Abstract
Background
Recent studies have examined the impact of the COVID-19 pandemic on the practice of total joint arthroplasty. A scoping review of the literature with compiled recommendations is a useful tool for arthroplasty surgeons as they resume their orthopedic practices during the pandemic.
Methods
In June 2020, PubMed, Embase (Ovid), Cochrane Library (Wiley), Scopus, LitCovid, CINAHL, medRxiv, and bioRxiv were queried for articles using controlled vocabulary and keywords pertaining to COVID-19 and total joint arthroplasty. Studies were characterized by their region of origin, design, and Center of Evidence Based Medicine level of evidence. The identified relevant studies were grouped into 6 categories: changes to future clinical workflow, education, impact on patients, impact on surgeons, technology, and surgical volume.
Results
The COVID-19 pandemic has had a significant impact on arthroplasty practice, including the disruption of the clinical teaching environment, personal and financial consequences for patients and physicians, and the drastic reduction in surgical volume. New pathways for clinical workflow have emerged, along with novel technologies with applications for both patients and trainees.
Conclusions
The COVID-19 pandemic emphasizes the recent trend in arthroplasty toward risk stratification and outpatient surgery, which may result in improved clinical outcomes and significant cost-savings. Furthermore, virtual technologies are a promising area of future focus that may ultimately improve upon previous existing inefficiencies in the education and clinical environments.
Keywords: COVID-19, Pandemic, Total joint arthroplasty
Introduction
During the pandemic caused by SARS-CoV-2 (COVID-19), the number of elective surgeries has significantly decreased around the world to control the spread of the disease, conserve personal protective equipment (PPE), and decrease strain on health-care systems [1,2]. Total joint arthroplasty has been among the surgical procedures that has seen its volume drastically reduced [1]. Projections have estimated that up to 30,000 primary and 3000 revision hip and knee arthroplasty procedures were canceled every week that restrictions for elective surgery were in place, leading to the progression of patient symptoms and significant financial losses for both hospitals and individual care providers [[3], [4], [5]].
In addition to being redeployed to the front lines of the pandemic, orthopedic surgeons have encountered significant changes to their practice, including the adoption of strict COVID-19 screening protocols, the alteration of teaching responsibilities, and the implementation of virtual health-care visits for patients [[5], [6], [7]]. Furthermore, orthopedic surgeons have documented these substantial alterations in the literature, resulting in an explosion of publications related to COVID-19 [8,9]. Recently, as the initial wave of the pandemic has slowed down and many institutions have begun to resume elective surgery, guidelines from expert panels and individual physicians have been published, offering their recommendations on how to safely and effectively resume elective orthopedic surgery [10,11]. Owing to the high volume of scientific publications related to COVID-19, Gazendam et al. highlighted the role of a review article in synthesizing the plethora of information into relevant data to guide policy and decision-making [9]. However, no study has performed a comprehensive literature review to provide future recommendations specific for arthroplasty surgeons in the COVID-19 era. Thus, the aims of the present study are to perform a scoping review of the literature to 1) summarize the high volume of information about the impact of COVID-19 on total joint arthroplasty and 2) compile recommendations for arthroplasty surgeons as they resume their orthopedic practices during the pandemic.
Material and methods
A scoping review of the literature was performed to identify articles that pertained to the effects of the COVID-19 pandemic on total joint arthroplasty. In June 2020, a library research specialist performed searches of PubMed, Embase (Ovid), Cochrane Library (Wiley), Scopus, LitCovid, CINAHL, and the pre-print servers medRxiv and bioRxiv, using both controlled vocabulary and keywords (See Supplementary Document for specific database strategies.). All references were exported to Covidence, an online tool for managing the review. Two independent reviewers screened articles for inclusion, first at the title and abstract stage and then at the full-text stage. A third reviewer resolved cases of screener conflict.
The inclusion criteria for the present review were studies pertaining to COVID-19 describing future implications and recommendations for joint arthroplasty or studies pertaining to COVID-19 describing future implications and recommendations for general orthopedics that could be applied to joint arthroplasty. Exclusion criteria were review articles that involved a literature search, non-English publications, studies with a primary focus of another orthopedic specialty, and studies with a primary focus of documenting initial changes to orthopedic practice due to COVID-19. Initial changes were excluded because of the focus of the review on providing surgeons forward-looking information as practices resume amid the pandemic.
After extraction of the relevant studies, the following data were collected: author, date of publication, journal, study design, and originating geographic region. In addition, the Center of Evidence Based Medicine Level of Evidence was determined [12]. The studies were then grouped into the following categories based on area of arthroplasty practice affected: changes to future clinical workflow, education, impact on patients, impact on surgeons, technology, and surgical volume.
Results
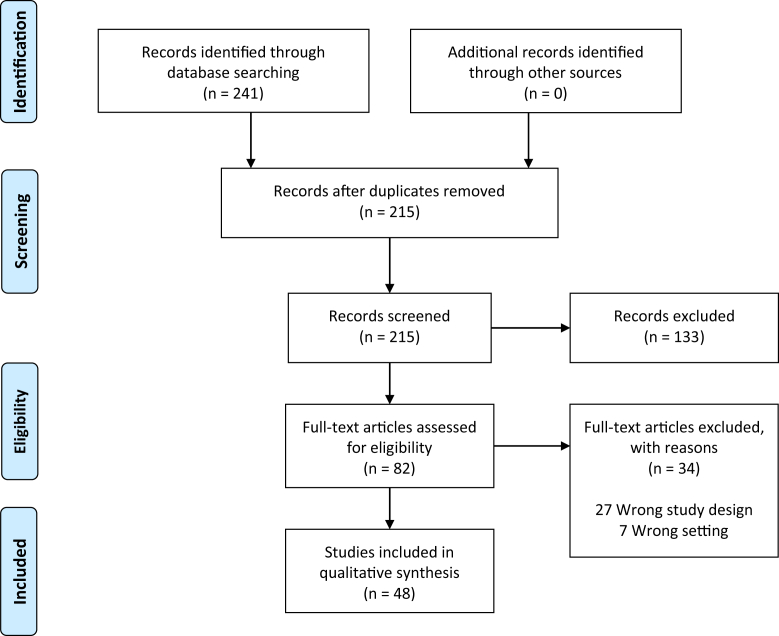
The initial search of the databases identified 241 references that were imported for screening. After the initial title/abstract screen, 78 articles were assessed for eligibility in the full-text phase. Ultimately, 48 studies met the inclusion and exclusion criteria and were included for analysis [1,[3], [4], [5], [6], [7],10,11,[13], [14], [15], [16], [17], [18], [19], [20], [21], [22], [23], [24], [25], [26], [27], [28], [29], [30], [31], [32], [33], [34], [35], [36], [37], [38], [39], [40], [41], [42], [43], [44], [45], [46], [47], [48], [49], [50], [51], [52]]. All these studies were categorized as level IV or level V evidence, representing low-quality studies (Table 1). The majority of the studies originated from the United States. A full PRISMA flow diagram is shown in Figure 1.
Table 1.
Author, date of publication, region of origin, design of the study, and CEBM level of evidence [12].
| Author | Date | Region of origin | Study design | CEBM level of evidence |
|---|---|---|---|---|
| Ambrosio et al. [6] | 27 May | Italy | Expert opinion | V |
| Askari et al. [13] | 1 May | Iran | Expert opinion | V |
| Athey et al. [14] | 24 April | Global | Cross-sectional survey | IV |
| Awad et al. [15] | 1 June | United States | Expert opinion | V |
| Bedard et al. [1] | 24 April | United States | Expert opinion | V |
| Bini et al. [16] | 22 April | United States | Expert opinion | V |
| Brown et al. [17] | 22 April | United States | Cross-sectional survey | IV |
| Chisari et al. [19] | 22 April | Global | Expert opinion | V |
| Culp et al. [20] | 24 April | United States | Cross-sectional survey | IV |
| D’Apolito et al. [21] | 24 April | Italy | Cross-sectional study | IV |
| DePhillipo et al. [22] | 13 April | United States | Expert opinion | V |
| Erickson et al. [23] | 18 April | United States | Expert opinion | V |
| Fillingham et al. [24] | 20 April | United States | Expert opinion | V |
| Gilbert et al. [25] | 21 May | United Kingdom | Cross sectional study | IV |
| Gruskay et al. [26] | 8 June | United States | Case series | IV |
| Haffer et al. [27] | 19 May | Germany | Cross sectional study | IV |
| Hinckley et al. [28] | 13 May | United States | Expert opinion | V |
| Huddleston et al. [3] | 22 April | United States | Expert opinion | V |
| Iyengar et al. [29] | 4 May | India | Expert opinion | V |
| Jacofsky et al. [30] | 20 April | United States | Expert opinion | V |
| Jain et al. [31] | 12 May | United States | Expert opinion | V |
| Jain et al. [32] | 21 April | India | Expert opinion | V |
| Khanuja et al. [33] | 24 April | United States | Expert opinion | V |
| Liang et al. [18] | 3 June | Singapore | Expert opinion | V |
| Loeb et al. [34] | 1 June | United States | Expert opinion | V |
| MacKechnie et al. [35] | 19 May | United States | Expert opinion | V |
| Makhni et al. [36] | 25 May | United States | Expert opinion | V |
| Meneghini et al. [37] | 22 April | United States | Expert opinion | V |
| Navarro et al. [38] | 11 May | United States | Expert opinion | V |
| O’Connor et al. [4] | 18 April | United States | Expert opinion | V |
| Oussedik et al. [10] | 15 May | Europe | Expert opinion | V |
| Parisien et al. [39] | 1 June | United States | Cross-sectional survey | IV |
| Parvizi et al. [11] | 14 May | Global | Expert opinion | V |
| Pelt et al. [7] | 21 April | United States | Expert opinion | V |
| Plancher et al. [40] | 27 April | United States | Expert opinion | V |
| Raghavan et al. [41] | 24 April | United Kingdom | Expert opinion | V |
| Ranuccio et al. [42] | 19 May | Italy | Cross-sectional study | IV |
| Rao et al. [43] | 23 April | United States | Expert opinion | V |
| Rizkalla et al. [44] | 22 May | United States | Expert opinion | V |
| Saxena et al. [45] | 18 April | United States | Expert opinion | V |
| Stambough et al. [46] | 18 April | United States | Expert opinion | V |
| Tanaka et al. [47] | 24 April | United States | Expert opinion | V |
| Thaler et al. [48] | 2 May | Europe | Cross-sectional survey | IV |
| Vaccaro et al. [49] | 1 June | United States | Expert opinion | V |
| Williams et al. [50] | 23 April | United Kingdom | Expert opinion | V |
| Wright et al. [51] | 1 June | United States | Expert opinion | V |
| Zagra et al. [52] | 24 May | Italy | Cross-sectional study | IV |
| Zeegen et al. [5] | 22 April | United States | Expert opinion | V |
CEBM, Center of Evidence Based Medicine [12].
Figure 1.
Mean scores on the Postoperative Discomfort Inventory for symptoms after laparoscopy and open abdominal surgery.
Changes to future clinical workflow
Twenty-five studies documented the impact of COVID-19 on future clinical or operational workflow (Table 2) [[4], [5], [6], [7],10,11,15,18,19,22,24,26,29,30,32,33,35,37,38,41,44,45,49,50]. Of these, 14 studies detailed the importance of establishment and updating of an effective COVID-19 screening protocol [5,6,10,11,18,19,22,24,26,29,32,33,37,38]. Themes of these studies included the necessity of COVID-19 reverse transcription polymerase chain reaction for all patients, the importance of history and physical for the screening of COVID-19 symptoms, the assumption that all patients will be a carrier for the virus, and the possibility for reinfection. Developed in conjunction with 77 leading international physicians, Parvizi et al. extensively documented the preoperative screening considerations of resuming elective surgery in the COVID-19 era [11]. Furthermore, Gruskay noted that a positive chest radiograph did not significantly improve the negative predictive value of symptom screening [26]. Eleven studies documented the importance of risk stratification of patients undergoing orthopedic surgery [[4], [5], [6], [7],10,11,18,22,29,44,45]. Owing to poorer surgical outcomes of patients with comorbidities, these authors noted that potential complications would result in excessive consumption of additional hospital resources postoperatively. Furthermore, they argued that the initial resumption of elective surgery should prioritize those without comorbidities.
Table 2.
Author and area of focus.
| Author | Changes to clinical workflow | Education | Patients | Surgeons | Technology | Volume |
|---|---|---|---|---|---|---|
| Ambrosio et al. [6] | Y | Y | N | Y | Y | N |
| Askari et al. [13] | N | Y | N | N | N | N |
| Athey et al. [14] | N | Y | N | Y | Y | Y |
| Awad et al. [15] | Y | N | Y | N | Y | N |
| Bedard et al. [1] | N | N | N | N | N | Y |
| Bini et al. [16] | N | Y | N | N | Y | N |
| Brown et al. [17] | N | N | Y | N | N | N |
| Chisari et al. [19] | Y | N | N | N | N | N |
| Culp et al. [20] | N | Y | N | Y | N | N |
| D’Apolito et al. [21] | N | N | N | N | N | Y |
| DePhillipo et al. [22] | Y | N | N | N | N | N |
| Erickson et al. [23] | N | N | N | Y | N | N |
| Fillingham et al. [24] | Y | N | N | Y | N | N |
| Gilbert et al. [25] | N | N | N | N | Y | N |
| Gruskay et al. [26] | Y | N | N | N | N | N |
| Haffer et al. [27] | N | N | N | Y | N | N |
| Hinckley et al. [28] | N | N | N | N | Y | N |
| Huddleston et al. [3] | N | N | Y | Y | N | N |
| Iyengar et al. [29] | Y | N | Y | N | Y | N |
| Jacofsky et al. [30] | Y | N | N | N | N | N |
| Jain et al. [31] | N | N | N | N | N | Y |
| Jain et al. [32] | Y | N | N | N | Y | N |
| Khanuja et al. [33] | Y | N | Y | Y | Y | N |
| Liang et al. [18] | Y | N | N | N | N | N |
| Loeb et al. [34] | N | N | N | N | Y | N |
| MacKechnie et al. [35] | Y | N | N | N | N | N |
| Makhni et al. [36] | N | N | N | N | Y | N |
| Meneghini et al. [37] | Y | N | N | N | N | Y |
| Navarro et al. [38] | Y | N | Y | N | Y | Y |
| O’Connor et al. [4] | Y | N | Y | Y | Y | Y |
| Oussedik et al. [10] | Y | N | Y | N | N | Y |
| Parisien et al. [39] | N | N | N | N | Y | N |
| Parvizi et al. [11] | Y | N | N | N | Y | N |
| Pelt et al. [7] | Y | Y | Y | N | Y | Y |
| Plancher et al. [40] | N | Y | N | N | N | N |
| Raghavan et al. [41] | Y | N | N | N | N | N |
| Ranuccio et al. [42] | N | N | N | N | Y | N |
| Rao et al. [43] | N | N | N | N | Y | N |
| Rizkalla et al. [44] | Y | N | N | N | N | N |
| Saxena et al. [45] | Y | N | N | N | Y | N |
| Stambough et al. [46] | N | Y | N | N | N | N |
| Tanaka et al. [47] | N | N | N | N | Y | N |
| Thaler et al. [48] | N | Y | N | Y | N | Y |
| Vaccaro et al. [49] | Y | N | N | Y | Y | N |
| Williams et al. [50] | Y | N | N | N | N | N |
| Wright et al. [51] | N | Y | N | N | N | N |
| Zagra et al. [52] | N | N | Y | N | N | Y |
| Zeegen et al. [5] | Y | Y | Y | Y | Y | Y |
Y: Yes, area discussed in individual article; N: No, area not discussed in individual article.
Thirteen studies considered intraoperative considerations during orthopedic surgery during the COVID-19 era [6,7,10,11,15,18,19,24,29,32,38,41,50]. Themes discussed included the recommendation of negative pressure operating rooms (ORs) or the presence of a high-efficiency particulate air filter if operating in a positive pressure OR, separate ORs for COVID-19–positive patients, adequate PPE and low setting power tools during aerosol-generating procedures, the utilization of regional over general anesthesia, and thorough decontamination after operation.
Eight studies discussed the importance of outpatient orthopedic surgery practice in the COVID-19 era [4,5,19,22,35,37,38,49]. Meneghini noted that outpatient elective surgery would save inpatient hospital beds for COVID-19 patients but also that this alteration would result in the challenge of doing the more complex surgeries with increased blood loss in an outpatient setting with potential limitations including inexperienced staff, insufficient physical space, and inadequate central sterile processing capacity [37]. Furthermore, O’Connor et al. noted that the hours of outpatient surgery would need to be extended to keep up with the backlog in surgical cases and that those necessitating traditional inpatient surgery should be shifted to rapid recovery protocols [4]. Finally, MacKechnie et al. described their experience in implementing an outpatient orthopedic walk-in clinic, which was able to significantly reduce nonemergent musculoskeletal emergency department referral by 40% [35].
Education
In total, 11 studies addressed the effect of COVID-19 on the education of orthopedic surgery residents and fellows (Table 2) [[5], [6], [7],13,14,16,20,40,46,48,51]. Three studies provided quantitative data on the significant disruption of learning for orthopedic surgery trainees [14,20,48]. In 2 cross-sectional surveys, Athey et al. and Thaler et al. determined that 44% and 52.2% of surgeons, respectively, reported a disruption in the teaching of students, residents, and fellows [14,48]. However, Culp and Frisch noted that 14 out of 15 arthroplasty fellows surveyed felt ready for their career as an attending [20]. Culp and Frisch further note that education of trainees has been enhanced through webinars and other technologies but also that trainees may ultimately require a “mini-fellowship” if they still feel unprepared for practice [20].
Seven studies commented on the current and future use of virtual learning in orthopedic and arthroplasty education [[5], [6], [7],13,16,40,46]. Recommendations included the importance of virtual teaching for residents in formats such as online conferences, case presentations, webinars, journal clubs, and readings. Furthermore, 4 studies documented the potential for technological applications in surgical simulation training, through cadavers, virtual and augmented reality technology platforms, and arthroscopic simulators [6,16,40,46]. Furthermore, 2 studies suggested that future national and international meetings take place partly in a virtual format [40,46]. Stambough et al. suggested that these virtual meetings would result in a lower overall cost, improve the ability to attend poster sessions that were scheduled at similar times, and improve networking among different institutions [46].
Four studies described the responses or changes from accrediting bodies, including the American Board of Orthopedic Surgery (ABOS) and the Accreditation Council for Graduate Medical Education [5,6,20,46,51]. Wright et al. documented the changes and strategies of the ABOS in adapting to the pandemic [51]. They noted potential changes to ABOS residency requirements, the ABOS Part I Written Examination, the ABOS Part II Oral Examination, and ABOS Continuing Certification. In a cross-sectional survey of 81 young arthroplasty surgeons, Culp and Frisch noted that 84% of physicians felt capable of completing the ABOS Part II examination given the climate, while the other 16% felt like they might require a delay due to the lack of completed cases [20]. Stambough et al. commented on the Accreditation Council for Graduate Medical Education response, which describes the reorganization of residents based on the severity of the pandemic in their respective geographic region [46]. They, along with Zeegan et al., argued for residency programs to adopt an altered curriculum, such as virtual learning, in accordance with these guidelines [5].
Impact on patients
Six studies noted the adverse economic effects of the COVID-19 pandemic, which could lead to significant financial consequences and gaps in insurance coverage for patients [[3], [4], [5],29,33,38]. In turn, this would potentially hinder or delay arthroplasty patients from receiving timely surgical care. O’Connor et al. noted that issues with insurance coverage may preferentially affect younger patients [4]. Furthermore, Zeegan et al. speculated that the COVID-19 pandemic could bring about a widening disparity of care for poorer patients, as hospitals may prioritize patients with straightforward cases and favorable insurance plans [5]. Huddleston et al. noted that the American Association of Hip and Knee Surgeons (AAHKS) was encouraging lawmakers to close insurance coverage gaps for patients that were receiving treatment for COVID-19 [3]. Finally, Iyengar et al. advised orthopedic surgeons and hospital administrators in India to consider the increased costs of surgery in the COVID-19 era, such as due to the additional hospital costs of PPE and extra COVID-19 testing [29]. They imply that these added hospital costs could potentially be transferred to patients [29].
Two studies directly compared the outcomes of patients undergoing orthopedic surgery during the pandemic to the same time period in the previous year [10,52]. Both studies noted a higher rate of postoperative deaths this year in the same 7- or 8-week period in March and April than last year, and both noted that the majority or all of the deaths were COVID-19 related.
Three studies commented on the psychological distress that patients are facing due to the COVID-19 pandemic and the cancellation of their scheduled surgeries [7,15,17]. In a cross-sectional survey among 360 arthroplasty patients, Brown et al. determined that the greatest anxiety of patients was not knowing when their elective joint arthroplasty would be scheduled [17]. In addition, 54% of patients noted that their arthritis symptoms have worsened since the pandemic [17]. Ultimately, Awad et al. called upon orthopedic surgeons to be aware of these psychological stressors and to support their patients during these times [15].
Impact on surgeons
Twelve studies detailed the effects of COVID-19 pandemic on personal implications for orthopedic and arthroplasty surgeons (Table 2) [[3], [4], [5], [6],14,20,23,24,27,33,48,49]. Four studies documented significant financial and career consequences for arthroplasty surgeons [14,20,27,49]. Athey et al. noted that 44% of surveyed surgeons had to forego salary because of COVID-19, and respondents estimated that their practices could only handle the economic strain for an average of 8 weeks [14]. Similarly, Culp and Frisch noted that 52 out of 103 young arthroplasty surgeons had decreased compensation because of the pandemic [20]. In addition, they noted that 2 of the 6 residents with job offers in arthroplasty had their offers rescinded, and of the 10 young attendings wishing to relocate before the crisis, 3 were now unable to do so [20]. In Germany, Haffer et al. noted that as of early April, the average financial loss among 52 orthopedic surgeons was already 29.3%, and directors determined that not meeting financial projections would have financial and personnel consequences for surgeons and staff [27].
Four studies discussed the response of the United States government in providing monetary aid for orthopedic surgeons [[3], [4], [5],49]. Specifically, these studies discussed the passage of the Coronavirus Aid, Relief, and Economic Security Act Act, which provides $100 billion for hospitals and $350 billion for small business, including private orthopedic practices. All these authors agreed that these loans would be instrumental for orthopedic practices under 500 people and may offset loss of revenue and allow for the retention of the workforce during the pandemic. In addition, Huddleston et al. documented the efforts of the AAHKS in advocating for the economic interests of arthroplasty surgeons [3]. In addition to obtaining COVID-19 relief, Huddleston et al. noted that the AAHKS’s usual advocacy efforts, including negotiating against reductions in Medicare and Medicaid reimbursement for hip and knee arthroplasty, continued during the pandemic [3].
Three studies documented the personal effect that the COVID-19 pandemic had on the lives of orthopedic surgeons [6,24,48]. Two studies detailed the extra precautions and difficulty that surgeons faced when encountering their families at home [24,48]. Specifically, Thaler et al. noted that 22.6% of surgeons avoided physical contact with their families, and 21.7% performed thorough disinfection of their homes [48]. Furthermore, Ambrosio et al. observed that the death of providers and the reassignment and deployment of orthopedic surgeons have led to significant burnout [6].
Outside of the redeployment of orthopedic surgeons, 2 studies commented on the humanitarian efforts of arthroplasty surgeons during the pandemic [23,33]. Khanuja et al. documented the commitment of the AAHKS in developing resources for humanitarian work [33]. Similar to Erickson et al., who highlight the modification of arthroplasty helmets to PPE, Khanuja et al. emphasized the role of surgeons in making and donating PPE and commended the individual or group work that arthroplasty physicians have performed during the pandemic [23].
Technology
Twenty-two articles addressed the current and future use of technology in providing care for orthopedic patients (Table 2) [[4], [5], [6], [7],11,[14], [15], [16],25,28,29,[32], [33], [34],36,38,39,42,43,45,47,49]. Two studies reported cross-sectional data on the usage of telemedicine, noting that the vast majority of providers had adopted the technology, but that there were differences in adoption by country and associations of adoption with the presence of a COVID-19 hotspot location [14,39]. Five studies addressed their institution’s experience with the establishment of telehealth during the COVID-19 pandemic [6,7,25,34,38,49]. Gilbert et al. noted that satisfaction in using telehealth for both physicians and patients was high but ultimately determined that telehealth would be preferred less than 50% of the time outside the pandemic [25]. In their institution, Loeb et al. described the workflow for their telehealth practice and emphasized the importance of initially determining the suitability of patients for telehealth and the establishment of functioning technology in compliance with local regulations [34]. Ultimately, they determined that they were able to successfully see 25% of their normal clinic volume within a week of implementation with telehealth [34].
Twelve studies commented on the clinical applications of telehealth, with all agreeing that telemedicine has a role in the postoperative follow-up and/or rehabilitation of orthopedic surgery patients [[4], [5], [6], [7],11,15,16,29,32,42,45,47]. O’Connor et al. noted that virtual postoperative visits could improve time efficiency for both patients and providers, especially for patients undergoing total joint arthroplasty [4]. Furthermore, Bini et al. determined that virtual physical therapy had significant cost savings but similar functional outcomes as traditional in person physical therapy [16]. In addition to postoperative visits and rehabilitation, Bini et al. described potential future applications of technology and innovation in orthopedics, including virtual scribes, chatbots to triage patients, wearable sensor devices for postoperative patient monitoring, surgical scheduling applications, patient engagement platforms, and 3D printing technologies [16]. Finally, Tanaka et al. detailed how to perform a thorough hip and knee examination over a video platform [47].
Four studies described the future considerations that practices would need to consider to effectively implement telehealth during and after the COVID-19 pandemic [28,33,36,43]. Makhni et al. noted that in the United States, the government allows for virtual care in states in which providers do not hold licenses, telemedicine coverage expansion for Medicare patients, improved provider reimbursement between in-person and telemedicine visits, and the permissibility of telemedicine across non–HIPAA-secure platforms [36]. However, these governmental regulations are set to expire once the pandemic ends [36]. In addition, Rao et al. described general recommendations to allow for the adoption of telemedicine outside the pandemic, including the optimization of federal and state rules regarding physician licensing requirements for telemedicine, the harmonization of reimbursement policies, and the education of patients and physicians about the use and benefits of telemedicine [43].
Surgical volume
In total, 12 studies addressed the effect of COVID-19 on orthopedic and arthroplasty surgical volume (Table 2) [1,4,5,7,10,21,31,37,38,48,52]. Of these, 6 studies addressed the specific number of cases that were canceled or projected to be canceled because of COVID-19 [1,7,14,21,48,52]. Two studies, in comparing their hospital’s orthopedic surgical volume from 2020 to the same time period in 2019, noted a 70% reduction in surgical volume [21,52]. Two studies used a cross-sectional survey among their arthroplasty societies to determine the significant reduction in volume of cases caused by COVID-19 [14,48]. Furthermore, Pelt et al. noted that as of early April 1450, elective arthroplasty cases would need to be rescheduled across 2 hospitals in the United States [7]. Finally, Bedard et al. projected the number of canceled elective arthroplasty procedures in the United States, assuming 25%, 50%, 75%, and 100% cancellation [1]. They noted that with a 25% cancellation of nonessential joint arthroplasties, this would equate to a cancellation of 7501 primary and 717 revision joint arthroplasties. However, with a 100% cancelation, this number would rise to 30,002 canceled primary joint arthroplasties and 2870 canceled revision joint arthroplasties (Table 3) [1].
Table 3.
Key studies describing surgical volume and strategies to aid recovery.
| Author | Results | Conclusions |
|---|---|---|
| Bedard et al. [1] | Projected canceled primary and revision arthroplasty procedures per month:
|
|
| O’Connor et al. [4] | Six economic pillars are crucial or the resumption of elective total joint arthroplasty
|
|
| Jain et al. [31] | Using a Monte-Carlo simulation-based analysis, the time it will take for the healthcare system to perform 90% of pre-pandemic forecasted volume of surgery:
|
|
Six studies commented on forecasted surgical volume after the resumption of elective surgery [4,5,10,31,37,38]. Three studies agreed that there would be a significant pressure to ramp up surgical volume, leading to an increased volume due to a period of decreased activity [5,10,37]. Navarro et al. noted that not all the lost surgical volume would be recovered [38]. O’Connor et al. argued for the projection of joint arthroplasty demand 3-6 months in advance to better prepare hospital systems (Table 3) [4]. Finally, Jain et al. used a simulation model to project the number of months required to achieve a 90% prepandemic volume of surgery [31]. They noted that 7 months would be required to achieve this volume in their optimistic scenario, 12 months would be required in their ambivalent scenario, and 16 months would be required in their pessimistic scenario. Even with their optimistic scenario, they projected that over 1 million orthopedic surgery cases would be backlogged at 2 years in the United States (Table 3) [31]. In order to combat this backlog, O’Connor et al. and Jain et al. argue for the use of strategies including increased OR schedules and the increased utilization of outpatient and ambulatory surgical centers [4,31].
Discussion
The COVID-19 pandemic has resulted in significant changes to total joint arthroplasty practice. As a result, orthopedic surgeons from around the world have documented these changes in the literature, through the sharing of their personal experience, cross-sectional studies, and expert guidelines. However, no study has compiled these findings into a comprehensive review of the literature as it pertains to joint arthroplasty. Thus, the present study provides a thorough, scoping literature review and compiles these disparate recommendations into the following 6 categories: changes to future clinical workflow, education, impact on patients, impact on surgeons, technology, and surgical volume.
Notably, the results of the present study demonstrate that the COVID-19 pandemic highlights previous trends in arthroplasty, including patient risk stratification and the importance of outpatient surgery. In the arthroplasty literature, there has been an emphasis on the risk stratification of patients, as it may limit potential complications and allow for the appropriate allocation of perioperative resources [53]. Further, before the pandemic, there has been a recent trend toward outpatient arthroplasty due to the favorable outcomes and cost savings metrics. In an analysis of over 100,000 patients undergoing total joint arthroplasty, Courtney et al. showed that the rate of complications was lower in outpatients (8%) than inpatients (16%) [54]. In addition, in patients undergoing both total hip and knee arthroplasties, outpatient procedures result in a significantly lower cost than inpatient procedures [55,56]. As health-care costs rise in the United States, there is thus an emerging focus of health-care reform that emphasizes the importance of minimizing cost while also improving the value of care [57]. In summary, the COVID-19 pandemic highlights the need of risk stratification and outpatient surgery to minimize complications and length of stay.
Virtual technology has emerged from the pandemic as a promising tool with a place in orthopedic education. While there is no substitute for in-person clinical training, alternative technologies such as the increasing utilization of cadavers, virtual and augmented reality technology platforms, and arthroscopic simulators hold promise in augmenting surgical training in the future [6,16,40]. Furthermore, while current national and international conferences are often hindered by the conference hall location, the timing of presentation, and the individual cost for participants, virtual meetings may facilitate learning, networking, and decrease the cost of participation [40,46].
In addition, these virtual technologies have significant implications for patient care and may have a role in arthroplasty practice after the pandemic. Notably, the COVID-19 pandemic has challenged providers to rapidly adopt and implement telehealth practices when previously, they may not have had the same urgency [25,34,39]. In their department, Loeb et al. highlighted that only one out of thirty-six physicians was trained to use video technologies before the pandemic but that they were able to see successfully 25% of normal clinic volume within 1 week of implementation [34]. Furthermore, Parisien et al. determined that 63% of orthopedic residency programs in the United States are now currently using telehealth in their practices, and for the majority, the primary reason for this adoption was COVID-19 [39]. This experience with telehealth, initially driven by necessity, will be instrumental in the future as administrative and technical issues will have been sorted out. Furthermore, Bini et al. noted that the infrastructure for telehealth is largely in place and that significant investments have already been made into the sector [16]. Previous studies have indicated that telemedicine can provide comparable quality as in-person visits, but significant cost-savings [36,58]. In a randomized control trial before the pandemic, Bettger et al. noted that a virtual physical therapy program after total knee arthroplasty decreased 3-month associated health-care–related costs and provided comparable clinical outcomes with traditional in-person physical therapy [58]. Furthermore, many postoperative visits for patients who underwent total joint arthroplasty can be performed virtually, leading to potential cost and time savings for patients and providers [36].
There are several limitations to the present study. First, the COVID-19 pandemic is ongoing and subject to rapid changes. While this review captured the literature in early June 2020, guidelines and management are certainly evolving, and published articles after this date were notably excluded. However, the majority of the included articles for this present study were from April 2020, and as the initial wave of the pandemic has subsided, it is likely that this review has captured the most important guidelines and recommendations. Of course, there is much to be learned as the pandemic continues, including the backlog of cases and the exacerbation of health-care disparities, which our review could not possibly capture at the time of writing. Then, the articles included originated from different geographic regions with different burden and impact of COVID-19 at the time of their publication. Thus, while the present study noted the date of publication and the country of origin, the recommendations of the individual authors may not be applicable to all regions given the varying burden and impact of COVID-19. The present study represents a compilation of studies designated as low-quality evidence, highlighting the lack of higher quality data from the pandemic. Despite these limitations, the present study offers a comprehensive scoping review of the literature with a rigorous and reproducible methodology and provides an effective map of the available literature.
To conclude, the COVID-19 has had tremendous clinical and economic consequences for joint arthroplasty. However, the pandemic highlights important principles of risk stratification and the shift toward more outpatient surgery, which could ultimately lead to improved care and cost savings in the future. Furthermore, the innovation of virtual technologies and the application of new technologies to education and clinical care may potentially improve upon existing inefficiencies in the previous system. Thus, despite the setback caused by the pandemic, there is great optimism for the future of total joint arthroplasty.
The manuscript submitted does not contain information about medical device(s)/drug(s). Relevant financial activities outside the submitted work: none.
Conflicts of interest
Declaration of interests
E. P. Su received royalties from Kyocera corporation, OrthAlign, and United Orthopedic Corporation; is a paid consultant for Smith & Nephew and United Orthopedic Corporation; has stock or stock options in Engage Uni and Insight Medical Systems, Inc; received research support from Smith & Nephew and United Orthopedic Corporation; received other financial and material support from Engage Uni (designer, inventor, founder) and Kyocera Corporation (designer and royalties); published Techniques in Orthopaedics (Wolters Kluwer).
For full disclosure statements refer to https://doi.org/10.1016/j.artd.2020.12.028.
Appendix
Supplemental Table 1.
Database search strategies.
| Database | Date of Search | Search Run |
|---|---|---|
| PubMed | June 2, 2020 | (("COVID-19"[tw] OR "COVID19"[tw] OR COVID-19[nm] OR "2019-nCoV"[tw] OR "2019nCoV"[tw] OR "HCoV-19"[tw] OR "HCoV19"[tw] OR "SARS-CoV-2"[tw] OR "SARS-CoV2"[tw] OR "coronavirus"[tw] OR "corona virus"[tw] OR "2019 ncos"[tw] OR "severe acute respiratory syndrome coronavirus 2"[nm] OR "nCov 2019"[tw])) AND (((((((("Orthopedics"[Mesh]) OR "Orthopedic Procedures"[Mesh]) OR "Orthopedic Surgeons"[Mesh])) OR ((hip replac∗[Text Word] OR hip repair∗[Text Word] OR hip reconstruct∗[Text Word]))) OR (((knee replac∗[Text Word] OR knee repair∗[Text Word] OR knee reconstruct∗[Text Word])))) OR ((((joint replac∗[Text Word] OR joint repair∗[Text Word] OR joint reconstruct∗[Text Word]))))) OR ((arthroplast∗[Text Word] OR orthopedic∗[Text Word] OR orthopedic∗[Text Word]))) |
| LitCovid | June 3, 2020 | Separate keyword searches using the following terms: arthroplasty, orthopedics, orthopedics, hip/knee/joint replacement/reconstruction/repair |
| Ovid Embase | June 3, 2020 | 1. ("COVID-19" or "COVID19" or "2019-nCoV" or "2019nCoV" or "HCoV-19" or "HCoV19" or "SARS-CoV-2" or "SARS-CoV2" or "novel coronavirus" or "novel corona virus" or "2019 ncos" or "Severe Acute Respiratory Syndrome Coronavirus 2" or "severe acute respiratory syndrome coronavirus 2" or "corona virus disease 2019" or "coronavirus disease 2019" or "new corona virus" or "new coronavirus" or "nCov 2019" or "SARS Coronavirus 2" or "SARS Corona virus 2").tw. 2. exp orthopedic surgery/ 3. orthopedics/ 4. orthopedic surgeon/ 5. or/2-4 6. ((hip or knee or joint) adj2 (replac∗ or reconstruct∗ or repair∗)).tw. 7. (arthroplast∗ or orthopedic∗ or orthopedic∗).tw. 8. or/6-7 9. 5 or 8 10. 1 and 9 |
| Scopus | June 3, 2020 | ( TITLE-ABS-KEY ( "COVID-19" OR "COVID19" OR covid-19or "2019-nCoV" OR "2019nCoV" OR "HCoV-19" OR "HCoV19" OR "SARS-CoV-2" OR "SARS-CoV2" OR "coronavirus" OR "corona virus" OR "2019 ncos" OR "severe acute respiratory syndrome coronavirus 2" OR "nCov 2019" ) ) AND ( ( TITLE-ABS-KEY ( ( hip OR knee OR joint ) W/2 ( repair∗ OR reconstruct∗ OR replac∗ ) ) ) OR ( TITLE-ABS-KEY ( arthroplast∗ OR orthopedic∗ OR orthopedic∗ ) ) ) |
| Cochrane Library (Wiley) | June 6, 2020 | ID Search Hits #1 "COVID-19" or "2019-nCoV" or "SARS-CoV∗" or "SARSCOV2":ti,ab,kw #2 "2019-nCov" or "2019 coronavirus∗" or "2019 corona virus∗" or "covid19" or "ncov∗":ti,ab,kw #3 "COVID19" or "2019nCoV" or "HCoV-19" or "HCoV19" or "SARS-CoV-2" or "coronavirus" or "corona virus" or "2019 ncos" or "severe acute respiratory syndrome coronavirus 2" or "nCov 2019":ti,ab,kw #4 MeSH descriptor: [Orthopedic Surgeons] this term only #5 MeSH descriptor: [Orthopedics] this term only #6 MeSH descriptor: [Orthopedic Procedures] explode all trees #7 (hip or knee or joint) NEAR/2 (repair∗ or replac∗ or reconstruct∗):ti,ab,kw #8 arthroplast∗ or orthopedic∗ or orthopedic∗:ti,ab,kw #9 #1 or #2 or #3 #10 #4 or #5 or #6 or #7 or #8 #11 #9 and #10 |
| CINAHL (EBSCOhost) | June 6, 2020 | S11 S9 AND S10 S10 TX "COVID-19" OR "COVID19" OR COVID-19OR "2019-nCoV" OR "2019nCoV" OR "HCoV-19" OR "HCoV19" OR "SARS-CoV-2" OR "SARS-CoV2" OR "coronavirus" OR "corona virus" OR "2019 ncos" OR "severe acute respiratory syndrome coronavirus 2" OR "nCov 2019" S9 S3 OR S8 S8 S4 OR S5 OR S6 OR S7 S7 TX "joint replacement" OR "joint reconstruction" OR "joint repair" S6 TX "knee replacement" OR "knee reconstruction" OR "knee repair" S5 TX "hip replacement" OR "hip reconstruction" OR "hip repair" S4 TX arthroplast∗ OR orthopedic∗ OR orthopedics S3 S1 OR S2 S2 (MH "Orthopedics") S1 (MH "Orthopedic Surgery+") |
| medRxiv & bioRxiv | June 6, 2020 | Separate keyword searches combining the following 2 sets of terms: 1) arthroplasty, orthopedics, orthopedics, hip/knee/joint replacement/reconstruction/repair and 2) COVID-19, COVID19, 2019-nCoV, 2019nCoV, HCoV-19, HCoV19, SARS-CoV-2, SARS-CoV2, coronavirus, corona virus, 2019 ncos, severe acute respiratory syndrome coronavirus 2, nCov 2019 |
Supplementary data
References
- 1.Bedard N.A., Elkins J.M., Brown T.S. Effect of COVID-19 on hip and knee arthroplasty surgical volume in the United States. J Arthroplasty. 2020;35:S45. doi: 10.1016/j.arth.2020.04.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Diaz A., Sarac B.A., Schoenbrunner A.R., Janis J.E., Pawlik T.M. Elective surgery in the time of COVID-19. Am J Surg. 2020;219(6):900. doi: 10.1016/j.amjsurg.2020.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Huddleston J.I., 3rd, Iorio R., Bosco J.A., 3rd, Kerr J.M., Bolognesi M.P., Barnes C.L. American Association of hip and knee surgeons advocacy efforts in response to the SARS-CoV-2 pandemic. J Arthroplasty. 2020;35:S82. doi: 10.1016/j.arth.2020.04.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.O'Connor C.M., Anoushiravani A.A., DiCaprio M.R., Healy W.L., Iorio R. Economic recovery after the COVID-19 pandemic: resuming elective orthopedic surgery and total joint arthroplasty. J Arthroplasty. 2020;35:S32. doi: 10.1016/j.arth.2020.04.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zeegen E.N., Yates A.J., Jevsevar D.S. After the COVID-19 pandemic: returning to normalcy or returning to a new normal? J Arthroplasty. 2020;35:S37. doi: 10.1016/j.arth.2020.04.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ambrosio L., Vadala G., Russo F., Papalia R., Denaro V. The role of the orthopaedic surgeon in the COVID-19 era: cautions and perspectives. J Exp Orthop. 2020;7(1):35. doi: 10.1186/s40634-020-00255-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pelt C.E., Campbell K.L., Gililland J.M. The rapid response to the COVID-19 pandemic by the arthroplasty divisions at two academic referral centers. J Arthroplasty. 2020;35:S10. doi: 10.1016/j.arth.2020.04.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kambhampati S.B.S., Vaishya R., Vaish A. Unprecedented surge in publications related to COVID-19 in the first three months of pandemic: a bibliometric analytic report. J Clin Orthop Trauma. 2020;11:S304. doi: 10.1016/j.jcot.2020.04.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gazendam A., Ekhtiari S., Wong E. The “infodemic” of journal publication associated with the novel Coronavirus disease. J Bone Joint Surg Am. 2020;102:e64. doi: 10.2106/JBJS.20.00610. [DOI] [PubMed] [Google Scholar]
- 10.Oussedik S., Zagra L., Shin G.Y., D'Apolito R., Haddad F.S. Reinstating elective orthopaedic surgery in the age of COVID-19. Bone Joint J. 2020;102-B:807. doi: 10.1302/0301-620X.102B7.BJJ-2020-0808. [DOI] [PubMed] [Google Scholar]
- 11.Parvizi J., Gehrke T., Krueger C.A. Resuming elective orthopaedic surgery during the COVID-19 pandemic: guidelines developed by the international consensus group (ICM) J Bone Joint Surg Am. 2020;102:1205. doi: 10.2106/JBJS.20.00844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Oxford Centre for Evidence-Based Medicine: Levels of evidence. Oxford University; 2009. [Google Scholar]
- 13.Askari A., Arasteh P., Jabalameli M., Bagherifard A., Razi M. COVID-19 and orthopaedic surgery: experiences from Iran. J Bone Joint Surg Am. 2020;102:1126. doi: 10.2106/JBJS.20.00631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Athey A.G., Cao L., Okazaki K. Survey of AAHKS international members on the impact of COVID-19 on hip and knee arthroplasty practices. J Arthroplasty. 2020;35:S89. doi: 10.1016/j.arth.2020.04.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Awad M.E., Rumley J.C.L., Vazquez J.A., Devine J.G. Perioperative considerations in urgent surgical care of suspected and confirmed COVID-19 orthopaedic patients: operating room protocols and recommendations in the current COVID-19 pandemic. J Am Acad Orthop Surg. 2020;28(11):451. doi: 10.5435/JAAOS-D-20-00227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bini S.A., Schilling P.L., Patel S.P. Digital orthopaedics: a glimpse into the future in the midst of a pandemic. J Arthroplasty. 2020;35:S68. doi: 10.1016/j.arth.2020.04.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Brown T.S., Bedard N.A., Rojas E.O. The effect of the COVID-19 pandemic on electively scheduled hip and knee arthroplasty patients in the United States. J Arthroplasty. 2020;35:S49. doi: 10.1016/j.arth.2020.04.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chang Liang Z., Ye Chong M.S., Sim M.A. Surgical considerations in patients with COVID-19: what orthopaedic surgeons should know. J Bone Joint Surg Am. 2020;102:e50. doi: 10.2106/JBJS.20.00513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chisari E., Krueger C.A., Barnes C.L., Van Onsem S., Walter W.L., Parvizi J. Prevention of infection and disruption of the pathogen transfer chain in elective surgery. J Arthroplasty. 2020;35:S28. doi: 10.1016/j.arth.2020.04.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Culp B.M., Frisch N.B. COVID-19 impact on young arthroplasty surgeons. J Arthroplasty. 2020;35:S42. doi: 10.1016/j.arth.2020.04.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.D'Apolito R., Faraldi M., Ottaiano I., Zagra L. Disruption of arthroplasty practice in an orthopedic center in Northern Italy during the Coronavirus disease 2019 pandemic. J Arthroplasty. 2020;35:S6. doi: 10.1016/j.arth.2020.04.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.DePhillipo N.N., Larson C.M., O'Neill O.R., LaPrade R.F. Guidelines for ambulatory surgery centers for the care of surgically necessary/time-sensitive orthopaedic cases during the COVID-19 pandemic. J Bone Joint Surg Am. 2020;102:933. doi: 10.2106/JBJS.20.00489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Erickson M.M., Richardson E.S., Hernandez N.M., Bobbert D.W., 2nd, Gall K., Fearis P. Helmet modification to PPE with 3D printing during the COVID-19 pandemic at Duke University Medical Center: a novel technique. J Arthroplasty. 2020;35:S23. doi: 10.1016/j.arth.2020.04.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fillingham Y.A., Grosso M.J., Yates A.J., Austin M.S. Personal protective equipment: current best practices for orthopedic teams. J Arthroplasty. 2020;35:S19. doi: 10.1016/j.arth.2020.04.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gilbert A.W., Billany J.C.T., Adam R. Rapid implementation of virtual clinics due to COVID-19: report and early evaluation of a quality improvement initiative. BMJ Open Qual. 2020;9(2):e000985. doi: 10.1136/bmjoq-2020-000985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gruskay J.A. Universal testing for COVID-19 in essential orthopaedic surgery reveals a high percentage of asymptomatic infections. J Bone Joint Surg Am. 2020;102:1379. doi: 10.2106/JBJS.20.01053. [DOI] [PubMed] [Google Scholar]
- 27.Haffer H., Schomig F., Rickert M. Impact of the COVID-19 pandemic on orthopaedic and trauma surgery in University Hospitals in Germany: results of a nationwide survey. J Bone Joint Surg Am. 2020;102:e78. doi: 10.2106/JBJS.20.00756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hinckley N.B., Henley M.B., McIntyre L., Stiefel E., Davidson J., Chhabra A. Orthopaedic documentation and coding primer for telemedicine and electronic patient communication for the COVID-19 pandemic. J Bone Joint Surg Am. 2020;102:1105. doi: 10.2106/JBJS.20.00649. [DOI] [PubMed] [Google Scholar]
- 29.Iyengar K.P., Jain V.K., Vaish A., Vaishya R., Maini L., Lal H. Post COVID-19: planning strategies to resume orthopaedic surgery -challenges and considerations. J Clin Orthop Trauma. 2020;11:S291. doi: 10.1016/j.jcot.2020.04.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jacofsky D., Jacofsky E.M., Jacofsky M. Understanding antibody testing for COVID-19. J Arthroplasty. 2020;35:S74. doi: 10.1016/j.arth.2020.04.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jain A., Jain P., Aggarwal S. SARS-CoV-2 impact on elective orthopaedic surgery: implications for post-pandemic recovery. J Bone Joint Surg Am. 2020;102:e68. doi: 10.2106/JBJS.20.00602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jain V.K., Vaishya R. COVID-19 and orthopaedic surgeons: the Indian scenario. Trop Doct. 2020;50(2):108. doi: 10.1177/0049475520921616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Khanuja H.S., Chaudhry Y.P., Sheth N.P., Oni J.K., Parsley B.S., Morrison J.C. Humanitarian needs: the arthroplasty community and the COVID-19 pandemic. J Arthroplasty. 2020;35:S85. doi: 10.1016/j.arth.2020.04.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Loeb A.E., Rao S.S., Ficke J.R., Morris C.D., Riley L.H., 3rd, Levin A.S. Departmental experience and lessons learned with accelerated introduction of telemedicine during the COVID-19 crisis. J Am Acad Orthop Surg. 2020;28(11):e469. doi: 10.5435/JAAOS-D-20-00380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.MacKechnie M.C., Nadeau M., Deering E., Thaller J., MacKechnie M.A. Orthopaedic walk-in clinics: a model to lessen the burden on emergency departments during the COVID-19 pandemic. J Orthop. 2020;20:293. doi: 10.1016/j.jor.2020.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Makhni M.C., Riew G.J., Sumathipala M.G. Telemedicine in orthopaedic surgery: challenges and opportunities. J Bone Joint Surg Am. 2020;102:1109. doi: 10.2106/JBJS.20.00452. [DOI] [PubMed] [Google Scholar]
- 37.Meneghini R.M. Resource reallocation during the COVID-19 pandemic in a suburban hospital system: implications for outpatient hip and knee arthroplasty. J Arthroplasty. 2020;35:S15. doi: 10.1016/j.arth.2020.04.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Navarro R.A., Reddy N.C., Weiss J.M. Orthopaedic systems response to and return from the COVID-19 pandemic: lessons for future crisis management. J Bone Joint Surg Am. 2020;102:e75. doi: 10.2106/JBJS.20.00709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Parisien R.L., Shin M., Constant M. Telehealth utilization in response to the novel Coronavirus (COVID-19) pandemic in orthopaedic surgery. J Am Acad Orthop Surg. 2020;28(11):e487. doi: 10.5435/JAAOS-D-20-00339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Plancher K.D., Shanmugam J.P., Petterson S.C. The changing face of orthopedic education: searching for the new reality after COVID-19. Arthrosc Sports Med Rehabil. 2020;2:e295. doi: 10.1016/j.asmr.2020.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Raghavan R., Middleton P.R., Mehdi A. Minimising aerosol generation during orthopaedic surgical procedures- Current practice to protect theatre staff during COVID-19 pandemic. J Clin Orthop Trauma. 2020;11(3):506. doi: 10.1016/j.jcot.2020.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ranuccio F., Tarducci L., Familiari F., Mastroianni V., Giuzio E. Disruptive effect of COVID-19 on orthopaedic daily practice: a cross-sectional survey. J Bone Joint Surg Am. 2020;102:e77. doi: 10.2106/JBJS.20.00604. [DOI] [PubMed] [Google Scholar]
- 43.Rao S.S., Loeb A.E., Amin R.M., Golladay G.J., Levin A.S., Thakkar S.C. Establishing telemedicine in an academic total joint arthroplasty practice: needs and opportunities highlighted by the COVID-19 pandemic. Arthroplast Today. 2020;6:617. doi: 10.1016/j.artd.2020.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Rizkalla J.M., Gladnick B.P., Bhimani A.A., Wood D.S., Kitziger K.J., Peters P.C., Jr. Triaging total hip arthroplasty during the COVID-19 pandemic. Curr Rev Musculoskelet Med. 2020;13:416. doi: 10.1007/s12178-020-09642-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Saxena A., Bullock M., Danoff J.R. Educating surgeons to educate patients about the COVID-19 pandemic. J Arthroplasty. 2020;35:S65. doi: 10.1016/j.arth.2020.04.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Stambough J.B., Curtin B.M., Gililland J.M. The past, present, and future of orthopedic education: lessons learned from the COVID-19 pandemic. J Arthroplasty. 2020;35:S60. doi: 10.1016/j.arth.2020.04.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Tanaka M.J., Oh L.S., Martin S.D., Berkson E.M. Telemedicine in the era of COVID-19: the virtual orthopaedic examination. J Bone Joint Surg Am. 2020;102:e57. doi: 10.2106/JBJS.20.00609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Thaler M., Khosravi I., Hirschmann M.T. Disruption of joint arthroplasty services in Europe during the COVID-19 pandemic: an online survey within the European Hip Society (EHS) and the European Knee Associates (EKA) Knee Surg Sports Traumatol Arthrosc. 2020;28(6):1712. doi: 10.1007/s00167-020-06033-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Vaccaro A.R., Getz C.L., Cohen B.E., Cole B.J., Donnally C.J., 3rd Practice management during the COVID-19 pandemic. J Am Acad Orthop Surg. 2020;28(11):464. doi: 10.5435/JAAOS-D-20-00379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Williams M., Blake S., Matthews H. Mitigating the risk of aerosol generation from power tools during the COVID-19 pandemic. Ann R Coll Surg Engl. 2020;102(5):393. doi: 10.1308/rcsann.2020.0082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wright R.W., Armstrong A.D., Azar F.M. The American board of orthopaedic surgery response to COVID-19. J Am Acad Orthop Surg. 2020;28(11):e465. doi: 10.5435/JAAOS-D-20-00392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Zagra L., Faraldi M., Pregliasco F. Changes of clinical activities in an orthopaedic institute in North Italy during the spread of COVID-19 pandemic: a seven-week observational analysis. Int Orthop. 2020;44:1591. doi: 10.1007/s00264-020-04590-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Gronbeck C., Cote M.P., Lieberman J.R., Halawi M.J. Risk stratification in primary total joint arthroplasty: the current state of knowledge. Arthroplast Today. 2019;5(1):126. doi: 10.1016/j.artd.2018.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Courtney P.M., Boniello A.J., Berger R.A. Complications following outpatient total joint arthroplasty: an analysis of a national database. J Arthroplasty. 2017;32(5):1426. doi: 10.1016/j.arth.2016.11.055. [DOI] [PubMed] [Google Scholar]
- 55.Aynardi M., Post Z., Ong A., Orozco F., Sukin D.C. Outpatient surgery as a means of cost reduction in total hip arthroplasty: a case-control study. HSS J. 2014;10(3):252. doi: 10.1007/s11420-014-9401-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Huang A., Ryu J.J., Dervin G. Cost savings of outpatient versus standard inpatient total knee arthroplasty. Can J Surg. 2017;60(1):57. doi: 10.1503/cjs.002516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Bozic K.J. What's important: preparing for the transition to value-based health care: an American Orthopaedic Association (AOA) 2016 OrthoTalk. J Bone Joint Surg Am. 2017;99(13):1150. doi: 10.2106/JBJS.16.01307. [DOI] [PubMed] [Google Scholar]
- 58.Bettger J.P., Green C.L., Holmes D.N. Effects of virtual exercise rehabilitation in-home therapy compared with traditional care after total knee arthroplasty VERITAS, a randomized controlled trial. J Bone Joint Surg Am. 2020;102(2):101. doi: 10.2106/JBJS.19.00695. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.