Abstract
Objective
As an effective measure to prevent the COVID-19 pandemic, wearing mask is widely recommended in countries around the world. This study aims to identify factors that explain the behavioral intention of Wuhan City urban residents to wear masks.
Methods
A theoretical model was extended on UTAUT by incorporating the feature on residents having relevant knowledge and sufficient awareness on the pandemic. During early stages of the COVID-19 outbreak, an online survey was conducted in Wuhan City and 728 valid samples were collected from 35 communities. Structural equations modeling and bootstrapping were applied.
Results
Sample data present acceptable reliability and validity. Performance expectancy, effort expectancy, social influence, and knowledge about COVID-19 have positive effects on behavioral intention. Facilitating condition, knowledge, and behavioral intention have significant effects on use behavior. Gender, age, education, income, and current marital status are significant moderators in the theoretical model.
Conclusion
Having relevant knowledge on the pandemic, together with performance expectancy, effort expectancy, social influence, and facilitating condition, affects behavioral intention and usage behavior of Wuhan residents to wear masks at early stages of the COVID-19 pandemic. Subgroups have different psychological mechanisms based on their demographic characteristics.
Practice implications
Health policy makers should focus on enhancing residents’ knowledge on infectious disease and their awareness of the risk mitigation, and develop personalized measures for different subgroups.
Keywords: Knowledge, COVID-19, Psychological mechanisms, UTAUT, Wuhan
1. Introduction
According to Coronavirus disease (COVID-19) pandemic reports released by the World Health Organization, there had been more than 61.87 million confirmed cases and more than 1.45 million confirmed deaths worldwide by 29 November, 2020 (WHO). Fast-spreading COVID-19 emerged as a global pandemic. Countries around the world have adopted various measures to control the pandemic. President Trump announced that the United States was in a state of emergency and suspended immigration into US for 60 days. China [1], Italy [2], and Iran [3] implemented city lockdown and community quarantine (total stay-at-home) policies. Poland introduced border sanitary control on the fifth day after reporting the first laboratory confirmed case of COVID-19 [4].
Due to the absence of specific treatments and efficacious vaccines against COVID-19, personal precautions are necessary. A mathematical modeling study based on the cumulative number of confirmed cases and cumulative deaths estimated that the initial basic reproduction number (R0) of COVID-19 was 5.32, which is significantly higher than the initial R0 value of SARS (i.e., 2.90) [5]. The virus typically causes respiratory and gastrointestinal diseases in humans and animals, and it can be transmitted through aerosols and direct/indirect contact, as well as during the handling of medical cases and laboratory samples [6]. Non-pharmaceutical interventions, e.g. wearing facemasks or washing hands, are effective measures to block the epidemics of COVID-19 and many other respiratory infectious diseases [7]. Wearing a mask can significantly reduce the exposure of air pollutants into the body through the respiratory route, and this measure is an easy and effective protection method. Therefore, health departments in most Asian countries recommend that residents wear masks in public during the COVID-19 outbreak [3,6,7]. In particular, China has many megacities with large populations, such as 11.21 million in Wuhan. Due to the huge number of infections and presence of asymptomatic patients, it is necessary for people in large cities to wear masks in public settings and when around people who don’t live in the same household, especially when other social distancing measures are difficult to maintain.
At early stages of this pandemic, Wuhan (the Chinese city with the most severe outbreak of COVID-19) municipal government and health experts repeatedly urged the public to wear masks. However, urban residents did not have much motivation to wear masks [8]. Many Wuhan residents appeared without wearing masksin public places, such as subways, airports, and railway stations. This is a period of rapid increase in new infected cases in Wuhan. On February 6, the Wuhan government strictly implemented the policy of "residents must wear masks" and mandatory quarantine measures. Residents' willingness to wear masks reversed significantly, which led to masks out-of-stock and skyrocketing price in the Chinese market. Then the number of new infected cases showed a turning point on February 16. While some studies do not agree that healthy urban residents wear masks when in public [9,10], Wuhan's data suggest the necessity of implementing the policy in this city. There is an urgent need for research on the willingness to wear masks, and particularly, among Wuhan’s urban residents at early stages of the pandemic, which appears to have rarely been the focal population of previous research in this field.
In this paper, we address this research gap with the development of a comprehensive theoretical model. We use the model to characterize the impact mechanism of willingness to wear masks among urban residents during the early period of the pandemic, and the influencing psychological and demographic factors.
2. Theoretical model
The theoretical framework of our study was expanded on the Unified Theory of Acceptance and Use of Technology (UTAUT) [11,12]. UTAUT developed by integrating elements from eight models, i.e. Theory of Reasoned Action (TRA), Technology Acceptance Model (TAM), Motivational Model (MM), Theory of planned behavior (TPB), Combined TAM and TPB(C- TAM- TPB), Model of PC utilization (MPCU), Innovation diffusion theory (IDT), and Social cognitive theory (SCT) [11]. Given that UTAUT explains up to 70% of the variance in behavioral intentions, it is widely used to explore individual acceptance to medical technology, device and service, including Canadian patients’ intention to use online postings of ED wait times [13], physicians' adoption of electronic health record in the healthcare system of Bangladesh [14], health information technology adoption in Thailand's community health centers [15], elderly persons’ perception and acceptance of using wireless sensor networks to assist healthcare in Australia [16], and wearable technology acceptance in healthcare [17].
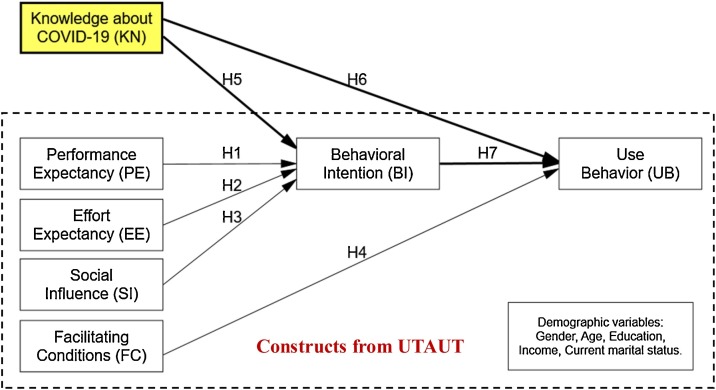
Previous studies demonstrate the general applicability of UTAUT model in the field of individual health behavior, and the reliability and validity of constructs in the theoretical model have been extensively verified [13,18,19]. In view of the significant influence of knowledge on the behavioral intention of individuals in the context of acceptance of health technologies, we incorporated Knowledge about COVID-19 as a new construct in the extended theoretical model. Then, an extended UTAUT model (Fig. 1 ) was developed to explain Wuhan city residents’ intention and use behavior of wearing masks in early stages of the pandemic.
Fig. 1.
An Extended UTAUT Model.
UTAUT suggests three constructs acting as direct determinants of behavioral intention, namely performance expectancy, effort expectancy, and social influence. Performance expectancy is defined as the degree to which an individual believes that using the system (masks) will help him or her to attain gains in job performance. It was represented as perceived usefulness, usefulness and extrinsic motivation, usefulness and relative advantage [11]. The performance expectancy construct in a UTAUT model is the strongest predictor to individual behavioral intentions [20,21]. Effort expectancy is defined as the degree of ease associated with the use of the system (masks). It was developed by perceived ease of use in TAM, complexity in MPCU, and ease of use in IDT [11]. Empirical studies show that effort expectancy has a significant impact on behavioral willingness and the relationship is moderated by gender, age, and experience, especially at early stages [17,22,23]. Social influence is defined as the degree to which an individual perceives that important others believe he or she should use the new system. It was represented as a subjective norm in TRA, TAM2, TPB/DTPB and C-TAM-TPB, social factors in MPCU, and image in IDT [11]. Previous research confirmed the significant impact of social influence on behavioral intentions. It was moderated by gender, age, voluntariness and experience, and the effect would be stronger for women, particularly older women [24,25]. Based on the previous research and the current context, we developed the following three hypotheses:
H1
Performance expectancy will have a positive influence on residents' behavioral intention of wearing masks.
H2
Effort expectancy will have a positive influence on urban residents' behavioral intention of wearing masks.
H3
Social influence will have a positive influence on urban residents' behavioral intention of wearing masks.
Facilitating conditions is defined as the degree to which an individual believes that an organizational and technical infrastructure exists to support the use of the system. It captures concepts embodied by perceived behavioral control (TPB/DTPB, C-TAM-TPB), facilitating conditions (MPCU), and compatibility (IDT) [11]. Under the UTAUT theoretical framework, facilitating conditions and behavioral intention influence user acceptance and use behavior. It is confirmed by empirical evidence that facilitating conditions has a significant influence on use behavior but does not significantly affect behavioral intention [14,15]. Consistent with the theoretical model of behavioral intention discussed in previous studies, we assume that behavioral intention will have a significant positive impact on the behavior of urban residents wearing masks [11]. Then, the following two hypotheses were proposed:
H4
Facilitating conditions will have a positive influence on urban residents' use behavior of wearing masks.
H7
Behavioral intention will have a positive influence on urban residents' use behavior of wearing masks.
Furthermore, previous studies found that the knowledge level of individuals has a general positive or negative intention to using healthcare technology, device, and service, such as HPV vaccination [[26], [27], [28]], electronic health record (EHR) [14], and face masks [29,30]. On this basis, we add knowledge about COVID-19 into our research model as a direct determinant to behavioral intention and use behavior. This construct (Knowledge about COVID-19) is defined as the degree to which an individual has relevant knowledge about the COVID-19 pandemic, including incubation period, difference with seasonable flu, preventive measures, and case fatality rate. We added the following two hypotheses:
H5
Knowledge about COVID-19 will have a positive influence on urban residents' behavioral intention of wearing masks.
H6
Knowledge about COVID-19 will have a positive influence on urban residents' use behavior of wearing masks.
Previous studies suggested that direct effects of determinants in the UTAUT model are moderated by demographic variables, i.e. age, gender, experience, educational level, health insurance, ethnicity/race, and voluntariness of use [[11], [12], [13],15,19]. Based on the current research context, we adjusted demographic variables as control factors. First, given that our study adds the construct of use behavior into the research model, difference on the knowledge about the infectious disease was considered. Second, at early stages of the COVID-19 pandemic, wearing masks was voluntary among Wuhan’s urban residents. Therefore, we removed the two control variables, experience and voluntariness of use. Third, we considered characterizing the demographic variables of different segments and incorporating them into the research model, including education, annual household income before tax, and current marital status. These five demographic variables will mediate the relationship between the constructs in the research model.
3. Methods
3.1. Questionnaire design
The questionnaire consists of two parts. The first part (socioeconomic information) includes five choice questions on gender, age, education, annual household income before tax, and current marital status. The second part (behavioral intentions scale) includes questions (variables) to measure respondents’ behavioral intentions, and all measurement items were derived from previous studies and scored on a seven-point Likert scales. The questionnaire was pretested by a pilot survey, and confirmatory factor analysis (CFA) was applied to the validated sample data. Items with standardized factor loading less than 0.5 were deleted, and some language expressions were revised. Table 1 lists the detailed items of each construct and their sources.
Table 1.
Summary of construct with measurement items.
| Constructs | Items Item in questionnaire | Mean (scale range: 1 to 7) | Standard Error | Sources | |
|---|---|---|---|---|---|
| Performance Expectancy (PE) | PE1 | Wearing a mask can greatly reduce the risk of COVID-19 transmission from others. | 4.97 | 1.1677 | (K. Magsamen-Conrad et al., 2015; V. Venkatesh et al., 2003) |
| PE2 | Wearing a mask is an effective protective measure against COVID-19. | 4.90 | 1.1787 | ||
| PE3 | Wearing a mask can prevent viruses in the air from invading my lungs. | 4.82 | 1.1464 | ||
| PE4 | Wearing a mask and going out, I will be much safer. | 4.97 | 1.2677 | ||
| Effort Expectancy (EE) | EE1 | It is easy to learn how to wear a mask properly. | 5.08 | 1.1007 | (J. Jewer, 2018; R. A. Dunn et al., 1998; R. J. Holden, 2011) |
| EE2 | The economic burden of daily use of masks is affordable. | 4.69 | 1.0943 | ||
| EE3 | I can easily buy masks. | 4.74 | 1.1148 | ||
| EE4 | For me, it is easy to get into the habit of wearing a mask when going out. | 4.80 | 1.1720 | ||
| Social Influence (SI) | SI1 | People who are important to me think I should wear a mask in public. | 4.35 | 1.3338 | (K. Magsamen-Conrad et al., 2015) |
| SI2 | People who influence my behavior suggest that I should wear a mask. | 5.37 | 1.4283 | ||
| SI3 | Residents wearing masks will be regarded as health-conscious people. | 4.91 | 1.4399 | ||
| Facilitating Condition (FC) | FC1 | The government provided convenient conditions for residents to wear masks. | 4.52 | 1.4102 | (S. B. Peterson, J. J. Michalek, 2013; K. Palmer et al., 2018) |
| FC2 | My life will not become inconvenient after wearing a mask. | 4.44 | 1.4541 | ||
| FC3 | The community and my family supported me in wearing a mask. | 4.27 | 1.3271 | ||
| Knowledge about COVID-19 (KN) | KN1 | The incubation period of COVID-19 is 0−24 days, and it generally does not exceed 14 days. | 3.53 | 1.4111 | (H. S. W. Ho, 2012; J. Kumar et al., 2020) |
| KN2 | COVID-19 is not flu, and it can cause severe lung inflammation. | 3.71 | 1.3508 | ||
| KN3 | To prevent COVID-19, it is necessary to wash your hands and wear a mask. | 3.89 | 1.4713 | ||
| KN4 | The case fatality rate of COVID-19 is about 2.5%, which is lower than other viruses such as SARS and MERS. | 3.66 | 1.3878 | ||
| Behavioral intention (BI) | BI1 | I would like to wear a mask when I go out. | 4.87 | 1.4890 | (V. Venkatesh et al., 2003; M. Zhou et al., 2019) |
| BI2 | I plan to form a habit of going out with a mask in the future. | 4.58 | 1.3583 | ||
| BI3 | Wearing a mask when going out is a safe experience. | 3.84 | 1.4403 | ||
| BI4 | I will always wear a mask in public until the COVID-19 epidemic is resolved. | 4.28 | 1.4053 | ||
| Use Behavior (UB) |
UB1 | Recently, I wore a mask when I went out. | 4.92 | 1.4342 | (S. Wang et al., 2017; W. Li et al., 2017) |
| UB2 | I would recommend the benefits of wearing a mask to friends and relatives. | 4.72 | 1.3950 | ||
| UB3 | When I need to go shopping or socializing, wearing a mask is my first choice. | 4.66 | 1.3774 | ||
3.2. Data collection
It is a necessary premise that the sample size meets the statistical requirements. The sample size has been extensively discussed in previous studies, but it is difficult to reach a broad consensus. Even if the sample size is small, the structural equation model can implement meaningful tests [31]. Generally, N = 100 is considered the smallest acceptable sample size [32,33]. Some researchers believe that a larger sample size is required for structural equation model analysis, for example, N = 200 [34]. Simulation studies show that for normally distributed variables and no missing data, the reasonable sample size of the simple CFA model is about N = 150 [[35], [36], [37]]. The ratio (N: q) of the sample size (N) to the number of free variables (q) in the model is a widely adopted rule. The rule of thumb is at least N/q = 5 [38]; for complexity models, N/q should be 10–20 [32,39]. Considering the above studies and the number of variables in currently studied (25), we set the valid sample size required for this study to be over 500.
The survey was conducted in the center area of Wuhan city from January 1, 2020 (Wuhan Municipal Government announced the discovery of unexplained pneumonia) to January 22, 2020 (Wuhan closed all transportation channels in January 23). Wuhan is located on the Yangtze River in central China, with a total population of 14 million. This questionnaire survey was implemented with the assistance of a local community government. According to the last two digits of residents’ ID number, 860 participants were randomly selected from 35 communities in seven districts of Wuhan, namely Jiangan, Jianghan, Qiaokou, Hanyang, Wuchang, Qingshan and Hongshan. A written informed consent was signed before the investigation. An online shopping coupon was offered to the participants who successfully submitted their responses.
3.3. Statistical analysis
We used Windows SPSS 22.0 as descriptive statistics, and compared the quantitative proportion, average score, cumulative percentage and other indicators in different subgroups. One-way analysis of variance (one-way ANOVA), also known as F-test, was used to verify whether the mean of subgroup samples is different in data variation among each construct. For example, we placed "Performance Expectancy" on the dependent variable list, select "Gender" as an independent variable, and use the post-hoc multiple comparison method to implement the homogeneity test of variance.
We used the confirmatory factor analysis (CFA) to assess the reliability and validity of the measurement model. Reliability refers to the internal consistency and stability of the measurement results, including item reliability, construct reliability and discriminant validity. Content validity refers to the degree to which the measurement items can accurately represent the domain of constructs, or the usefulness of the measurements. In the current study, all items were selected and revised from the well-established measurements in previous studies, then the content validity was assured. The measurement reliability was tested by factor loadings with recommended threshold set at above 0.5 [40]. Scale reliability was assessed with Cronbach’s alpha and composite reliability (CR) with both thresholds set at 0.7. The discriminant validity can be verified by that all square root of the AVE are greater than the off-diagonal values in the corresponding rows and columns. Given that the data were collected by a single method, it is necessary to test the common method deviation (CMB) in confirmatory factor analysis [41,42]. The Harman's single-factor test method was adopted in current study, and the largest initial eigenvalue should not exceed the acceptable threshold of 50%. To evaluate the fitness of the theoretical model and survey data, we referred to common guidelines as following indicators and recommended values: CHI/DF < 3; NFI > 0.9; IFI > 0.9; RFI > 0.9; TLI > 0.9; CFI > 0.9; GFI > 0.9; AGFI > 0.9; P-value<0.05; RMSEA < 0.08 [43].
To verify the theoretical hypotheses proposed in the current study, structural equation modeling (SEM), maximum likelihood estimates and Bootstrapping methods were adopted. We used Amos 24.0 to transform the theoretical framework into a structural equation model, and the hypotheses were tested by factor and path analysis. Regarding the estimates of regression weights, p < 0.05 is the acceptable significant level.
The moderating effects of demographic variables have been confirmed in previous studies about health behavior, such as health information technologies and systems [15,18], mHealth [19] and wearable technology in healthcare [17]. The moderating effects of the five demographic variables in current study was tested by regression analysis based on unstandardized coefficients between the comparison groups. The different qualities between the two groups of variances do not affect the moderating effects evaluation [44]. For the five demographic variables, two groups with the largest difference were taken as the comparison groups: Gender (Male, Female), Age (Under 20, Over 65), Education (High school education or below, Bachelor degree and above), Income (Below 60,000 Yuan, More than 180,000 Yuan), Current marital status (Married, Unmarried). Then we calculated the unstandardized slope, based on the path loading coefficient (b) and standard error (SE) of comparison groups on relationship paths. If the absolute value of Z is greater than 1.96, it means that the moderating effects of control variable on this path is valid with the 0.05 confidence level [45,46].
4. Results
4.1. Demographic characteristics
We collected 728 valid samples from 860 respondents (84.7% completion rate) from Wuhan city residents, and samples that included missing data in the present study were eliminated. The sample size is in accordance with the structural equation analysis requirements [[35], [36], [37]].
As shown in Table 2 , the demographic characteristics of respondents including gender, age, education, household income and marital status. Overall, there are more female respondents (416) than male respondents (312). Survey participants aged 36–50 are mainstream and account for 44.0%, and the numbers of other four age groups are as follows: 79 respondents are under 20 years old, 116 respondents are 21–35 years old, 147 respondents are 51–65 years old, and 66 respondents are over 65 years old. From the perspective of education level of the respondents, those with vocational college degree, bachelor degree or higher education are the mainstream (84.5%). As to the annual household income before tax, 15.2% respondents stated under $10,000, 31.5% are $ 10,001–$ 20,000, 25.7% are $ 20,001–$ 30,000, 14.7% are $ 30,001–$ 40,000, and 12.9% are more than $ 40,000. Regarding current marital status, about three-quarters (72.9%) of the respondents are married.
Table 2.
Sample demographics and one-way ANOVA (N = 728).
| Items | n | % | PEa |
EEb |
SIc |
FCd |
KNe |
BIf |
UBg |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Meanh | Pi | Mean | p | Mean | p | Mean | p | Mean | p | Mean | p | Mean | p | |||
| Gender | 0.625 | 0.149 | 0.686 | 0.692 | 0.457 | 0.042* | 0.000*** | |||||||||
| Male (1) | 312 | 42.9 | 4.89 | 4.77 | 4.85 | 4.43 | 3.74 | 4.29 | 4.95 | |||||||
| Female (2) | 416 | 57.1 | 4.93 | 4.87 | 4.89 | 4.39 | 3.67 | 4.47 | 4.63 | |||||||
| Age | 0.272 | 0.754 | 0.017* | 0.269 | 0.770 | 0.008** | 0.368 | |||||||||
| Under 20 (1) | 79 | 10.9 | 4.32 | 4.90 | 4.72 | 4.28 | 3.84 | 4.17 | 4.92 | |||||||
| 21–35 years old (2) | 116 | 15.9 | 5.00 | 4.93 | 4.87 | 4.49 | 3.75 | 4.48 | 4.73 | |||||||
| 36–50 years old (3) | 320 | 44.0 | 5.07 | 4.95 | 4.84 | 4.46 | 3.66 | 4.47 | 4.79 | |||||||
| 51–65 years old (4) | 147 | 20.2 | 4.96 | 4.77 | 4.80 | 4.25 | 3.68 | 4.15 | 4.62 | |||||||
| 65+ years old (5) | 66 | 9.1 | 4.91 | 5.06 | 4.89 | 4.52 | 3.70 | 4.67 | 4.87 | |||||||
| Education | 0.700 | 0.165 | 0.166 | 0.134 | 0.304 | 0.434 | 0.256 | |||||||||
| High school education or below (1) | 113 | 15.5 | 4.92 | 4.76 | 4.78 | 4.29 | 3.85 | 4.26 | 4.91 | |||||||
| Vocational college degree (2) | 341 | 46.8 | 4.94 | 4.89 | 4.82 | 4.50 | 3.67 | 4.43 | 4.78 | |||||||
| Bachelor degree and above (3) | 274 | 37.6 | 4.88 | 4.77 | 4.99 | 4.34 | 3.67 | 4.40 | 4.69 | |||||||
| Annual household income before tax | 0.543 | 0.178 | 0.690 | 0.064 | 0.377 | 0.359 | 0.007** | |||||||||
| Under $ 10,000 (1) | 111 | 15.2 | 4.96 | 4.83 | 4.93 | 4.63 | 3.82 | 4.52 | 5.08 | |||||||
| $ 10,001–$ 20,000 (2) | 229 | 31.5 | 4.89 | 4.88 | 4.88 | 4.37 | 3.73 | 4.33 | 4.81 | |||||||
| $ 20,001–$ 30,000 (3) | 187 | 25.7 | 4.87 | 4.76 | 4.85 | 4.35 | 3.63 | 4.40 | 4.67 | |||||||
| $ 30,001–$ 40,000 (4) | 107 | 14.7 | 5.05 | 4.95 | 4.75 | 4.53 | 3.77 | 4.52 | 4.75 | |||||||
| More than $ 40,001 (5) | 94 | 12.9 | 4.86 | 4.68 | 5.00 | 4.20 | 3.54 | 4.24 | 4.51 | |||||||
| Current marital status | 0.920 | 0.799 | 0.762 | 0.089 | 0.010* | 0.982 | 0.000*** | |||||||||
| Married (1) | 531 | 72.9 | 4.91 | 4.82 | 4.87 | 4.36 | 3.63 | 4.39 | 4.61 | |||||||
| Unmarried (2) | 197 | 27.1 | 4.92 | 4.84 | 4.90 | 4.53 | 3.88 | 4.39 | 5.20 | |||||||
Note: a-g PE: Performance Expectancy; EE: Effort Expectancy; SI: Social Influence; FC: Facilitating Conditions; KN: Knowledge about COVID-19; BI: Behavioral Intention; UB: Use Behavior; h Average scores of items among groups (7-point Likert scale); i Results of the one-way ANOVA, ***p < 0.001, **p < 0.01, *p < 0.05.
The results of one-way ANOVA suggest that gender is a significant factor on two constructs, and females had a higher average score than males on behavioral intention (4.29 vs 4.47, p < 0.05), while males had a higher average score than females on use behavior (4.95 vs 4.63, p < 0.001). Young residents (under 20) have lower scores than older people (65+ years old) in two constructs, including social influence (4.72 vs 4.89, p < 0.05) and behavioral intention (4.17 vs 4.67, p < 0.01). It shows that young people are less affected by the opinions from others, and their willingness to wear masks is lower than that of the elderly. The subgroup with lowest annual household income before tax (under $ 10,000) had a significantly higher score in on use behavior than the highest income subgroup (5.08 vs 4.51, p < 0.01). Marital status is also an important variable on two constructs, and the unmarried subgroup scores higher, including knowledge about COVID-19 (3.63 vs 3.88, p < 0.01) and use behavior (4.61 vs 5.20, p < 0.001). This implies that unmarried people have more knowledge about the new crown pneumonia virus and are more active in wearing masks. Education did not show significant difference among all constructs.
4.2. Reliability and validity of constructs
The Harman's single-factor test method was adopted in current study for detecting Common Method Bias, and the results showed that the largest initial eigenvalue is 31.6% (<the threshold of 50%). The above results show that the common method bias of the sample data is statistically acceptable. Confirmatory factor analysis (CFA) was implemented before evaluating the reliability and effectiveness of constructs, and four items were deleted because their standardized regression weights were observed to be under 0.5 (cut-off value) [47]. As shown in Table 3 , the reliability and validity of the research model are acceptable. All standardized factor loadings (minimum value is 0.694) exceed the threshold of 0.5, then the measurement reliability is acceptable. All Cronbach’s alphas (minimum value is 0.794) and CRs (minimum value is 0.795) are greater than 0.7, which indicate that each construct has good scale reliability. The variance inflation factor (VIF) is used to measure the degree of multicollinearity. VIFs are all less than 5 in all constructs, indicating that the multicollinearity of model rates negligible. Furthermore, the average variance extracted (AVE) of each construct (minimum value is 0.530) is greater than the threshold of 0.5, which indicates the convergent validity is acceptable. Constructs' correlations and square roots of AVE are shown in Table 4 . All square roots of each AVE are greater than the off-diagonal values in the corresponding rows and columns, which implies the discriminant validity is verified. As shown in Table 5 , the statistical results show that all goodness-of-fit indicators of the structural model are within the thresholds and are acceptable. For example, RMSEA is 0.047, CHI/DF is 2.619, IFI is 0.956, CFI is 0.956, and these four indicators are in the range of “good”. The other five indicators, including NFI, RFI, TLI, GFI, and AGFI, are all in the interval of (0.9, 0.95) and are statistically acceptable. To summarize, the measurement model of the current study meets the requirements of structural equation modeling with evidence on reliability and validity, and the sample data has a good fit with the theoretical model.
Table 3.
Composite reliability and convergent validity of the measures.
| Constructs | Variables | Loadings | C.R | Cronbach's Alpha | AVE |
|---|---|---|---|---|---|
| PE | PE1 | 0.783 | 0.862 | 0.862 | 0.610 |
| PE2 | 0.758 | ||||
| PE3 | 0.820 | ||||
| PE4 | 0.761 | ||||
| EE | EE1 | 0.731 | 0.819 | 0.818 | 0.530 |
| EE2 | 0.761 | ||||
| EE3 | 0.725 | ||||
| EE4 | 0.694 | ||||
| SI | SI1 | 0.779 | 0.879 | 0.876 | 0.709 |
| SI2 | 0.939 | ||||
| SI3 | 0.799 | ||||
| FC | FC1 | 0.718 | 0.795 | 0.794 | 0.564 |
| FC2 | 0.776 | ||||
| FC3 | 0.758 | ||||
| KN | KN1 | 0.861 | 0.843 | 0.842 | 0.576 |
| KN2 | 0.719 | ||||
| KN3 | 0.729 | ||||
| KN4 | 0.716 | ||||
| BI | BI1 | 0.738 | 0.878 | 0.877 | 0.643 |
| BI2 | 0.826 | ||||
| BI3 | 0.796 | ||||
| BI4 | 0.844 | ||||
| UB | UB1 | 0.741 | 0.801 | 0.800 | 0.573 |
| UB2 | 0.725 | ||||
| UB3 | 0.803 |
Loading: standardized factor loading; AVE: Average Variance Extracted; CR = Composite Reliability.
Table 4.
Constructs' correlations and square roots of AVE.
| PE | EE | SI | FC | KN | BI | UB | |
|---|---|---|---|---|---|---|---|
| PE | 0.781 | ||||||
| EE | 0.357 | 0.728 | |||||
| SI | 0.311 | 0.287 | 0.842 | ||||
| FC | 0.383 | 0.409 | 0.297 | 0.751 | |||
| KN | 0.290 | 0.277 | 0.245 | 0.403 | 0.759 | ||
| BI | 0.728 | 0.622 | 0.559 | 0.638 | 0.495 | 0.802 | |
| UB | 0.451 | 0.433 | 0.302 | 0.591 | 0.738 | 0.681 | 0.757 |
Bold signifies square roots of AVE for each pair of constructs.
Table 5.
The overall fitness indices of research model.
| Goodness of fit indices | Model value | Good fit | Acceptable fit | Comments |
|---|---|---|---|---|
| RMSEA | 0.047 | 0 ≤ RMSEA ≤ 0.05 | 0.05 < RMSEA ≤ 0.08 | Good |
| CHI/DF | 2.619 | 3 | 5 | Good |
| NFI | 0.931 | 0.95 ≤ NFI ≤ 1 | 0.90 ≤ NFI < 0.95 | Acceptable |
| IFI | 0.956 | 0.95 ≤ IFI ≤ 1 | 0.90 ≤ IFI < 0.95 | Good |
| RFI | 0.920 | 0.95 ≤ RFI ≤ 1 | 0.90 ≤ RFI < 0.95 | Acceptable |
| TLI | 0.949 | 0.97 ≤ TLI ≤ 1 | 0.95 ≤ NFI < 0.97 | Acceptable |
| CFI | 0.956 | 0.97 ≤ CFI ≤ 1 | 0.95 ≤ CFI < 0.97 | Good |
| GFI | 0.934 | 0.95 ≤ GFI ≤ 1 | 0.90 ≤ GFI < 0.95 | Acceptable |
| AGFI | 0.917 | 0.90 ≤ NFI ≤ 1 | 0.85 ≤ NFI < 0.90 | Acceptable |
Note: 4000 bootstrap samples.
4.3. Hypothesis testing and moderating effects
By running the bootstrapping calculations with 4000 samples, the significance of path was determined and all paths were significant as shown in Table 6 . Then, seven hypotheses were all supported at the significance level of 0.05. H1 predicts that performance expectancy positively affects the urban residents' behavioral intention of wearing masks. As expected, a significant positive relationship is confirmed (β1 = 0.554, t = 13.164). Similarly, H2 and H3 predict that effort expectancy and social influence positively affect urban residents' behavioral intention of wearing masks, respectively. As predicted, these two paths are positive and significant at (β2 = 0.447, t = 9.768) and (β3 = 0.253, t = 9.063). Two hypotheses regarding urban residents' use behavior of wearing masks are all supported, i.e. H4 refers to facilitating conditions (β4 = 0.217, t = 4.866), and H7 refers to behavioral intention (β7 = 0.203, t = 7.268). As a new construct added into the theoretical model, knowledge about COVID-19 significantly affects urban residents' behavioral intention (β5 = 0.465, t = 11.505) and use behavior (β6 = 0.287, t = 7.092) of wearing masks, thus supporting H5 and H6. The R2 values extracted in the endogenous factors are: 81% for behavioral intention and 70% for use behavior.
Table 6.
Hypotheses testing.
| Hypotheses | Paths | t | β | Significance h | Comments | ||
|---|---|---|---|---|---|---|---|
| H1 | BI | <--- | PEa | 13.164 | 0.554 | *** | Supported |
| H2 | BI | <--- | EEb | 9.768 | 0.447 | *** | Supported |
| H3 | BI | <--- | SIc | 9.063 | 0.253 | *** | Supported |
| H4 | UB | <--- | FCd | 4.866 | 0.217 | *** | Supported |
| H5 | BIf | <--- | KNe | 7.268 | 0.203 | *** | Supported |
| H6 | UBg | <--- | KN | 11.505 | 0.465 | *** | Supported |
| H7 | UB | <--- | BI | 7.092 | 0.287 | *** | Supported |
Note: a-g PE: Performance Expectancy; EE: Effort Expectancy; SI: Social Influence; FC: Facilitating Conditions; KN: Knowledge about COVID-19; BI: Behavioral Intention; UB: Use Behavior; h Results of Significance, ***p < 0.001, **p < 0.01, *p < 0.05; i 4000 bootstrap samples.
The results of demographic variables' moderating effects are listed in Table 7 . Gender is a significant moderator on four paths: behavioral intention <--- social influence (Z = 2.646), behavioral intention <--- knowledge (Z=−4.119), use behavior <--- knowledge (Z = 9.182), and use behavior <--- behavioral intention (Z=−12.346). Age is a significant moderator on two paths: behavioral intention <--- social influence (Z = 2.216), and use behavior <--- knowledge (Z=−2.463). Education acts as moderator between behavioral intention and use behavior (Z=−2.058). Income is a significant moderator on four paths: behavioral intention <--- effort expectancy (Z = 1.973), behavioral intention <--- knowledge (Z=−3.018), use behavior <--- knowledge (Z = 4.640), and use behavior <--- behavioral intention (Z=-6.394). Marital status is a significant moderator on four paths: behavioral intention <--- performance expectancy (Z=−1.969), behavioral intention <--- knowledge (Z = 4.470), use behavior <--- knowledge (Z=−7.779), and use behavior <--- behavioral intention (Z = 14.040).
Table 7.
Moderating effects of demographic variables.
| BI <--- PE a | BI <--- EE b | BI <--- SI c | UB <--- FC d | BI <--- KN e | UB <--- KN | UB g <--- BI f | ||
|---|---|---|---|---|---|---|---|---|
| Gender | Male | 0.560 | 0.391 | 0.325 | 0.187 | 0.119 | 0.613 | 0.011 |
| Female | 0.449 | 0.346 | 0.201 | 0.092 | 0.320 | 0.124 | 0.713 | |
| Z-value | 1.888 | 0.698 | 2.646*h | 1.585 | −4.119* | 9.182* | −12.346* | |
| Age | Under 20 | 0.423 | 0.361 | 0.417 | 0.313 | 0.157 | 0.414 | 0.164 |
| Over 65 | 0.515 | 0.378 | 0.163 | 0.033 | 0.06 | 0.740 | 0.047 | |
| Z-value | −0.632 | −0.097 | 2.216* | 1.833 | 0.916 | −2.463* | 0.815 | |
| Education | High school education or below | 0.506 | 0.397 | 0.27 | 0.21 | 0.192 | 0.522 | 0.118 |
| Bachelor degree and above | 0.46 | 0.365 | 0.342 | 0.22 | 0.263 | 0.412 | 0.315 | |
| Z-value | 0.480 | 0.350 | −0.954 | −0.096 | −1.026 | 1.180 | −2.058* | |
| Income | below $10,000 | 0.516 | 0.562 | 0.238 | 0.206 | 0.051 | 0.626 | 0.172 |
| More than $40,000 | 0.462 | 0.296 | 0.295 | 0.233 | 0.339 | 0.124 | 0.566 | |
| Z-value | 0.545 | 1.973* | −0.608 | −0.220 | −3.018* | 4.640* | −3.394* | |
| Marital status | Married | 0.450 | 0.351 | 0.248 | 0.105 | 0.316 | 0.145 | 0.668 |
| Unmarried | 0.580 | 0.428 | 0.253 | 0.220 | 0.080 | 0.584 | 0.243 | |
| Z-value | −1.969* | −0.989 | −0.092 | −1.497 | 4.470* | −7.779* | 3.040* |
Note: a-g PE: Performance Expectancy; EE: Effort Expectancy; SI: Social Influence; FC: Facilitating Conditions; KN: Knowledge about COVID-19; BI: Behavioral Intention; UB: Use Behavior; h * p < 0.05.
5. Discussion and conclusion
5.1. Theoretical contributions
First, the theoretical model extended from UTAUT by adding a new construct has higher explanatory power than the original UTAUT, which improves the applicability of this theory. The purpose of our study is to empirically investigate the factors that explain the willingness of Wuhan citizens to wear masks in the early days of the COVID-19 epidemic, and thus to clarify causes for the low rate of adoption in wearing masks at this stage. In this context, we developed an extended UTAUT theoretical framework by adding “Knowledge about COVID-19” as the new construct, and collected 728 valid samples to verify it. The empirical research results show that our research model explains approximately 81% of the variance in behavioral intention and 70% in usage behavior to wear masks among Wuhan residents in the early days of the COVID-19 pandemic. Compared with the 46% of explanation rate in behavioral intention of the original UTAUT model, the current model has been significantly improved in explanatory power. In previous studies based on the UTAUT theoretical framework of healthcare behavior analysis, the R2 value of behavioral intention is between 25% and 60% [13,17,20,21], and they were all lower than the results in the current study. Furthermore, to the best of our knowledge, the research at hand is the first explanatory study on acceptance of wearing masks in the context of COVID-19 epidemic. The current study has expanded the structural framework of the theoretical model and has also enriched the application fields of the theory.
Second, the verification results of the paths relationship in the current hypotheses are partially consistent with previous studies, and there are also some new findings. The empirical research results show that four constructs (knowledge, performance expectancy, effort expectancy, and social influence) are significantly associated with the residents’ intention to wear a mask, and three constructs (knowledge, facilitating conditions, and behavioral intention) are significant determinants of use behavior. In addition, the current study incorporates demographic variables as moderators into the theoretical framework and has obtained interesting findings. Five demographic variables (gender, age, education, income, and marital status) significantly moderate the strength of relationships among constructs. The detailed discussion is listed below:
Knowledge about COVID-19 was added to the UTAUT theoretical model as a new construct, and the empirical results confirmed that this construct is a significant factor affecting the intention and behavior of Wuhan City urban residents to wear masks. This result is roughly consistent with the empirical studies based on the KAP (Knowledge, Attitude and Practice) model, that is, knowledge is an important determinant of individual behavioral intentions to adopt new medical services, including human papillomavirus (HPV) vaccination [28], dietary supplements (DS) [48], and seasonal influenza vaccination [49]. When faced with public health emergencies, individuals inevitably feel panic, nervousness, anxiety, irritability and other negative emotions, especially among those who lack knowledge [49]. In early days of the COVID-19 pandemic, Wuhan residents lacked necessary knowledge on the measures to prevent infectious diseases, and residents' willingness to wear masks during this period was very low. At the outbreak of the epidemic, massive news campaigns and expert speeches appeared on social media, and the individual's knowledge about viruses and prevention strategies significantly increased. At this stage, there has been a panic buying spree targeting personal protection equipment, and the price of each surgical mask has also increased from $ 0.1 to $ 1.2 within a few weeks. These phenomena are consistent with a study conducted in Pakistan, that knowledge is a positive determinant of residents' behavior and willingness to wear masks, including healthcare workers (HCWs) wearing masks to reduce the spread (COVID -19) [30]. In addition, samples from different subgroups have significant moderating effects. Specifically, gender, income, and marital status are significant moderating variables on the relationship path from knowledge to behavioral intention, and there is a significantly stronger relationship among the subgroups of women, high-income, and married persons. Gender, age, income, and marital status are significant moderating variables on the relationship path from knowledge to use behavior, and the relationships are significantly stronger in the subgroups of men, the elderly, low-income, and married persons. This is an interesting conclusion that even the same subgroup, such as women, has higher willingness and lower actual behavior under the influence of knowledge. The possible explanation is that there are significant differences in the relationship strength from intention to behavior between subgroups.
The results also show that there is a significant relationship between performance expectancy and behavioral intention, and it is moderated by participants’ marital status. This theoretically implies that perceived functional utilities (performance expectancy) are the focus of attention for Wuhan citizens to wear masks. The majority of previous studies using UTAUT as the conceptual model has confirmed that performance expectancy is an important factor influencing behavioral intention in the context of health promotion [13,21,50]. Interestingly, the results also reveal that the standardized regression weight of performance expectancy on behavioral intention is significantly greater for unmarried-residents than married-residents. This shows that unmarried residents are more likely to have behavioral intentions because they feel that wearing a mask can effectively prevent themselves from being infected by the virus. Married individuals may be exposed more to cognitive and social participation than those who are not married [51]. The cumulative effects of such engagements may prevent them from sensitively adjusting their behavioral intentions because of the perceived utilities.
Our study supports that effort expectancy is significantly associated with behavioral intention of Wuhan residents to wear masks. In the context of health technologies, effort expectancy is often used as an influencing factor in behavioral intentions in previous studies. This effect is significant in some cases, e.g. health information technology adoption in Thailand's community health centers [15], and physicians’ technology acceptance for e-health in ambulatory care [52], while in other cases it is not significant, such as physicians' adoption of electronic health record (EHR) in healthcare system of Bangladesh [14], and clinician adoption of health information systems in Cameroon [18]. Our empirical research confirms that residents purchasing masks easily and developing a habit of wearing masks is an important factor affecting their behavioral intentions. Further, we confirmed that income is a moderator that significantly regulates the strength of relationship between effort expectancy and behavioral intention, and the low-income groups are more likely to generate stronger behavior intentions than high-income groups. For low-income groups, reducing their effort expectancy to wear masks, e.g. free or low-cost masks, education on how to wear masks correctly, is conducive to enhancing their behavioral intentions.
Another important finding is that social influence is a positive factor on behavioral intention to wear masks, and this is in line with studies on other public health intervention adoption [14,15,53]. A possible explanation is that residents of Wuhan (along with residents of other cities around the world) generally lacked knowledge and experience pertaining to this unprecedented pandemic in the early stages of the COVID-19 outbreak. Panic and rumors spread quickly on social media and the Internet, which has created chaotic social situations. An authoritative voice can greatly influence people's decisions, for example, Zhong Nanshan's speech on infectious disease and control became the principal guidance by most Chinese people. In addition, we found that gender and age are two significant moderators that affect the strength of relationship between social influence and behavioral intention. Specifically, regarding behavioral intentions due to social influence, men are more likely to be affected than women, and young people are more likely to be affected than the elderly. The possible reason is that men and young people are more engaged to online social activities and are more likely to obtain the relevant information from social media, which makes them more sensitive about wearing masks.
Our study further reveals that facilitating conditions are significantly positively correlated with the usage behavior of Wuhan residents to wear masks, which is generally consistent with the recent findings of technology acceptance in other healthcare fields [13,14,21,54]. This means that when supporting conditions for wearing a mask are effective, for example, the convenience offered by the government and communities, the respondents will be more likely to wear a mask. Interestingly, we found that the relationship path from facilitating conditions to use behavior, unlike the other six paths, is not significantly moderated by demographic variables. The possible explanation is that the difference of facilitating conditions in different subgroups is not significant, so it has no statistically moderating effects.
Current empirical results confirm that behavioral intention is a positive determinant of use behavior. This result is consistent with previous studies in the context of healthcare technology acceptance, e.g. the adoption of mHealth by the elderly [19], the adoption behavior of mobile healthcare systems in USA, Canada, and Bangladesh [55]. Furthermore, our study confirms that the relationship path from behavioral intention to use behavior is moderated by four demographic variables, i.e. gender, education, income, and marital status. Specifically, women have a stronger relationship than that of male subgroups, indicating that women are more likely to transform their willingness into mask-wearing behaviors. From the perspective of the influencing degree of education level on this relationship, the subgroup of high school education or below is weaker than the subgroup of bachelor degree and above. The highly educated people are more rational in wearing masks, and they are positive activists. It is interesting that with regard to the effect of income on this path, low-income groups have weaker correlations than high-income groups. The possible reason is that low-income people have a weaker perception of health risks, and they believe that they are less likely to be infected. Married subgroups have stronger relationship than unmarried subgroups, which may be attributed to married people having more opportunities to communicate between them and promote the necessary protection measure.
The limitations of our study are as follows: First, while the sample size meets the requirements of structural equation model analysis, the universality of the results should be treated with caution. The samples were all collected from Wuhan, the first city with the COVID-19 pandemic. In the following weeks, the pandemic quickly swept through many cities around the world. It is valuable to implement cross-regional comparative research. Second, our investigation was carried out in the early stage of the outbreak (January 1 to January 22), and did not compare with the severe stage of the outbreak. The main reason is that the latter stage of the investigation was interfered by the government's mandatory policies. The Chinese government's ability to control the public is significantly stronger than other countries, including the mandate of wearing masks to individuals. During the severe outbreak in Wuhan, the government mobilized police forces, community workers, and property security officers to request all citizens to wear masks. At this stage, all Wuhan citizens wear masks regardless of individual’s will. The COVID-19 pandemic in Wuhan has been effectively controlled at present. It is anticipated that the mandate will be lifted in the near future, so the investigation after the pandemic will be of comparative value. Finally, the current study does not consider the impact of residents’ religious beliefs on their behavior of wearing masks. More than 90% of Chinese residents do not have a clear religious belief, and more than half of the population are self-identified atheists. When the current results are extended to other regions, the moderating effects of individual religious beliefs need to be considered.
5.2. Practice implications
The results of this study offer suggestions for policy makers and medical workers to formulate effective strategies and guide residents to wear masks to prevent the spread of epidemic. For policymakers, active health induction policies should be mainstream, and enforcement measures must be implemented cautiously and restrictively. China has established an authoritarian system, and the government is keen to issue mandatory policies to implement public management. However, with rapid progress of democratization, mandatory policies have become a major obstacle to China's development. For the policy-making on wearing masks, it is effective and acceptable to improve residents’ knowledge by health education [56]. Only when the knowledge and awareness about disease prevention has been popularized among residents, they will act rationally and wear masks voluntarily. In addition, personalized strategies for different groups should be the principles of policy formulation, e.g. it is effective for women to provide more health education to improve their knowledge level, while men should be implemented with positive social influence. It is worth mentioning that, the Wuhan municipal government did not implement the policy to mandate all its residents to wear masks at the early stages of the COVID-19 pandemic. The situation was similar to many other cities in the world, that is, residents were free to choose whether to wear masks. Therefore, our research not only has practical implications on controlling the spread of epidemic situation in Wuhan, but its generalizability allows it to be applied to other cities.
For medical workers, authoritative experts, scholars and family doctors, they should publish unanimous prevention recommendations at the beginning of public health emergencies, so as to implement a positive influence on the public. Open, transparent, and timely information release is helpful to control psychological panic during the epidemic [57]. In the early days of the COVID-19 pandemic, the Wuhan government's information blockade strategy led to severe panic. On the eve of the Wuhan closure on January 23, millions of residents departed from Wuhan. Residents left behind snapped up all the commodities in the supermarket, and the feeling of despair spread quickly. It was not until Academician Zhong Nanshan released the true infection characteristics of COVID-19 and correct protection measures that the public became calm and started to wear masks. Current research also confirms the positive effect of social influence on residents wearing masks. For medical scholars and family doctors who have significant influence on the public, they should promote the benefits of wearing masks to residents by public channels such as TV and social media.
5.3. Conclusion
Wearing a mask is generally considered to be an effective health intervention for residents to prevent pandemics, especially in densely populated megacities. However, in the early stages of the COVID-19 epidemic, Wuhan residents’ willingness to wear masks remained low. The purpose of this study is to explore the determinants that affect residents’ intention and behavior of wearing masks, including psychological factors and demographic variables. The empirical results confirm performance expectancy, effort expectancy, social influence, and knowledge are significantly associated with the residents’ intention to wear a mask, and facilitating conditions, knowledge, and behavioral intention are significant determinants of use behavior. Five demographic variables, i.e., gender, age, education, income, and marital status significantly moderate the strength of relationships among constructs. Although have been many studies focusing on the causative source of COVID-19 and its treatment measures, little research has been devoted to examining the psychological decision-making mechanism of residents’ intention to wear masks. Therefore, the results of this study contribute to the existing research on public health interventions with the epidemiology of COVID-19. These findings provide useful suggestions for policy makers and medical workers to formulate effective strategies.
Funding
This work was supported by Changsha Natural Science Foundation (grant numbers KQ2007081), and key scientific research project of Hunan Provincial Department of Education (grant number 20A129).
CRediT authorship contribution statement
Min Zhou: Conceptualization, Methodology, Writing - original draft, Project administration. Piao Long: Investigation, Validation, Data curation. Nan Kong: Conceptualization, Writing - original draft. Kathryn S. Campy: Supervision, Writing - review & editing.
Declaration of Competing Interest
The authors report no declarations of interest.
References
- 1.Boldog P., et al. Risk assessment of novel coronavirus COVID-19 outbreaks outside China. J. Clin. Med. 2020;9(2) doi: 10.3390/jcm9020571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sjodin H., et al. Only strict quarantine measures can curb the coronavirus disease (COVID-19) outbreak in Italy, 2020. Eurosurveillance. 2020;25(13):7–12. doi: 10.2807/1560-7917.ES.2020.25.13.2000280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Raoofi A., et al. COVID-19 pandemic and comparative health policy learning in Iran. Arch. Iran. Med. 2020;23(4):220–234. doi: 10.34172/aim.2020.02. [DOI] [PubMed] [Google Scholar]
- 4.Pinkas J., et al. Public health interventions to mitigate early spread of SARS-CoV-2 in Poland. Med. Sci. Monit. 2020:26. doi: 10.12659/MSM.924730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhou W.K., et al. Effects of media reporting on mitigating spread of COVID-19 in the ear y phase of the outbreak. Math. Biosci. Eng. 2020;17(3):2693–2707. doi: 10.3934/mbe.2020147. [DOI] [PubMed] [Google Scholar]
- 6.Pal M., et al. Severe acute respiratory syndrome coronavirus-2 SARS-CoV-2 an update. Cureus. 2020;12(3) doi: 10.7759/cureus.7423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Williams L., et al. Protection motivation theory and social distancing behaviour in response to a simulated infectious disease epidemic. Psychol. Health Med. 2015;20(7):832–837. doi: 10.1080/13548506.2015.1028946. [DOI] [PubMed] [Google Scholar]
- 8.Pan A., et al. Association of public health interventions with the epidemiology of the COVID-19 outbreak in Wuhan, China. JAMA. 2020;323(19):1–9. doi: 10.1001/jama.2020.6130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Geldsetzer P. Use of rapid online surveys to assess people’s perceptions during infectious disease outbreaks: a cross-sectional survey on COVID-19. J. Med. Internet Res. 2020;22(4) doi: 10.2196/18790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Modi P.D., et al. COVID-19 awareness among healthcare students and professionals in Mumbai metropolitan region: a questionnaire-based survey. Cureus. 2020;12(4) doi: 10.7759/cureus.7514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Venkatesh V., et al. User acceptance of information technology: toward a unified view. MIS Q. 2003;27(3):425–478. [Google Scholar]
- 12.Venkatesh V., Thong J.Y.L., Xu X. Consumer acceptance and use of information technology: extending the unified theory of acceptance and use of technology. MIS Q. 2012;36(1):157–178. [Google Scholar]
- 13.Jewer J. Patients’ intention to use online postings of ED wait times: a modified UTAUT model. Int. J. Med. Inform. 2018;112:34–39. doi: 10.1016/j.ijmedinf.2018.01.008. [DOI] [PubMed] [Google Scholar]
- 14.Hussain A., Quaresma R., Rahman H. Investigating factors influencing the physicians’ adoption of electronic health record (EHR) in healthcare system of Bangladesh: an empirical study. Int. J. Inf. Manage. 2019;44:76–87. [Google Scholar]
- 15.Kijsanayotin B., Pannarunothai S., Speedie S.M. Factors influencing health information technology adoption in Thailand’s community health centers: applying the UTAUT model. Int. J. Med. Inform. 2009;78(6):404–416. doi: 10.1016/j.ijmedinf.2008.12.005. [DOI] [PubMed] [Google Scholar]
- 16.Steele R., et al. Elderly persons’ perception and acceptance of using wireless sensor networks to assist healthcare. Int. J. Med. Inform. 2009;78(12):788–801. doi: 10.1016/j.ijmedinf.2009.08.001. [DOI] [PubMed] [Google Scholar]
- 17.Gao Y., et al. An empirical study of wearable technology acceptance in healthcare. Ind. Manag. Data Syst. 2015;115(9):1704–1723. [Google Scholar]
- 18.Bawack R.E., Kamdjoug Jean Robert Kala. Adequacy of UTAUT in clinician adoption of health information systems in developing countries: the case of Cameroon. Int. J. Med. Inform. 2018;109:15–22. doi: 10.1016/j.ijmedinf.2017.10.016. [DOI] [PubMed] [Google Scholar]
- 19.Hoque R., Sorwar G. Understanding factors influencing the adoption of mHealth by the elderly: an extension of the UTAUT model. Int. J. Med. Inform. 2017;101:75–84. doi: 10.1016/j.ijmedinf.2017.02.002. [DOI] [PubMed] [Google Scholar]
- 20.Zhou M., et al. Factors influencing behavior intentions to telehealth by Chinese elderly: an extended TAM model. Int. J. Med. Inform. 2019;126:118–127. doi: 10.1016/j.ijmedinf.2019.04.001. [DOI] [PubMed] [Google Scholar]
- 21.Tavares A.I. eHealth, ICT and its relationship with self-reported health outcomes in the EU countries. Int. J. Med. Inform. 2018;112:104–113. doi: 10.1016/j.ijmedinf.2018.01.014. [DOI] [PubMed] [Google Scholar]
- 22.Tsai M.-F., et al. Understanding physicians’ adoption of electronic medical records: healthcare technology self-efficacy, service level and risk perspectives. Comput. Stand. Interfaces. 2019;66(2):1–11. doi: 10.1016/j.csi.2019.04.001. [DOI] [Google Scholar]
- 23.Berglund E., Lytsy P., Westerling R. The influence of locus of control on self-rated health in context of chronic disease: a structural equation modeling approach in a cross sectional study. BMC Public Health. 2014:14. doi: 10.1186/1471-2458-14-492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zou H., et al. Awareness and acceptance of human papillomavirus (HPV) vaccination among males attending a major sexual health clinic in Wuxi, China: a cross-sectional study. Hum. Vaccines Immunother. 2016;12(6):1551–1559. doi: 10.1080/21645515.2015.1099771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kiani Z., et al. Structural equation modeling of psychosocial determinants of health for the empowerment of Iranian women in reproductive decision making. BMC Womens Health. 2020;20(1):19. doi: 10.1186/s12905-020-0893-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yu Y., et al. Human papillomavirus infection and vaccination: awareness and knowledge of HPV and acceptability of HPV vaccine among mothers of teenage daughters in Weihai, Shandong, China. PLoS One. 2016;11(1) doi: 10.1371/journal.pone.0146741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zhang Y.R., et al. Awareness and knowledge about human papillomavirus vaccination and its acceptance in China: a meta-analysis of 58 observational studies. BMC Public Health. 2016:16. doi: 10.1186/s12889-016-2873-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Leung J.T.C., Law C.K. Revisiting knowledge, attitudes and practice (KAP) on human papillomavirus (HPV) vaccination among female university students in Hong Kong. Hum. Vaccines Immunother. 2018;14(4):924–930. doi: 10.1080/21645515.2017.1415685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ho H.S.W. Use of face masks in a primary care outpatient setting in Hong Kong: knowledge, attitudes and practices. Public Health. 2012;126(12):1001–1006. doi: 10.1016/j.puhe.2012.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kumar J., et al. Knowledge, attitude, and practices of healthcare workers regarding the use of face mask to limit the spread of the new coronavirus disease (COVID-19) Cureus. 2020;12(4) doi: 10.7759/cureus.7737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Little T.D., et al. To parcel or not to parcel: exploring the question, weighing the merits. Struct. Equ. Model. 2002;9(2):151–173. [Google Scholar]
- 32.Preacher K.J., Hayes A.F. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav. Res. Methods. 2008;40(3):879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- 33.Staiger D., Stock J.H. Instrumental variables regression with weak instruments. Econometrica. 1997;65(3):557–586. [Google Scholar]
- 34.Qureshi I., Compeau D. Assessing between-group differences in information systems research: a comparison of covariance-and component-based SEM. MIS Q. 2009:197–214. [Google Scholar]
- 35.Tueller S., Lubke G. Evaluation of structural equation mixture models: parameter estimates and correct class assignment. Struct. Equ. Model. 2010;17(2):165–192. doi: 10.1080/10705511003659318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Jedidi K., Jagpal H.S., DeSarbo W.S. Finite-mixture structural equation models for response-based segmentation and unobserved heterogeneity. Mark. Sci. 1997;16(1):39–59. [Google Scholar]
- 37.Becker J.M., et al. Discovering unobserved heterogeneity in structural equation models to avert validity threats. MIS Q. 2013;37(3) p. 665-+ [Google Scholar]
- 38.Bentler P.M., Chou C.-P. Practical issues in structural modeling. Sociol. Methods Res. 1987;16(1):78–117. [Google Scholar]
- 39.MacKinnon D.P., Lockwood C.M., Williams J. Confidence limits for the indirect effect: distribution of the product and resampling methods. Multivariate Behav. Res. 2004;39(1):99–128. doi: 10.1207/s15327906mbr3901_4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ping R.A. Estimating latent variable interactions and quadratics: the state of this art. J. Manage. 1996;22(1):163–183. [Google Scholar]
- 41.Podsakoff P.M., et al. Common method biases in behavioral research: a critical review of the literature and recommended remedies. J. Appl. Psychol. 2003;88(5):879–903. doi: 10.1037/0021-9010.88.5.879. [DOI] [PubMed] [Google Scholar]
- 42.Mohamed M., et al. The influence of vehicle body type in shaping behavioural intention to acquire electric vehicles: a multi-group structural equation approach. Transp. Res. Part A-Policy Pract. 2018;116:54–72. [Google Scholar]
- 43.Bollen K., Lennox R. Conventional wisdom on measurement – a structural equation perspective. Psychol. Bull. 1991;110(2):305–314. [Google Scholar]
- 44.Duncan O.D. In: Introduction to Structural Equation Models. Duncan O.D., editor. Academic Press; San Diego: 1975. Introduction to structural equation models; pp. 1–173. [Google Scholar]
- 45.James L.R., Brett J.M. Mediators, moderators, and tests for mediation. J. Appl. Psychol. 1984;69(2):307–321. [Google Scholar]
- 46.Baron R.M., Kenny D.A. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J. Pers. Soc. Psychol. 1986;51(6):1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 47.Hair J.F., et al. An assessment of the use of partial least squares structural equation modeling in marketing research. J. Acad. Mark. Sci. 2012;40(3):414–433. [Google Scholar]
- 48.Alhomoud F.K., Basil M., Bondarev A. Knowledge, attitudes and practices (KAP) relating to dietary supplements among health sciences and non-health sciences students in one of the universities of United Arab Emirates (UAE) J. Clin. Diagn. Res. 2016;10(9):JC5–JC9. doi: 10.7860/JCDR/2016/19300.8439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ma Y., et al. Knowledge, Attitudes and Practices (KAP) toward seasonal influenza vaccine among young workers in South China. Hum. Vaccin. Immunother. 2018;14(5):1283–1293. doi: 10.1080/21645515.2017.1423157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Zhou M., et al. Understanding psychological determinants to promote the adoption of general practitioner by Chinese elderly. Health Policy Technol. 2019;8(2):128–136. [Google Scholar]
- 51.Foong H.F., et al. Predicting cognitive function of the Malaysian elderly: a structural equation modelling approach. Aging Ment. Health. 2018;22(1):109–120. doi: 10.1080/13607863.2016.1231172. [DOI] [PubMed] [Google Scholar]
- 52.Dunnebeil S., et al. Determinants of physicians’ technology acceptance for e-health in ambulatory care. Int. J. Med. Inform. 2012;81(11):746–760. doi: 10.1016/j.ijmedinf.2012.02.002. [DOI] [PubMed] [Google Scholar]
- 53.Hennemann S., et al. Acceptance and barriers to access of occupational e-mental health: cross-sectional findings from a health-risk population of employees. Int. Arch. Occup. Environ. Health. 2018;91(3):305–316. doi: 10.1007/s00420-017-1280-5. [DOI] [PubMed] [Google Scholar]
- 54.Emmert M., Wiener M. What factors determine the intention to use hospital report cards? The perspectives of users and non-users. Patient Educ. Couns. 2017;100(7):1394–1401. doi: 10.1016/j.pec.2017.01.021. [DOI] [PubMed] [Google Scholar]
- 55.Dwivedi Y.K., et al. A generalised adoption model for services: a cross-country comparison of mobile health (m-health) Gov. Inf. Q. 2016;33(1):174–187. [Google Scholar]
- 56.Huang Y., et al. Measures undertaken in China to avoid COVID-19 infection: internet-based, cross-sectional survey study. J. Med. Internet Res. 2020;22(5) doi: 10.2196/18718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Zhao Y.X., et al. Chinese public’s attention to the COVID-19 epidemic on social media: observational descriptive study. J. Med. Internet Res. 2020;22(5) doi: 10.2196/18825. [DOI] [PMC free article] [PubMed] [Google Scholar]