Abstract
Objectives
We aimed to estimate the time-varying transmission dynamics of COVID-19 in China, Wuhan City, and Guangdong province, and compare to that of severe acute respiratory syndrome (SARS).
Methods
Data on COVID-19 cases in China up to 20 March 2020 was collected from epidemiological investigations or official websites. Data on SARS cases in Guangdong Province, Beijing, and Hong Kong during 2002–3 was also obtained. We estimated the doubling time, basic reproduction number (R0), and time-varying reproduction number (Rt) of COVID-19 and SARS.
Results
As of 20 March 2020, 80,739 locally acquired COVID-19 cases were identified in mainland China, with most cases reported between 20 January and 29 February 2020. The R0 value of COVID-19 in China and Wuhan was 5.0 and 4.8, respectively, which was greater than the R0 value of SARS in Guangdong (R0 = 2.3), Hong Kong (R0 = 2.3), and Beijing (R0 = 2.6). At the start of the COVID-19 epidemic, the Rt value in China peaked at 8.4 and then declined quickly to below 1.0 in one month. With SARS, the Rt curve saw fluctuations with more than one peak, the highest peak was lower than that for COVID-19.
Conclusions
COVID-19 has much higher transmissibility than SARS, however, a series of prevention and control interventions to suppress the outbreak were effective. Sustained efforts are needed to prevent the rebound of the epidemic in the context of the global pandemic.
Keywords: COVID-19, SARS, China, Time-varying reproduction number
Introduction
Eighteen years ago, severe acute respiratory syndrome (SARS) broke out globally, with more than 8000 cases and a fatality rate of 9.6% (World Health Organization, 2003a). Since December 2019, an emerging pneumonia infection caused by the novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), now named as coronavirus disease 2019 (COVID-19), broke out in Wuhan, China. COVID-19 has now become a global pandemic (Nation Health Commission of the People’s Republic of China, 2020a, Epidemiology Working Group for NCIP Epidemic Response et al., 2020, World Health Organization, 2020). As of 17 July 2020, 215 countries or regions have reported cases of the COVID-19 infection, with more than 14 million infections and approximately 0.6 million deaths (https://www.worldometers.info/coronavirus/).
It is necessary to understand the etiological, epidemiological and clinical characteristics of an emerging infectious disease in order to take effective prevention and control measures. Several studies have described the epidemiological and clinical characteristics of COVID-19 (Chen et al., 2020a, Epidemiology Working Group for NCIP Epidemic Response et al., 2020). A few studies have also estimated the basic reproduction number (R0) of COVID-19 at the early stage of the epidemic (Liu et al., 2020, Tang et al., 2020, Tian et al., 2020). Li et al computed an R0 value of 2.2 using daily COVID-19 data before 4 January 2020 in Wuhan (Tang et al., 2020) and Tian et al reported an R0 value of 3.15 before 23 January 2020 across China (Tian et al., 2020). Our study, using early epidemic stage data, found the R0 value of COVID-19 was 2.9 in China (Liu et al., 2020). As indicated, most of these studies looked at daily reporting of cases only at the very early stage of the epidemic or were based purely on mathematical modeling.
It has been suggested that unknown etiology and the lack of a diagnostic protocol at the early stage of the epidemic (Zhao et al., 2020) may have led to an underestimation of the R0 value. In addition, for control measures to be optimized during an epidemic, temporal changes in the reproduction number must be tracked. However, none of the previous studies estimated the time-varying reproduction number (Rt) for the whole of China, which is an important index for assessing whether the control and prevention measures are effective (Inglesby, 2020, Pan et al., 2020a, Thompson et al., 2019). Moreover, the cases from Hubei Province were exported to other provinces in China and led to secondary cases in those provinces, however, the Rt value of the secondary cases in those provinces was not fully known.
As a milestone in global public health, the transmission dynamics of SARS have been much studied (Bauch et al., 2005, Hui et al., 2004). However, the difference in transmission characteristics between COVID-19 and SARS are not well understood. Comparing the transmissibility of COVID-19 with SARS could assist decision making on the prevention and control of COVID-19. In this study, we describe the transmission dynamics of COVID-19 as well as the synchronous public health interventions in China.
Methods
Data collection
The record of daily confirmed COVID-19 cases across China was collected for up to and including 20 March 2020; at this date there had been no local cases reported in China for three consecutive days. Though some imported cases from other countries were reported between 26 February and 20 March, no local linked cases were reported as of 20 March. Therefore we used these locally acquired cases in China to study transmission dynamics during this period. Each COVID-19 case was defined based on the Diagnosis and Treatment Scheme of COVID-19 released by the National Health Commission of China (National Health Commission of the People’s Republic of China, 2020b). For cases in Guangdong Province, China, individual data including the date of onset of symptoms, hospitalization and diagnosis was obtained from medical records and epidemiological investigations. We collected the daily number of reported cases in other provinces of China from official websites (http://www.nhc.gov.cn/).
We obtained the daily number of SARS cases during 2002–3 in Guangdong Province from the Guangdong Provincial Center for Disease Control and Prevention (GDCDC). The daily number of SARS cases in Beijing (from 5 March to 29 May 2003) and Hong Kong (from 15 February to 31 May 2003) were obtained from Pang et al’s report (Pang et al., 2003) and the WHO website (World Health Organization, 2003b), respectively.
Estimating the daily incidence of COVID-19
In this study, since we did not have the symptoms onset date of COVID-19 cases outside Guangdong Province, the daily incidences in Wuhan and China were estimated using a generalized additive model (GAM) on the basis of the relationship between the date of onset of symptoms and the date of case reporting. First, we collected the onset date and the reporting date for each case in Guangdong province, which was considered as a sample of all confirmed cases in China. Second, a GAM was used to establish the relationship between onset date and reporting date, which provided a lagged probability distribution of daily incidences (Figure S1). Third, we used the lagged probability distribution to predict daily incidence based on the daily number of reported cases in Wuhan and China. We used the onset date and reporting date of cases outside the GAM as test sets to verify the effectiveness and accuracy of this method. We applied linear regression to estimate the association between actual incidence and estimated incidence, and the results of cross-validation showed that the β was 0.84 (P < 0.05), the R2 was 89.7%, and the root mean square error (RMSE) was 4.11 (Figure S2).
Estimation of reproduction number
Basic reproduction number (R0)
In this study, we estimated the R 0 value by analyzing data on the cases with symptoms onset between 1 January and 6 February 2020, because we expected the number of infections identified would increase rapidly after the festival of New Year's Day on 1 January. The Level-I response to major public health emergency was issued in succession from 23 January across China, however, the cases continued to increase for days with a peak on 6 February. The R0 value is defined as the expected number of secondary cases produced by an infected case in a fully susceptible population. Since the daily incidence data is an integer, Poisson regression was used to fit the exponential growth rate. A likelihood-based (ML) method was used to estimate the R0 value which assumes that the total number of secondary cases infected by a single primary case follows a Poisson distribution. The formula is as follows:
Where Nt denotes the number of symptoms onset cases observed on day t and w denotes the generation time distribution. We applied a Gamma distribution for the generation time, with a shape parameter (mean generation time [GT] of 7.5 days) and a scale parameter (standard deviation [SD] of 3.4 days) following a previous study (Tang et al., 2020).
We also estimated the R0 value for secondary cases of COVID-19 in Guangdong Province. Given that Guangdong has implemented countermeasures in early stage of COVID-19 epidemic, the R0 value in Guangdong Province could also be regarded as effective reproduction number.
Time-varying reproduction number (Rt)
The time-varying reproduction number (Rt) represents the average number of secondary cases that would be produced by a typical primary case infected at time t if conditions remained constant after time t (Thompson et al., 2019), Rt is an indicator to measure the transmission of COVID-19 before and after the interventions.
We applied a Bayesian framework to estimate the Rt value of COVID-19, following a previous study (Thompson et al., 2019), which used a Gamma distributed prior, conjugated to the Poisson likelihood, and obtained an analytical formulation of the posterior distribution of Rt. In this process, the posterior distribution for Rt given the incidence data, is conditional on the GT distribution. To maintain the accuracy of the prediction and without hiding the underlying time trend, Rt values were estimated over a 10-day moving window. For the period of estimation, the end date was selected as the latest date of the available data, and the starting date was selected as the earliest date for which the 10-day instantaneous reproduction number estimated above could be assumed constant. We estimated the Rt value of COVID-19 transmission in China, and in Wuhan, and for secondary COVID-19 transmission in Guangdong Province. We also estimated the Rt value of SARS transmission in Guangdong Province, Hong Kong, and Beijing.
Statistical analysis
We applied frequency and percentages (%) to describe categorical variables and used mean ± SD to describe the continuous variables. The doubling time of COVID-19 and SARS cases were defined and estimated using a method proposed by Galvani et al. (2003).
Sensitivity analysis
A series of sensitivity analyses were conducted to quantify the impact of parameter changes on the R0 value. We changed the shape parameter of Gamma distribution from 7.0 to 8.0 days for estimating the R0 value of COVID-19 transmission and changed the same parameter from 8.0 to 9.0 for estimating the R0 value of SARS transmission.
R software (version 3.6.0) was used for data analyses, “R0” package was used for calculating R0 and “EpiEstim” package was used for estimating Rt. Two tailed P < 0.05 were considered statistically significant for all statistical tests.
Ethics statement
Data collection and analysis of cases was determined by the National Health Commission of the People’s Republic of China to be part of a continuing public health outbreak investigation and was thus considered exempt from institutional review board approval.
Results
Description of the outbreak
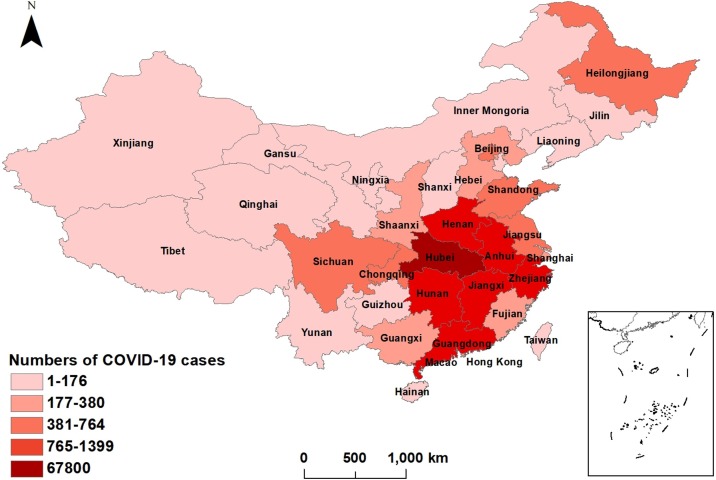
As of 20 March 2020, a total of 80,739 local acquired cases were identified across mainland China. Hubei Province reported the most cases (n = 67,800), with 50,005 (73.8%) cases reported in Wuhan, the capital city of Hubei. COVID-19 was responsible for 3139 deaths (4.6%, 3139/67,800) in Hubei Province by 20 March 2020. A total of 1353 cases were reported in Guangdong Province, including 1014 (75.1%) cases imported from other provinces and 339 (24.9%) secondary cases (Figure 1 ).
Figure 1.
Distribution of COVID-19 cases in China, as of March 20, 2020.
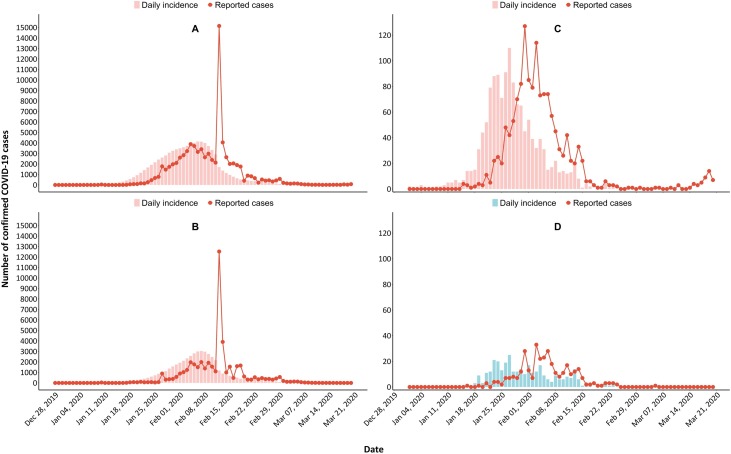
Figure 2 displays the epidemic trend of COVID-19 in China, Wuhan, and Guangdong Province. Most cases were reported between 20 January and 29 February 2020, with a peak between 3 and 9 February, and a spike on 12 February in China and Wuhan. The epidemic peak of reported cases in Guangdong Province was on 31 January, followed by a significant decrease. The delay period between the onset date and the reporting date was approximately 6 days. The epidemic curve of predicted daily incidence showed a similar trend to that of reported daily cases.
Figure 2.
Temporal distribution of confirmed COVID-19 cases in China, Wuhan, and Guangdong Province. Panel A: Temporal distribution of COVID-19 cases in China; Panel B: Temporal distribution of COVID-19 cases in Wuhan; Panel C: Temporal distribution of all confirmed COVID-19 cases in Guangdong Province; Panel D: Temporal distribution of secondary COVID-19 cases in Guangdong Province.
Estimation of doubling time and basic reproduction number (R0)
The estimated doubling time of COVID-19 in the initial outbreak period was 2.2, 2.4, and 3.1 days in China, Wuhan, and Guangdong Province, respectively (Table 1 ), while the doubling time of SARS in the period prior to the peak in Guangdong, Hong Kong, and Beijing was 14.3, 5.7 and 12.4 days, respectively (Table 1, Figure S2). The R0 value of COVID-19 was 5.0 (95%CI: 4.9−5.1) in China and 4.8 (95%CI: 4.6−5.0) in Wuhan. The effective reproduction number for secondary COVID-19 cases in Guangdong Province was 0.7 (95%CI: 0.6−0.9). The R0 value of SARS was 2.3 (95%CI: 2.0−2.7), 2.3 (95%CI: 2.0−2.5), and 2.6 (95%CI: 2.4−2.8) in Guangdong, Hong Kong, and Beijing, respectively (Table 1).
Table 1.
General characteristics of COVID-19 cases nationwide, in Wuhan and in Guangdong Province, up to March 20, 2020.
| COVID-19 | Nationwide | Wuhan | Guangdong |
|---|---|---|---|
| Total number of confirmed cases | 80,739 | 50,005 | 1353 |
| Doubling time (day) | 2.2 | 2.4 | 3.1 |
| R0 (95%CI) | 5.0 (4.9−5.1) | 4.8 (4.6−5.0) | 0.7a (0.6−0.9) |
| SARS | Beijing | Hong Kong | Guangdong |
|---|---|---|---|
| Total number of confirmed cases | 2521 | 1734 | 1511 |
| Doubling time (day) | 12.4 | 5.7 | 14.3 |
| R0 (95%CI) | 2.6 (2.4−2.8) | 2.3 (2.0−2.5) | 2.3 (2.0−2.7) |
The R0 value of COVID-19 was estimated in secondary cases in Guangdong Province and the R0 in Guangdong is also named as an effective reproduction number which represents the transmissibility based on the countermeasures implemented.
Estimation of time-varying reproduction number (Rt)
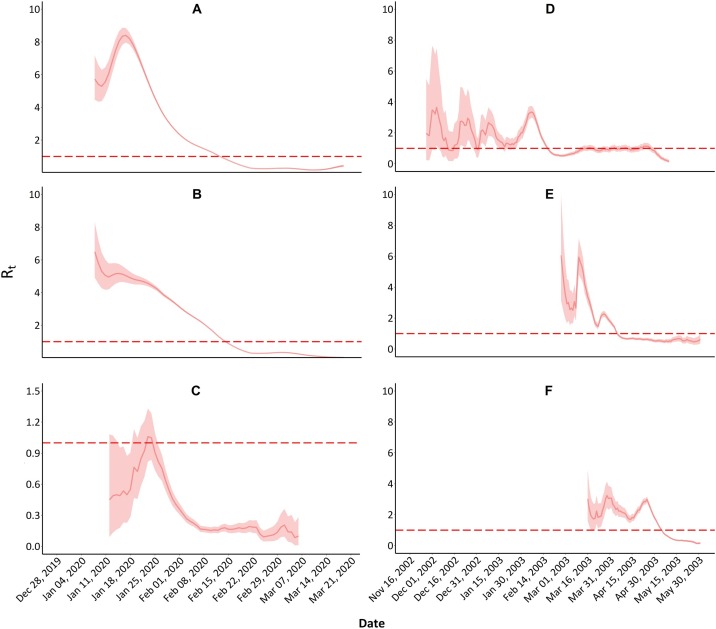
During the epidemic, the Rt value of COVID-19 in China increased from 8 January 2020 onwards, peaking at 8.4 (95%CI: 8.0–8.8) on 17 January. Subsequently the Rt value gradually decreased and fell below 1.0 on 14 February. The Rt value in Wuhan continuously declined from 6.5 (95%CI: 4.9–8.3) on 8 January to below 1.0 on 14 February. By contrast, the Rt value for secondary cases in Guangdong Province showed a rising trend from 12 January, peaking at 1.1 (95%CI: 0.8–1.3) on 23 January and then decreasing rapidly to 0.2 on 1 March (Figure 3 ).
Figure 3.
Time-varying reproduction number (Rt) of COVID-19 and SARS in China.
Panel A: Rt of COVID-19 nationwide; Panel B: Rt of COVID-19 in Wuhan; Panel C: Rt of secondary COVID-19 in Guangdong Province; Panel D: Rt of SARS in Guangdong Province; Panel E: Rt of SARS in Hong Kong; Panel F: Rt of SARS in Beijing.
With SARS, the Rt value in Guangdong Province fluctuated for about 6 months from November 2002 to May 2003, and the peak was 3.6 (95%CI: 1.2–7.5). The Rt value in Beijing and Hong Kong had a similar fluctuating trend for about three months (March to May 2003) with a peak Rt of 3.2 (95%CI: 2.5–4.1) and 6.1 (95%CI: 3.1–9.9), respectively.
Sensitivity analyses
In the sensitivity analyses, when we changed the GT in calculating the R0 value of COVID-19 (GT changed from 7.0 to 8.0 days) and SARS (GT changed from 8.0 to 9.0 days), we found that the R0 value of COVID-19 varied slightly from 4.5 to 5.7, but was still much higher than the R0 value of SARS (Figure S3).
Discussion
COVID-19 is a novel coronavirus infection disease, which is different from SARS and other SARS-like viruses (World Health Organization, 2020a) and the transmission characteristics of COVID-19 are not fully understood (Parry, 2020). In this study, we found that the R0 value of COVID-19 was 5.0 in China and 4.8 in Wuhan. Our estimates were larger than those reported by Li et al (R0 = 2.2) for Wuhan between 10 December 2019 and 4 January 2020, the very early stage of this epidemic (Tang et al., 2020). It has been suggested that the number of COVID-19 cases may have been seriously underreported in the early stage (Read et al., 2020, Tian et al., 2020), since SARS-CoV-2 was confirmed on 7 January 2020, and the official diagnostic protocol was not released by the WHO until 17 January 2020 (Zhao et al., 2020). In addition, surveillance was not widely conducted, and many infections may not have been documented. Read et al estimate that only 5.1% of infections in Wuhan were identified in the early period (Read et al., 2020). Zhao et al. estimate that the R0 value of COVID-19 was >5.0 using national reported data from 10 to 24 January 2020 (Zhao et al., 2020).
We observed a higher R0 value and much shorter doubling time of COVID-19 than SARS (Bauch et al., 2005, Fraser et al., 2004, Peak et al., 2017), indicating the higher transmissibility of COVID-19. These differences may be due to two reasons. First, epidemiological and clinical evidence suggests that asymptomatic or mild COVID-19 cases during their incubation periods could transmit COVID-19 (Chen et al., 2020b). This differs from SARS where most cases were infected by “super spreaders”; SARS cases in their incubation period and mild cases could not infect a susceptible population (Lipsitch et al., 2003). The average incubation period of COVID-19 was 4.8 days, ranging from 1 to 14 days, and the average period from onset of symptoms to isolation was 2.9 days (Liu et al., 2020), indicating a long transmission period. Second, the COVID-19 epidemic coincided with the approach of the Chinese Lunar New Year holiday, during which an estimated 3 billion trips were made, with 15 million trips in Wuhan alone (Wang et al., 2020). This dramatic increase in population mobility accelerated the spread of COVID-19. Although Wuhan prohibited all transport in and out of the city as of 10:00 on 23 January 2020, millions of citizens had left Wuhan before that time, and they may have become the major exporter of COVID-19 infection into other regions in China. Fortunately, the intervention of travel restrictions was effective in slowing the spread of COVID-19 into new locations (Tian et al., 2020).
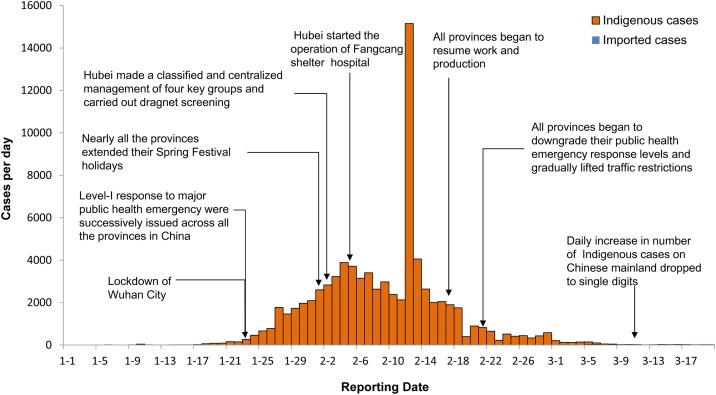
We observed a significant decrease in the time-varying Rt value of COVID-19 in China and Wuhan. More importantly, the daily reported cases began to decline after 12 February. These results indicate that the rigorous measures of prevention and control taken by Chinese governments were taking effect (Lai et al., 2020, Pan et al., 2020b, WHO-China Joint Mission, 2020). For example, following the Wuhan travel restriction, most provinces and cities also implemented travel restrictions and imposed quarantine on all outpatients with fever, close contacts of COVID-19 cases, and persons traveling from Hubei Province. The Chinese Lunar New Year holiday was extended and all gatherings and public activities were restricted to prevent the transmission of COVID-19. More importantly, almost all provinces and regions in China initiated the highest level of public health emergency response (Figure 4). Communication on COVID-19 was broadly conducted, which improved the public’s understanding of the risk of COVID-19 and their motivation to take voluntary actions to detect, diagnose and treat earlier. This can be verified by the decrease in the period between onset of symptoms and diagnosis during the epidemic in Guangdong Province.
Figure 4.
The epidemic curve, key events, and public health interventions in mainland China.
We also observed that the effective reproduction number was less than 1.0, and the Rt value of secondary COVID-19 cases in Guangdong continuously declined after 23 January 2020 when Guangdong Province initiated the Level-I emergency response (Health Commission of Guangdong Province, 2020), and conducted a range of public interventions including traffic restrictions, social distancing, home isolation and centralized quarantine, and improvement of medical resources. This demonstrates that prevention and control measures have significantly suppressed the local transmission of COVID-19; the reported COVID-19 cases were dominated by imported cases (Li et al., 2020, WHO-China Joint Mission, 2020).
When comparing the Rt value of COVID-19 with SARS, we found that the peak of COVID-19 was higher than SARS, which indicates higher transmissibility of COVID-19. However, for COVID-19 the period with an Rt value of >1.0 was 38 days in Wuhan, 37 days in China, and 2 days in Guangdong, compared with 82 days in Guangdong, 51 days in Beijing and 38 days in Hong Kong for SARS. In addition, the Rt curve of COVID-19 had one peak while the Rt curve of SARS had fluctuations with more than one peak, indicating epidemic rebound and ineffective prevention strategies. The timely control of the COVID-19 epidemic could be attributed to the improvement of the disease surveillance system since the SARS period, and substantial progress in the ability to diagnose and report infectious disease. In addition, the prevention strategy was more effective than during the SARS epidemic even though COVID-19 has higher transmissibility.
This study has several strengths. First, this is the first study to date to assess the time-varying transmission dynamics of COVID-19 based on national incidence data. We also estimate the instantaneous reproduction number for secondary cases in Guangdong Province. Second, we compare the transmission dynamics of COVID-19 with SARS. Third, we make an initial assessment of the effect of control measures taken by governments.
Our study has several limitations. First, the daily COVID-19 incidence in China and Wuhan, except for Guangdong Province, was estimated using a GAM, which may lead to misclassification bias. However, the cross-validation indicated good performance of the GAM. In addition, the effective reproduction number estimated for imported cases in Guangdong Province, as a sample of the total confirmed cases nationwide, was comparable with the R0 value estimated nationwide, indicating that our results are robust. Second, there were differences in the ability to diagnose and report infectious disease between the SARS and COVID-19 epidemics, which may cause inconsistency in data accuracy and introduce bias on the transmissibility estimation of the two diseases. Third, no data was available on the proportion of asymptomatic cases. Future studies are urgently needed to fill these knowledge gaps.
Conclusions
COVID-19 has higher transmissibility than SARS, however, COVID-19 control measures in China have achieved an initial effect (Lai et al., 2020, WHO-China Joint Mission, 2020). Rigorous COVID-19 control and prevention measures should be sustained in order to prevent a rebound of the epidemic in the context of the global pandemic.
Author contributions
All authors meet the criteria for authorship as recommended by the International Committee of Medical Journal Editors. WJM and JFH designed the study. LFL, HJZ, QH, APD, XHT, JSL, YL, LMS, WJL, and TS participated in the field investigation. JPX, JXH, GHH, TL, ZHR, WLZ, SQZ, ZHZ, DXG, DHW, SWC, YHL, and LCG analyzed and interpreted the data. JPX, JXH, GHH, TL, and MK wrote and edited the paper. JFH, WJM, MK, LFL, HJZ, QH, APD, XHT, JSL, YL, LMS, WJL, and TS reviewed, revised, and edited the manuscript.
Support
This study was supported by [the National Key Research and Development Program of China #1] under Grant [number 2018YFB0505500, 2018YFB0505503, 2018YFA0606202]; [Key-Area Research and Development Program of Guangdong Province #2] under Grant [number 2019B111103001]; [the Science and Technology Program of Guangdong Province #3] under Grant [number 2018B020207006, 2019B020208005]; [Guangzhou Science and Technology Plan Project #4] under Grant [number 201804010383]; [Chinese Postdoctoral Science Foundation #5] under Grant [number 2020T130020ZX]; and [Foshan Key Technology Project for COVID-19 #6] under Grant [number 2020001000376].
Conflict of interest
None declared.
Acknowledgments
We thank all the members from the health department and CDC in Guangdong Province for their contribution to data collection, and to COVID-19 control and prevention.
Footnotes
Supplementary material related to this article can be found, in the online version, at doi:https://doi.org/10.1016/j.ijid.2020.11.005.
Appendix A. Supplementary data
The following is Supplementary data to this article:
References
- Bauch C.T., Lloyd-Smith J.O., Coffee M.P., Galvani A.P. Dynamically modeling SARS and other newly emerging respiratory illnesses: past, present, and future. Epidemiology. 2005;16(6):791–801. doi: 10.1097/01.ede.0000181633.80269.4c. [DOI] [PubMed] [Google Scholar]
- Chen T., Wu D., Chen H., Yan W., Yang D., Chen G., et al. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study. BMJ. 2020;368:m1091. doi: 10.1136/bmj.m1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Y., Aihong W., Bo Y., Keqin D., Haibo W., Jianmei W., et al. The epidemiological characteristics of infection in close contacts of COVID-19 in Ningbo city. Chin J Epidemiol. 2020;41(5):668–672. [Google Scholar]
- Epidemiology Working Group for NCIP Epidemic Response CcfDCaP., Prevention CcfDCa., Yanping Z. The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) in China. Chin J Epidemiol. 2020;41(2):145–151. [Google Scholar]
- Fraser C., Riley S., Anderson R.M., Ferguson N.M. Factors that make an infectious disease outbreak controllable. Proc Natl Acad Sci U S A. 2004;101(16):6146–6151. doi: 10.1073/pnas.0307506101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galvani P.A., Lei X., Jewell P.N. Severe acute respiratory syndrome: temporal stability and geographic variation in case-fatality rates and doubling times. Emerging Infect Dis. 2003;9(8):991–994. doi: 10.3201/eid0908.030334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Health Commission of Guangdong Province . 2020. Guangdong Province Decides to Initiate Level-I Respond to Public Health Emergency.http://wsjkw.gd.gov.cn/gkmlpt/content/2/2878/post_2878900.html#2569 Available from: [Google Scholar]
- Hui D.S.C., Chan M.C.H., Wu A.K., Ng P.C. Severe acute respiratory syndrome (SARS): epidemiology and clinical features. Postgrad Med J. 2004;80(945):373–381. doi: 10.1136/pgmj.2004.020263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inglesby T.V. Public health measures and the reproduction number of SARS-CoV-2. JAMA. 2020;323(21):2186–2187. doi: 10.1001/jama.2020.7878. [DOI] [PubMed] [Google Scholar]
- Lai S., Ruktanonchai N.W., Zhou L., Prosper O., Luo W., Floyd J.R., et al. Effect of non-pharmaceutical interventions to contain COVID-19 in China. Nature. 2020 doi: 10.1038/s41586-020-2293-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Z., Chen Q., Feng L., Rodewald L., Xia Y., Yu H., et al. Active case finding with case management: the key to tackling the COVID-19 pandemic. Lancet. 2020;396(10243):63–70. doi: 10.1016/S0140-6736(20)31278-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipsitch M., Cohen T., Cooper B., Robins J.M., Ma S., James L., et al. Transmission dynamics and control of severe acute respiratory syndrome. Science. 2003;300(5627):1966–1970. doi: 10.1126/science.1086616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu T., Hu J., Kang M., Lin L., Zhong H., Xiao J., et al. Transmission dynamics of 2019 novel coronavirus (2019-nCoV) bioRxiv. 2020 [Google Scholar]
- Nation Health Commission of the People’s Republic of China . 2020. Epidemic Situation of Novel Coronavirus Infection.http://www.nhc.gov.cn/xcs/yqtb/list_gzbd.shtml Available from: [Google Scholar]
- National Health Commission of the People’s Republic of China . 2020. Prevention and Control Scheme of Novel Coronavirus.http://www.nhc.gov.cn/xcs/zhengcwj/202002/a5d6f7b8c48c451c87dba14889b30147.shtml Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pan A., Liu L., Wang C., Guo H., Hao X., Wang Q., et al. Association of public health interventions with the epidemiology of the COVID-19 outbreak in Wuhan, China. JAMA. 2020;323(19):1–9. doi: 10.1001/jama.2020.6130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pang X., Zhu Z., Xu F., Guo J., Gong X., Liu D., et al. Evaluation of control measures implemented in the severe acute respiratory syndrome outbreak in Beijing, 2003. JAMA. 2003;290(24):3215–3221. doi: 10.1001/jama.290.24.3215. [DOI] [PubMed] [Google Scholar]
- Parry J. China coronavirus: cases surge as official admits human to human transmission. BMJ. 2020:368. doi: 10.1136/bmj.m236. [DOI] [PubMed] [Google Scholar]
- Peak C.M., Childs L.M., Grad Y.H., Buckee C.O. Comparing nonpharmaceutical interventions for containing emerging epidemics. Proc Natl Acad Sci U S A. 2017;114(15):4023–4028. doi: 10.1073/pnas.1616438114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Read J.M., Bridgen J.R., Cummings D.A., Ho A., Jewell C.P. Novel coronavirus 2019-nCoV: early estimation of epidemiological parameters and epidemic predictions. medRxiv. 2020 doi: 10.1098/rstb.2020.0265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang B., Wang X., Li Q., Bragazzi N.L., Tang S., Xiao Y., et al. Estimation of the transmission risk of the 2019-nCov and its implication for public health interventions. J Clin Med. 2020;9(2) doi: 10.3390/jcm9020462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson R., Stockwin J., van Gaalen R., Polonsky J., Kamvar Z., Demarsh P., et al. Improved inference of time-varying reproduction numbers during infectious disease outbreaks. Epidemics. 2019;29:100356. doi: 10.1016/j.epidem.2019.100356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tian H., Liu Y., Li Y., Wu C.H., Chen B., Kraemer M.U.G., et al. An investigation of transmission control measures during the first 50 days of the COVID-19 epidemic in China. Science. 2020 doi: 10.1126/science.abb6105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Chen, Horby Peter W, Hayden Frederick G, Gao George F. A novel coronavirus outbreak of global health concern. Lancet. 2020;395:470–473. doi: 10.1016/S0140-6736(20)30185-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO-China Joint Mission . 2020. Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19) [Google Scholar]
- World Health Organization . 2003. Summary of Probable SARS Cases with Onset of Illness from 1 November 2002 to 31 July 2003.https://www.who.int/csr/sars/country/table2004_04_21/en/ Available from: [Google Scholar]
- World Health Organization . 2003. Epidemic Curves-Severe Acute Respiratory Syndrome (SARS)https://www.who.int/csr/sars/epicurve/epiindex/en/ Available from: [Google Scholar]
- World Health Organization . 2020. Coronavirus Disease (COVID-19) Pandemic.https://www.who.int/emergencies/diseases/novel-coronavirus-2019 Available from: [Google Scholar]
- Zhao S., Lin Q., Ran J., Musa S.S., Yang G., Wang W., et al. Preliminary estimation of the basic reproduction number of novel coronavirus (2019-nCoV) in China, from 2019 to 2020: a data-driven analysis in the early phase of the outbreak. Int J Infect Dis. 2020 doi: 10.1016/j.ijid.2020.01.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.