Abstract
Background
Pregnancy is a period of elevated risk for mental health difficulties, which are likely exacerbated by the COVID-19 pandemic. This study aims to understand the impact of COVID-19 on mental health and identify risk and protective factors during pregnancy.
Methods
Participants were 303 pregnant individuals from Ontario, Canada. Depression, anxiety and insomnia were measured using validated questionnaires. COVID-related experiences (i.e., financial difficulties, relationship conflict, social isolation) were assessed in relation to mental health. Social support and cognitive appraisal of the pandemic were examined as protective factors.
Results
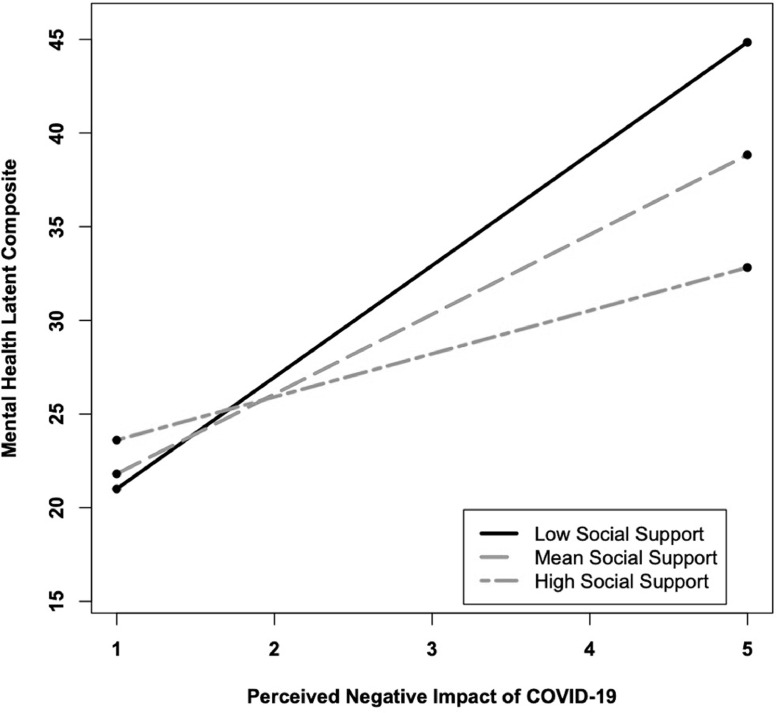
57% of the sample reported clinically elevated depression, >30% reported elevated worries, and 19% reported elevated insomnia. Depression (t = 25.14, p < .0001) and anxiety (t = 17.21, p < .0001) levels were higher than non-COVID pregnant samples. Social isolation, financial trouble, relationship difficulties and threat of COVID-19 were associated with mental health. Social support (rrange −.24 to −.38, p <.01) was associated with lower mental health problems and negative cognitive appraisal (rrange .20 to .33, p <.01) was linked to more mental health problems. Furthermore, social support and cognitive appraisal interacted (β = -.92, SE = .41, p < .05), such that higher social support acted as a protective factor, particularly for those who appraise the impact of COVID-19 to be more negative.
Conclusions
Findings underscore the need to address the high rates of mental health during pregnancy and outline potential targets (cognitive appraisal and social support) to protect pregnant people from experiencing mental health problems during the COVID-19 pandemic.
Keywords: Pregnancy, Coronavirus; COVID-19; Mental health; Social support; Cognitive appraisal
1. Introduction
Since December 2019, the emergence of the novel coronavirus (COVID-19) has resulted in a devastating global health crisis. Secondary to the morbidity and mortality associated with this viral infection, the social and physical distancing measures (including the termination of non-essential services and school closures), which have been implemented to slow the spread of COVID-19, have resulted in unprecedented disruptions to normal routines, social connections, education, and employment. Although the psychological impact of this pandemic is not yet fully understood, the consequences are anticipated to be harmful. Pregnancy is a critical period of elevated risk for mental health difficulties (Field, 2011; Rees et al., 2019). Therefore, there is an urgent need to understand how the COVID-19 pandemic impacts pregnant individuals, in order to prevent the emergence of secondary health outcomes for them and their unborn children.
Although research on the COVID-19 pandemic is in its infancy, prior work has examined the impact of epidemics on psychological outcomes (Brooks et al., 2020 for a review). For instance, research on the SARS epidemic in Toronto and Hong Kong indicates that individuals who were quarantined reported a high prevalence of psychological distress and disorder, including depression (Hawryluck et al., 2004), insomnia(Lee et al., 2005), and stress (DiGiovanni et al., 2004). Prolonged periods of quarantine were associated with more severe psychological distress (Hawryluck et al., 2004). Similarly, research conducted during the immediate aftermath of the COVID-19 outbreak, in China, Italy, Greece, and the UK, indicates that the general population experienced elevated depression, anxiety, and insomnia symptoms (Huang and Zhao, 2020; Moccia et al., 2020; Qiu et al., 2020; Rettie & Daniels, 2020; Voitsidis et al., 2020; Wang et al., 2020).
Preliminary COVID-19 research also suggests that pregnant people are experiencing elevated rates of anxiety and depression. In the immediate aftermath of the pandemic (January to February), 26-29% of a sample of pregnant women in China endorsed elevated rates of depression (Wu et al., 2020). In addition, during the initial COVID-19 lockdown in Belgium, 25.3% and 13.6% of pregnant women endorsed clinically elevated levels of depression and anxiety, respectively (Ceulemans et al., 2020). A Canadian study conducted in April 2020 revealed that 37% and 57% of pregnant individuals endorsed clinically elevated symptoms of depression and anxiety, respectively (Lebel et al., 2020). Furthermore, a study of perinatal women in the United States, conducted between May and August, found that 36% endorsed high levels of depression and 23% reported generalized anxiety (Liu et al., 2020). This indicates that pregnant women are experiencing elevated depression and anxiety symptoms in the immediate aftermath and after the initial phase of the pandemic.
Although there is currently no available data indicating whether COVID-19 exacerbates sleep difficulties in pregnant individuals, evidence suggests higher rates of insomnia, particularly in women, in the general population during COVID-19 (Voitsidis et al., 2020). Further, pregnant women are prone to experience sleep difficulties (Mindell et al., 2015) and sleep problems during pregnancy are closely tied to depression and anxiety (Swanson et al., 2011). Therefore, sleep should be considered, in conjunction with anxiety and depression, when examining the impact of COVID-19 on pregnancy. Furthermore, given that the COVID-19 pandemic potentially impacts numerous aspects of life (e.g., economic, social, physical), it is important to identify which COVID-19 experiences exacerbate these mental health difficulties.
From an intervention perspective, it is also vital to identify factors that modulate the mental health outcomes resulting from this pandemic. Lazarus’ appraisal theory suggests that an individual's cognitive appraisal of a stressful event can impact their emotional and behavioural response (Lazarus and Stress, 1984; Lazarus, 1991). Indeed, negative appraisal of traumatic events and epidemics exacerbate mental health outcomes (Cheng et al., 2004; Kucharska, 2017; Ng et al., 2006). In particular, cognitive appraisal (i.e., perceived negative impact) of natural disasters, rather than objective exposure, uniquely impacts pregnancy and child outcomes (Cao-Lei et al., 2015; Moss et al., 2017; Simcock et al., 2017). Thus, in addition to specific COVID experiences (e.g., financial difficulties, social isolation), it is important to assess whether an individual's subjective appraisal of the pandemic is associated with their mental health.
Furthermore, social support acts as a protective factor against the adverse mental health difficulties resulting from epidemics and natural disasters (e.g., Bonanno et al., 2008; King et al., 2012). Preliminary evidence demonstrates that social support is directly related to lower mental health symptoms, in non-pregnant individuals, during the COVID-19 pandemic (Cao et al., 2020; Lebel et al., 2020, Xiao et al., 2020). There is also evidence that social support moderates the impact of cognitive appraisal, attitudes and perceived stress on wellbeing (Abshire et al., 2018; Demirtas et al., 2015; Elliott et al., 1992; Liu, 2002). Therefore, cognitive appraisal and social support are two factors that independently, or combined, have the potential to influence the mental health of pregnant individuals during the COVID-19 pandemic.
1.1. The current study
The present study has three primary objectives. (1) To describe the prevalence of mental health difficulties (i.e., depression, anxiety, and insomnia) experienced by pregnant individuals during the COVID-19 pandemic. (2) To determine which COVID-19 related experiences (i.e., social isolation, economic hardship, and/or relationship difficulties) impact mental health symptoms. (3) To evaluate whether cognitive appraisal of COVID-19 and social support act as independent or interactive protective factors, to buffer against adverse mental health outcomes.
2. Methods
2.1. Participants
Participants were 303 pregnant individuals who completed the COVID-19 and Wellbeing During Pregnancy Study. Online surveys were completed between June 3 and July 31, 2020. Pregnant individuals were recruited through social media (Facebook and Instagram) advertisements, pamphlets distributed to midwifery groups, and word of mouth. As such, this work is based on an opportunistic sample. Inclusion criteria were that individuals must (1) live in Ontario, Canada, (2) read and write in English, (3) be 18 years of age or older, and (4) be ≤ 36 weeks gestation. This study was approved by the Hamilton Integrated Research Ethics Board under Project #11034.
2.2. Measures
2.2.1. COVID-19 Experiences
Participants completed a questionnaire about their experiences during the pandemic. This questionnaire was developed by one of the co-authors (L.A.) for studies completed by our research group. Questions were largely based on prior work on the impact of natural disasters on families (e.g., King et al., 2012). Specifically, participants were asked yes/no questions about COVID-19 diagnoses, infections, and quarantine. Participants were also asked, on a scale of 1 (Not at all) to 7 (A lot), how much they have experienced social isolation, relationship difficulties, financial changes, and risk of COVID-19 infection (see Table 1 for specific items).
Table 1.
Descriptive statistics.
| Measure | M (SD) | Range | Cronbach's Alpha |
|---|---|---|---|
| COVID-19 Experiences | |||
| Social Isolation | |||
| I have contact with fewer people in general than I used to because of COVID-19. | 6.34 (1.20) | 1-7 | – |
| Risk of COVID-19 Infection | |||
| Someone close to me is in danger of catching COVID-19. | 4.11(1.76) | 1-7 | – |
| Financial Difficulties | .81 | ||
| I lost income due to COVID-19. | 2.83 (2.34) | 1-7 | |
| My partner lost income due to COVID-19. | 2.41 (2.00) | 1-7 | |
| My job security is vulnerable because of COVID-19. | 2.54 (2.05) | 1-7 | |
| My partner's job security is vulnerable because of COVID-19. | 2.57 (1.93) | 1-7 | |
| I have difficulty paying my rent or mortgage because of COVID-19. | 1.77 (1.35) | 1-7 | |
| Loss of income affects the kind of groceries I buy. | 2.29 (1.84) | 1-7 | |
| Relationship Difficulties | .75 | ||
| My partner and I argue more because of COVID-19 restrictions. | 2.40 (1.56) | 1-7 | |
| My partner and I disagree about how to deal with COVID-19. | 2.06 (1.40) | 1-7 | |
| Mental Health | |||
| Cambridge Worry Scale (CWS) | 30.05 (15.31) | 1-71 | .88 |
| Center for Epidemiologic Studies Depression Scale (CES-D) | 11.50 (6.36) | 0-26 | .87 |
| Insomnia Severity Index (ISI) | 9.67 (5.67) | 0-28 | .88 |
| Cognitive Appraisal | |||
| Taking everything about COVID-19 into account, the effects of COVID-19 on me and my household have been _____ | 3.71 (0.72) | 2-5 | – |
| Social Support | |||
| Multidimensional Scale of Perceived Social Support (MSPSS) | 5.60 (1.20) | 1-7 | .95 |
2.2.2. Mental Health Questionnaires
Participants completed questionnaires to assess symptoms of anxiety, depression, and insomnia.
Cambridge Worry Scale (CWS). Participants completed the 16-item CWS (Statham et al., 1997) to assess anxiety. The CWS assesses pregnancy-specific anxiety (e.g., something being wrong with the baby, possibility of miscarriage, giving birth), as well as general anxiety (e.g., health, money problems, relationship with their partner). Participants indicated the degree to which they worry about each item, on a scale of 0 (not a worry) to 5 (major worry). Although clinically significant cut scores have not been established, item-specific endorsements of 4 or 5 are considered to represent a ‘major worry’ (Statham et al., 1997). The CWS has shown good reliability and validity (Green et al., 2003).
2.2.3. Centre for Epidemiologic Studies Depression Scale (CES-D)
Participants completed the 10-item CES-D (Anderson et al., 1994), which assesses depressive symptoms over the past week. Responses range from 0 ‘rarely or never (less than 1 day)’ to 3 ‘most or all of the time (5-7 days)’. The CES-D total score ranges from 0 to 30, and a score of ten or higher indicates the presence of clinically significant depressive symptoms (Anderson et al., 1994). The CES-D has shown good reliability and validity in pregnant and postpartum samples (Beeghly et al., 2003).
2.2.4. Insomnia Severity Index (ISI)
Participants completed the 7-item ISI (Bastien et al., 2001) to measure the severity of insomnia problems, sleep satisfaction, sleep interference, and worry about sleep. The ISI total score ranges from 0 to 28; scores between 0-7 indicate no clinically significant insomnia, scores between 8-14 indicate subthreshold insomnia, and scores between 15-28 indicate clinical insomnia (moderate to severe severity) (Bastien et al., 2001).
2.2.5. Cognitive appraisal
Based on prior research indicating that cognitive appraisal of stressors uniquely affects pregnancy and child outcomes (Cao-Lei et al., 2015; Moss et al., 2017; Simcock et al., 2017), participants were asked “Taking everything about COVID-19 into account, the effects of COVID-19 on me and my household have been”, ranging from 1 (Very Positive,) to 5 (Very Negative). Higher ratings indicate a more negative cognitive appraisal of the impact of COVID-19.
2.2.6. Social support
Multidimensional Scale of Perceived Social Support (MSPSS). Participants completed the 12-item MSPSS (Zimet et al., 1988) to measure perceived social support from significant others, family members, and friends. Items range from 1 (very strongly disagree) to 7 (very strongly agree). The MSPSS total score is an average composite of all 12 items, ranging from 1-7. The MSPSS has strong psychometric properties in pregnant samples (Carlsson et al., 2015; Mirabzabeh et al., 2013).
2.3. Statistical analyses
Descriptive and correlation analyses were conducted using SPSS 26. Linear regression analyses were conducted in Mplus Version 8 using full information maximum likelihood (FIML) and bootstrapping to account for missing data and potential non-normality (Fox, 2015). Bias-corrected confidence intervals (CIs) were used; CIs that do not contain zero are significant at p < 0.05. Regression analyses were conducted to assess the unique effects of COVID-specific experiences on depression, anxiety, and insomnia symptoms. In addition, cognitive appraisal and social support were explored as risk/protective factors by testing whether they independently or interactively predicted mental health problems.
The fit of all models was assessed using the comparative fit index (CFI), root mean squared error of approximation (RMSEA), and Standardized Root Mean Square Residual (SRMR). Values greater than .90 for CFI, and less than .08 for RMSEA and SRMR are considered indicative of good model fit (Schumacker & Lomax, 2010).
Missing Data. 0.3% (k=1) of the CES-D, 1.0% (k=3) of the ISI, 2.0% (k=6) of the CWS, and 2.6% (k=8) of the MSPSS were missing. None of the COVID-related or cognitive appraisal items were missing. Based on Little's Missing Completely at Random (MCAR) test, χ2(12) = 11.85, p = .4958, these data were deemed to be missing at random and thus are appropriate for the use of FIML.
3. Results
3.1. Sample
Participants were between 19 and 44 years old (M = 32.13, SD = 4.22 years), 94.4% were married or in common-law relationships, and 47.2% did not have other children (35.6% had one child, 13.2% had two children, and 4.0% had three or more children). Participants ranged from 4 to 36 weeks gestation (M = 21.47 weeks, SD = 8.92 weeks); 24.1% (n= 73) were in the first trimester, 45.2% (n= 137) were in the second trimester, and 30.7% (n= 93) were in the third trimester of pregnancy. A large portion of the sample identified as Caucasian (84.8%), with a smaller portion identifying as Asian (6.9%), Native (0.7%), Mixed Race (3.0%) and Other Race (4.6%). The majority (96.4%) of participants reported completing education beyond high school. Participants reported a median annual household income range of $110,000-$149,999.
3.2. COVID-19 experiences
The Ontario provincial government declared a state of emergency in response to the COVID-19 pandemic on March 17, 2020, mandating schools, public libraries, recreational facilities, childcare centres, bars and restaurants, and other non-essential businesses to close (Office of Premier of Ontario, 2020). On average, participants completed the survey 111.80 days (SD= 13.98 days) after this state of emergency was enacted. At the time of the survey, 5.9% of the sample (n=18) reported visiting a doctor about COVID-19, 1% (n =3) reported being diagnosed with COVID-19, 42.6% (n =129) reported being under self-quarantine, and 71.0% (n = 215) reported not going to their place of work because of COVID-19.
The majority (78.5%) of participants reported that their prenatal appointments and services had not been cancelled because of the pandemic; rather, most participants (72.9%) had phone or video instead of in-person appointments. 91.1% of participants were not allowed to bring a support person to prenatal appointments. Almost half of the sample (44.9%) reported experiencing changes to their birth plan because of COVID-19. In addition, participants reported having trouble accessing other health-care services, including prenatal classes (39.3%), massage therapy (50.8%), and psychological counselling (10.2%).
Means, standard deviations (SDs), and ranges of the COVID-19 experiences Likert items, which range from 1 to 7, are reported in Table 1. Single items were used to represent social isolation (M = 6.34, SD = 1.20) and a loved one being at risk of getting COVID-19 (M = 4.11, SD = 1.76). Given the conceptual similarity and high intercorrelations between items, the six items related to financial difficulties were averaged to compute a Financial Difficulties subscale (M = 2.40, SD = 1.39), which had good internal consistency (Cronbach's alpha = .81). Similarly, the two items related to relationship functioning were averaged to derive a Relationship Difficulties subscale (M = 2.23, SD =1.32), which had good internal consistency (Cronbach's alpha = .75).
Regarding cognitive appraisal of the impact of COVID-19, 5.0% of the sample indicated that the overall effect of COVID-19 has been Very Negative, 72.3% indicated a Negative effect, 11.9% indicated No effect, 10.9% indicated a Positive effect, and zero participants indicated a Very Positive effect of COVID-19 on themselves and their household.
3.3. Anxiety, depression, and sleep
Means, SDs, and ranges of the depression (CES-D), anxiety (CWS), and insomnia (ISI) measures are shown in Table 1. Depression (F (2, 301) = 0.87, p = .42), anxiety (F (2, 296) = 0.80, p = .45), and insomnia (F (2, 300) = 2.25, p = .11) symptom severity did not significantly differ by trimester of pregnancy, thus subsequent analyses were conducted with data combined across trimesters.
57.1% (n = 173) of the sample scored ≥ 10 on the CES-D, indicating clinically significant levels of depression. In the present study, the average CES-D score (M = 11.50, SD = 6.36) was significantly higher than the average scores reported in a pre-COVID sample of pregnant women (M = 5.11, SD = 3.50; t = 25.14, SE= 0.25, p < .0001) (Kiviruusu et al., 2020).
Participants in the current study also reported higher levels of anxiety on the CWS compared to prior samples. As shown in Table 2 , significant worries (ratings of 4 or 5; Statham et al., 1997) were endorsed for several items of the CWS. The most highly endorsed worry items were something being wrong with the infant (43.3%), whether my partner will be at the birth (41.8%), and giving birth (39.6%). Descriptive comparisons show that rates of significant worries (4 or 5) in the present sample are higher than pre-COVID pregnancy samples (Gourounti et al., 2012; Öhman et al., 2003; Petersen et al., 2009). For example, in a pre-COVID sample of pregnant women (Petersen et al., 2009), only 15.5% worried about something being wrong with the infant, 4.5% worried about whether their partner will be at the birth, and 20.8% worried about giving birth. In addition, in the present study, the average CWS mean score (M = 1.94, SD = .97) was significantly higher than the average score (M = 1.16, SD = 0.68) reported in the initial validation study of the CWS (t = 17.21, SE= .045, p < .0001) (Green et al., 2003).
Table 2.
Responses to the Cambridge Worry Scale (CWS).
| Item | 0 | 1 | 2 | 3 | 4 | 5 | 4 and 5 | Mean (SD) |
|---|---|---|---|---|---|---|---|---|
| Not a worry |
Major Worry |
|||||||
| % | % | % | % | % | % | % | ||
| Possibility of something wrong with infant | 7.6 | 13.8 | 16.6 | 18.7 | 14.9 | 28.4 | 43.3 | 3.04 (1.64) |
| Whether your partner will be at birth | 27.1 | 8.6 | 11.1 | 11.4 | 10.7 | 31.1 | 41.8 | 2.63 (2.03) |
| Giving birth | 9.7 | 11.8 | 18.8 | 20.1 | 13.2 | 26.4 | 39.6 | 2.94 (1.65) |
| Coping with the new baby | 13.1 | 14.1 | 14.8 | 20.6 | 17.2 | 20.3 | 37.5 | 2.76 (1.68) |
| The possibility of miscarriage | 22.5 | 17.0 | 12.8 | 13.5 | 10.4 | 23.9 | 34.3 | 2.44 (1.89) |
| The health of someone else close | 16.8 | 9.8 | 21.8 | 21.4 | 16.8 | 13.3 | 30.1 | 2.52 (1.61) |
| Going to the hospital | 25.8 | 13.2 | 16.7 | 15.3 | 8.4 | 20.6 | 29.0 | 2.29 (1.85) |
| Your own health | 14.3 | 17.8 | 21.3 | 21.3 | 13.2 | 12.2 | 25.4 | 2.38 (1.57) |
| Money problems | 26.7 | 11.9 | 22.1 | 18.9 | 12.3 | 8.1 | 20.4 | 2.02 (1.61) |
| Employment problems | 44.1 | 11.4 | 12.4 | 13.1 | 6.6 | 12.4 | 19.0 | 1.64 (1.81) |
| Giving up work | 50.9 | 4.9 | 10.1 | 15.3 | 4.2 | 14.6 | 18.8 | 1.61 (1.89) |
| Internal examinations | 54.4 | 11.2 | 10.5 | 11.9 | 3.4 | 8.5 | 11.9 | 1.24 (1.66) |
| Your housing | 58.6 | 14.5 | 9.3 | 7.9 | 5.9 | 3.8 | 9.7 | 0.99 (1.46) |
| Relationship with family & friends | 38.9 | 19.1 | 20.5 | 13.7 | 4.4 | 3.4 | 7.8 | 1.36 (1.40) |
| Relationship with partner | 51.4 | 21.1 | 11.2 | 9.2 | 3.1 | 4.1 | 7.2 | 1.04 (1.39) |
| Problems with the law | 95.5 | 2.1 | 1.7 | 0 | 0 | 0.7 | 0.7 | 0.09 (0.50) |
In terms of sleep difficulties, 39.5% (n = 119) of the sample reported no clinically significant insomnia (ISI score ≤ 7), 41.2% (n = 124) reported subthreshold insomnia (ISI score 8-14), 19.2% (n = 58) reported clinical insomnia (ISI score ≥ 15). The average ISI total score for the sample was not significantly different (t = 0.00, SE= .50, p = .99) from a non-COVID sample of pregnant individuals in Canada (Sedov et al., 2019).
3.4. COVID experiences in relation to mental health symptoms
To determine which variables should be included as covariates, Pearson correlations were conducted between mental health outcomes and potential confounders. As shown in Table 3 , education and income were significantly correlated with depression, anxiety, and insomnia; race was correlated with depression and anxiety; and number of children was correlated with anxiety. For consistency across models, education, income, race, and number of children were covaried in all subsequent analyses.
Table 3.
Correlations between mental health symptoms, social support, and potential covariates.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Depression (CES-D) | — | |||||||||||
| 2. Anxiety (CWS) | .60** | — | ||||||||||
| 3. Insomnia (ISI) | .58** | .49** | — | |||||||||
| 4. Social Support (MSPSS) | −.38** | −.25** | −.24** | — | ||||||||
| 5. Negative cognitive appraisal | .33** | .20** | .20** | −.08 | — | |||||||
| 6. Age | .04 | .10 | .08 | −.04 | −.05 | — | ||||||
| 7. Race | .14* | .19** | .06 | −.02 | .04 | −.01 | — | |||||
| 8. Education | −.33** | −.21** | −.28** | .22** | −.07 | .15* | .15** | — | ||||
| 9. Household income | −.20** | −.18** | −.14* | .11 | −.03 | .27** | −.05 | .45** | — | |||
| 10. Number of children | .05 | −.15* | .07 | −.07 | −.03 | .30** | −.14* | −.11 | .01 | — | ||
| 11. Trimester of pregnancy | −.02 | −.07 | .10 | .02 | .04 | .02 | −.02 | −.01 | −.00 | .08 | — | |
| 12. Days since state of emergency enacted | −.00 | −.05 | .05 | .01 | −.04 | .10 | .04 | .11* | .09 | .02 | −.10 | — |
Note: CES-D = Centre for Epidemiologic Studies Depression Scale, CWS = Cambridge Worry Scale, ISI = Insomnia Severity Index; MSPSS = Multidimensional Scale of Perceived Social Support
** p < .01, * p < .05
Linear regression analyses, with bootstrap CIs, were conducted to assess which COVID experiences were uniquely associated with severity of depression, anxiety, and insomnia symptoms, after controlling for relevant covariates (Table 4 ). The overall model significantly predicted depressive symptoms, F(8, 294) = 14.65, p < .001, adjusted R2 = .285, and the main effects of risk of COVID infection, social isolation, and relationship difficulties were significantly associated with elevated depression. The overall model also significantly predicted anxiety symptoms, F(8, 294) = 20.76, p < .001, adjusted R2 = .361, and the main effects of risk of COVID infection, social isolation, financial difficulties, and relationship difficulties were all significantly associated with higher anxiety symptoms. Lastly, the overall model significantly predicted insomnia symptoms, F(8, 294) = 10.31, p < .001, adjusted R2 = .219, and the main effects of risk of COVID infection, financial difficulties, and relationship difficulties were significantly related to more sleep problems (see Table 4).
Table 4.
Linear regression results of COVID-19 experiences predicting mental health symptoms
| β | Std. Error | Bootstrap CI [95%] |
|
|---|---|---|---|
| Depression (CES-D) | |||
| Race | 0.151* | 0.059 | 0.037, 0.273 |
| Education | −0.261⁎⁎ | 0.056 | −0.369, −0.152 |
| Income | −0.046 | 0.059 | −0.162, 0.068 |
| Number of children | 0.058 | 0.050 | −0.039, 0.155 |
| Risk of COVID infection | 0.126* | 0.052 | 0.021, 0.226 |
| Social Isolation | 0.115* | 0.053 | 0.006, 0.218 |
| Financial Difficulties | 0.088 | 0.059 | −0.031, 0.200 |
| Relationship Difficulties | 0.272⁎⁎ | 0.051 | 0.169, 0.371 |
| Anxiety (CWS) | |||
| Race | 0.133* | 0.052 | 0.031, 0.235 |
| Education | −0.105 | 0.060 | −0.224, 0.015 |
| Income | −0.055 | 0.055 | −0.165, 0.056 |
| Number of children | −0.115⁎⁎ | 0.047 | −0.209, −0.026 |
| Risk of COVID infection | 0.236⁎⁎ | 0.052 | 0.135, 0.338 |
| Social Isolation | 0.115* | 0.049 | 0.017, 0.209 |
| Financial Difficulties | 0.255⁎⁎ | 0.056 | 0.138, 0.361 |
| Relationship Difficulties |
0.236⁎⁎ | 0.054 | 0.129, 0.343 |
| Insomnia (ISI) | |||
| Race | 0.068 | 0.047 | −0.027, 0.161 |
| Education | −0.208⁎⁎ | 0.056 | −0.313, −0.093 |
| Income | 0.008 | 0.065 | −0.122, 0.133 |
| Number of children | 0.076 | 0.051 | −0.027, 0.174 |
| Risk of COVID infection | 0.240⁎⁎ | 0.051 | 0.139, 0.336 |
| Social Isolation | 0.022 | 0.057 | −0.088, 0.136 |
| Financial Difficulties | 0.167⁎⁎ | 0.059 | 0.051, 0.279 |
| Relationship Difficulties | 0.155⁎⁎ | 0.056 | 0.044, 0.267 |
Note. CES-D = Centre for Epidemiologic Studies Depression Scale, CWS = Cambridge Worry Scale, ISI = Insomnia Severity Index. Results include bootstrap CIs. Fit indices for all models: CFI = 1.00, RMSEA = .00, SRMS = .00.
p < .01,
p < .05
3.5. Cognitive appraisal and social support as protective factors
As shown in Table 3, negative cognitive appraisal was significantly correlated with higher depression, anxiety, and insomnia symptoms, whereas social support was correlated with lower mental health symptoms. Given these bivariate associations, we tested whether social support and cognitive appraisal acted as independent or interactive predictors of mental health symptoms. In this model, we used a latent composite of mental health symptoms as the outcome variable because depression, anxiety, and insomnia symptoms were intercorrelated (Table 3).
The final regression model included relevant covariates, the main effects of COVID-19 cognitive appraisal and social support, and their interaction as predictors of the latent mental health variable. This model demonstrated good model fit (CFI = 0.95, RMSEA = .07, SRMR = .03). The main effect of negative cognitive appraisal was significant (β = .936, SE = .305, 95% CI [0.247, 1.445]), however, social support was not significant (β = .369, SE = .324, 95% CI [-0.351, 0.923]). The interaction between negative cognitive appraisal of COVID-19 and total social support was significantly associated with mental health symptoms (β = -.917, SE = .409, 95% CI −1.602, −0.010]).
To illustrate this interaction effect, a figure was created using the unstandardized regression coefficients (Preacher et al., 2006). While continuous measures were used in the regression model, 1 SD above and below the mean of total social support was used for graphing the interaction (Aiken and West, 1991; Preacher, Curran, & Bauer, 2004, 2006). As shown in Fig. 1 , individuals who endorsed more negative appraisal of COVID-19 experienced higher mental health symptoms if they also experienced lower social support (black solid line), compared to if they experienced higher social support (grey dotted line). In contrast, individuals who perceived the impact of COVID-19 to be positive had lower mental health symptoms regardless of their level of social support. This suggests that higher levels of social support act as a protective factor for those who appraise the impact of COVID-19 to be more negative.
Fig. 1.
Social support moderates the effect of negative cognitive appraisal of COVID-19 on mental health symptoms.
4. Discussion
The present study provides empirical evidence that pregnant women are experiencing high levels of anxiety and depressive symptoms during the COVID-19 pandemic. Although a portion of the sample also reported clinically elevated insomnia, rates of sleep problems did not differ from pre-COVID pregnancy samples. Findings also indicate specific COVID-experiences (i.e., financial difficulties, social isolation, relationship difficulties, and health concerns) are differentially related to depression, anxiety, and insomnia symptoms. Lastly, results indicate an interactive effect of cognitive appraisal and social support in buffering pregnant individuals from experiencing elevated mental health outcomes. Taken together, these findings underscore the dire need to decrease mental health problems experienced by pregnant individuals and outline potential intervention targets (cognitive appraisal and social support) to protect pregnant people from experiencing these mental health outcomes as a result of the COVID-19 pandemic.
Since the COVID-19 outbreak in December 2019, scholars have documented the detrimental effects of this pandemic on mental health (e.g., Di Nicola et al., 2020; Moccia et al., 2020; Voitsidis et al., 2020; Wang et al., 2020), and have anticipated the likely compounded impact on pregnant people (e.g., Abdoli et al., 2020; Ceulemns et al., 2020; Fakari et al., 2020). The present findings confirm that pregnant individuals are experiencing elevated mental health problems. Of the current sample, 57% endorsed clinically elevated rates of depression. In comparison, systematic reviews and meta-analyses indicate that between 7 and 12% of individuals typically experience clinically significant depression during pregnancy (Bennett et al., 2004; Woody et al., 2017). In addition, prior to COVID-19, 7.7% of pregnant women in Ontario, Canada endorsed clinically elevated depression (Public Health Ontario, 2017). Further, the mean depression scores on the CES-D for the current sample were significantly higher than those reported by other samples of pregnant people prior to the COVID-19 pandemic (e.g., Kiviruusu et al., 2020). In line with these results, preliminary empirical evidence from the immediate aftermath of the pandemic also indicated that pregnant people experienced elevated rates of clinical depression (Ceulemans et al., 2020; Lebel et al., 2020; Wu et al., 2020). Although the rates are not perfectly comparable, because of methodological heterogeneity, the rate of clinically elevated depression in the current sample (57%) is even higher than studies conducted earlier in the COVID-19 pandemic (March-April 2020), which reported rates between 25% and 37% (Ceulemans et al., 2020; Lebel et al., 2020). This is particularly relevant given that the current study occurred in June and July 2020, an average of 111 days after the state of emergency was declared in Ontario, Canada. It is plausible that as the pandemic continues, and social distancing measures are prolonged, pregnant individuals will endure intensified depression. Prior research indicates that longer quarantine is related to more severe psychological distress (Hawryluck et al., 2004). Thus, as the COVID-19 pandemic prolongs, there is a strong need for immediate and continued mental health support for pregnant people.
In addition, this sample endorsed high rates of anxiety. Across the different items on the CWS, between 30% and 40% of participants endorsed significant worries related to pregnancy and general health (Table 2). The average ratings on the CWS are significantly higher than non-COVID pregnancy samples (Green et al., 2003). These findings are also in line with recent meta-analytic findings that perinatal women are experiencing higher rates of anxiety during COVID-19 compared to before the pandemic (Hessami et al., 2020). Further, examination of individual item endorsements indicates that the current sample is worrying more about their delivery (e.g., whether their partner will be present, giving birth) and their infant's health (e.g., something being wrong with the infant), in comparison to non-COVID samples (Ohman et al., 2003; Petersen et al., 2009; Statham et al., 1997). It is important to understand the specific worries that pregnant people are experiencing, so that these worries and concerns can be addressed through public health initiatives and mental health interventions.
In addition to anxiety and depression, sleep quality is an important predictor of wellbeing. Of the current sample, 19.2% experienced clinically significant insomnia symptoms. Although insomnia rates were not significantly different from pre-COVID samples (Sedov et al., 2019), they indicate that a substantial portion of pregnant women are experiencing sleep problems and that these sleep problems are exacerbated by specific difficulties resulting from COVID-19. Prior research demonstrates that sleep problems are common during pregnancy (Sedov et al., 2018) and that sleep difficulties are related to adverse birth outcomes (Okun et al., 2011) and maternal mental health in the perinatal period (Tomfohr et al., 2015; Skouteris et al., 2008).
Furthermore, risk of COVID-19 infection and relationship difficulties were associated with elevated depression, anxiety, and insomnia symptoms; social isolation was associated with elevated anxiety and depression, but not insomnia symptoms; and financial difficulties were associated with anxiety and sleep difficulties. Together, these findings confirm that several secondary outcomes of this pandemic contribute to elevated mental health problems.
Mental health difficulties during pregnancy are known to have both acute and long-term consequences for pregnant people and their children. In particular, anxiety, depression and insomnia during pregnancy can increase the risk of miscarriage and preterm birth (Accortt et al., 2015; Dancause et al., 2011; Grigoriadis et al., 2018; Li et al., 2017). Stress and mental health during pregnancy is also predictive of child physical health (Turcotte-Tremblay et al., 2014) and mental health difficulties (Davalos et al., 2012; Madigan et al., 2018). Systematically targeting specific COVID-related experiences (e.g., social isolation, relationship conflict) and the associated mental health difficulties, through governmental, public health, and mental health initiatives will be key to reducing the mental health problems experienced by pregnant people and preventing adverse developmental and health outcomes for their unborn children.
These findings also highlight the important role of cognitive appraisal and social support in modulating mental health severity. Prior work has demonstrated that appraisal of stressful events, including natural disaster and epidemics, strongly impacts the severity of stress and mental health outcomes (Cheng et al., 2004; Kucharska, 2017; Ng et al., 2006) and, in the case of pregnant individuals, directly impacts child outcomes (Cao-Lei et al., 2015; Moss et al., 2017; Simcock et al., 2017). In addition, ample research indicates that, in the context of stressful life events, social support buffers against mental health problems (Bonanno et al., 2008; Cohen, 2004; King et al., 2012). In addition to establishing that negative cognitive appraisal of COVID-19 and social support are related to higher and lower mental health symptom severity, respectively, we demonstrate an interactive effect of these two factors in predicting mental health. At high levels of negative cognitive appraisal, individuals with lower social support experienced the greatest mental health problems, whereas individuals with higher social support experienced ameliorated mental health problems. In contrast, at low levels of negative cognitive appraisal, perceived social support did not impact mental health severity. This suggests that social support has the potential to buffer against adverse mental health outcomes, particularly for those who perceive a more negative impact of COVID-19.
These findings have important clinical implications. First, this research highlights the need for heightened support for pregnant individuals. Pregnant women are continuing to experience high levels of anxiety and depression, several months after the pandemic initially began. Further, as suggested by others (e.g., Sani et al., 2020), these mental health outcomes are directly linked to secondary effects of COVID-19 (i.e., social isolation, relationship difficulties, financial burden). It is vital to address these mental health concerns, as well as the associated COVID-related risk factors, before they worsen and further impact the health of pregnant women and their unborn children. Second, these findings highlight two specific risk and protective factors, cognitive appraisal and social support, which modulate mental health outcomes. Cognitive appraisal and social support are both highly modifiable and can be targeted through various interventions.
Given that this sample was drawn from the general population and that a large portion of participants were receiving prenatal care (albeit via phone or video), assessing and initially addressing these mental health problems will likely fall on professionals that typically manage prenatal care (i.e., primary care practitioners, midwives, public health nurses, and obstetricians). Thus, there is a need to increase clinician awareness of the heightened risk for these mental health issues, provide health care professionals with the appropriate tools to assess for perinatal depression and anxiety, and ensure that inquiries about social supports and appraisal of/coping with the pandemic are part of these assessments. Furthermore, health care providers must have clear evidence-informed guidelines in place for either treating individuals or referring to other professionals, and, in the event of referral, ensuring that patients are assisted with service navigation (Sani et al., 2020). In terms of specific interventions, there is strong evidence that Cognitive Behavioral Therapy (CBT) and mindfulness-based approaches are effective in reducing depression and anxiety in perinatal women (e.g., Sockel, 2015; Shi & MacBeth, 2017). CBT is a manualized intervention, which can be employed by a range of primary health care professionals. With these enhanced rates of depression and anxiety, there may be a need for more primary health care professionals to develop skills to provide CBT and to ensure that family health teams have mental health professionals that can provide counselling.
Employing widespread public health and clinical interventions in the context of the pandemic can be challenging, however, there is support that electronic interventions can effectively address mental health concerns (e.g., Heller et al., 2020; Tanhan et al., 2020; Sani et al., 2020). For example, in Ontario, the Canadian Mental Health Association (CMHA) has developed a self-guided manualized intervention called Bounceback, which includes a skill-building program that individuals can access over the phone with a coach and through online videos (Lau and davis, 2019). Given the elevated rates of mental health problems, electronic interventions should be further evaluated.
These findings must be understood in the context of study limitations. First, given the health and safety regulations, this study was conducted exclusively using online questionnaires. Although this ensured safety and allowed for broader recruitment, it is possible that this questionnaire-based mental health data might differ from in-person clinical interviews. Second, we did not gather information about prior psychiatric diagnoses or treatment, and thus are unable to determine whether the high rates of depression and anxiety during the pandemic are related to prior mental health problems. However, given that this is a demographically low-risk sample, recruited from online sources, there is little reason to suspect higher psychiatric risk compared to the general population. Related, this is a socio-demographically low-risk sample, in that many participants were high income and in a relationship, all participants have access to universal healthcare in Ontario, Canada, and few participants were diagnosed with COVID-19 (as Ontario, Canada had lower rates of infection compared to other Canadian provinces and countries). In a sense, the relatively low-risk nature of this sample combined with the high rates of mental health problems underscores the urgent need for enhanced mental health support during the COVID-19 pandemic. Future work is needed to determine whether similar (or more severe) mental health problems are experienced by pregnant women dealing with greater health, interpersonal, or socioeconomic burdens, or by those living in regions more harshly impacted by COVID-19. In addition, longitudinal work is needed to understand the long-term impact of mental health problems for pregnant individuals as the pandemic progresses.
5. Conclusions
Pregnant people are experiencing significantly elevated symptoms of depression and anxiety and comparable rates of insomnia, compared to pre-COVID pregnancy samples. Direct threat of contracting COVID-19, economic hardship, social isolation, and relationship difficulties are all associated with elevated mental health symptoms. In addition, social support acts as a protective factor to buffer individuals from experiencing exacerbated mental health symptoms, in the context of negative cognitive appraisal of COVID-19. The role of social support and cognitive appraisal highlight two potentially modifiable factors that can be targeted through intervention. These data underscore the critical need to improve the mental health of pregnant individuals during this extremely stressful time.
Author statement
J.E. Khoury, A. Gonzalez, and A. Atkinson designed the study and wrote the protocol. S. Jack and T. Bennett oversaw the clinical aspects and implications of the study. J.E. Khoury carried out the data collection and management and undertook the statistical analysis. J.E. Khoury wrote the first draft of the manuscript. All authors contributed to editing the manuscript and have approved the final manuscript.
Funding
This work was supported by a Tier II Canadian Institute of Health Research (CIHR) Canadian Research Chair (CRC) in Family Health and Preventive Interventions (Project#: 20011917) awarded to Dr. Andrea Gonzalez and by a CIHR Postdoctoral Fellowship awarded to Dr. Jennifer Khoury.
Declaration of Competing Interest
None of the authors of this manuscript have affiliations with or involvement in any organization or entity with any financial interest, or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Acknowledgements
We'd like to thank all of the pregnant people who participated in this research and the research assistants who helped carry out this work.
References
- Abdoli A., Falahi S., Kenarkoohi A., Shams M., Mir H., Jahromi M.A.M. The COVID-19 pandemic, psychological stress during pregnancy, and risk of neurodevelopmental disorders in offspring: a neglected consequence. J. Psychosom. Obstet. Gynaecol. 2020;1 doi: 10.1080/0167482X.2020.1761321. [DOI] [PubMed] [Google Scholar]
- Abshire M., Russell S.D., Davidson P.M., Budhathoki C., Han H.R., Grady K.L., Himmelfarb C.D. Social support moderates the relationship between perceived stress and quality of life in patients with a left ventricular assist device. J. Cardiovasc. Nurs. 2018;33(5) doi: 10.1097/JCN.0000000000000487. E1-E9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Accortt E.E., Cheadle A.C., Schetter C.D. Prenatal depression and adverse birth outcomes: an updated systematic review. Matern. Child Health J. 2015;19(6):1306–1337. doi: 10.1007/s10995-014-1637-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aiken L.S., West S.G. Sage; Thousand Oaks: 1991. Multiple Regression: Testing and Interpreting Interactions. [Google Scholar]
- Anderson E.M., Malmgren J.A., Carter W.B., Patrick D.L. Screening for depression in well older adults: evaluation of a short form of the CES-D. Am. J. Prev. Med. 1994;10(2):77–84. [PubMed] [Google Scholar]
- Bastien C.H., Vallières A., Morin C.M. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001;2(4):297–307. doi: 10.1016/s1389-9457(00)00065-4. [DOI] [PubMed] [Google Scholar]
- Beeghly M., Olson K.L., Weinberg M.K., Pierre S.C., Downey N., Tronick E.Z. Prevalence, stability, and socio-demographic correlates of depressive symptoms in Black mothers during the first 18 months postpartum. Matern. Child Health J. 2003;7(3):157–168. doi: 10.1023/a:1025132320321. [DOI] [PubMed] [Google Scholar]
- Bennett H.A., Einarson A., Taddio A., Koren G., Einarson T.R. Prevalence of depression during pregnancy: systematic review. Obstetr. Gynecol. 2004;103(4):698–709. doi: 10.1097/01.AOG.0000116689.75396.5f. [DOI] [PubMed] [Google Scholar]
- Bonanno G.A., Ho S.M., Chan J.C., Kwong R.S., Cheung C.K., Wong C.P., Wong V.C. Psychological resilience and dysfunction among hospitalized survivors of the SARS epidemic in Hong Kong: a latent class approach. Health Psychol. 2008;27(5):659–667. doi: 10.1037/0278-6133.27.5.659. [DOI] [PubMed] [Google Scholar]
- Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., Rubin G.J. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet North Am. Ed. 2020;10227:912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cao W., Fang Z., Hou G., Han M., Xu X., Dong J., Zheng J. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 2020 doi: 10.1016/j.psychres.2020.112934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cao-Lei L., Elgbeili G., Massart R., Laplante D.P., Szyf M., King S. Pregnant women’s cognitive appraisal of a natural disaster affects DNA methylation in their children 13 years later: project Ice Storm. Transl. Psychiatry. 2015;5(2) doi: 10.1038/tp.2015.13. e515-e515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlsson M., Ziegert K., Nissen E. The relationship between childbirth self-efficacy and aspects of well-being, birth interventions and birth outcomes. Midwifery. 2015;31(10):1000–1007. doi: 10.1016/j.midw.2015.05.005. [DOI] [PubMed] [Google Scholar]
- Ceulemans M., Hompes T., Foulon V. Mental health status of pregnant and breastfeeding women during the COVID-19 pandemic: a call for action. Int. J. Gynecol. Obstetr. 2020 doi: 10.1002/ijgo.13295. [DOI] [PubMed] [Google Scholar]
- Cheng S.K., Wong C.W., Tsang J., Wong K.C. Psychological distress and negative appraisals in survivors of severe acute respiratory syndrome (SARS) Psychol. Med. 2004;34(7):1187–1195. doi: 10.1017/s0033291704002272. [DOI] [PubMed] [Google Scholar]
- Cohen S. Social relationships and health. Am. Psychol. 2004;59(8):676–684. doi: 10.1037/0003-066X.59.8.676. [DOI] [PubMed] [Google Scholar]
- Davalos D.B., Yadon C.A., Tregellas H.C. Untreated prenatal maternal depression and the potential risks to offspring: a review. Arch. Women’s Mental Health. 2012;15(1):1–14. doi: 10.1007/s00737-011-0251-1. [DOI] [PubMed] [Google Scholar]
- Dancause K.N., Laplante D.P., Oremus C., Fraser S., Brunet A., King S. Disaster-related prenatal maternal stress influences birth outcomes: Project Ice Storm. Early Hum. Dev. 2011;87(12):813–820. doi: 10.1016/j.earlhumdev.2011.06.007. [DOI] [PubMed] [Google Scholar]
- Demirtas O., Ozdevecioglu M., Capar N. The relationship between cognitive emotion regulation and job stress: moderating role of social support. Asian Soc. Sci. 2015;11(12):168–173. [Google Scholar]
- DiGiovanni C., Conley J., Chiu D., Zaborski J. Factors influencing compliance with quarantine in Toronto during the 2003 SARS outbreak. Biosecurity Bioterrorism: Biodefense Strat. Pract. Sci. 2004;2(4):265–272. doi: 10.1089/bsp.2004.2.265. [DOI] [PubMed] [Google Scholar]
- Di Nicola M., Dattoli L., Moccia L., Pepe M., Janiri D., Fiorillo A., Sani G. Serum 25-hydroxyvitamin D levels and psychological distress symptoms in patients with affective disorders during the COVID-19 pandemic. Psychoneuroendocrinology. 2020;122 doi: 10.1016/j.psyneuen.2020.104869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elliott T.R., Herrick S.M., Witty T.E. Problem-solving appraisal and the effects of social support among college students and persons with physical disabilities. J. Counsel. Psychol. 1992;39(2):219–226. [Google Scholar]
- Fakari F.R., Simbar M. Coronavirus pandemic and worries during pregnancy; a letter to editor. Arch. Acad. Emergency Med. 2020;8(1) [PMC free article] [PubMed] [Google Scholar]
- Field T. Vol. 34. Infant Behavior and Development; 2011. pp. 1–14. (Prenatal Depression Effects on Early Development: a Review). [DOI] [PubMed] [Google Scholar]
- Fox J. Sage Publications; Los Angeles: 2015. Applied Regression Analysis and Generalized Linear Models. [Google Scholar]
- Gourounti K., Lykeridou K., Taskou C., Kafetsios K., Sandall J. A survey of worries of pregnant women: reliability and validity of the Greek version of the Cambridge Worry Scale. Midwifery. 2012;28(6):746–753. doi: 10.1016/j.midw.2011.09.004. [DOI] [PubMed] [Google Scholar]
- Green J.M., Kafetsios K., Statham H.E., Snowdon C.M. Factor structure, validity and reliability of the Cambridge Worry Scale in a pregnant population. J. Health Psychol. 2003;8(6):753–764. doi: 10.1177/13591053030086008. [DOI] [PubMed] [Google Scholar]
- Grigoriadis S, Graves L, Peer M, Mamisashvili L, Tomlinson G, Vigod SN, Dennis CL, Steiner M, Brown C, Cheung A, Dawson H, Rector NA, Guenette M, Richter M. Maternal anxiety during pregnancy and the association with adverse perinatal outcomes: systematic review and meta-analysis. J. Clin. Psychiatry. 2018;(5):79. doi: 10.4088/JCP.17r12011. [DOI] [PubMed] [Google Scholar]
- Hawryluck L., Gold W.L., Robinson S., Pogorski S., Galea S., Styra R. SARS control and psychological effects of quarantine, Toronto, Canada. Emerg. Infect. Dis. 2004;10(7):1206–1212. doi: 10.3201/eid1007.030703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heller H.M., Hoogendoorn A.W., Honig A., Broekman B.F., van Straten A. The effectiveness of a guided internet-based tool for the treatment of depression and anxiety in pregnancy (MamaKits Online): randomized controlled trial. J. Med. Internet Res. 2020;22(3):e15172. doi: 10.2196/15172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hessami K., Romanelli C., Chiurazzi M., Cozzolino M. COVID-19 pandemic and maternal mental health: a systematic review and meta-analysis. J. Matern. Fetal Neonatal Med. 2020:1–8. doi: 10.1080/14767058.2020.1843155. [DOI] [PubMed] [Google Scholar]
- Huang Y., Zhao N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psychiatry Res. 2020 doi: 10.1016/j.psychres.2020.112954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King S., Dancause K., Turcotte-Tremblay A.M., Veru F., Laplante D.P. Using natural disasters to study the effects of prenatal maternal stress on child health and development. Birth Defects Res. Part C: Embryo Today: Rev. 2012;96(4):273–288. doi: 10.1002/bdrc.21026. [DOI] [PubMed] [Google Scholar]
- Kiviruusu O., Pietikäinen J.T., Kylliäinen A., Pölkki P., Saarenpää-Heikkilä O., Marttunen M., Paavonen E.J. Trajectories of mothers’ and fathers’ depressive symptoms from pregnancy to 24 months postpartum. J. Affect. Disord. 2020;260:629–637. doi: 10.1016/j.jad.2019.09.038. [DOI] [PubMed] [Google Scholar]
- Kucharska J. Sex differences in the appraisal of traumatic events and psychopathology. Psychol. Trauma: Theory, Res. Pract. Policy. 2017;9(5):575–582. doi: 10.1037/tra0000244. [DOI] [PubMed] [Google Scholar]
- Lau M.A., Davis S. Evaluation of a cognitive behavior therapy program for BC primary care patients with mild to moderate depression with or without anxiety: bounce back. Br. Columbia Med. J. 2019;61(1):25–32. 2008–2014. [Google Scholar]
- Lazarus RS, Stress Folkman S. N.Y: Springer; 1984. Appraisal and Coping. [Google Scholar]
- Lazarus RS. Oxford University Press; New York: 1991. Emotion and Adaptation. [Google Scholar]
- Lebel C., MacKinnon A., Bagshawe M., Tomfohr-Madsen L., Giesbrecht G. Elevated depression and anxiety symptoms among pregnant individuals during the COVID-19 pandemic. J. Affect. Disord. 2020;277(1):5–13. doi: 10.1016/j.jad.2020.07.126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee S., Chan L.Y., Chau A.M., Kwok K.P., Kleinman A. The experience of SARS-related stigma at Amoy Gardens. Soc. Sci. Med. 2005;61(9):2038–2046. doi: 10.1016/j.socscimed.2005.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li R., Zhang J., Zhou R., Liu J., Dai Z., Liu D., Zeng G. Sleep disturbances during pregnancy are associated with cesarean delivery and preterm birth. J. Matern. Fetal Neonatal Med. 2017;30(6):733–738. doi: 10.1080/14767058.2016.1183637. [DOI] [PubMed] [Google Scholar]
- Liu Y.L. The role of perceived social support and dysfunctional attitudes in predicting Taiwanese adolescents’ depressive tendency. Adolescence. 2002;37(148):823–835. [PubMed] [Google Scholar]
- Liu C.H., Erdei C., Mittal L. Risk factors for depression, anxiety, and PTSD symptoms in perinatal women during the COVID-19 Pandemic. Psychiatry Res. 2020 doi: 10.1016/j.psychres.2020.113552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madigan S., Oatley H., Racine N., Fearon R.P., Schumacher L., Akbari E., Tarabulsy G.M. A meta-analysis of maternal prenatal depression and anxiety on child socioemotional development. J. Am. Acad. Child Adolesc. Psychiatry. 2018;57(9):645–657. doi: 10.1016/j.jaac.2018.06.012. [DOI] [PubMed] [Google Scholar]
- Mindell J.A., Cook R.A., Nikolovski J. Sleep patterns and sleep disturbances across pregnancy. Sleep Med. 2015;16(4):483–488. doi: 10.1016/j.sleep.2014.12.006. [DOI] [PubMed] [Google Scholar]
- Mirabzadeh A., Dolatian M., Forouzan A.S., Sajjadi H., Majd H.A., Mahmoodi Z. Path analysis associations between perceived social support, stressful life events and other psychosocial risk factors during pregnancy and preterm delivery. Iranian Red Crescent Med. J. 2013;15(6):507–514. doi: 10.5812/ircmj.11271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moccia L., Janiri D., Pepe M., Dattoli L., Molinaro M., De Martin V., Di Nicola M. Affective temperament, attachment style, and the psychological impact of the COVID-19 outbreak: an early report on the Italian general population. Brain Behav. Immunity. 2020 doi: 10.1016/j.bbi.2020.04.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moss K.M., Simcock G., Cobham V., Kildea S., Elgbeili G., Laplante D.P., King S. A potential psychological mechanism linking disaster-related prenatal maternal stress with child cognitive and motor development at 16 months: the QF2011 Queensland Flood Study. Dev. Psychol. 2017;53(4):629–641. doi: 10.1037/dev0000272. [DOI] [PubMed] [Google Scholar]
- Ng S.M., Chan T.H., Chan C.L., Lee A.M., Yau J.K., Chan C.H., Lau J. Group debriefing for people with chronic diseases during the SARS pandemic: Strength-Focused and Meaning-Oriented Approach for Resilience and Transformation (SMART) Community Ment. Health J. 2006;42(1):53–63. doi: 10.1007/s10597-005-9002-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ontario Office of Premier of. Government of Ontario Newsroom; 2020. Ontario Enacts Declaration of Emergency to Protect the Public.https://news.ontario.ca/opo/en/2020/3/ontario-enacts-declaration-of-emergency-to-protect-the-public.html March. [Google Scholar]
- Öhman S.G., Grunewald C., Waldenström U. Women’s worries during pregnancy: testing the Cambridge Worry Scale on 200 Swedish women. Scand. J. Caring Sci. 2003;17(2):148–152. doi: 10.1046/j.1471-6712.2003.00095.x. [DOI] [PubMed] [Google Scholar]
- Okun M.L., Schetter C.D., Glynn L.M. Poor sleep quality is associated with preterm birth. Sleep. 2011;34:1493–1498. doi: 10.5665/sleep.1384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petersen J.J., Paulitsch M.A., Guethlin C., Gensichen J., Jahn A. A survey on worries of pregnant women-testing the German version of the Cambridge Worry Scale. BMC Public Health. 2009;9(1):490–499. doi: 10.1186/1471-2458-9-490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preacher K.J., Curran P.J., Bauer D.J. Computational tools for probing interactions in multiple linear regression, multilevel modeling, and latent curve analysis. J. Educ. Behav. Stat. 2006;31(4):437–448. [Google Scholar]
- Qiu J., Shen B., Zhao M., Wang Z., Xie B., Xu Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen. Psychiatry. 2020;33(2) doi: 10.1136/gpsych-2020-100213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rees S., Channon S., Waters C.S. The impact of maternal prenatal and postnatal anxiety on children’s emotional problems: a systematic review. Eur. Child Adolesc. Psychiatry. 2019;28:257–280. doi: 10.1007/s00787-018-1173-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sani G., Janiri D., Di Nicola M., Janiri L., Ferretti S., Chieffo D. Psychiatry and Clinical Neurosciences; 2020. Mental health during and after the COVID-19 emergency in Italy. [DOI] [PubMed] [Google Scholar]
- Schumacker, R. E., & Lomax, R. G. (2010). A beginner's guide to structural equation modeling (third).
- Sedov I.D., Cameron E.E., Madigan S., Tomfohr-Madsen L.M. Sleep quality during pregnancy: a meta-analysis. Sleep Med. Rev. 2018;38:168–176. doi: 10.1016/j.smrv.2017.06.005. [DOI] [PubMed] [Google Scholar]
- Sedov I., Madsen J.W., Goodman S.H., Tomfohr-Madsen L.M. Couples’ treatment preferences for insomnia experienced during pregnancy. Families, Syst. Health. 2019;37(1):46–55. doi: 10.1037/fsh0000391. [DOI] [PubMed] [Google Scholar]
- Simcock G., Kildea S., Elgbeili G., Laplante D.P., Cobham V., King S. Prenatal maternal stress shapes children’s theory of mind: the QF2011 Queensland Flood Study. J. Dev. Origins Health Dis. 2017;8(4):483–492. doi: 10.1017/S2040174417000186. [DOI] [PubMed] [Google Scholar]
- Skouteris H., Germano C., Wertheim E.H., Paxton S.J., Milgrom J. Sleep quality and depression during pregnancy: a prospective study. J. Sleep Res. 2008;17:217–220. doi: 10.1111/j.1365-2869.2008.00655.x. [DOI] [PubMed] [Google Scholar]
- Statham H., Green J.M., Kafetsios K. Who worries that something might be wrong with the baby? A prospective study of 1072 pregnant women. Birth. 1997;24(4):223–233. doi: 10.1111/j.1523-536x.1997.tb00595.x. [DOI] [PubMed] [Google Scholar]
- Swanson L.M., Pickett S.M., Flynn H., Armitage R. Relationships among depression, anxiety, and insomnia symptoms in perinatal women seeking mental health treatment. J. Women’s Health. 2011;20(4):553–558. doi: 10.1089/jwh.2010.2371. [DOI] [PubMed] [Google Scholar]
- Tanhan A., Yavuz K.F., Young J.S., Nalbant A., Arslan G., Yıldırım M., Çiçek İ. A proposed framework based on literature review of online contextual mental health services to enhance wellbeing and address psychopathology during COVID-19. Electr. J. Gen. Med. 2020;17(6):em254. [Google Scholar]
- Tomfohr L.M., Buliga E., Letourneau N.L., Campbell T.S., Giesbrecht G.F. Trajectories of sleep quality and associations with mood during the perinatal period. Sleep. 2015;38:1237–1245. doi: 10.5665/sleep.4900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Voitsidis P., Gliatas I., Bairachtari V., Papadopoulou K., Papageorgiou G., Parlapani E., Diakogiannis I. Insomnia during the COVID-19 pandemic in a Greek population. Psychiatry Res. 2020 doi: 10.1016/j.psychres.2020.113076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiao H., Zhang Y., Kong D., Li S., Yang N. The effects of social support on sleep quality of medical staff treating patients with coronavirus disease 2019 (COVID-19. Med. Sci. Monit. 2020;26 doi: 10.12659/MSM.923549. January and February 2020 in China. e923549-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S., Ho R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Public Health. 2020;17(5):1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woody C.A., Ferrari A.J., Siskind D.J., Whiteford H.A., Harris M.G. A systematic review and meta-regression of the prevalence and incidence of perinatal depression. J. Affect. Disord. 2017;219:86–92. doi: 10.1016/j.jad.2017.05.003. [DOI] [PubMed] [Google Scholar]
- Wu Y., Zhang C., Liu H., Duan C., Li C., Fan J., Guo Y. Perinatal depressive and anxiety symptoms of pregnant women along with COVID-19 outbreak in China. Am. J. Obstet. Gynecol. 2020;240 doi: 10.1016/j.ajog.2020.05.009. e1-240.e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimet G.D., Dahlem N.W., Zimet S.G., Farley G.K. The multidimensional scale of perceived social support. J. Pers. Assess. 1988;52(1):30–41. doi: 10.1080/00223891.1990.9674095. [DOI] [PubMed] [Google Scholar]