Corresponding Author
Key Words: COVID-19 (coronavirus), fibrinolysis, medical decision-making, percutaneous coronary intervention, ST-segment elevation myocardial infarction
In 2020, the global pandemic of coronavirus disease-2019 (COVID-19) has resulted in a substantial increase in mortality arising from acute respiratory distress syndrome and fatal complications, thus dramatically disturbing the society and all segments of the global population (1). Although the immediate threat posed by COVID-19 is the morbidity and mortality related to the viral infection, COVID-19 also carries another significant threat: the shift of medical attention and resources away from other acute diseases including acute coronary syndromes (ACS). The COVID-19 pandemic has necessitated an unprecedented reorganization and rapid reshuffling of emergency care facilities worldwide to accommodate the increased clinical workload. Countries severely affected by COVID-19 have reported notable reductions in the number of patients presenting to the emergency department due to ACS and significant decreases in the number of cardiac procedures including primary percutaneous coronary intervention (PCI) (2), as well as dramatic changes in reperfusion strategies (3). Yet, the status, nature, and true impact of the COVID-19 pandemic on the treatment and outcome of patients with ST-segment elevation myocardial infarction (STEMI) undergoing primary PCI are still a matter of debate.
In this issue of the Journal, De Luca et al. (4) report the incidence of primary PCI, delayed treatment, and in-hospital mortality in patients presenting with STEMI in high-volume PCI centers in Europe (77 centers in 9 countries). Through a retrospective evaluation of the registry, the authors evaluated 2,956 patients who underwent primary PCI for STEMI between March 1 and April 30 in 2020 and compared them with 3,653 patients with STEMI treated during the same period in 2019. The number of patients with STEMI had significantly dropped by 18.9% in 2020, with a significant heterogeneity present among the centers. Specifically, the decrease in the number of hospitalizations for STEMI was significantly associated with the presence of hypertension. Interestingly, the reduction in the number of STEMI procedures was not significantly associated with the number of COVID-19 cases and COVID-19–related deaths. With respect to the primary PCI characteristics, a significantly longer total ischemia time and door-to-balloon time were observed during the COVID-19 pandemic compared with the previous year (approximately 34% increase of ischemia time longer than 12 h and 17% increase of door-to-balloon time longer than 30 min). In-hospital mortality had also significantly increased by approximately 40% compared with 2019.
Some findings of the current study need to be highlighted, whereas other parts call for cautious interpretation. First, a unique strength of this international study is that it demonstrated significantly heterogeneous practices in primary PCI for STEMI according to each country and hospital. The exact reasons for such discrepancies in the responses for primary PCI are unknown, and the clinical implications of such heterogeneity for the next wave of the pandemic should be further determined. Second, considering that there is no clinical evidence of harm associated with the use of specific classes of antihypertensive medications such as angiotensin-converting enzyme inhibitors and angiotensin-receptor blockers in the risk of COVID-19 (5), the subgroup finding on the more significant reduction of primary PCI in hypertensive patients might be due to chance. A similar trend was also observed in nonhypertensive patients, albeit to a lesser degree. Last, the dramatic reduction in the number of patients with STEMI was not significantly related to the incidence of COVID-19 and related mortality. This finding is unusual and may have been influenced by several unmeasured confounders (e.g., out-of-hospital cardiac arrest, pre-hospital death, indirect effects of lockdown, disparities in health care services or facilities, and adjustments in specific COVID-19 management) (6). Also, the incidence of COVID-19 is highly heterogeneous as it depends on the numbers of COVID-19 testing and local strategy; therefore, the incidence and mortality of COVID-19 in some areas might have been underestimated.
Prior studies showed similar findings. An Italian multicenter study (7) reported a 48.4% reduction in the admission for acute myocardial infarction (AMI) and more than 3 times-increase in STEMI fatality compared with the same period in 2019. Similar findings were observed in other European countries: the number of hospital admissions for AMI declined by 40% in England (2) and Austria (8) during the early period of the pandemic, and this trend coincided with the peaks of COVID-19 and the lockdown. Similarly, in 9 high-volume centers in the United States, a time-corrected model showed a 38% decrease in the number of STEMI activation during the spread of COVID-19 (9). Moreover, in Northern California, the incidence of hospitalization for AMI decreased by 48% during the COVID-19 pandemic, especially after the implementation of the shelter-in-place order; the decreases in hospitalization were similar among patients with non–ST-segment elevation MI and those with STEMI (10).
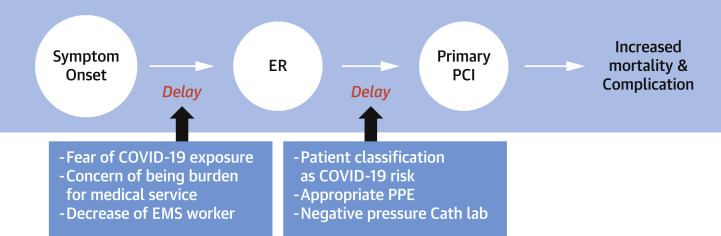
The key finding of the current study is that the spread of COVID-19 was directly related to a substantial decrease in the number of patients with STEMI undergoing primary PCI, a significantly longer ischemia time, a higher rate of late presentation, and delayed door-to-balloon time. Several factors might contribute to these phenomena. In the COVID-19 pandemic, strict social containment measures and health care policies have been adopted worldwide, and the daily media broadcastings are spreading concerns on the paucity of medical capacity with regard to medical staff and equipment for critically ill patients with COVID-19. Thus, patients with suspected ACS may avoid hospital visits because of fear of COVID-19 infection in-hospital and to avoid medical burden (11). Also, even after the STEMI patients arrive at the emergency room, time delays to receiving primary PCI are unavoidable. Medical attention and stringent screening have been primarily focused on the avoiding the nosocomial spread of COVID-19 rather than maintaining proper management of STEMI. Thus, when treating patients with high risks of COVID-19, all participating staffs should wear the highest-degree personal protective equipment and perform primary PCI in the facilities with negative-pressure air conditioning. These multifactorial factors collectively lead to longer time delays in the diagnosis and treatment of STEMI and impose a detrimental effect on providing optimal myocardial salvage, thus resulting in increased STEMI-related complications and mortality (Figure 1 ).
Figure 1.
Possible Causes for the Delays in Primary PCI in Patients With STEMI During the COVID-19 Pandemic
Multifactorial factors are likely associated with the significant time delays in the diagnosis and treatment of ST-segment elevation myocardial infarction (STEMI), which subsequently results in increases in complications and mortality. Each circle represents a step from symptom onset to primary percutaneous coronary intervention (PCI), and each box represents the possible causes of time delay in each step. First, patients with suspected STEMI may avoid hospital visits owing to the fear of in-hospital exposure to coronavirus disease-2019 (COVID-19), avoidance of medical burden, and a lack of emergency medical service (EMS) workers for patient transfer, through which time delay between initial symptom onset and emergency room (ER) visit occurs. Second, even after arriving at the ER, patients with STEMI may inevitably experience further time delay due to the COVID-19 screening process and the mandatory requirement of the highest-degree personal protective equipment (PPE) and facilities with negative-pressure air conditioning for performing primary PCI in patients with high risks for COVID-19. Cath lab = catheterization laboratory.
Many countries are now experiencing second waves of the COVID-19 outbreak, in which optimal and well-timed STEMI management seems like a candle flickering in the wind. Which strategies can be helpful for adequately managing patients with STEMI during the COVID-19 pandemic? First, health care authorities, supported by scientific societies, must adapt the existing guidance for the public and health care professionals and highlight the importance of recognition and response to the characteristic symptoms of STEMI. Vigorous action also should be taken to prevent patients from neglecting the characteristic symptoms of AMI. An encouraging report from England showed that the decline in hospital admission for AMI was reversed following a publicity campaign from a scientific society (2). Second, the strategy for primary PCI should be reorganized to cope with the considerable safety concerns ranging from initial risk evaluation to procuring a safer setting for primary PCI. Also, health care workers should receive optimal training to be accustomed to the new strategies in the COVID-19 pandemic.
In conclusion, the COVID-19 pandemic is continuing to present an unprecedented challenge for health care systems and is negatively affecting timely dependent STEMI management. Although primary PCI remains the preferred reperfusion strategy if it could be provided in a timely manner, an unconditional application of primary PCI for all patients with STEMI may not be feasible during the current pandemic. Therefore, shifting the balance in operations in favor of fibrinolytic strategies from primary PCI may be considered in areas with significant COVID-19 outbreaks, and it could be timely modified according to the status of COVID-19.
Author Relationship With Industry
The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Footnotes
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the JACCauthor instructions page.
References
- 1.Banerjee A., Pasea L., Harris S. Estimating excess 1-year mortality associated with the COVID-19 pandemic according to underlying conditions and age: a population-based cohort study. Lancet. 2020;395:1715–1725. doi: 10.1016/S0140-6736(20)30854-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mafham M.M., Spata E., Goldacre R. COVID-19 pandemic and admission rates for and management of acute coronary syndromes in England. Lancet. 2020;396:381–389. doi: 10.1016/S0140-6736(20)31356-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Xiang D., Xiang X., Zhang W. Management and outcomes of patients with STEMI during the COVID-19 pandemic in China. J Am Coll Cardiol. 2020;76:1318–1324. doi: 10.1016/j.jacc.2020.06.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.De Luca G., Verdoia M., Cercek M. Impact of COVID-19 pandemic on mechanical reperfusion for patients with STEMI. J Am Coll Cardiol. 2020;76:2321–2330. doi: 10.1016/j.jacc.2020.09.546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Reynolds H.R., Adhikari S., Pulgarin C. Renin-angiotensin-aldosterone system inhibitors and risk of Covid-19. N Engl J Med. 2020;382:2441–2448. doi: 10.1056/NEJMoa2008975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Baldi E., Sechi G.M., Mare C. Out-of-hospital cardiac arrest during the Covid-19 outbreak in Italy. N Engl J Med. 2020;383:496–498. doi: 10.1056/NEJMc2010418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.De Rosa S., Spaccarotella C., Basso C. Reduction of hospitalizations for myocardial infarction in Italy in the COVID-19 era. Eur Heart J. 2020;41:2083–2088. doi: 10.1093/eurheartj/ehaa409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Metzler B., Siostrzonek P., Binder R.K., Bauer A., Reinstadler S.J. Decline of acute coronary syndrome admissions in Austria since the outbreak of COVID-19: the pandemic response causes cardiac collateral damage. Eur Heart J. 2020;41:1852–1853. doi: 10.1093/eurheartj/ehaa314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Garcia S., Albaghdadi M.S., Meraj P.M. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic. J Am Coll Cardiol. 2020;75:2871–2872. doi: 10.1016/j.jacc.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Solomon M.D., McNulty E.J., Rana J.S. The Covid-19 pandemic and the incidence of acute myocardial infarction. N Engl J Med. 2020;383:691–693. doi: 10.1056/NEJMc2015630. [DOI] [PubMed] [Google Scholar]
- 11.De Filippo O., D'Ascenzo F., Angelini F. Reduced rate of hospital admissions for ACS during Covid-19 outbreak in Northern Italy. N Engl J Med. 2020;383:88–89. doi: 10.1056/NEJMc2009166. [DOI] [PMC free article] [PubMed] [Google Scholar]