Abstract
Background
The communication process of preparing patients and families facing progressive neurodegenerative diseases for future illness has not been empirically elucidated; the goal of this qualitative study was to explore neurology interdisciplinary health professionals' communication experiences, including current approaches, facilitators, and challenges.
Methods
Three focus groups were conducted with 22 clinicians representing a range of health professions from several multidisciplinary neurology outpatient clinics at a large academic medical center. A thematic analysis approach was used to develop a coding structure and identify overarching themes.
Results
Neurology clinicians highlighted that in their practice, (1) conversations are triggered by acute events and practical needs; (2) conversations occur routinely but are rarely documented; (3) loss of patient capacity and resultant surrogate decision-making can be ethically fraught, especially in times of family conflict; (4) prognostic uncertainty, unfamiliarity with disease trajectories, and patient or surrogate avoidance pose communication challenges; and (5) generalist- and specialty-level palliative care roles should be better defined.
Conclusions
There is a need for a systematic, structured approach to communication that can be applied early in the disease trajectory and considered when developing integrated neuro-palliative care programs.
Many neurologic diseases remain incurable and fatal, with death preceded by gradual, deteriorating trajectories involving debility and stress for patients and caregivers.1–5 Unique challenges associated with neurodegenerative diseases include a lack of curative therapies, heterogeneous trajectories, and communication or cognitive impairment. Given the reduced life expectancy, associated symptoms, and caregiver strain, these patients are one of the nononcologic populations most in need of palliative care,2–5 a specialty that aims to improve the quality of life of seriously ill patients by providing relief from symptoms and stress throughout the illness.6,7
In preparing patients for future illness, neurologists often undertake multiple types of palliative care communication2,8 including advance care planning, understanding wishes and priorities, discussing prognosis and treatment goals, and addressing psychosocial needs. However, neurologists receive little formal training in palliative care9–14 and little is known about the communication challenges faced by neurology clinicians. To understand current palliative care communication approaches, facilitators, and challenges, we conducted focus group interviews with interdisciplinary clinicians from memory disorders (dementia) and amyotrophic lateral sclerosis (ALS) clinic settings.
Methods
Design
This qualitative study took place at a single academic institution providing specialist care to patients with neurodegenerative conditions. Focus groups were chosen to encourage self-disclosure and allow for real-time data verification; this also allows members to enrich each other's participation and explore differing opinions. Three focus groups were conducted with medical and nursing clinic staff using a semistructured interview guide (appendix e-1, links.lww.com/CPJ/A161). Physician and nurse practitioner (NP) focus groups were separated by clinic type (ALS and dementia) to explore potential thematic differences between clinics. We conducted a separate nursing focus group to ensure nurses' comfort in reporting perspectives without supervisors present.
Participants
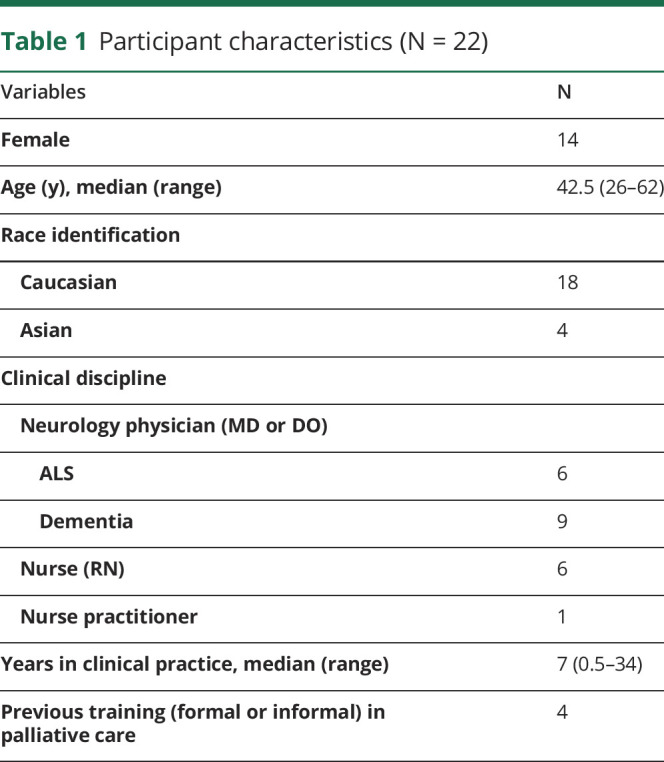
The multidisciplinary ALS clinic consists of physicians, NPs, nurses, and therapists and provides care from diagnosis to death plus clinical research opportunities; patients are typically seen every 3 months or sooner if needed. The multidisciplinary memory disorders clinic consists of physicians, psychologists, and nurses providing care to patients throughout the illness, with patients typically seen every 3–6 months. Physicians, NPs, and nurses from both clinics were invited in person and through email to voluntarily participate in the study. Clinicians were eligible if they provided clinical care in these practices within one of these disciplines. We used a sample size that balanced the likelihood of thematic data saturation and study feasibility. A total of 22 clinicians participated (table 1).
Table 1.
Participant characteristics (N = 22)
Data collection
Focus groups were held in private rooms and moderated by a licensed clinical psychologist with expertise in qualitative research methodology who was unknown to the participants (L.T. or J.A.G.). Interviewers had training in eliciting participant responses and encouraging disclosure and different opinions. With participant consent, discussions were audio recorded and transcribed verbatim. Based on a literature review and experience, our interdisciplinary research team (composed of clinicians in palliative care, neurology, and psychology) developed and iteratively modified the semistructured interview guide before conducting the focus groups. The literature review involved multiple database searches for original research studies across all health disciplines about nervous system diseases, palliative care, and communication. Several other neurology experts reviewed the guide to improve clarity and reduce bias. The questionnaire consisted of open-ended questions about the timing, nature and quality of palliative care communication, facilitators, challenges and improvement opportunities, and perceived support and training needs. Participant sociodemographic data were collected (table 1).
Data analysis
We used a thematic analysis approach and analyzed data using the constant comparison method. Three members of the team (A.M.H., J.A.G., M.N.-L.) developed a coding scheme inductively. Using qualitative data analysis software (QSR NVIVO 10) to maintain an audit trail, 2 study members (A.M.H. and M.N.-L.) independently coded transcriptions line by line and then compared for agreement. Codes were added, modified, or merged iteratively on coder agreement, and a third researcher resolved discrepancies. We examined the coded data to identify organizing themes and selected reflective quotes for each. We explored potential thematic differences between clinics and disciplines and did not identify any except as noted below.
Standard protocol approvals, registrations, and consents
Our hospital's Institutional Review Board provided ethical approval for this study. We obtained verbal informed consent from all study participants before starting each focus group interview.
Data availability
The data in this manuscript cannot be shared for ethical reasons because it must remain protected per the Health Insurance Portability and Accountability Act per our consent process.
Results
We conducted 3 focus groups: one with ALS clinic providers (n = 7), one with memory disorders clinic providers (n = 9), and one with nurses from both clinics (n = 6) (table 1). All medical and nursing staff of each clinic were invited. Enrollment rates were 70% for the ALS group, 90% for the memory disorders group, and 100% for the nursing group. Participant characteristics are shown in table 1. Of the clinicians, 64% were women and 82% were Caucasian. The median reported age was 42.5 years, and median years in practice was 7, with 18% of participants endorsing some previous palliative care training such as didactics (e.g., lectures, continuing education courses) and/or clinical electives.
Themes
Participants identified several issues associated with palliative care communication with their patients, and we categorized these into 5 overarching themes (table 2). Below outlines a description of each.
Table 2.
Themes and supporting quotations
Conversations are triggered by acute events and practical needs
ALS clinicians viewed procedural events, such as gastrostomy tube placement, as the main impetus for initiating larger conversations with patients. One clinician described having in-depth “goals of care” discussions “under the guise of” periprocedural necessity. Others recognized the importance of such conversations in this setting given the associated procedural risk, including identifying a legal surrogate decision maker and documenting life-sustaining treatment preferences. Although procedures were convenient triggers, this approach was also recognized as potentially overwhelming for patients and families. As one clinician stated, “one thing leads to another” and “it's a lot.”
Both ALS and memory disorders clinicians felt that a patient's practical care needs (including increasing home needs or need for institutionalization) factor heavily into medical decision-making conversations, including hospice discussions. As one clinician explained, the initiation of conversations and care plan are sometimes “driven by logistics” rather than a philosophical shift in goals.
Many conversations happen but are rarely documented
Neurology clinicians reported that frequent in-person team communication allows them to track each patient's clinical progression, cognitive processing, and coping over time. This information is not formally documented in the health record, but “everyone is kind of aware of what's going on with every patient.” This strategy works within a closed clinic setting, but a lack of structured, centrally located documentation that is accessible to other clinicians or institutions is a common challenge. Perceived “missed opportunities” during care transitions include the lack of a shared communication framework, burdensome written documentation that does not capture clinical complexities and nuances, and poor retrievability of useful information in the health record.
Cognitive impairment prompts increased surrogate decision-making, which can be ethically fraught when conflict arises
Cognitive impairment was identified as a unique communication challenge. Clinicians expect the decision-making burden will shift from patient to surrogate over time and emphasized the importance of identifying a patient's primary caregiver “up front.” One clinician noted that this had been routinized in the memory clinic: “Before setting up the very first visit in our unit, we always identify who's the caregiver.” Clinicians also identified the importance of early goals and values conversations while patients can still participate. These conversations help guide decision-making with surrogates later in the illness. One memory disorders clinician recalled many conversations with cognitively intact or “mildly impaired” patients in which “you get to hear what their wishes are,” adding that some patients “make it very clear.” Clinicians did not discuss documenting these verbalized wishes.
Despite the expected shift to surrogate decision-making over time, this change is fraught when conflict arises. Family conflict was identified as “very problematic” when patients' wishes were not known in advance. Although participants did not specify the frequency of these situations, they discussed the resultant clinician unease: clinicians worry that the patient's voice is not being represented or that a surrogate's emotional burden or competing agendas may overshadow patient autonomy. Because these issues are “very hard to resolve,” conflict leads to stagnation in care. Multiple clinicians remarked how useful it would be to have timely access to an ethicist for such situations.
Multiple clinician-, patient-, and disease-related factors pose communication challenges
Clinicians identified several clinician-related factors that impair communication and decision-making. First, non-neurology clinicians often lack familiarity with neurodegenerative diseases and associated care needs.15,16 Second, skilled nursing facility care is “quite variable”: clinicians reported difficulty contacting facility staff, varying receptivity to the neurology clinician's recommendations, and a lack of structured communication as barriers to enacting medically appropriate, goal-concordant care for nursing home residents. Third, the lack of neurology expertise in hospice affects the quality of end-of-life care. One ALS clinician noted the hospice approach “isn't always on target” because these patients' needs are often “totally different” than cancer patients': they need frequent attention and assistance with activities of daily living rather than intensive symptom management.
Patient-related factors also impaired communication and decision-making. Clinicians noted that many people have some pre-existing knowledge of common diseases such as cancer. However, in these lesser understood neurodegenerative illnesses, a lack of disease familiarity combined with highly variable patterns of decline makes it difficult for patients and families to understand the multitude of medical decisions that arise, including (1) how to approach “reversible” medical problems in the context of a progressive, life-limiting illness, (2) how to weigh the risks and benefits of repeat hospitalizations, (3) when to prioritize comfort and where hospice care should be provided, and (4) when to forego “standard” care for unrelated medical issues because cognitive impairment limits one's ability to tolerate treatment. This unfamiliarity underscores the need for ongoing patient education by staff. Neurology clinicians viewed their role in “reframing” the medical situation as an important facilitator in these situations. This includes deepening patients' and families' illness understanding and guiding decisions based on the medical reality. Clinicians also reflected that communication during these situations can be challenging, especially given the prognostic uncertainty. Explaining to patients with ALS that underlying disease progression is the reason for repeated “reversible” pneumonias is “harder because there's even more uncertainty” regarding recovery potential. Helping people recognize these staccato medical setbacks (which seem quite treatable in isolation) as an actual worsening of their terminal illness is difficult. One clinician wondered “if there's thinking about that in palliative care that could…help people understand” this.
Communication is further challenged by patients or families who are reticent to acknowledge the terminality of these illnesses. Resistance to discussing prognosis was particularly difficult when patients' and caregivers' communication preferences differed. Sometimes patients “want to hear about it,” but their caregivers do not. One clinician said of this dilemma, “Sometimes you get stuck in a situation where there is an adamant caregiver that will try and block that communication.” If the patient is “more impaired,” clinicians often acquiesce to the caregiver's request, given their increased decision-making responsibility.
Specifying the role of specialty palliative care is difficult because much of neurologic care is palliative
Neurology clinicians perceived that given the incurable, progressive nature of neurodegenerative diseases, in essence, all care is palliative. One clinician described feeling “like a palliative nurse more days of the week than a neuro nurse” because her focus is patients' comfort. Palliative care provided by neurology clinicians is given throughout the illness and is an “evolution,” characterized by ongoing symptom management, slowly deepening patients' and families' illness understanding, and increasing caregiver support over time.
This gradual escalation is reflected in the treatment approach and communication strategies used. In neurology, many disease-directed therapies are not as burdensome or “toxic” as cancer treatments and are often reasonable to continue even late in the disease. As one clinician stated, “There's not this tension between “Will we do this horrible thing that's going to make the person really sick?”…it's just ‘How do you frame this…?’” Beyond the communication skill of reframing, many neurology clinicians effectively manage symptoms without specialist palliative care involvement. ALS clinicians noted that many of their patients “don't have a lot of pain” and dyspnea is often “pretty easy to treat.”
Neurology clinicians described the difficulty in distinguishing between generalist- and specialty-level palliative care and appropriate triggers for specialty referral. As one clinician expressed, “It would be really, really useful to understand very clearly what a palliative care team can offer our patient population at what time point.”
Discussion
We conducted a qualitative study to understand neurology clinicians' current approaches, challenges, and facilitators to palliative care communication with patients facing neurodegenerative illnesses. Our analysis identified 5 themes that highlight the critical role of the neurology clinician as a de facto palliative care clinician across the illness trajectory, particularly in the realm of communication.
Our work revealed that the current approach to communication unfolds over time with multiple people. Complex patient-, clinician-, and disease-related factors affect the timing and nature of communication. Conversations are usually reactive to acute medical events or increasing care needs. Even later discussions about hospice mostly stem from escalating care needs rather than a frameshift in philosophy of care. Once triggered, conversations are often led by neurology physicians or NPs with support from nursing staff. In-person interdisciplinary team communication about such conversations is commonplace, whereas written documentation is not. Conversations usually include caregivers, so identifying these individuals is an early clinical priority. When capacity is in question or conflict emerges, clinicians report having little support to navigate these situations.
Neurology clinicians highlight 3 communication challenges. The first is when to begin. Although procedures and increasing care needs are convenient triggers, clinicians recognize this timing is suboptimal. When patients and families are facing acute medical issues, they are often overwhelmed with immediate details, with little capacity to engage in conversations about planning ahead. Alternatively, early conversations during stable times enable preparation. For patients with ALS and dementia, it has been suggested that conversations occur routinely during scheduled clinic visits.8 Event-driven milestones have also been proposed,8,17 including increasing symptom burden, declining functional status, caregiver strain, hospitalization, nutritional concerns, wandering or driving concerns for dementia, and dysphagia or hypoventilation for ALS.18
The second challenge is how to support patients and surrogates in a decision-making process over time. Clinicians struggle to respect patient autonomy and ensure safe decision-making, especially when capacity is in question. This dynamic can be further complicated by the surrogate's fear of losing a loved one and miscommunication with clinicians.19 Evidence suggests that patients and surrogates can best be supported through high-quality communication and preparation,19,20 including forecasting common medical decisions such as nursing home placement and recommending that patients grant surrogates decision-making flexibility as the illness evolves.
The third challenge is a general unfamiliarity with neurodegenerative diseases. Neurology clinicians report what has been shown elsewhere: that many patients and families lack understanding of their illness or treatment goals and hold unrealistic views about their prognosis.21,22 Non-neurology clinicians can be equally unfamiliar with these diseases and associated care needs, including variable disability and complex cognitive, behavioral, or communication problems.23 Clinicians' lack of expertise complicates team communication and care coordination. For example, neurology clinicians struggle to convey medical and behavioral management plans to skilled nursing facilities. A lack of understanding has also led to resource gaps, and neurology clinicians express concern that organizations such as hospice cannot adequately accommodate patients' needs. Hospice and palliative care specialists echo this perspective, reporting staff and facility shortcomings and a need for additional training in neurology care.23
Neurology clinicians also identified several communication facilitators. Clinicians highlighted the value of early, upstream discussions with competent patients about goals and priorities to inform later decision-making. Conversations were especially useful when they included caregivers because this prepares them for their future surrogate decision-making role and ideally avoids future conflict. Most importantly, clinicians identified that regardless of conversation timing, it is useful to have a common communication framework and specific language to deepen patients' and families' understanding, elicit goals and values, and support goal-concordant medical decisions. Using an intentional, structured approach and effective language is considered best practice,24,25 and evidence suggests that these skills can be taught and learned.26–30 Clinicians also recognized that after conversations occur, having an equally systematized approach to documentation results in more efficient team communication and care coordination across settings. A systems-based solution to communication has been reported and improves the occurrence rate, timing, quality, and accessibility of documented conversations.31,32
This study has several important strengths. It is one of very few studies exploring communication facilitators and challenges faced by neurology clinicians. Interdisciplinary clinicians were studied, so multiple experiences and viewpoints were represented. Although participating clinicians specialize in dementia and ALS care, many of the themes apply across neurologic diagnoses. A multidisciplinary research team participating in all study phases helped reduce individual bias. The use of software to maintain an audit trail to document coding decisions further enhanced study rigor.
This study also has some limitations. The study was conducted at a single academic site and reflects clinician viewpoints within 2 specific clinics providing ALS and dementia care. Many seriously ill neurology patients receive care outside of this practice setting; an important next step is to examine the viewpoints of private practice or community-based clinicians whose practice patterns and needs may differ. Other neurologic conditions were not represented here; examining the needs of other vulnerable neurology patient populations is another important area for future research. Some study participants may have not disclosed views that differed from most of the group. Only medical and nursing disciplines were interviewed, so the roles and challenges of other clinicians may not be represented in our data. Participants were part of a well-established team, many of whom had worked together for years; this may confer some degree of homogeneity in clinical practice styles, which may not be true everywhere.
Neurology clinicians have a critical role to play in providing generalist palliative care to patients with progressive neurodegenerative diseases, particularly regarding communication. Our study illustrates when and how conversations unfold over time and challenges and facilitators of high-quality communication. These findings are an important starting point to enhance palliative care for this vulnerable population.
Acknowledgment
The authors thank Anne Griggs and Sean Langan, PhD (Massachusetts General Hospital, Division of Palliative Care & Geriatric Medicine) and Abagail Stacey, Jennifer Scalia, NP, Liang Yap, PhD, and Teresa Gomez-Isla, MD, PhD (Massachusetts General Hospital, Department of Neurology) for their administrative assistance; Darlene Sawicki, MSN, NP-BC (Massachusetts General Hospital, Department of Neurology) for her administrative assistance and expert input; and Bradford Dickerson, MD (Massachusetts General Hospital, Department of Neurology) for his expert input.
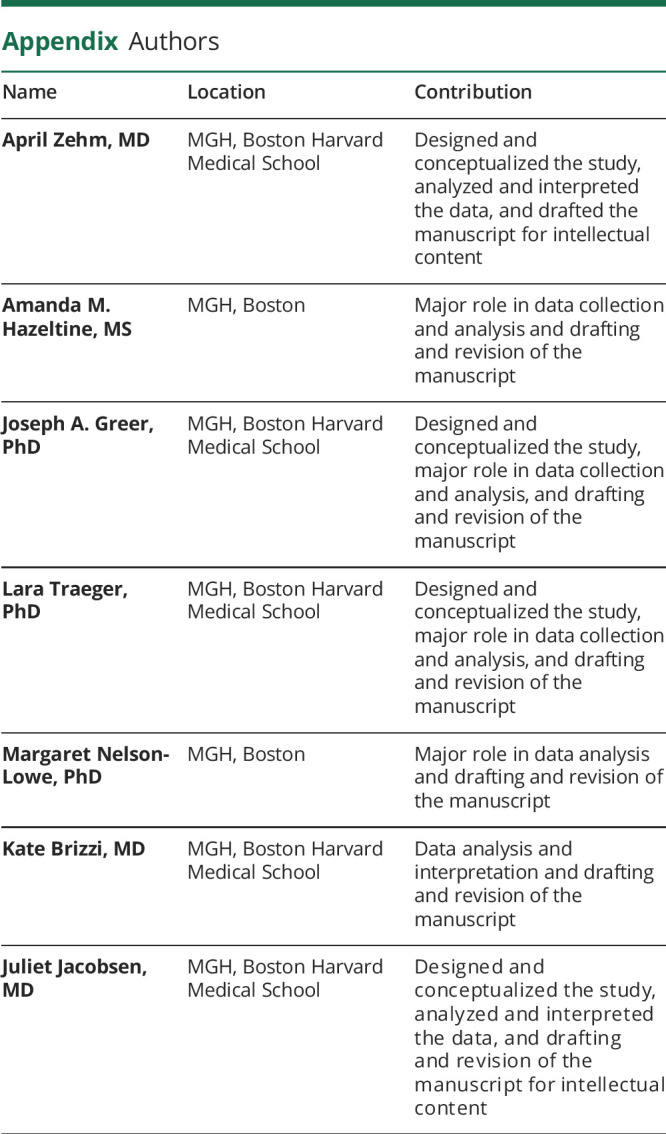
Appendix. Authors
Study funding
No targeted funding reported.
Disclosure
A. Zehm, A.M. Hazeltine, J.A. Greer, and L. Traeger report no disclosures relevant to the manuscript. M. Nelson-Lowe reports stock options in Praxis Precision Medicines. K. Brizzi and J. Jacobsen report no disclosures relevant to the manuscript. Full disclosure form information provided by the authors is available with the full text of this article at Neurology.org/cp.
References
- 1.Borasio GD, Voltz R. Palliative care in neurology. J Palliat Care 2005;21:188–189. [PubMed] [Google Scholar]
- 2.Boersma I, Miyasaki J, Kutner J, Kluger B. Palliative care and neurology: time for a paradigm shift. Neurology 2014;83:561–567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Foley KM, Carver AC. Palliative care in neurology. Neurol Clin 2001;19:789–799. [DOI] [PubMed] [Google Scholar]
- 4.Oliver DJ, Borasio GD, Caraceni A, et al. A consensus review on the development of palliative care for patients with chronic and progressive neurological disease. Eur J Neurol 2016;23:30–38. [DOI] [PubMed] [Google Scholar]
- 5.Palliative care in neurology. The American academy of neurology Ethics and humanities subcommittee. Neurology 1996;46:870–872. [PubMed] [Google Scholar]
- 6.World Health Organization. WHO definition of palliative care. Available at: who.int/cancer/palliative/definition/en/. Accessed March 18, 2019.
- 7.Center to Advance Palliative Care (CAPC). CAPC definition of palliative care. Available at: capc.org/about/palliative-care/. Accessed March 18, 2019.
- 8.Creutzfeldt CJ, Robinson MT, Holloway RG. Neurologists as primary palliative care providers: communication and practice approaches. Neurol Clin Pract 2016;6:40–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schuh LA, Adair JC, Drogan O, Kissela BM, Morgenlander JC, Corboy JR. Education research: neurology residency training in the new millennium. Neurology 2009;72:e15–e20. [DOI] [PubMed] [Google Scholar]
- 10.Creutzfeldt C, Gooley T, Walker M. Are neurology residents prepared to deal with dying patients? Arch Neurol 2009;66:1427–1428. [DOI] [PubMed] [Google Scholar]
- 11.Dallara A, Meret A, Saryan J. Mapping the literature: palliative care within adult and child neurology. J Child Neurol 2014;29:1728–1738. [DOI] [PubMed] [Google Scholar]
- 12.Harris J, Herrel L, Healy M, Wancata L, Perumalswami C. Milestones for the final mile: interspecialty distinctions in primary palliative care skills training. J Pain Symptom Manage 2016;52:345–352.e5. [DOI] [PubMed] [Google Scholar]
- 13.Carver AC, Vickrey BG, Bernat JL, Keran C, Ringel SP, Foley KM. End-of-life care: a survey of US neurologists' attitudes, behavior, and knowledge. Neurology 1999;53:284–293. [DOI] [PubMed] [Google Scholar]
- 14.Mehta A, Najjar S, May N, Shah B, Blackhall L. A needs assessments of palliative care education among the United States adult neurology resident programs. J Palliat Med 2018;21:1448–1457. [DOI] [PubMed] [Google Scholar]
- 15.Quill T, Abernethy A. Generalist plus specialist palliative care—creating a more sustainable model. N Engl J Med 2013;368:1173–1175. [DOI] [PubMed] [Google Scholar]
- 16.McCormick E, Chai E, Meier D. Integrating palliative care into primary care. Mt Sinai J Med 2012;79:579–585. [DOI] [PubMed] [Google Scholar]
- 17.Hussain J, Adams D, Allgar V, Campbell C. Triggers in advanced neurological conditions: prediction and management of the terminal phase. BMJ Support Palliat Care 2014;4:30–37. [DOI] [PubMed] [Google Scholar]
- 18.Mitsumoto H, Bromberg M, Johnston W, et al. Promoting excellence in end-of-life care in ALS. Amyotroph Lateral Scler Other Mot Neuron Disord 2005;6:145–154. [DOI] [PubMed] [Google Scholar]
- 19.Sudore RL. Preparing surrogates for complex decision making: the often neglected piece of the advance care planning equation. JAMA Intern Med 2019;179:268–269. [DOI] [PubMed] [Google Scholar]
- 20.Reinhardt JP, Chichin E, Posner L, Kassabian S. Vital conversations with family in the nursing home: preparation for end-stage dementia care. J Soc Work End Life Palliat Care 2014;10:112–126. [DOI] [PubMed] [Google Scholar]
- 21.Temel JS, Greer JA, Admane S, et al. Longitudinal perceptions of prognosis and goals of therapy in patients with metastatic non-small-cell lung cancer: results of a randomized study of early palliative care. J Clin Oncol 2011;29:2319–2326. [DOI] [PubMed] [Google Scholar]
- 22.Weeks J, Catalano P, Cronin M, et al. Patients' expectations about effects of chemotherapy for advanced cancer. N Engl J Med 2012;367:1616–1625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Turner-Stokes L, Sykes N, Silber E, Khatri A, Sutton L, Young E. From diagnosis to death: exploring the interface between neurology, rehabilitation and palliative care in managing people with long-term neurological conditions. Clin Med (Lond) 2007;7:129–136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bernacki R, Block S. American College of Physicians High Value Care Task Force. Communication about serious illness care goals: a review and synthesis of best practices. JAMA Intern Med 2014;174:1994–2003. [DOI] [PubMed] [Google Scholar]
- 25.Back A, Park E, Greer J, et al. Clinician roles in early integrated palliative care for patients with advanced cancer: a qualitative study. J Palliat Med 2014;17:1244–1248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sullivan A, Lakoma D, Billings J, Peters A, Block S; PCEP Core Faculty. Teaching and learning end-of-life care: evaluation of a faculty development program in palliative care. Acad Med 2005;80:657–668. [DOI] [PubMed] [Google Scholar]
- 27.Back AL, Arnold RM, Baile WF, et al. Faculty development to change the paradigm of communication skills teaching in oncology. J Clin Oncol 2009;27:1137–1141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rao JK, Anderson LA, Inui TS, Frankel RM. Communication interventions make a difference in conversations between physicians and patients: a systematic review of the evidence. Med Care 2007;45:340–349. [DOI] [PubMed] [Google Scholar]
- 29.Back AL, Arnold RM, Baile WF, et al. Efficacy of communication skills training for giving bad news and discussing transitions to palliative care. Arch Intern Med 2007;167:453–460. [DOI] [PubMed] [Google Scholar]
- 30.McConigley R, Aoun S, Kristjanson L, et al. Implementation and evaluation of an education program to guide palliative care for people with motor neurone disease. Palliat Med 2012;26:994–1000. [DOI] [PubMed] [Google Scholar]
- 31.Bernacki R, Paladino J, Neville B, et al. Effect of the serious illness care program in outpatient oncology: a cluster randomized clinical trial. JAMA Intern Med 2019;179:751–759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Paladino J, Bernacki R, Neville B, et al. Evaluating an intervention to improve communication between oncology clinicians and patients with life-limiting cancer: a cluster randomized clinical trial of the serious illness care program. JAMA Oncol 2019;5:801–809. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data in this manuscript cannot be shared for ethical reasons because it must remain protected per the Health Insurance Portability and Accountability Act per our consent process.



