Abstract
Introduction
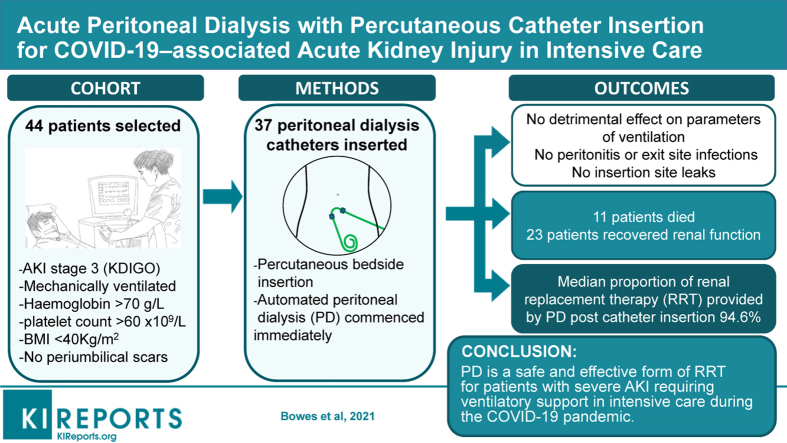
During the coronavirus disease 2019 (COVID-19) pandemic in 2020, high rates of acute kidney injury (AKI) in critically unwell patients are being reported, leading to an increased demand for renal replacement therapy (RRT). Providing RRT for this large number of patients is proving challenging, and so alternatives to continuous renal replacement therapies (CRRT) in the intensive care unit (ICU) are needed. Peritoneal dialysis (PD) can be initiated immediately after percutaneous insertion of the catheter, but there are concerns about impact on ventilation and RRT efficacy. We sought to describe our recent experience with percutaneous catheter insertion and peritoneal dialysis in patients in the ICU with COVID-19 infection.
Method
Patients were selected according to local protocol, and catheters were inserted percutaneously by experienced operators using a Seldinger technique. Sequential Organ Failure Assessment (SOFA) score and ventilation requirements were recorded at the time of insertion and 24 hours later. Procedural complications, proportion of RRT provided by PD, renal recovery, and RRT parameters (serum potassium and maximum base excess) during PD were assessed.
Results
Percutaneous PD catheters were successfully inserted in 37 of 44 patients (84.1%) after a median of 13.5 days (interquartile range [IQR] = 10.0, 20.3 days) in the ICU. No adverse events were reported; SOFA scores and ventilation requirements were comparable before and after insertion; and adequate RRT parameters were achieved. The median proportion of RRT provided by PD following catheter insertion was 94.6% (IQR = 75.0, 100%).
Conclusion
Peritoneal dialysis provides a safe and effective alternative to CRRT in selected patients with AKI and COVID-19 infection requiring ventilation on intensive care.
Keywords: acute kidney injury, COVID-19, percutaneous catheter insertion, peritoneal dialysis
Graphical abstract
In late December 2019, in Wuhan, Hubei, China, a new infectious respiratory syndrome emerged with clinical signs resembling viral pneumonia. The infective agent has been identified as a novel coronavirus called severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) causing COVID-19. It spread rapidly around the globe and was defined as a pandemic by the World Health Organization on 11 March 2020.1 Although most clinical presentations are mild, a substantial proportion of individuals affected require hospitalization and support within intensive care.2
Worldwide, the number of COVID-19 patients with AKI has been reported to be between 5% and 49%,3,4 with variability likely accounted for by variation in case mix, AKI definition, and geographic location. Data from 9505 COVID-19 patients in England, Wales, and Northern Ireland who were admitted to the ICUs up to 26 June 2020 showed that 26% required RRT, compared to 17% of patients admitted with non−COVID-19 viral pneumonia in 2017 to 2019 (n = 5626).5 Outside of pneumonia (with or without cardiovascular support), AKI is the most frequently encountered serious complication of infection with the SARS-CoV-2 virus.
These high rates of AKI have led to a critical and unpredicted shortage of resources for CRRT such as continuous veno-venous hemofiltration and hemodiafiltration (CVVHF/CVVHDF), both machine and consumable. Intermittent hemodialysis (IHD) is also sometimes used for RRT in the ICU but is reliant upon adequate numbers of highly skilled staff and appropriate infrastructure and/or machines to supply ultrapure water. If transferable solutions are not found that are suitable for both high- and low-income settings, this may lead to premature death from a potentially reversible condition for many patients as this pandemic spreads around the globe.
PD is rarely used to manage patients with AKI in high-resource settings, despite international guidelines recommending it as an appropriate alternative to CVVHF6 and evidence suggesting that PD provides outcomes comparable to those of IHD and CVVHF in critically ill patients with AKI.7, 8, 9 Acute PD is estimated to cost 50% less than CVVHF and can be delivered in settings without hemodialysis facilities following ICU discharge.10 There are no anticoagulation requirements; line-related problems are minimized (as PD catheters usually do not need to be changed); and solute removal is gradual, with less potential for hemodynamic compromise. In addition, nursing burden associated with anticoagulation, electrolyte replacement, and filter management is reduced.11
However, considerable concerns exist about the utility and safety of PD, which have resulted in very low uptake of this form of RRT in the ICU. The regulation of fluid balance is less predictable than with CVVHF; dialysis adequacy may be variable; and peritoneal infection and compromised ventilation due to diaphragmatic restriction are potential risks. Moreover, there may be substantial challenges involved in delivering PD in patients who are ventilated in the prone position; intra-abdominal pressure may be increased, risking compartment syndrome; and the effectiveness of PD in patients in the prone position is untested. In addition, insertion of PD catheters under local anesthesia requires good bowel preparation and an experienced operator.
At our center, we have an experienced PD team and have been providing urgent-start PD to patients with both AKI and chronic kidney disease for many years. Here we describe an audit of our experience to date of acute PD for treatment of AKI in patients in the ICU during the COVID-19 pandemic in a setting where CVVHDF resources became limited.
Materials and Methods
All patients had a proven diagnosis of COVID-19 and were intubated and ventilated on an ICU ward at King’s College Hospital, London, UK. They were assessed by trained PD nurses or doctors, and were considered to be suitable for bedside catheter insertion if the following criteria were met: AKI stage 3 (Kidney Disease: Improving Global Outcomes [KDIGO] criteria); hemoglobin >70 g/l; platelet count >60 × 109/l; activated partial thromboplastin time ratio (APTR) <1.9; international normalized ratio (INR) <1.3; no previous major abdominal surgery, particularly with scars by the umbilicus; estimated body mass index <40 kg/m2; no significant abdominal wall distension due to constipation or flatus; and fraction of inspired oxygen (Fi O2) <0.6.
Bowel preparation included 2 sachets of CitraFleet (containing light magnesium oxide, sodium picosulfate, citric acid; Casen Recordati, S.L., Zaragoza, Spain) each in 200 ml of water, 4 hours apart (at least 15 hours prior to procedure). Antibiotic prophylaxis of 1 g vancomycin was given i.v., 1 to 4 hours before, unless the patient was already receiving broad-spectrum antibiotics. Anticoagulation for CVVHDF or thromboprophylaxis was stopped 12 hours prior to catheter insertion. All patients had urinary catheters in situ.
Insertion was performed at the bedside and according to International Society of Peritoneal Dialysis guidelines.6
Kimal double-cuffed silicone and bent-necked pig-tailed PD catheters (57-, 62-, or 63-cm catheters depending on patient size) were inserted by medical or nursing staff using a blind Seldinger technique. After instillation of local anaesthetic (xylocaine 2% with adrenaline 1:200,000), a midline transverse incision was made below the umbilicus, and a pocket was made in the abdominal fat for the proximal catheter cuff and bent neck. A Seldinger guide wire was inserted through the linea alba into the peritoneal cavity via an 18-gauge needle. A dilator with a peel-away sheath was inserted over the wire and the catheter was introduced. Ultrasound guidance was used for more challenging cases with abdominal obesity.
In contrast to our usual practice, a decision was made to tunnel the catheter laterally with the exit site lateral and inferior to the incision, >3 cm beyond the distal Dacron cuff to allow for PD to be delivered to prone patients should it become necessary. This would increase ease of access to the catheter and would decrease the risk of catheter-related pressure areas developing in prone patients.
Blood tests were conducted by local hospital laboratory or point-of-care analysis according to standardized protocols.
A 3-phase PD prescription protocol was developed (Table 1), commencing with low-volume rapid exchanges in the first 24 to 48 hours after catheter insertion to minimize the risk of leak at the insertion site but to maximize fluid loss if required. The choice of prescription used thereafter depended upon clinical assessment by the renal consultant in partnership with the ICU consultant of the patient, including fluid balance, ultrafiltration (UF) goal, electrolyte status, and degree of uremia. Automated cyclers (Baxter Claria; Baxter, Thetford, United Kingdom and Homechoice machines) were used in all cases.
Table 1.
Peritoneal dialysis prescription protocol for first 3 sessions
| PD prescription parameters | Phase 1 | Phase 2 | Phase 3 |
|---|---|---|---|
| PD modality | Tidal or CCPD/IPD | CCPD/IPD | CCPD/IPD |
| Total treatment time, h | 12–18 | 12–16 | 12–16 |
| Total volume, ml | 20,000–30,000 | 20,000–30,000 | 15,000–25,000 |
| Fill volume, ml | 1200–1600 | 1500–2000 | 1500–2500 |
| Last fill volume, ml | 0 | 0 | 1000–1500 |
| Cycles | 9–14 | 9–20 | 9–20 |
| Dwell time, min | 20–39 | 30–75 | 30–75 |
| Dialysis solution | Dextrose concentration according to UF required | Dextrose concentration according to UF required | Dextrose concentration according to UF required; extraneal (icodextrin 7.5%) for final fill |
CCPD, continuous cyclic peritoneal dialysis; IPD, intermittent peritoneal dialysis; PD, peritoneal dialysis; UF, ultrafiltration.
Data were extracted from electronic and paper records. Outcome measures reported included the following: procedure-related complications, days of catheter function, renal recovery, and RRT parameters (serum potassium, urea, and maximum base excess up to 14 days). Laboratory parameters for patients receiving CVVHDF in addition to PD were not included in the analysis. The SOFA score and lowest PaO2:FiO2 ratio (i.e., arterial oxygen partial pressure:fractional inspired oxygen concentration) during 24 hours before and after insertion were recorded.
Patient mortality, proportion of patients with renal recovery (defined as RRT independence) and time to renal recovery, and total length of ICU stay (at time of writing, excluding deaths) were reported. Descriptive statistics were used for baseline demographics, clinical characteristics, laboratory parameters, and outcome measures.
The audit was registered at King’s Kidney Care in accordance with local governance processes (KKC/KCH/COVID/002).
Results
A total of 44 PD catheter insertions were attempted between 31 March 2020 and 30 May 2020 in patients who had been admitted to the ICU with COVID-19 and who required RRT. Demographics, clinical characteristics, and treatment of selected patients are shown in Table 2. The majority of patients were male, were Black, and had a history of hypertension, and many had diabetes. Six patients (13.6%) did not receive CVVHDF prior to catheter insertion. Patients receiving CVVHDF were identified for a switch to PD to conserve CVVHDF resources if they met the selection criteria described above.
Table 2.
Baseline characteristics of patients with attempted catheter insertions (n = 44)
| Characteristic | Value |
|---|---|
| Median age, yr (IQR) | 60 (55.0−64.0) |
| Male sex, n (%) | 35 (79.5) |
| Ethnicity, n (%) | |
| White | 8 (18.2) |
| Black | 26 (59.1) |
| Asian | 4 (9.1) |
| Other or mixed ethnic group | 6 (13.6) |
| Previous abdominal surgery | 3 (6.8) |
| Median body mass index (IQR) | 27.7 (23.3−31.8) |
| Comorbidities | |
| Diabetes, n (%) | 20 (45.5) |
| Hypertension, n (%) | 30 (68.2) |
| Cardiovascular disease, n (%) | 10 (22.7) |
| Median laboratory parameters at time of catheter insertion (IQR) | |
| Creatinine, μmol/l | 389 (220−475) |
| Urea, mmol/l | 24.6 (13.9−28.5) |
| Hemoglobin, g/dl | 79.0 (77.0−89.0) |
| Platelet count, ×109 /l | 270 (185−405) |
| APTTR | 1.3 (1.1−1.5) |
| INR | 1.1 (1.0−1.1) |
| Base excess | –1.4 (–4.9 to 0.4) |
| Median no. of days admission to ICU (IQR) | 13.5 (10.0−20.3) |
| Median SOFA score at time of catheter insertion | 16.0 (15.0−17.0) |
| Organ support prior to PD catheter insertion, n (%) | |
| Ventilation | 44 (100) |
| Median lowest PaO2:FiO2 ratio (n = 27) | 22.0 (17.0−29.5) |
| Vasopressorsa | 26 (61.9) |
| Median maximal dose of norepinephrinea, μg/kg per min | 0.14 (0.08−0.22) |
| CVVHDF | 39 (88.6) |
| Median no. of days of CVVHDF (IQR) | 9.0 (4.3−13.8) |
| Tracheostomy | 13 (29.5) |
APTTR, activated partial thromboplastin ratio; CVVHDF, continuous veno-venous hemodiafiltration; ICU, intensive care unit; INR, international normalized ratio; IQR, interquartile range; PD, peritoneal dialysis; SOFA, Sequential Organ Failure Assessment.
n = 42 (2 missing).
Five catheter insertions were unsuccessful because of abdominal obesity and failure to reach the peritoneum using a 50-mm needle. One catheter insertion attempt was abandoned because of complications from omental obstruction, and another was abandoned because of suspicion of needle puncture of the bowel. This latter patient remained stable with no features of intra-abdominal infection or bleeding; insertion was attempted for a second time the following day but was again unsuccessful because of an inability to advance the guidewire. There were no cases of bladder injury, hemorrhage, catheter-associated leaks, or exit site or peritoneal infections. Peritoneal dialysis was abandoned in 1 patient who developed a leak into a scrotal hernia.
The SOFA scores and lowest PaO2: FiO2 ratios within 24 hours before and after commencement of PD are shown in Table 3. There were no cases of PD therapy suspension because of concerns over ventilation adequacy. Two patients were proned, and clinician preference at the time was to switch them to CRRT. Peritoneal dialysis in the prone position was therefore not attempted, despite the lateral tube placement. Some organ support parameters are missing for 4 patients because of challenges in retrospectively locating components of paper charts in temporary COVID-19 ICU wards.
Table 3.
Clinical parameters of patients prior to and after peritoneal dialysis catheter insertion
| Parameter, median (IQR) n = 36a | 24 h Before PD catheter insertion | 24 h after PD catheter insertion |
|---|---|---|
| Lowest PaO2: FiO2 ratio | 22.0 (18.3−29.8) | 22.5 (18.5−31.0) |
| SOFA score | 16.0 (15.0−17.0) | 16.0 (15.0−17.0) |
| Requirement for vasopressor support, n (%) | 21 (58.3) | 18 (50.0) |
| Median maximal dose of norepinephrine, μg/kg per min | 0.14 (0.08−0.23) | 0.13 (0.01−0.31) |
IQR, interquartile range; PaO2:FiO2 ratio (arterial oxygen partial pressure [PaO2 in mm Hg] to fractional inspired oxygen [FiO2 expressed as a fraction]); PD, peritoneal dialysis; SOFA, Sequential Organ Failure Assessment.
One case missing because of paper notes used in new intensive care facility.
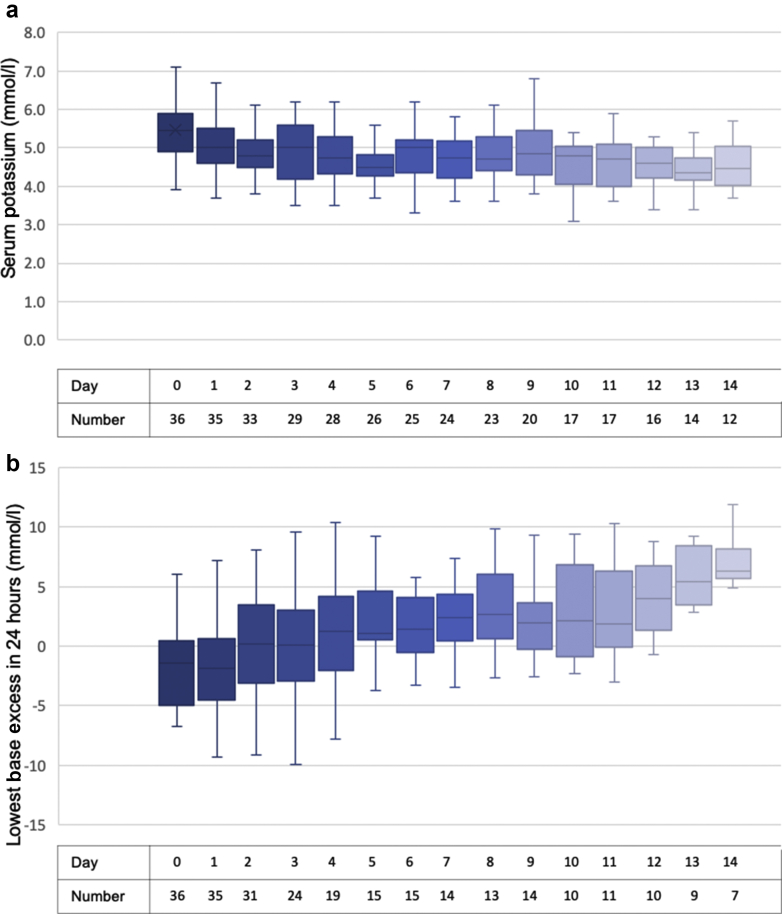
The RRT laboratory parameters in patients receiving PD exclusively from catheter insertion day to 30 May 2020 are presented in Figure 1a and b. The median urea of patients receiving PD exclusively was 26.9 mmol/l (IQR = 26.0−28.8), and the median UF achieved per PD session was 878 ml (IQR = 348−1467). In all, 27 of the 37 patients (73%) established on PD were receiving PD at the time of their renal recovery or death. Ten patients (27.0%) were switched to CRRT or IHD without returning to PD; 3 of these patients were deteriorating rapidly from multi-organ failure, and CRRT was believed to be more appropriate; another 3 patients were switched because of ICU clinician preference and increased availability of CRRT. Other reasons for switching included proning (n = 1), scrotal leak (n = 1), and abdominal pain (n = 1, PD peritonitis excluded), and 1 patient pulled out their PD tube while delirious following extubation. There were a further 16 temporary episodes of alternative RRT before returning to PD. The primary indications were ICU clinician preference (n = 8), temporary bowel issues causing poor flows (n = 3), to reduce urea prior to surgical tracheostomy (n = 2; urea <30 mmol/l cut-off protocol for surgery was increased to <40 mmol/l in mid-April), proning (n = 1), acidosis (n = 1), and hyperkalaemia (n = 1). The median duration of these temporary episodes was 48 hours (IQR = 24−72). At the time of switching from PD to CRRT or IHD, the median potassium was 5.4 mmol/l (IQR = 4.7−6.1) and median base excess 1.3 (IQR −2.8 to 2.1).
Figure 1.
(a) Serum potassium and (b) lowest base excess in patients with coronavirus disease 2019 (COVID-19) infection receiving acute peritoneal dialysis. Data are shown for patients on days in which they exclusively received peritoneal dialysis until renal recovery, death, or recommenced continuous veno-venous hemodiafiltration up to 14 days. The upper edge of each bar corresponds to the 75th percentile, the bottom edge to the 25th percentile; the central line represents the median, and the cross represents the mean. The whiskers are the highest and lowest values per day. The number of samples per day are shown in the table below the box plot.
Patient outcomes are reported in Table 4. In all, 11 of the 37 patients (29.7%) with PD catheter insertions died after a median of 9 days (range = 3−34 days) postinsertion, of multi-organ failure (n = 10) and stroke (n = 1); 5 of these patients received PD as their sole RRT modality (45%). A total of 23 patients (85.2%) recovered renal function, 11 of whom received PD as their sole RRT modality following catheter insertion (48%). As of 30 May 2020, 2 patients remained on ICU on CVVHDF (both have subsequently died), and 1 patient remained on PD (this patient has subsequently recovered renal function and has been discharged from the hospital). Of 37 patients, 16 (43%) received PD as their sole form of RRT.
Table 4.
Patient and Peritoneal Dialysis Catheter Outcomes for Patients with Successful Insertions
| Outcome (n = 37) | Value |
|---|---|
| Death, n (%) | 11 (29.7) |
| Median PD catheter in situ per patient, days (IQR) | 9.0 (7.0−20.0) |
| Median PD catheter use per patient, days (IQR) | 8.0 (6.0−16.0) |
| Median proportion of RRT provided by PD after insertion, % (IQR) | 94.6 (75.0−100) |
| Discharge from ICU, n (%) | 26 (70.3) |
| Median total length of stay in ICU, daysa (IQR) | 49.0 (29.0−62.8) |
| Renal recovery during study period, n (%)b | 23 (85.2) |
| Median time to renal recovery, days (IQR) | 12.0 (8.5−18.0) |
ICU, intensive care unit; IQR, interquartile range; PD, peritoneal dialysis.
n = 26 (Including 26 discharged, excluding 11 deaths).
n = 27 (Including 1 patient who had renal recovery before death, excluding 10 deaths).
Discussion
Major Findings
We report our initial experience of performing acute PD following bedside percutaneous catheter insertion in a tertiary critical care setting for patients with COVID-19 infection and AKI. Peritoneal dialysis catheter insertion was successful in the majority of selected patients without apparent ventilatory or hemodynamic compromise or insertion-related complications. The PD provided effective RRT in nearly all patients achieving stable correction of hyperkalemia, acidosis, and fluid balance. Although many patients received CVVHDF prior or subsequent to the commencement of PD, 43% received PD as their sole form of RRT.
Comparison to Other Studies
Safety of Catheter Insertion
Although others have reported the use of PD during the COVID-19 pandemic,12, 13, 14 our study is the largest to date and the only one to describe bedside percutaneous catheter insertion (as opposed to open or laparoscopic surgical insertion). In our study, no complications leading to significant harm were reported following catheter insertion, even in patients with failed catheter insertion attempts. Bowel and bladder injury are described in both blind and direct insertion,15 but did not occur other than a potential needle insertion into the bowel without adverse consequences. Although abdominal obesity was the most common limitation to catheter insertion, we have found that the use of ultrasound guidance can increase success, aiding judgment regarding needle insertion depth beyond the linea alba and visualization of the needle tip, wire, and fluid during the procedure. We suggest therefore that PD insertion can be safely attempted in an ICU setting in patients with abdominal obesity, when pre- and intraprocedural ultrasound, supported by interventional radiologists, may enhance success of insertion.
Impact on Ventilation
Severe COVID-19 infection is commonly associated with respiratory compromise due to direct viral injury and inflammatory response. The volume of PD fluid in the peritoneal cavity could further reduce functional residual capacity and lead to impaired ventilatory dynamics. A study of healthy continuous ambulatory PD patients reported a reduction in expiratory reserve volume and functional residual capacity, but inspiratory capacity increased when the abdomen was full.16 Although these findings will not be directly generalizable to patients who are supine, we did not find any evidence of immediate respiratory compromise after commencing acute PD, although we recognize the limitation of the small number of patients studied.
Two patients required prone position ventilation for refractory hypoxemia and, because of ICU clinician preference, PD was not attempted while patients were proned. However, catheter exit site position can be adapted to reduce pressure on the tube and exit site, and we consider that PD remains an option in patients who are ventilated in the prone position, based on a previous case report.17 One potential risk of PD in the prone patient is abdominal compartment syndrome, resulting in reduced perfusion to abdominal viscera. For this reason, we planned to transduce the intra-abdominal pressure through a urinary bladder catheter in proned patients, aiming to keep intra-abdominal pressure to <20 mm H2O, but this eventuality did not arise. In ventilated patients, measurement of transpulmonary pressure may add to safety, if intra-abdominal pressure is increased, because safe driving pressure can be maintained even if chest wall compliance is affected by PD fluid volume. In patients who are breathing spontaneously in pressure support, neutrally adjusted ventilator assist may be a safer mode, as the patient will self-adjust tidal volumes. The effects of PD on ventilation therefore requires further study, especially in proned patients.
Efficacy
Measures of dialysis adequacy have not been established for acute PD in patients with COVID-19. We report that hyperkalemia, acidosis, and fluid balance were adequately managed with PD treatment, but we were unable to quantify formal dialysis clearance with Kt/V because of staffing pressures and resource limitations. In our experience, there was initial anxiety about inadequate solute clearance, particularly in hypercatabolic patients or those with splanchnic hypoperfusion or on vasopressors. When patients established on PD were switched to other RRT modalities, either permanently or temporarily, the indication on the majority of occasions was related to clinician preference rather than PD “failure.” We recognize that the familiarity, clarity, and titratable nature of CVVHDF makes it an attractive treatment option when resources allow, despite adequate UF via PD in the previous 24 hours. With regard to fluid balance, enhanced UF was achieved via the use of high-dextrose dialysate concentrations on a case-by-case basis. Many patients, however, were not fluid overloaded and were therefore prescribed low-dextrose dialysate solutions, resulting in minimal or negative UF volumes.
Previous studies have reported that acute PD leads to earlier renal recovery in patients with AKI when compared with daily hemodialysis.18 At the end of the study period, more than 40% of our patients on acute PD had recovered renal function, but the numbers are too small and the mix of RRT modalities too complex to draw any conclusions from our data. It is worth noting that patients with COVID-19 have a high incidence of thromboembolic complications, which often leads to early clotting of CVVHDF circuits, necessitating anticoagulation.19 Patients who do not otherwise require systemic anticoagulation may therefore benefit from PD as opposed to CRRT.
Implications for Practice
Continuous renal replacement therapy (CRRT) has been available since the late 1970s, and, more recently, continuous veno-venous hemofiltration (CVVH) or hemodiafiltration (CVVHDF) has become the method of choice for treatment of AKI in the high-resource ICU setting.20 Although access to CRRT has been limited in low-resources settings, intensive care units in the United Kingdom and United States have never before been faced with the overwhelming numbers of patients presenting with AKI and the logistical burden of providing consumables such as hemofiltration sets and replacement fluid.
In recognition of this dilemma, the responsibility to provide RRT in the COVID-19 pandemic is increasingly being run in a collaborative manner with renal services. Alternatives to CRRT are being continuously developed at pace including methods of IHD such as slow, low-efficiency daily dialysis (SLEDD), but these require the installation of new infrastructure and cannot provide capacity quickly. Although nephrologists regularly manage patients with end-stage kidney disease with PD, there is little experience treating patients with AKI and even less in treating very unwell, ventilated patients. In addition, PD catheter insertion is most frequently undertaken by surgeons under direct vision, making local anaesthetic, Seldinger technique an infrequent skill within modern nephrology.
We recognize that our results are preliminary and from a single center with local expertise. They are also observational, and we were unable to compare outcomes to those in patients receiving other forms of RRT because of patient selection bias. However, we believe that they are sufficient to increase confidence in the use of PD in the ICU setting during times of crisis, offering an alternative to more traditional forms of CRRT.
In conclusion, we suggest that PD is a safe and effective form of RRT for patients with severe AKI requiring ventilatory support in the ICU during the COVID-19 pandemic, when resources for CVVHDF are in short supply.
Disclosure
All the authors declared no competing interests.
Acknowledgments
We acknowledge the contribution of all the King’s Kidney Care and Intensive Care Teams, especially Sunita Ghoorbin, Alison McCarthy, Dawn Bennett, Chris Clarke, Magda Valencia Reyes, Kirsten English Gilmari Lontoc, Kieran Palmer, Will Atkins, and Fatima Jumah. We would also like to acknowledge the help and advice received from Brett Cullis, Pietermaritzburg, South Africa, and Mignon McCulloch, University of Cape Town, South Africa.
References
- 1.European Centre for Disease Prevention and Control: situation update worldwide. https://www.ecdc.europa.eu/en/geographical-distribution-2019-ncov-cases Available at:
- 2.Huang D., Lian X., Song F. Clinical features of severe patients infected with 2019 novel coronavirus: a systematic review and meta-analysis. Ann Transl Med. 2020;8:576. doi: 10.21037/atm-20-2124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cheng Y., Luo R., Wang K. Kidney disease is associated with in-hospital death of patients with COVID-19. Kidney Int. 2020;97:829–838. doi: 10.1016/j.kint.2020.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pelayo J., Lo K.B., Bhargav R. Clinical characteristics and outcomes of community- and hospital-acquired acute kidney injury with COVID-19 in a US inner city hospital system. Cardiorenal Med. 2020;10:1–9. doi: 10.1159/000509182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Intensive Care National Audit and Reporting Centre: ICNARC COVID-19 reports. 2020. https://www.icnarc.org/Our-Audit/Audits/Cmp/Reports Available at: [Google Scholar]
- 6.Cullis B., Abdelraheem M., Abrahams G. Peritoneal dialysis for acute kidney injury. Perit Dial Int. 2014;34:494–517. doi: 10.3747/pdi.2013.00222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Almeida C.P., Balbi A.L., Ponce D. Effect of peritoneal dialysis vs. hemodialysis on respiratory mechanics in acute kidney injury patients. Clin Exp Nephrol. 2018;22:1420–1426. doi: 10.1007/s10157-018-1598-7. [DOI] [PubMed] [Google Scholar]
- 8.Liu L., Zhang L., Liu G.J. Peritoneal dialysis for acute kidney injury. Cochrane Database Syst Rev. 2017;12:CD011457. doi: 10.1002/14651858.CD011457.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ponce D., Brabo A.M., Balbi A.L. Urgent start peritoneal dialysis. Curr Opin Nephrol Hypertens. 2018;27:478–486. doi: 10.1097/MNH.0000000000000451. [DOI] [PubMed] [Google Scholar]
- 10.Li P.K., Chow K.M., Van de Luijtgaarden M.W. Changes in the worldwide epidemiology of peritoneal dialysis. Nat Rev Nephrol. 2017;13:90–103. doi: 10.1038/nrneph.2016.181. [DOI] [PubMed] [Google Scholar]
- 11.Parapiboon W., Ponce D., Cullis B. Acute peritoneal dialysis in COVID-19. Perit Dial Int. 2020 doi: 10.1177/0896860820931235. 896860820931235. [DOI] [PubMed] [Google Scholar]
- 12.El Shamy O., Patel N., Abdelbaset M.H. Acute start peritoneal dialysis during the COVID-19 pandemic: outcomes and experiences. J Am Soc Nephrol. 2020;31:1680–1682. doi: 10.1681/ASN.2020050599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.MY Sourial, MH Sourial, R Dalsan. Urgent peritoneal dialysis in patients with COVID-19 and acute kidney injury: a single-center experience in a time of crisis in the United States. Am J Kidney Dis. 2020;76:401–406. doi: 10.1053/j.ajkd.2020.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Vigiola Cruz M., Bellorin O., Srivatana V. Safety and efficacy of bedside peritoneal dialysis catheter placement in the COVID-19 era: initial experience at a New York City hospital. World J Surg. 2020;44:2464–2470. doi: 10.1007/s00268-020-05600-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yao J., Witherspoon L., McCormick B.B. Abdominal visceral perforation by buried peritoneal dialysis catheters: cause or coincidence? Semin Dial. 2018;31:305–308. doi: 10.1111/sdi.12690. [DOI] [PubMed] [Google Scholar]
- 16.Gokbel H., Yeksan M., Dogan E. Effects of CAPD applications on pulmonary function. Perit Dial Int. 1998;18:344–345. [PubMed] [Google Scholar]
- 17.Klisnick A., Souweine B., Filaire M. Peritoneal dialysis in a patient receiving mechanical ventilation in prone position. Perit Dial Int. 1998;18:536–538. [PubMed] [Google Scholar]
- 18.Gabriel D.P., Caramori J.T., Martim L.C. High volume peritoneal dialysis vs daily hemodialysis: a randomized, controlled trial in patients with acute kidney injury. Kidney Int Suppl. 2008;108:S87–S93. doi: 10.1038/sj.ki.5002608. [DOI] [PubMed] [Google Scholar]
- 19.Bikdeli B., Madhavan M.V., Jimenez D. COVID-19 and thrombotic or thromboembolic disease: implications for prevention, antithrombotic therapy, and follow-up. J Am Coll Cardiol. 2020;75:2950–2973. doi: 10.1016/j.jacc.2020.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ronco C. Continuous renal replacement therapy: forty-year anniversary. Int J Artif Organs. 2017;40:257–264. doi: 10.5301/ijao.5000610. [DOI] [PMC free article] [PubMed] [Google Scholar]