Abstract
Objective
The Novel Coronavirus19 (COVID19) arrived in northern New Jersey (NJ) in early March 2020, peaked at the beginning of April, and then declined. Starting in March, some patients who called 911 and required advanced life support (ALS) may have decompensated more rapidly than would have been expected, possibly because of concomitant COVID19 infection and/or delays in seeking medical care because of fear of exposure to the virus, and social isolation. In this study, our goal was to determine if there was an increase in prehospital ALS pronouncements and a decrease in ED visits for potentially serious conditions such as MI and stroke during the peak of the COVID-19 pandemic in northern NJ.
Methods study design
Retrospective cohort of prehospital patients pronounced dead by paramedics and patients with MI and stroke in the EDs of receiving hospitals of these paramedics. Study Setting and Population: Ten ground ALS units in northern NJ and nine receiving hospital EDs. Each ALS unit is staffed by two NJ-certified mobile intensive care paramedics and respond with a paramedic flycar in a two-tiered dispatch system. Data Analysis: We identified prehospital pronouncements using the EMSCharts electronic record (Zoll Medical, Chelmsford, Massachusetts). We tabulated the number of pronouncements by week from January 1 to June 30 in 2019 and 2020. We tabulated the combined total number of pronouncements and ED visits by month along with visits for MI and stroke and calculated the changes during the same timeframe. We used Chi-square to test for statistical significance for the monthly changes from 2019 to 2020.
Results
For January through June in 2019 and 2020, there were 12,210 and 13,200 ALS dispatches, and 366 and 555 prehospital pronouncements, respectively. In 2020, pronouncements rose from a weekly baseline of 13 in early March, reached a peak of 45 at the beginning of April, then returned to the baseline level by the end of May. April 2020, the month with the most pronouncements, had 183% more pronouncements than April 2019 but total ED visits and visits for MI and stroke were 49%, 46% and 42% less, respectively (p < 0.0001 for each of these changes).
Conclusion
Following the arrival of the COVID-19 pandemic in northern NJ, we found pre-hospital ALS death pronouncements increased and ED visits for MI and stroke decreased. Although we have speculated about the reasons for these findings, further studies are needed to determine what the actual causes were.
Keywords: Out-of-hospital cardiac arrest, Prehospital pronouncement, Emergency department, Myocardial infarction, Stroke
1. Introduction
In March 2020 the Novel Coronavirus19 (COVID19) arrived in Northern New Jersey (NJ), peaked in late March and April, and then declined [1]. By April 17, NJ had more cases than any other state except for New York [2]. Hospitals were overwhelmed caring for critical patients at near maximum capacity. In addition to patients' personal fear of contracting COVID19, they were being advised by primary care physicians, the media, and even healthcare systems to avoid public places, including the emergency department (ED) [3]. Many patients suffering from symptoms of chest pain, shortness breath, or weakness, for which people typically come to the ED and that are potential indicators of serious conditions, not necessarily associated with COVID19, did not seek medical care [4,5]. Starting in March, some patients who called 911 and required advanced life support (ALS) may have been more critically ill than they would have been before COVID19. There are several possible reasons for this, including: (1) they had unexpected precipitous decline from COVID19 itself [6], (2) they were further along in the course of their underlying disease(s) due to the delay in seeking care, including calling 911 [7,8], (3) they had COVID19 infection in addition to their underlying disease, (4) bystanders were less likely to perform cardio pulmonary resuscitation (CPR) because of fear of contracting COVID19 [9,10]; and/or (5) because of social isolation/distancing, more patients were alone when they arrested, delaying resuscitation and decreasing the likelihood of survival [11,12].
The precipitous decline in patients' conditions may have led to increased prehospital pronouncements for all the reasons given above. It also may have led to decrease in ED visits for myocardial infarction (MI) and stroke because: for the sicker patients, they may have declined too rapidly to get to the ED for reasons (1,2,3) above, and, for the less sick patients, they may just have decided not to come to the hospital at all.
In this study, our goal was to determine if there was an increase in prehospital ALS pronouncements and a decrease in ED visits for potentially serious conditions such as MI and stroke after arrival of COVID19 in northern NJ.
2. Methods
2.1. Study design: retrospective cohort
Study Setting and Population: Time period: January 1 to June 30 in 2019 and 2020. We examined the following:
(1) Patients who were pronounced dead by ten ground paramedic units in northern NJ. Each unit is staffed by two NJ-certified mobile intensive care paramedics that respond with a paramedic flycar in a two-tiered dispatch system.
(2) Total visits and visits for MI and stroke in the EDs of nine receiving hospitals for the paramedics. The nine hospitals are in urban, suburban and rural settings with 20,000 to 103,000 annual ED visits. Two of the hospitals have emergency medicine residencies.
Data Collection and Analysis: We identified pronouncements using an electronic patient care record (PCR) from the EMSCharts software (Zoll Medical, Chelmsford, MA). We searched the disposition field in the PCR and found the following pronouncement outcomes: Pronounced at Scene, Pronouncement, Termination of Resuscitative Efforts (TRE) without ALS, or Termination of Resuscitative Efforts (TRE) after ALS Treatment. We extracted data into an Excel (Microsoft Corp, Redmond, WA) spreadsheet. We computed and plotted the number of prehospital pronouncements by week for January 1 to June 30 in 2019 and 2020. For these time periods we also tabulated by month the following: pronouncements and the total number of ED, MI and stroke visits. We identified MIs and stroke using the International Classification of Diseases (Version 10) codes I21.xx and I63.xx, respectively. We calculated and plotted the percent changes by month from 2019 to 2020. We used Chi-square to test for statistical significance for the difference in monthly pronouncements and ED visits for MI and stroke between 2019 and 2020. We restricted our analysis to the months, March through June, because COVID 19 arrived in our area in March. We set alpha at 0.003, using the Bonferroni correction for multiple comparisons. The IRB approved the study.
3. Results
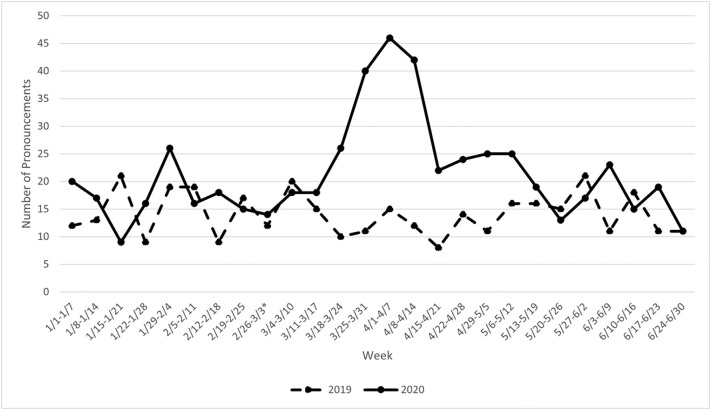
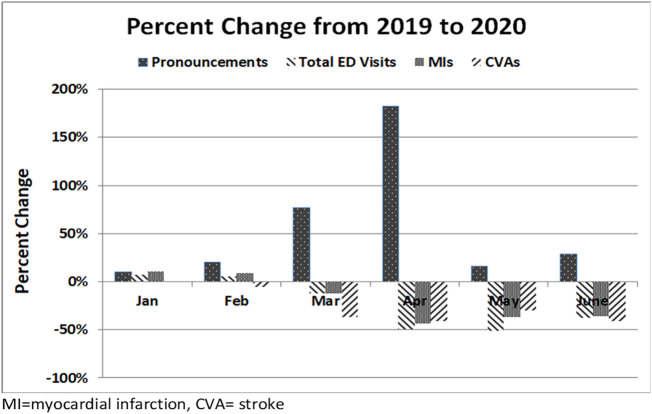
For January through June in 2019 and 2020, there were 12,210 and 13,200 ALS dispatches, and 366 and 555 prehospital pronouncements, respectively. In 2020, pronouncements rose from a weekly baseline of 13 in early March, reached a peak of 45 at the beginning of April, then returned to the baseline level by the end of May. (Fig. 1 ). For the period January 1 to June 30 the total ED visits were 302,272 and 233,518 for 2019 and 2020, respectively. The ED visits for MIs for the same time periods in 2019 and 2020 were 981 and 811, respectively; for strokes, they were 888 and 666, respectively. The percent change from 2019 to 2020 in monthly paramedic pronouncements, total ED visits and ED visits for MI and stroke are shown in Fig. 2 .
Fig. 1.
Weekly Number of Pre-Hospital Death Pronouncements in the First Six Months of 2019 and 2020.
Fig. 2.
Percent Change from 2019 to 2020 in Pre-Hospital Death Pronouncements, Total Emergency Departments Visits and Visits for Myocardial Infarction and Stroke.
April 2020, the month with most pronouncements, had 183% more pronouncements than April 2019 but total ED visits and visits for MI and stroke were 49%, 46% and 42% less, respectively (p < 0.0001 for each of these changes).
3.1. Discussion
Following the arrival of the COVID-19 pandemic in northern NJ, we found pre-hospital ALS death pronouncements and ED visits for MI and stroke decreased. The time course of the peak in pronouncements (Fig. 1) follows closely with the peak in COVID19 cases [1]. Although the pronouncements returned close to baseline by the end of May, the decrease in ED visits for stroke and MI continued for the entire remaining period of our study. This suggests that persistent concern about contracting COVID19 by coming to the ED was the predominant cause of the decreased ED visits for MI and stroke in May and June, because the number of COVID19 cases had decreased markedly by that time.
We found several previous studies that reported prehospital pronouncements after out-of-hospital cardiac arrest (OHCA) in the setting of this pandemic but none in any other epidemic. Baldi et al. compared the number of pronouncements in Lombardi, Italy in a two-month period from the end of February to the end of April during COVID19 in 2020 with the same period in 2019 and found a 62% increase, which is considerably less than our 183% increase [13]. Friedman et al. found a 145% increase in out-of-hospital deaths in Tijuana following arrival of COVID19 there [14]. In the six-week period of the pandemic in Paris, compared to the same six-week periods in 2012–2020 prehospital deaths following OHCA increased 54% [12]. Mountantonakis et al. found a six-fold increase in pronouncements in New York City, from March 20 to April 22, 2020 compared with the same period in 2019 [15]. In contrast to all these studies and our results, Paoli et al. found no increase in Padua, Italy, in out of hospital deaths, comparing March and April in 2020 with the same period in 2019 [16].
We found that at the peak of the pandemic in northern NJ, ED visits for stroke and MI decreased by 41% and 44%, respectively (Fig. 2). Others have found similar results. De Filippo et al. found a 26–30% decrease in admission rates for acute coronary syndrome [ACS] in 15 hospitals in northern Italy in the 40 days following the arrival of COVID19 [17]. Similarly, De Rosa et al. found 48% fewer intensive care unit admissions for MIs in Italy during the COVID19 outbreak [18]. Giamello et al. found a decrease in visits to an Italian ED for a number of conditions, including a 45% decrease in visits for ACS [19]. Metzler et al. found a decline in ACS as the pandemic arrived in Austria [20]. Percutaneous coronary intervention for MI decreased 32% in 20 centers in Italy following the arrival of COVID19 [21]. The number of ST-elevation MI (STEMI) patients decreased by 23% after COVID19 arrived in 75 centers in Spain [8]. Time from symptom onset to first medical care was 105 min during the pandemic compared to 71 min before (p < 0.001) and in-hospital mortality during the pandemic was 7.5% compared to 5.1% before (p < 0.019), suggesting a possible association between delay in seeking care and worse outcome. In a London hospital, weekly primary percutaneous coronary intervention referrals, catheterization laboratory activations and STEMI presentations decreased by 43%, 53% and 51%, respectively during COVID19 [22]. Although the time to call for help was significantly longer, in contrast to the report above mortality did not increase. STEMI activations decreased 45% during the pandemic in a Los Angeles hospital [23] and STEMI catheterizations decreased 14% in a hospital in North Carolina [24].
Stroke admissions decreased 90% in an Italian casualty department after the arrival of COVID19 [25]. A study of a network of health care organizations in over 30 countries showed a 25–43% decrease in the number of patients with stroke during the pandemic [26]. A study in hospitals in the Amsterdam area showed a 24% decrease in the number of patients with a suspected stroke during the height of the COVID19 pandemic, compared to a pre-COVID19 control period [27].
3.2. Limitations
Our study has a number of limitations. We performed a retrospective data abstraction from electronic medical records, which has innate problems and shortcomings [28]. In particular, our databases did not have information to determine the specific causes of the increased pre-hospital death pronouncements. We may have undercounted or over-counted the number of pronouncements and visits for MI and stroke, although we believe this effect to be small and, in any case, would be unlikely to have changed over the course of the study. Although the data abstracters were not blinded to the hypothesis of the study, there were well defined objective data present in the same place in the PCR. We analyzed data for ten ground ALS units and nine receiving hospitals, in northern NJ. This may not be representative of other areas in NJ or other states in the US or, indeed, other countries. Finally, retrospective studies such as ours can imply only association, not causation [28].
4. Conclusion
Following the arrival of the COVID-19 pandemic in northern NJ, we found pre-hospital ALS death pronouncements increased and ED visits for MI and stroke decreased. Although we have speculated about the reasons for these findings, further studies are needed to determine what the actual causes were.
Declaration of Competing Interest
None.
References
- 1.New Jersey Statistics 2020. https://www.state.nj.us/health/cd/documents/topics/NCOV/COVID_Confirmed_Case_Summary.pdf (Accessed 11/6/2020)
- 2.CDC COVID-19 Response Team. Geographic differences in COVID-19 cases, deaths, and incidence - United States, February 12–April 7, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:465–471. doi: 10.15585/mmwr.mm6915e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.CDC Coronavirus Disease 2019 (COVID-19) 2020. https://www.cdc.gov/coronavirus/2019-ncov/if-you-are-sick/steps-when-sick.html (Accessed 11/6/2020)
- 4.Czeisler M.É., Marynak K., Clarke K.E., et al. Delay or avoidance of medical care because of COVID-19–related concerns — United States, June 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1250–1257. doi: 10.15585/mmwr.mm6936a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Orthopoulos G., Santone E., Izzo F., et al. Increasing incidence of complicated appendicitis during COVID-19 pandemic. Am J Surg. 2020 Sep 28 doi: 10.1016/j.amjsurg.2020.09.026. S0002-9610(20)30595-X. [Online ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Guimaraes R.B., Falcão B., Costa R.A., et al. Acute coronary syndromes in the current context of the Covid-19 pandemic. Arq Bras Cardiol. 2020;114:1067–1071. doi: 10.36660/abc.20200358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shekhar A.C., Mercer C., Blumen I., et al. Suboptimal rates of return of spontaneous circulation with prehospital CPR in the COVID-19 era. Resuscitation. 2020;154:50–51. doi: 10.1016/j.resuscitation.2020.06.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rodriguez-Leor O., Cid-Álvarez B., de Prado A.P., et al. Impact of COVID-19 on ST-segment elevation myocardial infarction care. The Spanish experience. Rev Esp Cardiol (Engl Ed) 2020 Sep 8 doi: 10.1016/j.rec.2020.08.002. S1885-5857(20)30362-5. [Online ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Scquizzato T., Olasveengen T.M., Ristagno G., et al. The other side of novel coronavirus outbreak: fear of performing cardiopulmonary resuscitation. Resuscitation. 2020;150:92–93. doi: 10.1016/j.resuscitation.2020.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hammad T.A., Parikh M., Tashtish N., et al. Impact of COVID-19 pandemic on ST-elevation myocardial infarction in a non-COVID-19 epicenter. Catheter Cardiovasc Interv. 2020 Jun 1 doi: 10.1002/ccd.28997. [Online ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pranata R., Lim M.A., Yonas E., et al. Out-of-hospital cardiac arrest prognosis during the COVID-19 pandemic. Intern Emerg Med. 2020;15:875–877. doi: 10.1007/s11739-020-02428-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Marijon E., Karam N., Jost D., et al. Out-of-hospital cardiac arrest during the COVID-19 pandemic in Paris, France: a population-based, observational study. Lancet Public Health. 2020;5:e437–e443. doi: 10.1016/S2468-2667(20)30117-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Baldi E., Sechi G.M., Mare C., et al. COVID-19 kills at home: the close relationship between the epidemic and the increase of out-of-hospital cardiac arrests. Eur Heart J. 2020;41:3045–3054. doi: 10.1093/eurheartj/ehaa508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Friedman J., Calderon-Villarreal A., Bojorquez I., et al. Excess out-of-hospital mortality and declining oxygen saturation: the sentinel role of emergency medical services data in the COVID19 crisis in Tijuana. Mexico Ann Emerg Med. 2020;76:413–426. doi: 10.1016/j.annemergmed.2020.07.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mountantonakis S.E., Saleh M., Coleman K., et al. Out-of-hospital cardiac arrest and acute coronary syndrome hospitalizations during the COVID-19 surge. J Am Coll Cardiol. 2020;76:1271–1273. doi: 10.1016/j.jacc.2020.07.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Paoli A., Brischigliaro L., Scquizzato T., et al. Out-of-hospital cardiac arrest during the COVID-19 pandemic in the province of Padua. Northeast Italy Resuscitation. 2020;154:47–49. doi: 10.1016/j.resuscitation.2020.06.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.De Filippo O., D’Ascenzo F., Angelini F., et al. Reduced rate of hospital admissions for ACS during Covid-19 outbreak in northern Italy. N Engl J Med. 2020;383:88–89. doi: 10.1056/NEJMc2009166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.De Rosa S., Spaccarotella C., Basso C., et al. Reduction of hospitalizations for myocardial infarction in Italy in the COVID-19 era. Eur Heart J. 2020;41:2083–2088. doi: 10.1093/eurheartj/ehaa409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Giamello J.D., Abram S., Bernardi S., et al. The emergency department in the COVID-19 era. Who are we missing? Eur J Emerg Med. 2020;27:305–306. doi: 10.1097/MEJ.0000000000000718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Metzler B., Siostrzonek P., Binder R.K., et al. Decline of acute coronary syndrome admissions in Austria since the outbreak of COVID-19: the pandemic response causes cardiac collateral damage. Eur Heart J. 2020;41:1852–1853. doi: 10.1093/eurheartj/ehaa314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Piccolo R., Esposito G., et al. Population trends in rates of percutaneous coronary revascularization for acute coronary syndromes associated with the COVID-19 outbreak. Circulation. 2020;141:2035–2037. doi: 10.1161/CIRCULATIONAHA.120.047457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wilson S.J., Connolly M.J., Elghamry Z., et al. Effect of the COVID-19 pandemic on ST-segment-elevation myocardial infarction presentations and in-hospital outcomes. Circ Cardiovasc Interv. 2020 Jul;13(7) doi: 10.1161/CIRCINTERVENTIONS.120.009438. [DOI] [PubMed] [Google Scholar]
- 23.Tan W., Parikh R.V., Chester R., et al. Single center trends in acute coronary syndrome volume and outcomes during the COVID-19 pandemic. Cardiol Res. 2020;11:256–259. doi: 10.14740/cr1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zitelny E., Newman N., Zhao D. STEMI during the COVID-19 pandemic - an evaluation of incidence. Cardiovasc Pathol Sep-Oct. 2020;48:107232. doi: 10.1016/j.carpath.2020.107232. [Epub 2020 May 1] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Morelli N., Rota E., Terracciano C., et al. The baffling case of ischemic stroke disappearance from the casualty department in the COVID-19 era. Eur Neurol. 2020;83:213–215. doi: 10.1159/000507666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Onteddu S.R., Nalleballe K., Sharma R., et al. Underutilization of health care for strokes during the COVID-19 outbreak. Int J Stroke. 2020;15:NP9–NP10. doi: 10.1177/1747493020934362. [DOI] [PubMed] [Google Scholar]
- 27.Rinkel L.A., Prick J.C.M., Slot R.E.R., et al. Impact of the COVID-19 outbreak on acute stroke care. J Neurol. 2020 Jul 20:1–6. doi: 10.1007/s00415-020-10069-1. [Online ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gilbert E.H., Lowenstein S.R., Koziol-Mclain J., et al. Chart reviews in emergency medicine research: where are the methods? Ann Emerg Med. 1996;27:305–308. doi: 10.1016/s0196-0644(96)70264-0. [DOI] [PubMed] [Google Scholar]