Abstract
Within the last decade there has been a significant expansion in access to cannabis for medicinal and adult nonmedical use in the United States (U.S.) and abroad. This has resulted in a rapidly growing and diverse workforce that is involved with the growth, cultivation, handling and dispensing of the cannabis plant and its products. The objective of this review is to educate physicians on the complexities associated with the health effects of Cannabis exposure, the nature of these exposures, and the future practical challenges of managing these in the context of allergic disease. We will detail the biological hazards related to typical modern cannabis industry operations that may potentially drive allergic sensitization in workers. We will highlight the limitations that have hindered the development of objective diagnostic measures that are essential in separating ‘true’ cannabis allergies from non-specific reactions/irritations that ‘mimic’ allergy-like symptoms. Finally, we will discuss recent advances in the basic and translational scientific research that will aid the development of diagnostic tools and therapeutic standards to serve optimal management of cannabis allergies across the occupational spectrum.
Keywords: Cannabis, occupational, allergy
INTRODUCTION
Cannabis has a complex and controversial interaction with human society, albeit an enduring one. Historically, industrial hemp, the cannabis plant that contains less than 0.3% Δ9-tetrahydrocannabinol (THC) (soft hemp) has been an essential component in industries as an important source of fiber, paper, cordage, food and medicine.1 However, cannabis cultivation (containing more than 0.3% THC) and access to its products are largely restricted throughout the world due to its secondary properties of psychoactive compounds. In the United States (U.S.), cannabis and its components (particularly cannabinoids) are designated by the federal Drug Enforcement Administration (DEA) as Schedule I controlled substances, whereas in Canada and several European countries they have either been legalized or decriminalized for medicinal or adult nonmedical use. In the past few decades, cannabis has gained popularity primarily for its medicinal properties in managing symptoms of chronic illnesses including for pain management, post-traumatic stress disorder, and certain seizure disorders.2-4 Further, along with its psychotropic effects, it is a source of plant protein food and continues to be used in textile industries.5, 6
Worldwide, cannabis is the most frequently used illicit drug.7 The United Nations Office on Drugs and Crime (UNODC) survey recently reported that approximately 10% of the US population (and up to 5% of the world population) uses cannabis in some form for medicinal or adult nonmedical purposes.7 Increased legalization and expanding access to cannabis within the U.S. and elsewhere has also ushered in new economic and employment opportunities for this growing industry. Currently, more than 240,000 workers are estimated to be engaged in various cannabis-related business operations (e.g. cultivation, processing, dispensaries) across the U.S., and these numbers will likely increase in the near future.8 This brings into focus a concern for the health and well-being of workers who will be exposed to the plant and its byproducts, specifically potential allergic reactions to cannabis. While there is some evidence on allergic sensitization to cannabis, these are limited and consist mostly of case reports; consequently, it is not possible to definitively establish the true burden of cannabis allergy, especially within occupational environments. In this review, our goals are to provide a brief background into the biological hazards associated with job activities in the cannabis industry, identify the risk factors that may contribute towards development of cannabis-related allergic reactions and provide insight into the current practice of diagnostics and therapeutics for clinical management of occupational allergies to cannabis.
HEMP DUST AND BYSSINOSIS
Cannabis has been heavy utilized in the textile industry for the production of fiber-based raw material called hemp that is produced from a variety of cannabis plant that contains less than 0.3% (THC). Most of our understanding of occupational exposures within cannabis industries comes from a series of studies published on cultivation and processing of soft hemp.9-19 Collectively, these studies have shown that the pathophysiology of cannabis exposures in the workplace are complicated by the presence of other occupational hazards such as bacteria (endotoxins) and other non-specific irritants that result in dust-related disease called “byssinosis.” Further, endotoxin from bacteria present on plant may continue to persist in processed fibers and contribute to byssinosis,12 although more studies are needed. Byssinosis is a lung disease characterized by airflow obstruction and airway inflammation caused by airborne organic dust in the occupational environment.20 It was first described in hemp workers and termed “cannabosis,”10 and was a particular concern in workers who directly handled (batting and hackling) of retted soft hemp.12 Although byssinosis is commonly associated with other organic fibers such as cotton21, flax22 and jute23, hemp workers are most highly affected, with prevalence rates of up to 44% in some studies.11, 12 Byssinosis, regardless of the specific fiber involved, typically develops following sustained exposures for >10 years. It is characterized by symptoms of severe bronchial hyperresponsiveness on the first day of the work week, with declining symptoms on consecutive days of exposure.19 Symptoms will flare on re-exposure following several days away from work such as weekends or holidays. Byssinosis, however, is not mediated by specific IgE (sIgE) antibodies and is not explained by allergic sensitization to cannabis. We speculate that modern-day cultivation and manipulation practices of cannabis may be less likely to generate organic dust at the rates previously observed with hemp cultivation, although more studies are needed.
MODERN DAY CANNABIS OPERATIONS AND ASSOCIATED EXPOSURE RISKS
Cannabis industries in the 21st century
Within the last decade, numerous states have passed laws that have either expanded access to cannabis or decriminalized it for medicinal and/or adult nonmedical use. The Hemp Farming Act of 2018 rescheduled hemp to a legal agricultural commodity, while strains of cannabis with >0.03% THC continue to be identified as Schedule I controlled substance. This shift in approach and regulation has resulted in the emergence of businesses to cultivate cannabis, manufacture related products, and set up distribution/sales networks (including dispensaries). In 2018, the cannabis industry was valued at over $11 billion and recent estimates have projected an annual growth rate of 14.5% per year through 2025.24 The rapid growth of the cannabis industry in the U.S. has resulted in the employment of a workforce that has approached nearly 250,000 workers.25 However, because cannabis related operations are highly varied, there are emerging health concerns for workers within the industry. The growth of the cannabis industry has focused the attention of employee unions, state public health agencies such as the Colorado Department of Public Health and Environment (CDPHE), and federal government agencies such as the National Institute for Occupational Safety and Health (NIOSH) on workplace safety and health hazards.26, 27 In states such as Colorado, where medicinal and adult nonmedical use of cannabis is legal, specific guidelines have been established to ensure worker safety in this evolving economic endeavor.26 Although these recommendations are broad, they are intended to assist in identifying specific hazards present in the industry and are somewhat tailored to the practices within the cannabis industry.
Although, cannabis cultivation and harvesting operations are analogous to any other plant-based agricultural and manufacturing practices, recent investigations have revealed unique occupational safety and health considerations that need to be considered.27 In a recent study conducted by the researchers at the Colorado School of Public Health, potential respiratory hazards and health effects were among the most frequently reported concerns by cannabis cultivation workers.28
Figure 1 illustrates the occupational workflow within a contemporary cannabis grow facility, as well as the associated exposure risks, although specific practices may vary owing to the dynamic nature of the industry. Throughout the growth cycle of the cannabis plant, a number of tasks involve direct handling the plant. Although these tasks vary in duration, they carry a significant risk of allergic sensitization. Secondary exposure to other allergens (such as fungi), bacteria, endotoxin, pesticides, cannabinoids and volatile compounds, also poses health risks.
Figure 1. Primary and secondary health hazards associated with occupational exposures to cannabis.
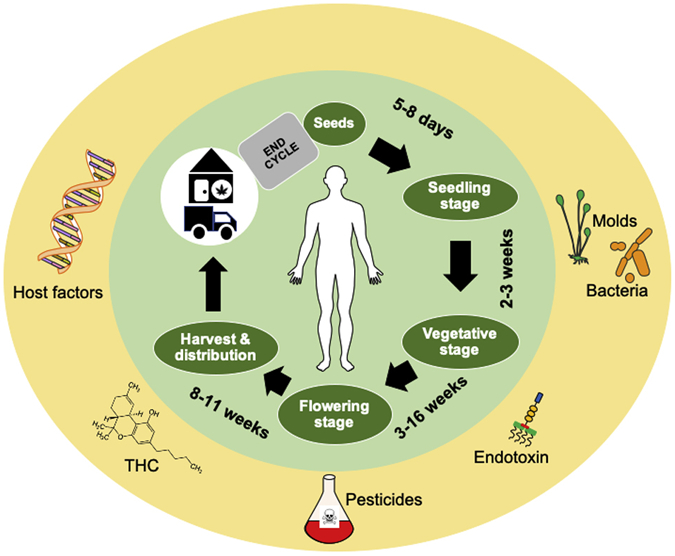
An investigation into a simplified flow of the occupational tasks that occur within the cannabis industry indicates numerous opportunities for direct (and possibly prolonged) exposures to cannabis that may affect worker health and drive allergic sensitization. The green sphere describes the cycle of cannabis cultivation, processing and distribution, and emphasizes the risk of direct exposures to the plant. Workers involved in cultivation, destemming and trimming operations may have elevated risks for disease owing to prolonged direct contact with the plant. Exposure to cannabis related biological hazards is not limited to just the grow facility, and could extend to transportation workers, budtenders or retailers. The yellow sphere identifies potential secondary risk factors that may drive sensitization alone (mold) or act as adjuvants (endotoxin, pesticides, THC) and promote cannabis sensitization. Further, underlying host factors such as atopy and asthma may also represent risks for exacerbation and diseases. Indoor work environments may also increase sensitization risk if poorly ventilated. Cannabis grow cycle details obtained from www.leafly.com.
Other occupational settings for Cannabis exposure
Additional occupations that are at risk of cannabis exposure include law enforcement personnel, laboratory technicians, and dispensary workers. Evidence of the adverse health effects of occupational exposure to cannabis (including allergies) emerges from studies evaluating law enforcement personnel with direct contact with illicitly grown cannabis,29, 30 or from second hand exposure at work.31 Law enforcement workers may also be exposed to pesticides and high concentrations of microbial bioaerosols when removing illicit cannabis plantations or ‘indoor grow’ operations.29, 30
In summary, many of those occupationally exposed to cannabis, whether it is on farms cultivating cannabis, downstream cannabis processing industries, or during forensic work, have the potential to experience respiratory and dermal allergic symptoms that could be potentially anaphylactic. A variety of biological and chemical hazards can contribute to this symptomology, as well as host specific factors.
OCCUPATIONAL CANNABIS ALLERGIES AND SYMPTOMS
Studies describing the health effects of working in a cannabis-rich environment have been limited. Nevertheless, some studies have demonstrated that direct handling of plant material can contribute to allergic sensitization in workers with infrequent exposures such as law enforcement officers and forensic technicians.32-36 Immediate respiratory symptoms in direct response to exposure are more common and are marked by nasal congestion, rhinoconjunctivitis, and/or chest symptoms such as cough, wheeze, chest tightness or shortness of breath related to bronchial hyperresponsiveness.32-35, 37 These are in contrast to the delayed respiratory symptoms of byssinosis in hemp workers, with temporal decrease in severity over the course of the work week. Further, cutaneous symptoms such as (contact) urticaria, angioedema33, 34, 36, 37 and rarely, delayed dermatitis-like32 symptoms have also been reported following direct contact with the cannabis plant. These are similar to those observed in adult nonmedical users with cannabis allergy, demonstrating varying degrees of respiratory, cutaneous, gastro-intestinal and cardiovascular symptoms.38-42 Up to 20% of affected individuals may also show anaphylactic-like reactions.38 Also rarely occurring, anaphylactic reactions have been reported in sensitized individuals associated with hempseed ingestion, which is marketed as a ‘healthy protein food’.43 One peculiar feature of cannabis allergy in European adult nonmedical users is the high prevalence of IgE-mediated cross-reactivity syndrome with multiple plant-foods (such as peach, tomatoes etc.).41, 44-46 Interestingly, the severe cross-reactivity with other plant allergens is not common in occupational cannabis allergy;47 although, detailed studies are lacking. It is possible that different routes of exposure, inhaled and ingested vs. primarily cutaneous contact, result in different patterns of allergic reactivity. A recent study of the Belgian police force could not objectively establish a cannabis allergy as the cause of the respiratory and/or cutaneous symptoms reported by 42% (34/81) of symptomatic participants during occupational cannabis exposure.44
Relevance of cannabis pollen to occupational exposures
Cannabis grow operations may also involve exposure to cannabis plant pollen. Similar to Birch trees that are highly allergenic,48 cannabis produces large quantities of anemophilous pollen. Pollen exposure of cannabis sensitized patients, established by skin prick test to cannabis pollen, has been shown to cause allergic symptoms such as rhinoconjunctivitis.35, 49-51 However, modern day cannabis cultivation practices have taken advantage of the dioecious nature of the plant. Specifically, practices involve seeding of the plant and early removal of male plants (that bear pollen) during growth to specifically enrich female plants to develop seedless buds (in absence of pollination) that are rich in cannabinoids.52 Other operations bypass pollination concerns through seedless propagation of only female clones. Thus, depending on the nature of the grow facility, pollen from male plants may not, or minimally be of concern for occupational exposures. However, breeders who are developing new genetic strains could be periodically exposed to pollen from male plants.
Cannabis allergens
Most biological allergens are typically classified as high molecular weight (HMW) – proteinaceous compounds such as Hevea latex, pollens, enzymes, and cereals etc.53 Investigations of adult nonmedical cannabis allergies have found type I hypersensitivity mechanisms involving allergen-specific IgE antibodies are predominant.38, 39, 42, 54 A growing number of studies have identified putative allergens from cannabis (Table 2), with nsLTP (Can s 3) as a major allergen, and oxygen evolving enhancing protein 2 ((OEEP2; Can s 4) as a relatively minor allergen.39, 41, 42, 47, 55, 56 Can s 3, the major cannabis allergen has been proposed as the driver of plant-food cross-reactivities observed in cannabis allergy in Europe (but not in U.S.)38, 41. This is primarily due to the high degree of similarities between the different nsLTP proteins in the plant kingdom and a sequence of conserved amino acid sequences in the C-terminal region of the mature protein.54, 57 It is important to emphasize that these cannabis allergens were primarily identified, and subsequently validated, in adult nonmedical users. In contrast, sensitization to nsLTP did not appear to be responsible for symptoms from cannabis exposures in law enforcement officers.44 Identification and validation of additional cannabis allergens relevant to occupational exposures is needed.
In addition, the cannabis plant contains a large number of LMW components including cannabinoids, terpenes, and volatile organic compounds (VOCs), which can exert immunomodulatory actions. Indeed, the first report describing cannabis allergies speculated a role for THC.58 However, these low molecular weight (LMW) cannabis chemicals have not been reported to act as allergens. Some studies have also suggested that carbohydrate moieties (including cross-reactive carbohydrates) on cannabis proteins could bind to serum IgE.39, 59 However, a mechanistic role for polysaccharides acting as cannabis allergens has not been investigated.
DIAGNOSIS OF CANNABIS ALLERGY
Currently, there are no diagnostic tests available to diagnose true cannabis allergies. In this section, we will provide an overview of the lessons learned from clinical management of suspected cannabis allergy cases. Further, we will discuss the research findings that have furthered our understanding of the underlying type I hypersensitivity mechanisms; although they have been applied in laboratory settings only.
Clinical diagnostics
a). Patient exposure history, symptoms and, physical exam
The first step in diagnosing occupational cannabis allergy is to clearly establish the nature of a patient’s job within the cannabis industry and a thorough evaluation of their exposure history. An emphasis should be placed on the timing of symptoms subsequent to exposure, with some period of latency before symptoms onset. Questions should be included regarding the history of exposure (e.g. duration of time in the job, type of exposure, working conditions), personal use (e.g. frequency and duration of use, routes of administration, adverse events), presence of plants grown within the home, as well as potential secondary exposures.
IgE-mediated allergies typically present with symptoms within minutes to 2-4 hours following exposure. They typically resolve promptly following cessation of exposures, although they may also induce non-specific bronchial hyperreactivity and/or a late phase response as classically was found with bakers.60 The pattern of symptoms is essential to rule out byssinosis, which is non-IgE-mediated. The spectrum of cannabis symptoms often includes allergic rhinitis and new onset or exacerbation of underlying asthma. Further, cutaneous manifestations such as contact urticaria may be present in workers who directly handle or come into contact with the plant.32 However, the potential for effects from non-specific irritants cannot be ruled out. Finally, atopy may be a risk factor for other IgE-mediated allergies such as cannabis, hence, establishing a patient’s history of atopy or asthma is also valuable.
As with other inhalant allergies, signs include allergic rhinoconjunctivitis, urticaria, dermatographism, along with wheeze, cough or a prolonged expiratory phase.37, 40, 55, 61, 62 Although a specific bronchial challenge (SBC) is considered the gold standard to diagnose cannabis-induced asthma, it is difficult to perform due to legal and ethical concerns.
b). Skin prick testing (SPT)
This is one of the most easily accessible diagnostic methods in a clinical office and can be performed with either purified extracts or fresh material. In occupational settings, samples can be collected from operational sites.13, 63 Tasks that involve direct handling of plant material may contribute to higher prevalence of SPT positivity.13, 63
c). Inhalation challenge
Although a specific bronchial challenge (SBC) is considered the gold standard to diagnose cannabis-induced asthma, it is difficult to perform due to legal and ethical concerns. As in other cases of occupational and non-occupational asthma, a methacholine challenge may be performed if needed to confirm an asthma diagnosis
d). Laboratory-based approaches for molecular diagnosis of cannabis allergies.
In an effort to develop standardized tests to diagnose cannabis sensitization, multiple researchers have sought to identify specific molecular mediators of sensitization (summarized in Table 1). As a result, a number of allergens relevant to adult cannabis use allergy have been identified and some validated (Table 2). However, none of these tests are available clinically.
Table 1. Laboratory-based approaches for molecular diagnosis of cannabis allergies.
Currently, a sIgE test for cannabis (hemp) is available for research use only. Can s 3 represents non-specific lipid transfer protein (nsLTP), which is a major allergen of cannabis.
| Diagnostic approach |
% Sensitivity (analyte) |
% Specificity (analyte) |
Relevant References |
|---|---|---|---|
| ImmunoCAP (hemp) | 86% (hemp extract) | 32% (hemp extract) | 38, 62 |
| Basophil activation test (BAT) | − 63% (crude cannabis extract) | − 67% (crude cannabis extract) | 38 |
| − 71% (recombinant Can s 3) | − 85% (recombinant Can s 3) | ||
| Cytometric bead array (CBA) | 63% (recombinant Can s 3) | 87% (recombinant Can s 3) | 38 |
| Immunoproteomics | Not applicable | Not applicable | For additional details 39 |
Table 2. List of cannabis allergens and allergen-candidates.
All allergens identified here have emerged from investigations into allergic sensitization to cannabis among adult nonmedical users. Can s 3 and Can s 4 allergens have been assigned as major and minor allergens, respectively. All allergens reported here have not been validated under occupational exposure settings. WHO/IUIS: World Health Organization/International Union of Immunological Societies.
| Cannabis allergen | WHO/IUIS Allergen Nomenclature |
References |
|---|---|---|
| Non-specific Lipid transfer protein (nsLTP) | Can s 3 | 41, 42, 45, 47, 56 |
| Oxygen-evolving enhancing protein 2 (OEEP2) | Can s 4 | 39, 55 |
| Ribulose-1,5-bisphospate carboxylase/oxygenase (RuBisCO) | Not validated | 39 |
| Thaumatin-like protein (TLP) | Not validated | 45 |
In summary, it is essential that the workplace conditions are taken into consideration when examining symptoms related to occupational cannabis exposure. The methods described herein to establish sensitization to cannabis allergens in occupational settings will require substantial validation for clinical use. As cannabis is often not the only allergen present in the grow operation or dispensary, symptoms can be elicited by other inhalant allergens (e.g. fungi).40 Efforts into identification and validation of relevant allergens and their integration into SPT-based in-clinic assessments can substantially improve the ability to establish true cannabis allergies in the clinic itself. Based on the diagnostic algorithm developed by our colleagues in Belgium for establishing cannabis allergy in adult nonmedical users,56 we propose modifications that may be suitable for assessing occupational cannabis allergies (Figure 2).
Figure 2. Flow chart showing proposed diagnostics steps in establishing occupational cannabis allergies.
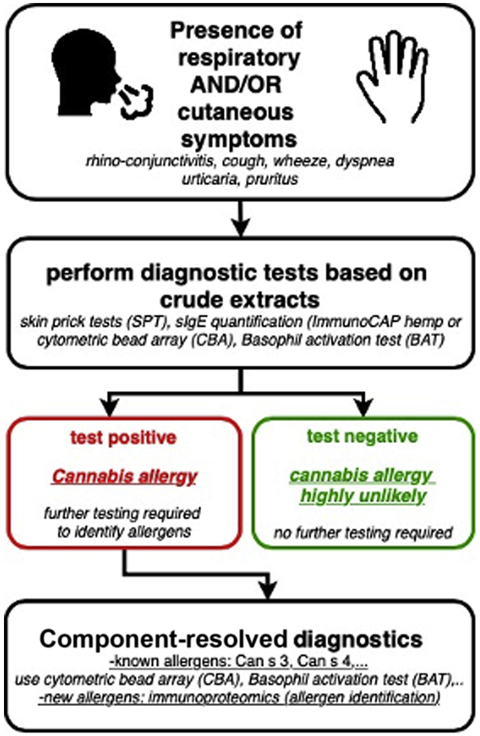
This scheme is based on evidence from examining allergic sensitization to cannabis among non-medicinal users. In absence of strong evidence from occupational allergy cases, this diagnostic algorithm should be considered as a proposal with an expectation that this approach will be refined as more data is available in the future. As indicated literature indicates that testing should be done only in symptomatic individuals. Any symptomatic exposure to cannabis in the workplace will need thorough evaluation of the exposure history. While asymptomatic workers are unlikely to seek medical attention, this group may be included in any employment pre-screening, surveillance and monitoring programs. Skin prick testing with crude protein extracts generated from cannabis or from dust samples from specific operations may be helpful in establishing specific allergic sensitization. Further, additional laboratory-based investigations using ImmunoCAP, BAT, CBA (with specific allergens Can s 3 and Can s 4) and immunoproteomics will assist in allergen identification and validation. In workers with a negative SPT to crude allergens, further testing is not essential. For negative SPT to specific allergens, cannabis allergies could be still possible, although it rules out Can s 3 and Can s 4 as potential allergens.
Challenges associated with developing diagnostics
While significant strides have been made in understanding the profile of true cannabis allergies, many challenges exist.64 Although cannabis is popularly understood as a single entity, there are over 10,000 varieties and the list is constantly growing with the introduction of new strains. Accounting for differences within strains is currently not feasible for each study. The current legal status of the plant, and the practical challenges of studying Schedule I substances in the U.S, have also contributed to the challenges. More recent studies indicate that cannabis exposure by itself is not always sufficient to explain symptomatic outcomes.44 Cannabis grow facilities are heterogeneous operations where workers are exposed to many other possible triggers that are associated with the plant, soil, or components of the surrounding environment. Indeed, secondary sources of exposure including bacteria, fungi and endotoxin have recently been identified in several NIOSH Health Hazard Evaluation studies.65-69 Overall, the endotoxin levels measured were substantially lower than those reported in earlier studies of the European hemp industry and were lower than the Dutch Expert Committee on Occupational Safety exposure limit of 90 EU/m3.17, 70 16S gene sequencing of worker’s breathing zone samples also identified a broad diversity of bacterial species including Actinobacteria.65, 68 Fungi are also common contaminants due to the requirement of high humidity conditions for cannabis plant growth, particularly during the seedling stage, and have been found in administrative areas and personal samples in the NIOSH’s health hazard evaluations.65, 66, 68 Pathogens such as Botrytis cinerea that causes grey mold disease on the cannabis plant have been reported, including in personal worker breathing zone samples.68
TREATMENT OF CANNABIS ALLERGIES
Typically, complete avoidance of the offending sources of allergen can lead to symptomatic improvement. This can be challenging in an occupational setting but may be necessary in the case of anaphylaxis. Use of personal protective equipment (PPE) and introduction of engineering and administrative mitigation efforts may also minimize or eliminate the risk for workers.
Antihistamines, topical nasal steroids, bronchodilators and inhalers may be helpful to manage symptoms. In general, immunotherapy has not been used extensively for treating occupational allergies.71, 72 There is only one case-report (conference proceeding) describing successful immunotherapy for occupational cannabis allergy symptoms (including anaphylaxis) with the help of omalizumab.73 In the future, designed protocols with exposure to smaller amounts of crude cannabis proteins may assist in establishing immunotolerance.
CONCLUDING REMARKS
With legalization of cannabis, there has been a gradual emergence of workers presenting with allergic symptoms from employment in the cannabis industry, handling cannabis during law enforcement activities, as well as adult nonmedical users.33, 40, 44 Less stigmatization, and a greater openness to discuss with healthcare providers may also play a role in increased documentation and awareness. There may be reservations about handling a federally illegal, even if state sanctioned, cannabis product; however, the priority of caring for the patient’s health may outweigh this dilemma, because getting clarity on what can be achieved clinically may be needed. Although the history and clinical presentation of symptoms can help in differentiating allergic from non-allergic cases, specific diagnostic measures may be critical to further help this distinction. The most accessible technique remains SPT, which can be performed with fresh materials preferentially originating from the patient’s environment or with laboratory produced standardized extracts. However, these techniques remain highly variable and the sensitivity may vary. Laboratory-based approaches may provide more insight in identifying the molecular drivers of cannabis allergy; however, these are currently for research use only. Symptoms may also be caused by irritant exposures leading to reactive airways dysfunction syndrome (RADS), complicated by the presence of plant cannabinoids that have immunomodulatory properties. There is some evidence as well for delayed type hypersensitivity reaction demonstrated by positive patch testing34 in a forensic worker, and in early in vitro experiments.74 Eventually,the development of objective diagnostic measures will be helpful in separating true IgE-mediated cannabis allergies from non-immunologic irritant reactions to the plant and the industry.
Supplementary Material
ACKNOWLEDGEMENTS
This work was supported in part by the National Institute of Allergy and Infectious Diseases (NIAID/NIH) Grant R21AI140411 (A.P.N.) and from The Lambert Center for The Study of Medicinal Cannabis & Hemp (Thomas Jefferson University, Philadelphia). This work was also supported by the Agency for Innovation by Science and Technology, Belgium (grant number 140185). Furthermore, D. G. Ebo is a senior clinical researcher of the Research Foundation Flanders/Fonds Wetenschappelijk Onderzoek (FWO: 1800614N). The findings and the conclusions in this report are those of the authors and do not necessarily represent the official position of the National Institute for Occupational Safety and Health, Centers for Disease Control and Prevention.
Abbreviations
- BAT
basophil-activation test
- CBA
cytometric bead array
- CDPHE
Colorado Department of Public Health and Environment
- CRD
Component Resolved Diagnostics
- HMW
high molecular weight
- LMW
low molecular weight
- NIOSH
National Institute for Occupational Safety and Health
- nsLTP
non-specific lipid transfer protein
- OEEP2
oxygen evolving and enhancing protein 2
- PELs
Permissible Exposure Limits
- PFT
pulmonary function test
- PVDF
polyvinylidene difluoride
- RADS
reactive airways dysfunction syndrome
- RELs
recommended exposure limits
- SPT
skin prick test
- THC
Δ9-tetrahydrocannabinol
- UNODC
United Nations Office on Drugs and Crime
- U.S.
United States
- VOCs
volatile organic compounds
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
CONFLICTS OF INTEREST
The authors have no conflict of interest.
REFERENCES
- 1.Johnson R Hemp as an agricultural commodity. Congressional Research Service, 2018. [Google Scholar]
- 2.Boehnke KF, Gangopadhyay S, Clauw DJ, Haffajee RL. Qualifying Conditions Of Medical Cannabis License Holders In The United States. Health Aff (Millwood) 2019; 38:295–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hill KP. Cannabis Use and Risk for Substance Use Disorders and Mood or Anxiety Disorders. JAMA 2017; 317:1070–1. [DOI] [PubMed] [Google Scholar]
- 4.Hill KP, Palastro MD. Medical cannabis for the treatment of chronic pain and other disorders: misconceptions and facts. Pol Arch Intern Med 2017; 127:785–9. [DOI] [PubMed] [Google Scholar]
- 5.Campbell G, Stockings E, Nielsen S. Understanding the evidence for medical cannabis and cannabis-based medicines for the treatment of chronic non-cancer pain. Eur Arch Psychiatry Clin Neurosci 2019; 269:135–44. [DOI] [PubMed] [Google Scholar]
- 6.Boehnke KF, Scott JR, Litinas E, Sisley S, Williams DA, Clauw DJ. Pills to Pot: Observational Analyses of Cannabis Substitution Among Medical Cannabis Users With Chronic Pain. J Pain 2019; 20:830–41. [DOI] [PubMed] [Google Scholar]
- 7.UNODC. World Drug Report. 2017.
- 8.Barcott B, Downs D, Chant I. Leafly Jobs Report 2020. Leafly, 2020. [Google Scholar]
- 9.Velvart J, Stavrovska O. [Health of Workers Engaged in the Processing of Hemp]. Prac Lek 1963; 15:153–7. [PubMed] [Google Scholar]
- 10.Barbero A, Flores R. Dust disease in hemp workers. Arch Environ Health 1967; 14:529–32. [DOI] [PubMed] [Google Scholar]
- 11.Valic F, Zuskin E, Walford J, Kersic W, Paukovic R. Byssinosis, chronic bronchitis, and ventilatory capacities in workers exposed to soft hemp dust. Br J Ind Med 1968; 25:176–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zuskin E, Kanceljak B, Pokrajac D, Schachter EN, Witek TJ Jr. Respiratory symptoms and lung function in hemp workers. Br J Ind Med 1990; 47:627–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zuskin E, Kanceljak B, Schachter EN, Witek TJ, Maayani S, Goswami S, et al. Immunological findings in hemp workers. Environ Res 1992; 59:350–61. [DOI] [PubMed] [Google Scholar]
- 14.Zuskin E, Mustajbegovic J, Schachter EN. Follow-up study of respiratory function in hemp workers. Am J Ind Med 1994; 26:103–15. [DOI] [PubMed] [Google Scholar]
- 15.Er M, Emri SA, Demir AU, Thorne PS, Karakoca Y, Bilir N, et al. Byssinosis and COPD rates among factory workers manufacturing hemp and jute. Int J Occup Med Environ Health 2016; 29:55–68. [DOI] [PubMed] [Google Scholar]
- 16.Bouhuys A, Zuskin E. Byssinosis: occupational lung disease in textile workers In: Frazier CA, editor. Occupational asthma. New York, NY: Von Nostrand Reinhold International; 1979. [Google Scholar]
- 17.Fishwick D, Allan LJ, Wright A, Curran AD. Assessment of exposure to organic dust in a hemp processing plant. Ann Occup Hyg 2001; 45:577–83. [PubMed] [Google Scholar]
- 18.Fishwick D, Allan LJ, Wright A, Barber CM, Curran AD. Respiratory symptoms, lung function and cell surface markers in a group of hemp fiber processors. Am J Ind Med 2001; 39:419–25. [DOI] [PubMed] [Google Scholar]
- 19.Smith GF, Coles GV, Schilling RS, Walford J. A study of rope workers exposed to hemp and flax. Br J Ind Med 1969; 26:109–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mc LNR, Pickering CA. Byssinosis: a review. Thorax 1996; 51:632–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bouhuys A, Wolfson RL, Horner DW, Brain JD, Zuskin E. Byssinosis in cotton textile workers. Respiratory survey of a mill with rapid labor turnover. Ann Intern Med 1969; 71:257–69. [DOI] [PubMed] [Google Scholar]
- 22.Elwood PC, Pemberton J, Merrett JD, Carey GC, McAulay IR. Byssinosis and Other Respiratory Symptoms in Flax Workers in Northern Ireland. Br J Ind Med 1965; 22:27–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Saha A, Das A, Chattopadhyay BP, Alam J, Dasgupta TK. A Comparative Study of Byssinosis in Jute Industries. Indian J Occup Environ Med 2018; 22:170–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.GVR. U.S. Cannabis Market Size, Share & Trends Analysis Report By Cannabis Type (Medical, Recreational), By Product Type (Buds, Oils, Tincture), By Medical Application, (Chronic Pain, Mental Disorder, Cancer), And Segment Forecasts, 2019 - 2025. San Francisco, CA: Grand View Research, 2019. [Google Scholar]
- 25.Barcott B, Whitney B. Special report: Cannabis jobs count. Leafly, 2020. [Google Scholar]
- 26.CDPHE. Guide to Worker Safety and Health in the Marijuana Industry. 2017.
- 27.Couch JR, Grimes GR, Green BJ, Wiegand DM, King B, Methner MM. Review of NIOSH Cannabis-Related Health Hazard Evaluations and Research. Ann Work Expo Health 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Brown CE, Shore E, Van Dyke MV, Scott J, Smith R. Evaluation of an Occupational Safety and Health Training for Cannabis Cultivation Workers. Ann Work Expo Health 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Martyny JW, Serrano KA, Schaeffer JW, Van Dyke MV. Potential exposures associated with indoor marijuana growing operations. J Occup Environ Hyg 2013; 10:622–39. [DOI] [PubMed] [Google Scholar]
- 30.Cuypers E, Vanhove W, Gotink J, Bonneure A, Van Damme P, Tytgat J. The use of pesticides in Belgian illicit indoor cannabis plantations. Forensic Sci Int 2017; 277:59–65. [DOI] [PubMed] [Google Scholar]
- 31.Wiegand DM, Methner MM, Grimes GR, Couch JR, Wang L, Zhang L, et al. Occupational Exposure to Secondhand Cannabis Smoke Among Law Enforcement Officers Providing Security at Outdoor Concert Events. Ann Work Expo Health 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Herzinger T, Schopf P, Przybilla B, Rueff F. IgE-mediated hypersensitivity reactions to cannabis in laboratory personnel. Int Arch Allergy Immunol 2011; 156:423–6. [DOI] [PubMed] [Google Scholar]
- 33.Lindemayr H, Jager S. [Occupational immediate type allergy to hemp pollen and hashish (author's transl)]. Derm Beruf Umwelt 1980; 28:17–9. [PubMed] [Google Scholar]
- 34.Majmudar V, Azam NA, Finch T. Contact urticaria to Cannabis sativa. Contact Dermatitis 2006; 54:127. [DOI] [PubMed] [Google Scholar]
- 35.Mayoral M, Calderon H, Cano R, Lombardero M. Allergic rhinoconjunctivitis caused by Cannabis sativa pollen. J Investig Allergol Clin Immunol 2008; 18:73–4. [PubMed] [Google Scholar]
- 36.Williams C, Thompstone J, Wilkinson M. Work-related contact urticaria to Cannabis sativa. Contact Dermatitis 2008; 58:62–3. [DOI] [PubMed] [Google Scholar]
- 37.Silvers WS. A Colorado allergist's experience with marijuana legalization. Ann Allergy Asthma Immunol 2016; 116:175–7. [DOI] [PubMed] [Google Scholar]
- 38.Decuyper II, Van Gasse AL, Faber MA, Elst J, Mertens C, Rihs HP, et al. Exploring the Diagnosis and Profile of Cannabis Allergy. J Allergy Clin Immunol Pract 2019; 7:983–9 e5. [DOI] [PubMed] [Google Scholar]
- 39.Nayak AP, Green BJ, Sussman G, Berlin N, Lata H, Chandra S, et al. Characterization of Cannabis sativa allergens. Ann Allergy Asthma Immunol 2013; 111:32–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tessmer A, Berlin N, Sussman G, Leader N, Chung EC, Beezhold D. Hypersensitivity reactions to marijuana. Ann Allergy Asthma Immunol 2012; 108:282–4. [DOI] [PubMed] [Google Scholar]
- 41.Gamboa P, Sanchez-Monge R, Sanz ML, Palacin A, Salcedo G, Diaz-Perales A. Sensitization to Cannabis sativa caused by a novel allergenic lipid transfer protein, Can s 3. J Allergy Clin Immunol 2007; 120:1459–60. [DOI] [PubMed] [Google Scholar]
- 42.Rihs HP, Armentia A, Sander I, Bruning T, Raulf M, Varga R. IgE-binding properties of a recombinant lipid transfer protein from Cannabis sativa. Ann Allergy Asthma Immunol 2014; 113:233–4. [DOI] [PubMed] [Google Scholar]
- 43.Stadtmauer G, Beyer K, Bardina L, Sicherer SH. Anaphylaxis to ingestion of hempseed (Cannabis sativa). J Allergy Clin Immunol 2003; 112:216–7. [DOI] [PubMed] [Google Scholar]
- 44.Decuyper II, Van Gasse A, Faber MA, Mertens C, Elst J, Rihs HP, et al. Occupational cannabis exposure and allergy risks. Occup Environ Med 2019; 76:78–82. [DOI] [PubMed] [Google Scholar]
- 45.Larramendi CH, Lopez-Matas MA, Ferrer A, Huertas AJ, Pagan JA, Navarro LA, et al. Prevalence of sensitization to Cannabis sativa. Lipid-transfer and thaumatin-like proteins are relevant allergens. Int Arch Allergy Immunol 2013; 162:115–22. [DOI] [PubMed] [Google Scholar]
- 46.Armentia A, Castrodeza J, Ruiz-Munoz P, Martinez-Quesada J, Postigo I, Herrero M, et al. Allergic hypersensitivity to cannabis in patients with allergy and illicit drug users. Allergol Immunopathol (Madr) 2011; 39:271–9. [DOI] [PubMed] [Google Scholar]
- 47.Rojas Perez-Ezquerra P, Sanchez-Morillas L, Davila-Ferandez G, Ruiz-Hornillos FJ, Carrasco Garcia I, Herranz Manas M, et al. Contact urticaria to Cannabis sativa due to a lipid transfer protein (LTP). Allergol Immunopathol (Madr) 2015; 43:231–3. [DOI] [PubMed] [Google Scholar]
- 48.Biedermann T, Winther L, Till SJ, Panzner P, Knulst A, Valovirta E. Birch pollen allergy in Europe. Allergy 2019; 74:1237–48. [DOI] [PubMed] [Google Scholar]
- 49.Freeman GL. Allergic skin test reactivity to marijuana in the Southwest. West J Med 1983; 138:829–31. [PMC free article] [PubMed] [Google Scholar]
- 50.Stokes JR, Hartel R, Ford LB, Casale TB. Cannabis (hemp) positive skin tests and respiratory symptoms. Ann Allergy Asthma Immunol 2000; 85:238–40. [DOI] [PubMed] [Google Scholar]
- 51.Torre FD, Limonta A, Molinari A, Masala E, Vercelloni S, Torre ED. Cannabaceae pollen in the atmosphere of Brianza, Northen Italy. Eur Ann Allergy Clin Immunol 2007; 39:9–11. [PubMed] [Google Scholar]
- 52.Parker KA, Di Mattia A, Shaik F, Ortega JCC, Whittle R. Risk management within the cannabis industry: Building a framework for the cannabis industry. Financial Markets, Institutions and Instruments 2019; 28:3–55. [Google Scholar]
- 53.Malo JL, Yeung MC. Occupational asthma In: Adkinson NF, Bochner BS, Busse WW, Holgate ST, Lemanske RF Jr., Simons FSR, editors. Middleton’s Allergy: Principles & Practice. Seventh ed: Mosby Elsevier; 2009. p. 939–56. [Google Scholar]
- 54.Nayak AP, Green BJ, Sussman G, Beezhold DH. Allergenicity to Cannabis sativa L. and methods to assess personal exposure. In: Chandra S, Lata H, ElSohly M, editors. Cannabis sativa L. - Botany and Biotechnology; 2017. [Google Scholar]
- 55.Decuyper II, Rihs HP, Mertens CH, Van Gasse AL, Elst J, De Puysseleyr L, et al. A new cannabis allergen in North-western Europe; the oxygen-evolving enhancer protein 2 (OEEP2). J Allergy Clin Immunol Pract 2020. [DOI] [PubMed] [Google Scholar]
- 56.Decuyper II, Rihs HP, Van Gasse AL, Elst J, De Puysseleyr L, Faber MA, et al. Cannabis allergy: what the clinician needs to know in 2019. Expert Rev Clin Immunol 2019; 15:599–606. [DOI] [PubMed] [Google Scholar]
- 57.Decuyper II, Van Gasse AL, Cop N, Sabato V, Faber MA, Mertens C, et al. Cannabis sativa allergy: looking through the fog. Allergy 2017; 72:201–6. [DOI] [PubMed] [Google Scholar]
- 58.Liskow B, Liss JL, Parker CW. Allergy to marihuana. Ann Intern Med 1971; 75:571–3. [DOI] [PubMed] [Google Scholar]
- 59.Armentia A, Herrero M, Martin-Armentia B, Rihs HP, Postigo I, Martinez-Quesada J. Molecular diagnosis in cannabis allergy. J Allergy Clin Immunol Pract 2014; 2:351–2. [DOI] [PubMed] [Google Scholar]
- 60.Gorski P, Krakowiak A, Ruta U. Nasal and bronchial responses to flour-inhalation in subjects with occupationally induced allergy affecting the airway. Int Arch Occup Environ Health 2000; 73:488–97. [DOI] [PubMed] [Google Scholar]
- 61.Decuyper II, Faber MA, Sabato V, Bridts CH, Hagendorens MM, Rihs HP, et al. Where there's smoke, there's fire: cannabis allergy through passive exposure. J Allergy Clin Immunol Pract 2017; 5:864–5. [DOI] [PubMed] [Google Scholar]
- 62.Ebo DG, Swerts S, Sabato V, Hagendorens MM, Bridts CH, Jorens PG, et al. New food allergies in a European non-Mediterranean region: is Cannabis sativa to blame? Int Arch Allergy Immunol 2013; 161:220–8. [DOI] [PubMed] [Google Scholar]
- 63.Chen KZ. [Occupational asthma induced by sisal hemp]. Zhonghua Yi Xue Za Zhi 1986; 66:282–5, 320. [PubMed] [Google Scholar]
- 64.Sussman GL, Beezhold DH, Cohn JR, Silvers WS, Zeiger JS, Nayak AP. Cannabis: An Emerging Occupational Allergen? Ann Work Expo Health 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Couch J, Lowe B, Burton NC, Green BJ, Nayak A, Lemons AR, et al. Evaluation of Potential Hazards during Harvesting and Processing Cannabis at an Outdoor Organic Farm Health Hazard Evaluation Program: USDHHS/CDC/NIOSH, 2017. [Google Scholar]
- 66.Couch J, Wiegand D, Grimes GR, Green BJ, Lemons AR, Glassford E, et al. Evaluation of a Medicinal Cannabis Manufacturing Faclity with an Indoor and Outdoor Grow Operation Health Hazard Evaluation Program: USDHHS/CDC/NIOSH, 2018. [Google Scholar]
- 67.Couch J, Burton NC, Victory KR, Green BJ, Lemons AR, Nayak AP, et al. Endotoxin exposures during harvesting and processing cannabis at an outdoor cannabis farm. Aerobiologia 2019; 35:367–71. [Google Scholar]
- 68.Green BJ, Couch JR, Lemons AR, Burton NC, Victory KR, Nayak AP, et al. Microbial hazards during harvesting and processing at an outdoor United States cannabis farm. J Occup Environ Hyg 2018; 15:430–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Couch JR, Grimes GR, Wiegand DM, Green BJ, Glassford EK, Zwack LM, et al. Potential occupational and respiratory hazards in a Minnesota cannabis cultivation and processing facility. Am J Ind Med 2019; 62:874–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.DECOS. Endotoxins: health-based recommended occupational exposure limit The Hague: Health Council of the Netherlands, Dutch Expert Committee on Occupational Safety, 2010. [Google Scholar]
- 71.Moscato G, Pala G, Sastre J. Specific immunotherapy and biological treatments for occupational allergy. Curr Opin Allergy Clin Immunol 2014; 14:576–81. [DOI] [PubMed] [Google Scholar]
- 72.Vandenplas O, Suojalehto H, Aasen TB, Baur X, Burge PS, de Blay F, et al. Specific inhalation challenge in the diagnosis of occupational asthma: consensus statement. Eur Respir J 2014; 43:1573–87. [DOI] [PubMed] [Google Scholar]
- 73.Engler DB, Malick AA, Saraf SK, Dargel LA. Severe Marijuana Allergy Controlled with Omalizumab. Journal of Allergy and Clinical Immunology 2013; 131:AB215. [Google Scholar]
- 74.Watson ES, Murphy JC, Turner CE. Allergenic properties of naturally occurring cannabinoids. J Pharm Sci 1983; 72:954–5. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


