Abstract
Background
The coronavirus disease 2019 (COVID-19) pandemic has demonstrated significantly worse outcomes for minority (black and Hispanic) individuals. Understanding the reasons for COVID-19–related disparities among patients with asthma has important public health implications.
Objective
To determine factors contributing to health disparities in those with asthma during the COVID-19 pandemic.
Methods
An anonymous survey was sent through social media to adult patients with asthma, and a separate survey was sent to physicians who provide asthma care. The patient survey addressed demographic information including socioeconomic status, asthma control, and attitudes/health behaviors during COVID-19.
Results
A total of 1171 patients (10.1% minority individuals) and 225 physicians completed the survey. Minority patients were more likely to have been affected by COVID-19 (eg, became unemployed, lived in a community with high COVID-19 cases). They had worse asthma control (increased emergency visits for asthma, lower Asthma Control Test score), were more likely to live in urban areas, and had a lower household income. Initial differences in attitudes and health behaviors disappeared after controlling for baseline demographic features. Institutional racism was demonstrated by findings that minority individuals were less likely to have a primary care physician, had more trouble affording asthma medications due to COVID-19, and were more likely to have lost health insurance because of COVID-19, and that 25% of physicians found it more challenging to care for black individuals with asthma during COVID-19.
Conclusions
Differences in socioeconomic status and the effects of institutional racism, but not health behaviors, sources of information, or attitudes, are playing a role in disparities seen for patients with asthma during COVID-19.
Key words: Asthma, COVID-19, Health disparities, Survey, Attitudes, Implicit bias, Institutional racism, Structural racism
Abbreviations used: ACT, Asthma Control Test; CDC, Centers for Disease Control and Prevention; LABA, Long-acting beta-agonist; OR, Odds ratio
What is already known about this topic? There is a disproportionate impact of coronavirus disease 2019 (COVID-19) on minority individuals. For minority individuals with asthma, the extent of, and reasons for, these disparities is not fully known.
What does this article add to our knowledge? Minority individuals with asthma are more likely to be affected (directly or indirectly) by COVID-19. Differences in attitudes toward COVID-19 between minority and white individuals disappear once socioeconomic and asthma characteristics are controlled.
How does this study impact current management guidelines? Health disparities exist for patients with asthma during the COVID-19 pandemic, and addressing underlying socioeconomic factors as well as institutional racism can help to decrease these disparities.
Introduction
The coronavirus disease 2019 (COVID-19) pandemic has been a catastrophic event, with more than 2.5 million cases and more than 125,000 deaths in the United States by the end of June 2020.1 Initial reports suggest that a number of individuals would be considered “high risk” for increased severe illness and mortality from COVID-19, including those with hypertension, diabetes, cardiovascular disease, and respiratory diseases.2 Asthma is a respiratory disease, and initially patients with asthma of any severity were considered high risk according to the United States Centers for Disease Control and Prevention (CDC). More recently, as new evidence has emerged regarding the associations between asthma and COVID-19 outcomes,3 , 4 the CDC has updated its guidelines to include only those with moderate to severe asthma as those who might be at increased risk for severe illness from COVID-19.5
Although underlying comorbidities such as asthma are potential risk factors, one of the most striking findings during the COVID-19 pandemic has been the incredible health disparities demonstrated in outcomes. For example, black individuals account for nearly 70% of deaths from COVID-19 in Chicago, despite representing only 30% of the population.6 In addition, the COVID-19 death rate among Hispanic individuals is significantly higher than that among non-Hispanic individuals in New York (74.3 vs 45.2 per 100,000, respectively).7 Such disparities in COVID-19 outcomes have renewed attention on other conditions with significant health disparities, such as asthma. Although the prevalence of asthma among black individuals is somewhat higher than that among white individuals (10.7 vs 8.0%, respectively), black individuals experience significantly worse outcomes. Asthma mortality rates are nearly 3 times higher in non-Hispanic blacks than in non-Hispanic whites (22.7 vs 8.1 per million).1 In addition, asthma hospitalization rates are 4 to 5 times higher for black individuals than for white individuals.8 , 9
The reasons for these extreme disparities in both COVID-19 and asthma outcomes may be multifactorial. Although genetic factors may play a role,10 these differences have been attributed more strongly to socioeconomic factors including environmental influences.11 , 12 In addition, differences in cultural beliefs, attitudes, and health-seeking behaviors may contribute to disparities in asthma.13 Finally, institutional racism (which refers to the systemic practices or individual attitudes that result in the blocking of people of color from the distribution of resources) has been recognized as another factor that promotes health disparities.14 A better understanding of the contribution and interaction of these elements is critical to develop programs to eliminate health disparities.
The purpose of this study was to determine the underlying factors (including demographic and asthma characteristics, patient behaviors, and physician attitudes or perceived barriers) that may be contributing to health disparities in those with asthma during the COVID-19 pandemic.
Methods
This project was designed as an anonymous survey sent to individuals with asthma. In addition, a short survey was developed and sent to physicians who provide care for patients with asthma. The study was approved by the University of Michigan Institutional Review Board, and given the anonymous design signed consent was not required.
Survey development for patients with asthma
The questionnaire was developed by the survey development team. The survey development team comprised 10 individuals from multiple states including rural, suburban, and urban areas. It was multidisciplinary and included individuals with asthma, primary care physicians, asthma specialists, and medical students. Minority individuals were part of the team, as were public health professionals with specific interests in health disparities, and leadership from the Asthma and Allergy Foundation of America. Face validity evaluation of the questionnaire was performed initially with a small group of patient and physician volunteers, who evaluated the survey for language clarity, ease of completion, timing, and health literacy, and whose feedback was incorporated before survey distribution. The survey was designed to be completed in 20 minutes.
Individuals with asthma were eligible to participate if they were older than 18 years and currently had asthma. The survey obtained basic demographic information including age, sex, and race/ethnicity. Medical comorbidities other than asthma (hay fever, heart disease, high blood pressure, stroke, cancer, depression, heart burn, and diabetes) were assessed. Asthma-specific information included National Institutes of Health–recommended measures of asthma assessment (the Asthma Control Test [ACT], emergency department/urgent care visits in the previous year, hospitalizations in the previous year, requirement for intensive care unit admission ever, and asthma medications). The survey also ascertained items such as medication compliance and asthma severity (mild, moderate, or severe). All information on the survey was obtained through self-report, and subjects were not compensated for their participation.
In discussions during survey development with individuals with asthma, we identified areas of concern during the COVID-19 pandemic. Items included in the survey related to stress, susceptibility to COVID-19 in patients with asthma, social distancing practices, overlapping symptoms, attitudes toward the government response to the pandemic, and sources of COVID-related information. In addition, individuals discussed concerns related to COVID-19 care in the setting of institutional racism. We therefore included questions related to household income, living environment (rural, urban, suburban/peri-urban), employment challenges from COVID-19, health insurance changes, medication accessibility, and financial worries.
Survey distribution
Distribution of the survey was performed through social media (primarily Facebook and Twitter) as well as through patient email Listserves and the Asthma and Allergy Foundation of America website. Through social media, a post with a link to the survey was placed on multiple Facebook asthma group pages, inviting individuals with asthma to participate. To ensure an adequate representation of minority subjects, an invitation to participate was also placed on Facebook group pages for African Americans. The survey remained open for a 3-week period in the period April to May 2020.
Physician survey development and distribution
A separate survey was developed for physicians who provide care to patients with asthma. This survey was also developed by the survey development team. The survey underwent face validity testing with a group of primary care provider and asthma specialist physicians, who provided suggestions on content and timing, which were incorporated before survey distribution. Specific questions related to the care of minority patients, and instances of perceived institutional racism, were included. These questions related to obstacles when managing black patients' asthma, outcomes of black patients with asthma during COVID-19, additional challenges during COVID-19 when dealing with black patients, and compliance of black patients with asthma medications during COVID-19. The physician survey was distributed through social media (primarily through Facebook physician group pages) and also through physician email Listserves. Physicians were informed that 20 survey respondents would randomly be chosen to receive a $100 Amazon gift card. Please see this article's Online Repository at www.jaci-inpractice.org for both patient and physician surveys.
Statistical analysis
Individuals with asthma were considered to be minority status if they selected a race category of black or if they answered they were Hispanic. Individuals with asthma were considered to be white if they selected a race category of white and no other races. Comparisons between groups were performed using χ2 analysis. To control for differences in baseline demographic and asthma-specific information, regression models were constructed (logistic regression for dichotomous independent variables, multinomial regression models for ordinal variables) and baseline characteristics that were significantly different at the 0.05 level on univariate analysis were entered.
Results
Individuals with asthma
A total of 1355 individuals submitted a survey. After removing responses from those who were younger than 18 years or who responded that they did not currently have asthma, 1171 surveys were available for analysis. Of these surveys, 845 (72.2%) were from white individuals whereas 118 (10.1%) were from minority (black or Hispanic) individuals. The remaining 208 individuals did not specify a racial category or were not one of the race categories above and were excluded from further analysis.
Demographics and asthma control
Of all respondents, 98% resided in the United States. As shown in Table I , white respondents were more likely to be female and older. Items related to institutional racism found that minority respondents had a lower household income, were less likely to have a primary care physician, and were more likely to live in an urban environment. In regard to asthma, minority individuals reported worse asthma control, because they required more frequent emergency department visits for asthma in the previous year, were more likely to have required intubation for asthma, and were more likely to require daily oral corticosteroids. In addition, minority individuals had a lower ACT score, and were more likely to have an “uncontrolled” asthma score (≤19) on the ACT. Minority individuals were also more likely to only have a rescue medication and not be on a controller medication. Although self-reported asthma severity appeared worse in minority individuals, and specific controller use also appeared lower in minority populations, neither of these reached statistical significance. When examining comorbidities (heart disease, hypertension, depression, gastroesophageal reflux disease, diabetes, or seasonal allergies), no differences were found.
Table I.
Patients' demographic characteristics
| Characteristic | White (n = 845) | Minority (n = 118) | P value |
|---|---|---|---|
| Age (y), mean ± SD | 26.0 ± 12.4 | 20.2 ± 12.6 | <.001 |
| Sex: female | 88.0 (743) | 70.3 (83) | <.001 |
| Household income ($) | <.001 | ||
| $25,000 | 7.3 (60) | 20.5 (23) | |
| 25,000-49,999 | 15.9 (130) | 25.9 (29) | |
| 50,000-$74,999 | 16.2 (132) | 12.5 (14) | |
| 75,000-99,999 | 17.7 (145) | 14.3 (16) | |
| 100,000+ | 42.8 (350) | 26.8 (30) | |
| Currently live | <.001 | ||
| Urban | 19.7 (166) | 38.1 (45) | |
| Peri-urban/suburban | 56.7 (477) | 50.8 (60) | |
| Rural | 23.6 (199) | 11.0 (13) | |
| Comorbidities | |||
| Heart disease | 3.9 (32) | 3.6 (4) | .869 |
| Hypertension | 21.1 (174) | 24.5 (27) | .415 |
| Depression | 38.4 (313) | 35.7 (40) | .582 |
| GERD | 41.3 (339) | 33.3 (38) | .102 |
| Diabetes | 6.6 (53) | 5.5 (6) | .645 |
| Seasonal allergies | 88.1 (734) | 85.3 (99) | .393 |
| Have a PCP | 94.4 (798) | 89.0 (105) | .022 |
| Have asthma specialist | 37.0 (313) | 30.5 (36) | .167 |
| Age at asthma diagnosis (y), mean ± SD | 20.8 ± 15.1 | 16.8 ± 13.8 | .006 |
| Asthma ED in past year | 25.3 (213) | 35.0 (41) | .025 |
| ICU or intubation ever for asthma | 6.0 (51) | 16.1 (19) | <.001 |
| Asthma severity | .122 | ||
| Mild | 44.2 (373) | 39.0 (46) | |
| Moderate | 45.0 (380) | 44.9 (53) | |
| Severe | 8.1 (68) | 14.4 (17) | |
| Not sure | 2.7 (23) | 1.7 (2) | |
| Current asthma medications | |||
| Albuterol | 93.6 (791) | 93.2 (110) | .872 |
| Montelukast | 34.8 (294) | 27.1 (32) | .099 |
| ICS | 24.7 (209) | 23.7 (28) | .812 |
| ICS w/LABA | 41.9 (354) | 36.4 (43) | .26 |
| Oral steroids | 4.7 (40) | 9.3 (11) | .037 |
| Biologics | 3.6 (30) | 5.1 (6) | .41 |
| ACT score, mean ± SD | 18.5 ± 4.8 | 17.4 ± 4.8 | .018 |
| ACT uncontrolled (score ≤ 19) | 47.9 (404) | 59.0 (69) | .024 |
ED, Emergency department; GERD, gastroesophageal reflux disease; ICS, inhaled corticosteroid; LABA, long-acting beta-agonist; PCP, primary care physician.
Data presented as % (n) unless otherwise noted. Bold indicates statistical significance (P < .05).
COVID-19–specific differences
Related to COVID-19, minority respondents were more likely to have become unemployed because of COVID-19, had more difficulty obtaining asthma medications during the pandemic, and were more likely to respond that they lived in a community with a high number of COVID-19 cases (Table II ). Although minority respondents were more likely to have been diagnosed with COVID-19, to have had symptoms of COVID-19, and to have lost health insurance because of COVID-19, none of these reached statistical significance.
Table II.
Challenges faced by patients with asthma during COVID-19
| Challenges | White | Minority | P value |
|---|---|---|---|
| Unemployed due to COVID-19 | 16.1 (135) | 29.1 (34) | .001 |
| Difficulty getting asthma medicines during COVID-19 | 12.8 (108) | 20.5 (24) | .023 |
| Live in community with high number of cases | 44.1 (371) | 54.2 (64) | .038 |
| Diagnosed with COVID-19 | 1.5 (13) | 3.4 (4) | .153 |
| Lost health insurance because of COVID-19 | 2.3 (19) | 4.2 (5) | .197 |
| Have had symptoms of COVID-19 | 34.8 (293) | 38.5 (45) | .432 |
| Essential employee | 25.3 (213) | 23.9 (28) | .750 |
Data presented as % (n). Bold indicates statistical significance (P < .05).
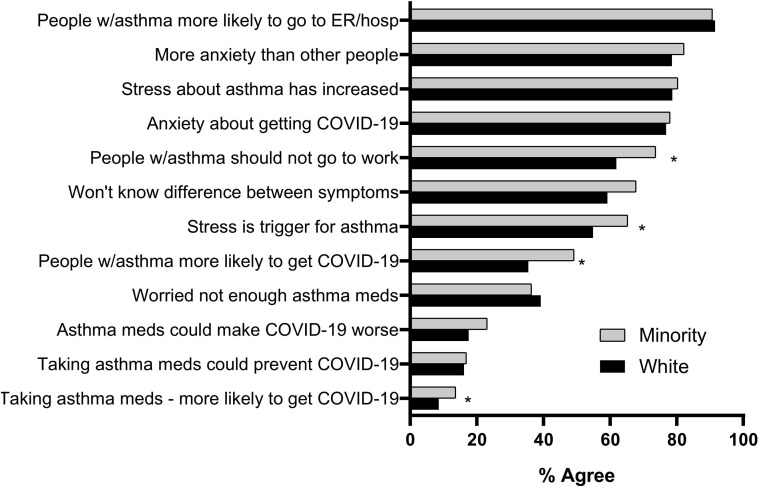
The survey also examined where patients with asthma were getting their sources of information related to COVID-19. As shown in Figure 1 , there were no differences between the 2 groups, with more than 80% of respondents selecting social media as one of their primary source of information. We next examined whether the respondents felt differently about the government response to the pandemic. Just over 50% of both groups felt that the CDC had a good understanding about the risks associated with COVID-19 to patients with asthma, but significantly more minority individuals felt that both the federal and state government responses were inadequate (Table III ). When examining behaviors and attitudes that could contribute to the spread of COVID-19, we found that there were no differences in social distancing practices and that approximately 80% of both groups noted they were taking the pandemic more seriously than others (Table III).
Figure 1.
Asthma patient's source for information about COVID-19. Each patient could select up to 3 sources. PCP, Primary care physician.
Table III.
Attitudes and behaviors during COVID-19
| Attitudes and behaviors | White | Minority | P value |
|---|---|---|---|
| Since COVID-19, taking medicines | .687 | ||
| More regularly than normal | 41.3 (241) | 45.8 (33) | |
| Less regularly than normal | 3.4 (20) | 4.2 (3) | |
| About the same as normally | 55.3 (323) | 50.0 (36) | |
| As of today, taking pandemic | .251 | ||
| Much more seriously than others | 47.7 (403) | 58.5 (69) | |
| A little more seriously than others | 29.0 (245) | 24.6 (29) | |
| With about same seriousness as others | 19.8 (167) | 15.3 (18) | |
| Less seriously than others | 3.6 (30) | 1.7 (2) | |
| CDC has good understanding about risks | 55.1 (461) | 61.0 (72) | .229 |
| Federal government response is | .016 | ||
| Too much | 4.5 (38) | 1.7 (2) | |
| Just right | 26.8 (226) | 16.9 (20) | |
| Too little | 68.6 (578) | 81.4 (96) | |
| State government response is | .001 | ||
| Too much | 10.1 (85) | 5.1 (6) | |
| Just right | 66.8 (563) | 55.9 (66) | |
| Too little | 23.1 (195) | 39.0 (46) | |
| As of today, I am | .259 | ||
| Interacting with others as usual | 0.7 (6) | 0.8 (1) | |
| Social distancing | 5.0 (42) | 6.8 (8) | |
| Only essential trips, interacting as usual | 1.8 (15) | 4.2 (5) | |
| Only essential trips and social distancing | 72.4 (612) | 64.4 (76) | |
| Completely isolating | 20.1 (170) | 23.7 (28) |
Data presented as % (n). Bold indicates statistical significance (P < .05).
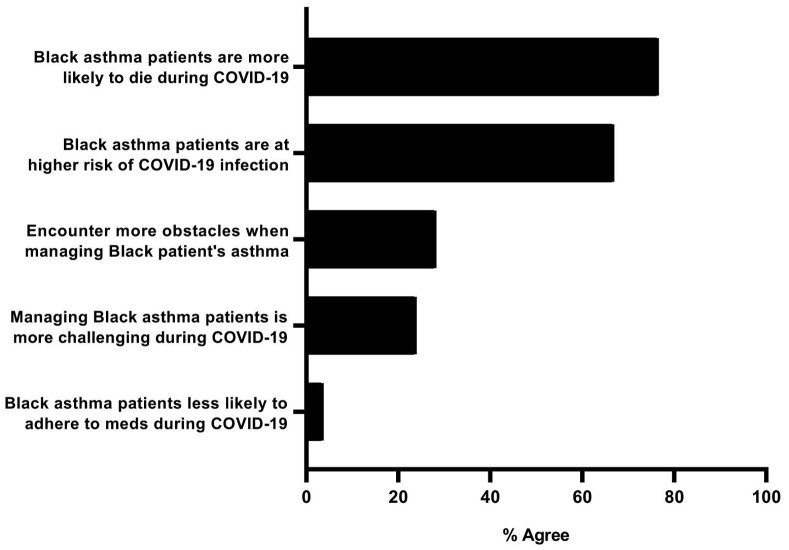
Minority individuals were more likely to feel that individuals with asthma were at a higher risk of contracting COVID-19, that people with asthma should not work during the COVID-19 pandemic, and that stress is a major trigger for asthma (Figure 2 ). Approximately 20% of both groups felt that asthma medications could make a COVID-19 infection worse, and more minority individuals felt that asthma medications would make an individual more likely to get a COVID-19 infection (13.7 vs 8.6%; P = .077). Both groups were worried that they would not be able to tell the difference between asthma symptoms and COVID-19 symptoms. Similarly, both groups had high levels of anxiety about getting COVID-19, and both groups reported more anxiety than those without asthma during this time.
Figure 2.
Percent of patients with asthma who agree with each statement regarding COVID-19. ER, Emergency room; hosp, hospital; meds, medicines. ∗P ≤ .05.
Regression analysis
We next examined whether differences in attitudes between minority and white respondents persisted after controlling for demographic and asthma-specific factors. After controlling for significant differences presented in Table I, there was no difference in attitudes related to asthma medications increasing the risk of COVID-19, the necessity of individuals with asthma to stay home from work, attitudes about federal or state response to COVID-19, or the ability to know the difference between COVID-19 and asthma symptoms (see Table E1 in this article's Online Repository at www.jaci-inpractice.org). However, after controlling for confounding variables from Table I, minority individuals remained more likely to feel that those with asthma were more likely to get COVID-19 (odds ratio, 1.61; P = .037).
Physician responses
A total of 225 physicians who care for patients with asthma completed a brief survey. The demographic characteristics of these physicians are listed in Table E2 in this article's Online Repository at www.jaci-inpractice.org. Briefly, the physicians were primarily primary care physicians (62.1%) and asthma specialists (31.9%) who had been in practice for an average of 10.7 years. Only 1.4% of respondents were black and 4.0% were Hispanic.
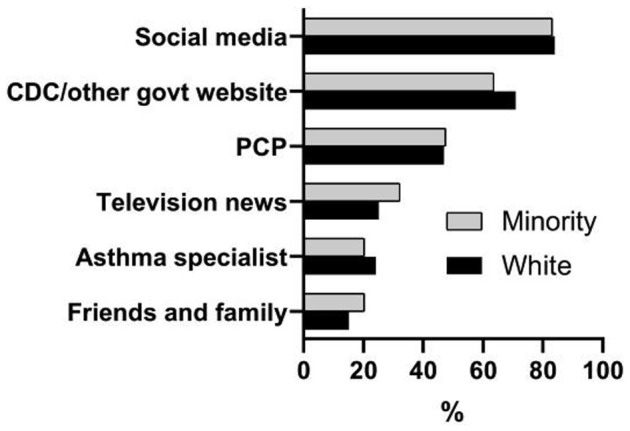
When inquiring about the administration of care for patients, 24% of physician respondents felt it was more difficult to care for black patients during COVID-19 and 28% of physician respondents noted they encounter more obstacles when managing asthma for a black patient. Figure 3 shows the percent of respondents who answered “Somewhat agree” or “Strongly agree” for each of 5 statements related to caring for black patients with asthma during COVID-19.
Figure 3.
Percent of physicians who agree with each of the following statements regarding the care of patients with asthma during COVID-19. Meds, Medicines.
Discussion
Since March 2020, the COVID-19 pandemic has disproportionately impacted minority populations in the United States. For decades, asthma outcomes have also been significantly worse among these same populations. This study was designed to determine the underlying factors that may be contributing to health disparities in those with asthma during the COVID-19 pandemic. We found that socioeconomic factors and institutional racism, but not health-seeking behaviors or cultural factors, appear to play a significant role.
This study demonstrated that the COVID-19 pandemic has been particularly difficult for minority individuals with asthma. For example, minority individuals reported they were more likely to have had a COVID-19 infection (though this did not reach statistical significance), more likely to have lost their jobs because of COVID-19, more likely to have difficulties obtaining asthma medications during COVID-19, and more likely to live in a community with a high number of cases (which may have been influenced by higher rates of urban residence). Such disparities may partially explain why minority individuals were significantly more likely to feel that both the state and federal governments were not doing enough during the COVID-19 pandemic. The study also reaffirmed socioeconomic disparities among minority individuals (eg, lower income levels), and worse control of asthma on multiple domains (eg, emergency visits and ACT score). We next wanted to determine whether differences in health-seeking behaviors and attitudes were responsible for the worse outcomes between minority and white populations with asthma. Although multiple differences were initially found, after adjusting for the baseline socioeconomic and asthma control differences, these virtually all disappeared.
The finding that minority individuals with asthma have similar health-seeking behaviors and practices as white individuals has important public health implications. Both groups felt that the CDC has a good understanding about the risks for patients with asthma with COVID-19 (55%-60% agree), both groups are using the same social distancing practices, and both groups report an increased compliance with asthma medications due to COVID-19. Just as importantly, the sources of information related to COVID-19 are the same in both groups. Therefore, a “minority-specific” campaign to distribute information related to COVID-19 for patients with asthma may not be effective.
This study also demonstrates that institutional racism may be a factor in the care of patients with asthma during the COVID-19 pandemic. Institutional racism is defined as “the collective failure of an organization to provide an appropriate and professional service to people because of their color, culture, or ethnic origin.”15 It does not require the actions or intent of individuals,16 but rather because of an establishment of patterns, procedures, practices, and policies within organizations, institutional racism penalizes and exploits people because of their race.17 As it pertains to medical care, examples in this study include findings that minority individuals were significantly more likely to have lost health insurance during COVID-19, to live in urban environments (where hospitals are often under significant financial constraints and are underresourced),18 to have difficulty affording asthma medications during COVID-19, and were less likely to have a primary care physician. Nearly 30% of physicians noted they encountered more obstacles when providing asthma care for black patients than for white patients, and approximately 25% of physicians felt that during COVID-19, it was more challenging to care for black patients.
Although not fully explored in this study, both institutional racism and individual physician implicit bias can contribute to health disparities in asthma. For example, physician responses regarding difficulties caring for minority patients may be related to factors such as perceived difficulties in affording medications, baseline health status, or attending office visits (examples of an institutional-wide problem). However, even when controlling for socioeconomic factors, previous studies have found unequal outcomes for minority individuals, thought to be due to larger social inequalities within societies, of which socioeconomic status is only one part.19 Another possibility is that implicit bias may be contributing to institutional racism,20 and implicit bias has been found to be prevalent among health care workers.21 Unlike overt racism, implicit bias refers to attitudes or stereotypes that affect understanding, actions, and decisions in an unconscious manner. One way to help overcome implicit bias is through workshops and education, which can improve clinical outcomes for minorities.22 In July 2020, in response to the disparities seen in COVID-19 outcomes, the state of Michigan issued a directive requiring all medical professionals to take implicit bias training—the first state to do so.23
There are limitations to this study. Because this was sent through social media and email, both patients and physicians who do not use this form of communication would be excluded. The age and socioeconomic status of the participants may not be representative of all patients with asthma or physicians, because those in the lowest socioeconomic strata who may be most vulnerable to COVID-19 are least likely to use social media.24 Additional factors that may influence asthma outcomes (eg, obesity and environmental tobacco exposure) were not assessed. Answers to all survey questions were self-reported and not verified through medical chart review. Given the method of distribution, it was not possible to calculate a response rate nor to evaluate whether those who responded were different than those who did not. The surveys were validated for face but not content validity. Testing of implicit bias in physician respondents was not done, because validated tools (such as the Implicit Association Test25) often take a significant amount of time to administer. A complete analysis of the factors contributing to institutional and systemic racism was not carried out. Follow-up questions or focus groups were not performed to further elucidate responses by patients or providers. Finally, because the study is cross-sectional rather than a prospective trial, cause and effect cannot be proven but rather associations between worse outcomes and factors.
Conclusions
Differences in socioeconomic factors and the effects of institutional racism, but not health-seeking behaviors, are playing a role in disparities seen for patients with asthma during COVID-19. There are challenges in correcting such differences, but it is critical to do so to eliminate health disparities.
Footnotes
This study was funded through a restricted donation from the Asthma and Allergy Foundation of America.
Conflicts of interest: All authors declare that there are no relevant conflicts of interest related to this work.
Online Repository
Table E1.
Regression analysis for attitudes/opinions among minority patients with asthma
| Attitudes/opinions | Odds ratio | 95% CI | P value | |
|---|---|---|---|---|
| Patients with asthma more likely to get COVID-19 | 1.61 | 1.03 | 2.5 | .037 |
| Asthma medications increase the risk of COVID-19 | 1.46 | 0.753 | 2.84 | .261 |
| Stress is a major trigger for asthma | 1.34 | 0.853 | 2.1 | .205 |
| Individuals with asthma should not go to work | 1.21 | 0.743 | 1.96 | .447 |
| Federal government response is inadequate | 4.83 | 0.631 | 36.9 | .13 |
| State government response is inadequate | 2.29 | 0.838 | 6.28 | .247 |
ED, Emergency department; ICU, intensive care unit; PCP, primary care physician.
Controlled for age, age of diagnosis, COVID in community, PCP, urban living, sex, household income, unemployed from COVID, ACT score, asthma ED visits, need for ICU visit, asthma medication adherence, and difficulties getting medicines.
Bold indicates statistical significance (P < .05).
Table E2.
Physician demographics
| Demographics | n = 225 | % |
|---|---|---|
| Specialty | ||
| Internal Medicine | 49 | 21.8 |
| Pediatrics | 47 | 20.9 |
| Family Practice | 30 | 13.3 |
| Med-Peds | 19 | 8.4 |
| Allergy/Immunology | 61 | 27.1 |
| Pulmonary | 11 | 4.8 |
| Other | 4 | 1.8 |
| Practice location | ||
| Urban | 46 | 20.4 |
| Peri-urban/suburban | 147 | 65.3 |
| Rural | 6 | 2.7 |
| Race | ||
| White | 147 | 65.3 |
| Asian | 45 | 20 |
| Hispanic | 8 | 4 |
| Black | 3 | 1.3 |
| Other | 6 | 2.7 |
| Female | 125 | 62.8 |
| Age (y), mean ± SD | 41 | 11.9 |
| Years in practice, mean ± SD | 9.7 | 11 |
| Asthma patient over year, median (IQR) | 50 | 75 |
IQR, Interquartile range.
References
- 1.Centers for Disease Control and Prevention Coronavirus disease 2019 (COVID-19) cases and deaths in the US. https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/us-cases-deaths.html Available from:
- 2.Zheng Z., Peng F., Xu B., Zhao J., Liu H., Peng J. Risk factors of critical & mortal COVID-19 cases: a systematic literature review and meta-analysis. J Infect. 2020;81:e16–e25. doi: 10.1016/j.jinf.2020.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lupia T., Scabini S., Mornese Pinna S., Di Perri G., De Rosa F.G., Corcione S. 2019 novel coronavirus (2019-nCoV) outbreak: a new challenge. J Glob Antimicrob Resist. 2020;21:22–27. doi: 10.1016/j.jgar.2020.02.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chhiba K.D., Patel G.B., Vu T.H.T., Chen M.M., Guo A., Kudlaty E. Prevalence and characterization of asthma in hospitalized and nonhospitalized patients with COVID-19. J Allergy Clin Immunol. 2020;146:307–314.e4. doi: 10.1016/j.jaci.2020.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention Coronavirus disease 2019 (COVID-19). People who are at increased risk for severe illness. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-at-increased-risk.html Available from:
- 6.Yancy C.W. COVID-19 and African Americans. JAMA. 2020;323:1891–1892. doi: 10.1001/jama.2020.6548. [DOI] [PubMed] [Google Scholar]
- 7.Kirby T. Evidence mounts on the disproportionate effect of COVID-19 on ethnic minorities. Lancet Respir Med. 2020;8:547–548. doi: 10.1016/S2213-2600(20)30228-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Doshi R.P., Aseltine R.H., Jr., Sabina A.B., Graham G.N. Racial and ethnic disparities in preventable hospitalizations for chronic disease: prevalence and risk factors. J Racial Ethn Health Disparities. 2017;4:1100–1106. doi: 10.1007/s40615-016-0315-z. [DOI] [PubMed] [Google Scholar]
- 9.Marchese M.E., Shamo F., Miller C.E., Wahl R.L., Li Y. Racial disparities in asthma hospitalizations following implementation of the Smoke-Free Air Law, Michigan, 2002-2012. Prev Chronic Dis. 2015;12:E201. doi: 10.5888/pcd12.150144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Willis-Owen S.A.G., Cookson W.O.C., Moffatt M.F. The genetics and genomics of asthma. Annu Rev Genomics Hum Genet. 2018;19:223–246. doi: 10.1146/annurev-genom-083117-021651. [DOI] [PubMed] [Google Scholar]
- 11.Forno E., Celedon J.C. Health disparities in asthma. Am J Respir Crit Care Med. 2012;185:1033–1035. doi: 10.1164/rccm.201202-0350ED. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Holsey C.N., Collins P., Zahran H. Disparities in asthma care, management, and education among children with asthma. Clin Pulm Med. 2013;20:172–177. doi: 10.1097/CPM.0b013e3182991146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Canino G., McQuaid E.L., Rand C.S. Addressing asthma health disparities: a multilevel challenge. J Allergy Clin Immunol. 2009;123:1209–1217. doi: 10.1016/j.jaci.2009.02.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bailey Z.D., Krieger N., Agenor M., Graves J., Linos N., Bassett M.T. Structural racism and health inequities in the USA: evidence and interventions. Lancet. 2017;389:1453–1463. doi: 10.1016/S0140-6736(17)30569-X. [DOI] [PubMed] [Google Scholar]
- 15.Esmail A. The prejudices of good people. BMJ. 2004;328:1448–1449. doi: 10.1136/bmj.328.7454.1448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gee G.C., Ford C.L. Structural racism and health inequities: old issues, new directions. Du Bois Rev. 2011;8:115–132. doi: 10.1017/S1742058X11000130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.American Academy of Family Practice Institutional racism in the health care system. https://www.aafp.org/about/policies/all/institutional-racism.html Available from:
- 18.Andrulis D.P., Duchon L.M. The changing landscape of hospital capacity in large cities and suburbs: implications for the safety net in metropolitan America. J Urban Health. 2007;84:400–414. doi: 10.1007/s11524-007-9163-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Williams D.R., Priest N., Anderson N.B. Understanding associations among race, socioeconomic status, and health: patterns and prospects. Health Psychol. 2016;35:407–411. doi: 10.1037/hea0000242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chapman E.N., Kaatz A., Carnes M. Physicians and implicit bias: how doctors may unwittingly perpetuate health care disparities. J Gen Intern Med. 2013;28:1504–1510. doi: 10.1007/s11606-013-2441-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hall W.J., Chapman M.V., Lee K.M., Merino Y.M., Thomas T.W., Payne B.K. Implicit racial/ethnic bias among health care professionals and its influence on health care outcomes: a systematic review. Am J Public Health. 2015;105:e60–76. doi: 10.2105/AJPH.2015.302903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Devine P.G., Forscher P.S., Austin A.J., Cox W.T. Long-term reduction in implicit race bias: a prejudice habit-breaking intervention. J Exp Soc Psychol. 2012;48:1267–1278. doi: 10.1016/j.jesp.2012.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.US News and World Reports Gov: health workers must get bias training; issues mask plea. https://www.usnews.com/news/best-states/michigan/articles/2020-07-09/whitmer-health-workers-must-get-implicit-bias-training Available from:
- 24.Pew Research Center Social media fact sheet. June 12, 2019. https://www.pewresearch.org/internet/fact-sheet/social-media/ Available from:
- 25.Harvard University Project Implicit The Implicit Association Test. https://implicit.harvard.edu/implicit/takeatest.html Available from:
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.