Abstract
Background and aim
The outbreak of the emerging coronavirus disease 2019 (COVID-19) is a global public health emergency. According to the findings, women with gestational diabetes mellitus (GDM) are at increased risk of this virus. Due to the need for quarantine and social distancing in the current disease situation and need to receive repeated medical care in GDM patients, this review study aimed to evaluate the self-care strategies for women with GDM during COVID-19 pandemic.
Methods
25 related articles from 2011 to 2020 and 3 guidelines were reviewed with the keywords of gestational diabetes mellitus, diabetes, pregnancy and COVID-19 in combination with self-care and self-management in PubMed, Google Scholar, Scopus, Science Direct, Elsevier, Springer, Wiley Online Library and SID.
Results
According to the results of the studies, face-to-face visits should be limited and instead, telemedicine services recommended. Self-care throughout telemedicine services were improved maternal and neonatal outcomes in women with GDM.
Conclusion
Although self-care program through telemedicine services is beneficial for women with GDM, performing clinical trials are recommended to assess maternal and neonatal outcomes in this condition.
Keywords: Gestational diabetes mellitus, COVID-19, Self-care, Self-management, Telemedicine, Telehealth
Highlights
-
•
Clinical services for pregnant women are based on social distance, proper personal protection and telemedicine.
-
•
Telemedicine reduces face-to-face consultations in GDM women during COVID-19 pandemic.
-
•
Self-care programs have shown improved maternal and neonatal outcomes in women with GDM.
-
•
Performing comprehensive clinical trials with an enough sample size is recommended.
1. Introduction
In late December 2019, a new coronavirus known as coronavirus disease 2019 (COVID-19) has emerged in Wuhan, China [1]. The World Health Organization (WHO) declared its outbreak as a public health emergency [2]. Since August 2, 2020, 213 countries have been affected by this virus with a total number of 18,141,109 infected cases and 690,890 deaths worldwide [3]. The infectious disease is spread through infected respiratory droplets, and clinical signs include fever, cough, and shortness of breath, which can lead to pneumonia, respiratory distress syndrome, and multi-organ failure [2]. The most vulnerable populations to this virus are those with chronic illness [4]. In addition, pregnant women are at increased risk of viral infections due to physiological changes in the respiratory, endocrine, immune and cardiovascular systems [5]. Pregnancy complications such as diabetes, heart failure and hypertension have known as a double risk factor of COVID-19 for pregnant women [6]. One of the most common complications of pregnancy is gestational diabetes mellitus (GDM), which is defined as a glucose intolerance that its onset or first diagnosed is during pregnancy [7]. Depending on population characteristics, screening methods, and diagnostic criteria, GDM affects 1–28% of pregnancies worldwide [8]. The prevalence of GDM in many developed and developing countries is increasing rapidly [9]. GDM-complicated pregnancies are associated with adverse maternal [reduced quality of life, increased risk of cesarean section, pregnancy induced hypertension (PIH), preeclampsia and type 2 diabetes] and neonatal outcomes [increased risk of macrosomia, large for gestational age (LGA), neonatal hypoglycemia, and adulthood type 2 diabetes mellitus] [8]. Daily blood glucose monitoring, repeated injections, regular clinical visits, and a healthy lifestyle program help to control the disease and its complications [10]. When people are being asked to keep the social distance and quarantine to minimize exposure to the virus, many people who need ongoing health care are avoiding receive cares due to the fear of infection [11]. On the other hand, the quarantine in diabetic patients cause to reduced physical activity, changes in diet and reduced access to anti-hyperglycemic drugs or insulin which leads to uncontrolled glycaemia [12]. In this situation the most important action for these patients is self-care [10]. Self-care is a set of self-stimulation activities in which someone looks after his or her own health and wellbeing independently [13].
Studies on self-care and diabetes [14] and self-care and GDM [13,15,16] have pointed to the effectiveness of self-care education using lectures and group discussions. However, the current situation challenges patients to receive face to face self-care training. Scott and colleagues in a study also expressed the challenges of self-care and diabetes in COVID-19 pandemic [11], but self-care information about GDM women during COVID-19 pandemic is limited. Due to the limited information in this field, the need for quarantine and social distancing especially for high-risk individuals in the current situation and the need to receive repeated medical care in GDM patients, this review study aimed to evaluate the self-care strategies for women with GDM during COVID-19 pandemic.
2. Evidence acquisition
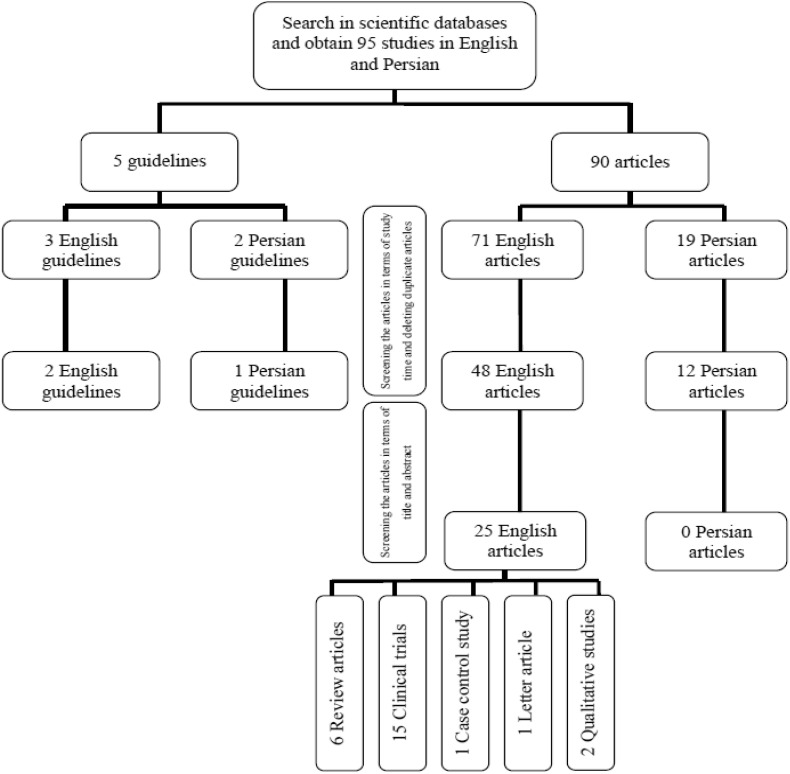
The present study aimed to review the literatures related to self-care strategies for women with GDM, which can be useful during the COVID-19 pandemic. In the initial search with the keywords of COVID-19, gestational diabetes mellitus, diabetes and pregnancy in combination with self-care and self-management in PubMed, Science Direct, Elsevier, Springer, Wiley Online Library, Scopus and Persian equivalent of these words in Google Scholar and SID, a total of 90 English and Persian articles and 5 guidelines were obtained. Of these, 71 articles and 3 guidelines were in English and 19 articles and 2 guidelines were in Persian. Access to full text articles, online access to articles from 2011 to 2020, and the language of articles (in English or Persian) were inclusion criteria in this article. So older and repetitive articles were removed, and studies from 2011 to April 2020 were reviewed. After reviewing the title and abstract of study, eventually 25 related English articles (including 6 review articles, 15 clinical trials, 1 case control study, 1 letter and 2 qualitative studies) and 3 guidelines (related to Canada, UK and Iran) were included in the study, as shown in Fig. 1 .
Fig. 1.
Flow diagram of the literature review process.
3. COVID-19 and GDM
Due to the more clinical complications of COVID-19 in pregnant women (increased preterm birth, preeclampsia, cesarean section and perinatal death) [17], clinical services for these individuals are based on social distance, proper use of personal protective equipment and telemedicine [18]. Tests of first visit in pregnant women with pre-existing diabetes should be included glycated hemoglobin (HbA1c), evaluating renal and thyroid function, and urine for protein: creatinine ratio. Face-to-face visits should be minimized and if necessary, planned with necessary tests and ultrasound appointments at 11–14 weeks, 28 and 32 weeks and 34–36 weeks’ gestation [19]. Gathering pregnant women in health centers should be avoided. A specific time must be set for the necessary visits and was noticed them via call or short message service (SMS) [20]. Visits time should be short and pregnant women should be alone if it is possible [21]. Due to prolonged waiting period in medical centers and limited resources, the 2-h oral glucose tolerance test (OGTT) is not recommended in GDM patients, instead, screening with HbA1c and random plasma glucose tests is recommended. In addition, postpartum screening can be delayed for 3–6 months after delivery instead of the previous 3 months [19,22]. But this postponement should not exceed one year [23]. Whenever possible and with clinical diagnosis, use the telemedicine technologies (video or phone call) for medical consultation and initial or follow-up visits, and share key clinical data (weight and blood pressure, etc.) obtained in face-to-face visits with interdisciplinary diabetes and pregnancy teams.
Dietary and insulin injections can also be trained using virtual courses in form of video calls [22]. The physician should routinely monitor the mental health status of diabetic patients and assist them in the preparation of medications through introducing online pharmacies [24].
4. Self-care and GDM
According to the results of studies conducted in pregnant women with GDM, awareness and ability (knowing the disease and mother’s empowerment), lifestyle (nutritional and physical activity training), mental health (counseling and interaction), and family support were self-care educational needs in Iranian culture [25]. Self-care program increased the awareness [16] improved the knowledge, attitude [16,26] self-care behaviors [16,[26], [27], [28]] and self-efficacy [27,28] and reduced perceived stress in women with GDM [15]. It also was affective in decreased the number of macrosomia, cesarean section [13,16], Preterm birth [16,27,29], polyhydramnios, pyelonephritis, placenta previa, vaginal infection, preeclampsia, abortion, obstructed labor, postpartum hemorrhage [16] and hospital admissions [10]. In addition, fetal complications immediately after labor such as ICU admission, and hypoglycemia were decreased [16] and reduced the costs [30]. This also improved quality of life [10,31,32], mean level of blood glucose at the time points of 1 h after GTT and 2 h after GTT [30], blood glucose 2 h postprandial [27,[33], [34], [35]], fast blood sugar (FBS) [27,33,34], and HbA1c [27,33,36].
While different studies expressed positive effects of self-care program in women with gestational diabetes, the results of some studies didn’t find it effective in terms of preterm labor [13], infection rate during labor, prematurity and respiratory distress, jaundice, internal uterine fetal death (IUFD) [16], birth weight, height and head circumference of their infants [13]. Also drug regimen compliance [16], quality of life [30], FBS [27,30,36] and HbA1c [27,35] did not change.
5. Telemedicine and GDM
Also, the results of studies on self-care using telemedicine and GDM stated that telemedicine services compared to routine care were associated with reduced preterm birth [37,38], premature rupture of membranes, neonatal asphyxia, polyhydramnios [37], and emergency cesarean section [38]. However, there were no differences in terms of quality of life [39], mean gestational age at birth [40], mean birth weight, and hospitalized in neonatal intensive care unit (NICU), LGA [38,40], hyperbilirubinemia and shoulder dystocia [38] in telemedicine compared to routine care. There was disagreement over the effectiveness of telemedicine compared to routine care in some parameters.
While telemedicine has been shown to improve the cesarean section [37,38], macrosomia, neonatal hypoglycemia, pregnancy complications, 2-h blood sugar, and fasting blood sugar [37], some studies have shown no difference of these parameters compared to routine care [[38], [39], [40], [41], [42]]. Also, the results of some studies have found the use of telemedicine to be beneficial in improving HbA1c [37,40,41] and mean blood sugar [42,43], however, the results of a study did not differ in HbA1c [39] and mean Blood sugar [38] compared to routine care. The results of two clinical trials indicate more satisfaction of GDM women in telemedicine technologies compared to routine care [38,44] and no difference in direct care costs in the two groups was reported [38].
In addition, telemedicine is effective in follow-up and monitoring patients after discharge, visiting susceptible patients, caring for patients with chronic illness, protecting medical personnel, and collecting information from the quarantine and the isolation period during COVID-19 pandemic [4].
6. Discussion
The aim of this study was to evaluate the self-care for women with GDM in COVID-19 pandemic. In general, the results of this study was showed its beneficial to train self-care activities through telemedicine services in GDM women during COVID-19 pandemic, however, it should be noted that in situations such as the first consultation for new diabetic cases and major changes in the prescription (including changing medications or adjusting the dose of multiple medications), face to face consultation is preferred [12].
Emamgholi Khooshehchin and colleagues in a qualitative study considered self-care facilitators to accept disease (desire to get information, hope, and adaptability) and others support (social support, appropriate notices, and family support and encouragement) [7].
The results of the meta-analysis performed by Ming and colleagues showed a relatively small but significant improvement in HbA1c status in telemedicine self-care [40]. In a systematic review, Ahmadi and colleagues also noted the use of telemedicine in follow-up and treatment, reducing the level of patients’ family anxiety, improving dietary adherence and glycemia in diabetic patients [45]. In this regard, So and Chung in a systematic review stated that telemedicine affects the self-management of diabetes control in primary care [46].
Due to the COVID-19 pandemic and forcing people to take home quarantine, disruption of the daily routine, increased sensitivity and obsessive cleaning disorder, organ closure, increased sensitivity and exhausting conditions in certain occupations to control and treat the disease, rumors of disease and the weakening of social capital, the prevalence of psychological problems in society has expanded [47]. Shojaei and Masoumi in a study advised to pay attention to the provision of the psychological services using various devices, including social media, telephone and online services [48]. In addition, Khadivzadeh and colleagues suggested self-care training as an effective method to reduce stress in GDM women [15].
Although the results of this study in some cases have been shown the effectiveness of telemedicine versus routine care in GDM patients, and in some cases lack of differences in the results were observed, there is no evidence of a negative effect on blood sugar control, maternal and neonatal outcomes, and pregnancy complications, which can be enough to encourage the use of telemedicine technologies to care of GDM patients in current situation. However, studies conducted in this field, such as studies examining the satisfaction of health care personnel and comparing the duration of the visit, are limited and only one study reported that telemedicine visits were 8 min less than standard care [49].
On the other hand, the barriers to self-care education in these patients as helplessness (difficulty of controlling diabetes, feelings of disability, ineffective effort, and unawareness) and perceived problems (neglect of physicians and personnels, others’ curiosity and blame, and stressful medical expenses) should not be ignored [7]. Banerjee and colleagues also looked at attitudes, communication, cultural, socioeconomic, and legal barriers to diabetes self-management education [24]. In addition, Ahmadi and colleagues have cited poor privacy practices, high costs and lack of the proper insurance system, clear guidelines and codified laws as telemedicine challenges. Today, technology in medical field plays an important role [45]. Up to now, the greatest potential of telemedicine has been its ability to help patients who could not be easily treated in existing clinics due to geographical limitation [37]. But in the modern world, information technology makes it possible for people to participate in their health as self-care, which means that cyberspace can serve the health system. Due to the possibility of using telemedicine technologies around the world, it seems necessary to strengthen the infrastructures, allocate sufficient funds and train people in this field [45].
The lack of clinical trial studies on self-care strategies in pregnant women, and especially women with pregnancy complications due to the new COVID-19 pandemic, as well as the lack of studies on self-care and GDM in epidemics were the limitations of this study.
7. Conclusions
Although the results of this review article suggest that self-care using telemedicine technology is effective in controlling the complications of GDM, comprehensive clinical trials with an enough sample size is recommended, especially in the current situation which most people in the community and the health care providers are imposed on using telemedicine, it is more possible to evaluate the cost-effectiveness, satisfaction of health care providers and pregnant women at different levels of society. Also, the needs assessment of pregnant women with GDM, aimed to reduce the short-term and long-term complications of the disease, as well as planning and policy reform at the macro level is recommended.
Authors’ contribution
Behnaz Enjezab designed the study. All of the authors conducted the search and gathered the data. Fatemeh Moradi wrote the initial draft of the manuscript and Behnaz Enjezab and Akram Ghadiri-Anari revised it.
Conflict of interests
The authors declare that there is no conflict of interest to be declared.
Funding/support
There was no funding for this study.
Acknowledgments
We thank to all authors whom articles were used in this manuscript.
References
- 1.Singhal T. A review of coronavirus disease-2019 (COVID-19) Indian J Pediatr. 2020;87(4):281–286. doi: 10.1007/s12098-020-03263-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mardani M., Pourkaveh B. A controversial debate: vertical transmission of COVID-19 in pregnancy. Arch Clin Infect Dis. 2020 February;15(1) e102286. [Google Scholar]
- 3.https://www.worldometers.info/coronavirus/
- 4.Aslani N, Garavand A. The role of telemedicine to control CoVID-19. Arch Clin Infect Dis Online ahead of Print; 15(COVID-19): e102949.
- 5.Zhao X., Jiang Y., Zhao Y., Xi H., Liu C., Qu F. Analysis of the susceptibility to COVID-19 in pregnancy and recommendations on potential drug screening. Eur J Clin Microbiol Infect Dis. 2020 Apr 23:1–12. doi: 10.1007/s10096-020-03897-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mimouni F., Lakshminrusimha S., Pearlman S.A., Raju T., Gallagher P.G., Mendlovic J. Perinatal aspects on the covid-19 pandemic: a practical resource for perinatal-neonatal specialists. J Perinatol. 2020;40:820–826. doi: 10.1038/s41372-020-0665-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Emamgholi Khooshehchin T., Keshavarz Z., Afrakhteh M., Shakibazadeh A., Faghihzadeh S. Explanation the experiences of mothers with gestational diabetes about the factors affecting self-care: a qualitative study. Journal of Clinical Nursing and Midwifery. 2017;5(4):76–89. [Google Scholar]
- 8.Nguyen C.L., Pham N.M., Binns C.W., Duong D.V., Lee A.H. Prevalence of gestational diabetes mellitus in Eastern and South eastern Asia: a systemic review and meta-analysis. J Diabetes Res. 2018;2018(3):1–10. doi: 10.1155/2018/6536974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Khan T., Macaulay S., Norris S.A., Micklesfield L.K., Watson E.D. Physical activity and the risk for gestational diabetes mellitus amongst pregnant women living in Soweto: a study protocol. BMC Wom Health. 2016;16(1):66. doi: 10.1186/s12905-016-0345-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sheikhi H.R., Saadatifar B., Dashtban R., Anvari N., Mastaelizadeh H. Self-care in patients with gestational diabetes: review article. J Biochem Technol. 2018;9(2):177–180. [Google Scholar]
- 11.Scott E., Jenkins A., Fulcher G.R. Challenges of diabetes management during the COVID-19 pandemic. Med J Aust. 2020;213(2):56–57. doi: 10.5694/mja2.50665. [DOI] [PubMed] [Google Scholar]
- 12.Ghosh A., Gupta R., Misra A. Telemedicine for diabetes care in India during COVID19 pandemic and national lockdown period: guidelines for physicians. Diabetes Metab Syndr Clin Res Rev. 2020;14:273–276. doi: 10.1016/j.dsx.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mirghafourvand M., Zandinava H., Sehhatti Shafaei F., Mohammad-Alizadeh-Charandabi S., Ghanbari-Homayi S. Effectiveness of self-care training on pregnancy consequences in gestational diabetes: a randomized controlled clinical trial. Shiraz E-Med J. 2019;20(6) e82704. [Google Scholar]
- 14.Shrivastava S.R., Shrivastava P.S., Ramasamy J. Role of self-care in management of diabetes mellitus. J Diabetes Metab Disord. 2013 Mar 5;12(1):14. doi: 10.1186/2251-6581-12-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Khadivzadeh T., Hoseinzadeh M., Azhari S., Esmaily H., Akhlaghi F., Sardar M.A. Effects of self-care education on perceived stress in women with gestational diabetes under insulin treatment. Evidence Based Care Journal. 2015;5(16):7–18. [Google Scholar]
- 16.Sayed Ibrahim R El, Mousa Saber N. Impact of self-care program for gestational diabetic women on pregnancy outcomes. American Journal of Nursing Research. 2019;8(1):122–131. [Google Scholar]
- 17.Di Mascio D., Khalil A., Saccone G., Rizzo G., Buca D., Liberati M. Outcome of Coronavirus spectrum infections (SARS, MERS, COVID -19) during pregnancy: a systematic review and meta-analysis. Am J Obstet Gynecol MFM. 2020;2(2):100107. doi: 10.1016/j.ajogmf.2020.100107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dashraath P., Wong J.L.J., Lim M.X.K., Lim L.M., Li S., Biswas A. Coronavirus disease 2019 (COVID-19) pandemic and pregnancy. Am J Obstet Gynecol. 2020;222(6):521–531. doi: 10.1016/j.ajog.2020.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Royal College of Obstetricians & Gynaecologist Guidance for maternal medicine in the evolving coronavirus (COVID-19) pandemic [Internet] London 2020 [cited 2020 June 12] https://www.rcog.org.uk/globalassets/documents/guidelines/2020-03-30-guidance-for-maternal-medicine-in-the-evolving-coronavirus-covid-19-pandemic.pdf
- 20.Guidelines for pregnant women care of coronavirus disease [Internet] 2020 [cited 2020 June 12] http://www.ghazvinmc.ir/admin/News/file/537.pdf
- 21.Guidelines for pregnant women, breastfeeding and, infants care of coronavirus disease [Internet] 2020 [cited 2020 June 12] https://www1.nyc.gov/assets/doh/downloads/pdf/imm/covid-19-guidance-for-pregnant-people-fa
- 22.Yamamoto J.M., Donovan L.E., Feig D.S., Berger H. Urgent update: temporary alternative screening strategy for gestational diabetes screening during the COVID-19 pandemic [Internet] Society of Obstetricians and Gynaecologists of Canada 2020 [cited 2020 June 12] https://www.waterloowellingtondiabetes.ca/userContent/documents/Newsflash/Canadian%20Alternative%20GDM%20Guidelines%20COVID-19.pdf
- 23.bernabeu Instituto. Diabetes & pregnancy during the COVID-19 pandemic [Internet] 2020 [cited 2020 June 12] https://www.institutobernabeu.com/foro/en/coronavirus-covid-19-and-gestational-diabetes
- 24.Banerjee M., Chakraborty S., Pal R. Diabetes self-management amid COVID-19 pandemic. Diabetes & metabolic syndrome. Clin Res Rev. 2020;14(4):351–354. doi: 10.1016/j.dsx.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kolivand M., Keramat A., Rahimi M.A., Motaghi Z., Shariati M., Emamian M.H. Self-care education needs in gestational diabetes tailored to the iranian culture: a qualitative content analysis. Iran J Nurs Midwifery Res. 2018 May-Jun;23(3):222–229. doi: 10.4103/ijnmr.IJNMR_108_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Saboula N.E., Ahmed N.A., Rashad R.H. Effect of nursing intervention on knowledge, attitude and self -care activities among gestational diabetic women. International Journal of Novel Research in Healthcare and Nursing. 2018 May – August;5(2):135–146. http://www.noveltyjournals.com/download.php?file=Effect%20of%20Nursing%20Intervention%20on%20knowledge-1396.pdf&act=book [Google Scholar]
- 27.Kolivand M., Rahimi M.A., Shariati M., Keramat A., Emamian M.H. The effect of self-care educational/training interventions on the outcomes of gestational diabetes: a review article. Iran J Public Health. 2018 Dec;47(12):1805–1815. [PMC free article] [PubMed] [Google Scholar]
- 28.Viswanath L., Jose A. Self-care agency of women with gestational diabetes mellitus - effectiveness of a self-care enhancing intervention. Int J Network Commun. 2014;2(1):26–31. [Google Scholar]
- 29.Amason J.S. The effect of an educational intervention in women with gestational diabetes: a pilot study. Dissertation, Georgia State Univ. 2013;1:23–48. [Google Scholar]
- 30.Zandinava H., Sehhatti Shafaei F., Mohammad-Alizadeh Charandabi S., Ghanbari Homayi S., Mirghafourvand M. Effect of educational package on self-care behavior, quality of life, and blood glucose levels in pregnant women with gestational diabetes: a randomized controlled trial. Iran Red Crescent Med J. 2017 April;19(4) e44317. [Google Scholar]
- 31.Petkova V., Dimitrov M., Geourgiev S. Pilot project for education of gestational diabetes mellitus (GDM) patients - can it be beneficial? African J Pharma Pharmacol. 2011;5(10):1282–1286. [Google Scholar]
- 32.Mirfeizi M., Mehdizadeh Tourzani Z., Asghari Jafarabadi M., Moghimi Hanjani S., Hasanzad M. Health education in gestational diabetes mellitus and quality of life. Journal of Midwifery and Reproductive Health. 2017;5(4) 10661074. [Google Scholar]
- 33.Youngwanichsetha S., Phumdoung S., Ingkathawornwong T.H. The effects of mindfulness eating and yoga exercise on Blood sugar levels of pregnant women with gestational diabetes mellitus. Appl Nurs Res. 2014;27(4):227–230. doi: 10.1016/j.apnr.2014.02.002. [DOI] [PubMed] [Google Scholar]
- 34.Abirami P., Judie A. Reduction of risk on newly detected gestational diabetes mellitus by multi model intervention- A hospital based study. Int J Pharmaceut Chem Res. 2014;6(4):370–374. [Google Scholar]
- 35.Yang X., Tian H., Zhang F., Zhang C., Li Y., Leng J. A randomized translational trial of lifestyle intervention using a 3-tier shared care approach on pregnancy outcomes in Chinese women with gestational diabetes mellitus but without diabetes. J Transl Med. 2014;12:290. doi: 10.1186/s12967-014-0290-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bo S., Rosato R., Ciccone G., Canil S., Gambino R., Poala C.B. Simple lifestyle recommendations and the outcomes of gestational diabetes. A 2×2 factorial randomized trial. Diabetes Obes Metabol. 2014;16(10):1032–1035. doi: 10.1111/dom.12289. [DOI] [PubMed] [Google Scholar]
- 37.Xie W., Dai P., Qin Y., Wu M., Yang B., Yu X. Effectiveness of telemedicine for pregnant women with gestational diabetes mellitus: an updated meta-analysis of 32 randomized controlled trials with trial sequential analysis. BMC Pregnancy Childbirth. 2020;(198):20. doi: 10.1186/s12884-020-02892-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mackillop L., Hirst J.E., Bartlett K.J., Birks J.S., Clifton L., Farmer A.J. Comparing the efficacy of a Mobile phone-based blood glucose management system with standard Clinic Care in Women with Gestational Diabetes: randomized controlled trial. JMIR Mhealth Uhealth. 2018;6(3):e71. doi: 10.2196/mhealth.9512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rasekaba T.M., Furler J., Blackberry I., Tacey M., Gray K., Lim K. Telemedicine interventions for gestational diabetes mellitus: a systematic review and meta-analysis. Diabetes Res Clin Pract. 2015;110(1):1–9. doi: 10.1016/j.diabres.2015.07.007. [DOI] [PubMed] [Google Scholar]
- 40.Ming W.K., Mackillop L.H., Farmer A.J., Loerup L., Bartlett K., Levy J.C. Telemedicine technologies for diabetes in pregnancy: a systematic review and meta-analysis. J Med Internet Res. 2016;18(11) doi: 10.2196/jmir.6556. e290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Guo H., Zhang Y., Li P., Zhou P., Chen L.M., Li S.Y. Evaluating the effects of mobile health intervention on weight management, glycaemic control and pregnancy outcomes in patients with gestational diabetes mellitus. J Endocrinol Invest. 2019;42(6):709–714. doi: 10.1007/s40618-018-0975-0. [DOI] [PubMed] [Google Scholar]
- 42.Miremberg H., Ben-Ari T., Betzer T., Raphaeli H., Gasnier R., Barda G. The impact of a daily smartphone-based feedback system among women with gestational diabetes on compliance, glycaemic control, satisfaction, and pregnancy outcome: a randomized controlled trial. Am J Obstet Gynecol. 2018;218(4):453. doi: 10.1016/j.ajog.2018.01.044. e1–7. [DOI] [PubMed] [Google Scholar]
- 43.Kim Y.S., Kim H.S., Kim Y.L. Effects of a web-based self-management program on the behavior and blood glucose levels of women with gestational diabetes mellitus. Telemed J e Health: The Official Journal of the American Telemedicine Association. 2019;25(5):407–414. doi: 10.1089/tmj.2017.0332. [DOI] [PubMed] [Google Scholar]
- 44.Hirst J.E., Mackillop L., Loerup L., Kevat D.A., Bartlett K., Gibson O. Acceptability and user satisfaction of a smartphone-based, interactive blood glucose management system in women with gestational diabetes mellitus. J Diabetes Sci Technol. 2015 Jan;9(1):111–115. doi: 10.1177/1932296814556506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ahmadi M., Meraji M., Mashoof jafarabad E. Evidence on telemedicine in Iran - systematic review. Journal of Paramedical Sciences & Rehabilitation. 2018;7(1):112–124. [Google Scholar]
- 46.So C.F., Chung J.W. Telehealth for diabetes self-management in primary healthcare–a systematic review and meta-analysis. J Telemed Telecare. 2018 Jun;24(5):356–364. doi: 10.1177/1357633X17700552. [DOI] [PubMed] [Google Scholar]
- 47.Javadi S.M.H., Arian M., Qorbani-Vanajemi M. The need for psychosocial interventions to manage the coronavirus crisis. Iran J Psychiatry Behav Sci. 2020;14(1) e102546. [Google Scholar]
- 48.Shojaei S F, Masoumi R. The importance of mental health training for psychologists in COVID-19 outbreak. Middle East J Rehabil Health Stud Online ahead of Print; 7(2): e102846.
- 49.Pérez-Ferre N., Galindo M., Fernández M.D., Velasco V., Runkle I., de la Cruz M.J. The outcomes of gestational diabetes mellitus after a telecare approach are not inferior to traditional outpatient clinic visits. Internet J Endocrinol. 2010;2010 doi: 10.1155/2010/386941. 386941. [DOI] [PMC free article] [PubMed] [Google Scholar]