Abstract
The emergence of alternate variants of SARS-CoV-2 due to ongoing adaptations in humans and following human-to-animal transmission has raised concern over the efficacy of vaccines against new variants. We describe human-to-animal transmission (zooanthroponosis) of SARS-CoV-2 and its implications for faunal virus persistence and vaccine-mediated immunity.
Keywords: SARS-CoV-2, zooanthroponosis, persistence, immunity, re-emergence
The emergence of alternate variants of SARS-CoV-2 due to ongoing adaptations in humans and following human-to-animal transmission has raised concern over the efficacy of vaccines against new variants. We describe human-to-animal transmission (zooanthroponosis) of SARS-CoV-2 and its implications for faunal virus persistence and vaccine-mediated immunity.
Main text
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) emerged as an evident human pathogen in December 2019 and has since infected millions. SARS-CoV-2 is speculated to have evolved in Rhinolophid bats before spilling over into humans, likely via an intermediate animal species which has yet to be confidently identified. The rapid transmission of SARS-CoV-2 in humans has caused the largest coronavirus pandemic in documented history and has caused tremendous loss to the economy in addition to unfathomable loss of human lives. Multiple vaccines have been or are being developed to curb the spread of SARS-CoV-2 among humans; however, there is an underlying threat that can set us back several months in our attempts to eliminate SARS-CoV-2: emergence of alternate variants of SARS-CoV-2 with epitopes that may escape neutralizing antibodies generated by current vaccines.
SARS-CoV-2 variants containing mutations in the spike protein (D614G mutation) with enhanced infection (in vitro) and transmission potential (in Syrian hamsters) have been reported (Hou et al., 2020). Recently, a naturally evolved N439K mutation in the spike protein of SARS-CoV-2 has been suggested to confer resistance to antibody-mediated neutralization (Thomson et al., 2020). More recently, multiple variants of SARS-CoV-2 with mutations have been detected independently in the United Kingdom, Brazil, Nigeria, and South Africa. Given the nature of coronavirus replication, it is likely that there are other variants circulating undetected in various parts of the world. Early epidemiological analyses indicate that the UK SARS-CoV-2 variant (VOC 202012/01) is transmitted at a much faster rate—up to 56% relative to pre-existing SARS-CoV-2 variants. More importantly, mutations within the spike protein of these variants have raised concerns about the efficacy of vaccine and natural infection-mediated protection against SARS-CoV-2. Questions remain about selection pressures that may have favored the evolution and transmission of these alternate variants of SARS-CoV-2. In addition to ongoing adaptations in SARS-CoV-2, the ability of SARS-CoV-2 to infect animal populations (Lam et al., 2020; Shi et al., 2020) raises important questions about 1) potential alternate animal reservoirs of SARS-CoV-2 and 2) emergence of vaccine-resistant variants of SARS-CoV-2 from animals. In this article, we discuss human-to-animal transmission (zooanthroponosis) of SARS-CoV-2 along with its implications for faunal virus persistence and vaccine-mediated immunity.
Zooanthroponotic potential of SARS-CoV-2
All pathogenic human coronaviruses (CoVs) have their origin in animals (Cui et al., 2019). However, the impact of human-to-animal transmission of CoVs has not been extensively studied. In light of the COVID-19 pandemic, it has now become critical to understand the range of animals that are susceptible and permissive to SARS-CoV-2, along with identifying variants of SARS-CoV-2 that evolve and are selected for in these animals. Recent observational and experimental studies have identified a range of animals—such as cats, ferrets, hamsters, non-human primates, minks, tree shrews, raccoon dogs, fruit bats, and rabbits—that are susceptible and permissive to SARS-CoV-2 infection (cross-referenced here: Oude Munnink et al., 2021). More recently, human-to-mink and mink-to-human transmission of SARS-CoV-2 was reported in mink farms in the Netherlands (Oude Munnink et al., 2021).
Although multiple species of animals have now been identified as susceptible to SARS-CoV-2, there are currently no attempts at active surveillance to identify additional animal species that may be susceptible to this virus. In the absence of such efforts, we are currently unaware of the full range of animals that may acquire SARS-CoV-2 from humans or other susceptible mammals. In addition, the health impacts of SARS-CoV-2 infection in animals are unknown. More importantly, we are unable to predict if SARS-CoV-2 will evolve in certain animal species to re-emerge and infect humans who have been naturally exposed to or vaccinated for SARS-CoV-2.
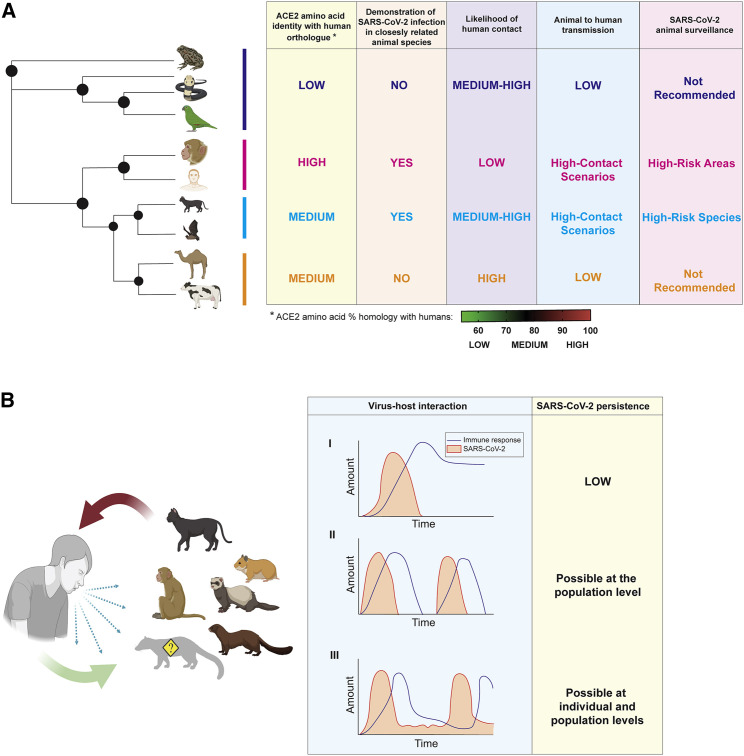
Logistically, it is difficult to survey every known animal species for SARS-CoV-2 susceptibility. To prioritize animal species for surveillance, we propose a hierarchical model based on three variables: (1) SARS-CoV-2 primary receptor angiotensin-converting enzyme 2 (ACE2) homology and evolutionary relationship with known mammalian species that have been identified as “susceptible,” (2) likelihood of that animal species to come in contact with infected humans, and (3) detection of natural or experimental SARS-CoV-2 infection in closely related animal species. The summation of the three variables will predict the likelihood of animal-to-human transmission of SARS-CoV-2 (Figure 1 A). For example, amphibians have low ACE2 homology with humans, and there have been no documented cases of SARS-CoV-2 infection in this group of animals. Thus, the impetus for SARS-CoV-2 surveillance in amphibians is currently low (Figure 1A). Similarly, although ACE2 homology is the highest between humans and non-human primates, the likelihood of contact between these species is low. Thus, surveillance should only be implemented in high-risk areas, such as zoos and wildlife conservation units, where human handlers should be monitored for SARS-CoV-2 infection.
Figure 1.
Zooanthroponotic transmission of SARS-CoV-2
Bidirectional transmission of SARS-CoV-2 between humans and animals raises important questions about surveillance of susceptible animal species and virus persistence in alternate animal reservoirs.
(A) Proposed hierarchical system to prioritize selected animal species for SARS-CoV-2 surveillance based on receptor homology, detection of virus infection, likelihood of animal-human interaction, and risk of animal-to-human transmission of the virus. A hypothetical phylogenetic tree is used to indicate mammalian species. Degree of ACE2 homology with human ACE2 sequence was extracted from recent data (Banerjee et al., 2020), and the heatmap indicates the range of percentages that constitute low, medium, and high ACE2 amino acid homology with the human ortholog. High-contact scenarios represent anthropogenic behavior that facilitates animal-human contact such as domestication and farming. High-risk species represent selected animal species, such as domestic cats, that are likely to be over-represented in high-contact scenarios. High-risk areas constitute environmental settings that would facilitate increased human-animal contact, such as zoos and wildlife conservation areas.
(B) SARS-CoV-2 can infect and replicate in cats, non-human primates, hamsters, ferrets, minks, and monkeys. There are likely other susceptible mammals that have not been discovered yet (indicated by ?). Thus, the risk of animal-to-human transmission of SARS-CoV-2 exists from all susceptible animal species. Virus-host interaction in susceptible species will dictate the long-term infection status of these animals, which could play out in three different ways.
Scenario I: limiting short-term infection with long-term protective immunity and low chances of virus persistence. In this scenario, infected animals would pose a short-term risk of infecting humans when viremic.
Scenario II: short-term viremia followed by a short period of immunity, which would allow the virus to infect members of an animal species in “waves” as immunity wanes in individuals. This would allow the virus to persist in susceptible animal species at the population level, thus creating long-term risks of virus evolution and re-emergence.
Scenario III: latent SARS-CoV-2 infection in susceptible animal species. The virus may emerge from these animals when immunity wanes. This scenario would enable SARS-CoV-2 to evolve and persist at both individual and population levels in susceptible animals, posing a high risk of re-emergence to infect humans.
A mammalian species with moderate ACE2 homology to humans could be identified as susceptible to SARS-CoV-2. An example of this is the detection of SARS-CoV-2 in cats (Shi et al., 2020; Figure 1A). However, within the family of cats, there are numerous species. In this scenario, prioritization of cat species for SARS-CoV-2 surveillance could be based on the likelihood of a species to come in contact with infected humans. High-risk species such as domestic cats should be studied and surveyed for SARS-CoV-2 prevalence, as should other closely related species that are likely to come in contact with humans through practices (high-contact scenarios) such as agriculture and domestication, e.g., minks and raccoon dogs. Cat species such as cheetahs and leopards are unlikely to come in contact with humans and should be surveyed in high-risk areas that facilitate high-contact scenarios, such as in zoos, animal impounds, and wildlife conservation zones. Similarly, other animals with moderate receptor homology that may have a high contact rate with humans, such as camels and cattle, do not have to be surveyed at the moment for SARS-CoV-2 due to lack of evidence of natural SARS-CoV-2 infection in ungulates. Indeed, experimental exposure of dairy calves to SARS-CoV-2 demonstrated limited virus replication, and no virus spread was observed between infected and co-housed naive calves (Ulrich et al., 2020). In the future, if reports of natural infection in evolutionarily closely related ungulates emerge, the priority for surveillance should be updated as necessary (Figure 1A).
Re-emergence of SARS-CoV-2 from animals
In addition to the unknown risks of SARS-CoV-2 infection on animal health, transmission of the virus to animals also risks the generation of alternate viral reservoirs (Figure 1B). A recent report of back-and-forth transmission of SARS-CoV-2 between humans and minks on mink farms in the Netherlands has sparked widespread interest in zooanthroponotic transmission of SARS-CoV-2 followed by re-emergence to infect human populations (Oude Munnink et al., 2021). Although the authors of this study identified human-to-mink and mink-to-human transmission of SARS-CoV-2 within the same farm, speculations still remain about factors that enabled farm-to-farm spread of the virus (Oude Munnink et al., 2021). More recently, the first case of SARS-CoV-2 infection in a free-ranging, native, wild-caught mink was confirmed in Utah, USA, raising concerns about the spread of SARS-CoV-2 among susceptible wild animals.
SARS-CoV-2 infections in minks can range from subclinical to severe interstitial pneumonia resulting in respiratory signs with increased mortality (Oreshkova et al., 2020; Oude Munnink et al., 2021). While the presence of respiratory disease might allow local authorities to identify and quarantine mink farms with SARS-CoV-2, other animal species, such as cats, may become infected without clinical signs and go undetected despite being highly infectious (Halfmann et al., 2020). Although animal-to-human transmission has only been documented between farmed mink and farm workers for now, it is imperative that we identify the risk of virus re-emergence from animals that are susceptible to SARS-CoV-2. Importantly, we also need to assess whether SARS-CoV-2 has the ability to persist in susceptible animals, similar to the known persistence of feline enteric CoVs in cats (Vogel et al., 2010). In addition, we need to determine the ecological, immunological, and anthropogenic factors that will facilitate the re-emergence of SARS-CoV-2 from alternate animal reservoirs to infect humans or other susceptible animals that share an ecological niche (Figure 1B).
Implications for ongoing human-to-animal and animal-to-human transmission
Infection in a new host provides opportunities for evolutionary changes in a virus, with potential consequences for transmissibility and pathogenicity in humans and effectiveness of a vaccine. Coronaviruses have a wide distribution in avian and mammalian species and exist as quasispecies in an infected host; there is a tendency for recombination when they co-infect the same host. This process can lead to the selection or generation of strains capable of switching hosts, posing a threat to human and animal health (Graham and Baric, 2010). In the case of SARS-CoV-1, which caused the SARS outbreak in 2002–2003, mutations in the spike gene appear to have been essential for the transition between animal-to-human transmission and human-to-human transmission (Song et al., 2005). Although the natural reservoir for SARS-CoV-2 is believed to be Rhinolophid bats, it is possible that a yet-to-be-identified intermediate host was also involved in the ultimate transmission of this virus to humans and likely played a role in its ability to infect humans.
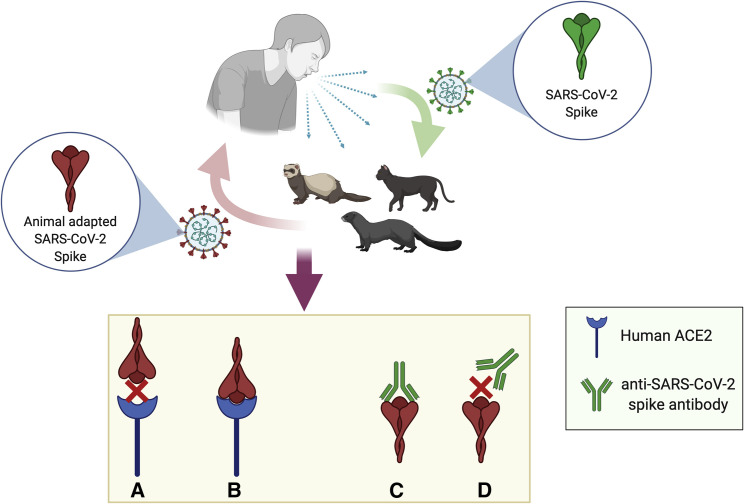
If SARS-CoV-2 were to adapt to and be established in a new animal reservoir, its ability to re-infect humans would depend not only on the interaction of the animal species with humans but also on the evolution of the virus within the new host (Figure 2 ). In spite of the proof-reading ability of the coronavirus replicase complex, coronaviruses exist as quasispecies within an infected host, possibly due to low fidelity of the RNA-dependent RNA polymerase. Thus, adaptive evolution within a new host could lead to the selection of viral variants that are no longer capable of infecting humans and causing disease. Alternately, adaptive evolution could select for viral variants that are more infectious or pathogenic in humans than SARS-CoV-2 and/or able to escape the effects of therapeutics, vaccines, or natural immunity developed against SARS-CoV-2 (Figure 2). If the infection resulted in a less fit virus, with no clinical consequences in the new host, it might go unnoticed. Among the mink-related variants identified to date, only the Cluster 5 variant, which carries four mutations in the spike protein, has raised some concern around vaccine efficacy. Although this variant has not been identified since September 2020, there is no room for complacency (ECDC, 2020).
Figure 2.
Implications of back and forth human-to-animal and animal-to-human transmission of SARS-CoV-2
As SARS-CoV-2 spreads from humans to susceptible animals via zooanthroponosis, the virus may undergo adaptive evolution in the animal host. Mutations within the spike protein of SARS-CoV-2 will determine the likelihood of animal-to-human transmission followed by human-to-human transmission of the animal-adapted variant of SARS-CoV-2. The animal-adapted SARS-CoV-2 will pose no health risk to humans if the altered spike protein can no longer interact with the human cellular receptor, angiotensin-converting enzyme 2 (ACE2) (A). Similarly, if SARS-CoV-2 spike antibodies, either from natural infection or vaccination, can bind to the animal-adapted SARS-CoV-2 spike, there would be no risk of significant disease in an exposed individual and low chances of human-to-human spread of the new virus (C). If the animal-adapted SARS-CoV-2 spike protein is able to bind to human ACE2 (B), the outcome could include enhanced virus transmission and pathogenicity. Alternately, the virus could enter human cells but cause mild to no disease, depending on the overall changes within the genome of the animal-adapted virus. Changes within the spike protein of the animal-adapted SARS-CoV-2 could also affect antibody binding, resulting in the loss of antibody-mediated immunity from vaccination or a previous exposure to SARS-CoV-2 (D).
Mutations within the spike protein of SARS-CoV-2 are particularly important because changes in the antigenic epitopes will create virus populations that would no longer be susceptible to neutralization by antibodies present in vaccinated or naturally infected individuals (Figure 2). A recent study noted that variants of Middle East respiratory syndrome coronavirus (MERS-CoV) with mutations in the spike protein were rapidly selected for and enriched on interacting with its cellular receptor, dipeptidyl peptidase 4 (DPP4), from different bat species in a species-dependent fashion. Subtle differences within the virus receptor (DPP4) in bat cells selected for the best-adapted MERS-CoV variants with mutations within the spike protein for optimal species-specific DPP4-spike interaction (Letko et al., 2018). Thus, as SARS-CoV-2 makes its way through susceptible animal populations, the virus is likely to select for adaptive mutations within the spike protein (Figure 2). The presence of additional SARS-CoV-2 variants with the ability to reinfect vaccinated or immune populations has the potential for devastating consequences for human health (Figure 2). Ongoing sequencing efforts are therefore critical to understanding the nature of SARS-CoV-2 mutations in humans and alternate animal hosts such as mink and also to understanding their implications for vaccine and therapeutic efficacy.
Solutions to curb SARS-CoV-2 transmission at the human-animal and animal-human interface
The global distribution of SARS-CoV-2 presents a challenge to curbing transmission between humans and other susceptible hosts. Recognizing animal species that are most susceptible to infection is the first step in preventing ongoing transmission from humans. However, interactions at the human-animal interface in high-risk areas will need to be carefully managed to avoid opportunities for human-to-animal transmission. This includes strict biosecurity measures such as controlled access to farms that house susceptible animals, bio-secure entry and exit protocols including dedicated personal protective equipment (PPE) such as Tyvek suits or coveralls for the farm, and respiratory and eye protection. Furthermore, disinfection protocols and down time for animal transport vehicles should be implemented along with daily assessments of human handlers for exposure to COVID-19. Much like COVID-19 regulations in senior care homes, working and traveling between multiple animal farms that house SARS-CoV-2-susceptible animals must be minimized or avoided. In the case of intense farming situations such as mink farms, stray cats and rodents have been identified as a potential opportunity for ongoing transmission beyond the farmed animals themselves; SARS-CoV-2 antibodies have been identified in stray cats (Oreshkova et al., 2020). Such animals pose a threat of ongoing transmission to domestic cats and other animals in close contact with humans.
Given the likely bat origin of SARS-CoV-2 (and other zoonotic diseases) and the high diversity of coronaviruses present in bats, this group of mammals has also been recognized as a concern for establishment of new wildlife reservoirs for SARS-CoV-2 (Olival et al., 2020). The highly mobile nature and diversity of bats combined with their ability to host viruses in the absence of clinical disease makes them a particular concern for virus persistence and ongoing transmission to other susceptible hosts. The entry of SARS-CoV-2 into susceptible bat species also presents the opportunity for continued mutation and recombination with endemic bat coronaviruses with unknown potential for pathogenicity and recombination in other susceptible hosts. Thus, strict biosecurity protocols must be followed by human bat handlers. Tourism in bat caves should also be carefully regulated, with mandatory respiratory protection and “no animal handling” policies. The presence of bats or bat colonies on farms that house SARS-CoV-2-susceptible animals, such as minks and ferrets, should be assessed and a contingency plan developed to restrict contact between farmed animals and bats.
While zooanthroponotic infection of farmed animals does pose a challenge, the risk of an ecosystem-level dispersal of SARS-CoV-2 via farmed animals is low. As the preferred first line of defense, biosecurity measures should be implemented in farms that house susceptible animals to prevent human-to-animal and animal-to-animal spread of SARS-CoV-2. If biosecurity measures fail, culling infected animals on the farm as a last resort will help curb the spread of the virus, albeit at the cost of animal life and economic losses. The challenges of controlling the transmission of SARS-CoV-2 within susceptible wildlife species are far greater. The current spread of African swine fever virus (ASFV) is a great example of the devastating impact of infection and virus transmission within domestic and wild animals. While AFSV outbreaks can be controlled in farms by culling infected pigs, uncontrolled movements of wild pigs make it impossible to contain the spread of the virus. ASFV can quickly spread in pig farms, causing billions of dollars in losses and threatening food security and trade. Similarly, raccoon dogs, which are native to South East Asia, are also an invasive species in Europe following their introduction for the fur trade. SARS-CoV-2 infection in raccoon dogs has been demonstrated, but the implications for population and ecosystem-level spread of the virus are unknown. Thus, wildlife infections of SARS-CoV-2 will require an international, coordinated effort for identification and containment along with assessment of the risk of re-emergence in naive and immune human populations.
Zoonotic diseases are continuing to emerge on a more regular basis due to changes in our interactions with wildlife resulting from a variety of anthropogenic factors, including deforestation, climate change, and urbanization. If SARS-CoV-2 were to adapt and be maintained by a new wildlife reservoir, the same principles apply to preventing SARS-CoV-2 from spilling back into humans as to preventing any zoonotic disease from emerging from wildlife in general. We need to avoid close contact between wildlife and humans and our domesticated animal species. Furthermore, we need to invest in awareness programs to educate local human populations about the risks of zoonosis and zooanthroponosis in high-risk areas of wildlife-human interactions. In addition, we need to implement a stronger, more proactive “One Health” research framework to prevent the emergence of novel pathogens at the animal-human interface.
Acknowledgments
A.B. is funded by the Natural Sciences and Engineering Research Council of Canada. This work was supported by a Canadian Institutes of Health Research Rapid COVID-19 grant to principal applicant K.M. and co-applicant A.B. Illustrations were created using GraphPad Prism (version 9), Adobe Illustrator (version 25.0.1), and BioRender.com.
References
- Banerjee A., Doxey A.C., Tremblay B.J., Mansfield M.J., Subudhi S., Hirota J.A., Miller M.S., McArthur A.G., Mubareka S., Mossman K. Predicting the recombination potential of severe acute respiratory syndrome coronavirus 2 and Middle East respiratory syndrome coronavirus. J. Gen. Virol. 2020;101:1251–1260. doi: 10.1099/jgv.0.001491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cui J., Li F., Shi Z.L. Origin and evolution of pathogenic coronaviruses. Nat. Rev. Microbiol. 2019;17:181–192. doi: 10.1038/s41579-018-0118-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ECDC Detection of new SARS-CoV-2 variants related to mink. European Centre for Disease Prevention and Control, Stockholm. 2020. https://www.ecdc.europa.eu/sites/default/files/documents/RRA-SARS-CoV-2-in-mink-12-nov-2020.pdf
- Graham R.L., Baric R.S. Recombination, reservoirs, and the modular spike: mechanisms of coronavirus cross-species transmission. J. Virol. 2010;84:3134–3146. doi: 10.1128/JVI.01394-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halfmann P.J., Hatta M., Chiba S., Maemura T., Fan S., Takeda M., Kinoshita N., Hattori S.I., Sakai-Tagawa Y., Iwatsuki-Horimoto K., et al. Transmission of SARS-CoV-2 in domestic cats. N. Engl. J. Med. 2020;383:592–594. doi: 10.1056/NEJMc2013400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hou Y.J., Chiba S., Halfmann P., Ehre C., Kuroda M., Dinnon K.H., 3rd, Leist S.R., Schäfer A., Nakajima N., Takahashi K., et al. SARS-CoV-2 D614G variant exhibits efficient replication ex vivo and transmission in vivo. Science. 2020;370:1464–1468. doi: 10.1126/science.abe8499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lam T.T., Jia N., Zhang Y.W., Shum M.H., Jiang J.F., Zhu H.C., Tong Y.G., Shi Y.X., Ni X.B., Liao Y.S., et al. Identifying SARS-CoV-2-related coronaviruses in Malayan pangolins. Nature. 2020;583:282–285. doi: 10.1038/s41586-020-2169-0. [DOI] [PubMed] [Google Scholar]
- Letko M., Miazgowicz K., McMinn R., Seifert S.N., Sola I., Enjuanes L., Carmody A., van Doremalen N., Munster V. Adaptive evolution of MERS-CoV to species variation in DPP4. Cell Rep. 2018;24:1730–1737. doi: 10.1016/j.celrep.2018.07.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olival K.J., Cryan P.M., Amman B.R., Baric R.S., Blehert D.S., Brook C.E., Calisher C.H., Castle K.T., Coleman J.T.H., Daszak P., et al. Possibility for reverse zoonotic transmission of SARS-CoV-2 to free-ranging wildlife: A case study of bats. PLoS Pathog. 2020;16:e1008758. doi: 10.1371/journal.ppat.1008758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oreshkova N., Molenaar R.J., Vreman S., Harders F., Oude Munnink B.B., Hakze-van der Honing R.W., Gerhards N., Tolsma P., Bouwstra R., Sikkema R.S., et al. SARS-CoV-2 infection in farmed minks, the Netherlands, April and May 2020. Euro Surveill. 2020;25:2001005. doi: 10.2807/1560-7917.ES.2020.25.23.2001005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oude Munnink B.B., Sikkema R.S., Nieuwenhuijse D.F., Molenaar R.J., Munger E., Molenkamp R., van der Spek A., Tolsma P., Rietveld A., Brouwer M., et al. Transmission of SARS-CoV-2 on mink farms between humans and mink and back to humans. Science. 2021;371:172–177. doi: 10.1126/science.abe5901. Published online November 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi J., Wen Z., Zhong G., Yang H., Wang C., Huang B., Liu R., He X., Shuai L., Sun Z., et al. Susceptibility of ferrets, cats, dogs, and other domesticated animals to SARS-coronavirus 2. Science. 2020;368:1016–1020. doi: 10.1126/science.abb7015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song H.D., Tu C.C., Zhang G.W., Wang S.Y., Zheng K., Lei L.C., Chen Q.X., Gao Y.W., Zhou H.Q., Xiang H., et al. Cross-host evolution of severe acute respiratory syndrome coronavirus in palm civet and human. Proc. Natl. Acad. Sci. USA. 2005;102:2430–2435. doi: 10.1073/pnas.0409608102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomson E.C., Rosen L.E., Shepherd J.G., Spreafico R., da Silva Filipe A., Wojcechowskyj J.A., Davis C., Piccoli L., Pascall D.J., Dillen J., et al. The circulating SARS-CoV-2 spike variant N439K maintains fitness while evading antibody-mediated immunity. bioRxiv. 2020 doi: 10.1016/j.cell.2021.01.037. https://www.biorxiv.org/content/10.1101/2020.11.04.355842v1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ulrich L., Wernike K., Hoffmann D., Mettenleiter T.C., Beer M. experimental infection of cattle with SARS-CoV-2. Emerg. Infect. Dis. 2020;26:2979–2981. doi: 10.3201/eid2612.203799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vogel L., Van der Lubben M., te Lintelo E.G., Bekker C.P., Geerts T., Schuijff L.S., Grinwis G.C., Egberink H.F., Rottier P.J. Pathogenic characteristics of persistent feline enteric coronavirus infection in cats. Vet. Res. 2010;41:71. doi: 10.1051/vetres/2010043. [DOI] [PMC free article] [PubMed] [Google Scholar]