Following the onset of the COVID-19 pandemic, by February 2020, there was widespread speculation circulating on social media and in the medical press that treatment with medications that inhibit the renin-angiotensin system might increase susceptibility to COVID-19.1 This concern was not insignificant because, globally, hundreds of millions of people are treated with renin-angiotensin system inhibitors, particularly angiotensin-converting enzyme inhibitors (ACEIs) or angiotensin-receptor blockers (ARBs) for hypertension, heart failure, or chronic kidney disease. Many wondered if they should discontinue these treatments, and inevitably some will have done.
The concern was fuelled by recognition that the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) gains entry into cells by binding to a component of the renin-angiotensin system notably ACE2, which is ubiquitously expressed on many cells, including the lung.2 Previous studies in rodents had suggested that inhibition of the renin-angiotensin system could lead to increased cellular expression of ACE2,3 driving speculation that this might facilitate more efficient viral entry into cells and thus increase the risk of COVID-19 infection and severity of infection. The situation was further complicated by a plausible counter hypothesis, that blockade of the renin-angiotensin system might actually protect against severe outcomes from COVID-19 by upregulating ACE2, resulting in protective, anti-inflammatory effects in the lung.4 Indeed, rather than withdrawing ACEIs or ARBs, studies were being initiated to treat hospitalised patients with COVID-19 with these drugs (eg, ClinicalTrials.gov, NCT04312009). Amidst the confusion, specialist clinical organisations issued cautious but reassuring statements for their patients, urging them not to discontinue their medications, while emphasising the urgent need for more data.
The scientific response to this dilemma, as for the pandemic in general, has been remarkable, characterised by global collaboration, scale, and speed. High-quality, large-scale, case-controlled observational cohort studies reported their results within weeks, importantly demonstrating that chronic treatment with ACEIs or ARBs was not associated with increased risk of becoming infected with SARS-CoV-2, or of becoming hospitalised or dying from COVID-19.5, 6, 7 This provided much-needed reassurance to clinicians and their patients. However, it is well recognised that observational studies have important limitations and despite best efforts, they can sometimes lead to the wrong conclusions due to unmeasured confounding. This limitation of observational studies was compounded by the fact that we soon became aware that many of the risk factors for severe COVID-19 disease and death are the same factors that co-segregate with likelihood of being treated with medications that inhibit the renin-angiotensin system (eg, advanced age, hypertension, diabetes, obesity, heart failure, and chronic kidney disease).8 Thus, it was complex to address confounding by indication and its associated multimorbidity, not to mention unmeasured confounding.
The optimal solution was to confirm the messages coming from the observational studies with randomised controlled trials (RCTs). Herein lay the next major challenge, could an RCT be rapidly designed, initiated, and completed to address whether renin-angiotensin system inhibition was safe to continue, or should be discontinued, in patients hospitalised with COVID-19? Moreover, this question is not mono-dimensional because renin-angiotensin system inhibition is usually prescribed for a reason. Inhibition of the renin-angiotensin system improves the outcomes of patients with the aforementioned comorbidities and thus a decision to withdraw these treatments may not be benign.
In The Lancet Respiratory Medicine, Jordana B Cohen and colleagues9 report the first results from an RCT (the REPLACE COVID trial) examining the impact of continuing or withdrawing chronic ACEIs or ARB treatment in 152 patients hospitalised with COVID-19 across 20 international centres. To compensate for the small size of the study and to increase power for the primary outcome, they used a hierarchical global rank score comprising time to the major outcomes of interest in patients with COVID-19 (ie, ventilation, multiorgan failure or support, or death). Their study showed that outcomes for patients previously treated with ACEIs or ARBs and hospitalised for COVID-19 were similar, irrespective of whether their renin-angiotensin system inhibitor treatment was continued or discontinued during their hospital admission.
Alone, a small study like this one would not provide sufficient reassurance regarding the impact of renin-angiotensin system inhibition on the outcomes of patients hospitalised with COVID-19. Nor does it address the question about whether chronic treatment with renin-angiotensin system inhibition affects the risk of becoming infected in the first place. However, these new data, allied to the data from the aforementioned large observational case-controlled studies, does provide a consistent message: that there appears to be no justification to withdraw renin-angiotensin system inhibitor treatment in the context of COVID-19. Further reassurance comes from the fact that the conclusions of this REPLACE COVID trial are broadly consistent with the results from a previously presented, but as yet unpublished, RCT, the BRACE CORONA study (ClinicalTrials.gov, NCT04364893), which also tested continuation versus discontinuation of ACEIs or ARBs in 659 hospitalised patients with COVID-19 in Brazil. This study also found no difference in outcomes based on days alive or out of hospital 30 days after continuation or discontinuation of renin-angiotensin system inhibition.
It should be noted that both the REPLACE COVID and BRACE CORONA trials are characterised by study populations with a younger mean age (62 years and 53 years, respectively) than we typically see in the most severely ill patients with COVID-19 in many hospitals. Indeed, the impact of age and comorbidity on outcomes in COVID-19 is clearly evident from the fact that many fewer people died or had intensive care dependency in the larger but younger study population of the BRACE CORONA trial than the smaller but older study population of the REPLACE COVID trial. An important caveat for both studies is that the data most reliably apply to patients previously receiving ACEIs or ARB treatment for hypertension and associated conditions, other than for heart failure, which was an important exclusion criteria for both studies because of the higher perceived risk of withdrawing the benefits of renin-angiotensin system inhibition in patients with heart failure.
It is an extraordinary scientific achievement by the investigators, and a remarkably selfless contribution by the unwell and hospitalised patients who took part in these studies, that less than a year after we first became aware of this pandemic and the nature of the virus, we are discussing the results of RCTs that better inform our clinical practice. The irony is, that alongside these RCTs, we have also discovered that the COVID-19 RAS-inhibition controversy was most likely ill-founded in the first place, as recent data suggest that these drugs do not seem to increase ACE2 expression, especially in the lung, after all.10, 11
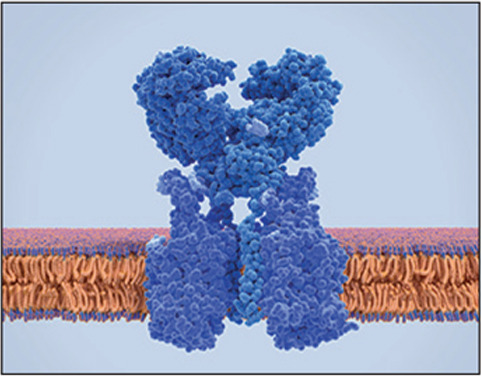
© 2021 Juan Gaertner/SPL
Acknowledgments
I have received honoraria from Pfizer, Daiichi Sankyo, Boehringer Ingelheim, Menerini, and Servier for lectures on hypertension. I am supported by the NIHR University College London Biomedical Research Centre.
References
- 1.Sommerstein R, Gräni C. Rapid response: re: preventing a COVID-19 pandemic: ACE inhibitors as a potential risk factor for fatal Covid-19. BMJ. 2020;368:m810. [Google Scholar]
- 2.Chen Y, Guo Y, Pan Y, Zhao ZJ. Structure analysis of the receptor binding of 2019-nCoV. Biochem Biophys Res Commun. 2020;525:135–140. doi: 10.1016/j.bbrc.2020.02.071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ferrario CM, Jessup J, Chappell MC, et al. Effect of angiotensin-converting enzyme inhibition and angiotensin II receptor blockers on cardiac angiotensin-converting enzyme 2. Circulation. 2005;111:2605–2610. doi: 10.1161/CIRCULATIONAHA.104.510461. [DOI] [PubMed] [Google Scholar]
- 4.Gurwitz D. Angiotensin receptor blockers as tentative SARS-CoV-2 therapeutics. Drug Dev Res. 2020;81:537–540. doi: 10.1002/ddr.21656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.de Abajo FJ, Rodríguez-Martín S, Lerma V, et al. Use of renin-angiotensin-aldosterone system inhibitors and risk of COVID-19 requiring admission to hospital: a case-population study. Lancet. 2020;395:1705–1714. doi: 10.1016/S0140-6736(20)31030-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mancia G, Rea F, Ludergnani M, Apolone G, Corrao G. Renin-angiotensin-aldosterone system blockers and the risk of Covid-19. N Engl J Med. 2020;382:2431–2440. doi: 10.1056/NEJMoa2006923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Reynolds HR, Adhikari S, Pulgarin C, et al. Renin-angiotensin-aldosterone system inhibitors and risk of Covid-19. N Engl J Med. 2020;382:2441–2448. doi: 10.1056/NEJMoa2008975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Williamson EJ, Walker AJ, Bhaskaran K, et al. Factors associated with COVID-19-related death using OpenSAFELY. Nature. 2020;584:430–436. doi: 10.1038/s41586-020-2521-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cohen JB, Hanff TC, William P, et al. Continuation versus discontinuation of renin–angiotensin system inhibitors in patients admitted to hospital with COVID-19: a prospective, randomised, open-label trial. Lancet Respir Med. 2021 doi: 10.1016/S2213-2600(20)30558-0. published online Jan 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wysocki J, Lores E, Ye M, Soler MJ, Batlle D. Kidney and lung ACE2 expression after an ACE inhibitor or an Ang II receptor blocker: implications for COVID-19. J Am Soc Nephrol. 2020;31:1941–1943. doi: 10.1681/ASN.2020050667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jiang X, Eales JM, Scannali D, et al. Hypertension and renin-angiotensin system blockers are not associated with expression of angiotensin-converting enzyme 2 (ACE2) in the kidney. Eur Heart J. 2020 doi: 10.1093/eurheartj/ehaa794. published online Oct 27. [DOI] [PMC free article] [PubMed] [Google Scholar]


