Abstract
Background
Helicobacter pylori (H. pylori) eradication therapy has been shown to reduce the risk of gastric cancer in patients who have a family history of gastric cancer in first-degree relatives. The aim of this study was to assess the cost-effectiveness of H. pylori eradication therapy in a select population in the People's Republic of China.
Methods
A Markov model was applied to evaluate the cost-effectiveness of H. pylori eradication therapy. The long-term costs of H. pylori eradication therapy were calculated from the Chinese perspective. Health outcomes were measured by quality-adjusted life years (QALYs). Epidemiological information and health utilities used in the model were collected from published literatures or statistical bureaus. A sensitivity analysis was conducted to explore the influence of parameters on the uncertainty of the model.
Results
Compared with the no eradication therapy group, H. pylori eradication therapy prolonged an average of 4.52 QALYs (32.64 QALYs vs 28.12 QALYs) and saved $3227.07 ($2472.83 vs $5699.90). The cost-effectiveness analysis demonstrated that no H. pylori eradication therapy cost more and produced less QALYs. It was dominated by H. pylori eradication therapy. The one-way sensitive analyses proved that the results were robust to the fluctuations of the input parameters.
Conclusion
H. pylori eradication therapy not only reduced the risk of gastric cancer in first-degree relatives of patients with gastric cancer but also was an economical strategy with lower costs and greater efficacy.
Keywords: Helicobacter pylori, eradication therapy, gastric cancer, cost-effectiveness analysis
Introduction
Currently, cancer remains an important focus of public health, and gastric cancer is the third cause of cancer-related death.1 Helicobacter pylori (H. pylori) is a Gram-negative bacterium, which could colonize in the stomach leading to gastric cancer and gastric mucosa-associated lymphoid tissue lymphoma.2 As the most common infectious agent, H. pylori contributes to approximately 89% non-cardia gastric cancer in the world.3 The People's Republic of China is the most populous country in the world, with an approximately 56% prevalence of H. pylori infection, accounting for more than 40% of global gastric cancer-related deaths.4–6
Considering that H. pylori plays an important role in gastric cancer, eradication therapy for H. pylori infected patients is an effective measure to decrease the incidence of gastric cancer. The Kyoto global consensus report agreed that eradication therapy of H. pylori infection was a primary strategy for preventing gastric cancer, which could reduce the risk of gastric cancer.7 However, it is challenging to actively screen and treat all H. pylori-positive patients on a national scale in countries where H. pylori infection is highly prevalent in reality. In fact, the indication of H. pylori screening and eradication is influenced by clinical judgment and the patient’s condition. H. pylori-infected patients who can reap more benefits from H. pylori eradication therapy are recommended for treatment. Peptic ulcer (regardless of activity or complications), chronic gastritis with dyspepsia and family history of gastric cancer had been listed as H. pylori eradication indications in the Fifth Chinese National Consensus Report.8 Although the fact that individuals with a family history of gastric cancer had strong correlation to gastric cancer, not all consensus or guidelines recommended the relatives of gastric cancer patients to receive routine screening for H. pylori infection and eradication therapy due to insufficient evidence.9–11 Recently, a research in Korea demonstrated that H. pylori eradication therapy in H. pylori-infected patients who had a family history of gastric cancer in first-degree relatives reduced the risk of gastric cancer.12 In this research, 1,676 individuals were randomly assigned to two groups. Therein, 1.2% in the H. pylori eradication therapy group and 2.7% in the placebo group developed gastric cancer (hazard ratio, 0.45; 95% confidence interval, 0.21 to 0.94. P=0.03 by Log rank test).
Nevertheless, whether H. pylori eradication therapy is cost-effective is unknown in these populations. The following concern has been raised about its application. Adverse events including diarrhea and vomiting induced by H. pylori eradication therapy may have an impact on the quality of life. Costs of drugs, costs of screening for H. pylori also cause economic burden for these people. Another concern is that the heavy antibiotic consumption would worsen antibiotic resistance. On account of these factors, conducting a cost-effectiveness analysis to estimate H. pylori eradication is of great importance, especially in countries with high H. pylori prevalence. The aim of our research was to evaluate the cost-effectiveness of eradication therapy for H. pylori-infected patients who had a family history of gastric cancer in first-degree relatives from a healthcare payer perspective in the People's Republic of China.
Methods
Clinical Information
Clinical information was derived from a randomized trial performed in Korea.12 The eligibility criterion was H. pylori-positive persons older than 40 years who had at least a first-degree relative with gastric cancer. A total of 1,676 people were randomly divided into two groups: one received eradication therapy and the other received placebo therapy. Patients in both groups received endoscopic monitoring every 2 years. These two groups had no significant differences in age, sex or other basic characteristics at baseline. The status of H. pylori infection was evaluated based on a rapid urease test and Wright-Giemsa staining of biopsy specimens. After follow-up, H. pylori was eradicated in 551 of 786 patients in the treatment group. Participants who still had H. pylori infection received bismuth-based quadruple therapy (a proton-pump inhibitor, bismuth, metronidazole, and tetracycline) for 10 days after the trial ended. Gastric cancer was confirmed by the use of biopsy in 5 of 608 H. pylori-negative participants, and 28 of 979 H. pylori-positive participants.
Decision Model
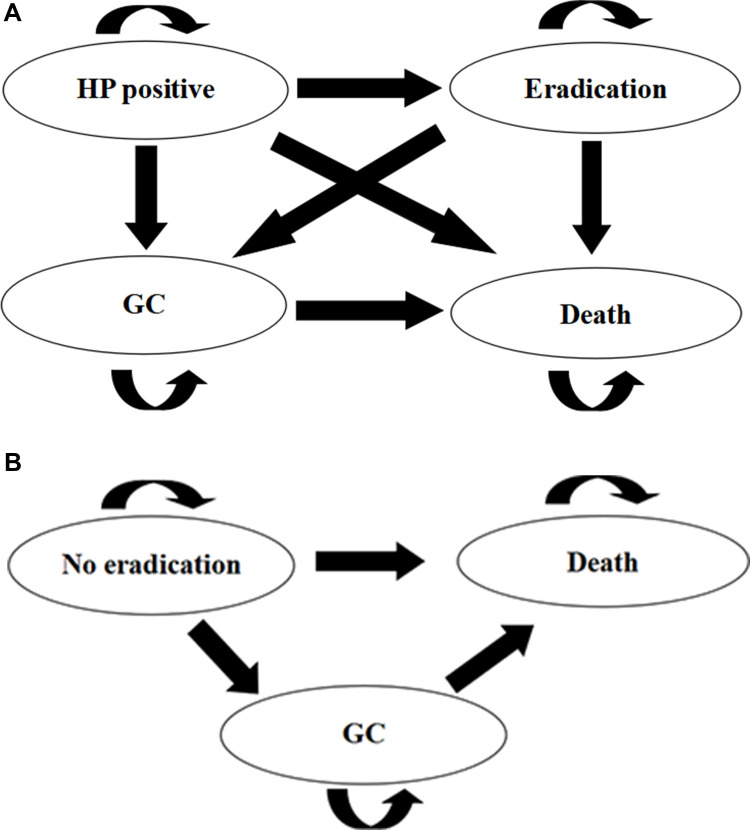
We used the TreeAge Pro (TreeAge Software, Williamstown, MA, USA) to construct a Markov model, which compared two treatment strategies: 1) subjects received eradication therapy (30 mg lansoprazole, 1000 mg amoxicillin, and 500 mg clarithromycin, each taken twice daily for 7 days); and 2) subjects received no therapy. The treatment group comprised four exclusive health states (H. pylori infection, H. pylori eradication, gastric cancer, dead) and the control group comprised three exclusive health states (H. pylori infection, gastric cancer, dead). These health states in the Markov model were applied to simulate the disease process of H. pylori-infected patients (Figure 1).
Figure 1.
The Markov model was used to compare two strategies comprising health states. (A) Eradication therapy group. (B) No eradication therapy group.
Abbreviations: HP, Helicobacter pylori; GC, gastric cancer.
Model Parameters
Transition probabilities were calculated by the formula: Probability=1-exp(-rt), where r is the incidence of event over time period t.13 The parameters in the model such as the eradication rate of H. pylori and the incidence of gastric cancer in first-degree relatives of patients with gastric cancer were derived from the clinical trial in South Korea.12 We ignored the recurrence rate after H. pylori eradication, because it was rare with an annual incidence of 1.75‰.14 The population mortality was obtained from the China Statistics Bureau and the mortality of gastric cancer was 22.5 per 100,000 people.5 Therefore, the mortality rate for non-gastric cancer was approximately 6.92‰. The 5-year survival rate of gastric cancer patients in the People's Republic of China was 35.9%.15 By using the following formula: P=Pt(1/t), the mortality rate of gastric cancer patients was about 19% per year. Details are shown in Table 1. The model cycle was 1 year. Based on the average life expectancy of 76.34 years in the People's Republic of China, the operation time of this model was set at 40 years.
Table 1.
Base Parameters in the Markov Model
| Parameters | Value | Source |
|---|---|---|
| Clinical variables | ||
| H. pylori prevalence rate | 56% | [2] |
| Incidence of gastric cancer in H. pylori-positive population (%) | 2.9% | [13] |
| Incidence of gastric cancer in H. pylori eradication population (%) | 0.8% | [13] |
| Success H. pylori eradication rate (%) | 70.10% | [13] |
| Population mortality (‰) | 7.14‰ | National Bureau of Statistics of China |
| Nongastric cancer mortality rate (‰) | 6.92‰ | |
| Five-year survival rate for gastric cancer (%) | 35.9% | [16] |
| Costs variables ($) | ||
| H. pylori eradication therapy | 77.83 | |
| Gastric cancer screening | 29.96 | |
| H. pylori testing | 81.85 | |
| AEs of eradication therapy | 1.99 | |
| Average annual gastric cancer treatment | 9891 | [17] |
| Health utility | ||
| After H. pylori eradication | 1 | |
| H. pylori infection | 0.89 | [18] |
| Gastric cancer | 0.38 | [18] |
Note: H. pylori, Helicobacter pylori.
Abbreviation: AE, adverse events.
Costs and Utilities
Only direct costs included were calculated. The costs of H. pylori eradication therapy, costs of endoscopy screening, costs of H. pylori testing, and costs of adverse events management were estimated based on the prices in Sichuan province, the People's Republic of China. Costs of gastric cancer treatment were derived from a multicenter cross-sectional survey.16 All costs were converted into US dollars and quality-adjusted life years (QALYs) were used to measure health outcomes. The discount of costs and QALYs was 3% each year. We assumed that the health utility of participants who successfully eradicated H. pylori was 1. The health utilities of patients with H. pylori infection and gastric cancer came from the published literature, and were 0.89 and 0.38, respectively.17
Sensitivity Analysis
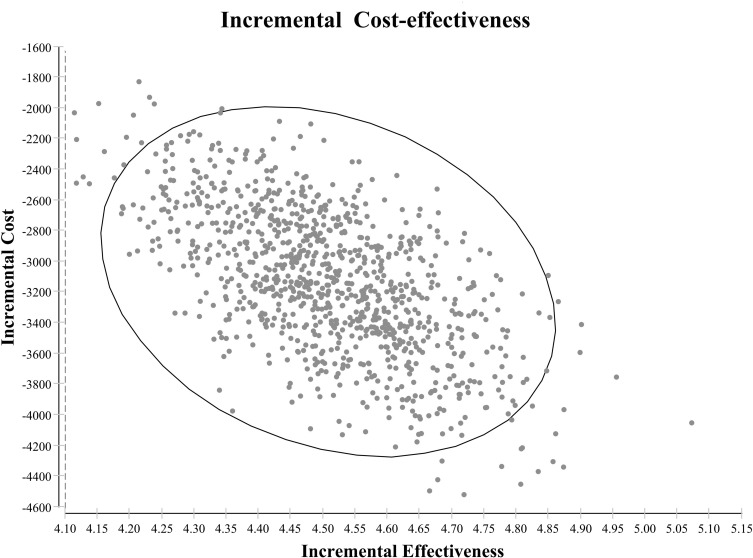
A sensitivity analysis was performed to explore the impact of parameters fluctuation on the robustness of the results. Probabilistic sensitivity analysis was conducted using the Monte Carlo simulation to iterate 1,000 times. The analysis results are shown by incremental cost-effect scatter plots.
Results
Base Case Analysis
The baseline results of our analysis are presented in Table 2. Within a 40-year time horizon, H. pylori eradication therapy in first-degree relatives of patients with gastric cancer yielded more benefits than no eradication therapy (32.64 QALYs vs 28.12 QALYs), leading to an extended 4.52 QALYs. It also yielded much lower costs than no eradication therapy ($2472.83 vs $5699.90). Therefore, incremental cost-effectiveness ratio (ICER) of H. pylori eradication therapy was $-713.95 per QALY compared to no eradication therapy, indicating that H. pylori eradication therapy was in the ascendant for having fewer costs and more benefits.
Table 2.
Results of Cost-Effectiveness Analysis
| Results | Cost ($) | Effectiveness (QALYs) | ICER ($/QALY) |
|---|---|---|---|
| Eradication group | 2472.83 | 32.64 | Dominant |
| Control group | 5699.90 | 28.12 |
Note: Dominant: more effective and less costly than others.
Abbreviations: QALYs, quality adjusted life-years; ICER, incremental cost-effectiveness ratio.
Sensitivity Analysis
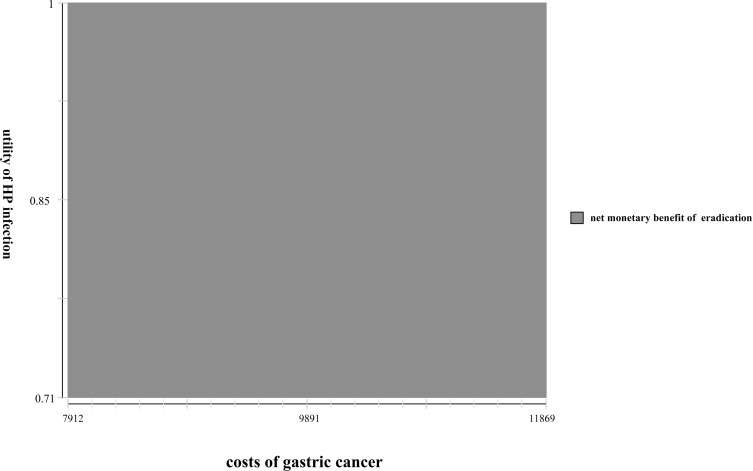
With 1,000 Monte Carlo simulations, the incremental cost-effectiveness scatterplots of eradication therapy and no eradication therapy are shown in Figure 2. The H. pylori eradication strategy cost less and generated more QALYs than no H. pylori eradication. As a result, no H. pylori eradication therapy was dominated by H. pylori eradication therapy. One-way sensitivity analyses of selected parameters are displayed in Table 3. The utility of H. pylori-infected people, the incidence of gastric cancer in the H. pylori-positive population, and the costs of gastric cancer treatment were the factors most affecting the results of the model. Although these parameters changed within the range of ± 20%, H. pylori eradication therapy produced more QALYs with lower costs, proving that H. pylori eradication therapy remains the dominant strategy. Additionally, we constructed a three-way sensitivity analysis on three parameters that had the greatest impact on the results. When the parameters were the most unfavorable for the implementation of the strategy, H. pylori eradication therapy still rendered net monetary benefit (Figure 3). The results were robust to the ranges of the variables.
Figure 2.
An incremental cost-effectiveness scatterplot comparing eradication therapy with no eradication therapy.
Table 3.
One-Way Sensitivity Analyses of Parameters
| Eradication Therapy | No Eradication Therapy | ||||
|---|---|---|---|---|---|
| Cost ($) | Effectiveness (QALYs) | Cost ($) | Effectiveness (QALYs) | ||
| Costs of gastric cancer treatment ($) | |||||
| 7912.80 | 2174.85 | 32.64 | 4760.89 | 28.12 | Dominated |
| 11,869.20 | 2770.81 | 32.64 | 6638.90 | 28.12 | Dominated |
| Costs of eradication therapy ($) | |||||
| 62.26 | 2472.47 | 32.64 | 5699.90 | 28.12 | Dominated |
| 93.40 | 2473.18 | 32.64 | 5699.90 | 28.12 | Dominated |
| Costs of H. pylori testing ($) | |||||
| 65.48 | 2472.46 | 32.64 | 5687.02 | 28.12 | Dominated |
| 98.23 | 2473.18 | 32.64 | 5699.90 | 28.12 | Dominated |
| Costs of gastric cancer screening ($) | |||||
| 23.97 | 2277.07 | 32.64 | 5511.85 | 28.12 | Dominated |
| 35.95 | 2668.58 | 32.64 | 5887.94 | 28.12 | Dominated |
| Costs of adverse events related to eradication therapy ($) | |||||
| 1.59 | 2472.79 | 32.64 | 5699.90 | 28.12 | Dominated |
| 2.39 | 2472.86 | 32.64 | 5699.90 | 28.12 | Dominated |
| Success H. pylori eradication rate | |||||
| 56.08% | 2513.66 | 32.58 | 5699.90 | 28.12 | Dominated |
| 84.12% | 2445.42 | 32.68 | 5699.90 | 28.12 | Dominated |
| Probability of developing gastric cancer in H. pylori-positive population | |||||
| 0.26% | 2428.77 | 32.67 | 4812.13 | 28.42 | Dominated |
| 0.38% | 2516.80 | 32.61 | 6569.05 | 27.83 | Dominated |
| Probability of developing gastric cancer in H. pylori eradication population | |||||
| 0.69‰ | 2226.78 | 32.73 | 5699.90 | 28.12 | Dominated |
| 1.04‰ | 2717.51 | 32.55 | 5699.90 | 28.12 | Dominated |
| Utility of H. pylori infection | |||||
| 0.71 | 2472.83 | 32.48 | 5699.90 | 22.53 | Dominated |
| 1 | 2472.83 | 32.74 | 5699.90 | 31.57 | Dominated |
| Utility of gastric cancer | |||||
| 0.30 | 2472.83 | 32.63 | 5699.90 | 28.08 | Dominated |
| 0.46 | 2472.83 | 32.65 | 5699.90 | 28.16 | Dominated |
Figure 3.
Sensitivity analysis on utility of HP-infected people and the costs of gastric cancer treatment when the probability of developing gastric cancer in the H. pylori-positive population was 0.26%.
Abbreviation: HP, Helicobacter pylori.
Discussion
Gastric cancer is one of the common malignant tumors, with a fatality rate of up to 75% in most regions of the world and it is a serious threat to public health.18 Of note, the highest fatality rates of gastric cancer are seen in Eastern Asia, especially in the People's Republic of China, Japan and Singapore.19 Risk factors of gastric cancer included H. pylori-infection, smoking, obesity, food habits and the environment.20 As the greatest risk factor for gastric cancer, the World Health Organization has classified H. pylori as a group I carcinogen.21,22 Another common risk factor of gastric cancer is a family history of gastric cancer. Several studies have found that a family history of gastric cancer patients significantly increased the incidence of gastric cancer, especially in first-degree relatives of patients.23 The familial clustering of gastric cancer attributed to the shared exposure to carcinogens, eating habits, and genetic susceptibility.24 Moreover, H. pylori infection and family history of gastric cancer had a synergistic effect on the development of gastric cancer.11 The incidence of gastric cancer can be reduced by the management high-risk gastric cancer population. A phase III clinical trial has proved that eradication of H. pylori reduced the risk of gastric cancer in first-degree relatives of patients with gastric cancer. Hence, the implementation of screening and eradication for H. pylori is a critical intervention to combat gastric cancer.
To the best of our knowledge, this is the first study to assess the economic influence of H. pylori eradication in first-degree relatives of patients with gastric cancer. In this study, we found that H. pylori eradication therapy for people who had at least one first-degree relative with gastric cancer resulted in an average of 4.52 longer QALYs (32.64 QALYs vs 28.12 QALYs) and the costs were reduced by $3,213.05 ($2,472.41 vs $5685.46). It was proved that H. pylori eradication therapy cost less and was more effective compared with no H. pylori eradication therapy in the People's Republic of China.
There have been several economic studies focused on H. pylori screening and eradication therapy in Asia. A cost-effectiveness analysis of Chinese in Singapore showed that among the Chinese population with a high incidence of gastric cancer, serology screening and eradication therapy were the dominant strategy compared to no screening.25 It was similar to our conclusion that we recommended H. pylori screening and eradication therapy for people who had first-degree family history of gastric cancer. Han et al17 performed a study to evaluate the cost-effectiveness of H. pylori screening and eradication therapy in the People's Republic of China, proving that H. pylori screening followed by eradication therapy was a cost-saving strategy. By this measure, it could save $168.45 per QALY per person. Kowada26 conducted decision trees to assess the cost-effectiveness of H. pylori screening followed by eradication therapy for employees aged 20, 30, 40, 50 and 60 years. Given that it gained more benefits with less costs than no screening, it could be popularized in Japan. Following this study, Kowada27 also found that people aged 50 years or older yielded more benefits in H. pylori screening than upper gastrointestinal series and endoscopy in high prevalence countries.
A recent consensus in the People's Republic of China announced that H. pylori eradication therapy was a cost-effective strategy in high-risk areas.28 The main reason for economic gains of H. pylori eradication therapy was that it reduced the incidence of gastric cancer, thereby reducing the total costs of gastric cancer. Nevertheless, in addition to the treatment costs, multiple factors including drug availability, and antibiotic resistance needs to be taken into consideration when carrying out a screen-and-treat program for H. pylori in the whole country, especially in countries with large populations and limited medical resources. Indeed, H. pylori has an increasing high primary resistance rate of clarithromycin, metronidazole, and levofloxacin in the People's Republic of China.29 The universal eradication treatment of H. pylori might increase serious antibiotic resistance and affect the application of antibacterial drugs in the future. In addition, the implementation of population-based screening would cause some intangible costs, such as human resources, publicity expenses of health authority. These obstacles have made H. pylori screening and treatment a complicated issue. Our results were similar to the situation described in the previous section and refined the detected population. At the same time, it was relatively easier to implement this program in first-degree relatives of patients with gastric cancer. Screening and eradication therapy of H. pylori infection in a high-risk gastric cancer population is relatively achievable from the perspective of health authorities.
Subjected to the insufficient data, several limitations existed in our analysis that deserve attention. Firstly, the eradication rate of H. pylori and the incidence of gastric cancer in first-degree relatives of patients with gastric cancer used in our study were derived from a single-center trial in Korea. Nevertheless, family history of gastric cancer was a global risk factor, so our results may be generally applicable.30 Secondly, the utility values of early gastric cancer and advanced gastric cancer may be different. Due to the lack of tumor staging for patients in this trial, we used an average utility of gastric cancer. Thirdly, regarding costs information, we only considered direct costs, neglecting the costs of lost working time and transportation fees. Additionally, the costs of rescue therapy for patients who failed first-line H. pylori therapy, secondary infection after antibiotic treatment and the daily expenses incurred by life extension were not calculated. As a result, the costs may be underestimated. However, they had little effect on the results according to the sensitivity analysis. Finally, the characteristics of the population in clinical trials may differ from the patients in clinical practice. Real world studies could be carried out in the future.
In summary, H. pylori eradication therapy significantly reduced the incidence of gastric cancer in first-degree relatives of patients with gastric cancer with economic benefits in the People's Republic of China. Based on our analysis, H. pylori eradication therapy is a dominant strategy. At present, in the People's Republic of China, where disease burden is heavy and economic resources are limited, eradication therapy is a cost-effective prevention strategy to prevent gastric cancer. The persistent H. pylori infection not only increased the risk of spreading among people, but also the risk of gastric cancer. It is worthy of being applied and promoted in clinical practice, especially in countries with high H. pylori prevalence.
Funding Statement
This study was funded by the National Natural Science Foundation of China (No. 81572988); Science & Technology Department of Sichuan Province Funding Project (2018SZ0117); the 1.3.5 Project for Disciplines of Excellence, West China Hospital, Sichuan University (ZYJC18008, ZYJC18010).
Ethics Approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424. doi: 10.3322/caac.21492 [DOI] [PubMed] [Google Scholar]
- 2.Maleki Kakelar H, Barzegari A, Dehghani J, et al. Pathogenicity of Helicobacter pylori in cancer development and impacts of vaccination. Gastric Cancer. 2019;22(1):23–36. doi: 10.1007/s10120-018-0867-1 [DOI] [PubMed] [Google Scholar]
- 3.Plummer M, Franceschi S, Vignat J, Forman D, de Martel C. Global burden of gastric cancer attributable to Helicobacter pylori. Int J Cancer. 2015;136(2):487–490. doi: 10.1002/ijc.28999 [DOI] [PubMed] [Google Scholar]
- 4.Feng R-M, Zong Y-N, Cao S-M, Xu R-H. Current cancer situation in China: good or bad news from the 2018 Global Cancer Statistics? Cancer Communications. 2019;39(1):22. doi: 10.1186/s40880-019-0368-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chen WQ, Zheng RS, Baade PD, et al. Cancer Statistics in China, 2015. CA: A Cancer Journal for Clinicians. 2016;66(2):115–132. doi: 10.3322/caac.21338 [DOI] [PubMed] [Google Scholar]
- 6.Wang F-H, Shen L, Li J, et al. The Chinese Society of Clinical Oncology (CSCO): clinical guidelines for the diagnosis and treatment of gastric cancer. Cancer Communications. 2019;39(1):10. doi: 10.1186/s40880-019-0349-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sugano K, Tack J, Kuipers EJ, et al. Kyoto global consensus report on Helicobacter pylori gastritis. Gut. 2015;64(9):1353–1367. doi: 10.1136/gutjnl-2015-309252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Liu WZ, Xie Y, Lu H, et al. Fifth Chinese National Consensus Report on the management of Helicobacter pylori infection. Helicobacter. 2018;23(2):e12475. doi: 10.1111/hel.12475 [DOI] [PubMed] [Google Scholar]
- 9.Chey WD, Leontiadis GI, Howden CW, Moss SF. ACG Clinical Guideline: treatment of Helicobacter pylori Infection. Am J Gastroenterol. 2017;112(2):212–239. doi: 10.1038/ajg.2016.563 [DOI] [PubMed] [Google Scholar]
- 10.El-Serag HB, Kao JY, Kanwal F, et al. Houston Consensus Conference on Testing for Helicobacter pylori Infection in the United States. Clin Gastroenterol Hepatol. 2018;16(7):992–1002. doi: 10.1016/j.cgh.2018.03.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Choi YJ, Kim N. Gastric cancer and family history. Korean J Intern Med. 2016;31(6):1042–1053. doi: 10.3904/kjim.2016.147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Choi IJ, Kim CG, Lee JY, et al. Family history of gastric cancer and Helicobacter pylori treatment. N Engl J Med. 2020;382(5):427–436. doi: 10.1056/NEJMoa1909666 [DOI] [PubMed] [Google Scholar]
- 13.Briggs A, Sculpher M. An introduction to Markov modelling for economic evaluation. Pharmacoeconomics. 1998;13(4):397–409. doi: 10.2165/00019053-199813040-00003 [DOI] [PubMed] [Google Scholar]
- 14.Xue Y, Zhou L-Y, Lu H-P, Liu J-Z. Recurrence of Helicobacter pylori infection: incidence and influential factors. Chin Med J. 2019;132(7):765–771. doi: 10.1097/CM9.0000000000000146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yang L, Zheng R, Wang N, et al. Incidence and mortality of stomach cancer in China, 2014. Chin J Cancer Res. 2018;30(3):291–298. doi: 10.21147/j.issn.1000-9604.2018.03.01 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Huang H-Y, Shi J-F, Guo L-W, et al. Expenditure and financial burden for common cancers in China: a hospital-based multicentre cross-sectional study. Lancet. 2016;388:10. doi: 10.1016/S0140-6736(16)31937-7 [DOI] [Google Scholar]
- 17.Han Y, Yan T, Ma H, et al. Cost-effectiveness analysis of Helicobacter pylori eradication therapy for prevention of gastric cancer: a Markov model. Dig Dis Sci. 2019;65(6):1679–1688. doi: 10.1007/s10620-019-05910-1 [DOI] [PubMed] [Google Scholar]
- 18.Fock KM. Review article: the epidemiology and prevention of gastric cancer. Aliment Pharmacol Ther. 2014;40(3):250–260. doi: 10.1111/apt.12814 [DOI] [PubMed] [Google Scholar]
- 19.Thrift AP, El-Serag HB. Burden of gastric cancer. Clin Gastroenterol Hepatol. 2020;18(3):534–542. doi: 10.1016/j.cgh.2019.07.045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Karimi P, Islami F, Anandasabapathy S, Freedman ND, Kamangar F. Gastric cancer: descriptive epidemiology, risk factors, screening, and prevention. Cancer Epidemiol Biomarkers Prev. 2014;23(5):700–713. doi: 10.1158/1055-9965.EPI-13-1057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Amieva M, Peek RM. Pathobiology of Helicobacter pylori–induced gastric cancer. Gastroenterology. 2016;150(1):64–78. doi: 10.1053/j.gastro.2015.09.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Blanchard TG, Czinn SJ. Identification of Helicobacter pylori and the evolution of an efficacious childhood vaccine to protect against gastritis and peptic ulcer disease. Pediatr Res. 2017;81(1–2):170–176. doi: 10.1038/pr.2016.199 [DOI] [PubMed] [Google Scholar]
- 23.Yusefi AR, Bagheri Lankarani K, Bastani P, Radinmanesh M, Kavosi Z. Risk factors for gastric cancer: a systematic review. Asian Pac J Cancer Prev. 2018;19(3):591–603. doi: 10.22034/APJCP.2018.19.3.591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yu GQ, Hu N, Wang LM, et al. Gastric microbiota features associated with cancer risk factors and clinical outcomes: A pilot study in gastric cardia cancer patients from Shanxi, China. Int J Cancer. 2017;141(1):45–51. doi: 10.1002/ijc.30700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Xie F, Luo N, Blackhouse G, Goeree R, Lee H-P. Cost-effectiveness analysis of Helicobacter pylori screening in prevention of gastric cancer in Chinese. Int J Technol Assess Health Care. 2008;24(1):87–95. doi: 10.1017/S0266462307080117 [DOI] [PubMed] [Google Scholar]
- 26.Kowada A. Cost-effectiveness of Helicobacter pylori screening followed by eradication treatment for employees in Japan. Epidemiol Infect. 2018;146(14):1834–1840. doi: 10.1017/S095026881800208X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kowada A. Cost-effectiveness of Helicobacter pylori test and eradication versus upper gastrointestinal series versus endoscopy for gastric cancer mortality and outcomes in high prevalence countries. Scand J Gastroenterol. 2019;54(6):685–689. doi: 10.1080/00365521.2019.1627408 [DOI] [PubMed] [Google Scholar]
- 28.Du Y, Zhu H, Liu J, et al. Consensus on eradication of Helicobacter pylori and prevention and control of gastric cancer in China (2019, Shanghai). J Gastroenterol Hepatol. 2020;35(4):624–629. doi: 10.1111/jgh.14947 [DOI] [PubMed] [Google Scholar]
- 29.Hu Y, Zhu Y, Lu N-H. Primary antibiotic resistance of Helicobacter pylori in China. Dig Dis Sci. 2017;62(5):1146–1154. doi: 10.1007/s10620-017-4536-8 [DOI] [PubMed] [Google Scholar]
- 30.Yaghoobi M, McNabb-Baltar J, Bijarchi R, Hunt RH. What is the quantitative risk of gastric cancer in the first-degree relatives of patients? A meta-analysis. World J Gastroenterology. 2017;23(13):2435–2442. doi: 10.3748/wjg.v23.i13.2435 [DOI] [PMC free article] [PubMed] [Google Scholar]