Abstract
Objectives
Following a surge in cases of coronavirus disease 2019 (COVID-19) in June 2020, India became the third-worst affected country worldwide. This study aims to analyse the underlying epidemiological situation in India and explain possible impacts of policy and technological changes.
Methods
Secondary data were utilized, including recently published literature from government sources, the COVID-19 India website and local media reports. These data were analysed, with a focus on the impact of policy and technological interventions.
Results
The spread of COVID-19 in India was initially characterized by fewer cases and lower case fatality rates compared with numbers in many developed countries, primarily due to a stringent lockdown and a demographic dividend. However, economic constraints forced a staggered lockdown exit strategy, resulting in a spike in COVID-19 cases. This factor, coupled with low spending on health as a percentage of gross domestic product (GDP), created mayhem because of inadequate numbers of hospital beds and ventilators and a lack of medical personnel, especially in the public health sector. Nevertheless, technological advances, supported by a strong research base, helped contain the damage resulting from the pandemic.
Conclusions
Following nationwide lockdown, the Indian economy was hit hard by unemployment and a steep decline in growth. The early implementation of lockdown initially decreased the doubling rate of cases and allowed time to upscale critical medical infrastructure. Measures such as asymptomatic testing, public–private partnerships, and technological advances will be essential until a vaccine can be developed and deployed in India.
Public interest summary
The spread of COVID-19 in India was initially characterized by lower case numbers and fewer deaths compared with numbers in many developed countries. This was mainly due to a stringent lockdown and demographic factors. However, economic constraints forced a staggered lockdown exit strategy, resulting in a spike in COVID-19 cases in June 2020. Subsequently, India became the third-worst affected country worldwide. Low spending on health as a percentage of gross domestic product (GDP) meant there was a shortage of hospital beds and ventilators and a lack of medical personnel, especially in the public health sector. Nevertheless, technological advances, supported by a strong research base, helped contain the health and economic damage resulting from the pandemic. In the future, measures such as asymptomatic testing, public–private partnerships, and technological advances will be essential until a vaccine against COVID-19 can be developed and rolled-out in India.
Keywords: India, Pandemic, Health, Policy
Introduction
The coronavirus disease 2019 (COVID-19) pandemic has posed an unprecedented challenge to the people and governments of every country in a very short period since its emergence in Wuhan, China, in December 2019 [1]. The first case of COVID-19 in India was reported on 30 January 2020 in the state of Kerala; this was a student who returned from Wuhan and tested positive for COVID-19, following which aggressive contact tracing followed by 14-day home quarantine for suspected cases were enforced [2]. The state remained on high alert. During March, cases began to be reported across India. Despite the aggressive measures taken by the Indian government to prevent and contain the epidemic, as of 12 August 2020 there were 652,473 active cases, 1,695,860 recovered cases, and 47,138 deaths due to COVID-19 [3].
India is the world's second-most populous and the third-worst affected country by COVID-19 to date (in terms of the total number of confirmed COVID-19 cases). Therefore, it is relevant to review how the country has fought the pandemic since its onset. Against this backdrop, the focus of this paper is to assess the impact of public policy and technological interventions on COVID-19 trends in India. First, India's diverse demographic profile followed by the status of health and hospital infrastructure prior to the COVID-19 pandemic are presented. Second, the impact of the pandemic on India and the measures taken by the government in response are discussed. Third, the technological advances that catalysed the overall recovery process are summarised. Finally, the economic impact of the pandemic is presented, followed by concluding observations with regards to the impact of these measures, their limitations and the way forwards.
Country description
Country and health system overview
India comprises 28 states and 8 union territories. Table 1 [4], [5], [6], [7], [8] shows that despite a huge population, the old-age dependency ratio and life expectancy in India are lower than the Organization for Economic Co-operation and Development (OECD) average of 0.264 and 80.7 years, respectively [9]. The current health expenditure in India as a percentage of gross domestic product (GDP) is one of the lowest in the world, which has left the country with insufficient doctors, nurses and beds to face an unprecedented situation such as a pandemic. Social distancing is a key part of tackling the spread of COVID-19, but a high population density can make social distancing challenging. Furthermore, more than half of the elderly population in India has co-morbidities, e.g. hypertension and diabetes, which could potentially increase these individuals’ risk of contracting COVID-19. However, India's median age reflects the fact that more than half of the country's population comprises the young, thereby lowering the anticipated fatality rates from COVID-19.
Table 1.
Overview of the demographics and the health system in India.
| Total population | 1.38 billion |
| Population density | 464 per km2 |
| Life expectancy | 68 years |
| Old-age dependency ratio | 9.256 |
| Median age | 28.4 years |
| Share of population > 65 years old | 6.2% |
| Diabetes (70–79 years) | 13.2% |
| Hypertension (65–74 years) | 51.5% |
| Hypertension (≥ 75 years) | 52.0% |
| Health care expenditure as a percentage of GDP | 1.02% |
| Healthcare expenditure per capita | USD 69.29 |
| Practicing doctors | 1/1457 people |
| Practicing nurses | 1/475 people |
| Beds per 100 population | 0.55 |
A health-system overview is critical for tracking the diverse demographic and health indicators across the country (see Table 2 ) [10], [11], [12]. Population density exhibits extreme variations, from 123 individuals per km2 in Himachal Pradesh to 1106 individuals per km2 in Bihar. The percentage of the population aged 60 years or more varies from 6.7% in Jharkhand to 12.9% in Kerala. Furthermore, the average life expectancy varies from 63.6 to 72.2 years and is higher for females than males. These variations result from the jurisdiction for health being decentralized, with states having the power to allocate health budgets. Health expenditure as a percentage of GDP is as high as 2.21% in Assam and as low as 0.60% in Maharashtra, even though the population of Maharashtra is 3.5 times that of Assam.
Table 2.
An overview of the health system in India by state.
| State | Health expenditure as a percentage of GSDP*(2015–16) | Population in millions (2013) | Population density (individuals/km2) (2011) | Percentage of the population aged ≥ 60 years (2012) | Average life expectancy (years)(2012–2016) |
|---|---|---|---|---|---|
| Andhra Pradesh | 0.76 | 87.0 | 308 | 9.60 | 69.7 |
| Assam | 2.21 | 32.2 | 398 | 6.60 | 65.6 |
| Bihar | 1.33 | 108.7 | 1,106 | 7.10 | 68.7 |
| Gujarat | 0.72 | 61.6 | 308 | 8.50 | 69.6 |
| Himachal Pradesh | 1.68 | 7.1 | 123 | 10.60 | 72.45 |
| Jharkhand | 1.25 | 34.1 | 414 | 6.70 | 67.9 |
| Kerala | 0.93 | 34.4 | 860 | 12.90 | 75.05 |
| Madhya Pradesh | 1.04 | 74.4 | 236 | 7.20 | 65.45 |
| Maharashtra | 0.60 | 117.0 | 365 | 9.50 | 72.25 |
| Punjab | 0.87 | 28.4 | 551 | 9.90 | 72.6 |
| Rajasthan | 1.44 | 71.7 | 200 | 7.50 | 68.4 |
| Tamil Nadu | 0.74 | 74.0 | 555 | 10.70 | 71.45 |
| Uttarakhand | 1.06 | 10.4 | 189 | - | 71.65 |
| Uttar Pradesh | 1.42 | 208.7 | 829 | 7.10 | 64.75 |
| West Bengal | - | 93.5 | 1,028 | 8.40 | 70.85 |
GSDP – gross state domestic product.
Differences in health spending result in major variations in health infrastructure in terms of hospitals, beds, ventilators, etc. across the states. For example, Jharkhand and Kerala have comparable populations but the number of hospitals, beds and ventilators in the public sector varies by almost 3.5 times (see Table 3 ) [6,13,14]. A visible mismatch between medical infrastructure supply and demand in the public sector will pose a big challenge to deal with the increasing number of cases across the country under the prevailing situation.
Table 3.
An overview of private versus public health infrastructure in India by state.
| Number of | Number of | Number of intensive | Number of | |||||
|---|---|---|---|---|---|---|---|---|
| State | hospitals |
hospital beds |
care unit (ICU) beds |
ventilators |
||||
| Public | Private | Public | Private | Public | Private | Public | Private | |
| Andhra Pradesh | 258 | 670 | 23,138 | 60,092 | 1,157 | 3,005 | 578 | 1,502 |
| Assam | 1,226 | 503 | 17,142 | 7,036 | 857 | 352 | 429 | 176 |
| Bihar | 1,147 | 1,887 | 11,664 | 19,193 | 583 | 960 | 292 | 480 |
| Gujarat | 438 | 970 | 20,172 | 44,690 | 1,009 | 2,234 | 504 | 1,117 |
| Jharkhand | 555 | 809 | 10,784 | 15,712 | 539 | 786 | 270 | 393 |
| Kerala | 1,280 | 2,062 | 38,004 | 61,223 | 1,900 | 3,061 | 950 | 1,531 |
| Madhya Pradesh | 465 | 506 | 31,106 | 33,833 | 1,555 | 1,692 | 778 | 846 |
| Maharashtra | 711 | 2,492 | 51,446 | 180,293 | 2,572 | 9,015 | 1,286 | 4,507 |
| Punjab | 682 | 1,638 | 17,933 | 43,064 | 897 | 2,153 | 448 | 1,077 |
| Rajasthan | 2,850 | 2,794 | 47,054 | 46,122 | 2,353 | 2,306 | 1,176 | 1,153 |
| Tamil Nadu | 1,217 | 1,222 | 77,532 | 77,843 | 3,877 | 3,892 | 1,938 | 1,946 |
| Uttar Pradesh | 4,635 | 12,468 | 76,260 | 205,142 | 3,813 | 10,257 | 1,907 | 5,129 |
| Uttarakhand | 460 | 829 | 8,512 | 15,331 | 426 | 767 | 213 | 383 |
| West Bengal | 1,566 | 697 | 78,566 | 34,969 | 3,928 | 1,748 | 1,964 | 874 |
Healthcare financing in India is a mix of public and private schemes; however, at least 75% of the population has no kind of insurance cover [15]. Furthermore, the private sector provides 58% of hospitals and 81% of doctors in India [16]. During the early days of the pandemic, public hospitals were involved in the testing and treatment of COVID-19. Insufficient public health infrastructure together with a surge in cases called for a policy revision in terms of participation of the private sector in testing and treatment for COVID-19. The public sector accounts for around 20% of the total healthcare expenditure in India, representing around 1% of GDP, one of the lowest proportions of any country in the world [17]. The remaining 80% contributed by the private sector is targeted towards financing and the creation of infrastructure facilities. While diagnosis and treatment were free for 500 million beneficiaries of the health insurance scheme ‘Ayushman Bharat’ in public hospitals, the costs of tests (USD 44) and treatment were capped at private facilities. For example, the Delhi government capped isolation facilities at USD 160–200 per day for isolation beds, USD 260–350 per day for an ICU bed without a ventilator, and USD 300–360 per day for an ICU bed with a ventilator [18].
Changes due to COVID-19
Other changes in India included contingency plans for an anticipated surge in cases. Railway coaches (2,500) were converted to isolation wards, making available an additional capacity of 40,000 beds [19]. Paramedical staff, including volunteers, ex-service people, homeopathic and ayurvedic practitioners, medical students, teachers, doctors (including retired doctors), and others, were identified at municipal, district and state levels to create an online data pool of 15,896,093 human resources for various activities required to fight COVID-19; each person was designated a ‘COVID warrior’, and a surveillance policy of one COVID warrior per 250 citizens was devised [20]. With the increased supply of infrastructure and human resources, it was equally important to match the demand for medical equipment and medicines. With the involvement of private hospitals, the demand for personal protective equipment (PPE) increased.
Zonal classification
Geographical areas within a city were classified as red (more than 15 confirmed cases on a given day), orange (up to 15 confirmed cases), or green (no cases) zones, based on levels of infections [21]. Containment zones were geographical areas where a cluster of confirmed cases (more than six) was found, especially in cramped locations where social distancing was not realistically possible. Specific guidelines in these areas include:
-
•
Entry only after a taking COVID-19 preventive drug.
-
•
Designated helpline numbers for the delivery of essential items, sanitisation drives, and health check-ups.
-
•
Restricted movement to other zones, with violators booked under sections of the Disaster Management Act (2005), the Epidemic Diseases Act (1897), and the Indian Penal Code (IPC).
-
•
Zones were reassessed within four weeks from the discharge of the last confirmed case.
This concept of zonal classification was based on the steep learning curve experienced during the 1918 influenza A virus (H1N1) pandemic in India. One of the lessons learned during this earlier pandemic was that even though the spread of a virus among the Indian population could be high, it is unlikely to affect all parts of the country uniformly [22].
COVID-19 trends
Overview of data availability and data transparency
State governments usually report COVID-19 data based on daily numbers of confirmed, deceased, recovered and active cases. The major channels for disseminating official data included the Ministry of Health and Family Welfare (MoHFW), the Aarogya Setu Mobile application, press conferences, and the COVID-19 India website [23], which was developed by a group of volunteers. Table 4 [23] provides an overview of the growth rate of the epidemic during different phases of the mitigation strategies.
Table 4.
COVID-19 spread during subsequent lockdowns in 2020.
| Lockdown duration | Mitigation strategy | Growth rate (%)(The number of new cases divided by the total number of confirmed cases on the previous date) |
|---|---|---|
| 24 March–14 April | Phase 1 (lockdown) | 15.06 (on 25 March) |
| 15 April–3 May | Phase 2 (lockdown) | 7.5 (on 25 April) |
| 4 May–17 May | Phase 3 (lockdown) | 6.4 (on 5 May) |
| 18 May–31 May | Phase 4 (towards exit strategy) | 4.63 (on 25 May) |
| 1 June–30 June | Phase 5 (unlock 1.0) | 3.85 (on 25 June) |
| 1 July–31 July | Phase 6 (unlock 2.0) | 3.63 (on 25 July) |
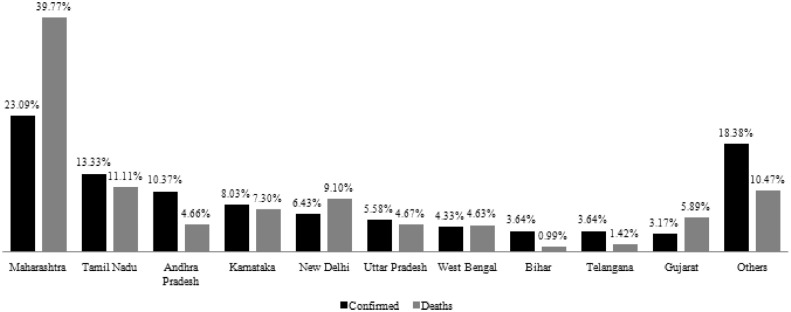
Fig. 1 [23] shows the top-ten states with the highest tally of confirmed cases (up to 12 August 2020). Maharashtra emerged as the epicentre of the virus, with clusters of infections in Asia's biggest slum, ‘Dharavi’. Although Telangana and Gujarat reported a similar percentage of confirmed cases, Gujarat reported a higher percentage of deaths. New Delhi had a lower percentage of confirmed cases than Karnataka but reported a higher percentage of deaths. These differences reflect differences in technological expertise and medical facilities across states.
Fig. 1.
State-wise share of COVID-19 confirmed cases and deaths (2020).
Trends in COVID-19 cases, deaths and recoveries
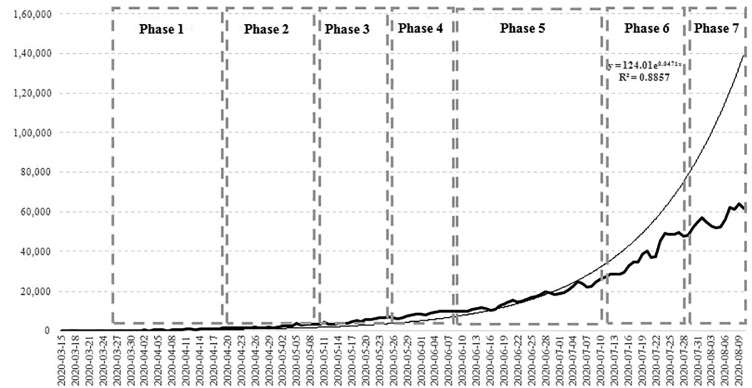
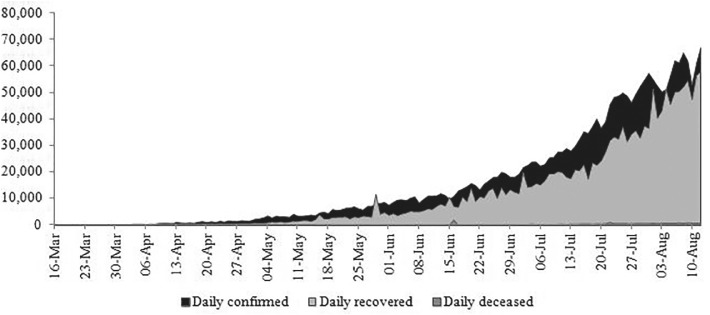
Fig. 2 [3] depicts the impact of various unlock phases on the increase in the number of new cases. It should be noted that until the end of phase 4, the trend was linear. However, during unlock phase 5, the trend resembled an exponentially increasing curve tapering off during unlock phase 6 (R2 = 88.57%). It was observed that during this time, the recovery rate was constantly increasing (see Fig. 3 ) [3], with less than 1% of confirmed cases on ventilators, less than 2% in ICUs and less than 3% in oxygen beds [24]. The growth in recovery rates started matching the growth in confirmed cases, possibly due to a better understanding of the nature and treatment of a novel disease from a technological perspective.
Fig. 2.
New cases of COVID-19 in India during 2020.
Fig. 3.
Trends in confirmed, recovered and deceased cases of COVID-19 (cumulative) during 2020.
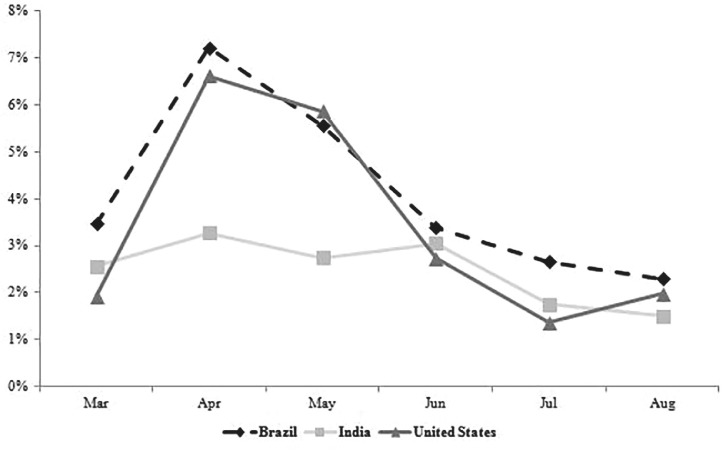
The case fatality rate (CFR), when comparing the top-three worst-affected countries (in terms of the total number of confirmed COVID-19 cases) shows that India's CFR (see Fig. 4 ) [3] was much lower [25]. This could possibly be attributable to demographic factors, such as a relatively young population, the effectiveness of an early lockdown [26], a possible inverse correlation between Bacille Calmette–Guérin (BCG) immunization and COVID-19 incidence and severity [27], missing data from untested deceased patients, or the temperature and humidity [28]. A slight increase in CFR during March 2020 was possibly due to states initiating the process to have their statistics audited by Death Audit Committees (DAC). A written explanation for any delay in reporting COVID-19 fatalities was mandated, to prevent any underreporting of actual numbers.
Fig. 4.
COVID-19 case fatality rate in the three worst-affected countries during 2020.
State-wise evolution of COVID-19
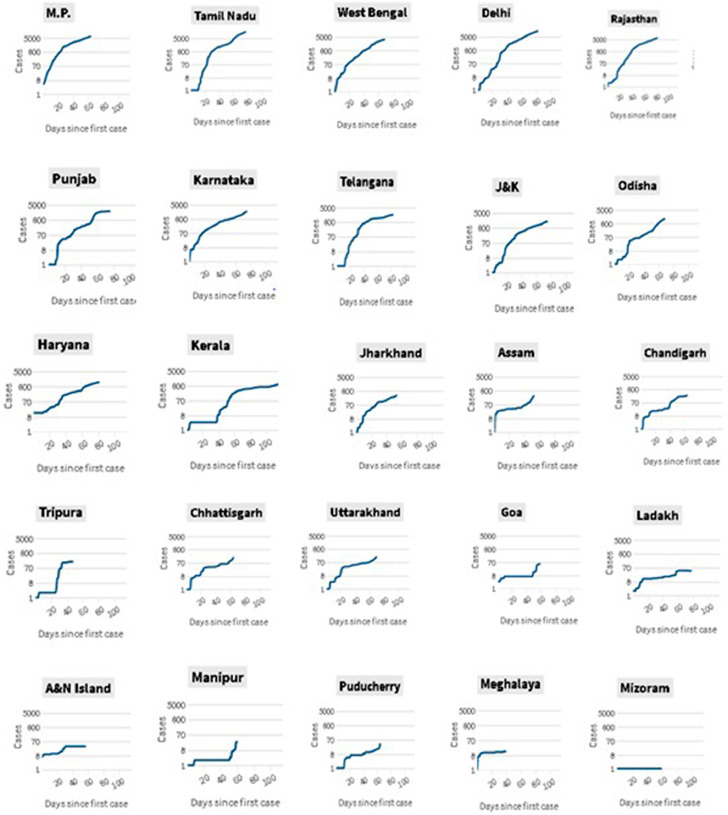
The state-wise evolution of the spread of COVID-19 during the first 100 days of the epidemic is shown in Fig. 5 [23], showing that the evolution of the disease differed across states. Kerala received accolades from the United Nations while leading India's early response to this pandemic [29]. The curve for Kerala was almost linear until day 40 after an initial spike in cases.
Fig. 5.
Evolution and spread of COVID-19 across states during the first 100 days.
Kerala ranks first in the overall health index [30], where public initiatives in health went hand in hand with private partnerships to fight COVID-19 [31]. A highly responsive and robust healthcare model started systematically preparing to handle a possible outbreak in January 2020. Kerala launched the ‘Break the Chain’ campaign as a means to highlight the importance of hygiene (handwashing) and social distancing. Standard operating procedures covered aggressive contact tracing; infection control for ambulances; careful management of biomedical waste and handling the spillage of body fluids; disinfection and sterilisation; management of dead bodies; use of PPE; and sample collection and transportation. Transparency in communication was maintained, in the form of reporting daily confirmed cases, revised guidelines related to quarantine, hospital admissions, and discharged cases. Additionally, the state undertook total financial responsibility for testing and treatment. However, during July, Kerala witnessed a sudden surge in COVID-19 cases, largely due to the easing of lockdown restrictions and an influx of migrants from other states and from abroad [32]. As a result, there was a sharp increase in the percentage of locally transmitted cases (contacts of the imported cases) [33]. During this time, the scale of testing was unable to match the scale of migrants, thereby delaying the contact tracing and treatment protocol. Additionally, the use of rapid antigen tests (with low accuracy) [59] possibly reduced the reliability of results [34].
Age and sex trends
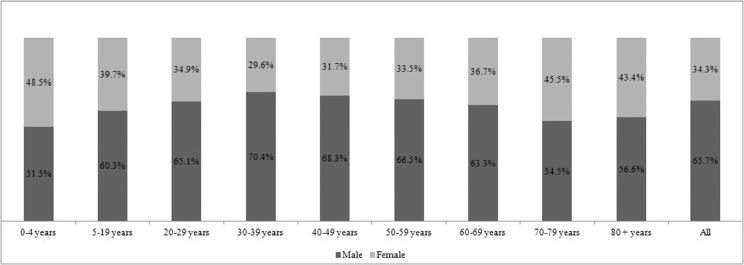
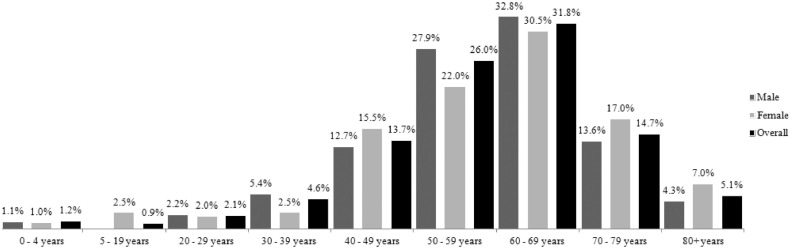
COVID-19 is more likely to infect the male population in India, with the highest percentage of cases in males aged 30 to 39 years (see Fig. 6 ) [35]. In the absence of specific COVID-19 statistics based on comorbidities, patients with diabetes, chronic kidney disease, hypertension, and heart disease have been considered at risk [36]. The male population aged more than 60 years accounts for the majority of deaths (see Fig. 7 ) [35].
Fig. 6.
The percentage of confirmed COVID-19 cases by age group.
Fig. 7.
The percentage of deaths from COVID-19 by age and sex.
Policy and technology road map
Policy mandates
For any country to make a rapid recovery from the effects of the pandemic, it is imperative to investigate the role of policy and technological changes. Tables 5a [37], 5(b) [37] and 5(c) [38] list government policies across India and by sector.
Table 5a.
Government policies in response to the COVID-19 pandemic.
| Timeline | Interventions (pre-peak) | Type* |
|---|---|---|
| Phase 1 and 2 | Curb of non-essential activities 1.3 billion people impacted Zonal classification of cities initiated | Medium Imprisonment (6 months– 2 years) or a fine imposed or both |
| Phase 3 (Towards an exit strategy) | Relaxation in all zones except containment zones Opening of stand-alone liquor shops Intrastate movement with a pass Government offices opened with 33% capacity Interstate movement permitted | Minimal |
| Phase 4 | Lockdown regulations indicating an exit strategy Domestic travel resumed The authority for opening commercial activities was decentralized to state level | Medium |
| Phase 5 Unlock 1.0 | Lockdown only in containment zones Metros and other social gathering venues closed | |
| Phase 6 Unlock 2.0 | Additional guidelines to Unlock 1.0 included a night-time curfew from 9 p.m. to 5 a.m. | |
| Phase 7 Unlock 3.0 | Additional guidelines to Unlock 2.0 included revocation of the night-time curfew Gymnasiums and yoga institutes open | |
Type: Medium – mandated by law (no punishment); Minimal – advisory; Significant – mandated by law (punishable) [39].
Table 5b.
Interventions introduced across industries in response to the COVID-19 pandemic.
| Sector | Timeline (2020) | Intervention (pre-peak) | Type* |
|---|---|---|---|
| Agriculture | January | Villages organised awareness meetings | Minimal |
| March, April | Agricultural activities curbed | ||
| May | Agricultural activities restarted | ||
| Education | March | Schools closed (New Delhi) | Significant
|
| April | All colleges (except medical) closed | ||
| April | Hostels vacated | Minimal | |
| May–August | Online learning | Medium | |
| Industry | March | Non-essential activities closed | Medium |
| May | Industries open with limited capacity | ||
| July–August | Seamless operation of industrial units in multiple shifts | Minimal | |
| Aviation | January | Screening of travellers from China Avoid non-essential travel to China | Minimal |
| February | E-visa for Chinese passport holders suspended International passengers quarantined Existing visas invalidated or suspended until April, except for a few categories | Medium Minimal Medium | |
| March, April | Flights banned | Medium | |
| May–August | Domestic and non-scheduled international flights for stranded citizens | Significant | |
| Entertainment | March–August | Cinemas, theatres and auditoriums closed | Significant, Disease Epidemic Act (1897), Section 188(IPC) Fine imposed 6 months imprisonment |
| June–August | Malls opened | Medium | |
| Religious | March | Mass gatherings limited in number | Medium |
| April | Amendment to Disease Epidemic Act, 1897 Acts of violence against health workers registered | Significant Maximum 5 years imprisonment, fine imposed. Grievous injury, could lead to 7 years’ imprisonment Fine imposed | |
| June–August | Religious places opened, with a ban on large religious gatherings | Medium | |
| May–August | Interstate trains and buses operational, metros remain closed | ||
Type: Medium – mandated by law (no punishment); Minimal – advisory; Significant – mandated by law (punishable) [39].
Table 5c.
Amendments in medical export policy.
| Sector | Timeline (2020) | Export interventions | Type* |
|---|---|---|---|
| Active pharmaceutical ingredients (APIs) | April | Prohibited for paracetamol APIs As an exception, HCQ was exported to 55 countries with COVID-19 [41] | Significant |
| May | Permitted for paracetamol APIs | ||
| Diagnostic kits | April | Restricted for certain diagnostic or laboratory reagents | |
| June | Restricted for viral transport medium (VTM) kits and reagents and reverse transcription polymerase chain reaction (RT-PCR) extraction kits and reagents | ||
| Ventilators | March | Prohibited for ventilators and any other breathing device | |
| August | Permitted | ||
| PPE | June | Prohibited for medical coveralls, goggles, gloves and face shields Upper cap on PPE medical coveralls | |
| July | Permitted for surgical drapes, isolation aprons, surgical wraps and X-ray gowns, face shields Restricted for medical goggles (upper cap on export volume) | ||
| Masks | May | Permitted for non-medical or non-surgical masks | |
| July | Restricted for surgical masks (upper cap on export volume) | ||
| Sanitisers | May | Prohibited for alcohol-based sanitisers | |
| June | Prohibited for alcohol-based hand sanitisers with dispenser pump | ||
| Textile raw material | July | Prohibited for fabrics used to make medical masks | |
Type: Medium – mandated by law (no punishment); Minimal – advisory; Significant – mandated by law (punishable) [39]
Table 5b shows that during March and April, schools planned to roll-out online learning, both in terms of formulating online content and upgrading their information technology (IT) infrastructure. The objective of opening liquor shops during phase 3 was to replenish state revenues through excise duty on liquor, which comprises between 10% and 15% of their tax revenue. The resumption of selected economic activities indicated a staggered lockdown exit strategy. From Phase 4 onwards, the responsibility for unlock policies was transferred to the state level, as the spread of disease varied across states.
India's pharmaceutical industry, which is third largest in the world by volume, sources the majority of its active pharmaceutical ingredients from China [40]. This supply was affected owing to the virus outbreak in China. Hence, during the initial phases of lockdown, Indian exports were prohibited or restricted to maintain an undisrupted supply chain for the nation, as shown in Table 5c . However, following a tremendous increase in indigenous manufacturing capacity, medical exports began opening up again during July.
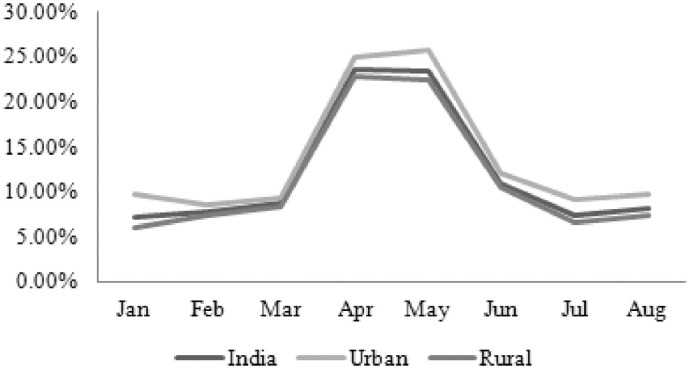
Economic relief measures taken by the Indian government
Within a month of lockdown, the unemployment rate in India increased dramatically, from 8.7% in March to 23.52% in April 2020 (see Fig. 8 ) [42]. This resulted in job losses for an estimated 140 million people and an income drop for more than 45% of households [43]. As evident from Fig. 8, the unemployment rate started to decline again after May because of the reopening of industries and other commercial activities and almost reached pre-COVID-19 levels. Relief measures were announced through different modes, via the central bank or existing schemes; however, they had limited social coverage considering the duration of lockdown (see Table 6) [44]. The Reserve Bank of India (RBI; central bank) eased the burden of loan payments by allowing companies to make late repayments. Schemes were launched to provide cash and essential items to vulnerable families. A stimulus package was announced, in four tranches, for small businesses and farmers.
Fig. 8.
The unemployment rate in India during the COVID-19 pandemic.
Table 6.
Economic relief measures introduced by the Indian government (pre-COVID-19 peak).
| Measure | Mode | Action | Type* |
|---|---|---|---|
| Fiscal, monetary rates | Reserve Bank of India (RBI) | Slashed repo rate⁎⁎ Extended the loan repayment period | Medium |
| Schemes | Pradhan Mantri Garib Kalyan Yojana | Payment (ex gratia) to poor senior citizens, widows and the disabled Insurance coverage for healthcare workers involved with COVID-19 treatment and care Medical insurance to cover all health workers | Minimal Medium |
| Pradhan Mantri Kisan Yojana | States to provide cash transfers in installments to farmers | Significant | |
| Jan Dhan accounts | Monthly cash transfers to 200 million women | Minimal | |
| Employee Provident Fund (EPF) | Government contribution to EPF (for both employer and employees for companies with less than 100 workers) | ||
| Food security | Scheme | Covered 800 million people | |
| Free liquefied petroleum gas (LPG) for ‘Ujjwala Scheme’ beneficiaries for a specified period of time | |||
| Construction funds | Scheme | States to use construction worker funds | Medium |
| Education | Fee | Private schools could not hike fees, could only charge a tuition fee | None |
| Atmanirbhar package | Stimulus package announced 13 May | Credit line to small businesses and support to shadow banks Food-grains to stranded workers for two months and credit to farmers Support for agriculture and allied sectors and , structural reforms | Significant |
Type: Medium – mandated by law (no punishment); Minimal – advisory; Significant – mandated by law (punishable) [39].
repo rate – the rate at which RBI lends money to commercial banks in the event of any shortfall of funds.
Technological advances
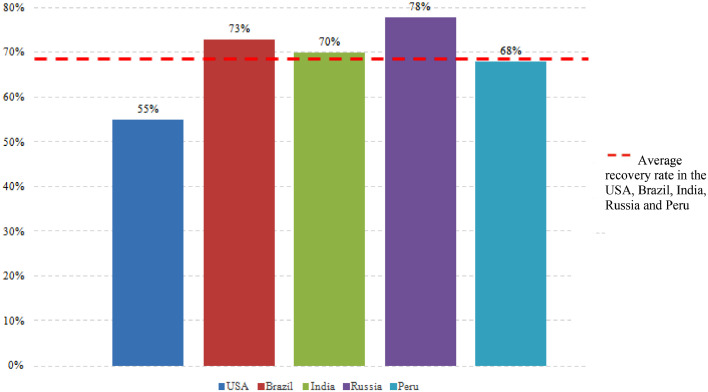
India is among the largest manufacturers of vaccines in the world and was the fifth country to isolate the strain of SARS-CoV-2, the virus that causes COVID-19 [45]. India could play an important role in terms of mass-producing a vaccine at an affordable cost [46]. Out of seven Indian firms racing to develop a vaccine, two had vaccine candidates already in the human trial phase as of August 2020 [46]. Around 12 August, India's proportion of recovered COVID-19 cases of 70%, shown in Fig. 9 [3], was higher than the average (69%) of the top-five countries (by total number of COVID-19 confirmed cases), representing more than 1.6 million [3] recovered cases in absolute terms. This was testimony to the technological advances applied at scale against the backdrop of lockdown measures. Furthermore, research advances, in the form of scaling-up of convalescent plasma therapy, where blood from individuals who have recovered from COVID-19 is given to other infected individuals to help them recover [47], gave an impetus to the treatment process.
Fig. 9.
Bench-marking the recovery rate from COVID-19 in India versus the top-five COVID-19 affected countries (2020).
Technological advances can be categorised into three broad categories based on testing, tracing and treatment. As shown in Table 7, many of the technological initiatives were ‘significant’ in type. The introduction of the world's cheapest COVID-19 testing kit in India was expected to change the paradigm of testing in the country both in terms of scale and cost. Lower cost kits facilitate more tests per million population. Existing drugs and alternative therapies [48,49], produced encouraging results. Furthermore, India increased its manufacturing capacity to 0.45 million PPE coveralls (second-largest manufacturer in the world) and 0.20 million N-95 masks every day, which means better availability of medical coveralls in the future [50]. The launch of the Aarogya Setu app at an all India level for contact tracing was followed by the launch of specialized apps at the state level to fill in the information gap in terms of occupancy and availability of hospital beds, ICUs and ventilators for patients with COVID-19 [51], [52], [53].
Table 7.
Technological initiatives initiated in response to COVID-19 (pre-COVID-19 peak).
| Category | Advance | Description | Type* |
|---|---|---|---|
| Testing | Indigenous testing kits | Testing kits at one-fourth the cost of imported kits with results in 2–3 hours Rapid antibody kits were designed The world's most affordable testing kit (to date) at a base price of USD 8 was developed [54] | Significant |
| Immunodiagnostic kits | Efforts were initiated since they can also detect asymptomatic cases | Significant | |
| Tracing | Manual process | Contact tracing through in-depth interviews | Minimal |
| Drones used for surveillance and public announcements | Monitoring whether areas in a city were following social distancing via an aerial view | Medium | |
| Aarogya Setu App | Real-time data update powered by Bluetooth technology and artificial intelligence Risk-assessment, contract tracing for individuals | Significant | |
| Treating | Vaccine | Launched phase II human trials | Significant |
| Thermal screening | Temperature checks during international and interstate travel | Minimal | |
| Selected drugs | Existing preventive drugs approved for emergency use | Medium | |
| Convalescent plasma therapy | Blood transfusion from recovered patients | Medium | |
| Tele-health | Online applications designed | Medium | |
| Laboratory-manufactured alcohol sanitisers | Manufactured as per WHO guidelines | Significant | |
| PPE, ventilators | Designed at a reduced cost. PPE could be taken off without touching the outer surface | Significant | |
| Disinfectant tunnel | To disinfect people when they walk through it | Significant | |
Significant: an innovation; Medium: successful use of an existing technology or therapy; Minimal: manual intervention for results [39].
While technology on one hand eased the hospitalisation process of patients with COVID-19, initiatives like the launch of telemedicine units for home-quarantined cases (asymptomatic) provided a digital platform for a COVID-19 treatment [55], thereby reducing the burden on the health infrastructure. Further, the success of policy and technological interventions applied together was evident in the form of a substantial reduction in the number of new COVID-19 infections reported from Asia's largest slum (Dharavi) in the state of Maharashtra, the financial capital of India [56]. Here, on the technological front, both swab and blood tests of suspected cases were conducted, while on the policy front an ‘Integrated Disease Surveillance Programme’ was activated, which involved healthcare workers going door to door to test suspected cases and their family members.
Evolution of testing criteria
Initially, the testing protocol was limited to symptomatic international passengers entering India, contact history with a positive case, and symptomatic healthcare workers. However, from April onwards people in infection hotspots with symptoms of cold, cough and fever; individuals who participated in large gatherings; and patients with severe acute respiratory illness could be tested. It was reported that nearly 80% of confirmed cases were asymptomatic or had mild symptoms [57]. A revised discharge policy (10 days) was recommended compared with the initial 14 days standard from symptom onset and no fever for three days, to reduce the pressure on medical infrastructure [58].
Evolution of testing methods
During the early phases of the COVID-19 outbreak, public hospitals used the RT-PCR method, which gave results of high accuracy but with a turnaround time of 24 hours. The scale of testing increased as private laboratories began performing tests and using the antibody blood test, which gave results in less than 30 minutes, but with an accuracy as low as 50%. The Indian Council of Medical Research (ICMR) issued guidelines for unconfirmed cases with negative results from antigen tests to have RT-PCR done; in Delhi alone less than 1% of those with negative antigen results received an RT-PCR test [32]. As of 4 August 2020, 30% of all tests being conducted were antigen tests [59]. The COVID-19 positivity rate may not have given a clear picture of the scale of the outbreak due to large numbers of false negatives. This hindered contact tracing and may have acted as a catalyst for new cases. Furthermore, India's testing rate continues to be one of the lowest in the world [60]. Despite a manufacturing capacity of 4.87 million test kits per day, the country could only conduct 0.7 million tests per day as of 12 August 2020. This could be attributed to the fact that the state governments paid private laboratories in the range of almost half of the price cap set by ICMR [61]. More tests per million people did not necessarily result in more positive cases being detected (see Table 8) [62]. For example, in Rajasthan and Bihar, more positive cases per 100 tests were found in Bihar than Rajasthan, even though more tests per million people were conducted in Rajasthan.
Table 8.
Variation in the scale of testing across states around 12 August 2020.
| State | Tests per millionpeople | Positive tests per million people | Positive per 100 testspeople |
|---|---|---|---|
| Bihar | 8,425 | 657 | 7.8 |
| Delhi | 59,308 | 7,235 | 12.2 |
| Gujarat | 14,355 | 1,033 | 7.2 |
| Madhya Pradesh | 10,705 | 469 | 3.9 |
| Maharashtra | 22,161 | 4,270 | 19.3 |
| Kerala | 27,803 | 970 | 3.5 |
| Punjab | 16,328 | 377 | 4.4 |
| Rajasthan | 22,260 | 671 | 3.0 |
| Tamil Nadu | 17,814 | 1,605 | 9.0 |
| Uttar Pradesh | 13,684 | 538 | 3.9 |
| West Bengal | 11,343 | 980 | 8.6 |
Healthcare system response data
Demand-side versus supply-side scenario
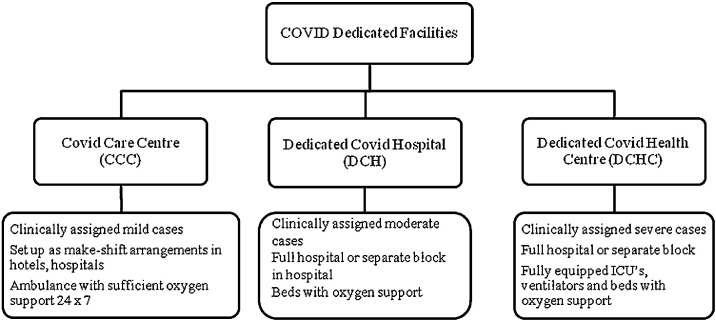
With increased testing capacity, infrastructure and human resources, India equipped itself to handle the expected surge in cases during the later phases of lockdown. In addition to public–private partnerships (PPPs) in the health sector, the government augmented health infrastructure through the creation of dedicated COVID-19 facilities. As shown in Fig. 10 [63], admission to a dedicated COVID-19 facility was based on the clinically assessed medical condition of a patient, as the three types of facilities were equipped with different medical infrastructure. Table 9 [64] provides information regarding the medical infrastructure in these facilities. However, estimating the percentage increase in medical infrastructure pre- and post COVID-19 remains a challenge, due to the absence of data regarding new infrastructure that has been built and existing private facilities that were reserved as COVID-19 wards.
Fig. 10.
Infrastructure dedicated to COVID-19.
Table 9.
Medical infrastructure in dedicated COVID-19 facilities.
| Category | DCH | DCHC | CCC |
|---|---|---|---|
| Dedicated facilities | 1,378 | 3,077 | 10,351 |
| Total ICU beds | 46,487 | ||
| Total oxygen support beds | 165,361 | ||
| Total ventilators | 21,738 | ||
Medicines and medical services
All elective surgeries were curtailed during phases 1 and 2 of the lockdown, with only life-saving surgeries taking place from 21 March 2020 [65]. Patients dealing with other ailments were encouraged to use telemedicine services, as outpatient departments were closed [66]. However, lockdown 4 included the opening of outpatient services for all ailments.
Economic and financial fluctuations
Fiscal value of human lives lost to COVID-19
Subsequent lockdown phases since the start of the pandemic have had an adverse impact on the Indian economy. Table 10 [67] shows an approximation of the total fiscal value (TFV) of human lives lost in India due to COVID-19 as USD 815 million (4% rate) and USD 703 million (6% rate) at the prevailing interest rates in India (to 12 August 2020). As shown in Eq. (1), the discounted fiscal value (DFV) for a particular age group has been calculated as the product of non-health GDP per capita (NGDPC), discounted years of life lost (DISYLL), and the number of deaths in the age group due to COVID-19 [67]. NGDPC has been calculated as the difference between GDP per capita and current health expenditure (CHE). Years of life lost (YLL) for each age group have been estimated as the difference between the life expectancy at birth (LE) and the average age at death from COVID-19 [56]. The discount factor 1/(1+r) k in Eq. (1) has been used to calculate DISYLL, where r is an interest rate that measures the opportunity cost of lost earnings. The summation (Eq. (1)) used k = 1 as the first year of life lost and k = n as the final year of the total number of YLL per case of COVID-19 within an age group. The number of deaths due to COVID-19 in a particular age group (N) has been approximated as a percentage of the total number of deaths (TD) due to COVID-19 (see Fig. 7). The fiscal value of life lost across the age groups in Table 10 was summed up, and finally the average monetary value per human life lost was calculated as total fiscal value divided by TD. Also, the average monetary value per human life lost from COVID-19 in India was found to be sensitive to the discount rate [67].
| (1) |
Table 10.
Fiscal valuation of life lost due to COVID-19 with 2020 as the base year.
| (A-B) | NGDPC(USD) | Deaths (N)(Years) | YLL(Years) | DISYLL(4%) | DFV(4%) | DISYLL(6%) | DFV(6%) |
|---|---|---|---|---|---|---|---|
| 0–4 | 2,034.81 | 565 | 67.41 | 24.15 | 27,799,376.07 | 17.32 | 19,934,549.17 |
| 5–19 | 2,034.81 | 424 | 57.41 | 23.26 | 20,083,290.86 | 17.04 | 14,713,486.88 |
| 20–29 | 2,034.81 | 989 | 44.91 | 21.53 | 43,374,123.95 | 16.38 | 32,987,048.09 |
| 30–39 | 2,034.81 | 2168 | 34.91 | 19.39 | 85,544,760.63 | 15.36 | 67,755,154.40 |
| 40–49 | 2,034.81 | 6,457 | 24.91 | 16.21 | 213,046,660.37 | 13.53 | 177,779,597.4 |
| 50–59 | 2,034.81 | 12,255 | 14.91 | 11.51 | 287,099,015.61 | 10.26 | 255,779,462.1 |
| 60-69 | 2,034.81 | 14,989 | 4.91 | 4.55 | 138,917,286.95 | 4.40 | 134,078,523.48 |
| *70–79 | 2,034.81 | 6,929 | - | – | – | – | – |
| *80+ | 2,034.81 | 2,404 | - | – | – | – | – |
| TFV (USD) 815,864,514.44 | 703,027,821.52 | ||||||
| Average monetary value per human life lost (USD) 17,308.00 | 14,914.25 | ||||||
International trade and sectoral impact
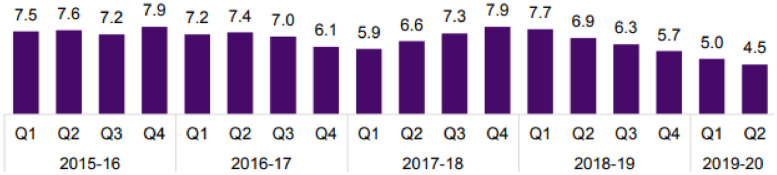
The World Bank downgraded India's growth for the fiscal year 2021 [68]. However, the International Monetary Fund's GDP growth projection (2021–22) for the country (1.9%) was the highest among the G20 nations [69], although the pandemic in India began when its GDP had already been on a downward trajectory since Q2 2018–19 and experienced a new low (4.5%) in Q2 2019–20 (see Fig. 11 ) [70,71]. The impact of any economic downturn will depend on the duration and severity of the pandemic. In an optimistic scenario, the recovery could be V-shaped, both in GDP growth and inflation, compared with a U-shaped recovery in an extended recovery scenario.
Fig. 11.
Real GDP growth percentage (constant 2011–12 prices).
Credit rating agencies have downgraded India's growth for the fiscal year 2021 [72,73]. Exports and imports form a crucial component of GDP. The effect of the COVID-19 pandemic reduced India's exports by 34.6% and 60.28% in March and April, respectively. The trade deficit narrowed to USD 9.76 billion in March 2020 [74], which was further aggravated by a sharp depreciation of the rupee against the dollar (INR 75 per USD on 20 March) [70]. Many sectors were expected to experience overall negative growth [73], especially import-driven sectors such as the automotive industry [75]. The Indian aviation industry (the world's third-largest domestic aviation market) [76] was near to collapse following the travel bans; however, it gradually started to revive with the opening up of domestic flights. Severe liquidity problems were experienced by the hospitality industry (airlines, hotels and restaurants). Amidst this economic uncertainty and a collapsing growth rate, the RBI slashed repo rates to provide stimulus to the economy, increase liquidity in the market and possibly reduce the cost of financing for the corporate sector. Despite these efforts, the growing number of COVID-19 cases casts a shadow on the recovery of the economy in the near future.
Discussion
Understanding the impact of the COVID-19 pandemic on any country and analysing the impact of interventions that were intended to contain it requires several critical considerations at the present (in addition to a lot more data in the future to substantiate any findings, in the absence of any precedents). One needs to appreciate the size of a nation; consider its population, the socio-economic fabric of which can support or cripple any policy intervention; have a thorough grasp of how good or bad its healthcare system was in the first place; have the right definition of success criteria in line with the extent of the spread of the virus; and possess the ability to identify relevant and useful data.
COVID-19 vis a vis the Indian context
In a developing country such as India, with the world's second-highest population, fifth-largest economy, the fastest-growing major economy [77], and one of the lowest healthcare expenditures per capita, it is easy to see how a disaster such as the COVID-19 pandemic would be catastrophic for the nation, both in terms of lives and livelihoods. Even the most earnest, massive, and unprecedented policy and technological interventions would be at best limited in their ability to solve the prevailing problems. Despite this, the country has fared much better than many other developing countries in managing the health impact of the crisis so far.
Health impact
Our study found that the high recovery rate from COVID-19 in India was a result of significant technological interventions, effective mitigation policies implemented in a phased manner by the government, complemented by the demographic dividend. However, any initial success of handling the pandemic will not last without continuous and reliable testing followed by contact tracing [78]. For instance, the state of Kerala, which was initially leading the country's war against the pandemic, later showed a significant drop in recovery rates due to a resurgence in confirmed cases [79]. With stark variations in the numbers of tests as well as COVID-19 trends across the states of India, they were uniquely equipped to handle the pandemic.
While increased testing has been proposed as the most potent solution to COVID-19 globally, it is important to understand country-specific nuances around how testing is being carried out and how it should be done, to arrive at the right solution for India. An increased capacity to manufacture testing kits in India is commendable but will only make a difference to the overall spread of the pandemic if it aligns with the number of tests conducted daily, dependent on the availability of healthcare services. Again, variations in COVID-19 tests conducted to accelerate national level testing should be based on the reliability of results, so as not to slow down contact tracing efforts.
Economic impact
On the economic side, high unemployment during the nationwide lockdown, instead of an initial lockdown policy based on disease spread within states [80], complemented by paid-for testing and expensive treatment for COVID-19 in private facilities, have only exacerbated the existing state of economic inequity [81]. On the surface, while the resumption of economic activity amid the pandemic looks set to lead to economic recovery, the economic modelling used shows that the average monetary value per human life lost from COVID-19 in India translates to 7.09–8.22-fold of the country's GDP per capita.
Conclusions and policy implications
The spread of COVID-19 in India has tested the country's pandemic preparedness in terms of its health infrastructure, technological capabilities and policy interventions. The initial impact of a timely and one of the most stringent lockdown policies was observed to slow the spread of the virus. At the same time, it helped the country to prepare critical medical infrastructure, human resources and technological advances. The severity of the COVID-19 pandemic in India has been relatively low compared with many other developing countries in terms of case fatality and recovery rates. However, the crisis has augmented the pre-existing risks of economic slowdown, while the underfunded public healthcare system has played havoc with the pandemic management strategy in the country. Overall, the pandemic has been a wake-up call and India is now consciously thinking about embracing long-term measures to develop a responsive, sustainable and robust healthcare system, to which PPPs and the manufacturing sector might make significant contributions.
Limitations of the study and scope of future work
Due to limitations of data relating to existing and augmented infrastructure facilities in terms of hospitals, beds and ventilators, a comparison of pre- and post-COVID-19 infrastructure is missing. Case fatality rate analysis based on co-morbidities is missing due to insufficient availability of secondary data. Future work could include recommendations for possible revisions to the existing population-level policy, taking a cue from other countries. This could help ensure comparable infrastructure and resources to face future pandemics.
Funding
None.
Ethical approval
Not required.
CRediT authorship contribution statement
Isha Goel: Conceptualization, Data curation, Formal analysis, Writing - original draft, Writing - review & editing. Seema Sharma: Supervision. Smita Kashiramka: Supervision, Writing - review & editing.
Declaration of Competing Interest
None declared.
Acknowledgment
We are thankful to Avinav Goel and Mohd. Ahmad Khalid.
References
- 1.Chen N., Zhou M., Dong X., Qu J., Gong F., Han Y. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(Feb. 10223):507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.WHO. Coronavirus Disease (COVID-19) India Situation Report 2020. Available from: https://www.who.int/india/emergencies/coronavirus-disease-(covid-19)/india-situation-report.
- 3.Worldometer. Coronavirus Cases 2020. Available from: https://www.worldometers.info/coronavirus/.
- 4.World Health Organization (WHO). Global Health Observatory Country Views. Available from: https://apps.who.int/gho/data/node.country.country-IND?lang=en.
- 5.The World Bank. Available from: https://data.worldbank.org/.
- 6.Central Bureau of Health Intelligence (CBHI). National Health Profile (2019); 2019:1-314. Available from: https://www.thehinducentre.com/resources/article29841374.ece/binary/8603321691572511495.pdf.
- 7.All India Institute of Medical Sciences. National Diabetes Retinopathy Survey 2015-2019;2019. Available from: https://neoiascap.com/2019/10/13/national-diabetes-and-diabetic-retinopathy-survey-report-2015-19/social-sector/health/.
- 8.Ramakrishnan S., Zachariah G., Gupta K., Shivkumar Rao J., Mohanan P.P., Venugopal K. CSI-great India BP campaign investigators. Prevalence of hypertension among Indian adults: results from the great India blood pressure survey. Indian Heart J. 2019;71(4):309–313. doi: 10.1016/j.ihj.2019.09.012. Jul–Aug. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.OECD Data. Available from: https://data.oecd.org/pop/population.htm.
- 10.National Health Accounts Technical Secretariat(NHATS). National Health Systems Resource Centre(NHSRC), MoHFW. Government Health Expenditures in India (2013-14); 2017. Available from: http://164.100.117.80/sites/default/files/Final%20Government%20Health%20Expenditure%20Report%20-%20Web%20Optimized%20Version%20-%2020.06.17.pdf.
- 11.CBHI. National Health Profile (2013). Available from: https://cbhidghs.nic.in/index1.php?lang=1&level=2&sublinkid=84&lid=75.
- 12.Insurance Regulatory and Development Authority of India. Handbook of Indian Insurance Statistics 2017-18; 2019. Available from: https://www.irdai.gov.in/ADMINCMS/cms/whatsNew_Layout.aspx?page=PageNo3729&flag=1.
- 13.Brookings. COVID-19 | Is India's health infrastructure equipped to handle an epidemic? Available from: https://www.brookings.edu/blog/up-front/2020/03/24/is-indias-health-infrastructure-equipped-to-handle-an-epidemic/.
- 14.The Centre for Disease Dynamics Economics and Policy. COVID-19 in India; 2020. Available from: https://cddep.org/wp-content/uploads/2020/04/State-wise-estimates-of-current-beds-and-ventilators_24Apr2020.pdf.
- 15.Business Standard. With 75% grossly underinsured, why aren't Indians sufficiently covered? Available from: https://www.business-standard.com/article/current-affairs/with-75-grossly-underinsured-why-aren-t-indians-sufficiently-covered-119011500150_1.html.
- 16.MoHFW. Government of India Report: task force on medical education for the National Rural Health Mission. Available from: http://www.mohfw.nic.in/NRHM/Documents/Task_Group_Medical_Education.pdf.
- 17.Confederation of Indian Industry. KPMG. The emerging role of PPP in Indian Health Sector. Available from: https://www.ibef.org/download/PolicyPaper.pdf.
- 18.The Indian Express. Price of COVID treatment capped in Delhi: how much you have to pay? Available from: https://indianexpress.com/article/explained/delhi-covid-19-test-price-6466528/.
- 19.Press Information Bureau (PIB). Government of India. Available from: https://pib.gov.in/PressReleseDetailm.aspx?PRID=1611539.
- 20.National Informatics Centre. Government of India. Available from: https://covidwarriors.gov.in/default.aspx.
- 21.India Today. Centre issues parameters for the classification of red, orange, and green zones. Available from: https://www.indiatoday.in/india/story/health-ministry-issues-parameters-for-classification-of-red-orange-and-green-zones-all-you-need-to-know-1679390-2020-05-18.
- 22.Chatterjee P., Seth B., Biswas T.. Hotspots of H1N1 influenza in India: analysis of reported cases and deaths (2010-2017) Trop Doct. 2020;50(Apr. 2):166–169. doi: 10.1177/0049475519879357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.COVID-19 India. Available from: https://www.covid19india.org/.
- 24.The Hindu. Coronavirus India lockdown day 116 updates. Available from: https://www.thehindu.com/news/national/india-coronavirus-lockdown-july-18-2020-live-updates/article32120554.ece.
- 25.Indian Institute of Population Sciences. Available from: https://iipsindia.ac.in/sites/default/files/iips_covid19_cfrr.pdf.
- 26.The Lancet India under COVID-19 lockdown. Lancet. 2020;395(Apr. 10233) doi: 10.1016/S0140-6736(20)30938-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sharma A., Kumar Sharma S., Shi Y., Bucci E., Carafoli E., Melino G. BCG vaccination policy and preventive chloroquine usage: do they have an impact on COVID-19 pandemic? Cell Death Dis. 2020;11(7):1–10. doi: 10.1038/s41419-020-2720-9. Jul. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Qasim, B., Yusuf, J. Will coronavirus pandemic diminish by summer? 2020. Available from: SSRN 3556998.
- 29.Brookings. How well is India responding to COVID-19? Available from: https://www.brookings.edu/blog/future-development/2020/07/02/how-well-is-india-responding-to-covid-19/.
- 30.Ayog NI. MoHFW, World Bank. Healthy States Progressive India; 2019. Available from: http://social.niti.gov.in/uploads/sample/health_index_report.pdf.
- 31.World Asia. Kerala's COVID-19 fight success due to public-private partnership. Available from: https://gulfnews.com/world/asia/india/keralas-covid-19-fight-success-due-to-public-private-partnership-1.71172128.
- 32.Matters India. Is Kerala losing its COVID battle. Available from https://mattersindia.com/2020/06/is-kerala-losing-its-covid-battle/.
- 33.The Hindu. COVID-19 resurges in Kerala as migrants return, testing rate drops. Available at: https://www.thehindu.com/data/covid-19-resurges-in-kerala-as-migrants-return-testing-rate-drops/article32087258.ece.
- 34.BBC. India coronavirus: How Kerala's COVID's success story came undone. Available at: https://www.bbc.com/news/world-asia-india-53431672.
- 35.Joe W., Kumar A., Rajpal S., Mishra U.S., Subramanian S.V. Equal risk, unequal burden? Gender differentials in COVID-19 mortality in India. J Glob Health Sci. 2020;2(1):1–65. doi: 10.1162/99608f92.60e08ed5. [DOI] [Google Scholar]
- 36.Ray D., Salvatore M., Bhattacharyya R., Wang L., Du J., Mohammed S., Purkayastha S., Halder A., Rix A., Barker D., Kleinsasser M. Predictions, role of interventions and effects of a historic national lockdown in India's response to the COVID-19 pandemic: data science call to arms. Harvard Data Sci Rev. 2020;2020(Suppl 1) doi: 10.1162/99608f92.60e08ed5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.PIB. Available from: https://pib.gov.in/newsite/bulletinn.aspx.
- 38.World Trade Organization. Available from: https://www.wto.org/.
- 39.Moy, N., Antonini, M., Kyhlstedt, M., Paolucci, F. Categorising policy & technology interventions to COVID-19: a comparative and conceptual framework. SSRN 2020. Available from: SSRN 3622966.
- 40.Pharmaceutical Drug Manufacturers. India 3rd largest producer of pharmaceuticals across the world. Available from: http://www.pharmaceutical-drug-manufacturers.com/news/india-3rd-largest-producer-pharmaceuticals.html.
- 41.The Economic Times. India sending hydrooxychloroquine to 55 coronavirus hit countries. Available from: https://economictimes.indiatimes.com/news/politics-and-nation/india-sending-hydroxychloroquine-to-55-coronavirus-hit-countries/articleshow/75186938.cms?from=mdr.
- 42.Centre for Monitoring Indian Economy. (2020). Available from: https://www.cmie.com/kommon/bin/sr.php?kall=warticle&dt=2020-04-28%2010:29:55&msec=990.
- 43.Business Today. India's unemployment rate hits 26% amid lockdown: CMIE 2020. Available from: https://www.businesstoday.in/current/economy-politics/india-unemployment-rate-hits-26-amid-lockdown-14-crore-lose-employment-cmie/story/401707.html.
- 44.The Economic Times. India's 20 lakh crore economic package. Available from: https://economictimes.indiatimes.com/news/economy/finance/latest-stimulus-package-among-largest-in-the-world/articleshow/75701976.cms.
- 45.Live Mint. India becomes fifth country to isolate virus strain. Available from: https://www.livemint.com/news/india/covid-19-india-becomes-5th-country-globally-to-isolate-virus-strain-11584102221498.html.
- 46.TSG. India emerges as world's key vaccine manufacturing hub. Available from: https://www.sundayguardianlive.com/news/india-emerges-worlds-key-vaccine-manufacturing-hub.
- 47.Khaleej Times. Coronavirus: Indian experts back blood plasma therapy to treat COVID-19. Available from: https://www.khaleejtimes.com/coronavirus-pandemic/coronavirus-indian-experts-back-blood-plasma-therapy-to-treat-covid-19.
- 48.Express Pharma. Remedesivir in India. Available at: https://www.expresspharma.in/covid19-updates/remdesivir-in-india-an-unfolding-story/.
- 49.Times of India. Homeopathy for Coronavirus treatment. Available from: https://timesofindia.indiatimes.com/life-style/health-fitness/home-remedies/homeopathy-for-coronavirus-treatment-does-it-work/photostory/76176772.cms?picid=76176796.
- 50.Live Mint. India now manufactures 5.5. lakh PPE suits a day in the fight against COVID-19. Available from: https://www.livemint.com/news/india/india-now-manufactures-4-5-lakh-ppe-suits-a-day-in-the-fight-against-covid-19-11589951566951.html.
- 51.The Indian Express. Delhi Corona App. Available from: https://indianexpress.com/article/explained/delhi-corona-mobile-application-covid-19-6438796/.
- 52.Deccan Herald. App to provide information on ICU beds, ventilators in Mumbai. Available from: https://www.deccanherald.com/national/app-to-provide-information-on-icu-beds-ventilators-in-mumbai-850892.html.
- 53.Directorate of Information and Public Relations. Punjab. Cova Mobile App. Available from: http://www.punjabtribune.com/news/228136-cova-mobile-app-helping-citizens-and-government-agencies-during-covid-19-pandemic-reaches-to-more-than-50-lac-users-v.aspx.
- 54.IIT Delhi. Available from: https://home.iitd.ac.in/news-diagnostic-kit.php.
- 55.Deccan Herald. Karnataka doctors suggest home isolation. Available from: https://www.deccanherald.com/state/karnataka-doctors-suggest-home-isolation-telemedicine-for-asymptomatic-covid-19-patients-855927.html.
- 56.BBC. How Asia's biggest slum contained the virus. Available from: https://www.bbc.com/news/world-asia-india-53133843.
- 57.The Times of India. COVID-19: 80% positive cases show no or mild symptoms, says govt. Available from: https://timesofindia.indiatimes.com/india/80-positive-cases-show-no-or-mild-symptoms-says-govt/articleshow/75261488.cms.
- 58.MoHFW. Revise discharge policy for COVID-19. Available from: https://www.mohfw.gov.in/pdf/ReviseddischargePolicyforCOVID19.pdf.
- 59.BBC. Coronavirus: India is turning to faster tests to meet the targets. Available from: https://www.bbc.com/news/world-asia-india-53609404.
- 60.The Times of India. India's COVID testing rate is low says WHO Chief Scientist. Available from: https://timesofindia.indiatimes.com/life-style/health-fitness/health-news/indias-covid-testing-rate-is-low-says-who-chief-scientist/articleshow/77364306.cms.
- 61.The Print. Capacity is not what is hindering India's testing rate, government price caps are. Available from: https://theprint.in/opinion/capacity-is-not-whats-hindering-indias-testing-rate-government-price-caps-are/460106/.
- 62.COVID-19 Resource Center. Available from: http://covidindiaupdates.in/testing.php.
- 63.MoHFW. 2020. Guidance document on appropriate management of suspected or confirmed cases of COVID-19 (2020); 2020. Available from: https://www.mohfw.gov.in/pdf/FinalGuidanceonMangaementofCovidcasesversion2.pdf.
- 64.PIB. Available from: https://pib.gov.in/PressReleasePage.aspx?PRID=1638792.
- 65.Press Trust of India. Coronavirus outbreak: AIIMS announces only life-saving surgeries be taken up. Available from: https://www.financialexpress.com/lifestyle/health/coronavirus-outbreak-aiims-announces-only-life-saving-surgeries-be-taken-up/1905092/.
- 66.Rahman M.S., Peeri N.C., Shrestha N., Zaki R., Haque U., Hamid S.H. Defending against the novel coronavirus (COVID-19) outbreak: how can the Internet of Things (IoT) help to save the world? Health Policy Technol. 2020:136–138. doi: 10.1016/j.hlpt.2020.04.005. Jun. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Kirigia J.M., Muthuri R.N. The fiscal value of human lives lost from coronavirus disease (COVID-19) in China. BMC Res Notes. 2020;13(Apr. 1):198. doi: 10.1186/s13104-020-05044-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Bloomberg. World Bank says Indian Economy to contract by 3.2% in FY21. Available from: https://www.bloombergquint.com/business/india-s-economy-to-contract-by-3-2-per-cent-in-fiscal-year-2020-21-world-bank.
- 69.Business Today. IMF's projection of 1.9% GDP growth for India highest in G-20, says RBI Governor Das. Available from: https://www.businesstoday.in/current/economy-politics/imf-projection-19-gdp-growth-for-india-highest-in-g20-rbi-governor-das/story/401295.html.
- 70.KPMG India. Potential impact of Covid-19 on Indian Economy (April 2020). 2020.Available from: https://home.kpmg/content/dam/kpmg/in/pdf/2020/04/potential-impact-of-covid-19-on-the-indian-economy.pdf.
- 71.Ministry of Statistics and Programme Implementation, Government of India. Available from: http://www.mospi.gov.in/press-release?field_press_release_category_tid=All&date_filter%5Bmin%5D&date_filter%5Bmax%5D&page=1.
- 72.Moody's. Moody's Investor Service. Available from: https://www.moodys.com/research/Moodys-downgrades-Indias-ratings-to-Baa3-maintains-negative-outlook–PR_424605.
- 73.Delloite India (2020). Impact of COVID-19 on consumer business in India. Available from: https://www2.deloitte.com/content/dam/Deloitte/in/Documents/consumer-business/in-consumer-impact-of-covid-19-on-consumer-business-in-india-noexp.pdf.
- 74.Live Mint. COVID-19 pulls down India's exports by 34.6% in March.; trade-deficit narrows to $ 9.8 bn. Available from: https://www.livemint.com/news/india/india-s-trade-deficit-narrows-to-9-8-bn-in-march-exports-dip-34-6-11586955282193.html.
- 75.McKinsey and Company. McKinsey Center for Future Mobility. Available from: https://www.mckinsey.com/~/media/McKinsey/Industries/Automotive%20and%20Assembly/Our%20Insights/The%20unexpected%20trip%20The%20future%20of%20mobility%20in%20India%20beyond%20COVID%2019/The-unexpected-trip-The-future-of-mobility-in-India-beyond-COVID-19-Final.pdf.
- 76.Media India Group. India is the third-largest domestic aviation market in the world. Available from: https://mediaindia.eu/aviation/india-is-the-third-largest-domestic-aviation-market-in-the-world/.
- 77.Nasdaq. The five largest economies in the world and their growth in 2020. Available from: https://www.nasdaq.com/articles/the-5-largest-economies-in-the-world-and-their-growth-in-2020-2020-01-22.
- 78.Salathé M., Althaus C.L., Neher R., Stringhini S., Hodcroft E., Fellay J. COVID-19 epidemic in Switzerland: on the importance of testing, contact tracing and isolation. Swiss Med Wkly. 2020;150(Mar. 11-12):w20225. doi: 10.4414/smw.2020.20225. [DOI] [PubMed] [Google Scholar]
- 79.The Hindu. Watch | Why COVID-19 cases are surging in Kerala. Available from: https://www.thehindu.com/news/national/kerala/covid-19-resurges-in-kerala/article32248324.ece.
- 80.Arora P., Kumar H., Panigrahi B.K. Prediction and analysis of COVID-19 positive cases using deep learning models: a descriptive case study of India. Chaos Solitons Fractals. 2020;139 doi: 10.1016/j.chaos.2020.110017. Oct. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Brookings. The impact of COVID-19 and the policy response in India. Available from: https://www.brookings.edu/blog/future-development/2020/07/13/the-impact-of-covid-19-and-the-policy-response-in-india/.