Abstract
Background and aims
Diabetes is a chronic metabolic condition characterized by hyperglycemia and is associated with several complications. Prevalence of Diabetes in adult population in India ranges from 10.9 to 14.2% in urban area and 3.0–7.8% in rural area. Glycemic control is an important factor in preventing the complications associated with diabetes. HBA1c is the indicator of long-term glycemic control and slight variation in it significantly alters the risk of diabetic complications. Thus, the aim of this study was to study the change in HBA1c levels due to lock down in patients with diabetes.
Methods
307 patients with diabetes who had attended our endocrine OPD in last 3 months before nationwide 68 days lockdown from 24 March 2020 to 31 May 2020, and had recent HBA1c report in past and willing to participate were included in the study after informed consent from 2nd June 2020 to 14th June 2020 when first phase of Unlock started, to identify the change in HBA1c levels during the lockdown period in our patients with diabetes.
Results
The patients were aged between 25–69 years and male to female ratio was 181:126 (1.44: 1). The mean age and mean duration of diabetes in our patients was 55.68 years and 7.95 years respectively. Increment of 0.51% was seen in mean HBA1c levels in our patient from 7.92% mean pre-lockdown HBA1c to mean of 8.43% after release of lock down.
Conclusion
Glycemic control got deranged during lockdown period with significant increase of mean HBA1c by 0.51% in immediate post lock down period which may significantly increase the annual incidence of complications related to diabetes.
Keywords: Diabetes, HBA1c, COVID 19, Lockdown, Glycemic control, Psychological wellbeing
1. Introduction
As world is facing the pandemic due to COVID-19 (Corona Virus Disease 2019) which has high infection rate, several measures are being taken to prevent its spread. And a major step taken by government of India in order to prevent its spread is temporary lock down of country along with all precautions advised like social distancing and social isolation [1].
People with diabetes and other co-morbid conditions like asthma, heart failure, raised serum creatinine and elderly people above the age of 65 years may be at higher risk. The Indian Council of Medical Research-India Diabetes (ICMR-INDIAB) study estimates that approximately 62 million people in India have diabetes [2,3].
Diabetes is a chronic metabolic condition characterized with hyperglycemia and associated with metabolic complications. It is not an uncommon endocrine disorder and prevalence in India ranges from 10.9 to 14.2% in urban area and 3.0–7.8% in rural area [2,3]. A recent survey by World health organization estimated that India have 72.96 million cases of diabetes in adult population [4].
Good Glycemic control is important factor in preventing the complications associated with diabetes. HBA1c is an indicator of long-term glycemic control and slight variation in it significantly alters the risk of diabetic complications. Adaption of good life style modifications which include balanced diet, exercise, proper sleep & psychological wellbeing along with proper medication under medical guidance are the pillars for good glycemic control. All these pillars may be shaken in the lock down period, thus altering the glycemic control [3,5,6].
Hence, aim of our study was to study the change in HBA1c levels due to lock down in patients with diabetes.
This study will help to predict the change in long-term complications in patients with diabetes due to change in HBA1c and to take appropriate steps to prevent such complications.
2. Material and methods
This was the observational cohort study performed at our Endocrine OPD which is a part of tertiary care center at central India, where regular management of all endocrine disorders is provided. In our diabetes clinics regular monitoring of blood sugar parameters like Fasting blood sugars (FBS), Post prandial blood sugars (PLBS) and HBA1c is performed and according to the clinical examination findings specific investigations like renal function tests, liver function tests, lipid profile and many more are performed and accordingly counseling for healthy life style and precautions are advised along with medications.
During COVID lockdown period regular monitoring become difficult but monitoring and management started with telemedicine and few patients actively participated through telemedicine and treatment was individualized according to patients. Patients were advised to consult nearby doctor in cases of emergency and procure medicines from nearby pharmacies.
307 Type 2 Diabetes Mellitus (T2DM) who attended the our endocrine OPD in last 3 months before the 68 days long lock down from 24th March 2020 due to COVID 19 and had HBA1c reporting done in recent past and willing to participate were included in study after informed consent obtained from all patients. The patients were enrolled from 2nd June to 14th June during the first phase of Unlock. The inclusion criteria for enrollment into the study included the following: (1) adult patients with previously diagnosed with T2DM on treatment with regular follow up in past, and (2) willing to participate in the study. Exclusion criteria included (1) Sick patients, (2) No record of HBA1c in last 3 months (3) pregnancy, (4) Not willing to participate in study.
Patients who met the above criteria were included and their clinical data was recorded and were advised for HBA1c and other necessary investigations like FBS, PLBS during the first two weeks of June 2020 after release of lockdown. Then statistical analysis was done with paired T – test, and pre- lock down and post- lock down data was compared were compared. And, Multiple Linear Regression analysis was done to identify the effects of change in weight, diet and physical activity on change in HBA1c levels.
Though Ideal targets for FBS, PLBS and HBA1c are based on age and associated co-morbid condition but for general population FBS, PLBS and HBA1c levels of less than 140 mg/dl, 180 mg/dl and 7.0 respectively is considered ideal.
3. Results
The patients were aged between 25–69 years with mean age of 55.68 years and male to female ratio was 181:126 (1.43:1). The summary of baseline characteristics is described in Table 1 .
Table 1.
Baseline characteristics of patients.
| Parameter | Male (N = 181) |
Female (N = 126) |
Overall (N = 307) |
|||
|---|---|---|---|---|---|---|
| Mean | Range | Mean | Range | Mean | Range | |
| Age (years) | 56.71 | 25–69 | 54.55 | 31–67 | 55.68 | 25–69 |
| BMI (Kg/m2) | 27.41 | 21.11–36.17 | 31.25 | 23.27–37.32 | 28.39 | 21.11–37.32 |
| Duration of DM (years) | 8.18 | 1–27 | 7.96 | 1–23 | 7.95 | 1–27 |
| Systolic blood pressure (mm of Hg) | 133.6 | 110–166 | 129.4 | 100–154 | 131.9 | 100–166 |
| Diastolic blood pressure (mm of Hg) | 81.2 | 60–110 | 74.6 | 60–100 | 78.5 | 60–110 |
In our patients pre lockdown mean weight in male, female and overall were 76.8 Kg, 68.9 Kg and 73.6 Kg respectively and post lock down mean weight in male, female and overall were 77.5 Kg, 70.1 Kg and 74.5 Kg respectively. Details mentioned in Table 2 .
Table 2.
Weight, blood sugar and HBA1c pre- and post-Lock down due to COVID 19 in male patients.
| Pre- lock down |
Post lock down |
P value | ||||
|---|---|---|---|---|---|---|
| Mean | Range | Mean | Range | |||
| Male (N = 181) | Weight (KG) | 76.8 | 55–108 | 77.5 | 55–106 | 0.6 |
| FBS (mg/dl) | 123.3 | 90–146 | 129.2 | 97–164 | 0.04 | |
| PLBS (mg/dl) | 139.7 | 93–227 | 159.5 | 112–355 | 0.01 | |
| HBA1c (%) | 7.85 | 6.1–13.0 | 8.37 | 6.0–15.0 | 0.03 | |
| Female (N = 126) | Weight (KG) | 68.9 | 54–110 | 70.1 | 57–111 | 0.1 |
| FBS mg/dl) | 127.3 | 94–181 | 135.6 | 102–203 | 0.03 | |
| PLBS (mg/dl) | 143.1 | 107–254 | 168.2 | 121–340 | 0.02 | |
| HBA1c (%) | 8.03 | 6.3–15.0 | 8.52 | 6.6–15.0 | 0.02 | |
| Overall (N = 307) | Weight (KG) | 73.6 | 54–110 | 74.5 | 55–111 | 0.4 |
| FBS (mg/dl) | 124.9 | 90–181 | 131.8 | 97–203 | 0.04 | |
| PLBS (mg/dl) | 141.1 | 93–254 | 163.1 | 112–355 | 0.01 | |
| HBA1c (%) | 7.92 | 6.1–15.0 | 8.43 | 6.0–15 | 0.02 | |
Thus, mean weight in immediate post lock down period was higher than pre lock down but statistical difference was not seen as described in Table 2.
In our patients pre lockdown mean FBS in male, female and overall were 123.3 mg/dl, 127.3 mg/dl and 124.9 mg/dl respectively and post lockdown mean FBS in male, female and overall were 129.2 mg/dl, 135.6 mg /dl and 131.8 mg/dl respectively. Details mentioned in Table 2.
In our patients pre lockdown mean PLBS in male, female and overall were 139.7 mg/dl, 143.1 mg/dl and 141.1 mg/dl respectively and post lockdown mean PLBS in male, female and overall were 159.5 mg/dl, 168.2 mg /dl and 163.1 mg/dl respectively. Details mentioned in Table 2.
Thus, both fasting and post prandial blood glucose in immediate post lock down period were higher than pre lock down period and statistically significant difference was seen as described in Table 2. But here statistical significance doesn't reflect clinical significance.
In our patients pre lockdown mean HBA1c in male, female and overall were 7.85%, 8.03% and 7.92% respectively and post lockdown mean HBA1c in male, female and overall were 8.37%, 8.52% and 8.43% respectively. Thus, HBA1c was significantly higher in immediate post lock down period. Results in details is explained in Table 2.
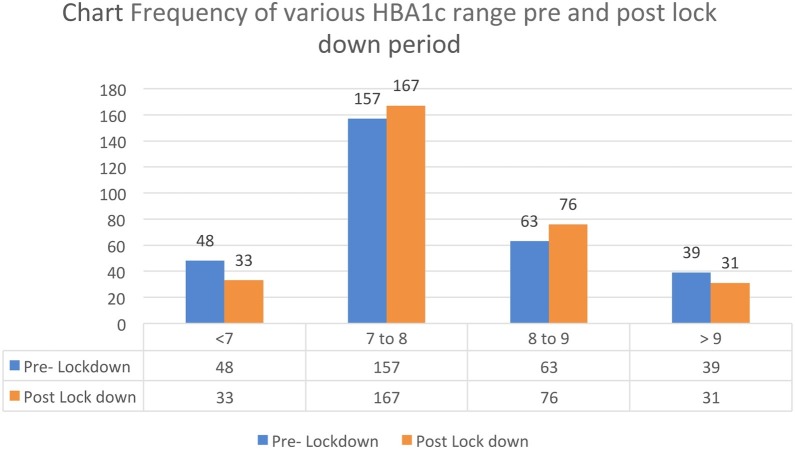
Frequency of HBA1c range during pre-lock down and post lock down period is described in Table 3 and bar Chart 1 . Significant number of patients lost their good glycemic control and came in HBA1c range above 7%.
Table 3.
Frequency of various HBA1c range pre- and post-lock down period.
| HBA1c | Pre-lockdown (%) | Post-lockdown (%) | Change | P value |
|---|---|---|---|---|
| <7 | 48 (15.64%) | 33 (10.75%) | 15 | 0.04 |
| 7–8 | 157 (51.14%) | 167 (54.40%) | 10 | 0.08 |
| 8–9 | 63 (20.52%) | 76 (24.75%) | 13 | 0.03 |
| >9 | 39 (12.70%) | 31 (10.10%) | 8 | 0.1 |
| Total | 307 | 307 |
Chart 1.
Frequency of various HBA1c range pre- and post-lock down period.
The details of change in weight pattern, diet pattern and physical activity pattern is described in Table 4 .
Table 4.
Change in diet, exercise and weight in our patients.
| N = 307 | Percentage (%) | |
|---|---|---|
| Diet | ||
| 1. Quantity | ||
| Same | 147 | 47.9 |
| Increased | 93 | 30.3 |
| Decreased | 67 | 21.8 |
| 2. Frequency | ||
| Same | 139 | 45.3 |
| Increased | 109 | 35.5 |
| Decreased | 59 | 19.2 |
| 3. Timing | ||
| Same | 79 | 25.7 |
| Early | 157 | 51.1 |
| Delayed | 71 | 23.2 |
| 4. Quality | ||
| Same | 81 | 26.4 |
| More healthy | 129 | 42.1 |
| Less healthy | 97 | 31.5 |
| Physical activity | ||
| 1. Duration | ||
| Same | 45 | 14.7 |
| Increased | 128 | 41.7 |
| Decreased | 134 | 43.6 |
| 2. Timing | ||
| Same | 54 | 17.6 |
| Changed | 253 | 82.4 |
| 3. Type | ||
| Same | 51 | 16.6 |
| More resistant | 37 | 12.1 |
| More aerobic | 28 | 9.1 |
| Both aerobic and resistant | 29 | 9.4 |
| Household works | 162 | 52.8 |
| Weight | ||
| 1. Same | 98 | 31.9 |
| 2. Decreased | 96 | 31.3 |
| 3. Increased | 113 | 36.8 |
Multiple linear regression analysis suggests that 14.8% of the variance in HbA1c after lock down can be predicted from the variables of change in weight, diet pattern, and physical activity pattern as described in Table 5 . The P value is 0.29, thus the group of independent variables (change in weight, diet pattern and physical activity pattern) does not show a statistically significant relationship with the dependent variable (HbA1c after lock down).
Table 5.
Multiple linear regression analysis summary.
| Change of statistics |
|||||||||
|---|---|---|---|---|---|---|---|---|---|
| R | R square | Adjusted R square | Std error of estimate | R square change | F change | dF1 | dF2 | P value | |
| 1 | 0.385 | 0.148 | 0.033 | 1.9777 | 0.148 | 1.285 | 37 | 270 | 0.269 |
a. Predictors: (constant), change in weight, diet and physical activity.
b. Dependent variable: Hba1c after lock down.
c. R is correlation coefficient.
d. R-square is the coefficient of determination.
e. dF is degree of freedom.
On sub analysis the coefficient for diet quantity (−.741) is statistically significant because its p-value of 0.04. But the coefficient for change in weight, diet (frequency, timing, quality), physical activity (duration, timing, and type) does not statistically significantly affect HbA1C values because its p-value is greater than 0.05 as described in Table 6 .
Table 6.
Sub analysis of predictors with change in HBA1c-.
| Unstandardized coefficients |
Standardized coefficients | 95% Confidence interval for B |
|||||
|---|---|---|---|---|---|---|---|
| Beta | Std Error | Beta | T value | P value | Lower bound | Upper bound | |
| weight change | .180 | .381 | .076 | .473 | .638 | −.582 | .942 |
| Diet quantity | −.741 | .361 | −.324 | −2.055 | .044 | −1.463 | −.020 |
| Diet frequency | −.047 | .445 | −.021 | −.105 | .917 | −.937 | .844 |
| Diet timing | −.195 | .352 | −.083 | −.556 | .581 | −.899 | .508 |
| Diet quality | .488 | .444 | .202 | 1.101 | .275 | −.399 | 1.376 |
| Activity duration | −.152 | .409 | −.054 | −.372 | .711 | −.971 | .667 |
| Activity timing | −.205 | .432 | −.081 | −.474 | .637 | −1.068 | .659 |
| Activity type | .267 | .246 | .136 | 1.085 | .282 | −.225 | .759 |
a. Dependent variable: Hba1c after lock down.
Out of 307 patients 143 patients were under regular follow up during lock down period through telemedicine. Of these 143 patients, 3 patients had hypoglycemic events during the lock down period and required stepping down of medications while 56 patients reported persistent hyperglycemia and required stepping up of medications during lock down period.
4. Discussion
Lockdown was the significantly important step to stop and prevent the spread of COVID 19 infection that was taken by government of India, but it may have affected the glycemic control in diabetic patients. Good glycemic control is important have good immunity and to prevent complications related diabetes.
HbA1c is an important indicator of long-term glycemic control which has the ability to reflect the cumulative glycemic history of previous two to three months. HbA1c not only provides information regarding long term glycemic control but it’s level also correlates well with the risk of long-term diabetes complications. Thus, a single HbA1c value has rendered it as a reliable biomarker for the diagnosis and prognosis of diabetes [7].
Laiteerapong et al. also described HBA1c as indicator of long-term glycemic control and slight variation in it significantly changes the risk of complications in their article The Legacy Effect in Type 2 Diabetes: Impact of Early Glycemic Control on Future Complications described that 1% increase in HBA1c levels doubles the risk of microvascular complications [8].
In our study mean FBS, PLBS and HBA1c was significantly higher in immediate post-lock down period as compared to previous non lock down period. Possible reason for it may be the change in amount and type of diet due to being at home with lack of exercise and psychological stress due to lockdown [9,10].
In our study the mean weight of our population increased by 0.9 Kg it was numerically high but statistically not significant. Studies have shown the association between the weight change and glycemic control in patients with diabetes and for every 1 kg loss of weight HBA1c reduction by 0.1% is seen [11,12].
Similar observations of worsening of glycemic control were made during previous stressful situations which mimics lock down situation like earthquakes, hurricane, war etc. [[13], [14], [15]].
Similar prediction was made by Ghosal et al. in their article and predicted that the duration of lockdown is directly proportional to the worsening of glycemic control and diabetes-related complications. And this increase in diabetes-related complications will put extra burden on already overburdened healthcare system, and also increase COVID19 infections in patients with such uncontrolled glycemic control. They predicted increment in HBA1c from baseline at the end of 30 days and 45 days lockdown by 2.26% & 3.68% respectively [16]. But in our study mean increment of HBA1c from baseline pre-lock down period was by 0.51% only but was significantly high. Possible factor for this difference may be sample bias and also 46.58% (143) patients were under regular follow up through telemedicine during lock down period and necessary steps were taken to avoid fluctuations in glycemic control.
Ghosal et al. also predicted that annual percentage increase in complication rates at the end of 30-day lockdown was 2.8% for non-proliferative diabetic retinopathy, 2.9% for proliferative diabetic retinopathy, 1.5% for retinal photocoagulation, 9.3% for microalbuminuria, 14.2% for proteinuria, 2.9% for peripheral neuropathy, 10.5% for lower extremity amputation, 0.9% for myocardial infarction, 0.5% for stroke and 0.5% for infections [16].
Thus, multidisciplinary approach is required which is patient centric and addresses the various issues like psychological stress, diet exercise along with proper medication is required for achieving good glycemic control and reduce the predicted annual percentage increase in complication rate [17].
5. Conclusion
Our study being among first of its kind, showed that overall glycemic control got deranged during lockdown period with significant increase of mean HBA1c by 0.51% in immediate post lock down period which may significantly increase the annual incidence of complications related to diabetes. But through early identification and multidisciplinary approach which is patient centric and addresses the various issues like psychological stress, diet exercise along with proper medication good glycemic control can be achieved back and reduce the predicted annual percentage increase in complication rate.
6. Limitation of study
Possibility of sample Bias cannot be ruled out as patients were from one center. It was an unblinded study and some patients were under regular follow up through telemedicine and interventions were taken if very high fluctuation in blood sugars noted. Identifying the possible factor responsible for the loss of glycemic control was not entertained in this study.
Conflict of interest
Declare that there is no conflict of interest that could be perceived as prejudicing the impartiality of the research reported.
Funding
This research did not receive any specific grant from any funding agency in the public, commercial or not-for-profit sector.
Acknowledgment
We would like to acknowledge Dr. Jalaj Khare, for helping in statistical analysis.
References
- 1.India COVID-19 Tracker. 2020. [Online] Available at: https://www.covid19india.org/.
- 2.Anjana R.M., Pradeepa R., Deepa M., Datta M., Sudha V., Unnikrishnan R., et al. Prevalence of diabetes and prediabetes (impaired fasting glucose and/or impaired glucose tolerance) in urban and rural India: phase I results of the Indian Council of Medical Research-India DIABetes (ICMR-INDIAB) study. Diabetologia. 2011;54:3022–3027. doi: 10.1007/s00125-011-2291-5. [DOI] [PubMed] [Google Scholar]
- 3.Mohan V., Shah S.N., Joshi S.R., Seshiah V., Sahay B.K., Banerjee S., et al. Current status of management, control, complications and psychosocial aspects of patients with diabetes in India: results from the DiabCare India 2011 Study. Indian J. Endocrinol. Metab. 2014;18(3):370–378. doi: 10.4103/2230-8210.129715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Government survey found 11.8% prevalence of diabetes in India. [ONLINE 2019] https://www.livemint.com/science/health/government-survey-found-11-8-prevalence-of-diabetes-in-india-11570702665713.html.
- 5.Standards of medical care in diabetes—2019, Diabetes care January 2019, 42 (Supplement 1) DOI: 10.2337/dc19-Sint01. [DOI]
- 6.Kalra S., Jena B.N., Yeravdekar R. Emotional and psychological needs of people with diabetes. Indian J. Endocr. Metab. 2018;22:696–704. doi: 10.4103/ijem.IJEM_579_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sherwani et al. Significance of HbA1c test in diagnosis and prognosis of diabetic patients. Biomarker Insights 2016:11 95–104 doi: 10.4137/Bmi.S38440. [DOI] [PMC free article] [PubMed]
- 8.Laiteerapong N., Ham S.A., Gao Y., Moffet H.H., Liu J.Y., Huang E.S., Karter A.J. The legacy effect in type 2 diabetes: impact of early glycemic control on future complications (The diabetes & aging study) Diabetes Care. 2019;42:416–426. doi: 10.2337/dc17-1144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ghosh A., Arora B., Gupta R., Anoop S., Misra A. Effects of nationwide lockdown during COVID-19 epidemic on lifestyle and other medical issues of patients with type 2 diabetes in north India. Diabetes Metab. Syndr. Clin. Res. Rev. 2020;14(5):917–920. doi: 10.1016/j.dsx.2020.05.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Khare J., Jindal S. Observational study on Effect of Lock Down due to COVID 19 on glycemic control in patients with Diabetes: experience from Central India. Diabetes Metab. Syndr. Clin. Res. Rev. 2020;14:1571–1574. doi: 10.1016/j.dsx.2020.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gummesson Anders, Nyman Elisabeth, Knutsson Mikael, Karpefors Martin. Effect of weight reduction on glycated haemoglobin in weight loss trials in patients with type 2 diabetes. Diabetes Obes. Metab. 2017;19(September (9)):1295–1305. doi: 10.1111/dom.12971. [DOI] [PubMed] [Google Scholar]
- 12.Umpierrez G.E., Pantalone K.M., Kwan A.Y.M., Zimmermann A.G., Zhang N., Fernández Landó L. Relationship between weight change and glycaemic control in patients with type 2 diabetes receiving once-weekly dulaglutide treatment. Diabetes Obes. Metab. 2016;18:615–622. doi: 10.1111/dom.12660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fonseca V.A., Smith H., Kuhadiya N., Leger S.M., Yau C.L., Reynolds K., et al. Impact of a natural disaster on diabetes. Diabetes Care. 2009;32:1632–1638. doi: 10.2337/dc09-0670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fujihara K., Saito A., Heianza Y., Gibo H., Suzuki H., Shimano H., et al. Impact of psychological stress caused by the Great East Japan earthquake on glycemic control in patients with diabetes. Exp. Clin. Endocrinol. Diabetes. 2012;120(9):560–563. doi: 10.1055/s-0032-1314873. [DOI] [PubMed] [Google Scholar]
- 15.Rubinstein A., Koffler M., Villa Y., Graff E. The Gulf War and diabetes mellitus. Diabet. Med. 1993;10:774–776. doi: 10.1111/j.1464-5491.1993.tb00163.x. [DOI] [PubMed] [Google Scholar]
- 16.Ghosal S., Sinha B., Majumder M., Misra A. Estimation of effects of nationwide lockdown for containing coronavirus infection on worsening of glycosylated haemoglobin and increase in diabetes-related complications: a simulation model using multivariate regression analysis. Diabetes Metab. Syndr. Clin. Res. Rev. 2020 doi: 10.1016/j.dsx.2020.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Juliana CN Chan, Lee-Ling Lim, Nicholas J Wareham, Jonathan E Shaw, Trevor J Orchard, Ping Zhang et al. The Lancet Commission on diabetes: using data to transform diabetes care and patient lives. The Lancet, 10.1016/S0140-6736(20)32374-6. [DOI] [PubMed]