Dear Editor,
The world is facing the pandemic of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), also known as COVID-19, this year. COVID-19 has shown various clinical presentations ranging from fever and dyspnea to seizures and other central nervous system (CNS) manifestations [[1], [2], [3]].
A 30-year-old man was admitted to Sina Hospital because of ataxia and confusion.
Four weeks prior to his admission, his father was hospitalized in an intensive care unit (ICU) with COVID-19, presenting with symptoms that included fever, coughing, and dyspnea. The patient was in direct contact with his father during this time. The father was discharged with total recovery two weeks before the patient's onset of symptoms.
The patient developed ataxia and confusion two days prior to his admission to Sina Hospital. His symptoms worsened gradually, but no falling, vertigo, hearing loss, tinnitus, or visual disturbances were reported. The patient reported he could stand and walk without help and had no fever, headache, diarrhea, coughing, or dyspnea. He had not used any medication for these symptoms.
The patient's past medical and medication histories were unremarkable, and the patient had been in his usual state of good health until the initiation of symptoms.
On physical examination, the patient had right side internuclear ophthalmoparesis and ataxic gait. Confusion was noted when patient attempted to answer the physician's questions. The patient also exhibited confabulation and repeated his words several times. No fever was detected, oxygen saturation was 98% without oxygen, and all other examinations were unremarkable.
The patient's laboratory data showed white blood cells: 10.44 (*103/μL) (normal range: 4–10.5), hemoglobin: 16.3 (gr/dl), CRP: 1 (mg/dl) (normal range: >6 mg/dl), and ESR: 13 (mm) (normal range: up to 18). Serum creatinine levels, sodium, potassium, TSH, and FT4 levels were within normal range as were his autoimmune panel and vasculitis tests.
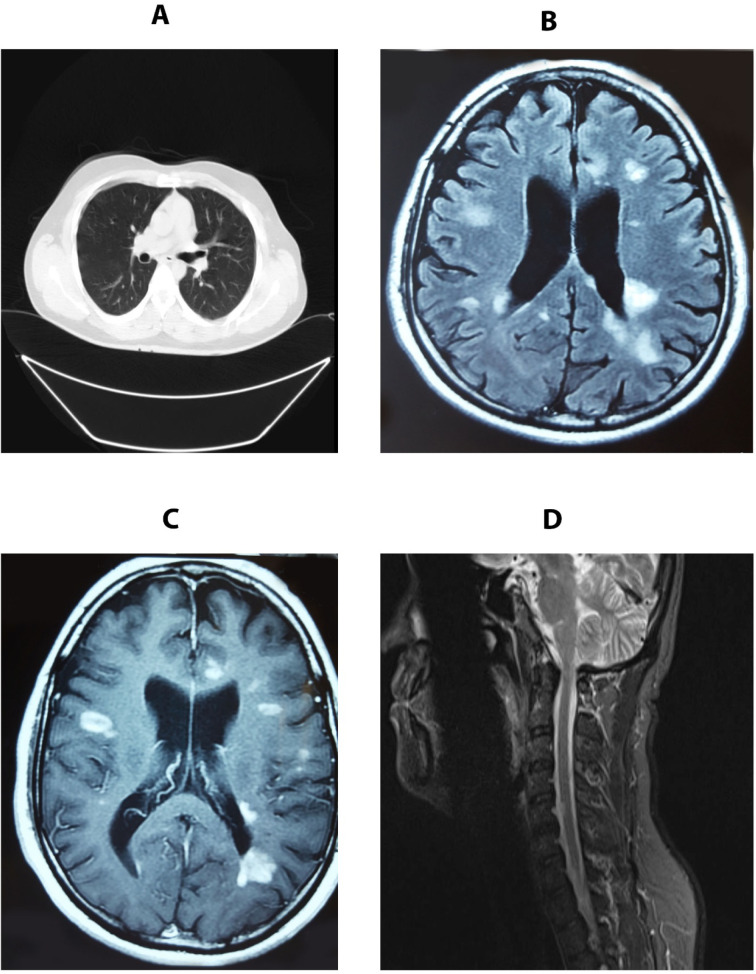
Due to the COVID-19 pandemic and the positive history of the patient's father, a diagnosis of neurological manifestation of COVID-19 was initially considered. A serologic test and a nasopharyngeal and oropharyngeal swab real-time polymerase chain reaction (rt-PCR) test for SARS-CoV-2 were performed. A chest computed tomography (CT) scan showed no pathologic lesions in favor of COVID-19 (Fig. 1 A). A brain magnetic resonance imaging (MRI) with and without gadolinium was also performed. The MRI showed multiple enhanced lesions suggestive of acute disseminated encephalomyelitis (ADEM) (Fig. 1 B & C). A cervical MRI without gadolinium showed a similar lesion (Fig. 1D).
Fig. 1.
A. Chest CT was normal. B & C. Brain MRI revealed multiple lesions with simultaneous enhancement. D. Cervical MRI revealed a plaque.
Due to the patient's confusion, a lumbar puncture was performed; the results showed a clear appearance, glucose: 58 mg/dl, protein: 45.7 mg/dl, WBC: 0, and RBC: 16 (mm3) as well as positive oligoclonal bands (OCBs). Additional tests showed negative anti-aquaporin antibody and negative myelin oligodendrocyte glycoprotein antibody (MOG-IgG) results.
Rt-PCR came back negative. The serologic test showed normal IgM levels and elevated IgG levels indicating a previous infection with SARS-CoV-2.
With diagnosis of acute disseminated encephalomyelitis (ADEM) secondary to COVID-19, treatment was begun with methylprednisolone pulse therapy 1 g intravenous (IV) daily for 5 days followed by rituximab 1 g IV. After the initiation of methylprednisolone, improvement in the patient's gait and mental status was obvious. The patient was discharged with relative recovery after 7 days.
In this study, a case of ADEM secondary to COVID-19 was demonstrated. Various studies have shown the neurological manifestations of COVID-19. A retrospective case series of 214 admitted patients by Mao et al. showed prevalence rates of 8% for impaired consciousness, 3% for acute cerebrovascular problems, and 0.5% for ataxia [4,5]. Viral infections can result in ADEM, and existing evidence points out that SARS-CoV-2 is no exception [6]. One study reported a complicated case of COVID-19; the patient was initially hospitalized for coronary surgical intervention but developed complications after surgery. The chest CT scan showed pulmonary involvement typical of COVID-19, and the patient tested positive for the mentioned disease. After 2 weeks of treatment, the patient died, and autopsy revealed multiple neuropathological injuries, both vascular and demyelinating. A perivascular acute disseminated encephalomyelitis (ADEM)-like appearance was also observed in the autopsy [7].
In the beginning of the spread of SARS-CoV-2 throughout the world, it was believed that this infection is primarily targeting the pulmonary system [8]. The importance of this study is the absence of pulmonary involvement, which complicates the diagnosis of COVID-19. The only clue in the current case was the serum IgG levels that were positive for SARS-CoV-2. Due to the current pandemic, COVID-19 should be considered as a differential diagnosis for patients with neurological symptoms, especially those with rare or bizarre manifestations.
Of course it can be argued that the association of COVID-19 infection and ADEM in this case might be a coincidence, but it is important to keep in mind that a cause-and-effect relationship is also a possibility.
Referencess
- 1.Shi Y., Wang G., Cai X.-P., Deng J.-W., Zheng L., Zhu H.-H., et al. An overview of COVID-19. J Zhejiang Univ Sci B. 2020:1. doi: 10.1631/jzus.B2000083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhou Z., Zhao N., Shu Y., Han S., Chen B., Shu X. Effect of gastrointestinal symptoms in patients With COVID-19. Gastroenterology. 2020;158(8):2294. doi: 10.1053/j.gastro.2020.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Abdi S., Ghorbani A., Fatehi F. The association of SARS-CoV-2 infection and acute disseminated encephalomyelitis without prominent clinical pulmonary symptoms. J Neurol Sci. 2020:416. doi: 10.1016/j.jns.2020.117001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mao L., Wang M., Chen S., He Q., Chang J., Hong C., et al. 2020. Neurological Manifestations of Hospitalized Patients with COVID-19 in Wuhan, China: A Retrospective Case Series Study. [Google Scholar]
- 5.Asadi-Pooya A.A., Simani L. Central nervous system manifestations of COVID-19: a systematic review. J Neurol Sci. 2020:116832. doi: 10.1016/j.jns.2020.116832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Marchioni E., Tavazzi E., Minoli L., Del Bue S., Ferrante P., Piccolo G., et al. Acute disseminated encephalomyelitis. Neurol Sci. 2008;29(Suppl. 2) doi: 10.1007/s10072-008-0966-6. (S286-8) [DOI] [PubMed] [Google Scholar]
- 7.Reichard R.R., Kashani K.B., Boire N.A., Constantopoulos E., Guo Y., Lucchinetti C.F. Neuropathology of COVID-19: a spectrum of vascular and acute disseminated encephalomyelitis (ADEM)-like pathology. Acta Neuropathol. 2020:1–6. doi: 10.1007/s00401-020-02166-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Koralnik I.J., Tyler K.L. COVID-19: a global threat to the nervous system. Ann Neurol. 2020;88(1):1–11. doi: 10.1002/ana.25807. [DOI] [PMC free article] [PubMed] [Google Scholar]