The retrospective study by Darvall and colleagues1 examined the impact of frailty on mortality among patients with (non-COVID-19) pneumonia admitted for intensive care. The authors commented that clinical frailty score (CFS) alone is not useful for guiding the allocation of critical care resources because lesser degrees of frailty (CFS 5–6) were not associated with mortality.1 Whether the findings could be extended to patients with coronavirus disease 2019 (COVID-19) is unknown. Many researchers have sought to determine if frailty predicts poor prognosis in hospitalised patients with COVID-19. We aim to summarise the available evidence from observational studies through meta-analysis regarding the association between frailty and mortality in patients with COVID-19.
We performed a comprehensive literature search in electronic databases that included PubMed, Scopus, Google Scholar, and preprint repositories (medRxiv and Research Square) from December 1, 2019 to November 26, 2020, using the following keywords: ‘COVID-19’ or ‘SARS-CoV-2’ or ‘severe acute respiratory syndrome coronavirus 2’ and ‘frailty’ or ‘frail’ with no language restriction. The reference lists of relevant articles were also hand-searched for additional studies.
Studies eligible for inclusion were those with observational study design, included patients aged 18 yr or older, with a positive diagnosis of COVID-19, assessed frailty with any validated frailty assessment tools, and reported mortality as related to frailty in acute hospital settings. We excluded studies without any adjustment of potential confounders for the measures of association between frailty and mortality, and article types such as comments, narrative reviews, conference papers, and case reports without reporting original data.
After removing duplicates, a pair of reviewers (CSK and SSH) independently reviewed the titles and full-text articles to identify articles potentially meeting eligibility criteria. Full-text screening was used to identify a final list of studies that met the inclusion and exclusion criteria. If multiple studies were available from the same cohort of patients, the study with the largest sample was included in the review. Two investigators (CSK and SSH) independently extracted relevant data from included studies: family name of the first author, publication year, study design, study setting (single centre, multicentre, or database review), age of participants, sample size, prevalence of frailty, frailty assessment scale, rate of mortality in patients with frailty, and adjusted effect size for the association between frailty and mortality. Two investigators (CSK and SSH) independently appraised the quality of observational studies using the Newcastle–Ottawa Scale with scores of >7 indicating high quality.
Disagreement between the two reviewers related to the inclusion of studies, extraction of data, and quality appraisal of included studies was resolved through discussions with the third investigator (KT). We used a random-effects model to estimate the association between frailty and mortality, with the results presented as pooled odds ratio or pooled hazard ratio and 95% confidence interval. For studies that presented independent effect measure of mortality with different categories of frailty score, we first pooled the effect measures in a single study before including the pooled effect measure for each study in the meta-analysis. We examined heterogeneity between studies using the I 2 statistic with 50% and using the χ2 test with P<0.10, as the thresholds for statistically significant heterogeneity.
We retrieved 598 records from the combination of two independent searches. After removing duplications and irrelevant records, 25 full-text articles were assessed for eligibility. A total of 14 studies that met the inclusion and exclusion criteria were included for further analysis. Supplementary Table S1 depicts the characteristics of included studies (including the full reference list). Of the 14 included studies, six studies presented hazard ratios of mortality with different categories of frailty score (Clinical Frailty Scale), four studies presented odds ratio of mortality per unit increase in frailty score (Clinical Frailty Scale), two studies presented odds ratios of mortality with different categories of frailty score (Clinical Frailty Scale and Hospital Frailty Risk Score), and two studies presented hazard ratio of mortality per unit increase in frailty score (Clinical Frailty Scale). Therefore, we could only pool in two separate meta-analyses, the hazard ratios of mortality with different categories of frailty score from six available studies2, 3, 4, 5, 6, 7 and the odds ratio of mortality per unit increase in frailty score from four available studies.8, 9, 10, 11
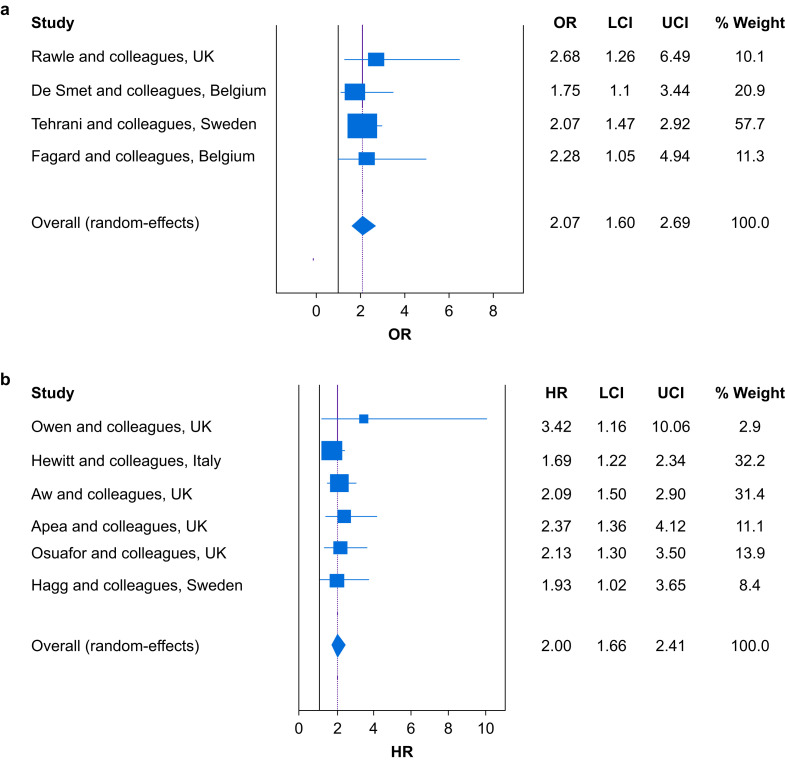
Of the six studies2, 3, 4, 5, 6, 7 that presented hazard ratios of mortality with different categories of Clinical Frailty Scale, five studies2, 3, 4, 5, 6 originated from the United Kingdom (UK) (inclusive of one study that included patients from both the UK and Italy), whereas the remaining one study7 originated from Sweden. Only two studies3 , 5 were of prospective multicentre design, whereas the remaining four studies2 , 4 , 6 , 7 were of retrospective single-centre design. The meta-analysis of six studies2, 3, 4, 5, 6, 7 that represented data from 3,824 patients with COVID-19 revealed that frailty status as determined using Clinical Frailty Scale was associated with a significantly higher hazard of mortality in patients with COVID-19 (Fig. 1 b; pooled hazard ratio=2.00; 95% confidence interval, 1.66–2.41), regardless of degree of frailty (mild, moderate, or severe).
Fig 1.
(a) Pooled odds ratio of mortality per unit increase in Clinical Frailty Scale among patients with COVID-19. (b) Pooled hazard ratio of mortality in frail patients with COVID-19 compared with non-frail patients with COVID-19. COVID-19, coronavirus disease 2019; OR, odds ratio; HR, hazard ratio; LCI, lower confidence limit; UCI, upper confidence limit.
Of the four studies8, 9, 10, 11 that presented the odds ratio of mortality per unit increase in Clinical Frailty Scale, two studies9 , 11 originated from Belgium, whereas the remaining two studies8 , 10 originated from the UK and Sweden. All studies were of single-centre design: three studies8 , 9 , 11 were retrospective whereas one study10 was prospective. The meta-analysis of four studies8, 9, 10, 11 that represented data from 463 patients with COVID-19 revealed that per unit increase in frailty score as determined using Clinical Frailty Scale was associated with a significantly higher odds of mortality in patients with COVID-19 (Fig. 1a; pooled odds ratio=2.07; 95% confidence interval, 1.60–2.69).
Studies that were not included in meta-analyses also demonstrated a significant association between frailty status (regardless of degrees of frailty) and higher odds of mortality, and significant association between increasing level of frailty and a higher hazard of mortality. Our findings indicate that increased risk of mortality spanned the continuum of frailty in patients with COVID-19, and hence Clinical Frailty Scale or other validated frailty assessment tools can be useful in prioritising allocation of critical care resources for patients with COVID-19.
Declarations of interest
The authors declare that they have no conflict of interest.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.bja.2020.12.002.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Darvall J.N., Bellomo R., Bailey M. Frailty and outcomes from pneumonia in critical illness: a population-based cohort study. Br J Anaesth. 2020;125:730–738. doi: 10.1016/j.bja.2020.07.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Owen R.K., Conroy S.P., Taub N. Comparing associations between frailty and mortality in hospitalised older adults with or without COVID-19 infection: a retrospective observational study using electronic health records. Age Ageing. July 17 2020 doi: 10.1093/ageing/afaa167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hewitt J., Carter B., Vilches-Moraga A. The effect of frailty on survival in patients with COVID-19 (COPE): a multicentre, European, observational cohort study. Lancet Public Health. 2020;5:e444–e451. doi: 10.1016/S2468-2667(20)30146-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Aw D., Woodrow L., Ogliari G., Harwood R. Association of frailty with mortality in older inpatients with Covid-19: a cohort study. Age Ageing. 2020;49:915–922. doi: 10.1093/ageing/afaa184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Apea V.J., Wan Y.I., Dhairyawan R. Ethnicity and outcomes in patients hospitalised with COVID-19 infection in East London: an observational cohort study. medRxiv. June 12 2020 doi: 10.1101/2020.06.10.20127621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Osuafor C.N., Davidson C., Mackett A.J. Clinical features and inpatient trajectories of older inpatients with COVID-19: a retrospective observational study. Res Square. August 26 2020 doi: 10.21203/rs.3.rs-61056/v1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hägg S., Jylhävä J., Wang Y. Age, frailty, and comorbidity as prognostic factors for short-term outcomes in patients with coronavirus disease 2019 in geriatric care. J Am Med Dir Assoc. 2020;21 doi: 10.1016/j.jamda.2020.08.014. 1555–1559.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rawle M.J., Bertfield D.L., Brill S.E. Atypical presentations of COVID-19 in care home residents presenting to secondary care: a UK single centre study. Aging Med. September 17 2020 doi: 10.1002/agm2.12126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.De Smet R., Mellaerts B., Vandewinckele H. Frailty and mortality in hospitalized older adults with COVID-19: retrospective observational study. J Am Med Dir Assoc. 2020;21 doi: 10.1016/j.jamda.2020.06.008. 928–932.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tehrani S., Killander A., Åstrand P., Jakobsson J., Gille-Johnson P. Risk factors for mortality in adult COVID-19 patients; frailty predicts fatal outcome in older patients. Int J Infect Dis. 2021;102:415–421. doi: 10.1016/j.ijid.2020.10.071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fagard K., Gielen E., Deschodt M., Devriendt E., Flamaing J. Risk factors for severe COVID-19 disease and death in patients aged 70 and over: a retrospective observational cohort study. Res Square. November 3 2020 doi: 10.21203/rs.3.rs-101387/v1. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.