Abstract
Objective
To undertake an effectiveness and safety analysis of EVT in patients with LVO and NIH Stroke Scale (NIHSS) score ≤6 using datasets of multicenter and multinational nature.
Methods
We pooled patients with anterior circulation occlusion from 3 prospective international cohorts. Patients were eligible if presentation occurred within 12 hours from last known well and baseline NIHSS ≤6. Primary outcome was modified Rankin Scale (mRS) score 0–1 at 90 days. Secondary outcomes included neurologic deterioration at 24 hours (change in NIHSS of ≥2 points), mRS 0–2 at 90 days, and 90-day all-cause mortality. We used propensity score matching to adjust for nonrandomized treatment allocation.
Results
Among 236 patients who fit inclusion criteria, 139 received EVT and 97 received medical management. Compared to medical management, the EVT group was younger (65 vs 72 years; p < 0.001), had more proximal occlusions (p < 0.001), and less frequently received concurrent IV thrombolysis (57.7% vs 71.2%; p = 0.04). After propensity score matching, clinical outcomes between the 2 groups were not significantly different. EVT patients had an 8.6% (95% confidence interval [CI] −8.8% to 26.1%) higher rate of excellent 90-day outcome, despite a 22.3% (95% CI, 3.0%–41.6%) higher risk of neurologic deterioration at 24 hours.
Conclusions
EVT for LVO in patients with low NIHSS score was associated with increased risk of neurologic deterioration at 24 hours. However, both EVT and medical management resulted in similar proportions of excellent clinical outcomes at 90 days.
Classification of evidence
This study provides Class III evidence that for patients with acute anterior circulation ischemic strokes and LVO with NIHSS < 6, EVT and medical management result in similar outcomes at 90 days.
Patients with acute ischemic stroke (AIS) due to large vessel occlusion (LVO) usually have severely disabling symptoms.1 However, a significant number of patients with LVO present with milder symptoms.2 Endovascular thrombectomy (EVT) is a standard of care for AIS due to LVO, but level 1A guideline recommendations for EVT are restricted to patients with LVO with NIH Stroke Scale (NIHSS) score ≥6, because only a limited number of patients with low baseline NIHSS score were enrolled in the randomized controlled trials.3,4
AIS with NIHSS ≤6 is routinely considered as mild and nondisabling. However, 1 in 4 patients with LVO with low baseline NIHSS score have early neurologic deterioration, resulting in poorer outcome.5–7 From a patient perspective, milder deficits can restrict daily activities and can be devastating to quality of life. Patients with LVO and low baseline NIHSS score often have distinct clinical, demographic, and hospital arrival characteristics.8 Multiple nonrandomized studies have sought to evaluate the efficacy and safety of EVT in such patients and showed mixed results. These studies were mostly limited by their nonrandomized design, small sample size, single-center experiences, varying practice, or including patients treated prior to the efficacy of EVT was proven and incorporated into the (inter)national guidelines.8–15
The aim of our observational multicenter study was to assess the effectiveness and safety of EVT vs medical management in patients with LVO and NIHSS ≤6 using recent data from comprehensive datasets and propensity score matching.
Methods
We retrospectively identified patients with acute stroke with CT angiography (CTA)–proven anterior circulation occlusion and admission NIHSS ≤6. For this purpose, we retrieved EVT data from the Safe Implementation of Treatments in Stroke–Thrombectomy Registry (SITS-TBY) and compared them with medical management data derived from the Identifying New Approaches to Optimise Thrombus Characterization for Predicting Early Recanalization and Reperfusion With IV Alteplase and Other Treatments Using Serial CT Angiography (INTERRSeCT) and Measuring Collaterals With Multiphase CT Angiography in Patients With Ischemic Stroke (PROVE-IT) studies. The data sources are described in further detail below and inclusion and exclusion criteria for each study are presented in table 1.
Table 1.
Inclusion and exclusion criteria of study cohorts
Standard protocol approvals, registrations, and patient consents
Permissions to analyze data of SITS-TBY (a nonprofit, quality improvement–driven, international registry) were provided by the ethics committee of St. Anne's University Hospital, Brno, Czech Republic; individual patient consent for the SITS-TBY registry was not sought. The PROVE-IT study used a waiver of consent, which was approved by the Conjoint Health Research Ethics Board at the University of Calgary. Written informed consent was provided by the patient or a surrogate for the INTERRSeCT study. The reviews of the institutional review boards for each study determined that informed consent was not required for this current pooled analysis. The study protocol was approved by scientific committees of each study.
Endovascular data source
National EVT data from the Czech Republic were extracted from the population-based SITS-TBY registry from January 2015 to December 2018 to cover the time period after the publication of positive endovascular trials.16–20 The SITS-TBY registry represents a nonprofit, research-driven, international registry collecting data on endovascular treatment. Anonymized patient-level data are entered at each stroke center either by a research nurse or physician at discharge or at 90-day follow-up. There has been no formal audit of the Czech SITS-TBY or SITS-TBY data. However, 12 (out of 15) comprehensive stroke centers participated in the registry in 2016 as part of a quality improvement program. Random hospital-level metrics reported to the Czech Ministry of Health were cross-checked with the SITS data and showed high level of consistency (Robert Mikulik, MD, PhD, April 23, 2020, oral communication). In addition, a nationwide questionnaire survey run in 2016 did not show major differences in clinical practice including neuroimaging, logistics, and treatment standards in all 15 comprehensive stroke centers in the Czech Republic.21 Furthermore, since 2016, the Czech Stroke Society has been providing feedback quarterly to all participating stroke centers on number of EVT cases and time metrics based on the data from the registry. Patients for endovascular treatment in the Czech Republic are selected through CT and (multiphase) CTA imaging.
Medical management data source
Medical management was based on current guidelines (Canadian Stroke Best Practice Recommendations, American Heart and Stroke Association), including intravenous alteplase in patients presenting within the first 4.5 hours from last seen normal. In patients not eligible for IV alteplase, an antiplatelet agent was administered on day 1, unless there was an indication for early anticoagulation.
The 2 nonthrombectomy cohorts were selected from the multicenter international observational studies: (1) PROVE-IT (patient enrollment between July 2014 and October 2017) and (2) INTERRSeCT (patient enrollment between March 2010 and March 2016).
PROVE-IT was a prospective multicenter cohort study of 500 consecutive patients with AIS presenting within 12 hours of stroke symptom onset with evidence of intracranial occlusion on routine CTA. The primary aim of this trial was to evaluate imaging selection for thrombolysis and intra-arterial (endovascular) decision-making in the setting of AIS.22 INTERRSeCT was a multicenter prospective cohort study that enrolled 575 patients with AIS with intracranial thrombi documented via CTA. The study included patients with a wide range of clinical presentations (within 12 hours from last known well), occlusion sites, and thrombus characteristics to identify clinical and imaging variables associated with recanalization with or without IV thrombolysis.23
For the current study, we only included patients who were independently functioning in the community immediately prior to their stroke (estimated baseline modified Rankin Scale [mRS] score 0–2). Patients were eligible if they presented to the emergency department with symptoms consistent with AIS 12 hours from time last known well, baseline NIHSS ≤6, and baseline CTA with evidence of symptomatic intracranial occlusion (internal carotid artery [ICA] or middle cerebral artery [MCA] including M1 and proximal M2 segments). Patients with primary posterior circulation occlusions were excluded.
Demographics, variables, and measurements
Information on baseline demographics, vascular risk factors (hypertension, diabetes mellitus, dyslipidemia, atrial fibrillation, smoking history [current/past], congestive heart failure), time last seen normal, NIHSS score (range 0–42, with higher scores indicating severe stroke), occlusion location (ICA, M1, M2, MCA), prior use of anticoagulation, prior use of antithrombotic treatment, and IV alteplase administration (if applicable, although many patients with low NIHSS are not thrombolysed) were collected. Other clinical endpoints were 24-hour NIHSS score and functional outcome at 90 days measured on the mRS.
Study outcomes
mRS 0–1 at 90 days was chosen as the primary outcome because patients with mild deficits at baseline are more likely to have excellent outcomes. Secondary outcomes were neurologic deterioration at 24 hours (defined as increase of NIHSS score by 2 or more points),24 mRS 0–2 at 90 days, and all-cause mortality at 90 days.
Missing/incomplete data
Among 236 patients, 4 had missing baseline NIHSS, 5 missing prior anticoagulation history, 6 missing prior smoking history, 6 prior atrial fibrillation history, 1 missing prior hypertension and prior dyslipidemia history, 14 missing 24-hour NIHSS, and 13 missing 90-day mRS. We imputed the missing NIHSS baseline values with the group median from the remaining available data and imputed “no” for missing binary variables. The 13 missing values for 90-day mRS were again imputed with the median of the remaining available data. Because all missing mRS scores were in the EVT group, we performed additional sensitivity analysis assuming that the missing 90-day mRS values indicated that the person did not reach a favorable outcome and was disabled or dead (i.e., worst-case scenario), did achieve a favorable outcome (i.e., best-case scenario), and omitted cases with missing mRS scores. For the 14 missing values of 24-hour NIHSS (all but 1 from the EVT group), we assumed that the patients had neurologic deterioration (i.e., worst-case scenario).
Data about intracranial hemorrhages were missing and unverifiable in the SITS-TBY registry and thus could not be analyzed in our study. Because the SITS-TBY registry is a study of implementation of thrombectomy in routine clinical practice, it was not mandated that time metrics were being collected. Onset-to-treatment times were thus not available for our analysis.
Statistical analysis
Standard descriptive statistics were used to measure central tendency and variability of baseline characteristics. Ordinal/continuous variables were compared by the Mann-Whitney test or t test based on their distribution. Categorical variables were compared using the Fisher exact test.
Because our data were not randomized, we used propensity score matching to estimate the adjusted treatment effect of EVT compared to the best medical management, accounting for differences in baseline variables. We used the treatment effect option with propensity score matching in STATA version 14.2 (College Station, TX). Derivation of standard error accounted for the fact that propensity scores are estimated rather than known. Propensity scores were derived from a multivariable logistic regression model that calculates the treatment probability for each participant. This model was adjusted for the following clinically relevant baseline variables: sex, age, occlusion location, thrombolysis status, baseline mRS, prior antithrombotic treatment, and NIHSS. The propensity scores were then used to impute the missing potential outcome (if a participant received EVT then medical management is considered counterfactual and if the participant received medical management then EVT is considered counterfactual) for each participant by taking the outcome of a similar participant who received the other treatment level (or multiple participants if there was a tie for similarity). Similarity between participants was based on the propensity scores. Common support was assessed using an overlap plot and examination of mean propensity scores by treatment group and quintiles and found to be adequate (figure 1 and table 2). The treatment effect was computed by taking the average of the difference among each EVT and medical management pair, where outcomes were either observed or derived as the counterfactual from the propensity matching process and presented as a risk difference with 95% confidence interval (CI). We used this method of matching and analysis for our primary, secondary, and safety outcomes. We visualized the unadjusted data and the results of our primary analysis using horizontally stacked bar graphs. Sensitivity analysis was performed for the primary outcome using the worst-case scenario, best-case scenario, and by omitting cases with missing primary outcome as described above.
Figure 1. Overlap plot of propensity scores to check for common support.
Table 2.
Mean propensity scores by quintiles and treatment group

All tests were 2-sided and the significance level was considered as 0.05. Statistical analyses were performed using STATA version 14.2 (College Station, TX).
Data availability
Anonymized data will be shared by reasonable request from a qualified investigator.
Results
Baseline characteristics
Our pooled dataset resulted in 281 patients with LVO and mild symptoms. We excluded 11 patients who were not independent at baseline, 33 patients with distal M2, M3, and no occlusion, and 1 patient treated with tenecteplase. This left 236 patients for analysis: 139 received EVT and 97 medical management. The 2 groups had similar baseline NIHSS, baseline mRS, and baseline vascular risk factors. The EVT group was younger (65 vs 72 years), with more proximal occlusions (50.4% M1 and 15.8% ICA vs 25.8% M1 and 2.1 ICA), and less concurrent intravenous alteplase treatment (57.7% vs 71.2%), as illustrated in table 3.
Table 3.
Baseline characteristics before propensity score matching process

Primary and secondary outcomes
Ninety-day excellent outcome (mRS 0–1) was achieved in 62.7% (n = 148) of patients overall, with no difference between the EVT and medical management group (61.9% vs 63.9%, p = 0.785) in unadjusted analysis. The raw distribution of mRS scores between the EVT and medical management group at 90 days is shown in figure 2. After propensity score matching, patients in the EVT group had an 8.6% (95% CI, −8.8% to 26.1%) higher chance of excellent outcome at 90 days compared to the medical management group. The distribution of mRS scores of the EVT and medical management group at 90 days after the propensity score matching is presented in figure 3. The result was unchanged in sensitivity analysis using the worst case scenario (missing outcomes assumed to have achieved mRS 2–6) and when cases with missing mRS were omitted (p = 0.33 and p = 0.250, respectively). However, assuming best-case scenario (missing outcomes actually achieved mRS 0–1), patients in the EVT group had a 17.6% (95% CI, 0.01%–35.4%) higher chance of excellent outcome at 90 days compared to the medical management group.
Figure 2. Unadjusted analysis of 90-day modified Rankin Scale (mRS) score shift.
EVT = endovascular treatment; MM = medical management.
Figure 3. Propensity score matched analysis of 90-day modified Rankin Scale (mRS) score shift.
EVT = endovascular treatment; MM = medical management.
Unadjusted analyses of the secondary outcomes are shown in table 4. After propensity score matching, patients in the EVT group had a 22.3% (95% CI, 3.0%–41.6%) higher risk of neurologic deterioration at 24 hours compared to patients in the medical management group. Patients in the EVT group also had a 2.2% (95% CI, −3.6% to 7.9%) higher risk of death from any cause within the first 90 days after the index event compared to the medical management group.
Table 4.
Unadjusted outcome analysis
Discussion
In our study, endovascular treatment and best medical management for large vessel anterior circulation occlusion in patients presenting with low NIHSS resulted in similar proportions of excellent functional outcome at 90 days and comparable all-cause 90-day mortality. This outcome parity occurred despite an increased endovascular treatment risk of neurologic deterioration at 24 hours.
In keeping with our results, other smaller multicenter studies have used propensity score matching and found no significant difference in excellent functional outcome at 90 days.9–11 Although the study by Nagel et al.10 (77 matched pairs) showed a 14.4% absolute difference in good clinical outcome (84.4% vs 70.1%, p = 0.03), defined as mRS 0–2 and an adjusted odds ratio of 3.1 (95% CI, 1.4–6.9) favoring immediate EVT, there was no such difference seen for excellent outcome defined as mRS 0–1 at 90 days. In addition, the study enrolled 7% of patients with basilar occlusions and 6% of patients with initial mRS >2 (20/300 patients). In the study by Haussen et al.,12 the protocol also allowed inclusion of patients with basilar occlusions, which then made up 23% of the EVT group. These and other previously published (mostly single-center) studies have selected individual sites with variability in their approach to patient care and differing local treatment guidelines. A more recent study by Asdaghi et al.8 looked at over 400 registry patients and found an association of EVT with favorable discharge outcomes and ambulatory status. However, the 90-day outcomes as well as the occlusion status and thrombus location were not documented consistently. All 3 of these studies included patients who received endovascular treatment before the publication of positive randomized control trials in 2015 and thus the incorporation of endovascular treatment as a standard of care into national guidelines. Thus, the results of these studies might be reflective of the heterogeneity in workflow and experience with such patients and might not be representative of the current clinical practice.
We found no difference in all-cause 90-day mortality in our study, which is in congruence with the smaller multicenter studies of Nagel et al.10 and Dargazanli et al.11 In the study of Sarraj et al.,9 the patients undergoing EVT had higher mortality (8.9% vs 1.1%, p = 0.03), possibly driven by increased risk of symptomatic intracranial hemorrhage (sICH; 5.8% vs 0%).9–11 Similarly, Asdaghi et al.8 reported mortality of 5.2% and sICH rate of 4.5%.
Endovascular treatment was associated with increased risk of neurologic deterioration at 24 hours (defined as ≥2 points increase of the NIHSS scale) in our propensity score–matched analysis. One possible explanation might be the occurrence of sICH with the endovascular treatment. Neurologic deterioration might have also been more apparent on formal testing in a setting of mild initial symptoms and thus been more diligently scored. Furthermore, other complications of EVT, including embolic events into other arterial territories, and arterial access adverse events such as hemorrhage, retroperitoneal hematoma, and pseudoaneurysm formation may affect 24-hour assessment.
Multiple studies have shown that because patients with low NIHSS score are generally considered to have disease too mild for thrombolysis and endovascular treatment, up to one third end up disabled or dead at the 90-day follow-up when left hyperacutely untreated.25–28 It is known that in stroke due to (large) vessel occlusion, there is a clear relationship between recanalization and favorable/excellent outcome even though our current study and various others have shown differing effect sizes (from 8.6% to 14.4%).10,29 Yet interventional treatment, whether medical with IV thrombolysis or surgical with EVT, has possible harm. The value of a future randomized controlled trial in this patient cohort is thus not to show the benefit of EVT but rather to assess if the benefit outweighs the potential harm of the treatment. Data about intracranial hemorrhages were missing and unverifiable in the SITS-TBY registry and could thus not be analyzed in our current study. However, 2 previous studies in low NIHSS strokes that have specifically measured sICH found a notable difference between the EVT and medical management group (Sarraj et al.9 5.8% vs 0% [p = 0.02], Nagel et al.10 5% vs 1.4% [p = 0.08]). However, these are sICH risks that we accept for moderate to severely disabling stroke and the acceptable risk of sICH must be significantly less in low NIHSS strokes to justify the risk of death and disability as a complication of EVT. Due to this uncertainty in numbers, despite several analyses from groups around the world, a well-designed randomized controlled trial would be able to finally answer the question about the risk:benefit ratio of EVT for low NIHSS strokes.
A strength of our study is the multicenter and multinational nature of the datasets. The national population-based EVT data were extracted from the SITS-TBY registry from January 2015 to December 2018 in order to cover the time period after the publication of positive endovascular trials and as such reflect current clinical practice. Our study is limited by its retrospective nature and even though we tried to account for confounding by using advanced statistical methods, there is still a risk of residual confounding due to unmeasured variables. For example, even though we incorporated occlusion location into our propensity score model, we were unable to also incorporate a measure of early ischemic change since these data were not available. Furthermore, onset-to-treatment times were not available for our analysis. Although 12 of total 15 comprehensive stroke centers in the Czech Republic contributed to the SITS-TBY registry during the study period, our previous study showed that over 80% of all thrombectomy cases in the Czech Republic were reported to the registry in 2016.30 We also had no data on the use of anesthesia/sedation during EVT available. Blood pressure changes during induction of general anesthesia may risk penumbral tissue perfusion and might thus contribute to neurologic deterioration at 24 hours.31,32 The mRS, although one of the most commonly used outcome markers in stroke and captured by the 3 observational data sources we have used, lacks sensitivity at the minor disability end of the scale and we might thus have not been able to detect a significant difference in our primary outcome. Our matched analysis is larger than the sample size of prior studies but still might have affected our statistical power to detect a true difference. Race and ethnicity were not collected in the 3 datasets used.
Our multicenter observational post hoc study showed that EVT for LVO in patients with low NIHSS resulted in similar 90-day outcomes compared to the best medical management despite an increased risk of neurologic deterioration at 24 hours.
Glossary
- AIS
acute ischemic stroke
- CI
confidence interval
- CTA
CT angiography
- EVT
endovascular thrombectomy
- ICA
internal carotid artery
- INTERRSeCT
Identifying New Approaches to Optimise Thrombus Characterization for Predicting Early Recanalization and Reperfusion With IV Alteplase and Other Treatments Using Serial CT Angiography
- LVO
large vessel occlusion
- MCA
middle cerebral artery
- mRS
modified Rankin Scale
- NIHSS
NIH Stroke Scale
- PROVE-IT
Measuring Collaterals With Multiphase CT Angiography in Patients With Ischemic Stroke
- sICH
symptomatic intracranial hemorrhage
- SITS-TBY
Safe Implementation of Treatments in Stroke–Thrombectomy Registry
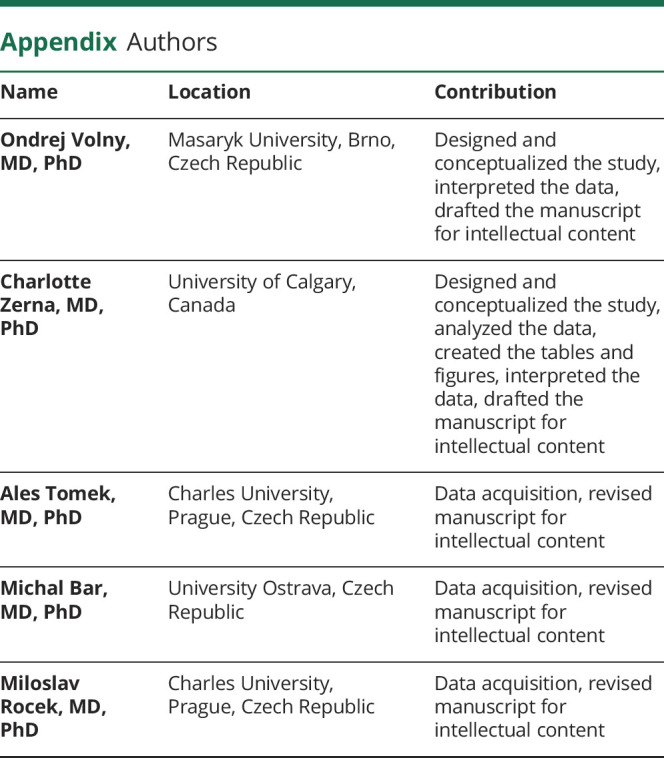
Appendix. Authors


Footnotes
Class of Evidence: NPub.org/coe
Study funding
No targeted funding reported.
Disclosure
O. Volny reports no disclosures relevant to this manuscript. C. Zerna holds a Clinician Fellowship Award from Alberta Innovates Health Solutions. A. Tomek, M. Bar, M. Rocek, R. Padr, F. Cihlar, M. Nevsimalova, L. Jurak, R. Havlicek, M. Kovar, P. Sevcik, V. Rohan, J. Fiksa, D. Cernik, R. Jura, D. Vaclavik, P. Cimflova, J. Puig, D. Dowlatshahi, A.V. Khaw, E. Feinardi, and M. Najm report no disclosures relevant to this manuscript. A.M. Demchuk is supported by the Heart and Stroke Foundation of Alberta Chair in Stroke Research. B.K. Menon is supported by the Heart and Stroke Foundation of Alberta Professorship in Stroke Imaging. R. Mikulik reports no disclosures relevant to this manuscript. M.D. Hill reports support from the Heart and Stroke Foundation of Alberta-Hotchkiss Brain Institute Professorship in Stroke Research. All other authors report no disclosures. Go to Neurology.org/N for full disclosures.
References
- 1.Heldner MR, Zubler C, Mattle HP, et al. National Institutes of Health Stroke Scale score and vessel occlusion in 2152 patients with acute ischemic stroke. Stroke 2013;44:1153–1157. [DOI] [PubMed] [Google Scholar]
- 2.Maas MB, Furie KL, Lev MH, et al. National Institutes of Health Stroke Scale score is poorly predictive of proximal occlusion in acute cerebral ischemia. Stroke 2009;40:2988–2993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Powers WJ, Rabinstein AA, Ackerson T, et al. 2018 Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2018;49:e46–e110. [DOI] [PubMed] [Google Scholar]
- 4.Goyal M, Menon BK, van Zwam WH, et al. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet 2016;387:1723–1731. [DOI] [PubMed] [Google Scholar]
- 5.Kim JT, Park MS, Chang J, Lee JS, Choi KH, Cho KH. Proximal arterial occlusion in acute ischemic stroke with low NIHSS scores should not be considered as mild stroke. PLoS One 2013;8:e70996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rajajee V, Kidwell C, Starkman S, et al. Early MRI and outcomes of untreated patients with mild or improving ischemic stroke. Neurology 2006;67:980–984. [DOI] [PubMed] [Google Scholar]
- 7.Coutts SB, Modi J, Patel SK, Demchuk AM, Goyal M, Hill MD. CT/CT angiography and MRI findings predict recurrent stroke after transient ischemic attack and minor stroke: results of the prospective catch study. Stroke 2012;43:1013–1017. [DOI] [PubMed] [Google Scholar]
- 8.Asdaghi N, Yavagal DR, Wang K, et al. Patterns and outcomes of endovascular therapy in mild stroke. Stroke 2019;50:2101–2107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sarraj A, Hassan A, Savitz SI, et al. Endovascular thrombectomy for mild strokes: how low should we go? Stroke 2018;49:2398–2405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nagel S, Bouslama M, Krause LU, et al. Mechanical thrombectomy in patients with milder strokes and large vessel occlusions. Stroke 2018;49:2391–2397. [DOI] [PubMed] [Google Scholar]
- 11.Dargazanli C, Arquizan C, Gory B, et al. Mechanical thrombectomy for minor and mild stroke patients harboring large vessel occlusion in the anterior circulation: a multicenter cohort study. Stroke 2017;48:3274–3281. [DOI] [PubMed] [Google Scholar]
- 12.Haussen DC, Lima FO, Bouslama M, et al. Thrombectomy versus medical management for large vessel occlusion strokes with minimal symptoms: an analysis from STOPStroke and GESTOR cohorts. J Neurointerv Surg 2018;10:325–329. [DOI] [PubMed] [Google Scholar]
- 13.Pfaff J, Herweh C, Pham M, et al. Mechanical thrombectomy in patients with acute ischemic stroke and lower NIHSS scores: recanalization rates, periprocedural complications, and clinical outcome. AJNR Am J Neuroradiol 2016;37:2066–2071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wolman DN, Marcellus DG, Lansberg MG, et al. Endovascular versus medical therapy for large-vessel anterior occlusive stroke presenting with mild symptoms. Int J Stroke 2020;15:324–331. [DOI] [PubMed] [Google Scholar]
- 15.Shang X, Lin M, Zhang S, et al. Clinical outcomes of endovascular treatment within 24 hours in patients with mild ischemic stroke and perfusion imaging selection. AJNR Am J Neuroradiology 2018;39:1083–1087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Berkhemer OA, van Zwam WH, Dippel DW. Stent-retriever thrombectomy for stroke. N Engl J Med 2015;373:1076. [DOI] [PubMed] [Google Scholar]
- 17.Goyal M, Demchuk AM, Menon BK, et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med 2015;372:1019–1030. [DOI] [PubMed] [Google Scholar]
- 18.Jovin TG, Chamorro A, Cobo E, et al. Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med 2015;372:2296–2306. [DOI] [PubMed] [Google Scholar]
- 19.Saver JL, Goyal M, Diener HC. Stent-retriever thrombectomy for stroke. N Engl J Med 2015;373:1077. [DOI] [PubMed] [Google Scholar]
- 20.Campbell BC, Mitchell PJ, Kleinig TJ, et al. Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med 2015;372:1009–1018. [DOI] [PubMed] [Google Scholar]
- 21.Volny O, Bar M, Krajina A, et al. A comprehensive nationwide evaluation of stroke centres in the Czech Republic performing mechanical thrombectomy in acute stroke in 2016. Ceska Slovenska Neurol Neurochir 2017;113:445–450. [Google Scholar]
- 22.Santos EMM, d'Esterre CD, Treurniet KM, et al. Added value of multiphase CTA imaging for thrombus perviousness assessment. Neuroradiology 2018;60:71–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Menon BK, Al-Ajlan FS, Najm M, et al. Association of clinical, imaging, and thrombus characteristics with recanalization of visible intracranial occlusion in patients with acute ischemic stroke. JAMA 2018;320:1017–1026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Siegler JE, Boehme AK, Kumar AD, Gillette MA, Albright KC, Martin-Schild S. What change in the National Institutes of Health stroke scale should define neurologic deterioration in acute ischemic stroke? J Stroke Cerebrovasc Dis 2013;22:675–682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Smith EE, Fonarow GC, Reeves MJ, et al. Outcomes in mild or rapidly improving stroke not treated with intravenous recombinant tissue-type plasminogen activator: findings from Get With the Guidelines–Stroke. Stroke 2011;42:3110–3115. [DOI] [PubMed] [Google Scholar]
- 26.Barber PA, Zhang J, Demchuk AM, Hill MD, Buchan AM. Why are stroke patients excluded from tPA therapy? An analysis of patient eligibility. Neurology 2001;56:1015–1020. [DOI] [PubMed] [Google Scholar]
- 27.Nedeltchev K, Schwegler B, Haefeli T, et al. Outcome of stroke with mild or rapidly improving symptoms. Stroke 2007;38:2531–2535. [DOI] [PubMed] [Google Scholar]
- 28.Smith EE, Abdullah AR, Petkovska I, Rosenthal E, Koroshetz WJ, Schwamm LH. Poor outcomes in patients who do not receive intravenous tissue plasminogen activator because of mild or improving ischemic stroke. Stroke 2005;36:2497–2499. [DOI] [PubMed] [Google Scholar]
- 29.Mishra SM, Dykeman J, Sajobi TT, et al. Early reperfusion rates with iv tPA are determined by CTA clot characteristics. AJNR Am J Neuroradiol 2014;35:2265–2272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Volny O, Krajina A, Belaskova S, et al. Mechanical thrombectomy performs similarly in real world practice: a 2016 nationwide study from the Czech Republic. J Neurointerv Surg 2018;10:741–745. [DOI] [PubMed] [Google Scholar]
- 31.Davis MJ, Menon BK, Baghirzada LB, et al. Anesthetic management and outcome in patients during endovascular therapy for acute stroke. Anesthesiology 2012;116:396–405. [DOI] [PubMed] [Google Scholar]
- 32.Campbell BCV, van Zwam WH, Goyal M, et al. Effect of general anaesthesia on functional outcome in patients with anterior circulation ischaemic stroke having endovascular thrombectomy versus standard care: a meta-analysis of individual patient data. Lancet Neurol 2018;17:47–53. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Anonymized data will be shared by reasonable request from a qualified investigator.







