Abstract
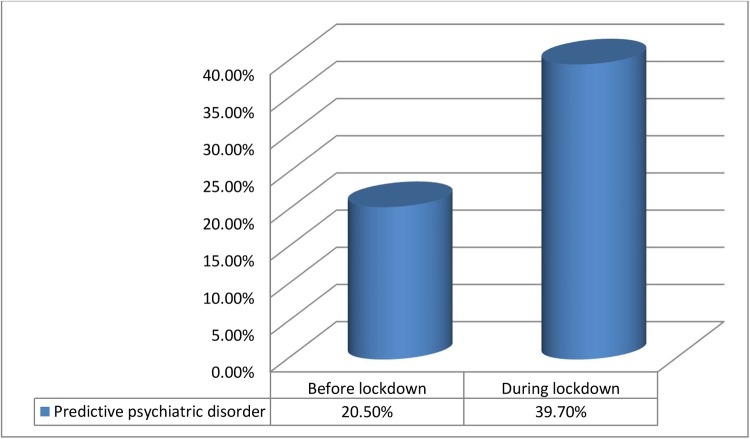
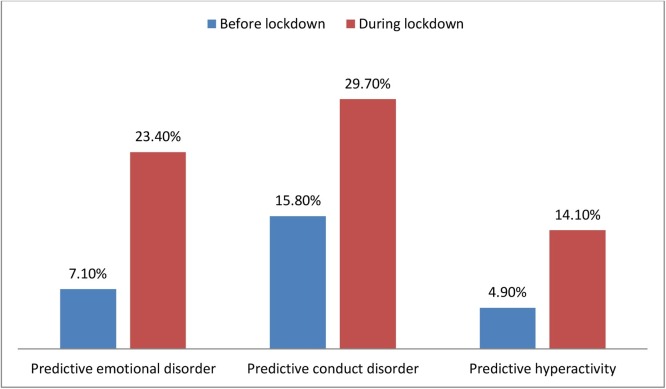
Lockdown, isolation, quarantine and social distancing are proved to be only effective measures to prevent and tackle COVID-19 till date. Unfortunately, these measures have caused physical, economical and mental health problems. Children and adolescents are not immune to the adverse mental health effect due to the new changes. Research around the globe shows children and adolescents are suffering from an increased number of depressive symptoms, clinginess, inattention, irritability and worry. This cross-sectional online-based survey type study was aimed to get a snapshot of the prevalence of predictive psychiatric disorders in the child and adolescent population in Bangladesh before and during lockdown. Validated Bangla parent version of Strengths and Difficulties Questionnaire was used to assess the psychopathology among subjects. Total sample was 552 aged from 4–17 years. Boy-girl ratio was 1.3:1. Prevalence of any predictive psychiatric disorder before lockdown was 20.5 % and within lockdown was 39.7 % and the difference was highly significant (P < 0.001). Prevalence of emotional, conduct disorder and hyperactivity were also increased significantly during the lockdown period than before. Conduct disorder and hyperactivity were more prevalent among boys both before and within lockdown. In contrast, prevalence of emotional disorder was higher among girls before lockdown but within the lockdown period, the boy-girl prevalence was almost the same. This study shows the new extreme measures to tackle COVID-19 has a disaster impact on mental health of children and adolescents. Subsequent studies and support should be developed to prevent conditions getting worse.
Keywords: COVID-19, Lockdown, Impact, Prevalence, Psychiatric disorders, Children and adolescents
1. Introduction
When the COVID-19 pandemic started there was very little we could do to prevent letting the situation get out of hand. Maintaining hygiene, following the lockdown, self-isolation, quarantine and social distancing —overall the non-pharmacological measures are proved only effective way (Flaxman et al., 2020) to prevent and tackle COVID-19 until any vaccine or specific treatment comes forward. Unfortunately, these measures have some adverse effects and people around the globe are suffering a great deal due to the strict measures. Alongside with physical and economic problems, mental health problems become a burning issue during this pandemic. A representative study among adults in China where the COVID-19 discovered first in the world showed 26 % of the people were suffering from mild to moderate depression and 4.3 % were suffering from severe and extremely severe depression. Moreover, 27.9 % were suffering from mild to moderate anxiety and 8.4 % were having severe and extremely severe forms of anxiety (Wang et al., 2020). In the New York City, USA, study showed 69 % of the people in the quarantine area of the city had moderate to severe anxiety/distress and 24.8 % people having anxiety/distress to such level, to had impairment in functioning (Rosen et al., 2020).
Sad but true, children and adolescents around the world are not immune to the psychological problem due to the measures taken to control the COVID-19 pandemic situation and this is not the first time the world has encountered health related disasters, and strict measures. During the Methicillin-Resistance Staphylococcus Aureus (MRSA), 42 % of primary care givers of 1–17 years old children reported changes in household interaction (Muenks et al., 2018). In West Africa, in the time of the Ebola epidemic children and adolescents developed stigma and disease fear (Denis-Ramirez et al., 2017). Children who were quarantined during the health hazard such as Influenza A virus subtype H1N1, SARS, Avian influenza had PTSD four times higher than those who were not and were suffering from acute stress disorder, adjustment disorder and grief (Sprang and Silman, 2013). During the Tsunami in South East Asia, there was increased level of posttraumatic stress reaction in children (Dyb et al., 2011).
What is the mental health situation of children and adolescents in this current COVID-19 pandemic? In Shaanxi province of China, a leading study among children and adolescents aged from 3 to 18 years showed people more than 35 % had clingy behavior, around 32 % had irritability and about 28 % showed worry (Jiao et al., 2020). In the US city of New York, 5.5 % parents reported that their children had significant distress (Rosen et al., 2020). Another study among 4–10 years children in Italy reported that 26.48 % had sleeping problems. These proportions of people were competent enough to sleep alone before COVID-19 pandemic, but during this emergency, they asked to sleep in their parents’ bed (Pisano et al., 2020). Italy and Spain are the one of the countries that suffers the most during the early stage of the Pandemic. A Study was conducted in both the countries measuring immediate psychological effect of the COVID-19 quarantine between child and adolescent aged from 3 to 18. This study showed the most frequent symptoms were difficulty concentrating, boredom, irritability, nervousness and worry (Orgilés et al., 2020). Moreover, children in isolated COVID-19 ward can lead to anxiety, loneliness, distress, fear and stress related problems that further exaggerated when parents or family members had COVID-19 infection for which psychological intervention were required to prevent serious consequences (Sahoo et al., 2020a). There are very little information regarding psychological effects due to the COVID-19 quarantine in children and adolescents in Bangladesh. One study showed 6.2 % children had moderate to severe depression, 6.9 % had moderate to severe anxiety and 4.9 % had moderate to severe sleeping problems (Yeasmin et al., 2020).
All most all countries are adapting the new ways to carry on the normal activities. Classes are converted into online classes and home based e-learning. Children are not the exception. School plays a very important role in healthy mental health development among children and adolescents.
The measures taken to prevent spreading coronavirus affected the mental health of all people, but the children and adolescents may face more negative mental health impact than adults. As coping is developmentally acquired skills (Fields and Prinz, 1997), young people find it difficult to cope with this new difficult situation. Thus, more study needs to be conducted regarding child and adolescent mental health in this pandemic in order to tackle the mental health burden of this population, which is at hand, and to be prepared for the future. No structured study was reported on children and adolescents to find out the mental health burden in this pandemic in Bangladesh. This study was aimed to delineate the changes of prevalence of predictive psychiatric disorders among children and adolescents in Bangladesh during the lockdown state due to Novel Coronavirus pandemic and to find out the impact of these disorders on them and burden to their families before and during COVID-19 lockdown.
2. Materials and methods
This was a one-stage, cross sectional survey type study carried out between June 2020 and August 2020. Sampling technique was purposive and a designed Google form was used to collect data. Children and adolescents aged between 4 and 17 years were included in the study. Parents of the children and adolescents who were willing to participate were approached. At the beginning of the questionnaire, the purpose of the study was mentioned and there were written instructions in Bangla regarding how to fill up the form. Parents were also instructed that they should choose one child by lottery if they have more than one child. The link of the Google form was made available in different social media by the authors. Furthermore, people were asked to share the link within their circle.
Two sets of questionnaires were used in the study. First one was a structured questionnaire designed by the researchers that contained socio-demographic and COVID-19 related variables such as any COVID-19 cases (both previous and current cases during the time of filling up the google form) and any death due to COVID-19 in the family. Second one was, validated parent version of Bangla Strengths and Difficulties Questionnaire (SDQ) for screening psychopathology (Mullick and Goodman, 2001). SDQ has three versions: self, parent and teacher. SDQ consists of 25 attributes both positive and negative, designed to detect the emotional problem, conduct problem, hyperactivity, peer problem and prosocial behavior. SDQ also includes a brief impact supplement to measure the overall distress, social impairment, burden and chronicity of the sample. Only the parent version was used in this study. For the best possible use in the lockdown situation, SDQ was tailored to get the overall picture of the child and adolescents mental health in both the six-month period before the starting of the lockdown and during the lockdown. Thus, the same questions were used to measure the mental health condition. Moreover, as the schools were closed during the pandemic, question number 4, 12, 20 and 22 were adjusted to match the new situation. Expert’s opinion was obtained and regarding finalizing the adjustments. On the 26 March 2020, lockdown was imposed officially in Bangladesh to tackle the Novel Coronavirus. Parents were instructed to give information of their children’s behavior six month prior 26 March 2020 and after.
During analysis, the prevalence of predicting any psychiatric disorder, emotional disorder, conduct disorder and hyperactivity problem were made using the cutoff algorithm of symptoms score and impact score. Prevalence was calculated for both before and during the lockdown. Moreover, paired sample t-test was used to detect any significant changes due to the lockdown. Further chi-square test was used to find out any association between predicting disorders and socio-demographic and other related variables.
3. Results
Upon analysis of the socio-demographic variables of the total sample 552, boy-girl ratio was 1.3:1. Age range of the sample was 4–17 years with the mean of 10.4 ± 4.1years. For the purpose of the analysis, the sample was clustered into children (4–10 years) and adolescents (11–17 years) which were 53.1 % and 46.9 % respectively. Majority of the subjects were from nuclear families (71.7 %) and the rest 28.3 % were from joint families. Most of the subjects were from the middle-income group (83.7 %). Only 9.1 % were from low and 7.2 % were from high income groups. Urban-rural distribution was 67.5 % and 32.5 % respectively. Exploring the COVID-19 cases within the family, 10.3 % were found COVID-19 positive and among them 1.4 % people died.
Fig. 1 shows the prevalence of predictive psychiatric disorder among the subjects before and during lockdown. It depicts that any predictive psychiatric disorder was found 20.5 % before lockdown and it increased into 39.7 % within the lockdown. The paired t-test showed high levels of significance between before and within lockdown (t = -14.812; P < 0.001).
Fig. 1.
Prevalence of predictive psychiatric disorders.
Fig. 2 shows the prevalence of specific psychiatric disorders among the subjects before and during lockdown due to the pandemic. Specifically, predictive emotional, conduct disorder and hyperactivity —all were increased during the lockdown. These differences of prevalence were found highly significant in paired t-test.
Fig. 2.
Prevalence of specific psychiatric disorders.
The boy-girl prevalence of predictive psychiatric disorders of the subjects were shown in the Table 1 . Boys suffered more from any psychiatric disorder than girls before the lockdown were. (22.1 % vs. 18.3 %) During the lockdown period boy-girl prevalence increased into 42.6 % and 35.7 % respectively. Emotional disorder before lockdown was found more among the girls (9.4 %) than boys (5.4 %) and it reached the level of significance at 5% level. During the lockdown period, prevalence of all forms of psychiatric disorders were increased in both the boys and girls, but the boys had slightly higher prevalence (24 %) than girls (22.6 %) did. Conduct disorder and hyperactivity was more prevalent among the boys both before and during lockdown. Chi-square test revealed that there was significant association between boys with conduct disorder during lockdown period (p < 0.05). Within the lockdown period, the prevalence of conduct disorder among the boys and girls were 32.8 % and 25.5 % respectively. Hyperactivity was significantly increased among the boys during the lockdown period than the girls which was highly significant (p < 0.001).
Table 1.
Prevalence of psychiatric disorders according to gender.
| Gender |
||||
|---|---|---|---|---|
| Predictive psychiatric disorder | Boy |
Girl |
||
| Before lockdown n (%) | During lockdown n (%) | Before lockdown n (%) | During lockdown n (%) | |
| Any psychiatric disorder | 70 (22.1) | 135 (42.6) | 43 (18.3) | 84 (35.7) |
| Emotional disorder | 17 (5.4) | 76 (24.0) | 22 (9.4) | 53 (22.6) |
| Conduct disorder | 56 (17.7) | 104 (32.8) | 31 (13.2) | 60 (25.5) |
| Hyperactivity | 20 (6.3) | 58 (18.3) | 7 (3.0) | 20 (8.5) |
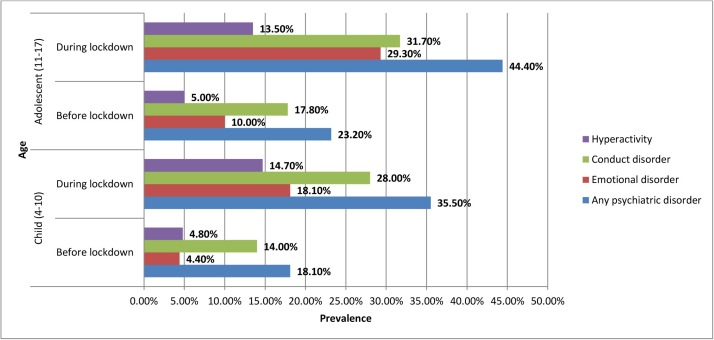
Analysis was done to compare the prevalence of predictive psychiatric disorders among the children and adolescents age groups of the subjects and it is shown in Fig. 3 . Adolescents had more any form of psychiatric, emotional, conduct disorder and hyperactivity than children were both before and during lockdown. Any psychiatric disorder during the lockdown period was found significantly (p < 0.05) higher among the adolescents (44.4 %) than children (35.5 %). Furthermore, emotional disorder both before and during lockdown was found statistically significant among the adolescents. Before the lockdown, prevalence of emotional disorder was 4.4 % among child and 10.0 % adolescent subjects and the difference was significant (p < 0.005). During the lockdown, prevalence of emotional disorder among children and adolescents was 18.1 % and 29.3 % respectively. This difference was also significant (p < 0.001).
Fig. 3.
Prevalence of specific psychiatric disorder by child and adolescent age group.
Other socio-demographic variables such as family type, habitat, and income group were analyzed and no statistically significant association was found between these variables and psychiatric disorders.
Further analysis was made to see any association between specific psychiatric disorders and death of the family members due to COVID-19. Only emotional disorder (62.5 %) was found statistically significant (p < 0.05) in those who had death due to COVID-19 in the family. In contrast, 22.8 % had emotional disorder without any history of death due to COVID-19.
Change in the impact on the subjects due to their mental health problems before and during lockdown was also significant. Before the lockdown, impact score was as follows: no impact 52.2 %, slight impact 6.0 %, high impact 5.6 %, and very high impact 36.2 %. On the other hand, the impact score during the lockdown was found as: no impact 43.1 %, slight impact 6.0 %, high impact 5.6 %, and very high impact 36.2 %. This change in the impact was found highly significant in paired sample t-test {Mean = -1.607 (-1.897 to -1.317, t = -10.864, P < 0.001)}.The impact on various areas of daily life is presented in Table 2 . It shows that all the areas namely, home life, friendship, learning and leisure activities of the subjects were significantly impaired during the lockdown than before lockdown.
Table 2.
Impact on the areas of daily life of the subjects before and during lockdown.
| Before lockdown |
During lockdown |
|||||||
|---|---|---|---|---|---|---|---|---|
| Aspects of life | Not at all n (%) | Only a little n (%) | A medium amount n (%) | A great deal n (%) | Not at all n (%) | Only a little n (%) | A medium amount n (%) | A great deal n (%) |
| Home life | 373(67.6) | 124(22.5) | 50(9.1) | 5(0.9) | 300(54.3) | 119(21.6) | 81(14.7) | 52(9.4) |
| Friendship | 378(68.5) | 107(19.4) | 59(10.7) | 8(1.4) | 324(58.7) | 101(18.3) | 99(17.8) | 28(5.1) |
| Lesson | 367(66.5) | 105(19.0) | 65(11.8) | 15(2.7) | 289(52.4) | 98(17.8) | 87(15.8) | 78(14.1) |
| Leisure | 400(72.5) | 98(17.8) | 44(8.0) | 10(1.8) | 321(58.2) | 98(17.8) | 102(18.5) | 31(5.6) |
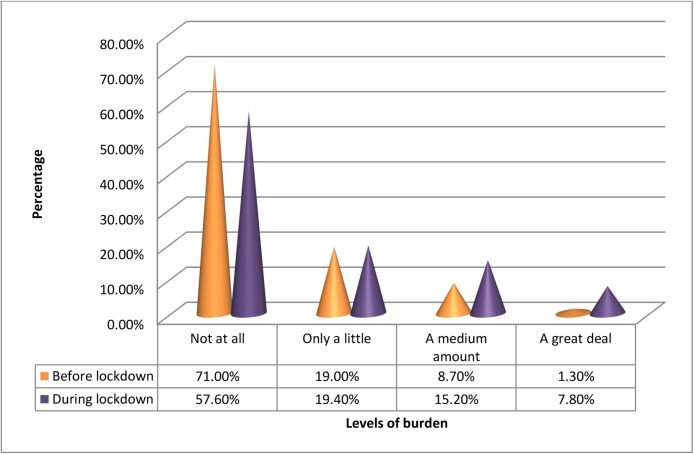
Fig. 4 shows different levels of burden on the families of the subjects before and during the lockdown. Overall, burden to the families of the subjects were also increased significantly (t = -10.534, p < 0.001) during the period of lockdown than before the lockdown.
Fig. 4.
Burden on the families of the subjects before and during the lockdown.
Analysis was also done on the continuity of psychiatric disorder before and during the lockdown period and newly developed psychiatric disorders during lockdown period. In total, 107(94.7 %) subjects either remained with the disorder or developed a new comorbid disorder during lockdown. Only six (5.3 %) subjects’ score did not reach the SDQ cut-offs of SDQ during the lockdown who had previous psychiatric disorders. On the other hand, newly developed any form of psychiatric disorder during lockdown was found 112 (25.5 %).
4. Discussion
The mental health problems are already a challenge, which we are facing. This study was able to find out the prevalence before the lockdown and what changes had occurred during the lockdown. Moreover, the study will be able to find out the role of lockdown to change predictive psychiatric disorder.
Overall, prevalence of predictive psychiatric disorders among children and adolescents was found 20 % before the lockdown in this study. This finding is very similar to the results of the first community-based study in Bangladesh, which revealed the prevalence of psychiatric disorder among 5–10 years old was 15 % (Mullick and Goodman, 2005). Another one-stage community study showed psychiatric disorders were present 18 % among the 5–17 years by using SDQ screening (Mullick and Goodman, 2001). A very representative meta-analysis included 41 studies from 27 countries around the world region showed the prevalence of psychiatric disorder among children and adolescents was 13.4 % (Polanczyk et al., 2015).Around the globe, overall prevalence is 10–20 % (Bird, 1996; Shaffer et al., 1996; Roberts et al., 1998; Hacket and Hacket, 1999; Meltzer et al., 2003; Malhotra and Patra, 2014; Shen et al., 2018).In this study, it was found that the prevalence of emotional disorder before lockdown was 7.1 %. In one study in Bangladesh emotional disorder was found 8.6 % by parent SDQ only (Mullick and Goodman, 2001).In one study in the US emotional disorders were found 6.7 % among young people aged from 6 to 17 years. (Blanchard et al., 2005). Another study revealed 6.8 % of children aged from 9 to16 years were suffering from emotional disorder (Costello et al., 2003). Conduct disorder was 15.8 % before lockdown. In Bangladesh, the prevalence of conduct disorder was found 3.1 % (Mullick and Goodman, 2001) according to the parent SDQ report. In US, conduct disorder was found 6.7 % (Blanchard et al., 2005). This study also revealed that before lockdown hyperactivity problem was found 4.9 %, which is slightly less than the representative study in Bangladesh. It was reported that 6.2 % children and adolescents aged between 4–16 years had hyperkinesis according to parent SDQ (Mullick and Goodman, 2001).In the US prevalence of hyperactivity was ranged from 0.9 to 8.8 %. (Blanchard et al., 2005; Costello et al., 2003). The variation of results might be due to the study design mainly one-stage screening of the psychopathology and sample collection technique. Moreover, the number may have changed as the time passes. In one study, it showed the worldwide coverage of conduct disorder, ADHD had doubled and emotional disorder had increased fourfold. Moreover, the prevalence of depression and anxiety disorder also increased significantly in recent years (Erskine et al., 2017).
This study revealed that during the lockdown period, the overall prevalence of any predictive psychiatric disorder had increased significantly than about the six-month period before the starting of the lockdown. Furthermore, the specific psychiatric disorders had also increased significantly among the child and adolescents. During the lockdown period, predictive psychiatric disorder had increased into 39.7 % and emotional disorder, conduct disorder and hyperactivity were increased into 23.4 %, 29.7 % and 14.1 % respectively. Other studies had also found the increased mental health burden among the children and adolescents. One study in China, during the COVID-19 pandemic, showed most prevalent symptoms among children and adolescents were anxiety 24.9 %, depression 19.7 % and stress 15.2 % (Tang et al., 2020). Another study in China showed 19 % adolescents suffer anxiety (Qi et al., 2020). In Italy, a representative study revealed that 53.5 % of young people were suffering from irritability, intolerance to rules and excessive demands (Pisano et al., 2020). Another study in Spain and Italy showed 45.5 % of Spanish children were restless, 15.7 % were anxious 49.4 % were bored. Italian children, on the other hand, 34.7 % restless, 20.5 % anxious and 53.8 % were bored (Orgilés et al., 2020). In our study, ADHD had increased more than three fold. One study reported that during the COVID-19 outbreak, children’s ADHD symptoms were significantly worse compared to normal states that raise the importance of focusing on a special vulnerable group during the disease outbreak (Zhang et al., 2020).
In the present study, emotional disorder was found significantly higher among the subjects who had lost their family members by death due to COVID-19. As part of grief reaction and extraordinary traumatic stress, emotional disorder can be expected to be higher among those who had such kind of death within the family.
The COVID-19 pandemic has made the mental burden of the children and adolescents worse. To prevent the spread of the coronavirus, the world has taken the non-pharmacological management (lockdown, isolation, social distancing, school closure etc.). Bangladesh has also implicated this kind of preventive management. Certainly, this measure has a negative impact on children and adolescents despite its effectiveness in COVID-19 prevention. Peer relationship, friendly classroom environment has a very positive effect on children and adolescents in their better emotional wellbeing and positive self-concept (Oberle, 2018). Though almost all countries have adapted the online classes and e-learning, it is not able to provide the same effect as the live school environment. It has been reported that online classes during lockdown due to COVID-19 have a negative impact on the behaviour and physical health of the children which is indicative that the level of learning with regular classes, cannot be matched by the online classes.information and support (Grover et al., 2020). Lack of such healthy milieu for a long period has detrimental effects on the mental health of children and adolescents. Therefore, an alternative supportive environment needs to be adopted for this population.
This study had found that any kind of psychiatric disorder among children was less than that of the adolescents both before and during the lockdown. This result matches with other studies before the pandemic. One representative study in the UK showed comparatively less prevalence of psychiatric disorder among children aged from 5–10 years (8%) than adolescents aged from 11 to 15 years (11.2 %) (Meltzer et al., 2003). One leading study in Bangladesh also showed the similar type of result (Mullick and Goodman, 2005). The adolescents tend to experience emotions more intensely. Having teenagers confined to their homes with constant parental attention/supervision can create a great degree of irritation, as they are not used to such situations. Moreover, adolescents find it quite difficult to practice social distancing. All these can also lead to excessive worrying, fear, and anxiety about contracting the infection and can create a sense of panic among teenagers. Further, the excessive abuse of social media and telecommunication materials can affect the mental well-being of teenagers and can lead to excessive worry and subsequent severe anxiety symptoms (Sahoo et al., 2020b). It can be said that the disease process is still the same during the lockdown situation but people, particularly children and adolescents, became more vulnerable due the huge amount of stress resulting from extreme measures for tackling the current pandemic. Thus, the increased amount of psychiatric disorders are prevalent in this population during the lockdown period.
Same light can be put on the difference between the prevalence of psychiatric disorders among boys and girls. In the present study, boys were more prone to behavioral disorder than girls were both before and during the lockdown state. On the other hand, girls were more prevalent to emotional disorder before the lockdown. Studies before the pandemic showed similar kinds of results (Meltzer et al., 2003; Fleitlich-Bilyk and Goodman, 2004; Shen et al., 2018; Mullick and Goodman, 2001;, 2005; Rabbani et al., 2009; Rutter, 1976). The present study revealed, during the lockdown emotional disorder found slightly high among the boys. This finding indicates that irrespective of gender, traumatic and enduring stress like COVID-19 causes increased mental health problems in general.
Due to the difficulties of the children and adolescents, parents also suffer substantially. In this study, the families of the subjects perceived the difficulties of their children and adolescents as “a great deal” which increased seven times during the lockdown than before the lockdown. Family members were already anxious regarding the COVID-19; they may worry about the health and economic condition of their family, preoccupied with management, outcome of the home schooling (Fontanesi et al., 2020). On top of that, they were dealing with the difficulties of their children. This can help to explain the reason for increased burden during the lockdown. From this result, it can be assumed that parents may also be vulnerable to psychiatric disorders during the lockdown period or they already had some kind of psychiatric disorders. Further exploration is required on this aspect. Existing increased rates of psychiatric disorders have a severe impact on the children and adolescents and that caused huge burden on their families. If these psychiatric disorders among children and adolescents are not treated, these impacts and burdens will certainly increase and have detrimental effects on both children and parents’ life.
Present study is the first to explore the prevalence and broad types of psychiatric disorders before and during COVID-19 in Bangladesh based on sound methodological foundation. However, it has few limitations. The sample size was relatively small to represent the child and adolescent population of Bangladesh. Sampling bias was present, as the link of the Google form was made available online within the authors’ circle; subjects were more from urban areas and middle-income families. The parents’ perception may be colored with the present extraordinary stressful situation in providing information on psychiatric problems of the subjects before lockdown. Thus, caution is necessary to generalize the findings of the study. Only parent rated information was collected for assessing psychiatric problems of the study population. However, the results have strong predictive value as we used a culturally adopted and validated screening tool. Subsequent large-scale studies including children and adolescents from all strata, using structured measures of psychiatric diagnostic interview are required to confirm the findings of the study.
Nearly 2–3 times increased rate of prevalence of psychiatric disorders among this population during COVID-19 lockdown must be addressed to prevent mental health epidemic among them. In this changing scenario for COVID-19, it is necessary to make an immediate and long-term strategic plan, resource allocation, task shifting and feasible intervention plan. In this crisis moment it is very difficult to seek expert advice. Therefore, alternative forms of wellness activities at home could help prevention as well as intervention. Internet-based assessment and management are proved to be effective in this regard.
Financial discloser
None.
Declaration of Competing Interest
The authors report no declarations of interest.
Acknowledgement
None.
References
- Bird H.R. Epidemiology of childhood disorders in a cross-cultural context. J. Child Psychol. Psychiatry. 1996;37:35–49. doi: 10.1111/j.1469-7610.1996.tb01379.x. [DOI] [PubMed] [Google Scholar]
- Blanchard L.T., Gurka M.J., Blackman J.A. Emotional, developmental and behavioral health of American children and their families: a report from the 2003 national survey of children’s health. Pediatrics. 2005;117:e1202–e1212. doi: 10.1542/peds.2005-2606. [DOI] [PubMed] [Google Scholar]
- Costello E.J., Mustillo S., Erkanli A., keeler G., Angold A. Prevalence and development of psychiatric disorder in childhood and adolescence. Arch. Gen. Psychiatry. 2003;60:837–844. doi: 10.1001/archpsyc.60.8.837. [DOI] [PubMed] [Google Scholar]
- Denis-Ramirez E., Sorensen K.H., Skovdal M. In the midst of a “perfect storm”: unpacking the cause and consequences of Ebola-related stigma for children orphaned by Ebola in Sierra Leone. Child. Youth Serv. Rev. 2017;73:445–453. [Google Scholar]
- Dyb G., Jensen T.K., Nygaard E. Children’s and parents’ posttraumatic stress reactions after the 2004 tsunami. Clin. Child Psychol. Psychiatry. 2011;16(4):621–634. doi: 10.1177/1359104510391048. [DOI] [PubMed] [Google Scholar]
- Erskine H.E., Baxter A.J., Patton G., et al. The global coverage of prevalence data for mental disorders in children and adolescents. Epidemiol. Psychiatr. Sci. 2017;26:395–402. doi: 10.1017/S2045796015001158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fields L., Prinz R.J. Coping and adjustment during childhood and adolescence. Clin. Psychol. Rev. 1997;17(8):937–976. doi: 10.1016/s0272-7358(97)00033-0. [DOI] [PubMed] [Google Scholar]
- Flaxman S., Mishra S., Gandy A., et al. Imperial College London; 2020. Estimating the Number of Infections and the Impact of Non-pharmaceutical Interventions on COVID-19 in 11 European Countries. [DOI] [Google Scholar]
- Fleitlich-Bilyk B., Goodman R. The prevalence of child psychiatric disorders in Southeast Brazil. J. Child Psychol. Psychiatric. 2004;43:727–734. doi: 10.1097/01.chi.0000120021.14101.ca. [DOI] [PubMed] [Google Scholar]
- Fontanesi L., Marchetti D., Mazza C., Di Giandomenico S., Roma P., Verrocchio M.C. Psychological Trauma: Theory, Research, Practice, and Policy. Advance Online Publication. 2020. The effect of the COVID-19 lockdown on parents: a call to adopt urgent measures. [DOI] [PubMed] [Google Scholar]
- Grover S., Goyal S.K., Mehra A., et al. A survey of parents of children attending the online classes during the ongoing COVID-19 pandemic. Indian J. Pediatr. 2020 doi: 10.1007/s12098-020-03523-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hackett R., Hackett L. Child psychiatry across cultures. Int. Rev. Psychiatry. 1999;11:225–235. [Google Scholar]
- Jiao W.Y., Wang L.N., Liu J., et al. Behavioral and emotional disorders in children during the COVID-19 epidemic. J. Pediatr. 2020;221:264–266. doi: 10.1016/j.jpeds.2020.03.013. e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malhotra S., Patra B.N. Prevalence of child and adolescent psychiatric disorders in India: a systematic review and meta-analysis. Child Adolesc. Psychiatry Ment. Health. 2014;8:22. doi: 10.1186/1753-2000-8-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meltzer H., Gatward R., Goodman R., Ford T. Mental health of children and adolescents in Great Britain. Int. Rev. Psychiatry. 2003;15:185–187. doi: 10.1080/0954026021000046155. [DOI] [PubMed] [Google Scholar]
- Muenks C.E., Sewell W.C., Hogan P.G., et al. Methicillin-Resistant Staphylococcus aureus: the effects are more than skin deep. J. Pediatr. 2018;199:158–165. doi: 10.1016/j.jpeds.2018.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mullick M.S.I., Goodman R. Questionnaire screening for mental health problems in Bangladeshi children: a preliminary study. Soc. Psychiatry Psychiatr. Epidemiol. 2001;36:94–99. doi: 10.1007/s001270050295. [DOI] [PubMed] [Google Scholar]
- Mullick M.S.I., Goodman R. The prevalence of psychiatric disorder among 5-10 years olds in rural, urban and slum areas in Bangladesh. Soc. Psychiatry Psychiatr. Epidemiol. 2005;40:663–671. doi: 10.1007/s00127-005-0939-5. [DOI] [PubMed] [Google Scholar]
- Oberle E. Early adolescents’ emotional well-being in the classroom: the role of personal and contextual assets. J. Sch. Health. 2018;88:101–111. doi: 10.1111/josh.12585. [DOI] [PubMed] [Google Scholar]
- Orgilés M., Morales A., Delvecchio E., Mazzeschi C., Espada J.P. 2020. Immediate Psychological Effects of the COVID-19 Quarantine in Youth From Italy and Spain. [WWW Document] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pisano L., Galimi D., Cerniglia L. 2020. A Qualitative Report on Exploratory Data on the Possible emotional/behavioral Correlates of Covid-19 Lockdown in 4-10 Years Children in Italy. [WWW Document]. [DOI] [Google Scholar]
- Polanczyk G.V., Salum G.A., Sugaya L.S., Caye A., Rohde L.A. Annual research review: a meta-analysis of the worldwide prevalence of mental disorders in children and adolescents. J. Child Psychol. Psychiatry. 2015;56(3):345–365. doi: 10.1111/jcpp.12381. [DOI] [PubMed] [Google Scholar]
- Qi H., Liu R., Chen X., et al. Prevalence of anxiety and associated factors for Chinese adolescents during the COVID-19 outbreak. Psychiatry Clin. Neurosci. 2020 doi: 10.1111/pcn.13102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rabbani M.G., Alam M.F., Ahmed H.U., Sarkar M., Islam M.S., Anwar N. Prevalence of mental disorders, mental retardation, epilepsy and substance abuse in children. Bangladesh J. Psychiatry. 2009;23:11–52. [Google Scholar]
- Roberts R.E., Attkisson C.C., Rosenblatt A. Prevalence of psychopathology among children and adolescents. Am. J. Psychiatry. 1998;155:715–726. doi: 10.1176/ajp.155.6.715. [DOI] [PubMed] [Google Scholar]
- Rosen Z., Weinberger-Litman S.L., Rosenzweig C., et al. 2020. Anxiety and Distress Among the First Community Quarantined in the U.S Due to COVID-19: Psychological Implications for the Unfolding Crisis. [WWW Document] [DOI] [Google Scholar]
- Rutter M. Isle of Wight study, 1964-1974. Psychol. Med. (Paris) 1976;6:313–332. doi: 10.1017/s003329170001388x. [DOI] [PubMed] [Google Scholar]
- Sahoo S., Mehra A., Suri V., et al. Handling children in COVID wards: a narrative experience and suggestions for providing psychological support. Asian J. Psychiatry. 2020;53 doi: 10.1016/j.ajp.2020.102207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sahoo S., Rani S., Shah R., Singh A.P., Mehra A., Grover S. COVID-19 pandemic-related anxiety in teenagers. Indian J. Psychiatry. 2020;62:328–330. doi: 10.4103/psychiatry.IndianJPsychiatry_327_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaffer D., Fisher P., Dulcan M.K., et al. The NIMH diagnostic interview schedule for children version 2.3 (DISC-2-3): description, acceptability, prevalence rates, and performance in the MECA study. J. Am. Acad. Child Adolesc. Psychiatry. 1996;35:865–877. doi: 10.1097/00004583-199607000-00012. [DOI] [PubMed] [Google Scholar]
- Shen Y.M., Chan B.S.M., Liu J.B., et al. The prevalence of psychiatric disorders among students aged 6-16 years old in central Hunan, China. BMC Psychiatry. 2018;18(243):1–9. doi: 10.1186/s12888-018-1823-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sprang G., Silman M. Posttraumatic stress disorder in parents and youth after health – related disasters. Disaster Med. Public Health Prep. 2013;7:105–110. doi: 10.1017/dmp.2013.22. [DOI] [PubMed] [Google Scholar]
- Tang S., Xiang M., Cheung T., Xiang Y.T. Mental health and its correlates among children and adolescents during COVID-19 school closure: the importance of parent-child discussion. J. Affect. Disord. 2020 doi: 10.1016/j.jad.2020.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S., Ho R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Public Health. 2020;17:1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeasmin S., Banik R., Hossain S., et al. Impact of COVID-19 pandemic on the mental health of children in Bangladesh: a cross-sectional study. Child. Youth Serv. Rev. 2020;117 doi: 10.1016/j.childyouth.2020.105277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang J., Shuai L., Yu H., et al. Acute stress, behavioural symptoms and mood states among school-age children with attention-deficit/hyperactive disorder during the COVID-19 outbreak. Asian J. Psychiatry. 2020;51 doi: 10.1016/j.ajp.2020.102077. [DOI] [PMC free article] [PubMed] [Google Scholar]