Abstract
Emotional eating, generally defined as (over)-eating in response to negative emotions, has been associated with poor physical and psychological outcomes. During a time of heightened negative affect, it is important to understand the impact of the COVID-19 pandemic and associated lockdown measures on eating behaviours, and further elucidate the ways in which emotional eating is related to emotion dysregulation and impaired abilities to identify emotions (i.e. alexithymia). The aims of this study were to explore perceived changes in eating behaviours in relation to self-reported negative affect during the pandemic and to examine direct and indirect effects of alexithymia on emotional eating. An online questionnaire measured these constructs in the general population of the United Kingdom (n = 136). Findings demonstrated that those who reported changes to their eating behaviours during the pandemic also reported greater levels of depression during the same time frame. Mediation analyses revealed that difficulties identifying and describing feelings both predicted emotional eating indirectly via emotion dysregulation. Findings contribute to the understanding of the mechanisms underpinning the relationship between alexithymia and emotional eating and describe changes to eating behaviours during COVID-19. We discuss how these findings should be applied, and recommendations for future research.
Keywords: Alexithymia, Emotion dysregulation, Emotional eating, Pandemic, Mediation
1. Introduction
The novel coronavirus disease (COVID-19) is an infectious respiratory virus, declared a global pandemic on 11th March 2020 (World Health Organization, 2020). As a result of implemented lockdowns to prevent transmission, movements and interactions have been limited with significant impacts upon daily routines (Brooks et al., 2020; Lima et al., 2020). Government guidance in the United Kingdom included explicit recommendations to avoid face-to-face interactions and gatherings with friends and family (Public Health England, 2020). This social distancing is a key public health measure to prevent transmission of COVID-19, but may pose its own significant mental health and wellbeing risks (Lades, Laffan, Daly, & Delaney, 2020). A panel study collecting weekly data of over 90,000 adults found that 35% of respondents reported their recent mental health to be worse than compared to usual before lockdown (Fancourt, Bu, Mak, & Steptoe, 2020b). Previous research has demonstrated that disordered eating behaviour in the general population can be triggered by feelings of boredom and loneliness (Bruce & Agras, 1992), and distress following a disaster (Kuijer & Boyce, 2012). Research exploring how COVID-19 lockdown measures impact on the general population found a third of individuals with no history of eating disorders reported increased binge eating behaviours compared to before the pandemic (Phillipou et al., 2020), and 17% of adults in the United Kingdom reported eating more food than usual, while 23% reported eating less healthfully than usual (Fancourt, Bu, Mak, & Steptoe, 2020a).
These changes may reflect emotional eating behaviours, due to lockdown measures eliciting feelings of isolation and distress (Brooks et al., 2020). Cross-sectional studies conducted during the primary lockdown periods in various countries have explored self-reported emotional eating. One study compared samples in Spain and Greece, finding that despite the disparity in severity of lockdown measures, both groups reported greater emotional eating than pre-pandemic community samples, with no significant difference in emotional eating levels between groups in each country (Papandreou, Arija, Aretouli, Tsilidis, & Bulló, 2020). An Italian study found that half of the respondents reported using food as a means of comfort in response to anxious states, increasing their food intake to feel better, and feeling anxious due to their current eating habits; within the sample, female respondents declared themselves to be more prone to these described behaviours (Di Renzo et al., 2020). This was also demonstrated in another Italian study, which found half of their sample felt they had modified their dietary habits during the lockdown, with 42% attributing an increase in food intake to higher anxiety levels (Scarmozzino & Visioli, 2020). An American study reported that perceived stress was significantly correlated with emotional eating during the pandemic, and that self-reported emotional eating mediated identified associations between perceived stress and food choice motives of mood, convenience, sensory appeal, price and familiarity (Shen, Long, Shih, & Ludy, 2020). It also discussed the role of comfort food during previous crises, with eating playing a significant role in alleviating stress and improving mood (see Shen et al., 2020). Situational explanations for increased emotional eating during this time may also include the fact that it is found to be more frequent when individuals are alone and eating at home (Baumeister, Heatherton, & Tice, 1994).
Emotional eating, as “the tendency to overeat in response to negative emotions” (van Strien et al., 2007, p. 106) is considered an atypical stress response, compared to the typical response of not eating (Gold & Chrousos, 2002). Emotional eating may be problematic for physical health, as negative affect and distress are associated with an increased quantity of consumed snacks (Oliver & Wardle, 1999; O'Connor & O'Connor, 2004; van Strien, Herman, & Verheijden, 2012) and less healthful choices such as opting for sweet and fatty foods (Oliver, Wardle, & Gibson, 2000; Wallis & Hetherington, 2009; Zellner et al., 2006). Psychological implications of emotional eating are reported from findings which suggest that eating in response to anxiety, anger, boredom and particularly depression was found to be associated with poorer wellbeing, greater eating disorder symptomatology and difficulties in emotion regulation (Braden, Musher-eizenman, Watford, & Emley, 2018; Gelibter & Aversa, 2003; Meule, Reichenberger, & Blechert, 2018; Nolan et al., 2010). Overeating in response to positive emotions has also been observed (Cardi, Leppanen, & Treasure, 2015; Evers et al., 2013), but this was not found to be related to the poorer physical and psychological outcomes implicated in negative emotional eating and may instead represent a functional, healthy eating style (Braden et al., 2018; Gelibter & Aversa, 2003; Meule et al., 2018; Nolan, Halperin, & Geliebter, 2010). Eating in response to negative and positive emotions may represent different constructs (van Strien et al., 2013), and predict overeating via different mechanisms (Sultson, Kukk, & Akkermann, 2017). There is a need to understand the mechanisms underlying emotional eating, particularly the atypical and potentially problematic response of eating in response to negative emotions.
Theories of emotional eating include the psychosomatic theory which posits that poor interoceptive awareness relates to an inability to recognise hunger and satiety signals and distinguish these from other bodily sensations (Bruch, 1973), resulting in eating in response to sensations such as emotional arousal. The homeostatic theory of obesity posits a circle of discontent involving increased body dissatisfaction, negative affect, and subsequent consumption of energy-dense foods (Marks, 2015). Research demonstrated that negative affect is associated with emotional eating urges, which in turn predict worsened negative affect (Haedt-Matt et al., 2014), partially reflecting this reciprocal model. Emotional eating has been related to an increase in sweet, fatty foods in response to stress (Oliver et al., 2000), although experimental research pinpointed increased food intake only in response to ego-threat stressors (Wallis & Hetherington, 2004), highlighting that emotional eating may function to alleviate negative self-focused emotions (Adam & Epel, 2007). This aligns with escape theory that describes eating to avoid aversive self-awareness and emotional distress (Heatherton & Baumeister, 1991). Integral to all theories of emotional eating is the role of emotion dysregulation, or difficulties in emotion regulation; these terms are used interchangeably. Gratz and Roemer (2004) proposed a model of emotion regulation which describes a multidimensional construct involving: the awareness, understanding and acceptance of emotions; the flexible use of non-avoidant, situationally appropriate strategies to modulate intensity and duration of emotion responses to meet desired goals and situational demands; and, the willingness to experience negative emotions. The relative absence of any of these abilities indicate difficulties in emotion regulation. Maladaptive emotion regulation, such as persistent avoidance or control of emotion (Gratz, Dixon, Kiel, & Tull, 2018), is thought to function to regulate emotions when putatively adaptive strategies are unavailable (Gratz, 2003). The role of emotion dysregulation is supported in loss-of-control eating (Kenardy, Arnow, & Agras, 1996) and disordered eating (Lavender & Anderson, 2010; Whiteside et al., 2007), with greater reports of bingeing and purging behaviours accompanying distress (Racine & Wildes, 2013). Emotion dysregulation has been identified as a moderator in the relationship between emotional eating and disordered eating, with difficulties in emotion regulation strengthening the relationship between negative emotional eating and disordered eating (Barnhart, Braden, & Price, 2021), and not positive emotional eating.
Alexithymia is a personality trait present in around 10% of the general population (Honkalampi et al., 2017), which conceptually overlaps with both emotion dysregulation and components of interoception (van Strien & Ouwens, 2007; Zamariola, Vlemincx, Luminet, & Corneille, 2018). Salient features are: (a) difficulty identifying feelings and distinguishing these from other bodily sensations; (b) difficulty describing feelings to others; (c) constricted imaginal processes; and, (d) a stimulus-bound, externally-oriented cognitive style (Taylor & Bagby, 2000). The impaired ability to distinguish feelings from other bodily sensations is conceptually similar to poor interoception and a diminished recognition and interpretation of bodily sensations (Murphy, Brewer, Hobson, Catmur, & Bird, 2018), as identified in the psychosomatic theory of emotional eating (Bruch, 1973). A recent review proposed alexithymia and emotion dysregulation among possible mechanisms of emotional eating (van Strien, 2018), yet the relationship between alexithymia and emotional eating has not been extensively researched. Significant positive relationships have been identified between these constructs, more specifically between emotional eating and the affective characteristics of difficulty identifying and describing feelings (Larsen, van Strien, Eisinga, & Engels, 2006; Ouwens, van Strien, & van Leeuwe, 2009; Pink, Lee, Price, & Williams, 2019). Emotional eating was found to be significantly predicted by difficulty identifying feelings in individuals with binge eating disorder (Pinaquy, Chabrol, Simon, Louvet, & Barbe, 2003), and experimental findings with student samples suggest those with difficulties identifying and describing their feelings showed more stress-induced eating (van Strien & Ouwens, 2007). Proposed pathways between these variables include the reported significant (positive) indirect effect of depression on emotional eating via difficulty identifying feelings (Ouwens et al., 2009); however, alexithymia as a relatively stable personality trait (Norman, Marzano, Coulson, & Oskis, 2019) may not make a suitable mediating variable for informing interventions to assist with emotional eating (Fiedler, Harris, & Schott, 2018). Pink et al. (2019) aimed to understand the role of alexithymia as an explanatory mechanism in emotional eating to explain body mass index (BMI) variability. The model identified a significant (positive) indirect effect of affective characteristics of alexithymia via negative affect (measured as anxiety), and via negative urgency and emotional eating, in a student sample. A self-replication study within a general population sample demonstrated that negative affect (as measured by both depression and anxiety) played roles in the indirect effect of alexithymia on BMI (Pink et al., 2019). Their findings also indicated that the characteristic of difficulty identifying feelings could be a key facet of alexithymia in relation to emotional eating. This model did not provide decisive mechanisms that underpin the relationship between alexithymia and emotional eating in the general population, but has methodological strengths stemming from its use of a self-replication study.
How alexithymia relates to emotional eating remains unclear. Two theoretical mechanisms have been proposed: (1) alexithymia as a deficit of interoception results in insensitivity to satiety cues, thus eating in response to bodily sensations that are not hunger such as emotional arousal; and (2) eating to regulate negative affective states common in alexithymia, thus emotional eating represents maladaptive regulation of those emotions. These mechanisms are not necessarily mutually exclusive (Lyvers, Brown, & Thorberg, 2019), and logically may both be supported through learning to identify and respond to emotions adaptively. The ability to identify and understand emotions is a necessary prerequisite to developing adaptive emotion regulation skills (Vine & Aldao, 2014). It has been suggested that teaching emotion regulation skills could result in decreased emotional eating (Roosen, Safer, Adler, Cebolla, & van Strien, 2012); however, for individuals with higher levels of affective alexithymic characteristics and associated deficits, focusing on these aspects must precede targeting emotion.
The relationship between alexithymia and eating behaviours in response to emotion is logical, as regulation of emotions first requires a level of emotion processing. Individuals with alexithymia experience an impaired ability to process emotions at an affective and cognitive level, captured by the characteristics of alexithymia (Goerlich, 2018). Therefore, emotion dysregulation may underpin the relationship between alexithymia and emotional eating; individuals with higher levels of alexithymia experience problems with processing and subsequently regulating emotions (Barrett, Gross, Christensen, & Benvenuto, 2001), increasing the risk of developing conditions characterised by (Goerlich, 2018) or behaviours associated with emotion dysregulation. It is important to examine alexithymia and emotion dysregulation to understand the relationship between them, and how they relate independently and synergistically with other constructs such as emotional eating. There is growing consensus for conceptualising alexithymia as a personality trait with relative, rather than absolute stability. This means whilst levels can fluctuate, individual differences remain similar over time (Norman et al., 2019), and it is unlikely to be affected through interventions (Iancu, Cohen, Yehuda, & Kotler, 2006; Schmidt, Jiwany, & Treasure, 1993). Therefore, theoretically it would have temporal precedence and as such should be a predictor when examining the direct and indirect effects on targetable skills such as emotion regulation and behaviours such as emotional eating (Fiedler et al., 2018).
There is a need to understand how people respond to, and cope with, the threat of a global pandemic (Arden & Chilcot, 2020). As emotional eating is underpinned by maladaptively regulating emotions, exhibited behaviours may differ during these times which may elicit greater feelings of isolation and distress in the general population (Brooks et al., 2020). Although a level of stress is essentially unavoidable when facing a pandemic, wellbeing remains key to supporting and facilitating good health (Vieira, Franco, Restrepo, & Abel, 2020) and preventing negative effects on psychological wellbeing should be considered a marker of a successful lockdown to support public health (Brooks et al., 2020). Therefore, there is a need to provide understanding and information to individuals, communities, and healthcare providers to support healthy behaviours during lockdowns (Balanzá–Martínez, Atienza–Carbonell, Kapczinski, & De Boni, 2020). Alexithymia is typically a risk factor for poorer outcomes in therapeutic eating interventions (Pinna, Sanna, & Carpiniello, 2015), and specifically, the characteristic of difficulty identifying feelings has been found to be a significant negative predictor of treatment outcomes (Speranza, Loas, Wallier, & Corcos, 2007). Exploring specific mechanisms of emotional eating in individuals with greater levels of alexithymia is important for supporting these individuals.
There were two aims of the current study. Firstly, to explore perceived changes in eating behaviour and self-reported negative affect during the COVID-19 lockdown, to understand the impact on individuals within the general population of the United Kingdom. The second aim of the study was to examine the direct and indirect effects of affective characteristics of alexithymia on emotional eating via emotion dysregulation, to expand upon previously proposed models and understand the mechanisms by which alexithymia may relate to emotional eating. It is predicted that the affective characteristics of alexithymia will predict emotion dysregulation, which will in turn predict emotional eating, as reported during the COVID-19 pandemic.
2. Methods
2.1. Participants
One hundred and fifty-eight participants were recruited through opportunity sampling using adverts on social media sites and the research participation platform, Prolific. Individuals with a history of eating, mood, addictive, or substance use disorders were excluded from taking part.
2.2. Measures
2.2.1. Demographics
Participants provided their age, gender, relationship status, ethnicity and educational level. They also provided anthropometric measurements (height and weight) and indicated their dieting status.
2.2.2. COVID-19 questions
Participants reported to what extent they were following guidance regarding social distancing, and how their general eating behaviours differed compared to usual before COVID-19.
2.2.3. Negative affect
The Depression, Anxiety and Stress Scale (DASS-21; Lovibond & Lovibond, 1995) measures self-reported negative emotional states over the past week. Three subscales comprising seven items measure depression (e.g. “I couldn't seem to experience any positive feeling at all”), anxiety (e.g. “I was worried about situations in which I might panic and make a fool of myself”) and stress (e.g. “I tended to overreact to situations”). Items are scored on a four-point Likert scale, indicating how much the statements applied over the last week (0 = Did not apply to me at all; 3 = Applied to me very much, or most of the time). Each scale can be scored independently by doubling the sum of its items or combined to provide a score of a higher-order general distress factor. Higher scores indicate a greater presence of a negative emotional state. The DASS-21 has demonstrated strong convergent and discriminant validity with other measures of depression and anxiety symptoms (e.g. Norton, 2007). Cronbach's alpha values indicate high internal consistency for each of the subscales: depression (α = 0.91), anxiety (α = 0.82), and stress (α = 0.86), as well as the higher-order general distress factor (α = 0.93).
2.2.4. Alexithymia
The Toronto Alexithymia Scale (TAS-20; Bagby, Parker, & Taylor, 1994) is a 20-item self-report scale measuring three facets of alexithymia: difficulty identifying feelings (DIF; e.g. “I am often confused about what I feel exactly”), difficulty describing feelings (DDF; e.g. “It is difficult for me to find the appropriate words for my feelings”), and externally-oriented thinking style (EOT; e.g. “I would rather talk to people about their daily routines than their feelings”). Participants use a five-point Likert scale to indicate how much they agree with each item (1 = strongly disagree; 5 = strongly agree). Summed scores of each subscale can be used independently or combined to create a global TAS-20 score. Higher scores indicate a greater presence of alexithymic characteristics. For research purposes, cut-offs are provided with global scores >60 indicating the presence of alexithymia. The TAS-20 is valid across situations and populations (Bagby, Parker, & Taylor, 2020), and valid for administering as an online version (Bagby, Ayearst, Morariu, Watters, & Taylor, 2014). Internal consistency of the scale was found to be high in the present study (α = 0.85), as were the DIF (α = 0.85) and DDF (α = 0.73) subscales. Consistent with previous research (Larsen, van Strien, Eisinga, & Engels, 2006; Pinaquy et al., 2003; Pink et al., 2019), internal consistency of the EOT subscale was much lower (α = 0.59).
2.2.5. Emotion dysregulation
The short-form version of the Difficulties in Emotion Regulation Scale (DERS-SF; Kaufman et al., 2016) comprises 18 items which measure six facets of emotion dysregulation: non-acceptance of emotional responses (e.g. “When I'm upset, I become irritated at myself for feeling that way”), difficulties in directing goal-directed behaviour (e.g. “When I'm upset, I have difficulty concentrating”), impulse control difficulties (e.g. “When I'm upset, I lose control over my behaviour”), lack of emotional awareness (e.g. “I pay attention to how I feel”), limited access to emotion regulation strategies (e.g. “When I'm upset, I believe there is nothing I can do to make myself feel better”), and lack of emotional clarity (e.g. “I have no idea how I am feeling”). Participants respond using a five-point scale to indicate how often the described items happen (1 = Almost never [0–10%]; 5 = Almost always [91–100%]). Responses can be scored using sums, with higher scores reflecting greater difficulties in emotion regulation, used continuously. The DERS-SF maintains the excellent psychometric properties of the original 36-item version developed by Gratz and Roemer (2004), and as a streamlined version is better suited to minimise fatigue (Kaufman et al., 2016). Internal consistency for the total score was high (α = 0.90), but as demonstrated in previous findings (Hallion, Steinman, Tolin, & Diefenbach, 2018), the DERS-SF is psychometrically stronger after removing the awareness subscale (α = 0.91).
2.2.6. Emotional eating urges
The Emotional Eating Scale (EES; Arnow, Kenardy, & Agras, 1995) assesses participants' reported urge to eat in response to 25 negative emotions. There are four emotional eating subscales: depression (e.g. “lonely”), anxiety (e.g. “worried”), anger/frustration (e.g. “furious”) and somatic (e.g. “jittery”) (Goldbacher et al., 2012). Participants indicate their urge to eat using a five-point scale (0 = no desire to eat; 4 = an overwhelming urge to eat), with higher summed scores indicating a greater urge to eat in response to emotions. The EES has been validated in nonclinical populations (Waller & Osman, 1998), and its internal consistency in the present study was high (α = 0.94), with acceptable Cronbach's alpha values for each of the subscales (α > 0.73 for all).
2.2.7. Emotional eating behaviours
The Salzburg Emotional Eating Scale (SEES; Meule et al., 2018) assesses reported eating behaviour, rather than urges, in response to 20 positive and negative emotions. Four subscales measure happiness (e.g. “When I am cheerful”), sadness (e.g. “When I feel lonely”), anger (e.g. “When I am irritated”), and anxiety (e.g. “When I am nervous”). Participants respond using a five-point scale to indicate whether they eat more or less in response to each emotion (1 = I eat much less than usual; 5 = I eat much more than usual). Mean scores are computed for each subscale which indicate whether individuals eat less when experiencing these emotions (scores < 3), eat the same amount (scores = 3), or eat more (scores > 3). There is preliminary support for the validity of the SEES (Meule et al., 2018), but limitations of the self-report nature are strongly acknowledged by authors. In the present study, Cronbach's alpha values indicate internal consistency was high for each of the subscales: happiness (α = 0.87), sadness (α = 0.83), anger (α = 0.84), and anxiety (α = 0.92).
2.3. Procedure
Ethical approval was obtained from the Faculty Academics Ethics Committee of a university in the West Midlands, United Kingdom (approval code 7327/Am/2020/Jul/BLSSFAEC), and this study was conducted in accordance with the Declaration of Helsinki. Participants recruited via Prolific (n = 133) received £2.15 remuneration, with no other financial or material incentives for any participants.
The study comprised a questionnaire survey which was completed online via the survey hosting website Qualtrics. Data collection took place in mid-July 2020, during the gradual easing of the initial lockdown measures across devolved nations of the United Kingdom. Participants were presented with information about the study before indicating their consent to take part. A battery of measures was presented, with the order of scales randomised to control for order and fatigue effects. Participants completed questions pertaining to their lives and behaviours during the pandemic. After completing the scales, participants completed questions pertaining to demographic information, which took place at the end of the questionnaire to minimise effects of fatigue on scale completion. The titles of each scale were omitted to reduce response bias. Upon completion, participants were presented with a debrief information page, outlining the purpose of the study.
2.4. Data analysis
Data were analysed using IBM SPSS Statistics 25.0 and PROCESS v3.5 (Hayes, 2017). Preliminary analyses examined for outliers and the assumptions of normality were met. T tests were employed to test for differences between those who reported changes in their eating behaviours over the previous week during COVID-19, and those who did not, to explore the first aim of the study. Pearson correlations were used to investigate the associations between measured continuous variables. PROCESS was used to test theorised models of the second aim, using a regression-based approach to mediation to explore the direct and indirect effects of alexithymia on emotional eating with emotion dysregulation a potential mediator. In this approach, effects are assessed with bias-corrected accelerated bootstrap confidence intervals (CI) that are considered significant when the upper and lower bound of the bias-corrected 95% CI do not span zero. Bootstrapping with 5000 samples was used, a method which is effective with smaller samples and the least vulnerable to Type 1 errors (Preacher & Hayes, 2008).
Gender, age and BMI have previously been associated with alexithymia and emotional eating (Geliebter & Aversa, 2003; Larsen et al., 2006; Mattila, Salminen, Nummi, & Joukamaa, 2006) so these were controlled for in all models alongside self-reported change in eaten amounts. Affective characteristics of alexithymia (DIF and DDF) were entered as predictor variables. Emotional eating urges as measured by EES total score, and emotional eating behaviours as measured by SEES subscales were entered as outcome variables. Emotion dysregulation was represented by DERS-SF total scores, omitting the awareness scale in all analyses.
3. Results
3.1. Participant characteristics
Twenty-two participants were discounted in the final analyses due to the provision of inaccurate data, or due to reporting height and weight values which may indicate potential eating disorder history (exclusion of BMI outside of 18.5 kg/m2 to 50 kg/m2 range, classifications of underweight and super obesity). The final sample of 136 participants was 64.7% female (34.6% male, 0.7% preferred not to disclose), with a mean age of 32 years (SD = 11.88; range = 18–72 years). The sample was 83.1% White (5.1% mixed/multiple ethnic groups, 4.4% Asian, 3.7% Black, 3.7% other ethnic groups) with the majority of individuals having completed a minimum of an undergraduate-level degree (61%). The majority of participants reported not currently dieting (82.4%), and the sample had a mean BMI of 26.21 kg/m2 (SD = 5.39; range = 18.55 to 47.47).
3.2. Descriptives
Mean total scores of continuous variables are presented in Table 1 . Levels of alexithymia were consistent with previously reported rates in general population samples (Pink et al., 2019; Salminen, Saarijärvi, Äärelä, Toikka, & Kauhanen, 1999) with 11.0% of participants (n = 15) scoring above categorical cut-offs indicating the presence of alexithymia. The presence of alexithymia was borderline in 27.2% of participants (n = 37) and there was an absence of alexithymia in 61.8% participants (n = 84).
Table 1.
Means and standard deviations of continuous variables.
| Measure | M | SD |
|---|---|---|
| DASS-21 | 31.98 | 24.79 |
| Depression | 11.57 | 10.42 |
| Anxiety | 6.41 | 7.36 |
| Stress | 12.29 | 8.97 |
| TAS-20 | ||
| Global score | 46.54 | 11.01 |
| DIF | 15.42 | 5.72 |
| DDF | 13.02 | 4.13 |
| EOT | 18.10 | 4.03 |
| DERS-SF | 36.38 | 11.05 |
| EES | 31.11 | 18.22 |
| SEES | ||
| Happiness | 2.94 | 0.52 |
| Sadness | 3.60 | 0.77 |
| Anxiety | 2.52 | 0.92 |
| Anger | 2.76 | 0.76 |
Note: DASS-21 = Depression, Anxiety and Stress Scale; TAS-20 = Toronto Alexithymia Scale; DIF = Difficulty identifying feelings; DDF = Difficulty describing feelings; EOT = Externally-oriented thinking; DERS-SF = Difficulties in Emotion Regulation short-form omitting the awareness subscale; EES = Emotional Eating Scale; SEES = Salzburg Emotional Eating Scale.
A majority of respondents showed “normal” levels of anxiety (64.7%) and stress (61.8%) over the previous week during COVID-19. Around half of respondents showed “normal” levels of depression (51.5%). A greater number of participants reported severe or extremely severe depression (19.1%) over the previous week during COVID-19, than severe or extremely severe anxiety (9.5%) or stress (9.6%).
Mean levels of self-reported emotional eating urges as measured with the EES were lower than that reported in previous research with a similar sample (Pink et al., 2019), with total scores around 20 points lower (out of a maximum score of 100). Mean levels of self-reported emotional eating behaviours as measured with the SEES were comparable to general population samples used for the development and preliminary validation of the scale (Meule et al., 2018).
3.3. Reported behaviours during the COVID-19 pandemic
Of the 136 participants, 5.9% reported living their life as normal compared to before the pandemic, 11.0% were completely isolating from other people, and 83.1% reported to adhering to Government guidance for social distancing.
A majority of participants (58.1%) reported no change in the amount of food they had eaten over the previous week compared to before COVID-19, whilst 16.2% reported eating less on average and 25.7% reported eating more. Those who reported a change in the amount they had eaten over the previous week also reported significantly more depression in the same time frame (M = 14.21; SD = 10.63), compared to those who had no change in their eating (M = 9.67 SD = 9.90), t (134) = 2.56, p = .012, with a medium effect size (d = 0.44). The group who reported a change in the amount they had eaten also reported significantly greater difficulties identifying feelings (M = 16.70; SD = 5.73), compared to those who reported no change (M = 14.49, SD = 5.57), t (134) = 2.25, p = .026, with a medium effect size (d = 0.39). There were no significant group differences for difficulties in emotion regulation; however, the group who had reported a change in the amount they had eaten over the previous week also reported greater scores on the ‘strategies’ subscale of emotion dysregulation, which approached significance. There were no differences for anxiety or stress reported over the past week when comparing these groups. Furthermore, those who reported a change in the amount they had eaten over the previous week also reported significantly greater emotional eating urges in response to depression as measured by the EES (M = 15.16; SD = 6.74), compared to those who reported no change in their eating (M = 12.24, SD = 7.80), t (134) = 2.28, p = .024, with a medium effect size (d = 0.40). In addition, those who reported a change also reported significantly greater emotional eating behaviours in response to sadness as measured by the SEES (M = 3.76; SD = 0.78), compared to those who reported no change (M = 3.49, SD = 0.75), t (134) = 2.06, p = .042, with a medium effect size (d = 0.35). These findings demonstrate associations between perceived change in eating behaviour with negative affect and reported emotional eating in response to negative emotion. Specific differences based on those who had reported eating more or less were not tested due to limited sample sizes in these groups.
Over half of respondents (53.7%) reported no change in the perceived healthfulness of the food they had consumed over the previous week compared to before COVID-19, whilst 27.9% reported eating less healthfully and 18.4% reported eating more healthfully. Those who reported eating more or less healthfully compared to usual did not report significant differences in the measured psychological variables (negative affect, alexithymia, or emotion dysregulation), nor in reported emotional eating urges or behaviour compared to those who reported no change in the healthfulness of the food consumed.
3.4. Correlation analyses
Pearson's correlations were conducted to explore the relationships between measured variables (see Table 2 for correlation matrix). Significant positive correlations were found between TAS-20 global scores and DERS-SF total scores (r = 0.616, p < .001), specifically with all DERS-SF subscales of non-acceptance (r = 0.466, p < .001), strategies (r = 0.483, p < .001), impulse (r = 0.436, p < .001), clarity (r = 0.678, p < .001) and goals (r = 0.347, p < .001). The DIF scale of the TAS reported significant positive correlations with the DERS-SF total scores (r = 0.687, p < .001), and again all subscales, non-acceptance (r = 0.455, p < .001), strategies (r = 0.582, p < .001), impulse (r = 0.505, p < .001), clarity (r = 0.708, p < .001) and goals (r = 0.438, p < .001). The DDF scale of the TAS reported significant positive correlations with the DERS-SF total scores (r = 0.553, p < .001), and again all subscales, non-acceptance (r = 0.483, p < .001), strategies (r = 0.425, p < .001), impulse (r = 0.317, p < .001, clarity (r = 0.652, p < .001) and goals (r = 0.288, p < .001). The EOT scale of the TAS reported no overall significant correlation with the DERS-SF total score, but it did report weak positive correlations with the impulse (r = 0.149, p = .042) and clarity (r = 0.180, p = .018) subscales.
Table 2.
Pearson's correlation matrix of the relationships between all measured variables: alexithymia, emotion dysregulation, self-reported emotional eating urges and emotional eating behaviours in response to positive and negative emotions.
| 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. | 10. | 11. | 12. | 13. | 14. | 15. | 16. | 17. | 18. | 19. | 20. | 21. | 22. | 23. | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. TAS-20 Global | – | ||||||||||||||||||||||
| 2. TAS-20 DIF | .856*** | – | |||||||||||||||||||||
| 3. TAS-20 DDF | .863*** | .667*** | – | ||||||||||||||||||||
| 4. TAS-20 EOT | .634*** | .236** | .387*** | – | |||||||||||||||||||
| 5. DERS-SF Total | .616*** | .687*** | .553*** | .140 | – | ||||||||||||||||||
| 6. DERS-SF Non-Accept | .466*** | .455*** | .483*** | .133 | .752*** | – | |||||||||||||||||
| 7. DERS-SF Strategies | .483*** | .582*** | .425*** | .059 | .847*** | .511*** | – | ||||||||||||||||
| 8. DERS-SF Impulse | .436*** | .505*** | .317*** | .149* | .786*** | .447*** | .616*** | – | |||||||||||||||
| 9. DERS-SF Clarity | .678*** | .708*** | .652*** | .180* | .706*** | .490*** | .502*** | .371*** | – | ||||||||||||||
| 10. DERS-SF Goals | .347*** | .438*** | .288*** | .031 | .791*** | .428*** | .649*** | .532*** | .425*** | – | |||||||||||||
| 11. EES Total | .123 | .124 | .072 | .086 | .259** | .248** | .240** | .292*** | .087 | .127 | – | ||||||||||||
| 12. EES Depression | .114 | .146* | .043 | .060 | .238** | .242** | .224** | .274** | .039 | .126 | .934*** | – | |||||||||||
| 13. EES Anxiety | .017 | .037 | .028 | -.033 | .191* | .184* | .194* | .251** | .018 | .084 | .902** | .851*** | – | ||||||||||
| 14. EES Anger | .149* | .101 | .108 | .153* | .243** | .211** | .215** | .257** | .133 | .120 | .878*** | .707*** | .733*** | – | |||||||||
| 15. EES Somatic | .142* | .128 | .087 | .117 | .248** | .233** | .219** | .254** | .138 | .113 | .845*** | .687*** | .652*** | .734*** | – | ||||||||
| 16. SEES Sadness | -.032 | -.004 | -.113 | .033 | .008 | .074 | -.014 | -.034 | -.066 | .054 | .453*** | .549*** | .448*** | .260** | .282*** | – | |||||||
| 17. SEES Happiness | .094 | .032 | .134 | .073 | -.036 | .008 | -.072 | -.044 | .068 | -.089 | -.039 | -.094 | -.090 | .037 | .037 | -.379*** | – | ||||||
| 18. SEES Anger | -.019 | -.007 | -.063 | .021 | -.002 | -.028 | -.027 | .032 | .030 | -.009 | .425*** | .359*** | .494*** | .389*** | .312*** | .511*** | -.117 | – | |||||
| 19. SEES Anxiety | -.022 | -.020 | -.059 | .027 | -.026 | .010 | -.046 | .004 | .006 | -.071 | .275** | .256** | .414*** | .114 | .230** | .431*** | -.191* | .604*** | – | ||||
| 20. DASS-21 Total | .476*** | .583*** | .391*** | .137 | .622*** | .534*** | .549*** | .414*** | .449*** | .455*** | .206** | .213** | .128 | .208** | .160* | -.005 | .041 | -.126 | -.097 | – | |||
| 21. DASS-21 Depression | .429*** | .465*** | .370*** | .132 | .538*** | .457*** | .491*** | .323*** | .394*** | .411*** | .157* | .194* | .096 | .124 | .106 | -.020 | .021 | -.159* | -.085 | .885*** | – | ||
| 22. DASS-21 Anxiety | .477*** | .503*** | .400*** | .180* | .534*** | .478*** | .416*** | .355*** | .469*** | .354*** | .127 | .105 | .052 | .185* | .101 | -.078 | .147* | -.125 | -.122 | .858*** | .634*** | – | |
| 23. DASS-21 Stress | .353*** | .452*** | .260** | .057 | .559*** | .469*** | .522*** | .412*** | .329*** | .419*** | .252** | .243** | .178* | .246** | .211** | .074 | -.039 | -.043 | -.054 | .877*** | .626*** | .682*** | – |
Note: EES = TAS-20 = Toronto Alexithymia Scale; DIF = Difficulty identifying feelings; DDF = Difficulty describing feelings; EOT = Externally oriented thinking; DERS-SF = Difficulties in Emotion Regulation Short Form; DERS-SF Total = Total score omitting the awareness subscale; Emotional Eating Scale; SEES = Salzburg Emotional Eating Scale; DASS-21 = Depression, Anxiety and Stress Scale.
* = p < .05, ** = p < .01, *** = p < .001 (one-tailed).
Neither of these psychological variables (alexithymia or emotion dysregulation), nor any of their subscales, were significantly related to emotional eating behaviours as measured by subscales of the SEES. However, EES total scores reported weak correlations with the DERS-SF total score (r = 0.259, p = .001) and the subscales of non-acceptance (r = 0.248, p = .002), strategies (r = 0.240, p = .002), and impulse (r = 0.292, p < .001). The EES subscale of depression reported a weak correlation with the DIF facet of alexithymia only (r = 0.146, p = .045), and again weak correlations with the DERS-SF total score (r = 0.238, p = .003), and the subscales of non-acceptance (r = 0.242, p = .002), strategies (r = 0.224, p = .004), and impulse (r = 0.274, p = .001). The EES subscale of anxiety reported weak correlations with the DERS-SF total score (r = 0.191, p = .013), and the subscales of non-acceptance (r = 0.184, p = .016), strategies (r = 0.194, p = .012), and impulse (r = 0.251, p = .002). The EES subscale of anger reported a weak correlation with the TAS-20 global scores (r = 0.149, p = .042), and more specifically the cognitive characteristic of EOT (r = 0.153, p = .038). It also reported weak correlations with the DERS-SF total score (r = 0.243, p = .002), and the subscales of non-acceptance (r = 0.211, p = .007), strategies (r = 0.215, p = .006), and impulse (r = 0.257, p = .001). Finally, the EES subscale of somatic feelings reported a weak correlation with the TAS-20 global score (r = 0.142, p = .049) but no significant relationships with any of the subscales. It also reported weak correlations with the DERS-SF total score (r = 0.248, p = .002), and the subscales of non-acceptance (r = 0.233, p = .003), strategies (r = 0.219, p = .005), and impulse (r = 0.254, p = .001).
The negative scales of the SEES (sadness, anger, anxiety) positively correlated with the items of the EES, except for SEES anxiety and EES anger which did not correlate significantly. All items of the EES are negative, indicating there is a relationship between urges to eat in response to negative emotions, and self-reported negative emotional eating behaviours. The SEES happiness subscale negatively correlated with SEES sadness, indicating they may reflect opposing constructs with individuals eating more in response to sadness and less in response to happiness, and vice versa.
3.5. Mediation analyses
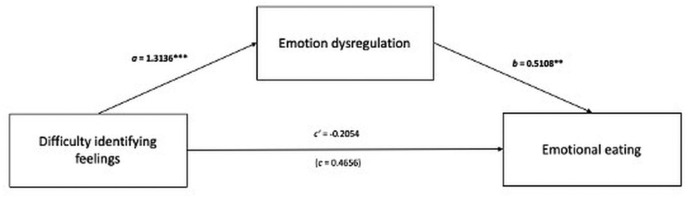
There was no overall significant association between emotional eating measures and DIF or DDF, but at present, there is consensus that mediation may exist in the absence of an overall significant association (Hayes, 2017). The PROCESS macro (Model 4) was used to examine the direct and indirect effects of alexithymia on emotional eating, via emotion dysregulation. First, DIF was entered as the predictor variable and emotional eating urges as measured by the EES as the outcome variable. Emotion dysregulation as the DERS-SF total score (omitting the awareness subscale) was entered as a potential mediating variable. There was no significant direct effect of DIF on EES total scores. Findings indicate that DIF was indirectly related to EES total scores through its relationship with emotion dysregulation. As seen in Fig. 1 , greater difficulty identifying feelings related to greater reported emotion dysregulation (B = 1.3136, p < .001), which was subsequently related to more emotional eating urges in response to negative emotions (B = 0.5108, p = .007). A 95% bias-corrected confidence interval based on 5000 bootstrap samples indicated that the indirect effect (B = 0.6710) was entirely above zero (CI = 0.0452–1.2178), with 13.7% of the variance in emotional eating urges accounted for by DIF and emotion dysregulation.
Fig. 1.
The mediating effect of emotion dysregulation in the relationship between difficulty identifying feelings and emotional eating. All presented effects are unstandardised; a is the effect of difficulty identifying feelings on emotion dysregulation; b is the effect of emotion dysregulation on emotional eating; c’ is the direct effect of difficulty identifying feelings on emotional eating; c is the total effect of difficulty identifying feelings on emotional eating.
* = p < .05, ** = p < .01, *** = p < .001.
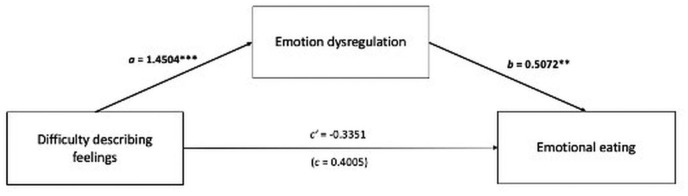
Next, DDF was entered as the predictor variable with emotional eating urges as measured by the EES as the outcome variable. Emotion dysregulation was again entered as the potential mediating variable. There was no significant direct effect of DDF on EES total scores. Findings indicate that DDF was indirectly related to EES total scores through its relationship with emotion dysregulation. As seen in Fig. 2 , greater difficulty describing feelings related to greater reported emotion dysregulation (B = 1.4504, p < .001), which was subsequently related to more emotion eating urges in response to negative emotions (B = 0.5072, p = .002). A 95% bias-corrected confidence interval based on 5000 bootstrap samples indicated that the indirect effect (B = 0.7356) was entirely above zero (CI = 0.1924–1.3360), with 13.9% of the variance in emotional eating urges accounted for by DDF and emotion dysregulation.
Fig. 2.
The mediating effect of emotion dysregulation in the relationship between difficulty describing feelings and emotional eating. All presented effects are unstandardised; a is the effect of difficulty describing feelings on emotion dysregulation; b is the effect of emotion dysregulation on emotional eating; c’ is the direct effect of difficulty describing feelings on emotional eating; c is the total effect of difficulty describing feelings on emotional eating.
* = p < .05, ** = p < .01, *** = p < .001.
There were no direct or indirect effects observed when self-reported negative emotional eating behaviour as measured by SEES subscales were entered as the outcome variables, with either DIF or DDF entered as the predictor variable. Specific subscales of the EES were explored with each predictor variable, identifying different significant models for each predictor. There were no direct effects for either predictor (DIF or DDF) for any of the EES subscales, but indirect effects were identified via emotion dysregulation. Greater DIF was indirectly related to greater emotional eating urges as measured by EES subscales of anxiety, anger and somatic feelings, whilst greater DDF was indirectly related to greater emotional eating urges as measured by EES subscales of depression, anger and somatic feelings. Testing the models with the mediator and outcome variables in the reverse order did not find any significant indirect effects for any models. These findings indicate that emotion dysregulation had a mediating effect on the relationship between affective characteristics of alexithymia and emotional eating urges in this order only.
4. Discussion
There were two aims of the present study. The first aim was to explore perceived changes in eating behaviour compared to usual before COVID-19, and compare with self-reported negative affect during the same time period. The second aim was to examine direct and indirect relationships between alexithymia and emotional eating, to expand upon previously proposed models and apply to eating behaviours during the pandemic.
Those who reported a change in the amount of food eaten (either more or less), also reported significantly greater negative affect as measured by the depression subscale over the same time frame (i.e. the previous week during lockdown), and significantly greater levels of DIF. This group also reported significantly greater emotional eating urges in response to depression, and emotional eating behaviours in response to sadness. These groups did not differ significantly in their reported difficulties in emotion regulation. There were no significant differences in negative affect, alexithymia, emotion dysregulation or self-reported emotional eating between those who reported eating more or less healthfully over the previous week and those who reported no change. Although the sample is relatively small, it echoes other findings examining changes in eating behaviours during COVID-19 and highlights the components of emotional eating (negative affect and change in eating behaviour) alongside self-reported emotional eating. Furthermore, the percentage of respondents who reported eating more (24.7%) and eating less healthfully (27.3%) is close to the number of respondents who reported this in the panel study of 90,000 respondents (17% and 23% respectively) (Fancourt et al., 2020a). Greater reported depression, and self-reported emotional eating urges and behaviours to this emotion, in those who reported a change in the amount eaten over the previous week compared to before lockdown indicates a presence of emotional eating during lockdown in these individuals. Emotional eating in response to depression is found to be the type most closely related to poorer psychological outcomes (Braden et al., 2018), so it is important to understand the role of emotional eating during the pandemic.
Previous pathways do not examine the mechanisms by which the alexithymic characteristics of impaired abilities to recognise and describe one's emotions result in greater eating in response to emotions. The findings of the mediation analyses indicate the indirect effects of DIF and DDF on emotional eating via emotion dysregulation. There is no direct effect observed by either predictor (DIF or DDF) on emotional eating; these models explain emotional eating as reported during the COVID-19 lockdown through indirect effects of difficulty identifying feelings and difficulty describing feelings, which in turn predict emotion dysregulation, which in turn predicts greater emotional eating urges as measured by the EES. There were no direct or indirect effects when factors of the SEES were entered as outcome variables with either predictor, which suggests the affective characteristics of alexithymia only exert indirect effects on self-reported emotional eating urges (as measured by EES) and not on self-reported emotional eating behaviours (as measured by SEES). Emotional eating was measured in the context of during the COVID-19 pandemic; as such, findings demonstrate the indirect effect of alexithymia on emotional eating during this time.
Correlation analyses highlighted that the EES total score and subscales positively correlated with SEES negative subscale scores. This indicates that urges to eat in response to negative emotions are related to greater self-reported negative emotional eating behaviours. However, the mediation regression analyses predicted only urges and not behaviours. This suggests that the mechanisms that influence self-reported behaviours differ from those that predict urges to eat in response to negative emotions. There may be barriers to eating behaviours, such as the accessibility and availability of foods creating a gap between desired eating and self-reported actual eating. The EES and SEES refer only to the amount of food which an individual self-reports how much they feel a desire to eat, or have eaten, in response to these emotions; these scales do not consider type of food, so the mechanisms involved in predicting the type of food eaten in response to emotions should be examined in future research.
The ‘apt’ response to negative affect or stress is to reduce eating (Schachter, Goldman, & Gordon, 1968), with the biologically ‘inapt’ response of eating food in response reflecting the definition of emotional eating. Recent literature posits that ‘unhappy overeating’ and ‘happy undereating’ may represent two sides of the same coin as behaviours exhibited by an individual, and this is considered less favourable than the opposing coin of ‘happy overeating’ and ‘unhappy undereating’ due to the association of poorer outcomes from negative emotional overeating (Braden et al., 2018). The present findings demonstrated a weak negative correlation between the happiness and sadness subscales of the SEES, which suggests that individuals who report eating more in response to sadness, also report eating less in response to happiness, and vice versa. These findings support this analogy (Meule et al., 2018), providing support for this inverse relationship within the general population during a global pandemic when approximately 40% of participants reported changes in their eating behaviours.
There are limitations to the present study. By definition, a mediator occurs after that which it mediates and before the outcome (Kraemer, Stice, Kazdin, Offord, & Kupfer, 2001), and the timing of alexithymia in the explored models is assumed based on theory, i.e. being a relatively stable personality trait, and therefore must precede behaviours (i.e. emotional eating) and learned skills (i.e. emotion dysregulation). However, the cross-sectional design does not allow for confirmation of causation in the mediation models. To address this limitation, the mediating and outcome variables were tested in a model in reverse order to test alternative causal models, as recommended by Fiedler et al. (2018). When EES preceded DERS, there were no significant direct or indirect effects identified, which is incompatible with mediation taking place; this was demonstrated with both DIF and DDF as predictors. Therefore, it is not the case that DIF or DDF predict emotional eating which in turn predicts emotion dysregulation. Limitations stemming from data collection include the self-report of perceived changes in how much individuals are eating and how healthful they perceive their diet to be, which are subject to bias and inaccurate recall. Similarly, self-report measures of alexithymia have been criticised due to the level of introspection required to respond to the items (Lane, Weihs, Herring, Hishaw, & Smith, 2015). Nonetheless, it is proposed that individuals with alexithymia are able to respond to related items on self-report measures (Bagby et al., 2020). Whilst other research designs are suited to mixed assessments of alexithymia via observer-reported alongside self-reported measures, online questionnaires can only make use of self-report measures. Furthermore, the emotional eating construct is multifaceted and influenced by context meaning it is not fully captured by questionnaire measures (Lattimore, 2020). The present study utilised the EES and SEES which measure self-reported emotional eating urges and behaviours respectively, to garner a wider measurement of the emotional eating construct.
The present study found that emotion dysregulation accounted for some of the variance between alexithymia and emotional eating, meaning there are other constructs involved, which may vary for each specific negative emotion. The present study found DIF and DDF had indirect effects on different subscales of the EES; greater DIF predicted greater emotion dysregulation which in turn predicted the anxiety, anger and somatic subscales of the EES, whilst greater DDF predicted greater emotion dysregulation which in turn predicted the depression, anger and somatic subscales of the EES. This suggests that different mechanisms may underpin the relationships with specific emotions and their subsequent impact on eating behaviours, and echoes previous research, which found self-reported depression and anxiety had differing relationships with alexithymia (Pink et al., 2019). Specific emotions may have varying influences on individuals’ eating behaviours, dependent on factors including their ability to identify broader and more specific emotions. It is thought that interoceptive reliance, which describes how much an individual trusts their bodily signals and determines how they respond, may underpin how an individual responds behaviourally to negative affect regardless of how well they identify and regulate it. It is suggested (Willem et al., 2020) that a lack of interoceptive reliance predicts greater emotion dysregulation and in turn a greater risk of emotional eating. Therefore, individuals may need to have the ability to first identify their emotions and also to trust them in order to adaptively regulate and respond to emotions.
A focus in the United Kingdom and its framing of COVID-19 risk has been greater body weight (see Department of Health and Social Care, 2020); stigma surrounding this may elicit greater negative affect (Puhl & Heuer, 2010) and contribute to emotional eating behaviours. Existing research investigating emotional eating is largely situated within the context of obesity and weight loss, often stigmatising due to its weight-normative approach despite weight stigma being identified as a risk factor for reduced quality of life (Puhl & Suh, 2015). Emotional eating can have negative psychological impacts irrespective of any influence on weight, with a need for mechanisms to be understood and interventions to be informed which go beyond a primary objective of weight management.
Eating in response to emotions can be positive for some individuals, as it is context-dependent (Lattimore, 2020). It has been found to buffer the association between adverse life events and perceived stress, but only in individuals without elevated levels of depressive symptoms (Finch & Tomiyama, 2015). Therefore, eating in response to stressors may protect some individuals, highlighting the nuances of eating behaviours in relation to informing interventions. Rather than targeting emotional eating itself, psychological predictor variables could be the focus to support individuals in their response to and regulation of emotions. The current study identified the role of emotion dysregulation for individuals with greater difficulty identifying their feelings, which may be a potential target for emotional eating interventions during both pandemics and similar situations for this population. Psychotherapies for emotional eating such as compassion-based and dialectical behaviour therapies (Roosen et al., 2012) are rooted in emotion regulation and acceptance, with identifying emotions key to promoting efficacy as a prerequisite to developing adaptive regulation skills (Vine & Aldao, 2014). Implications may involve psychoeducation for those delivering emotion regulation-based therapeutic interventions for eating behaviours, to inform about the importance of initial successful identification and description of feelings and identify individuals who need greater support to minimise poorer therapeutic outcomes. This could extend transdiagnostically across clinical and subclinical populations, particularly for interventions across the spectrum of emotional and binge eating behaviours.
The results of the current study should be interpreted within the context of the study's limitations and of the COVID-19 pandemic, with emotions and subsequent behaviours reported likely to be different compared to usual before the pandemic or once it has abated. Whilst not a laboratory study, the contemporary global pandemic and the impact on individual wellbeing and eating behaviours in the United Kingdom (Fancourt et al., 2020a, 2020b) has provided an opportunity for examining emotional eating in an atypical situation for large groups of the general population. Future research should seek to examine these mechanisms under conditions in which emotional eating can be observed. Deficits in emotion regulation and how they predict subsequent behaviour are likely to be better understood by assessing these difficulties in situations that approximate real-life situations with the use of state emotion dysregulation measures such as the S-DERS, which measures in the moment difficulties in emotion regulation, thus is better suited to laboratory-based research studies. Future research should seek to test the proposed model once the pandemic has abated.
To our knowledge, this is the first study to examine the indirect effects of alexithymia on emotional eating within the general population. The study identifies the indirect effects of both difficulty identifying and describing feelings on emotional eating urges, via emotion dysregulation. As this was demonstrated within a sample of the general population during the COVID-19 pandemic, findings should be followed up outside of the pandemic. These results extend beyond the current literature, and offer an insight into self-reported changes to eating behaviours during the COVID-19 pandemic.
Funding
This study was funded by a university in the West Midlands, United Kingdom as part of a PhD studentship. The work was not supported by any other funding bodies.
Contributors
KM and DW designed the study. KM conducted the data analyses. KM, DW, and MM interpreted the data. KM wrote the initial version of the manuscript. DW, MM and HE reviewed and edited the manuscript. All authors approved the final version of the manuscript.
Data statement
Data available upon request to the corresponding author.
Ethical statement
Ethical approval was obtained from the Faculty Academics Ethics Committee at Birmingham City University (approval code McAtamney/7327/Am/2020/Jul/BLSSFAEC), and this study was conducted in accordance with the Declaration of Helsinki. All participants were asked to read an information page before indicating that they consented to taking part in the study, and that they understood they could withdraw from the study at any time.
Declaration of competing interest
All authors declare that they have no conflicts of interest.
References
- Adam T.C., Epel E.S. Stress, eating and the reward system. Physiology & Behavior. 2007;91(4):449–458. doi: 10.1016/j.physbeh.2007.04.011. [DOI] [PubMed] [Google Scholar]
- Arden M.A., Chilcot J. Health psychology and the coronavirus (COVID-19) global pandemic: A call for research. British Journal of Health Psychology. 2020:231–232. doi: 10.1111/bjhp.12414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arnow B., Kenardy J., Agras W.S. International journal of eating disorders. 1995. The emotional eating scale: The development of a measure to assess coping with negative affect by eating. [DOI] [PubMed] [Google Scholar]
- Bagby R.M., Ayearst L.E., Morariu R.A., Watters C., Taylor G.J. The internet administration version of the 20-item Toronto alexithymia scale. Psychological Assessment. 2014;26(1):16–22. doi: 10.1037/a0034316. [DOI] [PubMed] [Google Scholar]
- Bagby R.M., Parker J.D.A., Taylor G.J. The twenty-item Toronto Alexithymia scale—I. Item selection and cross-validation of the factor structure. Journal of Psychosomatic Research. 1994;38(1):23–32. doi: 10.1016/0022-3999(94)90005-1. [DOI] [PubMed] [Google Scholar]
- Bagby R.M., Parker J.D.A., Taylor G.J. Twenty-five years with the 20-item Toronto alexithymia scale. Journal of Psychosomatic Research. 2020;131:109940. doi: 10.1016/j.jpsychores.2020.109940. [DOI] [PubMed] [Google Scholar]
- Balanzá–Martínez V., Atienza–Carbonell B., Kapczinski F., De Boni R.B. Lifestyle behaviours during the COVID‐19 – time to connect. Acta Psychiatrica Scandinavica. 2020;141(5):399–400. doi: 10.1111/acps.13177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnhart W.R., Braden A.L., Price E. Emotion regulation difficulties interact with negative, not positive, emotional eating to strengthen relationships with disordered eating: An exploratory study. Appetite. 2021;158(October 2020):105038. doi: 10.1016/j.appet.2020.105038. [DOI] [PubMed] [Google Scholar]
- Barrett L.F., Gross J., Christensen T.C., Benvenuto M. Knowing what you’re feeling and knowing what to do about it: Mapping the relation between emotion differentiation and emotion regulation. Cognition & Emotion. 2001;15(6):713–724. doi: 10.1080/02699930143000239. [DOI] [Google Scholar]
- Baumeister R.F., Heatherton T.F., Tice D.M. Academic Press, Inc; 1994. Losing control: How and how people fail at self-regulation. [Google Scholar]
- Braden A., Musher-eizenman D., Watford T., Emley E. Eating when depressed, anxious, bored, or happy: Are emotional eating types associated with unique psychological and physical health correlates? Appetite. 2018;125:410–417. doi: 10.1016/j.appet.2018.02.022. [DOI] [PubMed] [Google Scholar]
- Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., et al. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. The Lancet. 2020;395(10227):912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruce B., Agras W.S. Binge eating in females: A population‐based investigation. International Journal of Eating Disorders. 1992;12(4):365–373. [Google Scholar]
- Bruch H. Basic Books; 1973. Eating disorders: Anorexia nervosa, obesity and the person within. [Google Scholar]
- Cardi V., Leppanen J., Treasure J. Vol. 57. Elsevier Ltd; 2015. The effects of negative and positive mood induction on eating behaviour: A meta-analysis of laboratory studies in the healthy population and eating and weight disorders; pp. 299–309. (Neuroscience and biobehavioral reviews). [DOI] [PubMed] [Google Scholar]
- Department of Health and Social Care New obesity strategy unveiled as country urged to lose weight to beat coronavirus (COVID-19) and protect the NHS. 2020. https://www.gov.uk/government/news/new-obesity-strategy-unveiled-as-country-urged-to-lose-weight-to-beat-coronavirus-covid-19-and-protect-the-nhs
- Di Renzo L., Gualtieri P., Cinelli G., Bigioni G., Soldati L., Attinà A., et al. Psychological aspects and eating habits during covid-19 home confinement: Results of ehlc-covid-19 Italian online survey. Nutrients. 2020;12(7):1–14. doi: 10.3390/nu12072152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evers C., Adriaanse M., de Ridder D.T.D., de Witt Huberts J.C. Good mood food. Positive emotion as a neglected trigger for food intake. Appetite. 2013;68:1–7. doi: 10.1016/j.appet.2013.04.007. [DOI] [PubMed] [Google Scholar]
- Fancourt D., Bu F., Mak H.W., Steptoe P.A. 2020. Covid-19 social study week 14. June.https://www.covidsocialstudy.org/results [Google Scholar]
- Fancourt D., Bu F., Mak H.W., Steptoe P.A. Covid-19 social study week 15. July. 2020. https://www.covidsocialstudy.org/results 1-58.
- Fiedler K., Harris C., Schott M. Unwarranted inferences from statistical mediation tests – an analysis of articles published in 2015. Journal of Experimental Social Psychology. 2018;75(December 2017):95–102. doi: 10.1016/j.jesp.2017.11.008. [DOI] [Google Scholar]
- Finch L.E., Tomiyama A.J. Comfort eating, psychological stress, and depressive symptoms in young adult women. Appetite. 2015;95:239–244. doi: 10.1016/j.appet.2015.07.017. [DOI] [PubMed] [Google Scholar]
- Goerlich K.S. The multifaceted nature of alexithymia—a neuroscientific perspective. Frontiers in Psychology. 2018;9 doi: 10.3389/fpsyg.2018.01614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldbacher E.M., Grunwald H.E., LaGrotte C.A., Klotz A.A., Oliver T.L., Musliner K.L., et al. Factor structure of the Emotional Eating Scale in overweight and obese adults seeking treatment. Appetite. 2012;59(2):610–615. doi: 10.1016/j.appet.2012.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gold P., Chrousos G. Organization of the stress system and its dysregulation in melancholic and atypical depression: High vs low CRH/NE states. Molecular Psychiatry. 2002;7(3) doi: 10.1038/sj.mp.4001032. [DOI] [PubMed] [Google Scholar]
- Gratz K.L. Risk factors for and functions of deliberate self‐harm: An empirical and conceptual review. Clinical Psychology: Science and Practice. 2003;10(2):192–205. doi: 10.1093/clipsy.bpg022. [DOI] [Google Scholar]
- Gratz K.L., Dixon L.J., Kiel E.J., Tull M.T. In: The sage handbook of personality and individual differences. Zeigler-Hill V., Shackelford T.K., editors. Sage; 2018. Emotion regulation: Theoretical models, associated outcomes and recent advances; pp. 63–89. [Google Scholar]
- Gratz K.L., Roemer L. Difficulties in emotion regulation scale (DERS) Journal of Psychopathology and Behavioral Assessment. 2004;2004 doi: 10.1007/s10862-015-9514-x. http://cairncenter.com/forms/difficultiesinemotionalregulation_scale.pdf [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haedt-Matt A.A., Keel P.K., Racine S.E., Burt S.A., Hu J.Y., Boker S., et al. Do emotional eating urges regulate affect? Concurrent and prospective associations and implications for risk models of binge eating. International Journal of Eating Disorders. 2014;47(8):874–877. doi: 10.1002/eat.22247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hallion L.S., Steinman S.A., Tolin D.F., Diefenbach G.J. Psychometric properties of the difficulties in emotion regulation scale (DERS) and its short forms in adults with emotional disorders. Frontiers in Psychology. 2018;9(APR):1–12. doi: 10.3389/fpsyg.2018.00539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes A.F. Second. Guilford Publications; 2017. Introduction to mediation, moderation, and conditional process analysis. [Google Scholar]
- Heatherton T.F., Baumeister R.F. Binge eating as escape from self-awareness. Psychological Bulletin. 1991;110(1):86–108. doi: 10.1037/0033-2909.110.1.86. [DOI] [PubMed] [Google Scholar]
- Honkalampi K., Ruusunen A., Viinamäki H., Koivumaa‐Honkanen H., Valkonen‐Korhonen M., Lehto S.M. Dietary patterns are associated with the prevalence of alexithymia. Scandinavian Journal of Psychology. 2017;58(4):318–323. doi: 10.1111/sjop.12370. [DOI] [PubMed] [Google Scholar]
- Iancu I., Cohen E., Yehuda Y.B., Kotler M. Treatment of eating disorders improves eating symptoms but not alexithymia and dissociation proneness. Comprehensive Psychiatry. 2006;47(3):189–193. doi: 10.1016/j.comppsych.2006.01.001. [DOI] [PubMed] [Google Scholar]
- Kaufman E.A., Xia M., Fosco G., Yaptangco M., Skidmore C.R., Crowell S.E. The difficulties in emotion regulation scale short form (DERS-SF): Validation and replication in adolescent and adult samples. Journal of Psychopathology and Behavioral Assessment. 2016;38(3):443–455. doi: 10.1007/s10862-015-9529-3. [DOI] [Google Scholar]
- Kenardy J., Arnow B., Agras W.S. The aversiveness of specific emotional states associated with binge-eating in obese subjects. Australian and New Zealand Journal of Psychiatry. 1996;30(6):839–844. doi: 10.3109/00048679609065053. [DOI] [PubMed] [Google Scholar]
- Kraemer H.C., Stice E., Kazdin A., Offord D., Kupfer D. How do risk factors work together? Mediators, moderators, and independent, overlapping, and proxy risk factors. American Journal of Psychiatry. 2001;158(6):848–856. doi: 10.1176/appi.ajp.158.6.848. [DOI] [PubMed] [Google Scholar]
- Kuijer R.G., Boyce J.A. Emotional eating and its effect on eating behaviour after a natural disaster. Appetite. 2012;58(3):936–939. doi: 10.1016/j.appet.2012.02.046. [DOI] [PubMed] [Google Scholar]
- Lades L.K., Laffan K., Daly M., Delaney L. 2020. Brief Report COVID-19 Daily emotional well-being during the COVID-19 pandemic; pp. 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lane R.D., Weihs K.L., Herring A., Hishaw A., Smith R. Affective agnosia: Expansion of the alexithymia construct and a new opportunity to integrate and extend Freud's legacy. Neuroscience & Biobehavioral Reviews. 2015;55:594–611. doi: 10.1016/j.neubiorev.2015.06.007. [DOI] [PubMed] [Google Scholar]
- Larsen J.K., van Strien T., Eisinga R., Engels R.C.M.E. Gender differences in the association between alexithymia and emotional eating in obese individuals. Journal of Psychosomatic Research. 2006;60(3):237–243. doi: 10.1016/j.jpsychores.2005.07.006. [DOI] [PubMed] [Google Scholar]
- Lattimore P. Mindfulness-based emotional eating awareness training: Taking the emotional out of eating. Eating and Weight Disorders: EWD. 2020;25(3):649–657. doi: 10.1007/s40519-019-00667-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lavender J.M., Anderson D.A. Contribution of emotion regulation difficulties to disordered eating and body dissatisfaction in college men. International Journal of Eating Disorders. 2010;43(4):352–357. doi: 10.1002/eat.20705. [DOI] [PubMed] [Google Scholar]
- Lima C.K.T., Carvalho P.M.M., Lima I.A.A.S., Nunes J.V. A.O., Saraiva J.S.…de Souza R.I, et al. The emotional impact of Coronavirus 2019-nCoV (new Coronavirus disease) Psychiatry Research. 2020;287:112915. doi: 10.1016/j.psychres.2020.112915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovibond S.H., Lovibond P.F. 2nd ed. Psychology Foundation; 1995. Manual for the depression anxiety & stress scales. [Google Scholar]
- Marks D.F. Homeostatic theory of obesity. Health Psychology Open. 2015;2(1) doi: 10.1177/2055102915590692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mattila A.K., Salminen J.K., Nummi T., Joukamaa M. Age is strongly associated with alexithymia in the general population. Journal of Psychosomatic Research. 2006;61(5):629–635. doi: 10.1016/j.jpsychores.2006.04.013. [DOI] [PubMed] [Google Scholar]
- Meule A., Reichenberger J., Blechert J. Development and preliminary validation of the Salzburg emotional eating scale. Frontiers in Psychology. 2018;9:88. doi: 10.3389/fpsyg.2018.00088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy J., Brewer R., Hobson H., Catmur C., Bird G. Is alexithymia characterised by impaired interoception? Further evidence, the importance of control variables, and the problems with the heartbeat counting task. Biological Psychology. 2018;136:189–197. doi: 10.1016/j.biopsycho.2018.05.010. [DOI] [PubMed] [Google Scholar]
- Nolan L.J., Halperin L.B., Geliebter A. Emotional Appetite Questionnaire. Construct validity and relationship with BMI. Appetite. 2010;54(2):314–319. doi: 10.1016/j.appet.2009.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norman H., Marzano L., Coulson M., Oskis A. Effects of mindfulness-based interventions on alexithymia: A systematic review. Evidence-Based Mental Health. 2019;22(1):36–43. doi: 10.1136/ebmental-2018-300029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norton P.J. Depression anxiety and stress scales (DASS-21): Psychometric analysis across four racial groups. Anxiety, Stress & Coping. 2007;20(3):253–265. doi: 10.1080/10615800701309279. [DOI] [PubMed] [Google Scholar]
- Oliver G., Wardle J. Perceived effects of stress on food choice. Physiology & Behavior. 1999;66(3):511–515. doi: 10.1016/S0031-9384(98)00322-9. [DOI] [PubMed] [Google Scholar]
- Oliver G., Wardle J., Gibson E.L. Stress and food choice: A laboratory study. Psychosomatic Medicine. 2000;62(6):853–865. doi: 10.1097/00006842-200011000-00016. [DOI] [PubMed] [Google Scholar]
- Ouwens M.A., van Strien T., van Leeuwe J.F.J. Possible pathways between depression, emotional and external eating. A structural equation model. Appetite. 2009;53(2):245–248. doi: 10.1016/j.appet.2009.06.001. [DOI] [PubMed] [Google Scholar]
- O'Connor D.B., O'Connor R.C. Perceived changes in food intake in response to stress: The role of conscientiousness. Stress and Health. 2004;20(5):279–291. doi: 10.1002/smi.1028. [DOI] [Google Scholar]
- Papandreou C., Arija V., Aretouli E., Tsilidis K.K., Bulló M. Comparing eating behaviours, and symptoms of depression and anxiety between Spain and Greece during the COVID-19 outbreak: Cross-sectional analysis of two different confinement strategies. European Eating Disorders Review. 2020;28(6):836–846. doi: 10.1002/erv.2772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillipou A., Meyer D., Neill E., Tan E.J., Toh W.L., Van Rheenen T.E., et al. Eating and exercise behaviors in eating disorders and the general population during the <scp>COVID</scp> ‐19 pandemic in Australia: Initial results from the <scp>COLLATE</scp> project. International Journal of Eating Disorders. 2020;53(7):1158–1165. doi: 10.1002/eat.23317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinaquy S., Chabrol H., Simon C., Louvet J.-P.P., Barbe P. Emotional eating, alexithymia, and binge-eating disorder in obese women. Obesity Research. 2003;11(2):195–201. doi: 10.1038/oby.2003.31. [DOI] [PubMed] [Google Scholar]
- Pink A.E., Lee M., Price M., Williams C. A serial mediation model of the relationship between alexithymia and BMI: The role of negative affect, negative urgency and emotional eating. Appetite. 2019;133:270–278. doi: 10.1016/j.appet.2018.11.014. [DOI] [PubMed] [Google Scholar]
- Pinna F., Sanna L., Carpiniello B. Vol. 8. 2015. Alexithymia in eating disorders: Therapeutic implications; pp. 1–15. (Psychology research and behavior management). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preacher K.J., Hayes A.F. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods. 2008;40(3):879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- Public Health England Staying alert and safe (social distancing) 2020. https://www.gov.uk/government/publications/covid-19-guidance-on-social-distancing-and-for-vulnerable-people/guidance-on-social-distancing-for-everyone-in-the-uk-and-protecting-older-people-and-vulnerable-adults
- Puhl R.M., Heuer C.A. Obesity stigma: Important considerations for public health. American Journal of Public Health. 2010;100(6):1019–1028. doi: 10.2105/AJPH.2009.159491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puhl R., Suh Y. Vol. 4. 2015. Health consequences of weight stigma: Implications for obesity prevention and treatment; pp. 182–190. (Current obesity reports). Issue 2. [DOI] [PubMed] [Google Scholar]
- Racine S.E., Wildes J.E. Emotion dysregulation and symptoms of anorexia nervosa: The unique roles of lack of emotional awareness and impulse control difficulties when upset. International Journal of Eating Disorders. 2013;46(7):713–720. doi: 10.1002/eat.22145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roosen M.A., Safer D., Adler S., Cebolla A., van Strien T. Group dialectical behavior therapy adapted for obese emotional eaters; a pilot study. Nutricion Hospitalaria. 2012;27(4):1141–1147. doi: 10.3305/nh.2012.27.4.5843. [DOI] [PubMed] [Google Scholar]
- Scarmozzino F., Visioli F. Covid-19 and the subsequent lockdown modified dietary habits of almost half the population in an Italian sample. Foods. 2020;9(5) doi: 10.3390/foods9050675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schachter S., Goldman R., Gordon A. Effects of fear, food deprivation and obesity on eating. Journal of Personality and Social Psychology. 1968;10:91–97. doi: 10.1037/h0026284. [DOI] [PubMed] [Google Scholar]
- Schmidt U., Jiwany A., Treasure J. A controlled study of alexithymia in eating disorders. Comprehensive Psychiatry. 1993;34:54–58. doi: 10.1016/0010-440x(93)90036-4. https://www.cochranelibrary.com/central/doi/10.1002/central/CN-00525702/full (1 CC-HS-HANDSRCH CC-Common Mental Disorders) [DOI] [PubMed] [Google Scholar]
- Shen W., Long L.M., Shih C.H., Ludy M.J. A humanities-based explanation for the effects of emotional eating and perceived stress on food choice motives during the COVID-19 pandemic. Nutrients. 2020;12(9):1–18. doi: 10.3390/nu12092712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Speranza M., Loas G., Wallier J., Corcos M. Predictive value of alexithymia in patients with eating disorders: A 3-year prospective study. Journal of Psychosomatic Research. 2007;63(4):365–371. doi: 10.1016/j.jpsychores.2007.03.008. [DOI] [PubMed] [Google Scholar]
- van Strien T., Cebolla A., Etchemendy E., Gutiérrez-Maldonado J., Ferrer-García M., Botella C., et al. Emotional eating and food intake after sadness and joy. Appetite. 2013;66:20–25. doi: 10.1016/j.appet.2013.02.016. [DOI] [PubMed] [Google Scholar]
- van Strien T., Herman C.P., Verheijden M.W. Eating style, overeating and weight gain. A prospective 2-year follow-up study in a representative Dutch sample. Appetite. 2012;59(3):782–789. doi: 10.1016/j.appet.2012.08.009. [DOI] [PubMed] [Google Scholar]
- van Strien T., Ouwens M.A. Effects of distress, alexithymia and impulsivity on eating. Eating Behaviors. 2007;8:251–257. doi: 10.1016/j.eatbeh.2006.06.004. (2 CC-Metabolic and Endocrine Disorders) [DOI] [PubMed] [Google Scholar]
- van Strien T., Ouwens M.A. Effects of distress, alexithymia and impulsivity on eating. Eating Behaviors. 2007;8(2):251–257. doi: 10.1016/j.eatbeh.2006.06.004. [DOI] [PubMed] [Google Scholar]
- Sultson H., Kukk K., Akkermann K. Positive and negative emotional eating have different associations with overeating and binge eating: Construction and validation of the Positive-Negative Emotional Eating Scale. Appetite. 2017;116:423–430. doi: 10.1016/j.appet.2017.05.035. [DOI] [PubMed] [Google Scholar]
- Taylor G.J., Bagby R.M. In: The handbook of emotional intelligence. Bar–On R., Parker J.D.A., editors. Jossey–Bass; 2000. An overview of the alexithymia construct; pp. 41–67. [Google Scholar]
- Vieira C.M., Franco O.H., Restrepo C.G., Abel T. Maturitas COVID-19 : The forgotten priorities of the pandemic. Maturitas. 2020;136(April):38–41. doi: 10.1016/j.maturitas.2020.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waller G., Osman S. Emotional eating and eating psychopathology among non-eating-disordered women. International Journal of Eating Disorders. 1998;23(4):419–424. doi: 10.1002/(SICI)1098-108X(199805)23:4<419::AID-EAT9>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- Wallis D.J., Hetherington M.M. Stress and eating: The effects of ego-threat and cognitive demand on food intake in restrained and emotional eaters. Appetite. 2004;43(1):39–46. doi: 10.1016/j.appet.2004.02.001. [DOI] [PubMed] [Google Scholar]
- Wallis D.J., Hetherington M.M. Emotions and eating. Self-reported and experimentally induced changes in food intake under stress. Appetite. 2009;52(2):355–362. doi: 10.1016/j.appet.2008.11.007. [DOI] [PubMed] [Google Scholar]
- Whiteside U., Chen E., Neighbors C., Hunter D., Lo T., Larimer M. Difficulties regulating emotions: Do binge eaters have fewer strategies to modulate and tolerate negative affect? Eating Behaviors. 2007;8(2):162–169. doi: 10.1016/j.eatbeh.2006.04.001. [DOI] [PubMed] [Google Scholar]
- Willem C., Nandrino J.-L., Doba K., Roussel M., Triquet C., Verkindt, et al. Interoceptive reliance as a major determinant of emotional eating in adult obesity. Journal of Health Psychology. 2020 doi: 10.1177/1359105320903093. 135910532090309. [DOI] [PubMed] [Google Scholar]
- World Health Organization WHO Director‐General’s opening remarks at the media briefing on COVID‐19. 2020. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020
- Zamariola G., Vlemincx E., Luminet O., Corneille O. Relationship between interoceptive accuracy, interoceptive sensibility, and alexithymia. Personality and Individual Differences. 2018;125(December 2017):14–20. doi: 10.1016/j.paid.2017.12.024. [DOI] [Google Scholar]
- Zellner D.A., Loaiza S., Gonzalez Z., Pita J., Morales J., Pecora D., et al. Food selection changes under stress. Physiology & Behavior. 2006;87(4):789–793. doi: 10.1016/j.physbeh.2006.01.014. [DOI] [PubMed] [Google Scholar]
- Gelibter A., Aversa A. Emotional eating in overweight, normal weight, and underweight individuals. Eating Behaviors. 2003;3(4):341–347. doi: 10.1016/S1471-0153(02)00100-9. [DOI] [PubMed] [Google Scholar]
- Lyvers M., Brown T., Thorberg F.A. Is it the taste or the buzz? alexithymia, caffeine, and emotional eating. Substance Use & Misuse. 2019;54(4):572–582. doi: 10.1080/10826084.2018.1524490. [DOI] [PubMed] [Google Scholar]
- Vine V., Aldao A. Impaired emotional clarity and psychopathology: A transdiagnostic deficit with symptom-specific pathways through emotion regulation. Journal of Social and Clinical Psychology. 2014;33(4):319–342. doi: 10.1521/jscp.2014.33.4.319. [DOI] [Google Scholar]
- Salminen J.K., Saarijärvi S., Äärelä E., Toikka T., Kauhanen J. Prevalence of alexithymia and its association with sociodemographic variables in the general population of Finland. Journal of Psychosomatic Research. 1999;46(1):75–82. doi: 10.1016/S0022-3999(98)00053-1. [DOI] [PubMed] [Google Scholar]
- van Strien T. Causes of emotional eating and matched treatment of obesity. Current Diabetes Reports. 2018;18(6):35. doi: 10.1007/s11892-018-1000-x. [DOI] [PMC free article] [PubMed] [Google Scholar]