Abstract
Purpose
The aim of this study is to describe the incidence of Acute Kidney Injury (AKI) amongst patients admitted to the Intensive Care Unit (ICU) with COVID-19. In addition we aim to detail the range of Renal Replacement Therapy (RRT) modalities offered to these patients (including peritoneal dialysis - PD - and intermittent haemodialysis - IHD) in order to meet demand during pandemic conditions.
Materials and methods
Single-centre retrospective case note review of adult patients with confirmed COVID-19 admitted to ICU.
Results
Amongst 136 patients without a prior history of End Stage Kidney Disease (ESKD), 108 (79%) developed AKI and 63% of admitted patients received RRT. Due to resource limitations the range of RRT options were expanded from solely Continuous Veno-Venous HaemoDiaFiltration (CVVHDF - our usual standard of care) to include PD (in 35 patients) and IHD (in 15 patients). During the study period the proportion of RRT provided within ICU as CVVHDF fell from 100% to a nadir of 39%. There were no significant complications of either PD or IHD.
Conclusions
During periods of resource limitations PD and IHD can safely be used to reduce dependence on CVVHDF in select patients with AKI secondary to COVID-19.
Keywords: COVID-19, Acute kidney injury, Renal replacement therapy, Peritoneal Dialysis, Haemodialysis
Abbreviations: AKI, Acute Kidney Injury; APD, Automated Pertioneal Dialysis; CCPD, Continuous Cyclic Peritoneal Dialysis; CKD, Chronic Kidney Disease; CRE, Carbapenem Resistant Enterobaceriae; CVVHDF, Continuous Veno-Venous HaemoDiaFiltration; CRRT, Continuous Renal Replacement Therapy; ESKD, End Stage Kidney Disease; IHD, Intermittent Haemodialysis; PIRRT, Prolonged Intermittent Renal Replacement Therapy; RO, Reverse Osmosis; RRT, Renal Replacement Therapy; RT-PCR, Real-Time Polymerase Chain Reaction; SLED, Sustained Low-Efficiency Dialysis; UF, Ultrafiltration
1. Introduction
Between March and June 2020 the COVID-19 global pandemic caused by the novel coronavirus SARS-CoV-2 resulted in an unprecedented surge in admissions to intensive care units (ICU) across the United Kingdom [1]. Acute kidney Injury (AKI) occurs in a substantial proportion of patients who are critically ill with COVID-19. Early published literature from China reported AKI prevalence between 8% and 29% amongst patients admitted to intensive care [[2], [3], [4]], and a review of 13 studies reported a pooled incidence of AKI amongst critically ill patients of 24% but with considerable variation between studies (3% to 66%) [5]. During the early stages of the COVID-19 pandemic there was focus on ventilator availability. However, a shortage of renal replacement therapy (RRT) rapidly became a key limiting step in the ability to provide timely organ support to critically ill COVID-19 patients internationally [6], requiring us to consider approaches previously unused in our department including intermittent haemodialysis (IHD) and acute, automated peritoneal dialysis (aAPD).
King's College Hospital (KCH) is a large university teaching hospital situated in South London, the area of the UK which saw the largest number of ICU admissions during the initial phase of the COVID-19 pandemic [1]. Immediately prior to the onset of the pandemic the King's Critical Care Centre comprised 4 ICUs with 65 beds. 51 of these beds had the capacity to support patients requiring continuous renal replacement therapy (CRRT). In the period between 10/03/2020 and 21/04/2020 the critical care bed pool increased from 65 to a peak of 149.
We conducted a retrospective service evaluation of the incidence of AKI and provision of RRT to assess the efficacy of novel strategies and to inform management in future surges of AKI cases.
2. Methods
Medical records of all patients admitted to ICU with a positive SARS-CoV-2 real time Reverse Transcriptase Polymerase Chain Reaction (RT-PCR) result between 10/03/2020 and 10/05/2020 were reviewed. Patient's hospital outcomes were assessed until discharge or 31/10/2020 (which ever was earlier). Baseline demographic data and relevant co-morbidities including hypertension, diabetes, coronary artery disease and chronic kidney disease (CKD) were recorded.
AKI was defined using the rise from baseline of serum creatinine. When the patient did not have a previous serum creatinine result in the 12 months prior to hospital admission an estimated baseline serum creatinine was used based on age, gender and ethnicity as per international guidelines [7]. AKI stage was based on the Kidney Disease: Improving Global Outcomes (KDIGO) staging system [7].
Patients transferred from other ICUs were excluded from assessment of incidence of AKI as selection for transfer was frequently due to need for RRT.
Overall RRT requirements per day were calculated between 10/03/2020 and 10/05/2020 from the total number of patients admitted to ICU with COVID-19 (including those transferred from other hospitals), and modality of RRT received on that day for each patient. For patients who received PD and/or IHD we recorded any complications of therapy observed during the study period. For all patients who received either PD and/or IHD we recorded the number of days on which they received CRRT either in addition to or instead of PD/IHD, and the reasons for this. For patients receiving PD we recorded biochemical data prior to commencing PD and for the first 3 days afterwards.
This was within the scope of a departmental service evaluation (KCC06052020AIA).
3. Results
3.1. Incidence of acute kidney injury and renal replacement therapy
177 patients with COVID-19 were admitted to King's Critical Care during the time period. 143 patients were admitted from within King's College Hospital and 34 were transferred in from other ICUs. Baseline demographics for the 143 patients admitted from within King's are shown in Table 1 . Baseline serum creatinine concentrations were available for 64 patients (45%) and were estimated for the remaining patients. 23 patients had a diagnosis of chronic kidney disease, 2 with functioning renal transplants and 5 who were dialysis dependent (4 on IHD and 1 on APD) prior to ICU admission.
Table 1.
Baseline and clinical characteristics of patients admitted to critical care with COVID-19.
| Demographics | Total [n = 143] | No AKI [n = 28,19.6%] | AKI stage 1–2 [n = 15, 10.5%, stage1 = 8, 5.6%, stage 2 = 7, 4.9%) | AKI stage 3 [n = 93, 65.0%] |
|---|---|---|---|---|
| Age (years) | [n = 143] | [n = 28] | [n = 15] | [n = 93] |
| Mean (SD) | 56.3 (11.9) | 49.5 (12.2) | 53.3 (14.6) | 59.0 (10.8) |
| Median (IQR) | 57 (50–63) | 50.5 (42.5–60.5) | 57 (41–65) | 59 (52–65) |
| Sex, n (%) | [n = 143] | [n = 28] | [n = 15] | [n = 93] |
| Female | 48 (33.6) | 13 (46.4) | 5 (33.3) | 27 (29.0) |
| Male | 95 (66.4) | 15 (53.6) | 10 (66.7) | 66 (71.0) |
| Ethnicity, n (%) | [n = 141] | [n = 28] | [n = 14] | [n = 92] |
| White | 43 (30.5) | 9 (32.1) | 8 (57.1) | 24 (26.1) |
| Mixed | 0 | 0 | 0 | 0 |
| Asian | 15 (10.6) | 5 (17.9) | 0 | 9 (9.8) |
| Black | 74 (52.5) | 11 (39.3) | 4 (28.6) | 55 (59.8) |
| Other | 9 (6.4) | 3 (10.7) | 2 (14.3) | 4 (4.3) |
| BMI (kg/m2), n (%) | [n = 134] | [n = 27] | [n = 13] | [n = 88] |
| <18.5 | 1 (0.7) | 0 | 0 | 1 (1.1) |
| 18.5–<25 | 38 (28.4) | 9 (33.3) | 2 (15.4) | 26 (29.5) |
| 25–<30 | 46 (34.3) | 11 (40.7) | 4 (30.8) | 28 (31.8) |
| 30–<40 | 39 (29.1) | 6 (22.2) | 5 (38.5) | 27 (30.7) |
| 40+ | 10 (7.5) | 1 (3.7) | 2 (15.4) | 6 (6.8) |
| Comorbidities, n (%) | [n = 143] | [n = 28] | [n = 15] | [n = 93] |
| Hypertension | 78 (54.5) | 8 (28.6) | 8 (53.3) | 59 (63.4) |
| Diabetes Mellitus | 63 (44.1) | 6 (21.4) | 7 (46.7) | 45 (48.4) |
| Coronary Artery Disease | 11 (7.7) | 0 | 3 (20) | 8 (8.6) |
| Chronic Kidney Disease | 23 (16.1) | 1 (3.6) | 2 (13.3) | 13 (14.0) |
| Chronic Kidney Disease, n (%) | [n = 143] | [n = 28] | [n = 15] | [n = 93] |
| Stage 3a | 5 (3.5) | 1 (3.6) | 1 (6.7) | 3 (3.2) |
| Stage 3b | 7 (4.9) | 0 | 1 (6.7) | 6 (6.5) |
| Stage 4 | 4 (2.8) | 0 | 0 | 4 (4.3) |
| Stage 5 - PD/IHD | 5 (3.5) | 0 | 0 | 0 |
| Stage 5 - Transplant | 2 (1.4) | 0 | 0 | 0 |
| Organ support, n (%) | [n = 143] | [n = 28] | [n = 15] | [n = 93] |
| MV at any time | 133 (93.0) | 25 (89.3) | 10 (66.7) | 92 (98.9) |
| ECMO at any timea | 10 (7.0) | 1 (3.6) | 0 | 9 (9.7) |
Abbreviations: AKI, acute kidney injury; SD, standard deviation; IQR, interquartile range; BMI, body mass index; ACEi, angiotensin converting enzyme inhibitor; ARB, angiotensin II receptor blocker; MV, mechanical ventilation; ECMO, extracorporeal membrane oxygenation.
Of the 10 patients treated with ECMO, this therapy was provided at our trust in 1 case and the patient was transferred to a regional Severe Respiratory Failure centre in 9 cases.
Of the 136 patients without ESKD, 108 (79%) developed AKI stages 1–3 (Table 1) and 82 patients (60%) commenced RRT, including 12 patients with known CKD stage 3–4 and 70 patients with no prior history of CKD. In addition RRT was provided to 2 patients whose renal transplants failed in the context of severe COVID-19 infection and 5 patients who were already established on RRT for ESKD. In patients who developed AKI, RRT was first initiated a median of 4.5 (IQR 2–7) days after ICU admission. Clinical characteristics of patients prior to commencing RRT are shown in Table 2 . Urine output data for the 6 h prior to commencing RRT was available for 57 patients. 6 patients (11%) were anuric whilst 30 patients (53%) had oligo-anuria (urine output 0.01–0.29 ml/kg/h). Of the 11 patients who developed stage 3 AKI but did not receive RRT, 3 patients experienced renal recovery and were discharged alive, whilst all other patients died in ICU in the context of multiple organ failure. All decisions to withhold RRT in patients who did not survive were made on the grounds that they were not expected to survive irrespective of whether or not they received RRT. No patient did not receive RRT due to actual or potential resource limitations.
Table 2.
Clinical characteristics of patients with AKI prior to commencing RRT for the first time.
| Clinical characteristic | Median (IQR) |
|---|---|
| SCr (micromol/L) [n = 77] | 328 (226–506) |
| Urea (mmol/L) [n = 73] | 20.1 (15.6–30.5) |
| Potassium (mmol/L) [n = 71] | 5.1 (4.4–5.9) |
| Base Excess (mmol/L) [n = 68] | −1.6 (−4.9 − +4.4) |
| p/F ratio (kPa) [n = 66] | 17.9 (11.9–24.8) |
| Noradrenaline dose (mcg/kg/min) [n = 68] | 0.09 (0.00–0.24) |
| Urine output (ml/kg/h) [n = 57] | 0.14 (0.05–0.66) |
| Cumulative fluid balance (litres) [n = 61] | 4.6 (2.0–8.5) |
Abbreviations: SCr, serum creatinine; p/F ratio, ratio of arterial partial pressure of oxygen to fraction of inspired oxygen.
Overall 111 patients (63%) required RRT during the assessment period including those established on long-term RRT prior to ICU admission and 22 patients transferred from other ICUs. All patients received Continuous Veno-Venous HaemoDiaFiltration (CVVHDF) at least once during their admission with the exception of one patient established on PD prior to admission, which was continued; 35 patients (31.5%) received acute APD and 15 patients (13.5%) received IHD.
3.2. Outcomes of patients with AKI
At the time of writing, of the 143 patients admitted directly to KCH, 141 (99%) had a hospital outcome whilst 1 is still receiving care on ICU and 1 has been discharged from ICU but remains within hospital. The overall in-hospital mortality rate was 39.7%. In-hospital mortality was significantly greater in patients who developed AKI (any stage) compared to patients who never developed AKI (50.0% vs. 7.1%, p = 0.00002). In-hospital mortality rates for AKI stage 1, AKI stage 2, AKI stage 3 and AKI requiring RRT were 25.0%, 28.6%, 53.8% and 51.3% respectively.
All patients who received RRT for AKI who have not died in hospital (41 patients, including the 2 who remain as in-patients) have recovered adequate renal function as to be free of RRT. Dialysis-independence rates at 1 and 3 months were 76% and 95% respectively. Median duration of RRT for patients who had renal recovery was 21 days (IQR 13–30 days). Serum creatinine prior to hospital discharge was at or below the upper limit of our laboratory's reference range (120 micromol/L) in 26 patients (67%). Mean serum creatinine at discharge was 130 micromol/L (SD 113 micromol/L).
3.3. Changes to RRT provision during the COVID-19 pandemic
Initially, CVVHDF capacity was increased through obtaining more haemofiltration machines and attempting to improve the life span of filters and circuits by adjustments to our treatment protocols. However, within weeks the number of patients threatened to overwhelm ability to provide RRT to all in need, due to lack of haemofiltration machines and a national issue with the delivery of haemofiltration-related consumables. Thus two new modalities were introduced; firstly acute APD and later IHD. A nephrology consultant supported critical care seven days a week for the duration of the pandemic surge and daily meetings allowed the identification of patients suitable for non CRRT modes of RRT. Methods of acute APD and IHD are described below.
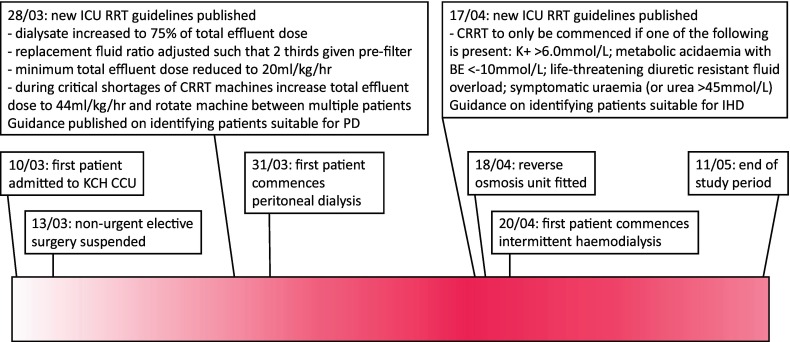
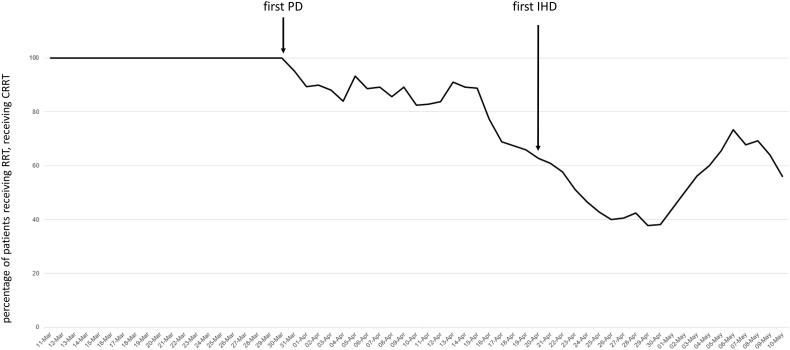
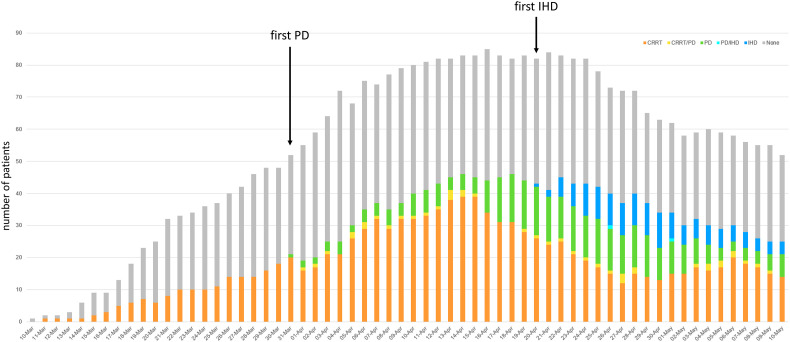
Fig. 1 shows a timeline of these changes. Between 10 March and 30 March 2020, RRT for critically ill COVID-19 patients was provided exclusively using CVVHDF (158 patient days). Between 31 March and 19 April, following the introduction of acute APD, the proportion of RRT provided as CVVHDF fell to 83% (581 out of 701 patient days). Between 20 April and 10 May, following the introduction of IHD the proportion of RRT provided as CVVHDF was 53% (389 out of 732 patient days). On 29 April only 39% of RRT provision was via CVVHDF. Fig. 2 shows the percentage of RRT provided as CVVHDF during the reported period and Fig. 3 demonstrates the number of patients receiving each modality of RRT on each day of the reported period. Between 31/03/2020 and 10/05/2020 a total of 463 patient days of CVVHDF were replaced with either acute APD or IHD.
Fig. 1.
Timeline of interventions introduced to maximise availability of RRT for patients with COVID-19 and severe AKI.
Fig. 2.
Percentage of patients receiving RRT, receiving CRRT.
Fig. 3.
Number of patients admitted to critical care with COVID-19 over time (by modality of RRT received).
3.4. Changes to CVVHDF provision
Our usual method of RRT for patients with AKI is CVVHDF, delivered using a PrisMax machine (Baxter Healthcare, Deerfield, Illinois, United States of America). Nine Prismaflex CRRT machines (Baxter Healthcare, Deerfield, Illinois, United States of America) were acquired from nephrology services and four Aquarius CRRT machines (Edwards Lifesciences AG, Irvine, CA, USA) from the paediatric intensive care unit which increased device capacity from 33 to 46 (an increase of 39%).
Prior to the pandemic our typical CVVHDF prescription was 24–44 ml/kg/h effluent dose (by ideal body weight). Effluent dose was divided on a 1:1 basis between dialysate and replacement fluid, with one third of the replacement fluid given as pre-dilution prior to the blood passing over the filter membrane, to minimise clotting. Anti-coagulation was with either heparin or epoprostenol.
Early in the pandemic that filter longevity appeared to be reduced in COVID-19 patients. An audit of filter usage found that between 10 March and 30 April 2020 we used an average of 0.23 filters/day/patient, and the average filter life-span was 24.3 h, compared with 0.10 new filters/day/patient with an average filter life-span of 31.6 h in 2019. To increase filter lifespan we adjusted ratio of dialysate to replacement fluid from 1:1 to 3:1 to reduce the impact of the procoagulatory effect of filtration [8,9]. In response to the high incidence of filter clotting and anecdotal accounts of a pro-thrombotic state in COVID-19 patients, systemic anti-coagulation with heparin was commenced for all patients receiving CVVHDF targeting an Activated Partial Thromboplastin Time ratio of 2.0–2.5 unless contraindicated.
3.5. Acute automated peritoneal dialysis
Selection of patients for APD was undertaken by a specialist team lead by a Senior Clinical Nurse Specialist, a Consultant Nephrologist and a Consultant in Critical Care. Patients were considered suitable for acute APD if they had a BMI <40 kg/m2, no mid-line laparotomy scar and no known abdominal aortic aneurysm (AAA). In general, patients who were deemed suitable for APD were those who demonstrated an improving clinical trend and who had evidence of a reduction in the level of cardiorespiratory support required (whilst there were no hard criteria for acceptable levels of cardiorespiratory support, patients were generally considered unsuitable if any of the following were present: >1 vasoactive infusion; noradrenaline dose >0.15μg /kg/min ideal body weight; fraction of inspired oxygen ≥0.6; positive end-expiratory pressure ≥ 12 cmH2O; requiring prone positioning). Catheter insertion technique and details of our dialysis prescriptions have been described extensively elsewhere [10]. In brief a three phase PD prescription protocol was developed commencing with low volume rapid exchanges in the first 24–48 h after catheter insertion to minimise the risk of leak at the insertion site but maximise fluid loss if required. The choice of prescription used there after depended upon clinical assessment by the Renal Consultant in partnership with the ICU Consultant and included assessment of fluid balance, ultrafiltration goal, electrolyte status and degree of uraemia. Automated cyclers (Baxter Claria and Homechoice machines) were used in all cases.
During the study period, PD catheter insertion was attempted in 41 patients and was successful in 34 (83%). Unsuccessful catheter insertion was attributed to failure to reach the peritoneum due to obesity (using a 50 mm needle) in 5 patients, omental obstruction in one patient and suspicion of bowel puncture in one patient (this patient was stable post-procedure, with no evidence of intra-abdominal infection or bleeding) [10]. Of the 34 patients who successfully had a PD catheter inserted, 15 (44%) were subsequently treated with PD alone, whilst 19 patients (56%) received supplemental CVVHDF and 2 patients (6%) received at least one session of intermittent haemodialysis. Of the 423 patient days after PD catheter insertion, PD was the sole modality of RRT on 328 days (78%). Reasons cited in the medical record for supplementing PD with CVVHDF or IHD were: clinical deterioration not attributed to PD (n = 5); elevated urea felt to be impacting on the patient's condition (n = 5, serum urea 44.1 ± 7,7 mmol/l), fluid overload or pulmonary oedema (n = 4), hyperkalaemia (n = 3, serum potassium 7.0 ± 0.1 mmol/l), ileus (n = 1) and scrotal oedema (n = 1). There were no reported adverse incidents relating to the use of PD having an impact on ventilatory parameters. No patient underwent prone positioning whilst receiving PD. There were no reported instances of peritonitis in patients receiving PD. Biochemical changes for the first three days following initiation of PD are summarised in Table 4. Mean daily ultrafiltration (UF) for the first three days of PD was 1083 ml (±846 ml).
Table 4.
Details of IHD sessions for patients who received IHD.
| Patient no. | Number of sessions | mean Session duration (hours) (SD) | mean Blood flow (ml/min) (SD) | mean Litres processed (litres) (SD) | mean UF (litres) (SD) | Sessions where filter clotted (n) (%) | Sessions where hypotension was documented (n) (%) |
|---|---|---|---|---|---|---|---|
| 1 | 11 | 3.4 (0.4) | 265 (44) | 42.0 (12.8) | 1.34 (0.52) | 0 | 1 (9.1) |
| 2 | 6 | 3.0 (0.6) | 217 (26) | 37.5 (13.4) | 1.10 (0.76) | 0 | 2 (33.3) |
| 3 | 3 | 2.5 (0.5) | 233 (29) | 37.2 (11.6) | 1.43 (0.40) | 0 | 1 (33.3) |
| 4 | 7 | 3.0 (0.5) | 231 (24) | 41.9 (12.2) | 1.60 (0.47) | 0 | 2 (28.6) |
| 5 | 4 | 2.6 (0.5) | 213 (25) | 36.3 (10.3) | 0.90 (0.14) | 0 | 0 |
| 6 | 7 | 3.1 (0.6) | 240 (34) | 43.9 (11.9) | 1.32 (0.93) | 2 (28.6) | 1 (14.3) |
| 7 | 1 | 2.4 | 200 | 28.8 | 2.00 | 0 | 0 |
| 8 | 3 | 2.2 (1.0) | 200 (0) | 29.7 (6.4) | 1.00 (0.87) | 0 | 2 (66.7) |
| 9 | 1 | 3.3 | 280 | 50.7 | 1.50 | 0 | 0 |
| 10 | 4 | 3.5 (0.8) | 273 (22) | 52.6 (19.0) | 1.46 (0.71) | 2 (50.0) | 1 (25.0) |
| 11 | 9 | 3.5 (0.7) | 276 (35) | 57.0 (16.5) | 1.97 (0.64) | 0 | 0 |
| 12 | 11 | 3.2 (0.8) | 248 (37) | 46.8 (13.1) | 1.20 (0.62) | 2 (18.2) | 0 |
| 13 | 7 | 3.3 (1.0) | 236 (24) | 43.9 (12.7) | 1.21 (0.76) | 1 (14.3) | 0 |
| 14 | 6 | 2.6 (1.3) | 220 (24) | 31.6 (14.8) | 0.87 (0.55) | 0 | 2 (33.3)a |
| 15 | 2 | 2.5 (0.7) | 290 (14) | 43.9 (6.9) | 1.10 (0.14) | 0 | 0 |
| Total | 82 | 3.1 (0.8) | 244 (37) | 43.1 (14.2) | 1.33 (0.66) | 7 (8.5) | 12 (14.6) |
Abbreviation: UF, ultrafiltration.
Includes one session where IHD was terminated due to marked hypotension.
3.6. Intermittent haemodialysis
To further reduce demand for CVVHDF we also introduced the ability to perform intermittent haemodialysis (IHD). Prolonged intermittent RRT (PIRRT) modalities such as sustained low-efficiency dialysis (SLED) were considered but not employed as the longer dialysis sessions would have meant the therapy could have been offered to fewer patients, given the available manpower and equipment.
A reverse osmosis (RO) plant was installed in one of the ICUs on 18th April 2020 and this allowed for the provision of IHD for up to four patients at once. The IHD area was staffed by two intensive care nurses with dialysis provided by dedicated haemodialysis nurses.
All patients receiving RRT were reviewed daily by a consultant nephrologist and consultant intensivist to assess suitability for IHD. Recommended criteria for suitability for IHD were a stable or improving clinical trajectory, modest ventilatory requirements (FiO2 < 0.5), and minimal cardiovascular support (norepinephrine dose < 0.15μg/kg/min). Patients received daily IHD for the first three days followed by three times weekly sessions once established.
A total of 82 haemodialysis sessions were delivered to 15 patients as shown in Table 4. There were no major complications of IHD therapy. Transient hypotension that did not interrupt therapy was reported during 11 sessions (13.4%). On one occasion, there was marked hypotension that led to the session being terminated after 30 min. Circuit thrombosis interrupting therapy occurred on seven occasions (8.5%).
Unfortunately, the use of IHD was curtailed from early May, as an outbreak of carbapenem resistant enterobaceriae (CRE) restricted the ability to transfer patients in and out of the unit where the RO facility was installed.
4. Discussion
During the COVID-19 pandemic our institution successfully reduced the proportion of RRT provided as CVVHDF from 100% to a nadir of 39% by introducing two techniques that are not commonly used in critically ill patients in the UK. These interventions were introduced rapidly but effectively with no significant adverse events.
Initial studies from Wuhan, China, reported wildly varied incidence of AKI in patients hospitalised with COVID-19, ranging from 0.5%to 15% [11,12]. More recently Richardson et al. have reported on 5700 hospitalised patients in New York (United States of America - USA) where incidence of AKI was 24% [13]. Cummings et al. reported that 31% of 257 patients admitted to ICU in New York (USA) required RRT [14]. In the UK the Intensive Care National Audit and Research Centre (ICNARC) have reported that 25.6% of 8533 patients admitted to ICU in the UK required RRT [1]. At 63%, the incidence of RRT requirement at our institution is greater than that reported nationally. Whilst this study was not designed to investigate the reasons for this, it is possible that our cohort had a higher incidence of organ failure, as 93.0% of our patients received invasive mechanical ventilation compared with 72.4% of the national cohort.
PD and IHD are far from novel modalities of RRT in AKI, having been first performed in humans in 1918 and 1924 respectively [15,16]. However, in the UK, it is not common for these modalities to be performed in critically ill patients admitted to Intensive Care. In a 2007 survey of ICUs in the UK only 10% reported ever using IHD (usually only infrequently) and none reported using PD. [17]
King's College Hospital has one of the largest automated peritoneal dialysis (APD) services in the UK and there is considerable local expertise in using PD as first line RRT for AKI. However, at our centre, acute PD is rarely, if ever, used in critically ill patients with AKI. During the pandemic, PD was performed in around one third of patients who received RRT. Our initial concerns prior to commencing PD for the first time included the impact on ventilation in patients receiving mechanical ventilation for ARDS, the risk of PD fluid leaks (especially when nursing patients in the prone position) and the risk of PD peritonitis (especially given patients might be receiving immunosuppression as part of their treatment regime). These anticipated complications did not materialise. No patient received PD whilst nursed in the prone position, therefore we cannot comment on the impact of PD on ventilation in the prone position nor the impact of prone positioning on the efficacy of PD.
However, there were several issues that arose worthy of discussion. Firstly PD did not result in the rapid fall in serum creatinine and urea seen with CRRT (Table 3 ). The majority of patients who received PD for AKI had previously been treated with CRRT (88%), therefore it was common for patients' serum creatinine and urea concentration to initially rise when first commencing PD. Five patients had supplemental CRRT or IHD due to concerns that elevated urea may be contributing to depressed level of consciousness. Secondly ultrafiltration (UF) was calculated daily, so fluid balance charts did not reflect fluid shifts on an hourly basis as they would with CRRT. Four patients had supplemental CRRT as the treating team wished to rapidly increase fluid removal (in the context of pulmonary oedema or global fluid overload) and felt this could be achieved more reliably with CRRT than by adjusting the PD prescription to favour greater UF. Thirdly these patients were critically ill, some deteriorated after commencing PD (never attributed to PD), and in minority of patients intensivists felt it was appropriate to discontinue PD and commence CRRT for this reason.
Table 3.
Biochemical changes after initiation of PD.
| Baseline (prior to commencing PD) | Change from baseline on day 1 | Change from baseline on day 2 | Change from baseline on day 3 | |
|---|---|---|---|---|
| SCr (micromol/L); Mean (SD) | [n = 31]; 378 (173) | [n = 31]; +62 (71) | [n = 28]; +111 (103) | [n = 20]; +134 (149) |
| Urea (mmol/L); Mean (SD) | [n = 28]; 24.4 (11.1) | [n = 24]; +3.0 (4.1) | [n = 23]; +4.9 (6.6) | [n = 17]; +4.4 (6.6) |
| Potassium (mmol/L); Mean (SD) | [n = 31]; 5.3 (0.7) | [n = 29]; −0.1 (0.5) | [n = 28]; −0.4 (0.6) | [n = 21]; −0.4 (0.9) |
Abbreviations: SCr, serum creatinine.
IHD was performed in approximately one in eight patients who received RRT. Our principal concern prior to initiating IHD was that it might induce haemodynamic instability due to more rapid fluid shifts than are seen with CRRT; however, whilst transient mild hypotension was often documented, only one IHD session was terminated early due to hypotension.
The substantial changes to the provision of RRT described were only possible due to a highly effective cross specialty and multi-disciplinary approach. A critical care “tactical team” consisting of a consultant in intensive care medicine and critical care matron worked alongside two renal teams, dedicated to PD and IHD, to identify patients and initiate and maintain them on these therapies. The anaesthetic department created a dedicated transfer team to transfer patients to the IHD suite within ICU. Critical Care pharmacists rapidly evolved existing guidelines to advise on drug dosing in the context of different RRT modalities.
5. Conclusions
We have demonstrated how a large tertiary critical care centre was able to make changes to the way in which a complex therapy can be delivered under challenging conditions. Acute APD and IHD can be successfully provided to critically ill patients with COVID-19 in the context of a pressured and resource constrained setting. It is hoped that the techniques and findings described here will be of use to other institutions facing a surge of admissions of critically ill patients with severe AKI requiring RRT during this and future pandemics.
Credit authorship contribution statement
Richard Fisher: Conceptualization, Methodology, Investigation, Writing - original draft. Jonathan Clarke: Investigation. Khaled Al-Arfi: Investigation. Rohit Saha: Methodology, Investigation. Eirini Lioudaki: Conceptualization, Writing - review & editing. Reena Mehta: Writing - review & editing. Clemens Pahl: Writing - review & editing. Claire Sharpe: Conceptualization, Writing - review & editing. Kate Bramham: Conceptualization, Writing - review & editing. Sam Hutchings: Conceptualization, Writing - review & editing, Supervision.
Declaration of Competing Interest
All authors declare: no support from any organisation for the submitted work; no financial relationships with any organisations that might have an interest in the submitted work; no other relationships or activities that could appear to have influenced the submitted work.
Acknowledgements
Additional data collection by: Jennifer Abthorpe; Cathy Bell; Saif Haddad; Ana Spataru; Leonie White. Set-up and maintained service and involved in conception of the manuscript: Elaine Bowes; Hugh Cairns; Philip Hopkins; Catriona Shaw.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- 1.ICNARC . 2020. ICNARCreport on COVID-19 in critical care 05 June 2020. [Google Scholar]
- 2.Wang D., Hu B., Hu C., et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan, China. JAMA. 2020;323(11):1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Huang C., Wang Y., Li X., et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yang X., Yu Y., Xu J., et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational. Lancet Respir Med. 2020;8(5):475–481. doi: 10.1016/S2213-2600(20)30079-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gabarre P., Dumas G., Dupont T., Darmon M., Azoulay E., Zafrani L. Acute kidney injury in critically ill patients with COVID-19. Intensive Care Med. 2020:1–10. doi: 10.1007/s00134-020-06153-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Goldfarb D.S., Benstein J.A., Zhdanova O., et al. Impending Shortages of Kidney Replacement Therapy for COVID-19 Patients. Clin J Am Soc Nephrol. 2020;15(6):880–882. doi: 10.2215/CJN.05180420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Khwaja A. KDIGO clinical practice guideline for acute kidney injury. Nephron Clin Pract. 2012;2:1–138. doi: 10.1159/000339789. (Kidney Disease: Improving global outcomes (KDIGO) Acute Kidney Injury Work Group) [DOI] [PubMed] [Google Scholar]
- 8.Klingel R., Schaefer M., Schwarting A., et al. Comparative analysis of procoagulatory activity of haemodialysis, haemofiltration and haemodiafiltration with a polysulfone membrane (APS) and with different modes of enoxaparin anticoagulation. Nephrol Dial Transplant. 2004;19(1):164–170. doi: 10.1093/ndt/gfg459. [DOI] [PubMed] [Google Scholar]
- 9.Davies H.T., Leslie G., Pereira S.M. Webb SA. A randomized comparative crossover study to assess the affect on circuit life of varying pre-dilution volume associated with CVVH and CVVHDF. Int J Artif Organs. 2008;31(3):221–227. doi: 10.1177/039139880803100305. [DOI] [PubMed] [Google Scholar]
- 10.Bowes E., Joslin J., Braide-Azikiwe D.C.B., et al. Acute Peritoneal Dialysis with Percutaneous Catheter Insertion for COVID-19-associated Acute Kidney Injury in Intensive Care: Experience form a UK Tertiary Centre. KI Rep. 2020 doi: 10.1016/j.ekir.2020.11.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Guan W.J., Ni Z.Y., Hu Y., et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zhou F., Yu T., Du R., et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort. Lancet. 2020;395(10229):1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Richardson S., Hirsch J.S., Narasimhan M., et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the new York City area. JAMA. 2020;323(20):2052–2059. doi: 10.1001/jama.2020.6775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cummings M.J., Baldwin M.R., Abrams D., et al. Epidemiology, clinical course, and outcomes of critically ill adults with COVID-19 in new York City: a prospective cohort study. Lancet. 2020;395(10239):1763–1770. doi: 10.1016/S0140-6736(20)31189-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ganter G. ÜberdieBeseitigunggiftigerStoffeausdemBlutedurch Dialyse. Münch Med Wochenschr. 1923;70:1478. [Google Scholar]
- 16.Gottschalk C.W., Fellner S.K. History of the science of dialysis. Am J Nephrol. 1997;17:289–298. doi: 10.1159/000169116. [DOI] [PubMed] [Google Scholar]
- 17.Gatward J.J., Gibbon G.J., Wrathall G., Padkin A. Renal replacement therapy for acute renal failure: a survey of practice in adult intensive care units in the United Kingdom. Anaesthesia. 2008;63(9):959–966. doi: 10.1111/j.1365-2044.2008.05514.x. [DOI] [PubMed] [Google Scholar]