Abstract
China had suffered the COVID-19 outbreak from the end of 2019, SARS-CoV-2 began to spread secretly within the community and in hospitals, causing numerous citizens to be infected without knowing it. After the official confirmation of COVID-19, hospital diagnosis and treatment systems were under great pressure, and medical supplies were scarce. Then the pandemic experienced an explosive growth and quickly peaked. In order to respond to the challenge, the Chinese government quickly built hospitals, adjusted the diagnosis and treatment systems, deployed medical staff to support areas affected by the epidemic, isolated and treated infected patients as much as possible, reminded citizens to use good protection, and controlled the epidemic step-by-step. In this paper, we used official published data and medical literature about the transmission of COVID-19 as well as prevention and control guidelines issued by the Chinese government and hospitals, adopted a multi-dimensional analysis framework, divided the outbreak into three phases: (1) “blind man touching the elephant” phase, (2) “opening Pandora’s box” phase, (3) “whole offensive and whole defensive tactics” phase. This was done to describe the development of and response to the pandemic. This paper suggested that when dealing with similar outbreaks in the future, we should do a better job of providing protective guidance and material reserves in advance, strengthen the emergency response capacity of medical institutions, and aim to share this information with the public medical systems of other countries which also face severe tests.
Keywords: Covid-19, Disease, Stage, Control, Resource
Introduction
COVID-19 appeared secretly in Wuhan, Hubei Province, China. Cases first appeared in early December 2019 [1]. However, the local health authorities did not accurately identify COVID-19 at the beginning. It took more than a month for the pandemic to spread throughout China. On January 20, 2020, the Chinese government had begun to announce COVID-19 as a “Class B” infectious disease and implemented a “First-Level” public health emergency response1 . On the one hand, the Chinese government had taken tough non-medical measures, including locked-down cities, canceled flights and road and rail transport, closed public places, extended Spring Festival holidays, restricted residents from going out in public, obliged citizens to wear masks, along with other severe measures. On the other hand, the Chinese government used a large number of medical resources, established fever clinics, special isolation wards, severe patient hospitals, and temporary shelter hospitals. Millions of medical staff participated in treating those diagnosed with the virus. It was not easy to control the pandemic, and the number of casualties was high. According to the statistics from the Chinese National Health Commission, at present there are more than 84,451 confirmed patients and 4664 deaths (These data do not include the number of asymptomatic infections. Since April 1, 2020, China had only counted asymptomatic infections, currently about 6000). 3019 Chinese medical staff were infected with SARS-CoV-2 according to nucleic acid tests and 1716 confirmed to have COVID-19. At least 13 medical staff members died2 . This set off a warning alarm worldwide. It was necessary to review publicly available information from Chinese health department documents, published journal articles, policies and guidelines. This study identified the infectious disease transmission environment and response mechanisms in the early stage of the outbreak in China and drew some lessons.
Aims
This report intended to retrace China’s pandemic chronologically, explained what response China’s disease control system had set, determined what treatment Chinese medical staff administered to combat COVID-19 in the past five months, and introduced experience and lessons about controlling the pandemic. This research may provide a different perspective from the fundamental research and review, for it used more health information than literature.
Access to Chinese Health Information
The data and information about COVID-19 in China had been gathered from various sources. First, we used official data from the Chinese National Health Commission, the Chinese Center for Disease Control and Prevention, and the Health Departments of various Provinces. These data were published online. Secondly, due to insufficient official data, we also used the infection data disclosed by the media and looked for hospital data and case reports using research reports. Third, we collected COVID-19 diagnosis and treatment plans, prevention and control guidelines, medical experts’ public statements, and hospital operation reports. These sources could more effectively reflect the actual state of China’s public health system in the past few months.
Result
The initial stage of “blind man touching the elephant”: from December 2019 to Mid-January 2020.
In early December 2019, some respiratory disease patients were found in Wuhan, Hubei, China. They had symptoms of fever and dry cough, similar to seasonal flu at initial diagnosis, but after lung imaging examination and respiratory tract specimen inspection, the symptoms were found to be more serious than the flu. Some patients had difficulty breathing and were transferred to the ICU ward. These people were earliest group of COVID-19 patients3 . Therefore, the hospital reported them as unexplained pneumonia cases to the Wuhan Municipal Health Department. The health department could not immediately assess the destructive power of the disease. In order to stabilize society, the official explanation was that the disease was preventable and controllable, and there was no need to panic. Residents were advised to open windows for ventilation to maintain indoor air circulation and avoid closed, non-ventilated, crowded places4 .
At the same time, the Wuhan Center of Disease Control and Prevention launched preliminary epidemiological investigations, and found these patients were closely related to a seafood market. The Wuhan Municipal Government decided to close this seafood market and implemented disinfection, but were unable to trace and isolate the businessmen of the market5 . After efforts of scientists, the virus samples collected from patients with unexplained pneumonia were confirmed as a new coronavirus [2]. On January 13, 2020, the World Health Organization officially named it 2019n-COV, or SARS-COV-2 [3].
Undoubtedly, SARS-CoV-2 had spread secretly throughout Wuhan city from that moment. The main means of transmission was community infection. Later research confirmed that SARS-CoV-2 was mainly transmitted through droplets virus concentration was high in confirmed patients and suspected patients [4]. The virus can also be transmitted by close contact. The virus had a strong vitality, with the ability to survive for 4 h on copper surfaces, 24 h on cardboard, and 3 days on plastic surfaces. If the temperature and humidity were appropriate, it can survive for about 7 days on the surface of masks [5]. The World Health Organization believed that the infectivity of the SARS-CoV-2 was very strong, and the R0 index estimated value of Chinese researchers was 1–2.5 [6]. Some foreign researchers believed that the R0 index had reached an astonishing 5.7 [7].
The second channel of infection was travel. It was estimated that at least 5 million people left Wuhan for other regions of the China and some foreign countries, and the population from other areas entering or passing through Wuhan cannot be estimated effectively. In closed vehicles, especially when using air conditioners, the virus density was very high. Some studies also suggested that aerosols may also be a way of transmission [8].
In addition to these modes of transmission, nosocomial infections were also quite serious. In the process of diagnosis, medical staff needed to contact patients closely to talk and examine, and easily touchedoral and nasal droplets from patients. Some literature found that patients’ saliva, tears, conjunctival secretions. Urine, feces, and anal swab samples can detect the virus [9]. In the clinic rooms and in-patient wards, the objects and medical instruments that patients had been exposed to may become the source of infection. Chinese medical staff in many hospitals did not have this information and had no additional personal protection, yet still performed common diagnosis and treatment processes and were infected by virus.
Since the COVID-19 data statistics system of the Chinese Health Commission only started on January 20, 2020, it was still a mystery how many people were infected with SARS-CoV-2 before this time. Some literature and news reports simulated the scale of infected people. For example, at Wuhan Union Hospital, 14 neurosurgery staff members who were infected by a COVID-19-positive patient during surgical treatment. (This was also the first nosocomial infection case confirmed by the high level expert group of the Chinese National Health Commission) [10].
The following phase of “opening Pandora’s box”: from Mid-January to the end of January 2020.
With the rise of pandemic in China and the appearance of cases abroad, some medical experts also issued warnings. Chinese officials realized the seriousness of the situation. The Wuhan Government began to advise people to wear masks when they went out. The Wuhan Health Department required all patients with fever to have lung CT examination, and patients with symptoms of lung infection were also required to take throat swab samples to be sent to the Center for Disease Control and Prevention for nucleic acid testing. Infectious disease specialist hospitals were ordered to use isolation wards to accommodate such patients6 . The Chinese National Health Commission also sent an expert group to Wuhan to investigate the conditions. The expert group concluded that the SARS-CoV-2 had already undergone severe human-to-human transmission in Wuhan. The scale of the spread was no less than that of the SARS in 2003, and the Chinese government recommended taking immediate measures to stop the pandemic7 .
After weighing the pros and cons, the Chinese government announced on January 20, 2020, that COVID-19 was graded as a kind of “Class B” infectious disease and upgraded its control measures to “Class A” level. In China, the current “Class B” infectious diseases include: SARS, AIDS, viral hepatitis, poliomyelitis, human infection with highly pathogenic avian influenza, measles, epidemic hemorrhagic fever, rabies, epidemic encephalitis B, dengue fever, anthrax, bacterial and amoebic dysentery, tuberculosis, typhoid and paratyphoid, epidemic cerebrospinal meningitis, pertussis, diphtheria, neonatal tetanus, scarlet fever, brucellosis, gonorrhea, syphilis, leptospirosis, schistosomiasis, malaria, influenza A (H1N1), etc. Among these diseases, human infection with highly pathogenic avian influenza, dengue fever and influenza A (H1N1) had occurred in China in recent years. However, there were only two kinds of “Class A” infectious diseases: plague and cholera, and both were very deadly diseases. Every Province had implemented “First-Level” public health emergency responses, and this made COVID-19 the top public health enemy in China.
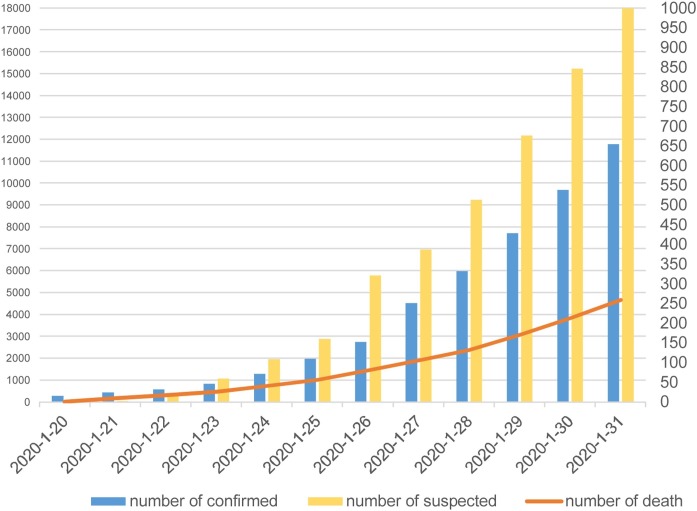
The announcement of the pandemic caused great panic, and a large number of patients with fever or cough symptoms flocked to hospitals. According to the Chinese National Health Commission daily reporting system, it can be seen that by January 24, 2020, the number of confirmed patients exceeded 1000, January 28 exceeded 5000, and January 31 exceeded 10,000 (Fig. 1 ). These were only data of people who had the opportunity to undergo nucleic acid testing, and there were a large number of suspected patients waiting for testing. Due to insufficient testing reagents and testing staff in the Centers for Disease Control and Prevention, many cases could not be confirmed in a short time.
Fig. 1.
The pandemic trend in the end of January 2020.
The real situation in the hospitals was confusing. In the face of a sudden increase in patients, the number of medical staff was not sufficient. According to data from Wuhan City, Hubei Province, there were 39,600 licensed doctors and 54,400 registered nurses in 20188 . The medical staff of respiratory departments, infectious disease departments and ICU departments were only a small part of the total number, and they were unable to cope with so many patients at once. Due to the urgency of the situation, medical staff from other departments also participated in the treatment of COVID-19 patients. They worked very diligently. The media concluded that from January to February 2020, the average working time of first-line doctors reached 50–60 h per week and the working time of nurses reached 40 h per week9 . According to statistics from the Wuhan Municipal Health Commission, in the last 10 days of January2020, at least 600 medical staff were infected10 . At the same time, many hospitals were facing the problem of a shortage of medical supplies, especially in Hubei Province, which was located at the center of the epidemic. Hubei had a serious shortage of medical devices, drugs, and protective materials. On the one hand, the rapid growth of patients led to a large consumption of medical masks, protective clothing, goggles and disinfectants; on the other hand, the original reserves were insufficient, coupled with the traffic blockade and the shutdown of factories during the Spring Festival holidays, a supply of materials was not guaranteed. According to regulations, disposable masks should be replaced after a single use, N95 medical masks should be replaced at most once every 4 h, medical protective clothing should avoid contact with water, and goggles must be equipped however, not every hospital could met these regulatory criteria11 .
The Chinese government began to think of various ways to quell the situation. Firstly, in terms of diagnosis, the Chinese National Health Commission integrated the laboratory test, imaging test, and reagent test methods and put forward two unified confirmed standards of COVID-19 testing. The first one was the RT-PCR of respiratory samples or blood samples reported positive, and the second was the viral gene sequencing of homologous accordance with SARS-CoV-212 . Secondly, in terms of virology research, the Chinese National Health Commission agreed that some medical institutions should carry out experimental activities related to the SARS-CoV-2 in order to help biotechnology companies develop nucleic acid test kits and vaccines. Thirdly, the Chinese National Medical Products Administration opened green channel and emergency approval for manufacturers of drugs, masks, protective clothing, etc.13 . Fourth, because hospitals had never encountered this disease before, the Chinese National Health Commission recommended several drugs in the diagnosis and treatment plan, including influenza drugs, antiviral drugs, drugs recommended by experts, and some traditional Chinese medicine14 . Fortunately, COVID-19 did not cause irreparable losses in this period, and this was mainly due to the destructive power of COVID-19 differing between various age groups. Infected young people have slight symptoms, sometimes no symptoms, and their lungs do not sustain lasting damage, which was similar to the effects of yearly influenza. The majority of severe cases and deaths were patients over 60-years-old15 .
The key phase of “whole offensive and whole defensive tactics”: from February 2020 to present.
The Chinese government was aware of the serious stress on the health-care system in the epidemic area, and also found that many suspected patients could not be tested and hospitalized, and thus became major sources of infection. If this situation had continued, it would be impossible to restart the economy. To this end, the health-care system must be given greater support. A reduced the burden on the health-care system by reducing the number of infected people in the community was necessary. The former was an offensive strategy, the latter was the defensive strategy.
In terms of the offensive strategy, the Chinese government adjusted the routine and adjusted the medical system. From February 2020, the Chinese National Health Commission had proposed a hierarchical diagnosis and treatment program. COVID-19 patients would be treated in infectious disease hospitals and respiratory diseases specialist hospitals (pulmonary hospitals) and large hospitals would be designated. These hospitals stopped other medical services. In Wuhan, Hubei, there were 37 hospitals serving these ends16 . These hospitals had been transformed according to the requirements of infectious disease hospitals to increase their protection equipment. Other hospitals were no longer permitted to treat patients with fever symptoms. The Chinese government had built two hospitals in Wuhan (Leishenshan Hospital and Huoshenshan Hospital), equipped with 2500 beds and ICU equipment, which were specially used for the treatment of severely ill patients. The Chinese government had also set up 16 Shelter Hospitals in Wuhan, and provided 20,000 beds for the treatment of mild patients17 . The Chinese National Health Commission began to dispatch troops and medical teams from various Provinces to support Hubei Province, and successfully convened more than 45,000 medical staff18 , greatly improving the medical staff/patient ratio in the epidemic’s center.
The Chinese National Health Commission and Chinese Center for Disease Control and Prevention compiled the COVID-19 Prevention and Control Plan and the COVID-19 Diagnosis and Treatment Plan to guide the diagnosis and treatment in hospitals. The expert group of the Chinese National Health Commission recommended ɑ-interferon, Lopinavir, Ritonavir, Ribavirin, Chloroquine hydrochloride, Remdesivir, Tozumab and Chinese Herbal Medicine for clinical use. The throat swab nucleic acid detection reagent was developed and SARS-CoV-2 IgG and IgM serological diagnostic kits were also developed as auxiliary diagnostic means19 . The Chinese government also accelerated the production and procurement of medical equipment, ensuring an adequate supply of masks, protective clothing, ventilators, and testing reagents.
Regarding the defensive strategy, the Chinese National Health Commission requested hospitals to strengthen the prevention of nosocomial infections. According to regulations published by the health department and hospitals, all patients and medical staff must wear masks and take temperature measurements and all hospitals had turned off the central air conditioning, even when it was still in winter. Furthermore, outpatient rooms and wards would only use electric blankets, heating lamps, other heat preservation measures, and disinfected the air20 . All hospitals that had COVID-19 patients upgraded disinfection measures, such as disposable waste syringes, transfusion devices, surgical or infected wound dressings, heavily contaminated clothing, and any other equipment and materials (clothing, bedding, towels, plates, cups, sputum boxes, toilets) that patients had ever touched such as chairs, door handles, faucets, floors, walls, doors, and window. Patients’ excrement and domestic garbage were disinfected completely. The medical staff working in fever clinics and in-patient departments wore surgical gowns on the inside, and then wore disposable surgical clothes on the outside. The third layer was a one-piece protective clothing and the fourth layer was disposable surgical clothing. One short shoe cover inside the protective clothing, one long shoe cover outside the protective clothing, three to four layers of gloves, one N95 mask, one surgical mask, and one eyepiece to ensure the COVID-19 virus was isolated in vitro21 . Besides the supplemental support, medical staff were also rotated and given vacation time. According toinformation released by the Chinese National Health Commission, it had recently been possible for doctors to work 1 day, rest 1.5–2 days, work 25–30 h a week and nurses to work 1 day, rest 2.5–3 days, and work 20 h a week. A rotation system was adopted in the shelter hospitals where the patients’ symptoms were less severe. A group of 4 medical staff was formed to take care of 50 patients, which would be rotated every 6 h22 .
In terms of preventing community infections, the Chinese government had implemented strict blockade and quarantine measures. Suspected patients would be isolated, observed and treated on site, and their close contacts would be subject to centralized or home-based medical observation according to the situation. The railway, transportation, and civil aviation stations, vehicles, passengers, and materials would be subject to quarantine inspection and interception.
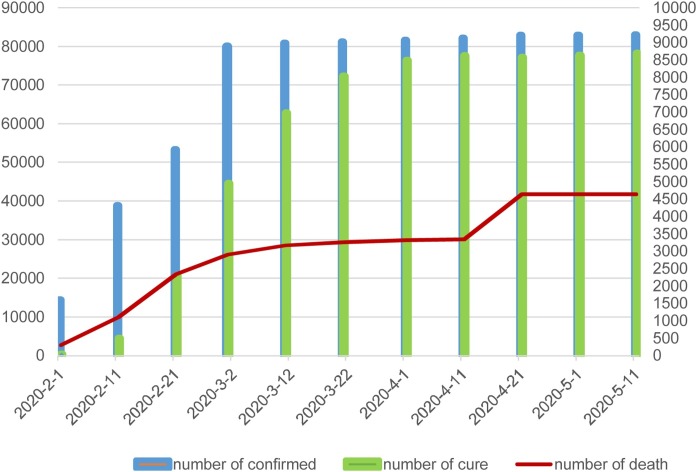
During this period, although the number of confirmed patients had exceeded 20,000 on February 3, exceeded 30,000 on February 6, exceeded 40,000 on February 9, exceeded 60,000 on February 14, exceeded 70,000 on February 16, and exceeded 80,000 on March 1, most patients were able to receive medical support or be taken care of in isolation, and the number of cured surpassed the number of confirmed cases, which were dropping rapidly. The pandemic was in a phase of reversal (Fig. 2 ). There were also some less optimistic messages, such as the source and host of the SARS-CoV-2 not being confirmed. Very few patients’ nucleic acid tests showed positive again after discharge, but we can be confident the medical system had passed the most difficult time.
Fig. 2.
The pandemic trends from February 2020 to May 2020.
Discussion
In recent years, hospital facilities and the quality of medical staff in China has improved greatly, but they still paid a heavy price when hurriedly confronted with the COVID-19 pandemic. First, it must be admitted that SARS-CoV-2 had many transmission channels, strong transmission powers, and high infectious risks. Secondly, in the face of the outbreak, the medical system was exhausted by coping with and had the “broken window” effect. Thirdly, protection guidelines were not comprehensive and the protection vigilance had not been upgraded to the highest level, and the supply of protective materials were not received in a timely manner. In addition, we can see some hidden problems in hospital construction and the public health emergency system in China from the above clues. In terms of hospital construction, the scale and funding of infectious disease departments in specialist hospitals and general hospitals were not enough to cope with a large-scale pandemic. In terms of the public health emergency system, infection prevention training for all medical staff also needs to be carried out continuously.
There are two aspects worth discussing. One was the actual scale of infection. The Chinese National Health Commission set strict standards for the diagnosis of the COVID-19, including clinical manifestations, chest imaging changes, and nucleic acid testing. The number of patients meeting the above three conditions was 84,451. But were there any uncounted patients? Early experts warned that there had been cases without fever symptoms and cases without a clear source of infection or direct contact history, which indicated that the SARS-CoV-2 may lurk in the population and spread from time to time [11]. Recently, the Chinese National Health Commission started compiling statistics and monitoring asymptomatic infections and also planned comprehensive nucleic acid testing in Wuhan, the epidemic center23 . The asymptomatic infections in China could be an unexploded bomb in the public health system.
Another issue was how to reduce infection. In front of the pandemic, medical measures were necessary, but they were not omnipotent. In addition to upgrade medical equipment, the interruption of the infection source was very important. China had forced isolation to a large number of suspected patients through regular hospitals, temporary hospitals, and hotels, forced all people wearing masks and measure temperature. These can reduce the pressure of the medical system, and can increase the difficulty of virus transmission. Taking this approach would not only increase the cost of social management, but also have an adverse impact on the economy, but compared to human life, this price was worth it.
Conclusion
COVID-19 was the most serious public health disaster that the world facing today [12]. China was the force to fight against the pandemic. It had brought some lessons, including lack of protective facilities, inadequate protection information and unscientific diagnosis and treatment system. This also prompted public health authorities to make early efforts to give a decisive warning, to establish a comprehensive protection network to prevent infection in terms of cognition, equipment, technology, etc.
Funding
Supported by the Fujian Pronvince Social Science Fund, China (Grant No. FJ2018B034) and project of Fujian Institute of Petition Theory and Practice, China (Grant No. 2020-12).
Competing interests
None declared.
Ethical approval
Not required.
Footnotes
According to the announcement of Chinese National Health Commission. Available at http://www.nhc.gov.cn/xcs/zhengcwj/202001/44a3b8245e8049d2837a4f27529cd386.shtml.
According to the data released by Chinese National Health Commission. Available at http://www.nhc.gov.cn/xcs/yqtb/list_gzbd.shtml.
According to the report of Wuhan Municipal Health Committee on viral pneumonia of unknown cause. Available at http://www.nhc.gov.cn/xcs/yqtb/202001/1beb46f061704372b7ca41ef3e682229.shtml.
According to the bulletin of novel coronavirus pneumonia by Wuhan Municipal Health Commission. Available at https://www.sohu.com/a/367976308_114731.
According to the information release by Wuhan Municipal Government. Available at http://finance.sina.com.cn/chanjing/gsnews/2020-01-02/doc-iihnzahk1439267.shtml.
According to the information released by Wuhan Municipal Health Commission. Available at http://wjw.wuhan.gov.cn/ztzl_28/fk/fkdt/202004/t20200430_1196725.shtml.
According to the information released by Chinese National Health Commission. Available at http://www.nhc.gov.cn/xcs/fkdt/202001/de5f07afe8054af3ab2a25a61d19ac70.shtml.
According to the data released by Chinese National Bureau of Statistics. Available at http://www.stats.gov.cn/tjsj/ndsj/2018/indexch.htm.
According to the data released by Chinese National Health Commission. Available at http://www.nhc.gov.cn/zhuz/zbwqhg/wqhg.shtml.
According to the data released by Wuhan Municipal Health Commission. Available at http://wjw.wuhan.gov.cn/front/web/ztzl/801.
According to the data released by China Xinhua News Agency. Available at http://www.xinhuanet.com/politics/xxgzbdgrdfyyq/kyqyp.htm.
According to the diagnosis and treatment plan of novel coronavirus infection pneumonia released by Chinese National Health Commission. Available at http://www.chinacdc.cn/jkzt/crb/zl/szkb_11803/jszl_11815/202001/t20200123_211391.html.
According to the information released by Chinese National Medical Products Administration. Available at http://www.nmpa.gov.cn/WS04/CL2578/374195.html.
According to the novel coronavirus infection common medical protective products use guidelines released by Chinese National Health Commission. Available at http://www.chinacdc.cn/jkzt/crb/zl/szkb_11803/jszl_11815/202001/t20200128_211490.html.
According to the news press information released by Chinese National Health Commission. Available at http://www.nhc.gov.cn/xcs/s7847/202001/d86af022fb8644bea764cffe5e119e69.shtml.
According to the data released by Wuhan Municipal Health Commission. Available at http://wjw.wuhan.gov.cn/ztzl_28/fk/fkdt/202004/t20200430_1197152.shtml.
According to the data released by Wuhan Municipal Health Commission. Available at http://wjw.wuhan.gov.cn/ztzl_28/fk/fkdt/202004/t20200430_1198778.shtml.
According to the data released by Chinese National Health Commission. Available at http://www.nhc.gov.cn/xwzb/webcontroller.do?titleSeq=11235&gecstype=1.
According to the news press information released by Chinese National Health Commission. Available at http://www.nhc.gov.cn/xcs/s3574/202003/c629cbbbe787428187119405e2d1187a.shtml.
According to the prevention and control plan of new coronavirus infection pneumonia released by Chinese National Health Commission. Available at http://www.chinacdc.cn/jkzt/crb/zl/szkb_11803/jszl_11815/202001/t20200123_211379.html.
According to the data released by Chinese National Health Commission. Available at http://www.nhc.gov.cn/xcs/yhfc/list_gzbd.shtml.
According to the data released by Chinese National Health Commission. Available at http://www.nhc.gov.cn/xcs/zhengcwj/list_gzbd.shtml.
According to the news press information released by Chinese National Health Commission. Available at http://www.nhc.gov.cn/xcs/s3574/202005/04140b74b7534064aef778258e668e4a.shtml.
References
- 1.Cohen J., Normile D. New SARS-like virus in China triggers alarm. Science. 2020;367:234–235. doi: 10.1126/science.367.6475.234. [DOI] [PubMed] [Google Scholar]
- 2.Peng F.J., Tu L., Yang Y.S., Peng H., Wang R.S., Hu Q.Y. Management and treatment of COVID-19: the Chinese experience. Can J Cardiol. 2020;36(6):915–930. doi: 10.1016/j.cjca.2020.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization . 2020. Coronavirus disease 2019 (COVID-19) situation report-1.https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200121-sitrep-1-2019-ncov.pdf?sfvrsn=20a99c10_4 Available at: [Google Scholar]
- 4.Chinese Center for Disease Control and Prevention . 2020. Epidemic update and risk assessment of 2019 novel coronavirus.http://www.chinacdc.cn/yyrdgz/202001/P020200128523354919292.pdf Available at. [Google Scholar]
- 5.Chen S.M., Yang J.T., Yang W.Z., Wang C., Bärnighausen T. Covid-19 control in China during mass population movements at new year. Lancet. 2020;395(10226):764–766. doi: 10.1016/S0140-6736(20)30421-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yu X., Li N. How did Chinese government implement unconventional measures against covid-19 pneumonia. Risk Manag Healthc Policy. 2020;13:491–499. doi: 10.2147/RMHP.S251351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Landes S., Stevens D., Turk M. Research Gate; 2020. COVID-19 and pneumonia: increased risk for individuals with intellectual and developmental disabilities during the pandemic. [DOI] [Google Scholar]
- 8.Novel Coronavirus Pneumonia Emergency Response Epidemiology Team The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) in China. Zhonghua Liu Xing Bing Xue Za Zhi. 2020;41(February (2)):145–151. doi: 10.3760/cma.j.issn.0254-6450.2020.02.003. [DOI] [PubMed] [Google Scholar]
- 9.Tang B., Bragazzi N.L., Li Q., Tang S.Y., Xiao Y.N., Wu J.H. An updated estimation of the risk of transmission of the novel coronavirus (2019-nCov) Infect Dis Model. 2020;5(February):248–255. doi: 10.1016/j.idm.2020.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Special Expert Group for Control of the Epidemic of Novel Coronavirus Pneumonia of the Chinese Preventive Medicine Association An update on the epidemiological characteristics of novel coronavirus pneumonia (COVID-19) Zhonghua Liu Xing Bing Xue Za Zhi. 2020;41(February (2)):139–144. doi: 10.3760/cma.j.issn.0254-6450.2020.02.002. [DOI] [PubMed] [Google Scholar]
- 11.Firth J.A., Hellewell J., Klepac P., Kissler S., CMMID COVID-19 Working Group, Kucharski A.J. Using a real-world network to model localized COVID-19 control strategies. Nat Med. 2020;26(10):1616–1622. doi: 10.1038/s41591-020-1036-1038. [DOI] [PubMed] [Google Scholar]
- 12.Berger Z.D., Evans N.G., Phelan A.L., Silverman R.D. Covid-19: control measures must be equitable and inclusive. BMJ. 2020;368:1141. doi: 10.1136/bmj.m1141. [DOI] [PubMed] [Google Scholar]