Abstract
Antiresorptive agent-related osteonecrosis of the jaw (ARONJ) causes severe pain that cannot be controlled well by common analgesic drugs. This is a first case report of intractable mandibular pain due to ARONJ that was eliminated by a continuous mandibular nerve block. A 72-year-old woman with osteoporosis had been administered bisphosphonate. One year after extraction of her tooth, she was diagnosed as having ARONJ. Jaw pain was so severe that she was unable to open her mouth and eat. We performed a continuous mandibular nerve block through an indwelling catheter with levobupivacaine for pain management. After the procedure, her rest pain was markedly improved, and the pain induced by opening her mouth disappeared. We conclude that a continuous mandibular nerve block may be helpful in the management of ARONJ.
Keywords: Pain management, Antiresorptive agent-related osteonecrosis of the jaw, Bisphosphonate, Continuous mandibular nerve block
INTRODUCTION
Antiresorptive agent-related osteonecrosis of the jaw (ARONJ) is rare [1], but it sometimes causes severe pain that cannot be controlled well by common analgesic drugs. Control of pain is listed as one of the major goals of treatment for ARONJ [7]. However, there is no detailed description of pain relief [7]. We report a case in which a continuous mandibular nerve block was effective for the management of intractable mandibular pain associated with ARONJ.
CLINICAL CASE
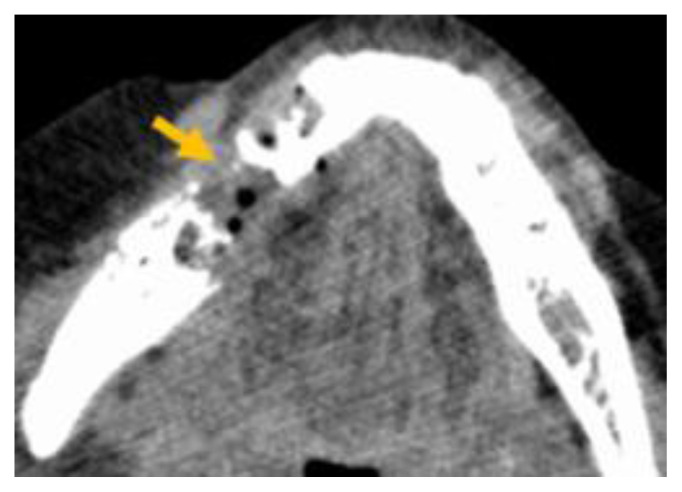
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A 72-year-old woman with osteoporosis had been administered bisphosphonate. Right lower jaw pain and sensory paralysis appeared one year after extraction of her right lower second premolar. After that, osteonecrosis progressed in the same region, and she was diagnosed as having ARONJ. Her right lower jaw pain gradually worsened, and she was unable to open her mouth and eat. The patient was hospitalized, and her maximum mouth opening was about 1.5 cm at admission. Bone exposure and small amount of pus discharge were observed around the tooth extraction socket (Figure 1). Rest pain was severe as expressed in the numerical rating scale (NRS) of 10/10, and more intense pain was induced by touching the right lower jaw region. A panoramic radiograph showed a tooth defect and osteolysis of the right lower jaw (Figure 2), and a computed tomography (CT) scan revealed bone destruction extending to the lower edge of the mandible (Figure 3).
Figure 1. Photo of the oral cavity.

Orange arrow: mandibular bone exposure.
Black arrow: small amount of pus discharge.
Figure 2. Panoramic tomography X-ray.
Image of a tooth defect and osteolysis in the right lower jaw.
Figure 3. Computed tomography of the lower jaw.
Orange arrow: bone destruction.
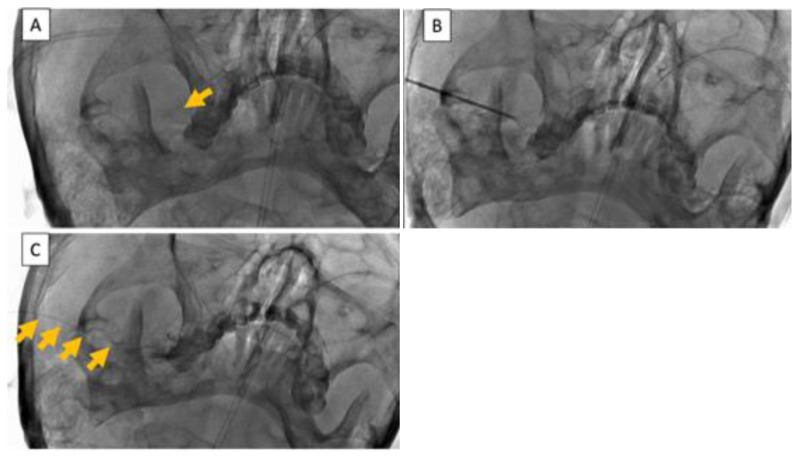
Surgery was planned to excise the necrosis of the jawbone; however, it was impossible to perform immediately because her systemic condition had dramatically worsened. First, enteral nutrition was started. As medical treatment, ampicillin/sulbactam at 3.0 g, acetaminophen at 2.4 g, and pregabalin at 50 mg were administered daily. Sixty mg of loxoprofen sodium was added when she felt a surge of pain. She rated the pain score as 7/10 on NRS; therefore, we judged that these medical treatments had no effect. Oral care could still not be performed because of severe jaw pain. Then she was referred to our pain clinic. Gasserian ganglion block or mandibular nerve block was considered to relieve her right lower jaw pain. The former puncture site is near the corner of the mouth, and the latter is in front of the earlobe. In this case, the Gasserian ganglion block was not selected because the site of infection was near the corner of the mouth. Thus, we performed a mandibular nerve block using the landmark method (via a lateral extraoral approach), and 4 ml of 0.75 % ropivacaine was injected with a 24-gauge 32 mm needle. After the procedure, rest pain completely disappeared and NRS was measured at 0/10. Despite subsequent continuous intravenous infusion of fentanyl (15 μg/hr), severe pain reappeared and persisted. Because the mandibular nerve block was sufficient to control the pain, we decided to treat her with a continuous mandibular nerve block using an indwelling catheter. The procedure was performed with the patient in the supine position under fluoroscopic guidance. Her face was turned to the left side, and a pillow was put under her shoulder so that her neck was bent backwards. An oblique image of the foramen ovale could be obtained when the fluoroscope was inclined caudally about 30° (Figure 4A). We adjusted the fluoroscope so that the foramen ovale could be seen on the anterior pyramidal ridge between the lateral maxillary sinus plate and the medial coronid process of the mandible. After skin disinfection, 1 % mepivacaine was injected below the zygomatic arch (2.5 cm in front of the tragus) for local anesthesia. Then an 18-gauge Tuohy needle was advanced toward the outer edge of the foramen ovale. After making contact with the skull base, the needle was directed closer to the foramen ovale until radiating pain was elicited in the mandible region (Figure 4B). The stylet was removed, and the indwelling catheter was inserted and advanced 1 cm from the tip of the needle (Figure 4C). The patient reported reduction in pain within a few minutes after administration of the initial bolus of 4 ml of 1 % mepivacaine through the catheter, allowing her mouth to open. NRS was measured at 0/10. We were able to touch her mandible and the inside of her oral cavity without her reporting pain.
Figure 4. X-ray image during the procedure.
A) Orange arrow: oblique image of the foramen ovale.
B) An 18G needle was placed closer to the foramen ovale.
C) Orange arrows: the catheter was indwelled.
Since a bolus dose of 4 ml of 0.5 % levobupivacaine was effective for only about 4 hours, a continuous mandibular nerve block with 0.25 % levobupivacaine at 2 ml/h was started using a patient-controlled analgesia (PCA) pump (bolus dose: 3 ml, lock out time: 60 min). After using the PCA, her rest pain was markedly improved, and the pain induced by opening her mouth or receiving oral care disappeared. At 33 days after admission, surgery including segmental resection of the right lower jawbone, right submandibular gland excision and tracheotomy was performed. There were no complications and the patient was discharged on the 40th day after surgery.
DISCUSSION
We described a case in which a continuous mandibular nerve block was successfully used for the management of intractable mandibular pain associated with ARONJ.
In the Position Paper 2014 Update of the American Association of Oral and Maxillofacial Surgeons, the major goals of treatment for preservation of the patient’s quality of life (QOL) are to eliminate pain, control infection, and minimize the progression or occurrence of bone necrosis [7]. Although pain relief is vitally important for performing oral care, there is no detailed description in that Position Paper of how to achieve analgesia. There are only three reports of pain treatment for ARONJ other than surgical treatment. One is a report of radiofrequency thermocoagulation of the Gasserian ganglion [10], and the others are reports of laser therapy [6,12]. There are four reports of pain management using a continuous mandibular nerve block: Umino et al. applied the method to a patient with trigeminal neuralgia [11], Kohase et al. used the method for cancer pain [3], and others used the method for perioperative analgesia [4,8]. Hence, this is the first report of a continuous mandibular nerve block for pain due to ARONJ.
Mandibular nerve block has been used for pain control in the mandibular region. In general, a local anesthetic is injected as a bolus. When its analgesic effect has been confirmed, a neuro-destructive procedure using radiofrequency thermocoagulation or alcohol is considered. A neuro-destructive procedure causes semi-permanent sensory loss and muscle weakness in the mandibular region [10], while a continuous mandibular nerve block with local anesthetics provides temporary and reversible effects. In this case, intense pain was accompanied by infection. If nerve destruction is required, more severe destruction is needed, resulting in increased risk of developing hyperalgesia [9]. Continuous mandibular nerve block may be useful in the management of pain for the following patients: (1) patients in whom it is not necessary to resect the jaw bone due to an early stage of ARONJ but in whom it is difficult to achieve relief from pain using acetaminophen, non-steroidal anti-inflammatory drugs, or an opioid and (2) the patients who refuse to undergo neuro-destruction.
There are two reports of the landmark method (lateral extra-oral approach) being used in the mandibular region for surgical patients [4,8]. In our patient, an indwelling catheter was inserted under fluoroscopic control in order to prevent procedural adverse events such as hemorrhagic complication, infection, and accidental auditory canal puncture.
In past studies, 0.5 ml/hr of 0.25 % bupivacaine was effective for pain relief [2,3]. In our patient, however, 2.0 ml/hr of 0.25 % bupivacaine was needed. As the reason for this variation, we considered that the indwelling catheter somewhat separately placed from the nerve. There is no evidence for the safe duration of indwelling catheter. The longest infusion of 88 consecutive days have been reported [5], but the incidence of catheter infection increases with the duration of indwelling catheter in general. Thus, we think the catheter placement period should be as short as possible.
In our patient, a continuous mandibular nerve block could provide adequate analgesia for intractable pain from ARONJ. We conclude that this nerve block may be a choice in the management of intractable mandibular pain associated with ARONJ.
ACKNOWLEDGEMENTS
None of the authors has any conflicts of interest or any financial ties to disclose.
REFERENCES
- 1.Khan AA, Morrison A, Hanley DA, Felsenberg D, McCauley LK, O'Ryan F, Reid IR, Ruggiero SL, Taguchi A, Tetradis S, Watts NB, Brandi ML, Peters E, Guise T, Eastell R, Cheung AM, Morin SN, Masri B, Cooper C, Morgan SL, Obermayer-Pietsch B, Langdahl BL, Al Dabagh R, Davison KS, Kendler DL, Sandor GK, Josse RG, Bhandari M, El Rabbany M, Pierroz DD, Sulimani R, Saunders DP, Brown JP, Compston J International Task Force on Osteonecrosis of the Jaw. Diagnosis and management of osteonecrosis of the jaw: a systematic review and international consensus. J Bone Miner Res. 2015;30:3–23. doi: 10.1002/jbmr.2405. [DOI] [PubMed] [Google Scholar]
- 2.Kohase H, Miyamoto T, Umino M. A new method of continuous maxillary nerve block with an indwelling catheter. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology. 2002;94:162–66. doi: 10.1067/moe.2002.124857. [DOI] [PubMed] [Google Scholar]
- 3.Kohase H, Umino M, Shibaji T, Suzuki N. Application of a mandibular nerve block using an indwelling catheter for intractable cancer pain. Acta Anaesthesiol Scand. 2004;48:382–3. doi: 10.1111/j.0001-5172.2004.0316.x. [DOI] [PubMed] [Google Scholar]
- 4.Kumar A, Banerjee A. Continuous maxillary and mandibular nerve block for perioperative pain relief: the excision of a complicated pleomorphic adenoma. Anesth Analg. 2005;101:1531–2. doi: 10.1213/01.ANE.0000181332.74791.FC. [DOI] [PubMed] [Google Scholar]
- 5.Pacenta HL, Kaddoum RN, Pereiras LA, Chidiac EJ, Burgoyne LL. Continuous tunnelled femoral nerve block for palliative care of a patient with metastatic osteosarcoma. Anaesth Intensive Care. 2010;38:563–5. doi: 10.1177/0310057X1003800324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Romeo U, Galanakis A, Marias C, Vecchio AD, Tenore G, Palaia G, Vescovi P, Polimeni A. Observation of pain control in patients with bisphosphonate-induced osteonecrosis using low level laser therapy: preliminary results. Photomed Laser Surg. 2011;29:447–52. doi: 10.1089/pho.2010.2835. [DOI] [PubMed] [Google Scholar]
- 7.Ruggiero SL, Dodson TB, Fantasia J, Goodday R, Aghaloo T, Mehrotra B, O’Ryan F American Association of Oral Maxillofacial Surgeons. American Association of Oral and Maxillofacial Surgeons position paper on medication-related osteonecrosis of the jaw--2014 update. J Oral Maxillofac Surg. 2014;72:1938–56. doi: 10.1016/j.joms.2014.04.031. [DOI] [PubMed] [Google Scholar]
- 8.Singh B, Bhardwaj V. Continuous mandibular nerve block for pain relief. A report of two cases. Can J Anaesth. 2002;49:951–3. doi: 10.1007/BF03016881. [DOI] [PubMed] [Google Scholar]
- 9.Taha JM, Tew JM, Jr, Buncher CR. A prospective 15-year follow up of 154 consecutive patients with trigeminal neuralgia treated by percutaneous stereotactic radiofrequency thermal rhizotomy. J Neurosurg. 1995;83:989–93. doi: 10.3171/jns.1995.83.6.0989. [DOI] [PubMed] [Google Scholar]
- 10.Taniguchi A, Fukazawa K, Hosokawa T. Selective Percutaneous Controlled Radiofrequency Thermocoagulation of the Gasserian Ganglion To Control Facial Pain Due to Medication-Related Osteonecrosis of the Jaw. J Palliat Med. 2017;20:1171–74. doi: 10.1089/jpm.2017.0153. [DOI] [PubMed] [Google Scholar]
- 11.Umino M, Kohase H, Ideguchi S, Sakurai N. Long-term pain control in trigeminal neuralgia with local anesthetics using an indwelling catheter in the mandibular nerve. Clin J Pain. 2002;18:196–9. doi: 10.1097/00002508-200205000-00010. [DOI] [PubMed] [Google Scholar]
- 12.Weber JB, Camilotti RS, Ponte ME. Efficacy of laser therapy in the management of bisphosphonate-related osteonecrosis of the jaw (BRONJ): a systematic review. Lasers Med Sci. 2016;31:1261–72. doi: 10.1007/s10103-016-1929-4. [DOI] [PubMed] [Google Scholar]