Abstract
A 57-year-old man acutely developed chest tightness and dyspnea. Given concern that his symptoms were consistent with COVID-19, the patient self-isolated. After 1 week of worsening symptoms, the patient presented with hypoxia and hypotension. He was found to have an occluded right coronary artery and ruptured posteromedial papillary muscle. (Level of Difficulty: Beginner.)
Key Words: COVID-19, papillary muscle rupture, ST-segment elevation myocardial infarction (STEMI)
Abbreviations and Acronyms: COVID-19, coronavirus disease-2019; ECMO, venoarterial extracorporeal membrane oxygenation; SARS-CoV-2, severe acute respiratory syndrome-coronavirus-2; STEMI, ST-segment elevation myocardial infarction
Graphical abstract
A 57-year-old man acutely developed chest tightness and dyspnea. Given concern that his symptoms were consistent with COVID-19, the…
History of Presentation
On April 3, 2020, a 57-year old man with a family history notable for premature coronary artery disease presented to the emergency department with 7 days of worsening chest tightness and shortness of breath. One week before presentation, the patient woke from sleep with chest tightness, diaphoresis, and shortness of breath. Given concern for coronavirus disease-2019 (COVID-19), the patient self-isolated at home, during which time he had intermittent fevers to 101°F and cough, worsening exertional dyspnea, orthopnea, and paroxysmal nocturnal dyspnea. On presentation, he was afebrile (99.3°F), hypotensive (86/68 mm Hg), tachycardic (103 beats/min), tachypneic (24 breaths/min), and hypoxic (86% on room air).
Learning Objectives
-
•
To appreciate the excess mechanical complications in patients presenting with late STEMI resulting from the COVID-19 pandemic.
-
•
To understand the origin and physiological consequences of post-infarction acute papillary muscle rupture.
Past Medical History
His past medical history included hypertension, hyperlipidemia, former tobacco use, family history of premature coronary artery disease, stage II chronic kidney disease, and intermittent asthma.
Investigations
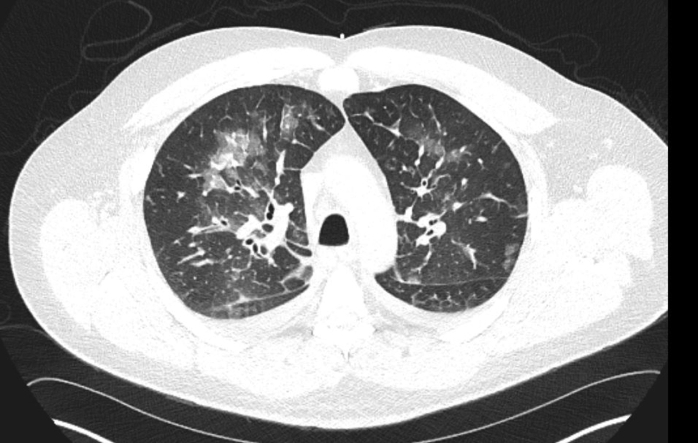
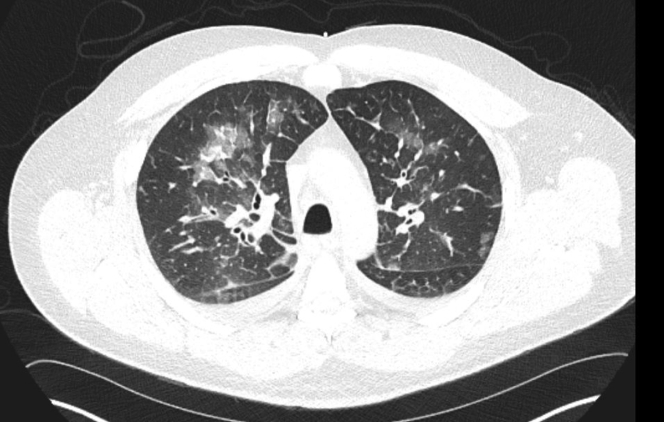
Laboratory investigations were notable for elevated creatinine (3.08 mg/dl), transaminitis (alanine aminotransferase 82 U/l, aspartate aminotransferase 44 U/l), leukocytosis (16.1 K/μl), and elevated troponin-T (1.29 ng/ml). The results of a respiratory pathogen profile, including influenza and Xpert Xpress severe acute respiratory syndrome-coronavirus-2 (SARS-CoV-2) assay (Cepheid, Sunnyvale, California), were negative. Portable chest radiograph revealed right upper lung patchy opacity consistent with focal pneumonia. Computed tomography of the chest was notable for bilateral patchy, rounded, ground-glass opacities predominantly located centrally and in the upper lobes (Figure 1). The patient’s electrocardiogram was notable for inferior Q waves and T-wave inversions with no ST-segment changes (Figure 2).
Figure 1.
Chest Computed Tomography on Presentation Showing Bilateral Central Ground-Glass Opacities With Thickened Interlobar Septa
Figure 2.
Presenting Electrocardiogram Showing Sinus Tachycardia With Inferior Q Waves and T-Wave Inversions
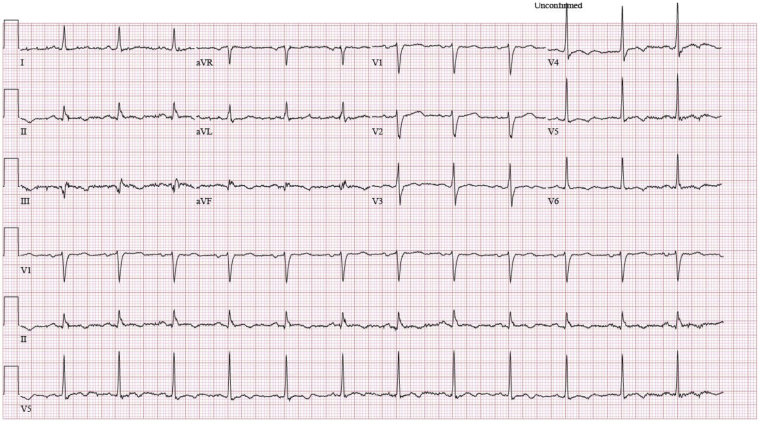
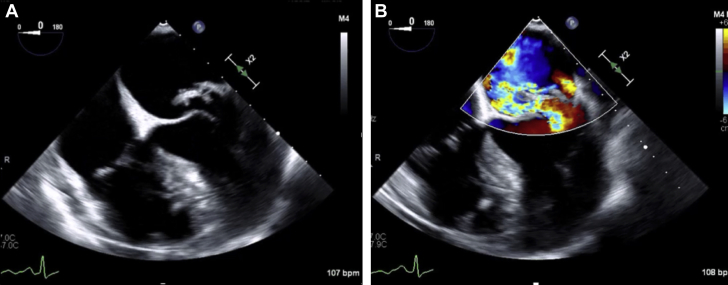
Given concern for hypoxia, fevers, and cough, the patient was admitted to the COVID-19 unit as a person under investigation. The result of a repeat SARS-CoV-2 test was negative. Bedside transthoracic echocardiogram demonstrated an ejection fraction of 65% with inferior hypokinesis and at least mild to moderate mitral regurgitation. Diagnostic coronary angiography was notable for an occluded right coronary artery with nonobstructive disease in the left system (Figures 3 and 4). Transesophageal echocardiography demonstrated severe mitral regurgitation with a ruptured posteromedial papillary muscle with flail P2 and P3 segments of the posterior mitral leaflet (Figure 5, Video 1).
Figure 3.
Diagnostic Coronary Angiography Demonstrating Occlusion of the Mid-Right Coronary Artery
Figure 4.
Diagnostic Coronary Angiography Demonstrating Nonocclusive Coronary Artery Disease in the Left Main, Left Circumflex, and Left Anterior Descending Coronary Arteries
Figure 5.
Transesophageal Echocardiographic Views
(A) Midesophageal 4-chamber view demonstrating posteromedial papillary muscle rupture with flail of the P2 portion of the mitral valve. (B) Color flow Doppler demonstrating severe anteriorly directed mitral regurgitation.
Online Video 1.
A 3-dimensional transesophageal echocardiogram demonstrated posterior leaflet flail with ruptured posteromedial papillary muscle.
Management
Despite placement of an intra-aortic balloon pump, the patient became increasingly hypoxic and hypotensive, and he required escalating doses of vasopressors. The patient was ultimately intubated and peripherally cannulated for venoarterial extracorporeal membrane oxygenation (ECMO). Two days later, following clinical improvement in oxygenation and renal function, the patient underwent mitral valve replacement with a No. 31 St. Jude mechanical mitral valve prosthesis (Abbott, Abbott Park, Illinois) and ECMO decannulation.
Discussion
The incidence of papillary muscle rupture has decreased dramatically following the widespread adoption of primary percutaneous coronary intervention in patients with STEMI. In modern series, the incidence of ischemic papillary muscle rupture in patients presenting with STEMI is 0.25% (1). Although this complication is rare, it carries a poor prognosis, with an in-hospital mortality exceeding 50% (2).
In the setting of acute myocardial infarction, the rupture of the posteromedial papillary muscle is much more common than anterolateral papillary muscle rupture given the single blood supply of the posteromedial papillary muscle from either the dominant right coronary artery or the dominant left circumflex coronary artery. The anterolateral papillary muscle has a dual blood supply and is thus considerably less susceptible to ischemic injury. Papillary muscle rupture generally occurs between 2 and 7 days following an inferior myocardial infarction and is responsible for 7% of patients presenting in cardiogenic shock following myocardial infarction (3).
The hemodynamic consequences of acute mitral regurgitation result from the rapid delivery of a large volume load on the left atrium and ventricle leading to right-sided dysfunction. As a result of acute volume loading of an un-remodeled left atrium, there is a marked rise in left atrial pressure leading to elevated pulmonary pressure and pulmonary edema. This can result in refractory hypoxemia and cardiogenic shock (4).
Medical management of acute mitral regurgitation consists primarily of afterload reduction with vasodilators and inodilators such as sodium nitroprusside and milrinone. These patients may also benefit from mechanical unloading with an intra-aortic balloon pump or venoarterial ECMO for circulatory and respiratory support (3). Despite a high perioperative mortality (24%), surgical replacement of the mitral valve remains the cornerstone of treatment (5). The timing of surgery is generally recommended to be as early in the patient’s course as is feasible (6).
Follow-Up
The patient was successfully extubated on post-operative day 1. His post-operative course was uncomplicated. He was discharged on post-operative day 9 with a therapeutic international normalized ratio. At a telemedicine visit with the patient 1 week after discharge, the patient reported no chest discomfort, shortness of breath, or activity limitations.
Conclusions
This case demonstrates the potential dangers of public messaging that encourages patients with respiratory symptoms to avoid medical care during the SARS-CoV-2/COVID-19 global pandemic. Additionally, potential anchoring bias in a patient reporting cough and fevers who presented with hypoxia led to delays in the diagnosis and management of severe mitral regurgitation secondary to a ruptured posteromedial papillary muscle and a completed inferior STEMI. Prompt recognition and surgical management of this mechanical complication of myocardial infarction are critical to ensure a satisfactory outcome.
Footnotes
Dr. Anwaruddin is on the advisory board of Medtronic; has received speaker fees from Medtronic and Edwards Lifesciences; has received honoraria from Medtronic and Siemens; and is a consultant for V wave. Dr. Kunkel has reported that she has no relationships relevant to the contents of this paper to disclose.
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the JACC: Case Reportsauthor instructions page.
Appendix
For a supplemental video, please see the online version of this paper.
References
- 1.French J.K., Hellkamp A.S., Armstrong P.W. Mechanical complications after percutaneous coronary intervention in ST-elevation myocardial infarction (from APEX-AMI) Am J Cardiol. 2010;105:59–63. doi: 10.1016/j.amjcard.2009.08.653. [DOI] [PubMed] [Google Scholar]
- 2.French J.K., Armstrong P.W., Cohen E. Cardiogenic shock and heart failure post-percutaneous intervention in ST-elevation myocardial infarction: observations from “Assessment of Pexelizumab on Acute Myocardial Infarction.”. Am Heart J. 2011;162:89–97. doi: 10.1016/j.ahj.2011.04.009. [DOI] [PubMed] [Google Scholar]
- 3.Kutty R.S., Hones N., Moorjani N. Mechanical complications of acute myocardial infarction Cardiol. Clin. 2013;31:519–531. doi: 10.1016/j.ccl.2013.07.004. [DOI] [PubMed] [Google Scholar]
- 4.Harari R., Bansal P., Yatskar L. Papillary muscle rupture following acute myocardial infarction: anatomic. echocardiographic, and surgical insights Echocardiography. 2017;34:1702–1707. doi: 10.1111/echo.13739. [DOI] [PubMed] [Google Scholar]
- 5.Chevalier P.E., Burri H., Fahrat F. Perioperative outcome and long-term survival of surgery for acute post-infarction mitral regurgitation. Eur J Cardiothorac Surg. 2004;26:330–335. doi: 10.1016/j.ejcts.2004.04.027. [DOI] [PubMed] [Google Scholar]
- 6.Nishimura R.A., Schaff H.V., Gersh B.J. Early repair of mechanical complications after acute myocardial infarction. JAMA. 1986;256:47–50. [PubMed] [Google Scholar]