. Energy production from plastic solid waste (PSW) pp. 45–64. [Google Scholar]
- Annan A., Baldwin H.J., Corman V.M., Klose S.M., Owusu M., Nkrumah E.E., Agbenyega O., Meyer B., Oppong S., Sarkodie Y.A., Kalko E.K.V., Lina P.H.C., Godlevska E.V., Reusken C., Seebens A., Gloza-Rausch F., Vallo P., Tschapka M., Drosten C., Drexler J.F. Human betacoronavirus 2c EMC/2012–related viruses in bats, Ghana and Europe. Emerg. Infect. Dis. 2013;19(3):456–459. doi: 10.3201/eid1903.121503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Association of cities and regions for sustainable resource management. 2020. www.acrplus.org/en/municipal-waste-management-covid- 19 [Google Scholar]
- Avio C.G., Gorbi S., Regoli F. Plastics and microplastics in the oceans: from emerging pollutants to emerged threat. Mar. Environ. Res. 2017;128:2–11. doi: 10.1016/j.marenvres.2016.05.012. [DOI] [PubMed] [Google Scholar]
- Au S.Y., Bruce T.F., Bridges W.C., Klaine S.J. Responses of Hyalella azteca to acute and chronic microplastic exposures. Environ. Toxicol. Chem. 2015;34(11):2564–2572. doi: 10.1002/etc.3093. [DOI] [PubMed] [Google Scholar]
- Battelle . FDA; 2016. Final Report for the Bioquell Hydrogen Peroxide Vapor (HPV) Decontamination for Reuse of N95 Respirators.https://www.fda.gov/media/136386/download U.S.A. Available on 9th April 2020 at. [Google Scholar]
- Belouzard S., Chu V.C., Whittaker G.R. Activation of the SARS coronavirus spike protein via sequential proteolytic cleavage at two distinct sites. Proc. Natl. Acad. Sci. U. S. A. 2009;106(14):5871–5876. doi: 10.1073/pnas.0809524106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belouzard S., Millet J.K., Licitra B.N., Whittaker G.R. Mechanisms of coronavirus cell entry mediated by the viral spike protein. Viruses. 2012;4(6):1011–1033. doi: 10.3390/v4061011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bennardo F., Buffone C., Giudice A. New therapeutic opportunities for COVID-19 patients with Tocilizumab: possible correlation of interleukin-6 receptor inhibitors with osteonecrosis of the jaws. Oral Oncol. 2020;106:104659. doi: 10.1016/j.oraloncology.2020.104659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Besseling E., Wegner A., Foekema E.M., van den Heuvel-Greve M.J., Koelmans A.A. Effects of microplastic on fitness and PCB bioaccumulation by the lugworm Arenicola marina (L.) Environ. Sci. Technol. 2013;47(1):593–600. doi: 10.1021/es302763x. [DOI] [PubMed] [Google Scholar]
- Bimedica Naturcare® vertical FFP2. 2020. https://www.bimedica.com/catalogo-de-productos/naturcare-mascarillas-de-proteccionvertical-ffp2 Available on 15th April 2020 at.
- Bimedica Naturcare® cónica FFP3. 2020. https://www.bimedica.com/catalogo-de-productos/naturcare-mascarillas-de-proteccionconica-ffp3 Available on 15th April 2020 at.
- Bir B. 2020. https://www.aa.com.tr/en/health/single-use-items-not-safest-option-amidcovid-19/1787067
- Bosch B.J., van der Zee R., de Haan C.A., Rottier P.J. The coronavirus spike protein is a class I virus fusion protein: structural and functional characterization of the fusion core complex. J. Virol. 2003;77(16):8801–8811. doi: 10.1128/JVI.77.16.8801-8811.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bourouiba L. Turbulent gas clouds and respiratory pathogen emissions - potential implications for reducing transmission of COVID-19. J. Am. Med. Assoc. 2020;323(18):1837–1838. doi: 10.1001/jama.2020.4756. [DOI] [PubMed] [Google Scholar]
- Bravo Rebolledo E.L., Van Franeker J.A., Jansen O.E., Brasseur S.M. Plastic ingestion by harbour seals (Phoca vitulina) in The Netherlands. Mar. Pollut. Bull. 2013;67(1–2):200–202. doi: 10.1016/j.marpolbul.2012.11.035. [DOI] [PubMed] [Google Scholar]
- Calma J. 2020. https://www.theverge.com/2020/3/26/21194647/the-covid-19-pandemic- is-generating-tons-of-medical-waste
- Carlos Rubio-Romero J., Del Carmen Pardo-Ferreira M., Antonio Torrecilla García J., Calero-Castro S. Disposable masks: disinfection and sterilization for reuse, and non-certified manufacturing, in the face of shortages during the COVID-19 pandemic. Saf. Sci. 2020;129:104830. doi: 10.1016/j.ssci.2020.104830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention Novel coronavirus, wuhan, China. 2020. 2019. https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/prevention.html Available online:
- Centers for Disease Control and Prevention Decontamination and reuse of filtering facepiece respirators. 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/ppe-strategy/decontamination-reuse-respirators.html Available on 9th April 2020 at.
- Centers for Disease Control and Prevention Use of cloth face coverings to help slow the spread of COVID-19. 2020. https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/diy-cloth-face-coverings.html Available on 12 th April 2020 at.
- Chan J.F.W., Kok K.H., Zhu Z., Chu H., To K.K.W., Yuan S., Yuen K.Y. Genomic characterization of the 2019 novel human-pathogenic coronavirus isolated from a patient with atypical pneumonia after visiting. Wuhan. Emerg. Microb. Infect. 2020;9(1):221–236. doi: 10.1080/22221751.2020.1719902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan J.F.W., Yuan S., Kok K.H., To K.K.W., Chu H., Yang J., Xing F., Liu J., Yip C.C.Y., Poon R.W.S., Tsoi H.W., Lo S.K.F., Chan K.H., Poon V.K.M., Chan W.M., Ip J.D., Cai J.P., Cheng V.C.C., Chen H., Hui C.K.M., Yuen K.Y. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-toperson transmission: a study of a family cluster. Lancet. 2020;395:514–523. doi: 10.1016/S0140-6736(20)30154-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen C., Zhang X.R., Ju Z.Y., He W.F. Advances in the research of cytokine storm mechanism induced by Corona Virus Disease 2019 and the corresponding immunotherapies. Zhonghua Shao Shang Za Zhi. 2020;36(6):471–475. doi: 10.3760/cma.j.cn501120-20200224-00088. [DOI] [PubMed] [Google Scholar]
- Chen Y., Guo Y., Pan Y., Zhao Z.J. Structure analysis of the receptor binding of 2019-nCoV. Biochem. Biophys. Res. Commun. 2020;525(1):135–140. doi: 10.1016/j.bbrc.2020.02.071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Y., Liu Q., Guo D. Emerging coronaviruses: genome structure, replication, and pathogenesis. J. Med. Virol. 2020;92:418–423. doi: 10.1002/jmv.25681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng S.Y., Tan X., Show P.L., Rambabu K., Banat F., Ashokkumar V., Lau B.F., Ng E.P., Ling T.C. Incorporating biowaste into circular bioeconomy: a critical review of current trend and scaling up feasibility. Environ. Technol. Innov. 2020;19:101034. [Google Scholar]
- Chhikara B.S., Rathi B., Singh J., Poonam F.N.U. Corona virus SARS-CoV-2 disease COVID-19: infection, prevention and clinical advances of the prospective chemical drug therapeutics. Chem. Biol. Lett. 2020;7(1):63-72. [Google Scholar]
- Cole M., Lindeque P., Fileman E., Halsband C., Goodhead R., Moger J., Galloway T.S. Microplastic ingestion by zooplankton. Environ. Sci. Technol. 2013;47(12):6646–6655. doi: 10.1021/es400663f. [DOI] [PubMed] [Google Scholar]
- Critchell K., Hoogenboom M.O. Effects of microplastic exposure on the body condition and behaviour of planktivorous reef fish (Acanthochromis polyacanthus) PloS One. 2018;13(3) doi: 10.1371/journal.pone.0193308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cui L., Wang H., Ji Y., Yang J., Xu S., Huang X., Wang Z., Qin L., Tien P., Zhou X., Guo D., Chen Y., The nucleocapsid protein of coronaviruses acts as a viral suppressor of RNA silencing in mammalian cells. J. Virol. 89, 9029–9043. The nucleocapsid protein of coronaviruses acts as a viral suppressor of RNA silencing in mammalian cells. J. Virol. 2015;89:9029–9043. doi: 10.1128/JVI.01331-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Czub M., Weingartl H., Czub S., He R., Cao J. Evaluation of modified vaccinia virus Ankara based recombinant SARS vaccine in ferrets. Vaccine. 2005;23:2273e9. doi: 10.1016/j.vaccine.2005.01.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- da Costa J.P., Santos P.S.M., Duarte A.C., Rocha-Santos T. Nano)plastics in the environment - sources, fates and effects. Sci. Total Environ. 2016;566–567:15–26. doi: 10.1016/j.scitotenv.2016.05.041. [DOI] [PubMed] [Google Scholar]
- Das O., Neisiany R.E., Capezza A.J., Hedenqvist M.S., Forsth M., Xu Q., Jiang L., Ji D., Ramakrishna S. The need for fully bio-based facemasks to counter coronavirus outbreaks: a perspective. Sci. Total Environ. 2020;736:139611. doi: 10.1016/j.scitotenv.2020.139611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Haan C.A.M., Kuo L., Masters P.S., Vennema H., Rottier P.J.M. Coronavirus particle assembly: primary structure requirements of the membrane protein. J. Virol. 1998;72(8):6838e50. doi: 10.1128/jvi.72.8.6838-6850.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeDiego M.L., Álvarez E., Almazán F., Rejas M.T., Lamirande E., Roberts A., Shieh W.J., Zaki S.R., Subbarao K., Enjuanes L. A severe acute respiratory syndrome coronavirus that lacks the E Gene is attenuated in vitro and in vivo. J. Virol. 2006;81:1701–1713. doi: 10.1128/JVI.01467-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Demogines A., Farzan M., Sawyer S. Evidence for ACE2-Utilizing Coronaviruses (CoVs) related to severe acute respiratory syndrome CoV in Bats. J. Virol. 2012;86:6350–6353. doi: 10.1128/JVI.00311-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong L., Hu S., Gao J. Discovering drugs to treat coronavirus disease 2019 (COVID-19) Drug Discov. Ther. 2020;14:58–60. doi: 10.5582/ddt.2020.01012. [DOI] [PubMed] [Google Scholar]
- Dutta A.K. Vaccine against covid-19 disease - present status of development. Indian J. Pediatr. 2020;87(10):810–816. doi: 10.1007/s12098-020-03475-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ESA 2020. https://www.esa.int/Applications/Observing_the_Earth/Copernicus/Sentinel-5P/COVID-19_nitrogen_dioxide_over_China
- ESA 2020. https://www.esa.int/Applications/Observing_the_Earth/Copernicus/Sentinel-5P/Coronavirus_lockdown_leading_to_drop_in_pollution_across_Europe
- European Centre for Disease Prevention and Control (ECDC) Using face masks in the community. 2020. https://www.ecdc.europa.eu/sites/default/files/documents/COVID-19-use-face-masks-community.pdf Available on 9th April 2020 at.
- European Centre for Disease Prevention and Control (ECDC) Cloth masks and mask sterilisation as options in case of shortage of surgical masks and respirators. 2020. https://www.ecdc.europa.eu/en/publications-data/clothmasks-sterilisation-options-shortage-surgical-masks-respirators Available on 8th April 2020 at.
- Fadda M., Albanese E., Suggs L.S. When a COVID-19 vaccine is ready, will we all be ready for it? Int. J. Publ. Health. 2020;65:711–712. doi: 10.1007/s00038-020-01404-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fehr A.R., Perlman S. vol. 1282. Springer; Berlin/Heidelberg, Germany: 2015. Coronaviruses: an overview of their replication and pathogenesis; pp. 1–23. (Therapeutic Antibodies). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Food and Drug Administration Stakeholders for non-NIOSH-approved imported FFRs. 2020. https://www.fda.gov/media/136403/download Available on 10th April 2020 at.
- Food and Drug Administration Stakeholders for non-NIOSH-approved imported FFRs made in China. 2020. https://www.fda.gov/media/136664/download Available on 10th April 2020 at.
- Gabbatiss J. Microplastics ‘pose major threat’ to whales and sharks, scientists warn. Independent. 2018 Monday 5 February 2018 06:15. [Google Scholar]
- Gao J., Tian Z., Yang X. Breakthrough: chloroquine phosphate has shown apparent efficacy in treatment of COVID-19 associated pneumonia in clinical studies. Biosci. Trends. 2020;14:72–73. doi: 10.5582/bst.2020.01047. [DOI] [PubMed] [Google Scholar]
- Gennaro F.D., Pizzol D., Marotta C., Antunes M., Racalbuto V., Veronese N., Smith L. Coronavirus diseases (COVID-19) current status and future perspectives: a narrative review. Int. J. Environ. Res. Publ. Health. 2020;17(8):2690. doi: 10.3390/ijerph17082690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghodrat M., Rashidi M., Samali B. In: Energy Technology 2017, 131-143. The Minerals, Metals & Materials Series. Zhang L., et al., editors. Springer; Cham: 2017. Life cycle assessments of incineration treatment for sharp medical waste. [Google Scholar]
- Global carbon Project. 2020. https://www.globalcarbonproject.org/carbonbudget/index [Google Scholar]
- Gorbalenya A.E., Lauber C., Siddell S. Reference Module in Biomedical Sciences. Elsevier; 2019. Taxonomy of viruses. [Google Scholar]
- Gralinski L.E., Menachery V.D. Return of the coronavirus: 2019-nCoV. Viruses. 2020;12(2):135. doi: 10.3390/v12020135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo Y.R., Cao Q.D., Hong Z.S., Tan Y.Y., Chen S.D., Jin H., Tan K.S., Wang D.Y., Yan Y. The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak - an update on the status. Mil. Med Res. 2020;7:1–10. doi: 10.1186/s40779-020-00240-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hankins C., Duffy A., Drisco K. Scleractinian coral microplastic ingestion: potential calcification effects, size limits, and retention. Mar. Pollut. Bull. 2018;135:587–593. doi: 10.1016/j.marpolbul.2018.07.067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hellewell J., Abbott S., Gimma A., Bosse N.I., Jarvis C.I., Russell T.W., Munday J.D., Kucharski A.J., Edmunds W.J., Sun F J T L GH. Feasibility of controlling COVID-19 outbreaks by isolation of cases and contacts. Lancet Glob. Health. 2020;8(4):488–496. doi: 10.1016/S2214-109X(20)30074-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ho K.F., Lin L.Y., Weng S.P., Chuang K.J. Medical mask versus cotton mask for preventing respiratory droplet transmission in micro environments. Sci. Total Environ. 2020;735:139510. doi: 10.1016/j.scitotenv.2020.139510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoffmann M., Kleine-Weber H., Schroeder S., Krüger N., Herrler T., Erichsen S., Schiergens T.S., Herrler G., Wu N.H., Nitsche A., Muller M.A., Drosten C., Pohlmann S. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. 2020;181:271–280. doi: 10.1016/j.cell.2020.02.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hong J., Zhan S., Yu Z., Hong J., Qi C. Life-cycle environmental and economic assessment of medical waste treatment. J. Clean. Prod. 2018;174:65–73. [Google Scholar]
- Hopman J., Allegranzi B., Mehtar S. Managing COVID-19 in low- and middle-income countries. J. Am. Med. Assoc. 2020;323(16):1549–1550. doi: 10.1001/jama.2020.4169. html. [DOI] [PubMed] [Google Scholar]
- Hui D.S., Azhar E.I., Madani T.A., Ntoumi F., Kock R., Dar O., Ippolito G., Mchugh T.D., Memish Z.A., Drosten C., Zumla A., Petersen E. The continuing 2019-nCoV epidemic threat of novel coronaviruses to global health - the latest 2019 novel coronavirus outbreak in Wuhan, China. Int. J. Infect. Dis. 2020;91:264–266. doi: 10.1016/j.ijid.2020.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hussain A., Kaler J., Tabrez E., Tabrez S., Tabrez S.S.M. Novel COVID-19: a comprehensive review of transmission, manifestation, and pathogenesis. Cureus. 2020;12(5) doi: 10.7759/cureus.8184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huynh J., Li S., Yount B., Smith A., Sturges L., Olsen J.C., Nagel J., Johnson J.B., Agnihothram S., Gates J.E., Frieman M.B., Baric R.S., Donaldson E.F. Evidence supporting a zoonotic origin of human coronavirus strain NL63. J. Virol. 2012;86(23):12816–12825. doi: 10.1128/JVI.00906-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ICTV Code . 2018. The International Code of Virus Classification and Nomenclature.https://talk.ictvonline.org/information/w/ictv-information/383/ictv-code 2018. [Google Scholar]
- Ilyas S., Srivastava R.R., Kim H. Disinfection technology and strategies for COVID-19 hospital and bio-medical waste management. Sci. Total Environ. 2020;749:141652. doi: 10.1016/j.scitotenv.2020.141652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jahangiri M., Adl J., Shahtaheri S.J., Rashidi A., Ghorbanali A., Kakooe H., Forushani A.R., Ganjali M.R. Preparation of a new adsorbent from activated carbon and carbon nanofiber (AC/CNF) for manufacturing organic-vacbpour respirator cartridge. Iran. J. Environ. Health Sci. Eng. 2013;10(1):15. doi: 10.1186/1735-2746-10-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jahangiri M., Shahtaheri S.J., Adl J., Rashidi A., Clark K., Sauvain J.J., Riediker M. Emission of carbon nanofiber (CNF) from CNF-containing composite adsorbents. J. Occup. Environ. Hyg. 2012;9:130–135. doi: 10.1080/15459624.2012.691335. [DOI] [PubMed] [Google Scholar]
- Kan B., Wang M., Jing H., Xu H., Jiang X., Yan M., Liang W., Zheng H., Wan K., Liu Q., Cui B., Xu Y., Zhang E., Wang H., Ye J., Li G., Li M., Cui Z., Qi X., Chen K., Du L., Gao K., Zhao Y.T., Zou X.Z., Feng Y.J., Gao Y.F., Hai R., Yu D., Guan Y., Xu J. Molecular evolution analysis and geographic investigation of severe acute respiratory syndrome coronavirus-like virus in palm civets at an animal market and on farms. J. Virol. 2005;79(18):11892–11900. doi: 10.1128/JVI.79.18.11892-11900.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaur S.P., Gupta V. COVID-19 Vaccine: a comprehensive status report. Virus Res. 2020;288:198114. doi: 10.1016/j.virusres.2020.198114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirchdoerfer R.N., Cottrell C.A., Wang N., Pallesen J., Yassine H.M., Turner H.L., Corbett K.S., Graham B.S., McLellan J.S., Ward A.B. Pre-fusion structure of a human coronavirus spike protein. Nature. 2016;531(7592):118–121. doi: 10.1038/nature17200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klemes J.J., Fan Y.V., Tan R.R., Jiang P. Minimising the present and future plastic waste, energy and environmental footprints related to COVID-19. Renew. Sustain. Energy Rev. 2020;127:109883. doi: 10.1016/j.rser.2020.109883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lau S.K., Li K.S., Tsang A.K., Lam C.S., Ahmed S., Chen H., Chan K.H., Woo P.C.Y., Yuen K.Y. Genetic characterization of Betacoronavirus lineage C viruses in bats reveals marked sequence divergence in the spike protein of pipistrellus bat coronavirus HKU5 in Japanese pipistrelle: implications for the origin of the novel Middle East respiratory syndrome coronavirus. J. Virol. 2013;87(15):8638–8650. doi: 10.1128/JVI.01055-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee S.Y., Sankaran R., Chew K.W., Tan C.H., Rambabu K., Chu D.T., Show P.L. Waste to bioenergy: a review on the recent conversion technologies. BMC Energy. 2019;1:4. [Google Scholar]
- Lei J., Kusov Y., Hilgenfeld R. Nsp3 of coronaviruses: structures and functions of a large multi-domain protein. Antivir. Res. 2018;149:58–74. doi: 10.1016/j.antiviral.2017.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Letko M., Marzi A., Munster V. Functional assessment of cell entry and receptor usage for SARS-CoV-2 and other lineage B betacoronaviruses. Nat. Microbiol. 2020;5:562–569. doi: 10.1038/s41564-020-0688-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li B., Si H.-R., Zhu Y., Yang X.-L., Anderson D.E., Shi Z.-L., Wang L.-F., Zhou P. Discovery of bat coronaviruses through surveillance and probe capture-based next-generation sequencing. mSphere. 2020;5:e00807–e00819. doi: 10.1128/mSphere.00807-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li W., Moore M.J., Vasilieva N., Sui J., Wong S.K., Berne M.A., Somasundaran M., Sullivan J.L., Luzuriaga K., Greenough T.C., Choe H., Farzan M. Angiotensin-converting enzyme 2 is a functional receptor for the SARS coronavirus. Nature. 2003;426(6965):450–454. doi: 10.1038/nature02145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li W.C., Tse H.F., Fok L. Plastic waste in the marine environment: a review of sources, occurrence and effects. Sci. Total Environ. 2016;566:333–349. doi: 10.1016/j.scitotenv.2016.05.084. [DOI] [PubMed] [Google Scholar]
- Li X., Geng M., Peng Y., Meng L., Lu S. Molecular immune pathogenesis and diagnosis of COVID-19. J. Pharm. Anal. 2020;10(2):102–108. doi: 10.1016/j.jpha.2020.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lim S., Yoon S.H., Shimizu Y., Jung H., Mochida I. Surface control of activated carbon fiber by growth of carbon nanofiber. Langmuir. 2004;20:5559–5563. doi: 10.1021/la036077t. [DOI] [PubMed] [Google Scholar]
- Liu H.C., You J.X., Lu C., Chen Y.Z. Evaluating healthcare waste treatment technologies using a hybrid multi-criteria decision-making model. Renew. Sustain. Energy Rev. 2015;41:932–942. [Google Scholar]
- Long Y., Hu T., Liu L., Chen R., Guo Q., Yang L., Che Y., Huang J., Du L. Effectiveness of N95 respirators versus surgical masks against influenza: a systematic review and meta-analysis. J. Evid. Base Med. 2020;2020:1–9. doi: 10.1111/jebm.12381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu H. Drug treatment options for the 2019-new coronavirus (2019-nCoV) Biosci. Trends. 2020;14:69–71. doi: 10.5582/bst.2020.01020. [DOI] [PubMed] [Google Scholar]
- Lu Y., Zhang Y., Deng Y., Jiang W., Zhao Y., Geng J., Ding L., Ren H. Uptake and accumulation of polystyrene microplastics in zebrafish (Danio rerio) and toxic effects in liver. Environ. Sci. Technol. 2016;50(7):4054–4060. doi: 10.1021/acs.est.6b00183. [DOI] [PubMed] [Google Scholar]
- Lu H., Stratton C.W., Tang Y.W. Outbreak of pneumonia of unknown etiology in Wuhan, China: the mystery and the miracle. J. Med. Virol. 2020;92:401–402. doi: 10.1002/jmv.25678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lupia T., Scabini S., Mornese Pinna S., Di Perri G., De Rosa F.G., Corcione S. 2019 novel coronavirus (2019-nCoV) outbreak: a new challenge. J. Glob. Antimicrob. Resist. 2020;21:22–27. doi: 10.1016/j.jgar.2020.02.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Makarichi L., Jutidamrongphan W., Techato K. The evolution of waste-to-energy incineration: a review. Renew. Sustain. Energy Rev. 2018;91:812–821. [Google Scholar]
- Martinez M.A. Compounds with therapeutic potential against novel respiratory 2019 coronavirus. Antimicrob. Agents Chemother. 2020. 2020;64(5) doi: 10.1128/AAC.00399-20. e00399-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masters P.S. vol. 66. Elsevier; Amsterdam, The Netherlands: 2006. pp. 193–292. (The Molecular Biology of Coronaviruses). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Millet J.K., Whittaker G.R. Host cell entry of Middle East respiratory syndrome coronavirus after two-step, furin-mediated activation of the spike protein. Proc. Natl. Acad. Sci. U. S. A. 2014;111(42):15214–15219. doi: 10.1073/pnas.1407087111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nerland I.L., Halsband C., Allan I., Thomas K.V. vol. 14338. 2014. (Microplastics in Marine Environments: Occurrence, Distribution and Effects. Oslo, Project). Report no. 6754-2014. [Google Scholar]
- Neuman B., Kiss G., Kunding A., Bhella D., Baksh M.F., Connelly S., Droese B., Klaus J.P., Makino S., Sawicki S.G., Siddell S.G., Stamou D.G., Wilson I.A., Kuhn P., Buchmeier M.J. A structural analysis of M protein in coronavirus assembly and morphology. J. Struct. Boil. 2010;174:11–22. doi: 10.1016/j.jsb.2010.11.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nirban L., Upendra K. Plastics and microplastics: a threat to environment. Environ. Technol. Innov. 2019;14:100352. [Google Scholar]
- Ou X., Liu Y., Lei X., Li P., Mi D., Ren L., Guo L., Guo R., Chen T., Hu J., Xiang Z., Mu Z., Chen X., Chen J., Hu K., Jin Q., Wang J., Qian Z. Characterization of spike glycoprotein of SARS-CoV-2 on virus entry and its immune cross-reactivity with SARS-CoV. Nat. Commun. 2020;11(1):1620. doi: 10.1038/s41467-020-15562-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paden C., Yusof M., Al Hammadi Z., Queen K., Tao Y., Eltahir Y., Elsayed E.A., Marzoug B.A., Bensalah O.K.A., Khalafalla A.I., Al Mulla M., Khudhair A., Elkheir K.A., Issa Z.B., Pradeep K., Elsaleh F.N., Imambaccus H., Sasse J., Weber S., Shi M., Zhang J., Li Y., Pham H., Kim L., Hall A.J., Gerber S.I., Al Hosani F.I., Tong S., Al Muhairi S.S.M. Zoonotic origin and transmission of Middle East respiratory syndrome coronavirus in the UAE. Zoonoses. Public. Health. 2018;65(3):322–333. doi: 10.1111/zph.12435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Papari S., Hawboldt K. A review on condensing system for biomass pyrolysis process. Fuel Process. Technol. 2018;180:1–13. [Google Scholar]
- Phan T.L., Ching C.T.S. A reusable mask for coronavirus disease 2019 (COVID-19) Arch. Med. Res. 2020;51(5):455–457. doi: 10.1016/j.arcmed.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pyle C.J., Uwadiae F.I., Swieboda D.P., Harker J.A. Early IL-6 signalling promotes IL-27 dependent maturation of regulatory T cells in the lungs and resolution of viral immunopathology. PLoS Pathog. 2017;13(9) doi: 10.1371/journal.ppat.1006640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rabaan A.A., Al-Ahmed S.H., Sah R., Al-Tawfiq J.A., Al-Qaaneh A.M., Al-Jamea L.H., Woodman A., Al-Qahtani M., Haque S., Harapan H., Bonilla-Aldana D.K., Kumar P., Dhama K. Rodriguez-Morales AJ. Recent advances in vaccine and immunotherapy for COVID-19. Hum. Vaccines Immunother. 2020;6:1–12. doi: 10.1080/21645515.2020.1825896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radonovich L.J., Simberkoff M.S., Bessesen M.T., Brown A.C., Cummings D.A., Gaydos C.A., Los J.G., Krosche A.E., Gibert C.L., Gorse G.J., Nyquist A., Reich N.G., Rodriguez-Barradas M.C., Price C.S., Perl T.M. N95 respirators vs medical masks for preventing influenza among health care personnel: a randomized clinical trial. J. Am. Med. Assoc. 2019;322(9):824–833. doi: 10.1001/jama.2019.11645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rose-John S. Interleukin-6 family cytokines. Cold Spring Harb. Perspect. Biol. 2018. 2018;10(2):a028415. doi: 10.1101/cshperspect.a028415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saadat S., Rawtani D., Hussain C.M. Environmental perspective of COVID-19. Sci. Total Environ. 2020;728:138870. doi: 10.1016/j.scitotenv.2020.138870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schlogl R., Abd H S B B O A. Nanocarbon-activated carbon composite. U.S. Patent. 2009;20 090,220,767A1. [Google Scholar]
- Schoeman D., Fielding B.C. Coronavirus envelope protein: current knowledge. Virol. J. 2019;16(1):69. doi: 10.1186/s12985-019-1182-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Setyo B.K., Muhammad F.I. Seasonal variation of plastic debris accumulation in the estuary of Wonorejo River, Surabaya, Indonesia. Environ. Technol. Innov. 2019;16:100490. [Google Scholar]
- Sharma S., Chatterjee S. Microplastic pollution, a threat to marine ecosystem and human health: a short review. Environ. Sci. Pollut. Res. Int. 2017;24(27):21530–21547. doi: 10.1007/s11356-017-9910-8. [DOI] [PubMed] [Google Scholar]
- Sharma O., Sultan A.A., Ding H., Triggle C.R. A review of the progress and challenges of developing a vaccine for COVID-19. Front. Immunol. 2020;11:585354. doi: 10.3389/fimmu.2020.585354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shereen M.A., Khan S., Kazmi A., Bashir N., Siddique R. COVID-19 infection: origin, transmission, and characteristics of human coronaviruses. J. Adv. Res. 2020;24:91–98. doi: 10.1016/j.jare.2020.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi Z., Hu Z. A review of studies on animal reservoirs of the SARS coronavirus. Virus Res. 2008;133(1):74–87. doi: 10.1016/j.virusres.2007.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siu Y., Teoh K., Lo J., Chan C., Kien F., Escriou N., Tsao S.W., Nicholls J.M., Altmeyer R., Peiris J.S.M., Bruzzone R., Nal B. The M, E, and N structural proteins of the severe acute respiratory syndrome coronavirus are required for efficient assembly, trafficking, and release of virus-like particles. J. Virol. 2008;82(22):11318–11330. doi: 10.1128/JVI.01052-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Syed Q., Sopwith W., Regan M., Bellis M.A. Behind the mask. Journey through an epidemic: some observations of contrasting public health responses to SARS. J. Epidemiol. Community Health. 2003;57(11):855–856. doi: 10.1136/jech.57.11.855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thanh Le T., Andreadakis Z., Kumar A., Gómez Román R., Tollefsen S., Saville M., Mayhew S. The COVID-19 vaccine development landscape. Nat. Rev. Drug Discov. 2020;19(5):305–306. doi: 10.1038/d41573-020-00073-5. [DOI] [PubMed] [Google Scholar]
- Thiel M., Luna-Jorquera G., Álvarez-Varas R., Gallardo C., Hinojosa I.A., Luna N., Miranda-Urbina D., Morales N., Ory N., Pacheco A.S., Portflitt-Toro M., Zavalaga C. Impacts of marine plastic pollution from continental coasts to subtropical Gyres -Fish, Seabirds, and other vertebrates in the SE Pacific. Front. Mar. Sci. 2018;5:238. [Google Scholar]
- UNE UNE Specification published to facilitate the manufacture of reusable hygienic masks. 2020. https://www.une.org/laasociacion/sala-de-informacion-une/noticias/especificacion-une-mascarillas Available on 9th of April 2020 at.
- Van Boheemen S., De Graaf M., Lauber C., Bestebroer T.M., Raj V.S., Zaki A.M., Osterhaus A.D.M.E., Haagmans B.L., Gorbalenya A.E., Snijder E.J., Fouchier R.A.M. Genomic characterization of a newly discovered coronavirus associated with acute respiratory distress syndrome in humans. mBio. 2012;3(6) doi: 10.1128/mBio.00473-12. e00473-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Doremalen N., Bushmaker T., Morris D.H., Holbrook M.G., Gamble A., Williamson B.N., Lloyd-Smith J.O. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N. Engl. J. Med. 2020;382:1564–1567. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walls A.C., Park Y.J., Tortorici M.A., Wall A., McGuire A.T., Veesler D. Structure, function, and antigenicity of the SARS-CoV-2 spike glycoprotein. Cell. 2020;181(2):281–292. doi: 10.1016/j.cell.2020.02.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J., Shen J., Ye D., Yan X., Zhang Y., Yang W., Li X., Wang J., Zhang L., Pan L. Disinfection technology of hospital wastes and wastewater: suggestions for disinfection strategy during coronavirus disease 2019 (COVID-19) pandemic in China. Environ. Pollut. 2020;262:114665. doi: 10.1016/j.envpol.2020.114665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO . Advice on the Use of Masks in the Community, during Home Care and in Health Care Settings in the Context of the Novel Coronavirus (2019-nCoV) Outbreak. World Health Organization. Interim Guidance 29 January 2020. 2020. https://apps.who.int/iris/bitstream/handle/10665/330987/WHOnCov-IPC_Masks-2020.1-eng.pdf?sequence=1&isAllowed=y Available on 9th April 2020 at. [Google Scholar]
- WHO . World Health Organization; 2020. Coronavirus Disease (COVID-19) Advice for the Public: when and How to Use Masks.https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public/when-and-how-to-use-masks Available on 9th of April 2020 at. [Google Scholar]
- WHO Advice on the use of masks in the context of COVID-19. Interim guidance 6 April 2020. 2020. https://www.who.int/publications-detail/advice-on-the-use-of-masks-in-the-community-during-home-care-and-in-healthcaresettings-in-the-context-of-the-novel-coronavirus-(2019-ncov)-outbreak Available on 9th April 2020 at.
- WHO Shortage of personal protective equipment endangering health workers worldwide. 2020. https://www.who.int/news-room/detail/03-03-2020-shortage-of-personal-protective-equipment-endangering-healthworkers- worldwide Available on 3th of April 2020 at.
- Wilcox C., Van Sebille E., Hardesty B.D. Threat of plastic pollution to seabirds is global, pervasive, and increasing. Proc. Natl. Acad. Sci. U. S. A. 2015;112(38):11899–11904. doi: 10.1073/pnas.1502108112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Windfeld E.S., Brooks M.S.L. Medical waste management - a review. J. Environ. Manag. 2015;163:98–108. doi: 10.1016/j.jenvman.2015.08.013. [DOI] [PubMed] [Google Scholar]
- Woo P.C.Y., Huang Y., Lau S.K.P., Yuen K.-Y. Coronavirus genomics and bioinformatics analysis. Viruses. 2010;2(8) doi: 10.3390/v2081803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization Coronavirus disease (COVID-19) advice for the public. 2019. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public Available online:
- World Health Organization 2020. https://apps.who.int/iris/handle/10665/330987 Available online:
- Wu A., Peng Y., Huang B., Ding X., Wang X., Niu P., Meng J., Zhu Z., Zhang Z., Wang J., Sheng J., Quan L., Xia Z., Tan W., Cheng G., Jiang T. Genome composition and divergence of the novel coronavirus (2019-nCoV) originating in China. Cell Host Microbe. 2020;27(3):325–328. doi: 10.1016/j.chom.2020.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu S.C. Progress and concept for COVID-19 vaccine development. Biotechnol. J. 2020;15(6) doi: 10.1002/biot.202000147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu X., Chen P., Wang J., Feng J., Zhou H., Li X., Zhong W., Hao P. Evolution of the novel coronavirus from the ongoing Wuhan outbreak and modeling of its spike protein for risk of human transmission. Sci. China Life Sci. 2020;63(3):457–460. doi: 10.1007/s11427-020-1637-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xuan-Thanh B., Thi-Dieu-Hien V., Phuong-Thao N., Van-Truc N., Thanh-Son D., Phuoc-Dan N. Microplastics pollution in wastewater: characteristics, occurrence and removal technologies. Environ. Technol. Innov. 2020;19:101013. [Google Scholar]
- Yang D., Leibowitz J.L. The structure and functions of coronavirus genomic 3’and 5’ ends. Virus Res. 2015;206:120e33. doi: 10.1016/j.virusres.2015.02.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang Y., Peng F., Wang R., Guan K., Jiang T., Xu G., Sun J., Chang C. The deadly coronaviruses: the 2003 SARS pandemic and the 2020 novel coronavirus epidemic in China. J. Autoimmun. 2020;109:102434. doi: 10.1016/j.jaut.2020.102434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu H., Sun X., Solvang W.D., Zhao X. Reverse logistics network design for effective management of medical waste in epidemic outbreaks: insights from the coronavirus disease 2019 (COVID-19) outbreak in Wuhan (China) Int. J. Environ. Res. Publ. Health. 2020;17:1770. doi: 10.3390/ijerph17051770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuki K., Fujiogi M., Koutsogiannaki S. COVID-19 pathophysiology: a review. Clin. Immunol. 2020;215:108427. doi: 10.1016/j.clim.2020.108427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zambrano-Monserrate M.A., Ruano M.A. Does environmental noise affect housing rental prices in developing countries? Evidence from Ecuador. Land Use Pol. 2019;87:104059. [Google Scholar]
- Zambrano-Monserrate M.A., Ruano M.A., Sanchez-Alcalde L. Indirect effects of COVID-19 on the environment. Sci. Total Environ. 2020;728:138813. doi: 10.1016/j.scitotenv.2020.138813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao S., Lin Q., Ran J., Musa S.S., Yang G., Wang W., Lou Y., Gao D., Yang L., He D., Wang M.H. Preliminary estimation of the basic reproduction number of novel coronavirus (2019-nCoV) in China, from 2019 to 2020: a data-driven analysis in the early phase of the outbreak. Int. J. Infect. Dis. 2020;92:214–217. doi: 10.1016/j.ijid.2020.01.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng B.J., Guan Y., Wong K.H., Zhou J., Wong K.L., Young B.W.Y., Lu L.W., Lee S.S. SARS-related virus predating SARS outbreak, Hong Kong. Emerg. Infect. Dis. 2004;10(2):176. doi: 10.3201/eid1002.030533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng J., Suh S. Strategies to reduce the global carbon footprint of plastics. Nat. Clim. Change. 2019;9(5):374–378. [Google Scholar]
- Zou X., Chen K., Zou J., Han P., Hao J., Han Z. Single-cell RNA-seq data analysis on the receptor ACE2 expression reveals the potential risk of different human organs vulnerable to 2019-nCoV infection. Front. Med. 2020;14(2):185–192. doi: 10.1007/s11684-020-0754-0. [DOI] [PMC free article] [PubMed] [Google Scholar]