Abstract
Objective
To assess the impact of ongoing COVID-19 pandemic on epilepsy care in India.
Methods
We conducted a three-part survey comprising neurologists, people with epilepsy (PWE), and 11 specialized epilepsy centers across India. We sent two separate online survey questionnaires to Indian neurologists and PWE to assess the epilepsy practice, seizures control, and access to care during the COVID-19 pandemic. We collected and compared the data concerning the number of PWE cared for and epilepsy procedures performed during the 6 months periods preceding and following COVID-19 lockdown from epilepsy centers.
Results
The survey was completed by 453 neurologists and 325 PWE. One third of the neurologist reported >50 % decline in outdoor visits by PWE and EEG recordings. The cumulative data from 11 centers showed 65–70 % decline in the number of outdoor patients, video-EEG monitoring, and epilepsy surgery. Working in a hospital admitting COVID-19 patients and use of teleconsultation correlated with this decline. Half of PWE had postponed their planned outpatient visits and EEG. Less than 10 % of PWE missed their antiseizure medicines (ASM) or had seizures due to the nonavailability of ASM. Seizure control remained unchanged or improved in 92 % PWE. Half of the neurologists started using teleconsultation during the pandemic. Only 4% of PWE were afflicted with COVID-19 infection.
Conclusions
Despite significant decline in the number of PWE visiting hospitals, their seizure control and access to ASMs were not affected during the COVID-19 pandemic in India. Risk of COVID-19 infection in PWE is similar to general population.
Keywords: COVID-19 pandemic, Lockdown, Epilepsy, Teleconsultation
1. Introduction
The ongoing global Coronavirus Disease (COVID-19) pandemic, caused by a novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has affected the health care including neurologic care worldover [1,2]. In addition to the direct affection of nervous system by the SARS−COV-2, the COVID-19 pandemic may have indirect impact on patients with non−COVID-19 diseases [3]. This indirect impact mainly results from the reluctance of the patients with non−COVID diseases to seek medical care because of the fear of contacting COVID-19 infection and the reduced availability of health care resources for non−COVID diseases. The stringent lockdown in several countries has also affected the access to health care services. The situation is likely to be much worse in low- and middle-income countries (LAMIC) where health care is suboptimal even otherwise. Few available data suggest that there is a worldwide decrease in the number of patients with neurologic disorders attending emergency departments and outpatient clinics during the pandemic [[4], [5], [6], [7]]. A retrospective study from a stroke unit in the Unites States of America (USA) reported a 22–60 % decline in number of emergency admissions, acute ischemic strokes, and transient ischemic attacks [6]. Likewise, in a recent survey by the American Epilepsy Society, almost all the 339 members surveyed felt some difficulty in providing care to people with epilepsy (PWE) [8]. The major problems faced by the patients were loss of employment, lack of access to health care, and the fear related to outbreak of viral infection.
The COVID-19 pandemic and resultant lockdowns might have resulted in limited access to antiseizure medicines (ASMs) and the health care facilities for PWE, particularly in LAMIC. Many neurologists are also reluctant to undertake electroencephalogram (EEG), long-term video-EEG monitoring (LTVEM), and epilepsy surgery during the pandemic. This is likely to further delay these procedures and the resultant chance of improved seizure control in many patients. However, no study has quantitatively assessed the impact of the current COVID pandemic on epilepsy care across the world. This prompted us to undertake this study to gauge the impact of the COVID-19 pandemic on epilepsy care in India, one of the most affected LAMIC in the world, through a tripartite questionnaire-based survey among the neurologists, PWE, and specialized epilepsy centers.
2. Methods
2.1. Survey methodology
We conducted a three-part survey involving neurologists, PWE, and specialized epilepsy centers across India. As the first part, we conducted an online survey among the general neurologists and epileptologists across India. We prepared a 22-item online questionnaire. The survey questionnaire was initially prepared by the principle investigator (CR). It was circulated among the co-investigators for face validity and content validity and was modified as per the suggestions. After due modifications, we shared the survey questionnaire among the 10 neurologists for their feedback regarding the content and clarity of the questions. We modified the questionnaire as per the feedback and shared the final survey link from 26th of September 2020 onwards through emails and cell phones (Supplementary file 1). We sent the survey link to all the registered members of the Indian Academy of Neurology through emails. In addition, we also shared the link with various academic neurology groups, neurologists of all the prominent neurology institutes in the country, and professional societies of various provinces in the country through email and phones. Two reminders were sent 5 days apart with a request to complete the survey. We disabled the online survey link after 10 days on 6th October 2020.
As the second part of the survey, we communicated with 11 epilepsy centers across India to obtain the quantitative details of epilepsy care during the pandemic. In India, nationwide lockdown was announced from 23rd March 2020 onwards. Through a structured proforma, we obtained following details for a period of 6 months from 23rd March 2020 to 23rd September 2020: (1) the number of PWE attending the outdoor clinics and indoor wards; and (2) number of routine EEG, LTVEM, and the epilepsy surgeries performed. We compared this data with the data of preceding 6 months, i.e., 22nd September 2019 to 22nd March 2020. We combined the number of all the PWEs attending the clinics, whether new registrations or follow-up visits. For this study, the LTVEM was defined as VEM for more than 8 h. Patients admitted to indoor neurology wards for the primary diagnosis and management of epilepsy, other than those admitted for LTVEM, were counted for the indoor epilepsy admissions. This mainly included patients with new onset seizures, acute symptomatic seizures, breakthrough seizures, or status epilepticus.
We conducted the third part of survey among the PWE. We randomly selected 200 PWE from epilepsy registries at each of the three epilepsy centers (Vadodara, Gujarat; Nagpur, Maharashtra; and Gurugram, Haryana) from a group of patients who have attended the epilepsy clinics during the last three years. The 23-item survey questionnaire was prepared, validated, and finalized by the same methodology as described above. The questionnaire was initially translated to local languages (Gujarati and Hindi) by the professional bilingual translators. The translated questionnaires were back-translated by the independent English language speakers and they were reviewed by a team of three bilingual study investigators for conceptual equivalence and clarity. The translated questionnaire was initially administered to 20 PWE attending the outpatient clinics to check for the clarity and comprehension. Minor changes in the questionnaire were made as per the feedback and final questionnaire was prepared. The online link to the final questionnaire was sent to the patients through emails and phones (Supplementary file 2). All the PWE were explained the objective and format of the survey by a medical social worker through a phone call. The link to survey was shared only after PWE or their caregivers were willing to participate in the survey. A single reminder was sent to the patients after 5 days. The survey link was kept active for 10 days from 5th October to 15th October 2020.
2.2. Statistical analysis
We used descriptive statistics including percentages, mean, and median to summarize the survey results. Additionally, we analyzed, using Pearson’s Chi-square test, the relationship of following factors with the decline in outpatient visits, routine EEG, LTVEM procedures, and epilepsy surgery numbers as reported by the neurologists: geographical location of the practice, type of work setup (teaching institutes vs. nonteaching institutes), whether their hospitals were admitting COVID patients or not, proportion of PWE coming from outside the province of practice (<50 % vs. > 50 %), whether any staff member was affected by COVID-19 infection, and routine use of teleconsultation. For the analysis, we divided the dependent variables (numbers of outdoor and indoor patients and procedures) as ≥50 % and <50 % decline in numbers. We defined the 6 Indian provinces with highest case numbers (Maharashtra, Tamil Nadu, Andhra Pradesh, Delhi, Uttar Pradesh, and Karnataka) as provinces with high patient load and compared data from these provinces to the rest of the provinces [9]. Subsequently, we undertook multivariate logistic regression analysis with forward stepwise (likelihood ratio) method. Those factors found to be significant on univariate analysis (p ≤ 0.05) were further entered into logistic regression models with probability for entry of the variables fixed as 0.05 and for removal 0.10. Similarly, we studied the demographic and epilepsy related factors associated with patients missing their hospital visits or worried about their seizure control using binary logistic regression analysis. We performed the analysis using IBM SPSS Statistics for Windows, Version 27.0. A p value of <0.05 was considered significant.
2.3. Standard procedures
The study was approved by the institutional ethics committees for human subjects of four major participating centers (Vadodara, Nagpur, Gurugram, and Hyderabad). A general informed consent was included at the beginning of both the online questionnaires stating that attempting and submitting the survey meant that the person has given the consent for participation. To preserve confidentiality, the survey forms did not contain any identifying information of the individuals and no physical signatures were collected from any of the participants. As it is not a clinical trial, the study was not registered with any trial registry.
3. Results
3.1. Survey 1: neurologists
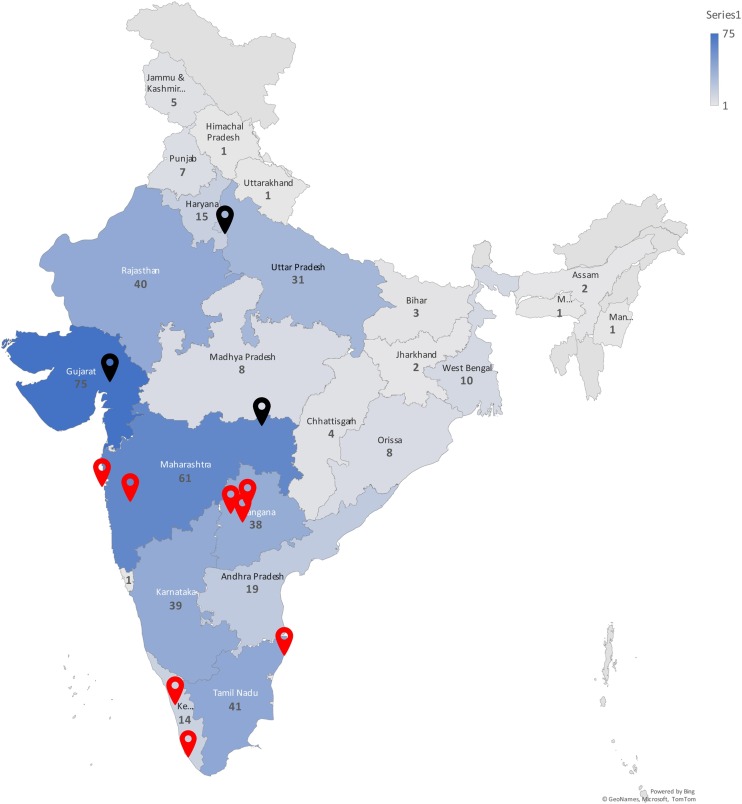
The first survey was completed by 453 neurologists. There are 1818 life members of Indian Academy of Neurology. Of these, approximately 150 members are not active presently. Additionally, with increasing sub-specialization within neurology, many neurologists do not attend to patients outside their field of specialization. Thus the survey covered ∼ 30 % of the Indian neurologists. The demographic details of the participating neurologists and their responses are provided in Table 1 . Of the 36 provinces and union territories in India, there are no neurologists in nine of them. Barring these 9 regions, the survey was completed by at least two neurologists from each of the 27 regions (range, 2–75; Fig. 1 ). The survey included equal number of respondents from academic and non-academic medical institutions (35 % each) as well as from solo practice (30 %). Similarly, the neurologists with different levels of experience were equally represented in the survey suggesting a wholesome representation of the neurology practice in India. More than two-thirds of the respondents manage 10 or more PWE in a week.
Table 1.
The attributes of neurologists who completed the survey and distribution of their responses (n = 453).
| Attributes and responses | n (%) | 95% CI of proportions (%) |
|---|---|---|
| Specialization | ||
|
362 (79.8) | 75.9-83.3 |
|
55 (12.1) | 9.0-15.0 |
|
29 (6.4) | 4.4-9.0 |
|
8 (1.8) | 0.8-3.5 |
| Work setup | ||
|
158 (34.8) | 30.6-39.3 |
|
160 (35.2) | 31.0-39.8 |
|
136 (30) | 25.9-34.4 |
| Years of experience | ||
|
153 (33.7) | 29.5-38.2 |
|
145 (31.9) | 27.8-36.4 |
|
156 (34.4) | 30.2-38.9 |
| Number of epilepsy patients seen in a week before pandemic | ||
|
34 (7.5) | 5.3 -10.3 |
|
108 (23.8) | 20.1-27.9 |
|
150 (33) | 28.9 -37.6 |
|
162 (35.7) | 31.4-40.3 |
| COVID-19 patients being admitted in their hospital | 322 (70.9) | 66.7-75.1 |
| Department member tested positive for COVID-19 | 235 (51.8) | 47.3-56.4 |
| Comfortable in offering antiseizure medicine withdrawal | 212 (46.7) | 42.3-51.4 |
| Patients willing for antiseizure medicine withdrawal | ||
|
200 (44.1) | 39.7-48.8 |
|
178 (39.2) | 34.9-43.9 |
|
76 (16.7) | 13.6-20.5 |
| COVID testing mandatory before video-EEG monitoring (n=222) | 163 (72) | 31.7-40.5 |
| Approximate number of patients who had breakthrough seizures due to difficulty in accessing medical care | ||
|
240 (52.9) | 48.4-57.5 |
|
152 (33.5) | 29.4-38.1 |
|
62 (13.6) | 10.8-17.1 |
| Any patient had life threatening seizures due to difficulty in accessing medical care | 129 (28.4) | 24.5-32.8 |
| Use of teleconsultation since the onset of COVID pandemic | ||
|
205 (45.2) | 40.7-49.9 |
|
172 (37.9) | 33.6-42.5 |
|
77 (17) | 13.8-20.7 |
| Patients demanding teleconsultation during pandemic | 363 (80) | 76.2-83.6 |
| Impact of COVID pandemic on your practice of epileptology | ||
|
304 (67) | 62.7-71.3 |
|
136 (30) | 25.9-34.4 |
|
14 (3) | 1.8-5.1 |
CI – confidence interval.
Fig. 1.
Map of India depicting the geographic distribution of survey centers and respondents. Numbers within the boundaries of each province represent the number of respondents from that province. Black map pins show the three centers where the patient surveys were conducted and red map pins represent the rest of the participating centers (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article).
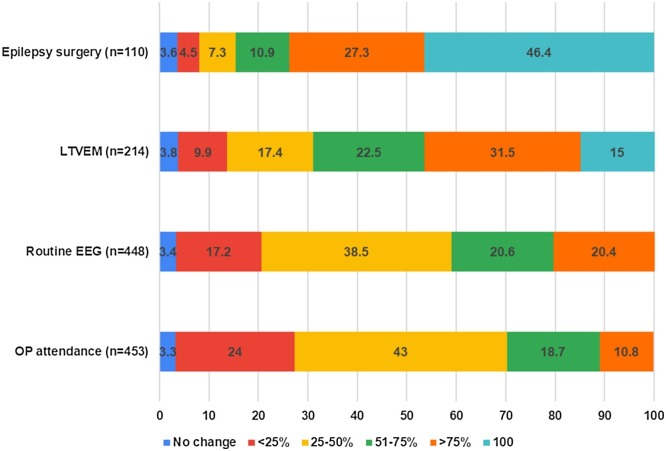
Taken as a whole, majority of the respondents reported 25–75 % decline in the number of PWE visiting outpatient epilepsy clinics and the number of routine EEG (Fig. 2). Only 20 % of the respondents reported either no change or a decline of less than 25 %. The decline in numbers of LTVEM and epilepsy surgery was more pronounced. More than 70 % of respondents reported 50 % or greater decline in number of LTVEM while approximately half of the respondents had stopped epilepsy surgery during this period. Two-thirds of the respondents felt that the pandemic has significantly impacted their practice of epilepsy. Approximately half of the neurologists felt uncomfortable in offering ASM withdrawal. Approximately half of the neurologists reported to have started using teleconsultation regularly. Approximately 28 % of the neurologists reported that at least one of their patients had seizures due to the non-availability of ASM or due to the difficulty in accessing medical care during the pandemic. The major reasons alluded to by the neurologists for the decline in the number of LTVEM and epilepsy surgery were unwillingness of the patients (n = 64) and amendment in hospitalization practices because of the pandemic (n = 65). Additionally, a small proportion of the respondents reported that they were not admitting PWE (n = 30) while 10 respondents reported various logistics reasons including lack of connectivity. Mandatory COVID testing before admitting the patient for LTVEM was reported by 70 % of the neurologists.
Fig. 2.
Proportion of neurologists reporting decline in patient numbers and various procedures during the 6-month period following COVID lockdown in India. [OP - Outdoor patient attendance; LTVEM - Long-term video-EEG monitoring].
3.2. Factors associated with decline in epilepsy practice
We compared the attributes of the neurologists reporting ≥ 50 % decline in the various practice parameters to those reporting less than 50 % decline (Table 2 ; Supplementary Table 1). On univariate analysis, working in a hospital recognized for COVID-19 care (p < 0.0001), working in a teaching hospital (p < 0.001), and the routine use of teleconsultation (p < 0.0001) were associated with decline in number of outdoor patients, routine EEG, and epilepsy surgery (Supplementary table-1). Factors such as working in a province with high case load, attending greater number of patients from other provinces, years of experience, and any staff member being affected with COVID-19 infection had no correlation with the decline in the number of patients and EEG. For the reason of brevity, we have only presented the analysis related to the outdoor patients. The factors found to be significant on univariate analysis were further entered into 2 step logistic regression models as described in the methods. On logistic regression analysis, working in a hospital recognized for COVID-19 care and the routine use of teleconsultation were significantly associated with the decline in number of outdoor patients. In the first model, hospital admitting COVID patients alone was included with 71 % variance (p ≤ 0.0001; crude odds ratio 5.46). In the second model we included both the factors and it showed the same variance of 71 % (p = 0.002). The results along with the adjusted odds ratio are presented in Table 2.
Table 2.
Factors associated with decline in outdoor patient numbers on multivariate analysis.
| Factor | Regression coefficient | SE of regression coefficient | Wald statistics | Degrees of freedom | P Value | Adjusted odds ratio (95 % confidence interval) |
|---|---|---|---|---|---|---|
| Hospital admitting COVID patients | 1.569 | .318 | 24.368 | 1 | .0001 | 4.80 (2.56–8.95) |
| Routine use of teleconsultation | .672 | .219 | 9.410 | 1 | .002 | 1·96 (1·28 – 3.1) |
| Constant | −3.119 | .426 | 53.717 | 1 | .0001 | 0·044 |
3.3. Survey 2: epilepsy centers
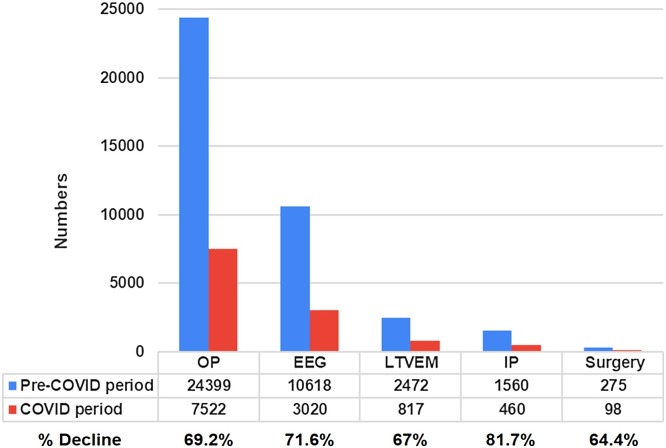
We have depicted the results of the second part of the survey in Fig. 3 . Altogether, 11 epilepsy centers had evaluated more than 24,000 patients and performed 10,618 EEG in the 6 months preceding the COVID lockdown in India. There was 65–70 % decline in the number of outdoor patients, routine EEG, LTVEM, and epilepsy surgery during the 6-month COVID period while the number of hospitalized PWE declined by 80 %.
Fig. 3.
Comparison of cumulative data from 11 participating centers during 6-month periods preceding the COVID pandemic and during the COVID pandemic.[OP - outdoor patient attendance; EEG – routine EEG; LTVEM - long-term Video-EEG monitoring; IPD - indoor epilepsy patients; Surgery – epilepsy surgery].
3.4. Survey 3: people with epilepsy
The survey was sent to 600 PWE across three centers and was completed by 325 (54 %) patients. The demographic details and responses of the patients are provided in Table 3 . Majority of the respondents were males, were living in the cities, and had long-standing epilepsy. Of the 325 PWE, 40 % had difficulty in their regular visits to the treating physicians and 50 % had postponed their planned visits. However, less than 10 % of the PWE missed their ASM or had seizures either due to the nonavailability of ASM or difficulty in procuring ASM. Likewise, only 15 % of PWE reported being apprehensive about missing ASM or hospital visits due to the lockdown. Seizure control either remained same or improved in the majority of the PWE. Half of the PWE reported that they were worried about their epilepsy control during the pandemic. However, only one fourth of PWE reported that the pandemic had affected their life significantly. Majority of the PWE expressed their desire to contact their treating neurologist through teleconsultation. The major reasons reported by the PWE for not visiting the treating physicians included the availability of teleconsultation (30 %), fear of being exposed to COVID-19 infection (29 %), and lockdown restrictions (26 %). Only 10 % of PWE were apprehensive of higher risk of COVID infection because of their epilepsy. Of the 325 respondents, 4% of the PWE reported that they had COVID-19 infection during the last 6 months.
Table 3.
Attributes of patients who responded to the survey (n = 325) and distribution of their responses.
| Mean age (years ± SD); Range |
26.4 ± 12.3 (1-70) |
|
|---|---|---|
| Attributes and responses | n (%) | 95% CI of proportions (%) |
| Male | 193 (59) | 53.9-64.6 |
| Residence | ||
|
231 (75) | 66.0-75.8 |
|
28 (9) | 5.9-12.2 |
|
48 (16) | 11.3-19.1 |
| Epilepsy duration | ||
|
61 (18.8) | 14.9-23.4 |
|
50 (15.4) | 11.9-19.7 |
|
59 (18.2) | 14.3-22.7 |
|
155 (47.7) | 42.3-53.1 |
| Number of seizures in last one year | ||
|
139 (42.8) | 37.5-48.2 |
|
73 (22.5) | 18.2-27.3 |
|
24 (7.4) | 4.9-10.8 |
|
25 (7.7) | 5.2-11.2 |
|
64 (19.7) | 15.7-24.8 |
| Number of current antiseizure medicines | ||
|
78 (24) | 19.7-28.9 |
|
102 (31.4) | 26.6-36.6 |
|
85 (26.2) | 21.7-31.2 |
|
60 (18.5) | 14.6-23.1 |
| Seizure control during last 6 months | ||
|
138 (42.5) | 37.2-47.9 |
|
162 (49.8) | 44.4-55.2 |
|
25 (7.7) | 5.2-11.1 |
| Missed medicines due to unavailability | 22 (6.8) | 4.4-10.1 |
| Had seizures due to unavailability of medicines | 37 (11.4) | 8.3-15.3 |
| Had difficulty in procuring medicines | 33 (10.2) | 7.3-13.9 |
| Missed regular visit to treating physician | 139 (42.8) | 37.5-48.2 |
| Postponed planned visit to treating physician (n=254) | 124 (49) | 42.7-54.9 |
| Postponed planned EEG or Video-EEG test (n=175) | 51 (29.1) | 22.9-36.3 |
| Postponed planned surgery (n=123) | 20 (16.3) | 10.7-23.9 |
| Had corona infection | 13 (4) | 2.3-6.8 |
| Family member had corona infection | 26 (8) | 5.5-11.5 |
| More worried about your epilepsy control during corona pandemic | 107 (32.9) | 28.1-38.2 |
| Impact of COVID pandemic on life | ||
|
55 (16.9) | 13.2-21.4 |
|
156 (48) | 42.6-53.4 |
|
114 (35.1) | 30.1-40.4 |
| Would like telephonic consultations with treating physician | 268 (82.5) | 77.9-86.2 |
CI – confidence interval.
On reviewing the responses, we noted that 61 (19 %) of the responses were provided by the caregivers rather than the patients. This was noted with young children (n = 48) or patients with cognitive problems (n = 13). The number of responders reporting that that they were worried about the seizure control during the pandemic was similar whether it was reported by the patient or the caregiver (37 % vs. 35 %; p = 0.44). Similarly, there was no difference in the numbers reporting that pandemic had affected their life significantly (17 % vs. 16 %; p = 0.52).
We compared the demographic and epilepsy related characteristics of PWE who missed their hospital visits (vs. who did not miss) or those who were worried about their seizure control (vs. who were not worried) during the pandemic using simple binary logistic regression analysis. None of the demographic (age, gender, and residence) or epilepsy related factors (duration of epilepsy, seizure frequency, and the use of teleconsultation) were associated with missing the hospital visits. Patients with more than 2 seizures per year (odds ratio: 3.87, 95 % CI = 2.37–6.34; p ≤ 0.0001) and those with worsening in their seizure control (odds ratio: 9.79, 95 % CI = 3.56–26.92; p ≤ 0.0001) were significantly more worried during the pandemic. These variables were analyzed for model creation and the results are illustrated in supplementary Table 2. The goodness of fit tested by Hosmer and Lemeshow test showed (p = 0.76, χ2 = 0.068) 72 % predictable variance in the 2 step model.
4. Discussion
Our tripartite survey showed that COVID-19 pandemic and subsequent lockdown has significantly impacted the epilepsy practice in India with a major decline in the number of PWE visiting hospitals or undergoing evaluation for epilepsy and epilepsy surgery. However, the pandemic had only a minor effect on the epilepsy control with more than 90 % of the PWE reporting neither difficultly in procuring ASM nor increased seizures due to the nonavailability of ASM. Inclusion of all the major stake holders of epilepsy care, including PWE, and the use of quantitative data from major epilepsy centers in India are the main strengths of the study. Inclusion of neurologists representing all the regions of India with various levels of experience and work setup, and PWE from different regions and backgrounds makes it an archetypical survey of epilepsy practice in India. Only few other studies have evaluated the impact of COVID pandemic on the epilepsy practice. [8,9] Ours is the one of the first comprehensive study from the most affected LAMIC in the world to include inputs from neurologists, PWE, and comprehensive epilepsy care centers.
India is the second most severely affected country with 7.3 million confirmed COVID-19 cases by 15th October 2020 [10]. India has witnessed one of the most stringent and longest lockdowns during the pandemic starting from 23rd March 2020, and continuing till date [11]. There were major restrictions in movement of people including public and private transport. Majority of the hospitals, including major government hospitals, had stopped routine outpatient clinics during the initial two months [12]. This resulted in a universal decline in the number of non−COVID patients attending outpatient clinics and undergoing elective procedures. Many of the hospitals were entirely converted into COVID care hospitals. This is also being reflected in our survey which showed a major decline in the number of PWE attending hospitals and undergoing elective procedures such as LTVEM and epilepsy surgery. India already has a huge surgical treatment gap of epilepsy and waiting lists for LTVEM and epilepsy surgery is almost 1−2 years at the major epilepsy centers [13]. The pandemic has further lengthened the waiting and has delayed the chance of seizure freedom and improved quality of life in many patients.
With a suboptimal health system and the strict lockdown, it was dreaded that epilepsy patients in India and many LAMIC will face enormous difficulties. However, our results show that only a minority of the PWE had difficulty in procuring ASMs or had seizure exacerbation due to the difficulty in accessing medical care. Majority of the PWE did not report any apprehensions related to difficulty in procuring ASM or visiting hospitals. The seizure control worsened only in a minority of the patients. In a similar questionnaire based survey involving 132 PWE from north India, only 12 % of patients reported difficulty in procuring ASMs during the pandemic which is similar to our results [9]. There may be several reasons for PWE not facing major difficulty during the lockdown period. Firstly, even during the strictest period of lockdown, medical stores and pharmacies were not closed. In India, PWE usually have the option of procuring prescriptions from their family physicians. Many of the patients on regular ASM, especially in small towns and villages, can procure medicines from local pharmacists without the need for a new prescription and the regulations are not strictly enforced. Secondly, one-third of PWE also procured prescriptions through teleconsultations. Teleconsultation regulations were modified during the lockdown period and patients could procure ASMs through teleconsultations [14]. These factors have probably allowed PWE to continue same doses of ASMs without affecting their seizure control. As expected, patients with uncontrolled epilepsy and those with worsening of seizure control during the pandemic were more worried during the corona pandemic.
One of the important findings of present study is the low prevalence of COVID-19 infection in PWE. Our survey results showed that 4% of PWE were affected with COVID-19 infection in last 6 months. The prevalence of 4% is lower than the sero-prevalence of 7.1 % in the general Indian population which has been recently reported by the Indian Council of Medical Research based on a national sero-surveillance study of COVID-19 infection [15]. People with epilepsy are generally not considered at a higher risk of COVID-19 infection [16]. However, there has been very little evidence supporting this notion. A previous study involving telephonic survey of 255 PWE reported COVID-19 infection in 2% of them [17]. This along with the present study support the notion that PWE do not have increased risk of having COVID-19 infection.
The hospitals admitting COVID patients saw a decline in outpatient visits, hospitalizations, and planned epilepsy procedures. During the initial part of the pandemic, the majority of the COVID patients were admitted in governmental and non-governmental academic medical institutions which resulted in decline in the number of non−COVID patients. Hospitals situated in the provinces with high patient load or hospitals catering to patients from distant places did not report more decline in the number of PWE attending hospitals suggesting that logistic factors such as travel restrictions were only minor deterrents for patients to seek medical care. This is further corroborated by the reasons cited by the neurologists and PWE for the decline in hospital visits.
Overall, the majority of the PWE had positive altitude about their epilepsy during the pandemic. Approximately two-thirds of them did not have any apprehension of seizure control or difficulty in consulting the doctor or procuring medicines during the pandemic. These results are more or less similar to the survey from north India in which majority of the patients did not report any difficulty in accessing medical care [9]. The majority of the PWE also felt that COVID pandemic has not affected their life significantly.
One of the factors which we encountered in practice and subsequently studied through this survey is the willingness of the neurologists and PWE to undertake ASM withdrawal, if indicated. There is always an apprehension of seizures on drug withdrawal and subsequent difficulty in accessing medical care especially during the pandemic. Approximately half of the neurologists and PWE were apprehensive of drug withdrawal. This is an additional aspect of epilepsy care which has been affected during the COVID pandemic.
The other positive aspect which has emerged during the pandemic is the use of telemedicine [18,19]. Teleconsultation was almost nonexistent in India prior to this pandemic. Almost all the major hospitals and individual neurologists have started the facility of teleconsultation within initial two months of pandemic. Approximately half of the neurologists who participated in the survey reported that they were routinely using teleconsultation. The use of teleconsultation was associated with decline in PWE attending hospitals which appears to have a bidirectional relationship. Three-fourths of the patients also reported readiness for teleconsultation. With Indian population being one of the largest users of mobile phones, this experience can be used to take epilepsy care to the remotest corners of the country and thus improving the primary and secondary treatment gaps in India and the other LAMIC [20,21].
Our study has certain limitations. It is a survey based study and represents the views and experiences of people who responded to the survey. There are few or no neurologists in certain provinces of India and hence these regions are underrepresented in the survey. Secondly, the patients not well versed with the technology might not have responded to the internet or mobile based survey. It is also possible that only those patients under regular follow-up or good seizure outcome might have responded. However, 57 % of the patients were not seizure free during the previous one year and two-third of the patients were receiving more than one ASM. Additionally, one-fourth of the PWE surveyed had drug-resistant epilepsy and were receiving more than three ASMs suggesting that seizure control was not the criteria for responding to the survey. In addition, majority of the respondents were from large cities and there was an under-representation of patients from small town and villages. Patients living in rural areas might have faced more difficulties in procuring ASMs and accessing medical care. Although our analysis did not show such association, we cannot rule out this possibility because of small number of rural patients in the survey. All these factors limit the generalizability of the results. Finally, we did a cross sectional survey during a single time point while the pandemic and its perception among the physicians and the patients could have changed significantly over the last 6 months. The number of PWE attending the hospitals and undergoing EEG and LTVEM has increased steadily over the last two months of pandemic. In spite of these limitations, our survey provides useful information about the effects of COVID pandemic on epilepsy care and patient perception in a developing region of the world, which can be utilized to improve epilepsy care not only in LAMIC but also in developed countries.
5. Conclusions
This tripartite survey involving neurologists, PWE, and specialized epilepsy centers showed that epilepsy care has been significantly affected during the ongoing COVID-19 pandemic in India. There has been significant decline in the number of patients visiting outdoor clinics and undergoing EEG, LTVEM, and epilepsy surgery. This is likely to further worsen the already existing medical and surgical treatment gap in developing countries. However, seizure control and access to ASMS remained largely unaffected during the COVID-19 pandemic. Our results also show that the risk of COVID-19 infection in PWE is similar to general population.
Declaration of Competing Interest
None of the authors have any conflict of interest related to this work.
Acknowledgments
We are grateful to all the neurologists of India and the patients who participated in the survey.
References
- 1.Coronavirus Disease (COVID-19) - events as they happen. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen(Accessed October 30, 2020).
- 2.Dong E., Du H., Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect Dis. 2020;20:533–534. doi: 10.1016/S1473-3099(20)30120-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ellul M.A., Benjamin L., Singh B., et al. Neurological associations of COVID-19. Lancet Neurol. 2020;19:767–783. doi: 10.1016/S1474-4422(20)30221-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kennedy K. Cleveland clinic says ER visits for heart attack and stroke patients are down 40% because of COVID-19 fears. https://www.cleveland19.com. https://www.cleveland19.com/2020/04/17/cleveland-clinic-says-ervisits-heart-attack-stroke-patients-are-down-becausecovid-fears (Accessed October 30, 2020).
- 5.Morelli N., Rota E., Terracciano C., et al. The baffling case of ischemic stroke disappearance from the casualty department in the COVID-19 era. EurNeurol. 2020;83:213–215. doi: 10.1159/000507666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Desai S.M., Guyette F.X., Martin-Gill C., Jadhav A.P. Collateral damage - Impact of a pandemic on stroke emergency services. J Stroke Cerebrovasc Dis. 2020;29 doi: 10.1016/j.jstrokecerebrovasdis.2020.104988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Boukhris M., Hillani A., Moroni F., et al. Cardiovascular implications of the COVID-19 pandemic: a global perspective. Can J Cardiol. 2020;36:1068–1080. doi: 10.1016/j.cjca.2020.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Albert D.V.F., Das R.R., Acharya J.N., et al. The impact of COVID-19 on epilepsy care: a survey of the american epilepsy society membership. Epilepsy Curr. 2020;20:316–324. doi: 10.1177/1535759720956994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sureka R.K., Gaur V., Gupta M. Impact of COVID-19 on people suffering with epilepsy. Ann Indian Acad Neurol. 2020 doi: 10.4103/aian.AIAN_623_20. (Ahead of print) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.COVID-19 Worldwide Dashboard - WHO Live World Statistics. https://www.covid19.who.int(Accessed October 16, 2020).
- 11.The Lancet India under COVID-19 lockdown. Lancet. 2020;395(10233):1315. doi: 10.1016/S0140-6736(20)30938-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sharma D.C. Lockdown poses new challenges for cancer care in India. Lancet Oncol. 2020;21:884. doi: 10.1016/S1470-2045(20)30312-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rathore C., Radhakrishnan K. Epidemiology of epilepsy surgery in India. Neurol India. 2017;65(Supplement):S52–S59. doi: 10.4103/neuroindia.NI_924_16. [DOI] [PubMed] [Google Scholar]
- 14.Board of Governors. Telemedicine Practice Guidelines Enabling Registered Medical Practitioners to Provide Healthcare Using Telemedicine. Available from: https://www.mohfw.gov.in/pdf/Telemedicine.pdf. Released on 25th March 2020 (Accessed October 30, 2020).
- 15.Koshy J. Coronavirus | 60 million Indians may have been exposed to COVID-19: ICMR sero-survey. https://www.thehindu.com/sci-tech/health/one-in-15-people-aged-10-and-above-estimated-to-be-exposed-to-sars-cov2-by-august-icmr-sero-survey/article32724417.ece (Accessed on 19th September, 2020).
- 16.French J.A., Brodie M.J., Caraballo R., et al. Keeping people with epilepsy safe during the COVID-19 pandemic. Neurology. 2020;94:1032–1037. doi: 10.1212/WNL.0000000000009632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fonseca E., Quintana M., Lallana S., et al. Epilepsy in time of COVID-19: a survey-based study. Acta Neurol Scand. 2020;16(August) doi: 10.1111/ane.13335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ghosh A., Gupta R., Misra A. Telemedicine for diabetes care in India during COVID19 pandemic and national lockdown period: guidelines for physicians. Diabetes MetabSyndr. 2020;14:273–276. doi: 10.1016/j.dsx.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Agarwal N., Jain P., Pathak R., Gupta R. Telemedicine in India: a tool for transforming health care in the era of COVID-19 pandemic. J Educ Health Promot. 2020;9:190. doi: 10.4103/jehp.jehp_472_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hatcher-Martin J.M., Adams J.L., Anderson E.R., et al. Telemedicine in neurology: Telemedicine Work Group of the American Academy of Neurology Update. Neurology. 2020;94:30–38. doi: 10.1212/WNL.0000000000008708. [DOI] [PubMed] [Google Scholar]
- 21.Rametta S.C., Fridinger S.E., Gonzalez A.K., et al. Analyzing 2,589 child neurology telehealth encounters necessitated by the COVID-19 pandemic. Neurology. 2020;95:e1257–e1266. doi: 10.1212/WNL.0000000000010010. [DOI] [PMC free article] [PubMed] [Google Scholar]