Abstract
Background
In the context of the COVID-19 pandemic, prone position (PP) has been frequently used in the intensive care units to improve the prognosis in patients with respiratory distress. However, turning patients to prone imply important complications such as pressure ulcers. The aim of this paper is to describe the prevalence and characteristics of prone-positioning pressure sores (PPPS) and analyze the related risk factors.
Methods
A case-control study was performed in Gregorio Maranon hospital in Madrid during the COVID-19 pandemic between April and May 2020. We enrolled 74 confirmed COVID-19 patients in critical care units with invasive mechanical ventilation who were treated with pronation therapy. There were 57 cases and 17 controls. Demographic data, pronation maneuver characteristics and PPPS features were analyzed.
Results
In the case group, a total number of 136 PPPS were recorded. The face was the most affected region (69%). Regarding the severity, stage II was the most frequent. The main variables associated with an increased risk of PPPS were the total number of days under pronation cycles, and PP maintained for more than 24 h. The prealbumin level at admission was significantly lower in the case group. All of the ulcers were treated with dressings. The most frequent acute complication was bleeding (5%).
Conclusions
According to our study, PPPS are related to the characteristics of the maneuver and the previous nutritional state. The implementation of improved positioning protocols may enhance results in critical patient caring, to avoid the scars and social stigma that these injuries entail.
Keywords: COVID-19, Sars-Cov-2, Prone positioning, Bedsores, Pressure ulcer prevention
Introduction
COVID-19 is a new respiratory disease caused by the SARS-CoV-2 virus, which produced a worldwide pandemic during the first months of 2020 1 and that affects the respiratory system causing an acute respiratory distress syndrome (ARDS) in 19% of the patients 2. Literature recommendations for ARDS include lung protective ventilation and prone position (PP) 3. Early start of PP with prolonged sessions (>16 h) has demonstrated to reduce mortality in these patients.4 , 5
Although PP has recognized the benefits, it has complications. They include unplanned extubation, removal of central or arterial lines, bronchoaspiration, transient desaturation, hypotension, facial edema, corneal abrasions, brachial plexus injury, and pressure ulcers. Among them, pressure ulcers are the most frequent.6 Pressure injuries are localized damage to the skin and underlying soft tissue usually over a bony prominence or in relation to a medical device.7 Their presence after PP is common,8, 9, 10 but frequently ignored given the severity of the primary clinical condition.
As prone positioning is likely to become a frequent occurrence in the intensive care units (ICUs) during the next months, this paper hopes to aware clinicians and nurses of the main risk factors of PPPS to improve the safety and avoid complications of PP in mechanically ventilated patients. To our knowledge, this is the first study that analyzes the risk factors for PPPS in critical care units.
Methods
A case-control study was performed in Gregorio Maranon hospital in Madrid during the COVID-19 pandemic between April and May 2020, in accordance with the ethical standards of the Declaration of Helsinki. We included patients with COVID-19+ disease confirmed by polymerase chain reaction who were on invasive mechanical ventilation and treated with PP therapy. Patients treated only with noninvasive ventilation and patients not treated with PP were excluded. In all, 74 patients met the inclusion criteria. Cases were defined as those who presented prone-positioning pressure sores (PPPS) such as ulcers in the forehead, cheek, ala nasi, lip, chin, chest, knee, leg or toes; whereas controls were classified as those who met inclusion criteria but did not present any PP pressure injuries. Ulcers because of supine position (occipital, sacral, heels, etc.) and ulcers on the bridge of the nose because of face masks related to noninvasive ventilation were not considered PPPS.
The presence, location, and severity of PPPS over bony prominences, as well as the injuries related to a medical or other device were recorded by the authors. The severity of the pressure injuries was evaluated according to the National Pressure Ulcer Advisory Panel (NPUAP).7 Medical history data were collected from the medical and nurse charts. Analysis included age, gender, previous tobacco use, body mass index (BMI), diabetes mellitus (DM), hypertension, peripheral vasculopathy, Braden scale, lactate, prealbumin, and albumin levels at the time of ICU admission, use of vasoactive drugs, total number of PP cycles, total number of days in pronation cycles, the use of prolonged PP beyond 24 h, number of days with double-lumen nasogastric tubes, length of stay in ICU, and PPPS outcome.
Our hospital protocol for PP (Supplementary data 1) followed the guidelines and recommendations of the Intensive Care Society and the Faculty of Intensive Care Medicine.11 Indication for PP was placed in patients with moderate to severe ARDS and PaO2:FiO2 ratio <150 mmHg and FiO2>0.6. Pronation cycle was defined as the period in which the patient is maintained in PP before returning to supine. The pronation cycle was planned for a minimum of 16 h, and then the patient was turned supine for 8 h. However, some patients were maintained prone for more than 16 h (prolonged pronation cycle) because they could not tolerate ventilation in supine position. PP was done manually by a team of 5 healthcare workers, including an airway doctor (intensivist/anesthetist/surgeon) and at least two other health workers (doctor/nurse/nursing auxiliary) either side of the patient. A specific prone ventilation checklist (Supplementary data 1) was used and read out loud to simplify the procedure of turning a patient to prone and enhance patient safety while preventing shear and pressure over bony prominences or medical devices. Preventive measures to avoid pressure ulcers are shown in Figure 1 . An anti-decubitus mattress (Primo™ dynamic low-pressure mattress, Hill-Rom INC, Bastesville, IN, USA) was used in every patient for pressure redistribution. Patients were made to lie in a swimmer crawl position with one arm above the head and the opposite arm alongside the body, alternating arm positions every 4 h and with a routine repositioning of the head. Foam head support (Gentle TouchⓇ Headrest Pillow, Mizuho OSI, Union City, CA, USA) was used to offload face pressure points. Pillows were used to raise the chest and shoulders, pelvis and shins off the bed to reduce pressure points. Hyperoxygenated fatty acids were used in vulnerable areas and stage I ulcers. Foam dressings made from polyurethane (BiatainⓇ Silicone, Coloplast, Humlebaek, Denmark) to provide cushioning, combined with silicone to protect the surrounding skin, or hydrocolloid dressings (ComfeelⓇ plus, Coloplast, Humlebaek, Denmark) were used in stage II and III ulcers and to protect nostril and lips from medical device-related pressure injuries. Skin was assessed before and after pronating to look for incipient sores, other dermatological lesions, infections, and vascular or thrombotic complications.
Figure 1.
Preventive measures. Figure 1A. Patient in a swimmer's crawl position. Note that pillows are used to raise the shoulders, pelvis, and shins. Figure 1B. Foam head support was used to offload face pressure points.
Mann Whitney U test was used to compare quantitative variables and Chi-square test to calculate the odds ratio between categorical variables. A p-value < 0.05 was considered as statistically significant.
Results
A total of 74 patients with ARDS caused by SARS-Cov-2 that were on invasive mechanical ventilation and treated with PP in our critical care units were recruited. Case and controls matched according to demographic characteristics as shown in Table 1 , with no substantial differences.
Table 1.
Descriptive characteristics of ICU patients with invasive mechanical ventilation and pronation therapy in both groups.
| Case (N = 57) | Control (N = 17) | ||
|---|---|---|---|
| Gender | Male | 41 (72%) | 13 (76%) |
| Female | 16 (28%) | 4 (24%) | |
| Age (years)* | 61 [56–69] | 64 [54–71] | |
| BMI (Kg/m2)* | 29.4 [26–33] | 28.1 [27–31] | |
| Length of ICU stay (days)* | 44 [35–54] | 37 [26–52] | |
| Braden scale21 (Very high-risk) | 57 (100%) | 17 (100%) | |
| Exitus | 21 (37%) | 5 (29%) | |
Results expressed in medians and interquartile ranges.
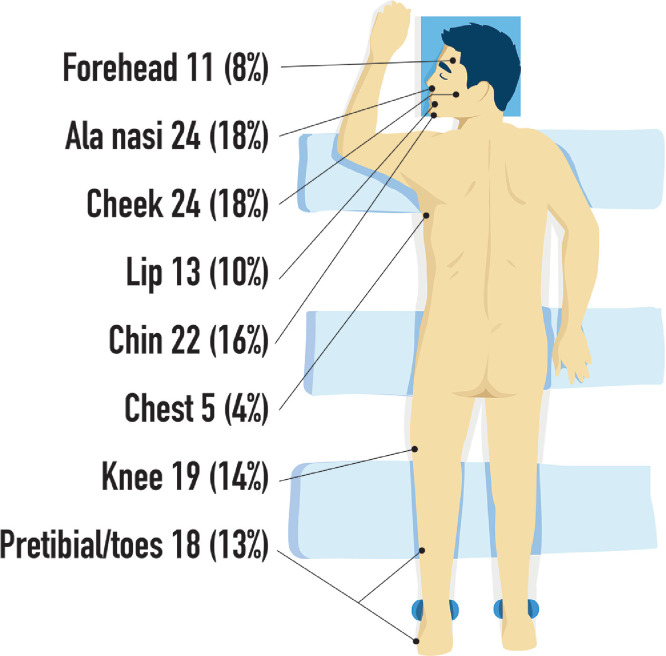
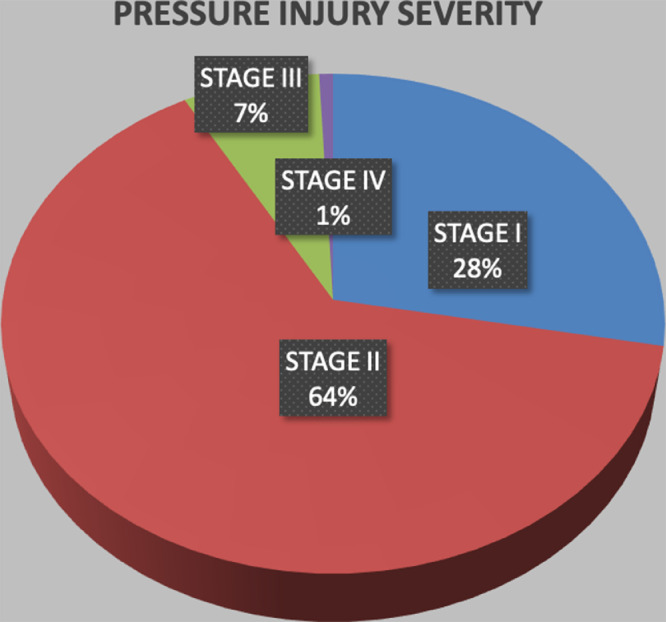
In the case group, a total number of 136 PPPS were recorded (Figure 2, Figure 3, Figure 4, Figure 5, Figure 6, Figure 7 ). Figure 8 shows the distribution by location, highlighting that the cheek (18%), ala nasi (18%), and chin (16%) were the most affected areas. Regarding the severity, Figure 9 shows that the prevalence of stage II ulcers was the highest (64%), followed by stage I ulcers (28%).
Figure 2.
Ulcer in the ala nasi and eyebrow.
Figure 3.
Ala-nasi pressure ulcer.
Figure 4.
Pressure ulcer in the nose, lips, and chin.
Figure 5.
Chin ulcer.
Figure 6.
Chest pressure ulcer.
Figure 7.
Bilateral pretibial pressure ulcers.
Figure 8.
Topographic distribution of pressure sores by location.
Figure 9.
Representation of the pressure injury severity.
All the PPPS were managed with dressings, achieving wound healing by secondary intention in all the survivors, but we found hyper/hypopigmentation of the scars in some patients. On the other hand, the only two patients with stage IV ulcers (one in the ala nasi and one in the tibia), that would have required a future surgery, died during the follow-up. There was a total of 12 complications as shown in Table 2 , where bleeding (5%) and cellulitis (3%) were the most commonly observed. Only one patient developed a skin abscess in the chin that required a bedside surgical drainage (Figure 10 ). Twenty-six patients (35%) died in the ICU during follow-up.
Table 2.
Complications of pressure ulcers due to prone position.
| Complication | N = 136 | % |
|---|---|---|
| Bleeding | 7 | 5 |
| Cellulitis | 4 | 3 |
| Skin abscess | 1 | 1 |
| Chronification | 0 | 0 |
Bleeding: Ulcer foam dressing saturated with blood, requiring the evaluation of a surgeon.
Cellulitis: Skin infection characterized by redness, warmth, swelling, and tenderness surrounding the pressure ulcer, needing antibiotics.
Skin abscess: Swollen, pus-filled lump under pressure-damaged skin, needing drainage.
Chronification: Pressure ulcer that does not heal after three months.
Figure 10.
Chin ulcer complicated with an abscess.
Risk factors that might have influenced the formation of PPPS were analyzed, showing that >24 h constant prone positioning significantly increased the presence of PPPS (OR: 2.88 and p = 0.015). In the same way, the total number of days in pronation cycles was significantly higher in the group of cases when compared with the control group (51% vs 18% and p = 0.011). However, although the total number of pronation cycles was higher in the case group, we could not find any statistical significance between both groups regarding this point (Table 3 ).
Table 3.
Parameters of prone-positioning maneuver between groups.
| Value | p-value | ||
|---|---|---|---|
| Total pronation cycles (average) | Case | 6 | 0.290 |
| Control | 5 | ||
| Days under pronation therapy (average) | Case | 13 | 0.011* |
| Control | 8 | ||
| Patients with prone position maintained for more than 24 h (number and percentage) | Case | 29 (51%) | 0.015* |
| Control | 3 (18%) | ||
p-value <0.05, statistically significant.
A comparison of the analytical parameters at the time of ICU admission between both groups is shown in Table 4 , demonstrating that prealbumin value was significantly higher in the case group (p = 0.019), but with no statistical differences with regard to lactic acid and serum albumin levels.
Table 4.
Analytic parameters at the time of ICU admission.
| Average value | p-value | ||
|---|---|---|---|
| Prealbumin (mg/dL) | Case | 24 | 0.019* |
| Control | 35 | ||
| Lactic acid (mmol/L) | Case | 2 | 0.899 |
| Control | 2 | ||
| Serum albumin (g/dL) | Case | 3 | 0.340 |
| Control | 3 | ||
p-value <0.05, statistically significant.
When comparing nostril and nasal alar sores alone between groups, time with double-lumen nasogastric tube was not significantly increased in this subgroup of cases (p = 0.573). Likewise, there were no differences between groups with respect to age, gender, Braden scale, previous tobacco use, BMI, DM, hypertension or peripheral vasculopathy, use of vasoactive drugs, and the length of stay in ICU.
Discussion
Ventilation in the PP has shown to reduce the mortality rate in severe ARDS.4 Despite being a low cost-effective measure,12 recent studies report that PP is still infrequently used, adopted only in 33%13 of patients with severe ARDS, and considered as a rescue maneuver.14 However, the pronation therapy has seen a recent resurgence and has played a key role during the COVID-19 pandemic in our ICUs. Indications for prone positioning are moderate to severe ARDS with a PaO2/FiO2 ratio <150 mmHg and a FiO2 ≥0.6.4 The main reasons for not pronating patients in our hospital were hemodynamic instability, insufficiently severe hypoxemia to justify PP or not previous response to PP, in accordance with other authors recommendations.13 In our ICUs, patients with tracheotomy or extracorporeal membrane oxygenation were only pronated if there was indication for it and a clear benefit in previous PP.
Despite the ventilation benefits of PP, the complications reported in the literature are significant.5 , 15 Among them, PPPS are the most frequent and a serious concern to consider.10
Previous research has emphasized that it is more likely to have a pressure injury when patients are in prone than in supine position.8 , 10 However, we can find a wide variability across studies concerning patients in PP who develop pressure sores, with rates varying from 14% to 57%;6 , 8, 9, 10 but this shows that better prevention measures and care can have an impact on lower complication rates.12
In our study, with the largest series of patients on invasive mechanical ventilation and PP therapy, 77% of the patients presented with PPPS. The substantially higher prevalence of PPPS in our units when compared with previous studies can be explained by the overwhelming situation during the pandemic, exceeding our hospital's capacity, opening new ICUs every week (from 2 ICUs with 18 beds we multiplicated to 7 ICUs with total capacity of 134 patients in one month) and triggering a sudden and unexpected increase of patients with ARDS requiring PP.
In this context, with the health workers exhausted by the stifling protective suits and the fear of dealing with COVID-19 patients, in combination with the staff shortage under quarantine, new undertrained staff not familiar with PP and ICU nursing cares, and volunteers from other medical fields without skills in the process of turning patients to PP, it is understandable that the complications of this procedure increased.
This result ties well with studies published before the COVID-19 pandemic, wherein complication rates reduce when PP is performed by an experienced team.13 Although it is clear that the prevention of PPPS was not adequate, we have now strengthened the preventive education of PPPS for medical and nursing staff, and hope this study can contribute to avoid this situation in the possible upcoming outbreaks.
A further novel finding of our study is the high incidence of Medical Device-Related Pressure injuries in mucosal tissues because of prone positioning, such as ulcers of the lips (10%) caused by endotracheal tubes, and in ala nasi and nostrils (18%) in relation with nasogastric tubes. However, we could not find a statistical association of these injuries with the duration of double-lumen nasogastric tube used for decompression, which is a thicker and more rigid tube than the nasogastric tube placed for enteral feeding.
These medical device injuries, added to the high prevalence of pressure ulcers on the forehead (8%), cheek (18%), and chin (16%), makes the face the likeliest region to develop a PPPS (69%), in line with the data of surgeries done in the PP.16, 17, 18 The physical and emotional impact of face injuries in these patients can be devastating, and social stigma associated with scarring because of COVID-19 can cause serious concerns.
Regarding the pressure ulcer severity, consistent with previous findings,12 the most frequent stage of the NPUAP was stage II (64%), followed by stage I (28%). These injuries, as well as small, stage III ulcers of the face, usually progress successfully with dressings. On the other hand, patients with stage IV ulcers who would have required a future surgery to cover an ulcer defect of the nose and tibia, died during follow-up. Therefore, stage IV ulcers may be seen as preterminal event markers.
Complications of PPPS have not been described in the literature. In our study, the most frequent acute complication of PPPS was bleeding in seven ulcers (7%), associated with the irritation of medical devices, coagulopathy, and the high doses of anticoagulants in obese patients. Chronic complications will need to be evaluated during the follow up. In addition to the hyper/hypopigmentation of the scars, we expect to find permanent loss of facial hair in the eyebrow and beard, unesthetic deformity, and retraction in ala nasi, among other sequelae.
It is widely described that the best management for pressure ulcers is its prevention. Risk factors related specifically to prone pressure ulcers in ICU patients with ADRS have not been previously studied. ICU patients usually have comorbidities and present multiple risk factors for the development of pressure ulcers,19 but no consensus exists on the best way to measure them.20 Risk assessment with the Braden scale21 (that measures sensory perception, skin moisture, activity, mobility, nutrition, and friction and shear) is widely used to identify those patients who require preventive measures. All of our patients were classified as a very high-risk score of presenting pressure ulcers in the Braden scale and therefore needed an extra care. Regarding nutritional status, we used serum albumin and prealbumin as objective criteria for nutritional assessment,22 demonstrating that prealbumin value was significantly higher in the case group but with no statistical differences with regard to serum albumin levels.
We could not find age, gender, BMI, or other comorbidity differences between both groups. However, we can say that patients with PP maintained for more than 24 h, or with higher number of days in pronation sessions, are associated with a greater risk of PPPS. A similar pattern of results is described in the literature of spine surgery, where authors affirm that the duration of the surgical procedure in the PP is the largest risk factor for the development of PPPS.23
Early start of PP with prolonged cycles (>16 h) has demonstrated to reduce mortality in patients with ADRS.4 However, the optimal duration of the PP is uncertain,24 , 25 and patients usually do not maintain PP for more than 24 h. Given the exceptional circumstances during the pandemic, if a patient needs a prolonged cycle beyond 24 h, we recommend paying additional attention and protection to prevent PPPS.
To our knowledge, this is the study with the largest series of pressure ulcers due to prone positioning and the first one done in COVID-19 patients. It shares valuable information about the prevalence, characteristics, and complications of pressure ulcers related to prone positioning in patients who require mechanical ventilation and pronation therapy in the ICUs of Madrid during the COVID-19 pandemic.
We describe how the total number of days of pronation therapy and a PP maintained for more than 24 h as well as the previous nutrition state measured by prealbumin levels, are significantly related to the development of PPPS. Even though PPPS are not life-threatening lesions, the implementation of improved positioning protocols may enhance results in critical patient care.
We believe that this is a current global underestimated problem as the incidence of COVID-19 patients requiring prone positioning (and therefore the presence of PPPS) is increasing day by day. We hope that the results of our effort can improve the awareness and the prevention of pressure ulcers due to prone positioning, so that those patients who survive COVID-19 can live without these preventable sequelae.
Acknowledgments
Acknowledgments
We would like to thank all of the medical staff who worked on the frontline of the COVID-19 pandemic.
Authorship Statement
All authors have made substantial contributions to all of the following:
(1) The conception and design of the study, or acquisition of data, or analysis and interpretation of data
(2) Drafting the article or revising it critically for important intellectual content
(3) Final approval of the version to be submitted.
Funding
None.
Conflicts of interest
None declared.
Ethical approval
Not required.
Footnotes
Supplementary data 1. Prone-positioning protocol. Hospital Universitario Gregorio Maranon. (Translated to English)
Supplementary data 2. Facial foam support.
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.bjps.2020.12.057.
Appendix. Supplementary materials
References
- 1.Chen N., Zhou M., Dong X. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395:507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhu J., Ji P., Pang J., Zhong Z., Li H., He C. Clinical characteristics of 3062 COVID - 19 patients : a meta - analysis. J Med Virol. 2020;(April):1–13. doi: 10.1002/jmv.25884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Abroug F., Ouanes-Besbes L., Elatrous S., Brochard L. The effect of prone positioning in acute respiratory distress syndrome or acute lung injury : a meta-analysis . Areas of uncertainty and recommendations for research. Intensive Care Med. 2008;34:1002–1011. doi: 10.1007/s00134-008-1062-3. [DOI] [PubMed] [Google Scholar]
- 4.Guérin C., Reignier J., Richard J.C. Prone positioning in severe acute respiratory distress syndrome. N Engl J Med. 2013;368:2159–2168. doi: 10.1056/NEJMoa1214103. [DOI] [PubMed] [Google Scholar]
- 5.Sud S., Friedrich J.O., Taccone P. Prone ventilation reduces mortality in patients with acute respiratory failure and severe hypoxemia : systematic review and meta-analysis. Intensive Care Med. 2010;36:585–599. doi: 10.1007/s00134-009-1748-1. [DOI] [PubMed] [Google Scholar]
- 6.Lucchini A., Bambi S., Mattiussi E. Prone position in acute respiratory distress syndrome patients: a retrospective analysis of complications. Dimens Crit Care Nurs. 2020;39:39–46. doi: 10.1097/DCC.0000000000000393. [DOI] [PubMed] [Google Scholar]
- 7.Edsberg L.E., Black J.M., Goldberg M., McNichol L., Moore L., Sieggreen M. Revised national pressure ulcer advisory panel pressure injury staging system. J Wound, Ostomy Cont Nurs. 2016;43:585–597. doi: 10.1097/WON.0000000000000281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gattinoni L.G., Tognoni G., Pesenti A. Effect of prone positioning on the survival of patients with acute respiratory failure. N Engl J Med. 2001;345:568–573. doi: 10.1056/NEJMoa010043. [DOI] [PubMed] [Google Scholar]
- 9.Sud S., Friedrich J.O., Adhikari N.K.J. Effect of prone positioning during mechanical ventilation on mortality among patients with acute respiratory distress syndrome: a systematic review and meta-analysis. Cmaj. 2014;186:381–390. doi: 10.1503/cmaj.140081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Girard R., Baboi L., Ayzac L., Richard J.C., Guérin C. The impact of patient positioning on pressure ulcers in patients with severe ARDS: results from a multicentre randomised controlled trial on prone positioning. Intensive Care Med. 2014;40:397–403. doi: 10.1007/s00134-013-3188-1. [DOI] [PubMed] [Google Scholar]
- 11.Bamford P., Denmade C., Newmarch C., et al. Guidance for : prone positioning in adult critical care. https://www.ficm.ac.uk/sites/default/files/prone_position_in_adult_critical_care_2019.pdf. Published 2019. Accessed 28 June 2020.
- 12.Bloomfield R., Dw N., Sudlow A. Prone position for acute respiratory failure in adults (Review) summary of findings for the main comparison. Cochrane Database Syst Rev. 2015:1–92. doi: 10.1002/14651858.CD008095.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Guérin C., Beuret P., Constantin J.M. A prospective international observational prevalence study on prone positioning of ARDS patients: the APRONET (ARDS prone position network) study. Intensive Care Med. 2018;44:22–37. doi: 10.1007/s00134-017-4996-5. [DOI] [PubMed] [Google Scholar]
- 14.Chiumello D., Coppola S., Froio S. Prone position in ARDS : a simple maneuver still underused. Intensive Care Med. 2018:16–18. doi: 10.1007/s00134-017-5035-2. [DOI] [PubMed] [Google Scholar]
- 15.Munshi L., Del Sorbo L., Adhikari N.K.J. Prone position for acute respiratory distress syndrome: a systematic review and meta-analysis. Ann Am Thorac Soc. 2017;14:S280–S288. doi: 10.1513/AnnalsATS.201704-343OT. [DOI] [PubMed] [Google Scholar]
- 16.Grisell M., Place H.M. Face tissue pressure in prone positioning spinal surgery. Spine (Phila Pa 1976) 2008;33:2938–2941. doi: 10.1097/BRS.0b013e31818b9029. [DOI] [PubMed] [Google Scholar]
- 17.Ling X.W., Raman S.K., Tan J.K.T., Hao Y., Saw K.M. Incidence of facial pressure ulcers following surgery in the prone position – experience in a tertiary care hospital. Sri Lankan J Anaesthesiol. 2019;27:139–144. [Google Scholar]
- 18.Nazerali R.S., Song K.R., Wong M.S. Facial pressure ulcer following prone positioning. J Plast Reconstr Aesthetic Surg. 2010;63:e413–e414. doi: 10.1016/j.bjps.2009.11.001. [DOI] [PubMed] [Google Scholar]
- 19.Keller B.P.J.A., Wille J., Ramshorst B Van, Werken C van der. Pressure ulcers in intensive care patients : a review of risks and prevention. Intensive Care Med. 2002;28:1379–1388. doi: 10.1007/s00134-002-1487-z. [DOI] [PubMed] [Google Scholar]
- 20.Cox J., Cwocn A. Predictors of pressure ulcers in adult critical care patients. Am J Crit Care. 2011;20:364–375. doi: 10.4037/ajcc2011934. [DOI] [PubMed] [Google Scholar]
- 21.Ayello E., Braden B. How and why to do pressure ulcer risk assessment. And Ski Wound Care. 2002;15:125–131. doi: 10.1097/00129334-200205000-00008. [DOI] [PubMed] [Google Scholar]
- 22.Chen H.L., Cao Y.J., Zhang W. Braden scale (ALB) for assesing pressure ulcer risk in hospital patients: a validity and reliability study. Appl Nurs Res. 2017;33:169–174. doi: 10.1016/j.apnr.2016.12.001. [DOI] [PubMed] [Google Scholar]
- 23.Depasse J.M., Palumbo M.A., Haque M. Complications associated with prone positioning in elective spinal surgery. World J f Orthop. 2015;6:351–359. doi: 10.5312/wjo.v6.i3.351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mcauley D.F., Giles S., Fichter H., Perkins G.D., Gao F. What is the optimal duration of ventilation in the prone position in acute lung injury and acute respiratory distress syndrome ? Intensive Care Med. 2002;28:414–418. doi: 10.1007/s00134-002-1248-z. [DOI] [PubMed] [Google Scholar]
- 25.Mancebo J., Fernandez R., Blanch L. A multicenter trial of prolonged prone ventilation in severe acute respiratory distress syndrome. Am J Respir Crit Care Med. 2006;173:1233–1239. doi: 10.1164/rccm.200503-353OC. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.