Abstract
Background
COVID-19, caused by the Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2), has great health implications in older patients, including high mortality. In general, older patients often have atypical symptom presentations during acute illness due to a high level of comorbidity. The purpose of this study was to investigate the presentation of symptoms at hospital admissions in older patients with COVID-19 and evaluate its impact on disease outcome.
Methods
This retrospective study included patients ≥80 years of age with a positive test for SARS-CoV-2, who were admitted to one of three medical departments in Denmark from March 1st to June 1st, 2020.
Results
A total of 102 patients (47% male) with a mean age of 85 years were included. The most common symptoms at admission were fever (74%), cough (62%), and shortness of breath (54%). Furthermore, atypical symptoms like confusion (29%), difficulty walking (13%), and falls (8%) were also present. In-hospital and 30-day mortality were 31% (n = 32) and 41% (n = 42), respectively. Mortality was highest in patients with confusion (50% vs 38%) or falls (63% vs 39%), and nursing home residency prior to hospital admission was associated with higher mortality (OR 2.7, 95% CI 1.1–6.7).
Conclusions
Older patients with SARS-Cov-2 displayed classical symptoms of COVID-19 but also geriatric frailty symptoms such as confusion and walking impairments. Additionally, both in-hospital and 30-day mortality was very high. Our study highlights the need for preventive efforts to keep older people from getting COVID-19 and increased awareness of frailty among those with COVID-19.
Keywords: Delirium, Falls, Frailty, Multimorbidities, SARS-CoV-2
1. Introduction
COVID-19, caused by the Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2), is a disease with greater health implications in older patients. In the UK, 56% of patients hospitalized with COVID-19 were ≥70 years old (Docherty et al., 2020), and in Sweden, 69% of SARS-CoV-2 positive fatalities were seen among patients above 80 years (Socialstyrelsen, 2020). Age has been reported as one of the strongest predictors of fatal outcomes with an early study from Italy suggesting mortality rates of >80% among patients ≥70 years (Abbatecola & Antonelli-Incalzi, 2020). A recent nationwide population-based cohort study among Danish patients reported a mortality rate of 34% among the patients above 80 years (Reilev et al., 2020). In addition to increasing age, worse outcomes in COVID-19 are related to comorbidities such as chronic cardiac disease, chronic pulmonary disease, hypertension, diabetes, and chronic kidney disease (Docherty et al., 2020; Reilev et al., 2020; Shahid et al., 2020). These conditions have an increased occurrence in the older population, making them more susceptible to poor outcomes of infection.
Aging is defined as a progressive decline in physical reserve and organ function (Resnick & Marcantonio, 1997). Older patients are a highly heterogeneous group, ranging from fit to frail with various comorbidities (Fried et al., 2001). In general, older patients are known to present themselves with atypical symptoms (Hofman, van den Hanenberg, Sierevelt, & Tulner, 2017), as the presentation of a new disease often depends on previous conditions and vulnerability within an organ system. A symptom or dysfunction related to an organ system may not always be the cause of the problem, as symptoms often appear from the “weakest link” in the system (Resnick & Marcantonio, 1997). This is illustrated by more than half of the older patients in an emergency department having an “atypical presentation of illness”, with symptoms such as falls or confusion, which are often primary symptoms of infections (Hofman, van den Hanenberg, Sierevelt, & Tulner, 2017).
COVID-19 usually causes cough, fever, and shortness of breath (Docherty et al., 2020; Shahid et al., 2020). Fatigue, confusion, sputum, diarrhea, and nausea/vomiting also appear frequently (Docherty et al., 2020). As symptoms of disease can be unspecific in older patients, it is crucial to diagnose older patients with unspecific symptoms of COVID-19 to avoid further transmission of the infection. However, the presentation of disease and impact on outcome has been less evaluated in older patients. Therefore, the purpose of this study was to investigate the disease presentation in older patients diagnosed with COVID-19 and evaluate its impact on disease outcome.
2. Method
2.1. Study design and setting
This study is a multi-center retrospective cohort study including older patients, admitted to the Departments of medicine or geriatric medicine at one of three Danish hospitals from March 1st until June 1st in 2020: Copenhagen University Hospital Herlev and Gentofte, Odense University Hospital, and Viborg Regional Hospital. All patients ≥80 years of age admitted to one of the three departments who were positive for SARS-CoV-2 by reverse transcriptase polymerase chain reaction on either pharyngeal swabs, sputum, or tracheal aspirate were eligible for study inclusion.
2.2. Data source
Data was collected from electronical hospital medical charts. Dates of death were linked to the Danish National Registry of Patients by the ten-digit Civil Registration Number assigned to all Danish citizens at birth or immigration (Andersen, Madsen, Jørgensen, Mellemkjoer, & Olsen, 1999).
2.3. Baseline data
Baseline demographic data was registered in a database after first COVID-19 related admission. This included symptom presentation on admission, preceding comorbidities and medication, walking impairment, blood test results, and radiological findings. Confusion included suspicion of delirium described in the medical chart. The degree of comorbidity was assessed according to the Charlson Comorbidity Index (CCI) (not age-adjusted) (Charlson, Pompei, Ales, & MacKenzie, 1987) and the Cumulative Illness Rating Scale (CIRS) (Parmelee, Thuras, Katz, & Lawton, 1995). The CCI evaluates the prevalence and severity of 19 chronic diseases using a rating system, and the total sum of points is used to estimate comorbidity according to a 10-year survival rate (Charlson, Pompei, Ales, & MacKenzie, 1987). We categorized CCI scores as 0, 1–2, or ≥3 points. CIRS is an assessment tool based on 14 individual organ systems where severity of disease is rated from 0 to 4 for each organ system. A high sum of points indicates a high chronical medical illness burden (Parmelee, Thuras, Katz, & Lawton, 1995). Both comorbidity scores were calculated based on ICD-10 hospital diagnoses, medical prescriptions, and information in medical records upon admission.
Polypharmacy was defined as the intake of ≥5 daily medications, and excessive polypharmacy as ≥10 daily medications. We grouped patients into four categories according to number of medications: 0, 1–4, 5–9, or ≥10.
2.4. Outcomes
The primary aim of the study was to evaluate symptoms on admission. Outcomes included discharge destination, and in-hospital and 30-day survival.
2.5. Statistical analyses
Baseline characteristics and blood test results were summarized by means with standard deviations (SD) for normally distributed data, and medians and interquartile ranges (IQR) for non-normally distributed data. Patients were followed from the date of verified SARS-CoV-2 infection and 30 days onward. 30-day mortality was defined as the proportion of patients deceased from any cause 30 days after the diagnosis. Confidence intervals (CIs) were computed using the exact approach by Clopper and Pearson (Clopper & Pearson, 1934). Odds ratios (ORs) for 30-day mortality and fitness for intensive care were computed using logistic regression models. Analyses were conducted in R (version 3.6.1).
2.6. Ethics
The study was approved by the Danish Health Authority (Approval number 31–1521–230) and the Danish Data Protection Agency (Journal nr. 20/13,067). The Danish council for patient safety (record no. 31–1521–230) and Ethics Committee (record no. 20,202,000, 53) waived informed consent according to Danish legislation due to the purely observational design, using data from routine clinical practice.
3. Results
A total of 102 hospitalized patients (47% men) with verified SARS-CoV-2 infection and a median age of 85 (IQR 4.0) years were included in this study. Baseline characteristics are presented in Table 1 . In total, 29 patients were admitted from nursing homes or intermediate care facilities. Seventy-three patients lived in their own residence prior to hospitalization, whereof 38 (53%) received home care. Excessive polypharmacy was reported in 47%. The median CCI was 2 (IQR 1–3) and the median CIRS was 10 (IQR 7–13).
Table 1.
Baseline characteristics in 102 Danish patients aged 80+ years admitted to hospital with COVID-19, stratified for sex and type of residence.
| All patients (N = 102) | Female (n = 54) | Male (n = 48) | Own home (n = 73) | Nursing home/intermediate care facilities (n = 29) | |
|---|---|---|---|---|---|
| Age, median (IQR) | 84 (82–88) | 84 (82–88) | 84 (82–88) | 84 (81–88) | 84 (83–89) |
| Medications, median (IQR) | 9.0 (7.0–12) | 9.0 (7.0–12) | 10 (6.0–13) | 9.0 (6.0–11) | 10 (7.0–14) |
| - 0–4 | 14 (14) | 6 (11) | 8 (17) | 11 (15) | 3 (10) |
| - 5–9 | 40 (39) | 25 (46) | 15 (31) | 30 (41) | 10 (35) |
| - ≥10 | 48 (47) | 23 (43) | 25 (52) | 32 (44) | 16 (55) |
| Walking aids, n (%) | |||||
| - None | 44 (43) | 24 (44) | 20 (42) | 36 (49) | 8 (28) |
| - Walking stick/frame | 42 (41) | 21 (39) | 21 (44) | 33 (45) | 9 (31) |
| - Wheelchair/bedridden | 16 (16) | 9 (17) | 7 (15) | 4 (5.5) | 12 (41) |
| Living conditions, n (%) | |||||
| - Own home | 73 (72) | 37 (69) | 36 (75) | 73 (100) | 0 (0) |
| - Nursing home/intermediate care facilities | 29 (28) | 17 (32) | 12 (25) | 0 (0) | 29 (100) |
| CIRS, median (IQR) | 10 (7.0–13) | 9 (7.0–12) | 11 (7.8–14) | 9 (7.0–12) | 12 (8.0–14) |
| CCI, median (IQR) | 2 (1.0–3.0) | 2 (1.0–3.0) | 3 (1.0–4.3) | 2 (1.0–3.0) | 2 (2.0–3.0) |
| - 0, n (%) | 11 (11) | 6 (11) | 5 (10) | 10 (14) | 1 (3.4) |
| - 1–2, n (%) | 49 (48) | 33 (61) | 16 (33) | 34 (47) | 15 (52) |
| - ≥3, n (%) | 42 (41) | 15 (28) | 27 (56) | 29 (40) | 13 (45) |
| Comorbidities n (%) | |||||
| - Hypertension | 54 (53) | 33 (61) | 21 (44) | 38 (52) | 16 (55) |
| - Heart disease | 53 (53) | 22 (42) | 31 (66) | 44 (62) | 9 (31) |
| - Respiratory disease | 46 (45) | 23 (43) | 23 (48) | 38 (52) | 8 (28) |
| - Diabetes | 23 (23) | 8 (15) | 15 (31) | 17 (23) | 6 (21) |
CCI Charlson comorbidity index score, CIRS Cumulative illness rating scale, IQR Interquartile range.
3.1. Symptoms and clinical presentation
The most common symptoms were fever (74%), cough (62%), and shortness of breath (54%), followed by fatigue (38%) and weight loss/loss of appetite (29%) (Table 2 ). Fever, cough, or shortness of breath was seen in 97% of the patients, and all patients had at least one classical symptom of COVID-19 (UpToDate, 2020). Furthermore, atypical COVID-19 symptoms (geriatric frailty symptoms) were present in many patients such as confusion (29%), difficulty walking (13%), and falls (8%).
Table 2.
Clinical presentation and paraclinical findings in 102 Danish patients aged 80+ years admitted to hospital with COVID-19.
| All patients (N = 102) | Female (n = 54) | Male (n = 48) | Own residence (n = 73) | Nursing home (n = 29) | |
|---|---|---|---|---|---|
| Symptoms, n (%) | |||||
| - Fever | 75 (74) | 39 (72) | 36 (75) | 56 (77) | 19 (66) |
| - Cough | 63 (62) | 30 (56) | 33 (69) | 51 (70) | 12 (41) |
| - Shortness of breath | 55 (54) | 30 (56) | 25 (52) | 42 (58) | 13 (45) |
| - Fatique | 39 (38) | 18 (33) | 21 (44) | 30 (41) | 9 (31) |
| - Confusion | 30 (29) | 13 (24) | 17 (35) | 19 (26) | 11 (38) |
| - Weight loss/Appetite loss | 30 (29) | 16 (30) | 14 (29) | 24 (33) | 6 (21) |
| - Nausea/vomiting | 19 (19) | 11 (20) | 8 (17) | 14 (19) | 5 (17) |
| - Vertigo | 15 (15) | 10 (19) | 5 (10) | 15 (21) | 0 (0) |
| - Diarrhea | 13 (13) | 6 (11) | 7 (15) | 10 (14) | 3 (10) |
| - Headache | 13 (13) | 9 (17) | 4 (8.3) | 13 (18) | 0 (0.0) |
| - Difficulty walking | 13 (13) | 6 (11) | 7 (15) | 11 (15) | 2 (6.9) |
| - Chest pain | 11 (101) | 8 (15) | 3 (6.2) | 11 (15) | 0 (0.0) |
| - Pharyngitis | 8 (7.8) | 3 (5.6) | 5 (10) | 5 (6.8) | 3 (10) |
| - Falls | 8 (7.8) | 4 (7.4) | 4 (8.3) | 8 (11) | 0 (0.0) |
| - Dehydration | 4 (3.9) | 3 (5.6) | 1 (2.1) | 2 (2.7) | 2 (6.9) |
| Blood samples, median (IQR) | |||||
| - Ferritin, ug/L (12–300 L) |
398 (168–630) |
291 (126–588) |
488 (270–675) |
405 (228–632) |
339 (144–602) |
| - Lactate dehydrogenase (115–255 U/L) |
261 (205–320) |
232 (196–304) |
290 (227–330) |
263 (206–318) |
245 (198–327) |
| - Lymphocytes (1.0–3.5 × 10^9/L) |
0.8 (0.6–1.1) |
0.9 (0.7–1.2) |
0.6 (0.5–0.9) |
0.7 (0.5–1.0) |
0.8 (0.7–1.1) |
| - Leukocytes (3.5–8.8 × 10^9/L) |
6.6 (5.3–8.3) |
6.5 (5.3–8.4) |
7.0 (5.3–8.0) |
6.6 (4.9–8.0) |
6.7 (5.5–9.1) |
| - C-reactive protein (<10 mg/L) |
74 (37–118) |
61 (31–103) |
90 (51–144) |
77 (39–115) |
69 (33–121) |
| - Albumin (34–45 g/L) |
32 (30–35) |
33 (31–35) |
32 (29–35) |
32 (30–34) |
33 (31–36) |
| - Alkaline phosphatase (35–105 U/L) |
81 (62–110) |
81 (65–101) |
81 (60–119) |
75 (60–102) |
94 (72–119) |
| Examinations results, n (%) | |||||
| - ECG normal | 20 (23) | 13 (28) | 7 (18) | 14 (23) | 6 (23) |
| - ECG known abnormality | 35 (41) | 12 (26) | 23 (58) | 29 (48) | 6 (23) |
| - ECG new abnormality | 23 (27) | 15 (33) | 8 (20) | 12 (20) | 11 (42) |
| Thoracic CT / X-ray, n (%) | |||||
| - Normal, n (%) | 23 (23) | 16 (30) | 7 (15) | 12 (17) | 11 (39) |
| - Lung consolidation, n (%) | 70 (70) | 33 (61) | 37 (80) | 53 (74) | 17 (61) |
| - Pleural effusion, n (%) | 18 (18) | 5 (9.3) | 13 (28) | 15 (21) | 3 (11) |
CT Computer tomography scan, ECG Electrocardiogram, IQR Interquartile range.
Lung consolidations confirmed by thoracic imaging appeared in 70% of patients and pleural effusions were seen in 18%. New electrocardiogram (ECG) abnormalities were found in 27% of patients with available ECG on admission (in 23 of 86 patients). Blood tests upon admission showed a median C-reactive protein (CRP) of 73.5 mg/L (IQR 37–118). The median leukocyte count was 6.6 10^9/L (IQR 5.3–8.3) and the median lymphocyte count was 0.8 10^9/L (IQR 0.6–1.1) for reference values (Referenceintervaller, 2020) see Table 2.
3.2. Initiated treatment
In total, 74% of the patients were treated with intravenous antibiotic therapy during hospitalization. Seventy five percent received oxygen treatment, and additional ventilatory support (non-invasive ventilation and/or continuous positive airway pressure) was registered in 17%.
3.3. Intensive care assessment
Decisions concerning fitness for intensive care were made on admission according to Danish hospital standard practice in 94 of 102 patients. In total, 79% (n = 74) of the patients were considered unfit for intensive care. Three patients received intensive care therapy, whereof two patients required mechanical ventilation.
Baseline characteristics associated with not being assessed fit for intensive care were admission from nursing home compared with patients admitted from own residence (OR 7.5, 95% CI 2.0–48.6), high grade of comorbidity (CCI ≥3 vs. <3; OR 2.7, 95% CI 1.1–7.5 and CIRS ≥10 vs. CIRS <10; OR 2.6, 95% CI 1.1–6.7), severe walking impairment compared with no or mild walking impairments (OR 6.9, 95% CI 1.3–127), and excessive polypharmacy compared with <10 daily medications (OR 4.8, 95% CI 1.8–14) (Fig. 1 ). Older age was also significantly associated with being assessed unfit for intensive care (OR 6.9, 95% CI 1.3–127), but this association was not persistent after adjusting for residency, medications, and walking impairment (OR 5.4, 95% CI 0.8–109).
Fig. 1.
The proportion of 102 hospitalized Danish geriatric patients with SARS-CoV-2 infection who were decided unfit for intensive care, stratified on baseline characteristics. The whiskers indicate 95% confidence intervals.
Footnote: CIRS, Cumulative Illness Rating Scale; CCI, Charlson Comorbidity Index.
3.4. Outcomes
The median number of in-hospital bed days during the first 30 days following SARS-CoV-2 infection was 7 days (IQR 4–11) with an in-hospital mortality of 31% (n = 32). Patients were discharged to nursing homes (n = 18), intermediate care/rehabilitation facilities (n = 10), or their own residence (n = 40) where initiation or intensification of home care was arranged for 22 patients, and 18 patients were discharged with a rehabilitation plan. A total of 27 patients (27%) were readmitted within 30 days. The overall 30-day mortality was 41% (n = 42) (Table 3 ).
Table 3.
Mortality and discharge destination in102 Danish patients aged 80+ years admitted to hospital with COVID-19.
| All patients (N = 102) | Female (n = 54) | Male (n = 48) | Own residence (n = 73) | Nursing home/intermediate care facility (n = 29) | |
|---|---|---|---|---|---|
| Days from symptoms to confirmed COVID, median (IQR) | 3.0 (1.0–9.5) | 2.0 (1.0–7.0) | 6.5 (2.0–10) | 6.0 (2.0–11) | 1.0 (0.0–2.0) |
| Hospitalization days, median (IQR) | 7.0 (4.0–11) | 6.0 (4.0–10) | 8.0 (5.0–14) | 7.0 (4.0–14) | 6.0 (4.0–9.0) |
| Re-admission < 30 days, n (%) | 27 (27) | 12 (22) | 15 (31) | 21 (29) | 6 (21) |
| 30-day mortality, n (%) | 42 (41) | 14 (26) | 28 (58) | 25 (34) | 17 (59) |
| - During hospitalization | 32 (31) | 11 (20) | 21 (44) | 22 (30) | 10 (35) |
| - After discharge | 10 (9.8) | 3 (5.6) | 7 (15) | 3 (4.1) | 7 (24) |
| Discharge destination, n (%) | |||||
| - Intermediate care facilities/rehabilitation | 10 (15) | 5 (12) | 5 (20) | 9 (18) | 1 (5.3) |
| - Own home (incl. nursing home) |
58 (85) | 38 (88) | 20 (80) | 40 (82) | 18 (95) |
IQR Interquartile range.
3.5. Associations between baseline characteristics and outcome
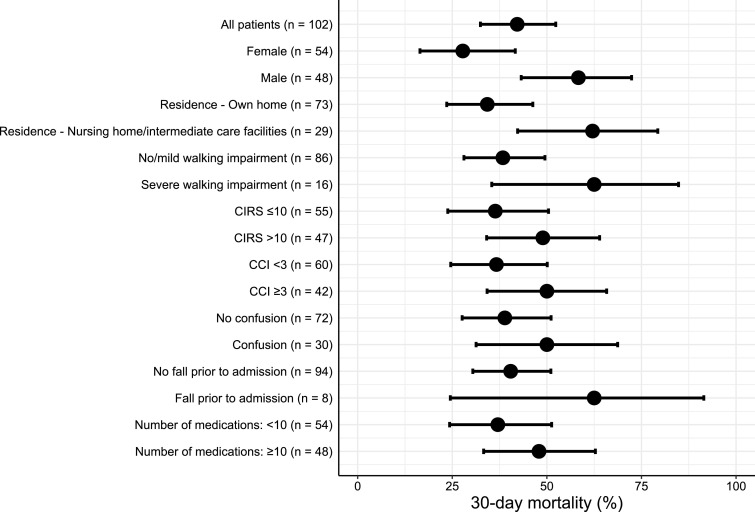
Admission from nursing homes or intermediate care facilities was significantly associated with higher mortality compared with admission from own residence (OR 2.7 95% CI 1.1–6.7) (Fig. 2 ), with a 30-day mortality of 59% and 34%, respectively (p = 0.026). Male sex was also found to be associated with a higher 30-day mortality (OR 4.0 95% CI 1.8–9.5, p = 0.001). 30-day mortality was 48% among patients with high levels of comorbidity (CCI ≥3) compared with 37% among patients with less comorbidity (p = 0.27), and 56% among patients with severe walking impairments (wheelchair or bedridden) compared with 38% among patients with no or mild walking difficulties (walking stick or walking frame) (p = 0.42). In total, 46% of the patients with excessive polypharmacy died within 30 days compared with 37% of the patients receiving less than 10 medications (p = 0.37). A tendency towards a higher 30-day mortality was also seen among patients with falls (63% vs. 39%, p = 0.21) and confusion (50% vs. 38%, p = 0.24) upon admission. In total, 79% of the nursing home residents either died or were readmitted within 30 days.
Fig. 2.
30-day mortality in 102 Danish geriatric patients stratified on baseline characteristics. The whiskers indicate 95% confidence intervals.
Footnote: CIRS, Cumulative Illness Rating Scale; CCI, Charlson Comorbidity Index.
4. Discussion
In this retrospective cohort study of 102 patients ≥80 years admitted with SARS-CoV-2 infection, most patients displayed classical symptoms of COVID-19; fever, cough, respiratory distress, and fatigue. However, many patients also had unspecific symptoms such as confusion, difficulty walking, and falls. Furthermore, the 30-day mortality was very high and associated with frailty.
4.1. Clinical presentation
Our findings are in line with previous data where fever, cough, respiratory distress, and fatigue were found to be the most common symptoms, both within the general population (Docherty et al., 2020; Grant et al., 2020) and among older patients (Niu et al., 2020). Lui et al. found fever to be less frequent (78%) among older patients (>60 years) compared to younger patients (Liu, Chen, Lin, & Han, 2020), which is consistent with the present study where only 75% had fever upon admission. More than half of the patients in a French study of 17 people with COVID-19, with a mean age of 86.5 years, experienced delirium during their hospital stay, and falls were reported in 23% (Godaert et al., 2020). Vrillon et al. also found a high incidence of confusion/delirium (71%) and falls (25%) prior to COVID-19 related hospitalizations among older patients ≥85 years (Vrillon et al., 2020). Unspecific symptoms, such as confusion, falls, and difficulty walking, were also common in the present study. There was a tendency towards higher mortality rates in patients experiencing confusion, although not statistically significant. It is unknown whether delirium is caused by a direct effect of SARS-CoV-2 on the central nervous system or due to multifactorial causes. Marengoni et al. found a significant association between delirium and increased mortality in patients with COVID-19 (Marengoni, Zucchelli, Grande, Fratiglioni, & Rizzuto, 2020), indicating that patients with COVID-19 and simultaneous confusion should be carefully handled. We did not find any significant association between mortality and the geriatric frailty symptoms such as falls, confusion, and difficulty walking. However, the percentage difference in mortality rates was pronounced, and the non-significant findings can probably be explained by the small sample size. Laboratory data including blood samples were also similar to those of more severely affected younger patients in previous studies (Hou et al., 2020) indicating a high severity of disease in our population.
4.2. Comorbidity
The most common pre-existing diseases in the present study were hypertension, heart disease, and respiratory disease. The prevalence of comorbidities was higher than in a previous Danish national cohort by Reilev et al., 2020 which included both hospitalized and community managed patients with SARS-CoV-2 (Reilev et al., 2020). In a recent Swedish study including both SARS-CoV-2 positive and negative patients admitted to a geriatric ward high levels of comorbidity was found to be associated with high in-hospital mortality (Hägg et al., 2020). The present only study found a non-significant association between comorbidity levels and mortality, possibly due to the small sample size.
4.3. Outcomes
The 30-day mortality was 41% in the present study. Whilst high, it is still lower than that seen in international studies where the 30-day mortality among patients above 70 years old has been reported up to 80% (Abbatecola & Antonelli-Incalzi, 2020). Reilev et al. found a 30-day mortality rate of 34% for Danish patients above 80 years (Reilev et al., 2020). The difference in fatalities may as noted above be explained by the inclusion of community managed cases.
The in-hospital mortality was 31%, which is higher than the 24% reported in a Swedish study including 250 geriatric patients with COVID-19. The Swedish patients had less comorbidities, and most patients were community dwelling (Hägg et al., 2020). It is thus unknown whether patients in the present study were frailer with 28% of patients being admitted from nursing homes or intermediate care facilities. Other reasons for the differences in mortality could be different national lock down measures and testing strategies in addition to different health care systems. The mortality rate in the present study was also higher than in previously published studies of COVID-19 cohorts in Denmark, also including younger patients, with mortality rates of 5–25% (Israelsen et al., 2020; Lendorf et al., 2020; Madsen et al., 2020). This confirms that patients aged >80 years have a higher COVID-19 related mortality compared to younger Danish patients with COVID-19. Finally, in the study of Vrillon et al. where a third of the included patients were admitted from long term care facilities in line with the present study, mortality rates were comparable (Vrillon et al., 2020).
In the present study, seventy-four patients were assessed unfit for intensive care at admission, and only three patients were treated in intensive care units. The decision thus relied on the medical assessment of the attending clinicians in cooperation with intensive care doctors, without use of any formal screening tool. It is unknown how many patients who were actually assessed fit for intensive care by the medical team, but who declined. In our study, nursing home/intermediate home residency, polypharmacy, and severe walking impairment was associated with reduced probability of being assessed fit for intensive care. Older age was also found to be negatively associated herewith, but after adjustments for residency, medications and walking impairment, the association was no longer significant. Our findings suggest that clinicians made appropriate decisions concerning fitness for intensive care for most patients. However, implementing a validated frailty screening tool might increase the awareness of identifying vulnerable patients in the future.
Many patients were discharged to rehabilitation units, intermediate care facilities, or were scheduled for municipal rehabilitation. However, many rehabilitation units were closed during the primary stages of the pandemic, which might have decreased the number of patients discharged to rehabilitation units. Overall, only 11 patients were discharged to their own residence without a specialized rehabilitation plan. Our findings indicate that COVID-19 is associated with a severe decline in physical function among older patients.
4.4. Strengths and limitations
To our knowledge, this is one of the first studies investigating the presentation of COVID-19 in an older population. The retrospective nature of this study enabled both living and deceased patients to be included. The use of national Danish Civil Registration numbers and linkage to medical charts made it possible to access all necessary data.
Due to retrospectively registration of symptoms, it is possible that included patients may have experienced further symptoms than described. We only found trends in association between baseline characteristics, geriatric symptoms, and 30-day mortality. This is likely due to the limited number of patients included. Furthermore, the study only included patients with positive SARS-CoV-2 tests, and it remains unknown whether more patients with unspecific symptoms were infected with SARS-CoV-2, but without formal confirmation.
4.5. Perspective and clinical implication
The first wave of the COVID-19 pandemic in Denmark was relatively mild with rapid disease control compared to many surrounding countries. However, mortality rates for older patients were high. The number of persons infected by SARS-CoV-2 is increasing worldwide and a rapid diagnosis of COVID-19 is crucial to prevent further spread of the disease and minimize fatalities. Therefore, preventive efforts to keep older people from being infected with SARS-CoV-2 is of eminent importance.
5. Conclusion
Older patients with SARS-CoV-2 display classical symptoms of COVID-19 such as fever, cough, respiratory distress, and fatigue upon hospital admission. However, unspecific symptoms including confusion, difficulty walking, and falls are also frequent. Patients were rarely assessed fit for intensive care, suffered further functional decline during hospitalization, and mortality rates were high. Our study highlights the need for preventive efforts to keep older people from getting COVID-19 as well as an increased awareness of frailty among older patients with COVID-19.
Funding
The research did not receive any specific grant from funding agencies in the public, commercial, or non-for-profit sectors. This study was funded by Velux foundation (salary to CL, grant number: 18310).
CRediT authorship contribution statement
Linda Katharina Karlsson: Data curation, Writing - original draft. Lasse Hjort Jakobsen: Methodology, Formal analysis, Visualization. Louise Hollensberg: Data curation, Writing - original draft. Jesper Ryg: Conceptualization, Investigation, Methodology, Project administration, Writing - review & editing. Mette Midttun: Data curation, Writing - review & editing. Henrik Frederiksen: Conceptualization, Methodology. Andreas Glenthøj: Conceptualization, Methodology. Anette Raskov Kodahl: Writing - review & editing. Joanna Secher-Johnsen: Data curation, Writing - review & editing. Lene Kongsgaard Nielsen: Data curation, Writing - review & editing. Nuria Gonzalez Bofill: Data curation, Writing - review & editing. Fredrikke Christie Knudtzen: Data curation, Writing - review & editing. Cecilia Margareta Lund: Conceptualization, Methodology, Investigation, Data curation, Project administration, Writing - original draft.
Declaration of Competing Interest
None of the authors reported any conflicts of interest.
References
- Abbatecola A.M., Antonelli-Incalzi R. Editorial: COVID-19 Spiraling of Frailty in Older Italian Patients. The journal of nutrition, health & aging. 2020;24(5):453–455. doi: 10.1007/s12603-020-1357-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andersen T.F., Madsen M., Jørgensen J., Mellemkjoer L., Olsen J.H, et al. The Danish National Hospital Register. A valuable source of data for modern health sciences. Danish medical bulletin. 1999;46(3):263–268. [PubMed] [Google Scholar]
- Charlson M.E., Pompei P., Ales K.L., MacKenzie C.R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. Journal of chronic diseases. 1987;40(5):373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- Clopper C.J., Pearson E.S. The use of confidence or fiducial limits illustrated in the case of the binomial. Biometrika. 1934;26(4):404–413. [Google Scholar]
- Docherty A.B., Harrison E.M., Green C.A., Hardwick H.E., Pius R., Norman L., et al. Features of 20 133 UK patients in hospital with covid-19 using the ISARIC WHO Clinical Characterisation Protocol: Prospective observational cohort study. BMJ (Clinical research ed.) 2020;369:m1985. doi: 10.1136/bmj.m1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fried L.P., Tangen C.M., Walston J., Newman A.B., Hirsch C., Gottdiener J., et al. Frailty in older adults: Evidence for a phenotype. The journals of gerontology. Series A, Biological sciences and medical sciences. 2001;56(3):M146–M156. doi: 10.1093/gerona/56.3.m146. [DOI] [PubMed] [Google Scholar]
- Godaert L., Proye E., Demoustier-Tampere D., Coulibaly P.S., Hequet F., Dramé M. Clinical characteristics of older patients: The experience of a geriatric short-stay unit dedicated to patients with COVID-19 in France. Journal of Infection. 2020;81(1):e93–e94. doi: 10.1016/j.jinf.2020.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant M.C., Geoghegan L., Arbyn M., Mohammed Z., McGuinness L., Clarke E.L., et al. The prevalence of symptoms in 24,410 adults infected by the novel coronavirus (SARS-CoV-2; COVID-19): A systematic review and meta-analysis of 148 studies from 9 countries. PloS one. 2020;15(6) doi: 10.1371/journal.pone.0234765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hägg S., Jylhävä J., Wang Y., Xu H., Metzner C., Annetorp M., et al. Age, Frailty, and comorbidity as prognostic factors for short-term outcomes in patients with coronavirus disease 2019 in geriatric care. Journal of the American Medical Directors Association. 2020 doi: 10.1016/j.jamda.2020.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofman M.R., van den Hanenberg F., Sierevelt I.N., Tulner S.R. Elderly patients with an atypical presentation of illness in the emergency department. The Netherlands journal of medicine. 2017;75(6):241–246. [PubMed] [Google Scholar]
- Hou W., Zhang W., Jin R., Liang L., Xu B., Hu Z. Risk factors for disease progression in hospitalized patients with COVID-19: A retrospective cohort study. Infectious diseases (London, England) 2020;52:1–8. doi: 10.1080/23744235.2020.1759817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Israelsen B.S., Kristiansen T.K., Hindsberger B., Ulrik C.S., Andersen O., Jensen M., et al. Characteristics of patients with COVID-19 pneumonia at Hvidovre Hospital, March-April 2020. Danish medical journal. 2020;67(6) [PubMed] [Google Scholar]
- Lendorf M.E., Boisen K.M., Kristensen L.P., Løkkegaard E.C.L., Krog S.M., Brandi L., et al. Characteristics and early outcomes of patients hospitalised for COVID-19 in North Zealand, Denmark. Danish medical journal. 2020;67(9) [PubMed] [Google Scholar]
- Liu K., Chen Y., Lin R., Han K. Clinical features of COVID-19 in elderly patients: A comparison with young and middle-aged patients. Journal of Infection. 2020;80(6):e14–e18. doi: 10.1016/j.jinf.2020.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madsen L.W., Lindvig O.S., Rasmussen D.L., Knudtzen F.C., Laursen C.B., Øvrehus A., et al. Low mortality of hospitalised patients with COVID-19 in a tertiary Danish hospital setting. International Journal of Infectious Diseases. 2020 doi: 10.1016/j.ijid.2020.10.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marengoni A., Zucchelli A., Grande G., Fratiglioni L., Rizzuto D., et al. The impact of delirium on outcomes for older adults hospitalised with COVID-19. Age and ageing. 2020 doi: 10.1093/ageing/afaa189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niu S., Tian S., Lou J., Kang Z., Zhang L., Lian H., et al. Clinical characteristics of older patients infected with COVID-19: A descriptive study. Archives of gerontology and geriatrics. 2020;89 doi: 10.1016/j.archger.2020.104058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parmelee P.A., Thuras P.D., Katz I.R., Lawton M.P. Validation of the Cumulative Illness Rating Scale in a geriatric residential population. Journal of the American Geriatrics Society. 1995;43(2):130–137. doi: 10.1111/j.1532-5415.1995.tb06377.x. [DOI] [PubMed] [Google Scholar]
- Referenceintervaller. Available: https://www.gentoftehospital.dk/afdelinger-og-klinikker/klinisk-biokemisk-afdeling/tilsundhedsfaglige/Documents/Referenceintervaller%2019.%20aug%202020.pdf Accessed October 19th, (2020). In Danish.
- Reilev M., Kristensen K.B., Pottegård A., Lund L.C., Hallas J., Ernst M.T., et al. Characteristics and predictors of hospitalization and death in the first 11 122 cases with a positive RT-PCR test for SARS-CoV-2 in Denmark: A nationwide cohort. International journal of epidemiology. 2020 doi: 10.1093/ije/dyaa140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resnick N.M., Marcantonio E.R. How should clinical care of the aged differ? Lancet (London, England) 1997;350(9085):1157–1158. doi: 10.1016/S0140-6736(05)63817-2. [DOI] [PubMed] [Google Scholar]
- Shahid Z., Kalayanamitra R., McClafferty B., Kepko D., Ramgobin D., Patel R., et al. COVID-19 and Older Adults: What We Know. Journal of the American Geriatrics Society. 2020;68(5):926–929. doi: 10.1111/jgs.16472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Socialstyrelsen. Statistik över antal avlidna i covid-19. Available: https://www.socialstyrelsen.se/statistik-och-data/statistik/statistik-om-covid-19/statistik-over-antal-avlidna-i-covid-19/ Accessed September 21st, (2020). In Swedish.
- UpToDate. Coronavirus disease 2019 (COVID-19): Clinical features Available: https://www.uptodate.com/contents/coronavirus-disease-2019-covid-19-clinical-features?search=coronavirus%20infection&source=search_result&selectedTitle=3~150&usage_type=default&display_rank=3 Accessed September 21st, (2020).
- Vrillon A., Hourregue C., Azuar J., Grosset L., Boutelier A., Tan S., et al. COVID-19 in older adults: A series of 76 patients 85 years old and above with COVID-19. Journal of the American Geriatrics Society. 2020 doi: 10.1111/jgs.16894. [DOI] [PMC free article] [PubMed] [Google Scholar]