Endoscopic transoesophageal fine-needle aspiration with a convex probe bronchoscope (EUS-B-FNA) is a complementary technique to endobronchial ultrasound (EBUS)-guided transbronchial needle aspiration (TBNA) for the staging of mediastinal lymph nodes [1]. The safety and feasibility of EUS-B-FNA for sampling pulmonary parenchymal lesions and adrenal lesions has been reported [2, 3]. Recent literature also suggest a role for EUS-B-FNA in the diagnosis of infective lymphadenitis [4]. Here we present two cases of successful sampling of coeliac lymph nodes to further extend the utility of EUS-B-FNA in the assessment of patients with suspected or confirmed lung cancer. Localisation of nodes during the procedure did not involve fluoroscopy and relied upon linear EBUS guidance. Sampling was successfully performed with a 22-G TBNA needle.
Short abstract
EUS-B-FNA is a feasible and accurate technique for diagnosis of extrathoracic lesions https://bit.ly/34TFMR8
To the Editor:
Endoscopic transoesophageal fine-needle aspiration with a convex probe bronchoscope (EUS-B-FNA) is a complementary technique to endobronchial ultrasound (EBUS)-guided transbronchial needle aspiration (TBNA) for the staging of mediastinal lymph nodes [1]. The safety and feasibility of EUS-B-FNA for sampling pulmonary parenchymal lesions and adrenal lesions has been reported [2, 3]. Recent literature also suggest a role for EUS-B-FNA in the diagnosis of infective lymphadenitis [4]. Here we present two cases of successful sampling of coeliac lymph nodes to further extend the utility of EUS-B-FNA in the assessment of patients with suspected or confirmed lung cancer. Localisation of nodes during the procedure did not involve fluoroscopy and relied upon linear EBUS guidance. Sampling was successfully performed with a 22-G TBNA needle.
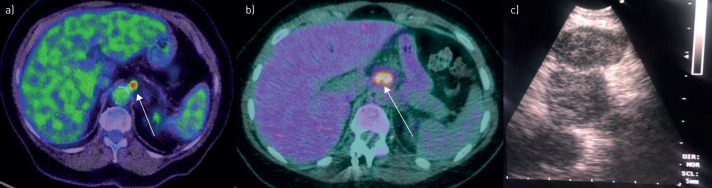
A 79-year-old female was referred for assessment after computed tomography of the chest revealed a 9 mm left upper lobe (LUL) spiculated nodule (case 1). Positron emission tomography (PET) demonstrated increased fluorodeoxyglucose (FDG) avidity in the LUL nodule, as well as in subcarinal and coeliac axis lymph nodes (figure 1a). The procedure was uncomplicated and both subcarina and coeliac axis lymph nodes confirmed adenocarcinoma.
FIGURE 1.
Positron emission tomography scan illustrating fluorodeoxyglucose-avid coeliac lymph nodes (arrows) for case a) 1 and b) 2. c) Para-aortic lymph nodes were visualised by endoscopic transoesophageal fine-needle aspiration with a convex probe bronchoscope.
An 18-year-old female with a past history of nodular sclerosing Hodgkin lymphoma (HL) underwent surveillance PET, which demonstrated mild FDG avidity in subcarina and extensive uptake in intra-abdominal lymph nodes (case 2) (figure 1b). Linear EBUS demonstrated only mildly enlarged rounded lymph nodes at the left carina, corresponding with the site of FDG avidity, and lymph nodes were visualised in the para-aortic region (figure 1c). Sampling was uncomplicated and confirmed recurrent HL.
Endoscopic ultrasound is an established and reliable method of detecting coeliac lymph node metastases [5, 6]. Our experience demonstrates the safety and feasibility of coeliac axis lymph node sampling via EUS-B-FNA, confirming the sole prior report describing EUS-B-FNA for accurate sampling of coeliac lymph nodes [7]. It also further supports the clear utility of EUS-B-FNA in extending the capacity of pulmonologists to sample suspicious lesions in patients with suspected or known malignancy. This supports the greater uptake of the procedure among interventional pulmonologists, where safe performance of EUS-B-FNA has been demonstrated [8]. These two cases further reinforce EUS-B-FNA as a feasible and accurate technique for diagnosis of extra-thoracic lesions.
Footnotes
Author contributions: M. Juneja and D.P. Steinfort wrote the manuscript. L.P. Irving reviewed the manuscript. D.P. Steinfort performed the procedure.
Conflict of interest: M. Juneja has nothing to disclose.
Conflict of interest: L.P. Irving has nothing to disclose.
Conflict of interest: D.P. Steinfort has nothing to disclose.
References
- 1.Vilmann P, Clementsen PF, Colella S, et al. Combined endobronchial and esophageal endosonography for the diagnosis and staging of lung cancer: European Society of Gastrointestinal Endoscopy (ESGE) Guideline, in cooperation with the European Respiratory Society (ERS) and the European Society of Thoracic Surgeons (ESTS). Endoscopy 2015; 47: 545–559. doi: 10.1055/s-0034-1392040 [DOI] [PubMed] [Google Scholar]
- 2.Steinfort DP, Farmer MW, Irving LB, et al. Pulmonologist-performed per-esophageal needle aspiration of parenchymal lung lesions using an EBUS bronchoscope: diagnostic utility and safety. J Bronchology Interv Pulmonol 2017; 24: 117–124. doi: 10.1097/LBR.0000000000000350 [DOI] [PubMed] [Google Scholar]
- 3.Crombag LMMJ, Szlubowski A, Stigt JA, et al. EUS-B-FNA vs conventional EUS-FNA for left adrenal gland analysis in lung cancer patients. Lung Cancer 2017; 108: 38–44. doi: 10.1016/j.lungcan.2017.02.011 [DOI] [PubMed] [Google Scholar]
- 4.Armstrong KA, Cohen JV, Shepard JO, et al. Case 16-2020: a 47-year-old woman with recurrent melanoma and pulmonary nodules. N Engl J Med 2020; 382: 2034–2043. doi: 10.1056/NEJMcpc1916258 [DOI] [PubMed] [Google Scholar]
- 5.Eloubeidi MA, Wallace MB, Reed CE, et al. The utility of EUS and EUS-guided fine needle aspiration in detecting celiac lymph node metastasis in patients with esophageal cancer: a single-center experience. Gastrointest Endosc 2001; 54: 714–719. doi: 10.1067/mge.2001.119873 [DOI] [PubMed] [Google Scholar]
- 6.Parmar KS, Zwischenberger JB, Reeves AL, et al. Clinical impact of endoscopic ultrasound-guided fine needle aspiration of celiac axis lymph nodes (M1a disease) in esophageal cancer. Ann Thorac Surg 2002; 73: 916–920. doi: 10.1016/S0003-4975(01)03560-3 [DOI] [PubMed] [Google Scholar]
- 7.Christiansen IS, Bodtger U, Naur TMH, et al. EUS-B-FNA for diagnosing liver and celiac metastases in lung cancer patients. Respiration 2019; 98: 428–433. doi: 10.1159/000501834 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Leong P, Deshpande S, Irving LB, et al. Endoscopic ultrasound fine-needle aspiration by experienced pulmonologists: a cusum analysis. Eur Respir J 2017; 50: 1–7. doi: 10.1183/13993003.01102-2017 [DOI] [PubMed] [Google Scholar]