Supplemental Digital Content is available in the text
Keywords: late tracheotomy, mechanical ventilation, meta-analysis, randomized controlled trials, unselected intensive care unit patients
Abstract
Background:
This study aimed to quantitatively analyze the available randomized controlled trials (RCTs) and investigate whether early tracheotomy can improve clinical endpoints compared with late tracheotomy in critically ill patients undergoing mechanical ventilation.
Methods:
The electronic databases of PubMed, Embase, and the Cochrane library were systematically searched in August 2019. The investigated outcomes were calculated using relative risks (RRs) and standardized mean differences (SMDs) with corresponding 95% confidence intervals (CIs) through the random-effects model for categories and continuous data, respectively.
Results:
The electronic searches yielded 2289 records, including 15 RCTs comprising a total of 3003 patients and found to be relevant for the final quantitative analysis. The summary RRs that indicated early versus late tracheotomy were not associated with the risk of short-term mortality (RR: 0.87; 95% CI: 0.74–1.03; P = .114) and ventilator-associated pneumonia (RR: 0.90; 95% CI: 0.78–1.04; P = .156). Moreover, early tracheotomy was associated with shorter intensive care unit (ICU) stay (SMD: –1.81; 95% CI: –2.64 to –0.99; P < .001) and mechanical ventilation duration (SMD: –1.17; 95% CI: –2.10 to –0.24; P = .014). Finally, no significant difference was observed between early and late tracheotomy for hospital stay (SMD: –0.42; 95% CI: –1.36–0.52; P = .377).
Conclusions:
The present meta-analysis suggests that early tracheotomy can reduce the length of ICU stay and mechanical ventilation duration, but the timing of the tracheotomy was not associated with the short-term clinical endpoints in critically ill patients undergoing mechanical ventilation.
1. Introduction
Tracheotomy is a frequently performed surgical procedure in critically ill patients, that is, patients admitted to the intensive care unit (ICU) and requiring prolonged mechanical ventilation or airway protection due to coma, asphyxia, respiratory muscular paralysis, and hypoxia.[1–3] Studies have already shown the advantages of tracheotomy compared with endotracheal intubation, including shorter ICU or hospital stay, lowered airway resistance, improved pulmonary toilet and fewer lung infections, protection for direct laryngeal injury, facilitated nursing care, improved patient comfort, and benefits for oral feeding, which are associated with the administration of smaller amounts of sedative.[4–6] Nevertheless, the risks of tracheotomy include bleeding, wound infection, tracheal stenosis, and, occasionally, death.[7,8]
The timing for tracheotomy in critically ill patients undergoing mechanical ventilation is an important question regarding the clinical outcomes. Tracheotomy should be used when the duration of mechanical ventilation exceeds 14 days.[9] Another recommendation is that the patient should be endotracheally intubated within 10 days, and tracheotomy should be performed if the duration of mechanical ventilation is predicted to be exceeding 21 days.[10] However, the optimal timing for tracheotomy in critically ill patients undergoing mechanical ventilation remains uncertain.
Numerous studies investigated the efficacy and safety of early versus late tracheotomy for critically ill patients undergoing mechanical ventilation. However, conflicting results were obtained, and hence clinicians have difficulty in making decisions. Several systematic reviews and meta-analyses explored the effects of early versus late tracheotomy on critically ill patients undergoing mechanical ventilation. One of them indicates that early tracheotomy is not associated with short-better outcomes in critically ill patients.[11] Two meta-analyses showed that early tracheotomy is associated with shorter ICU stay, shorter mechanical ventilation duration, and lower risk of mortality, but without impact on hospital-acquired pneumonia,[12,13] while yet another meta-analysis showed that the only improved outcome is short-term mortality.[14] Meng et al[15] reported that early tracheotomy might be able to reduce the duration of sedation but did not significantly alter the mortality or complications. Nevertheless, the previous meta-analysis based on RCTs did not include stratified analyses according to patient characteristics. In addition, some of those meta-analyses date from a few years, and novel RCTs were published since then.
Therefore, the present updated meta-analysis of RCTs was conducted to systematically compare the treatment efficacy of early tracheotomy versus late tracheotomy in critically ill patients undergoing mechanical ventilation.
2. Methods
2.1. Data sources, search strategy, and selection criteria
This study was carried out following the Preferred Reporting Items for Systematic Reviews and Meta-Analysis Statement issued in 2009.[16] The following databases were systematically searched through August 2019 on PubMed, Embase, and the Cochrane library, and “tracheotomy” OR “tracheostomy” OR “intratracheal intubation” AND (“mechanical ventilation” OR “artificial respiration”) AND “randomized controlled trials” were used as keywords. The ongoing trials were also searched from the website http://clinicaltrials.gov/ (US NIH) and the metaRegister of Controlled Trials to identify studies already completed but yet not published. Furthermore, the reference lists of retrieved studies were reviewed to identify other potential studies of interest.
The literature search and study selection were carried out by 2 independent authors, and discrepancies between the 2 authors were resolved by a third author. The inclusion criteria were: population: critically ill patients who received mechanical ventilation; intervention: early tracheotomy; control: late tracheotomy; outcomes: short-term mortality, ventilator-associated pneumonia, ICU stay, mechanical ventilation duration, and hospital stay; and study design: RCT.
2.2. Data collection and quality assessment
The data were extracted following a standardized form independently by 2 authors, and any inconsistencies between the authors were settled by group discussion or consulting the corresponding author. The collected information included the first authors’ surname, publication year, country, setting, sample size, age, percentage of male patients, disease severity, tracheotomy methods, timing of early and late tracheotomy, and reported outcomes. Early and late tracheotomies were based on the definition of each individual study. The quality of each included study was assessed using the Jadad scale for randomization, blinding, allocation concealment, withdrawals and dropouts, and the use of intention-to-treat analysis.[17] Each item was allocated 1 or 0 scores for each of the included studies, and the scoring system ranged from 0 to 5. The quality assessment was carried out independently by 2 authors, and any disagreement was settled by an additional author reviewing the original study.
2.3. Statistical analysis
The outcomes of early versus late tracheotomy were segregated as categorical and continuous data. Relative risks (RRs) or standardized mean differences (SMDs) with corresponding 95% confidence intervals (CIs) were calculated in an individual trial before data pooling. The pooled analyses for all reported outcomes were calculated using the random-effects model.[18,19] The heterogeneity across included trials was assessed using I2 and Q statistic, and I2 > 50.0% or P < .10 was considered as significant heterogeneity.[20,21] The robustness of pooled results was assessed using the sensitivity analysis by sequentially excluding individual trials.[22] Subgroup analyses for short-term mortality and ventilator-associated pneumonia were conducted based on country, sample size, mean age, percentage of male patients, tracheotomy methods, and study quality. The differences between subgroups were calculated using the interaction P-value, which was based on the t test due to the smaller number of included studies.[23] Publication biases for short-term mortality and ventilator-associated pneumonia were also evaluated using the funnel plots and Egger and Begg test results.[24,25] The P-value for pooled results was 2-sided, and the inspection level was .05. Stata software (Version 10.0; StataCorp, TX) was employed for all statistical analyses.
2.4. Ethical statement
As this meta-analysis was based on previously published studies, ethical approval was not necessary.
3. Results
3.1. Literature search
The details of the literature search and study selection processes are shown in Fig. 1. The initial electronic databases yielded 2289 records; 538 studies were excluded because of duplication. A total of 69 studies were retrieved for full-text evaluations after irrelevant topics were excluded. After this, 54 studies were excluded because of the following reasons: no appropriate control (n = 21); not RCT (n = 17); and review or meta-analysis (n = 16). The manual search of the reference lists of these studies did not yield any new eligible study, and all of these studies were contained in the initial electronic searches. Finally, 15 RCTs comprising a total of 3003 patients were selected for the final meta-analysis.[26–40]
Figure 1.
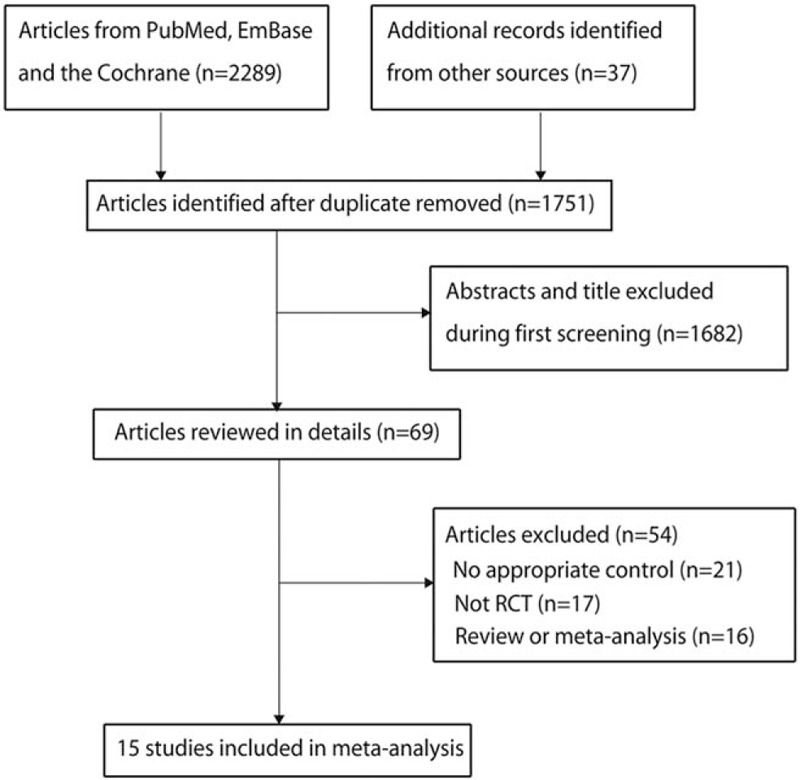
Flow diagram for the study selection process.
3.2. Study characteristics
The baseline characteristics of the included studies are summarized in Table 1. Of 15 included studies, 6 were conducted in the United States, and the remaining 9 studies were conducted in Morocco, France, Italy, Germany, UK, Spain, and China. The mean age of the included patients ranges from 37.6 to 67.7 years, and 44 to 899 patients were included in each individual trial. Four of the included trials used open tracheotomy, 7 used percutaneous tracheotomy, 2 used both methods, and the remaining 2 did not report the tracheotomy method. The study quality was assessed using the Jadad scale; 3 trials had a score of 5, 6 a score of 4, 4 a score of 3, 1 a score of 2, and the remaining a score of 1.
Table 1.
Baseline characteristic of studies included in the systematic review and meta-analysis.
| Study | Country | Setting | Sample size | Age, y | Percentage of male patients (%) | Disease severity | Tracheotomy methods | Early tracheotomy | Later tracheotomy | Jadad scale |
| Dunham 1984[26] | US | Trauma | 74 | 17.0–75.0 | NA | NA | Open | 4 days | 14 days | 2 |
| Rodriguez 1990[27] | US | Trauma | 106 | 37.6 | 79.2 | ISS: 28/27; GCS: 10/10 | NA | 1–7 days | >8 days | 1 |
| Sugerman 1997[28] | US | Mixed | 112 | NA | NA | NA | Both | 5 days | 14 days | 3 |
| Saffle 2002[29] | US | Burn | 44 | 48.0 | NA | NA | Open | 4 days | 14 days | 4 |
| Bouderka 2004[30] | Morocco | Head injury | 62 | 40.6 | 61.3 | SAPS score: 5.4/6.0 | NA | 5–6 days | Prolonged endotracheal intubation | 4 |
| Rumbak 2004[31] | US | Medical | 120 | 63.0 | 54.2 | APACHE II score: 27.4/26.3 | Percutaneous | 2 days | 14 days | 3 |
| Barquist 2006[32] | US | Trauma | 60 | 51.7 | 76.7 | APACHE II score: 12.1/13.1 | Open | 8 days | 28 days | 4 |
| Blot 2008[33] | France | Medical | 123 | 56.5 | 71.5 | SAPS II score: 50/50 | Open | 4 days | 14 days | 5 |
| Terragni 2010[34] | Italy | Mixed | 419 | 61.5 | 66.8 | SAPS II score: 51.1/49.7 | Percutaneous | 8 days | 15 days | 5 |
| Trouillet 2011[35] | France | After cardiac surgery | 216 | 65.0 | 66.2 | SAPS II score: 47.2/45.8 | Percutaneous | 5 days | 15 days | 5 |
| Koch 2012[36] | Germany | Neurosurgery or neurotrauma | 100 | 58.8 | 64.0 | APACHE II score: 21.0/22.0 | Percutaneous | 4 days | 6 days | 4 |
| Zheng 2012[37] | China | Medical | 119 | 67.7 | 62.2 | APACHE II score: 19.6/19.6 | Percutaneous | 3 days | 15 days | 3 |
| Bösel 2013[38] | Germany | Neurological illness, neurosurgery, or neurotrauma | 60 | 61.0 | 66.7 | APACHE score: 16.0/17.0 | Percutaneous | 3 days | 7 days | 4 |
| Young 2013[39] | UK | Mixed | 899 | 63.9 | 58.6 | APACHE II score: 19.6/20.1 | Both | 4 days | 10 days | 4 |
| Diaz-Prieto 2014[40] | Spain | Mixed | 489 | 64.7 | 67.3 | APACHE II score: 20.0/19.0 | Percutaneous | 8 days | 14 days | 3 |
3.3. Short-term mortality
The data for the effect of early versus late tracheotomy on the risk of short-term mortality were available in 14 trials. The summary RR indicated no significant difference between the effect of early and late tracheotomy on the risk of short-term mortality (RR: 0.87; 95% CI: 0.74–1.03; P = .114; Fig. 2), and no potential significant heterogeneity among included trials (I2 = 35.9%; P = .088). This conclusion was stable and not changed by sequentially excluding individual trials (Supplemental Digital Content [Figure S1]). The subgroup analyses suggested that early versus late tracheotomy might exert beneficial effects on the risk of short-term mortality if the trials were conducted in the United States (sample size ≥100, mean age ≥60.0 years, and patients used percutaneous tracheotomy, but with no statistically significant difference) (Table 2). Moreover, the interaction P test indicated that the country might affect the treatment effect of early and late tracheotomy on the risk of short-term mortality (P = .044).
Figure 2.
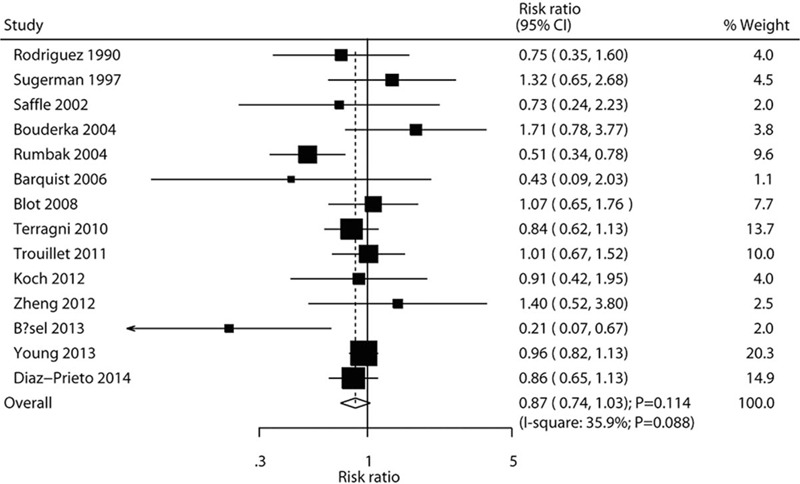
Effects of early versus late tracheotomy on the risk of short-term mortality.
Table 2.
Subgroup analyses for short-term mortality.
| Factors | Subgroup | RR and 95% CI | P-value | Heterogeneity (%) | P-value for heterogeneity | P-value between subgroups |
| Country | US | 0.70 (0.47–1.04) | .080 | 26.4 | .246 | .044 |
| Other | 0.93 (0.80–1.09) | .373 | 25.9 | .213 | ||
| Sample size | ≥100 | 0.89 (0.78–1.02) | .087 | 15.1 | .304 | .802 |
| <100 | 0.63 (0.23–1.70) | .358 | 68.8 | .022 | ||
| Mean age, y | ≥60.0 | 0.84 (0.69–1.03) | .090 | 54.3 | .032 | .548 |
| <60.0 | 0.94 (0.63–1.40) | .752 | 0.0 | .436 | ||
| Percentage of male patients (%) | ≥70.0 | 0.91 (0.61–1.36) | .638 | 0.0 | .454 | .782 |
| <70.0 | 0.85 (0.69–1.05) | .140 | 54.2 | .026 | ||
| Tracheotomy methods | Open | 0.94 (0.60–1.45) | .770 | 0.0 | .484 | .309 |
| Percutaneous | 0.78 (0.60–1.01) | .061 | 51.3 | .055 | ||
| Both | 0.97 (0.83–1.14) | .752 | 0.0 | .396 | ||
| Study quality | High | 0.92 (0.76–1.11) | .397 | 27.0 | .204 | .195 |
| Low | 0.82 (0.58–1.15) | .246 | 47.7 | .105 |
3.4. Ventilator-associated pneumonia
The data for the effect of early versus late tracheotomy on the risk of ventilator-associated pneumonia were available in 13 trials. The risk of ventilator-associated pneumonia in patients who underwent early tracheotomy was reduced by 10%, but with no statistically significant difference (RR: 0.90; 95% CI: 0.78–1.04; P = .156; Fig. 3). Moreover, significant heterogeneity was observed across included trials (I2 = 68.3%; P < .001). The sensitivity analysis indicated that the pooled conclusion was not altered by excluding any particular trial (Supplemental Digital Content [Figure S2]). The subgroup analysis indicated that early tracheotomy was associated with a reduced risk of ventilator-associated pneumonia if the sample size of pooled trials was ≥100, whereas no significant differences were detected between early and late tracheotomy (Table 3). Moreover, the interaction P test indicated that the effect of early versus late tracheotomy on the risk of ventilator-associated pneumonia was affected by sample size (P < .001), percentage of male patients (P = .005), and tracheotomy methods (P < .001).
Figure 3.
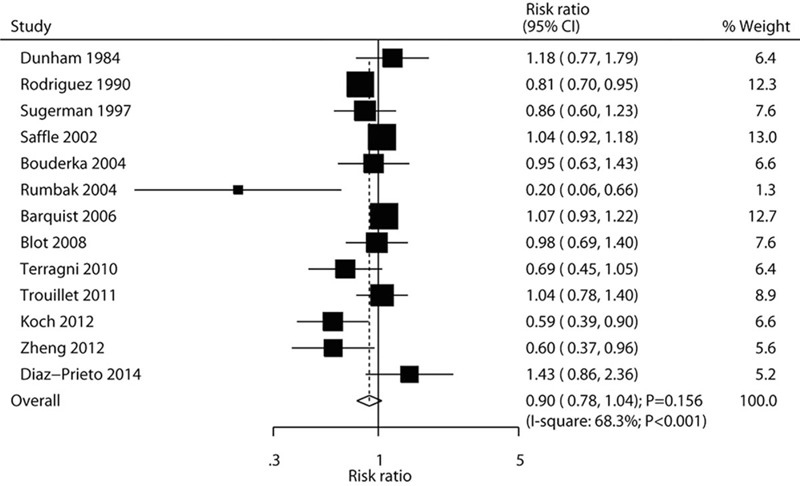
Effects of early versus late tracheotomy on the risk of ventilator-associated pneumonia.
Table 3.
Subgroup analyses for ventilator-associated pneumonia.
| Factors | Subgroup | RR and 95% CI | P-value | Heterogeneity (%) | P-value for heterogeneity | P-value between subgroups |
| Country | US | 0.94 (0.77–1.15) | .526 | 79.7 | <.001 | .535 |
| Other | 0.86 (0.69–1.07) | .185 | 53.2 | .046 | ||
| Sample size | ≥100 | 0.82 (0.68–0.98) | .033 | 56.9 | .017 | <.001 |
| <100 | 1.05 (0.97–1.15) | .229 | 0.0 | .895 | ||
| Mean age, y | ≥60.0 | 0.83 (0.60–1.15) | .257 | 67.4 | .009 | .237 |
| <60.0 | 0.94 (0.79–1.11) | .463 | 74.5 | .001 | ||
| Percentage of male patients (%) | ≥70.0 | 0.95 (0.77–1.16) | .598 | 72.5 | .026 | .005 |
| <70.0 | 0.78 (0.58–1.05) | .102 | 66.8 | .006 | ||
| Tracheotomy methods | Open | 1.05 (0.97–1.15) | .220 | 0.0 | .922 | <.001 |
| Percutaneous | 0.74 (0.52–1.06) | .103 | 71.5 | .004 | ||
| Both | 0.86 (0.60–1.23) | .401 | – | – | ||
| Study quality | High | 0.93 (0.78–1.11) | .432 | 69.5 | .003 | .061 |
| Low | 0.85 (0.64–1.13) | .262 | 65.8 | .012 |
3.5. ICU stay, mechanical ventilation duration, and hospital stay
The data for the effect of early versus late tracheotomy on ICU stay were available in 8 trials. The pooled SMD suggested that patients treated with early tracheotomy had shorter ICU stay (SMD: –1.81; 95% CI: –2.64 to –0.99; P < .001; Fig. 4); significant heterogeneity was observed among included trials (I2 = 98.4%; P < .001). This conclusion was robust and not changed by sequentially excluding individual trials (S1–S4 Figs.). Moreover, the data on the effect of early versus late tracheotomy on mechanical ventilation duration were available in 8 trials. Early tracheotomy was associated with shorter mechanical ventilation duration compared with late tracheotomy (SMD: –1.17; 95% CI: –2.10 to –0.24; P = .014; Fig. 5), and significant heterogeneity was detected across included trials (I2 = 98.0%; P < .001). Nevertheless, this conclusion was not stable, especially after excluding the trial conducted by Rodriguez et al,[27] which specifically included younger patients (Supplemental Digital Content [Figure S3 and Figure S4). Finally, only 3 trials reported the effect of early versus late tracheotomy on hospital stay, but with no significant difference (SMD: –0.42; 95% CI: –1.36–0.52; P = .377; Fig. 6); significant heterogeneity was observed across included trials (I2 = 93.4%; P < .001).
Figure 4.
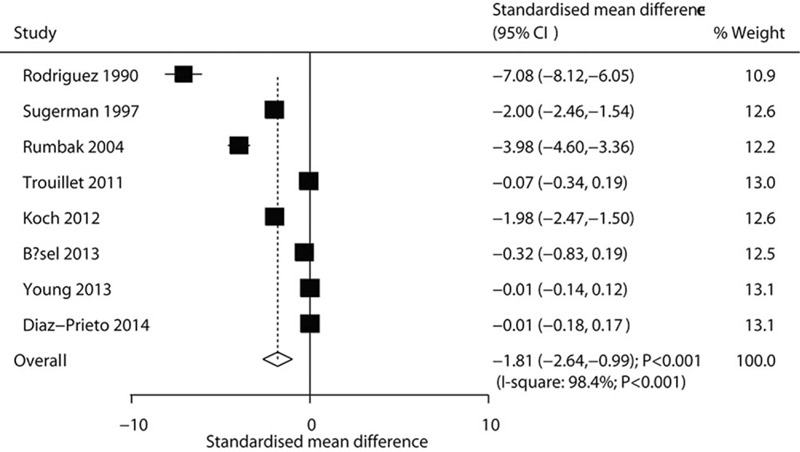
Effects of early versus late tracheotomy on ICU stay. ICU = intensive care unit.
Figure 5.
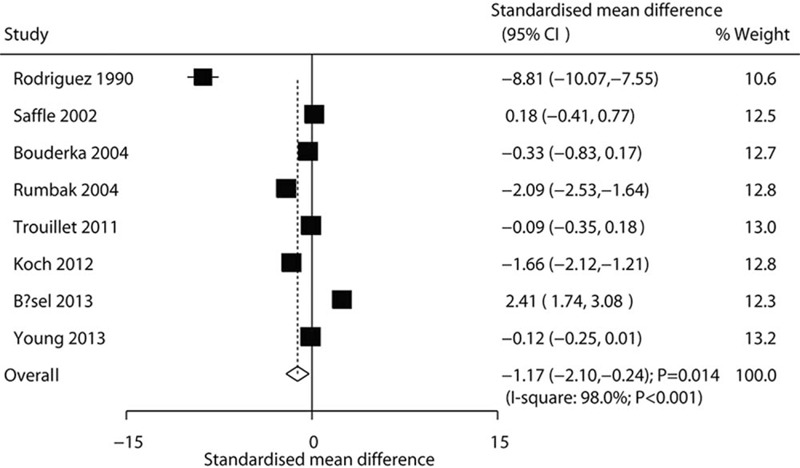
Effects of early versus late tracheotomy on the duration of mechanical ventilation.
Figure 6.
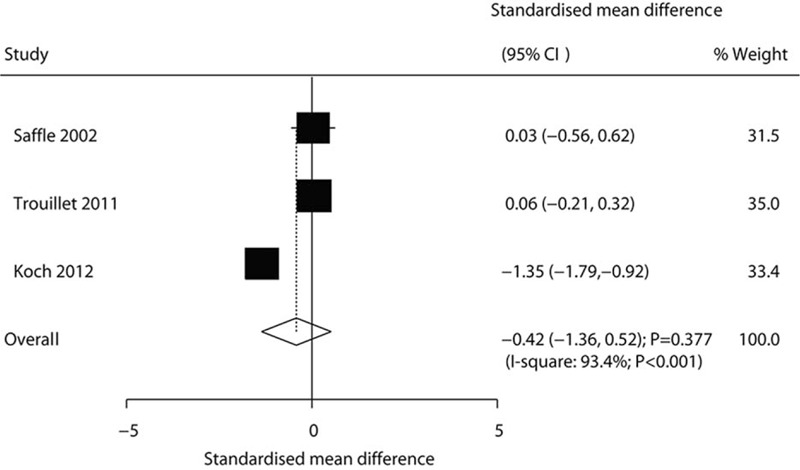
Effects of early versus late tracheotomy on hospital stay.
3.6. Publication bias
The publication biases for short-term mortality and ventilator-associated pneumonia were assessed using both qualitative and quantitative methods (Fig. 7). No significant publication biases were observed for short-term mortality (P-value for Egger: .513; P-value for Begg: .443) and ventilator-associated pneumonia (P-value for Egger: .117; P-value for Begg: .161).
Figure 7.
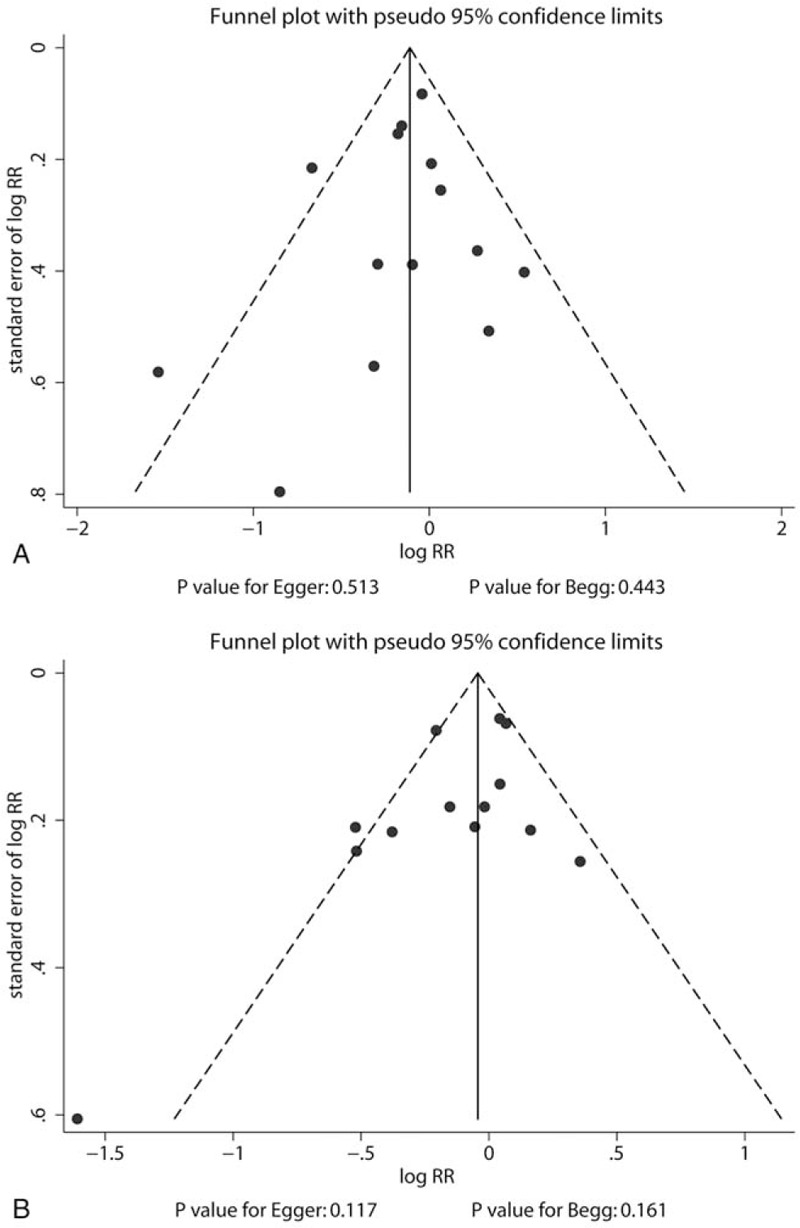
Funnel plots for short-term mortality (A) and ventilator-associated pneumonia (B).
4. Discussion
This systematic review and meta-analysis assessed the pooled effect of early versus late tracheotomy on critically ill patients undergoing mechanical ventilation. The present updated meta-analysis contained 3003 patients from 15 RCTs with a broad range of patient characteristics. The results of this study suggested that early versus late tracheotomy did not alter the risk of clinical endpoints, whereas early tracheotomy was associated with shorter ICU stay and mechanical ventilation duration. The subgroup analyses indicated the potential beneficial effects of early tracheotomy on the risk of short-term mortality and ventilator-associated pneumonia. The effects of early versus late tracheotomy were influenced by country, sample size, percentage of male patients, and tracheotomy methods.
Several systematic reviews and meta-analyses explored the effects of early versus late tracheotomy on critically ill patients undergoing mechanical ventilation. A meta-analysis conducted by Wang et al[11] included 7 RCTs and found that early tracheotomy was not associated with short-term mortality, long-term mortality, ventilator-associated pneumonia, mechanical ventilation duration, sedation duration, ICU stay, hospital stay, and potential adverse events in critically ill patients. Shan et al[12] conducted a meta-analysis of 6 RCTs and 5 observational studies and found that early tracheotomy was associated with shorter ICU stay, shorter mechanical ventilation duration, and lower risk of mortality, whereas no significant difference in the risk of hospital-acquired pneumonia was found between groups. However, these conclusions were variable with pooled RCTs or non-RCTs, suggesting that the conclusions should be interpreted cautiously. A meta-analysis conducted by Liu et al[14] included 11 RCTs and found that early tracheotomy was associated with a reduced risk of short-term mortality; however, it had no significant effect on the risk of ventilator-associated pneumonia. Moreover, another important meta-analysis of 11 RCTs and found that early tracheotomy conducted within 7 days of intubation could reduce the duration of ICU stay; no significant differences in hospital mortality, pneumonia, mechanical ventilation duration, laryngotracheal injury, and sedation use were observed between groups.[13] Meng et al[15] reported that early tracheotomy might be able to reduce the duration of sedation but did not significantly alter the mortality, incidence of VAP, duration of MV, and length of ICU stay. Nevertheless, the previous meta-analysis based on RCTs did not include stratified analyses according to patient characteristics. Therefore, the present updated meta-analysis of RCTs was conducted to systematically compare the treatment efficacy of early tracheotomy versus late tracheotomy in critically ill patients undergoing mechanical ventilation.
Compared with the previous meta-analysis, this meta-analysis noted no significant difference between the effects of early and late tracheotomy on the risk of short-term mortality and ventilator-associated pneumonia. Two of the included trials reported that patients treated with early tracheotomy had a reduced risk of short-term mortality.[31,38] The study by Rumbak et al[31] included 120 critically ill patients and found that early tracheotomy was superior to late tracheotomy in patients who were predicted to need ventilation for >14 days, in terms of shorter ICU stay and mechanical ventilation duration, lower risk of mortality and ventilator-associated pneumonia, less damage to the mouth and larynx, and less loss of airway control. Moreover, Bösel et al[38] found that early tracheotomy was associated with a lower risk of ICU mortality and 6-month mortality. The potential reason for this could be the reduction in the use of sedatives and opioids and the difference in illness severity and causes of death between groups. Unfortunately, the early termination of sedation could not be examined in this study because of inconsistent reporting among the included trials. This is an important clinical issue that should be the focus of future studies. Of note, training of the staff might influence the results, and it must be highlighted that ICU and emergency department staff should be trained for cricothyrotomy in emergency situations.[41]
The summary result indicated no significant difference between the effects of early and late tracheotomy on the risk of ventilator-associated pneumonia. The subgroup analysis indicated that early tracheotomy was superior to late tracheotomy when the sample size of pooled trials was >100. Four of the included trials indicated that early tracheotomy was associated with a reduced risk of ventilator-associated pneumonia.[27,31,36,37] This might be because of the large destruction of the structure by late tracheotomy. Moreover, the definition of early tracheotomy varied among included trials, and surgeons always chose the timing of tracheotomy according to their experience.[42]
An early tracheotomy was associated with shorter ICU stay and mechanical ventilation duration, whereas no significant difference in hospital stay was found between groups. This is because early tracheotomy was associated with reduced dead space, less airway resistance, decreased breathing work, better secretion removal by suctioning, reduced risk of tube obstruction risk, and better glottic function.[43] Again, early termination of sedation, one of the most important aspects of early tracheotomy, could not be examined in any reliable manner in this meta-analysis. Moreover, although no significant difference in hospital stay was found between groups, this conclusion might be unreliable due to the smaller number of included trials.
This study has several limitations. First, the illness severity of the patients was defined with various criteria, restricting stratified analyses according to the severity of the disease. Second, the use of various tracheotomy methods biased the impact of the timing of tracheotomy on critically ill patients, and 2 of the included trials even did not report the type of tracheotomy method. Third, the definition of early and late tracheotomy differed across the included trials, affecting the prognosis of critically ill patients. This results in an overlap between the 2 groups of included RCTs (early tracheotomy ranging from 1 to 8 days and late tracheotomy ranging from 6 to 28 days). Because we had no access to the raw data of each included study, we could not reclassify the patients according to a unified definition of early versus late tracheotomy, and we had to use the grouping of each study. This possibly influences the results. Fourth, the analysis is based on published RCTs, and publication bias is inevitable. Fifth, in some trials, the patients randomized to late tracheotomy ultimately do not receive tracheotomy at all because of marked improvement in condition, worsening of the condition, or death. This, of course, affects all the outcomes across all included studies, as well as the present meta-analysis. Last but not least, the level of heterogeneity was very high for all analyses, indicating that the results must be taken with caution despite the use of the random effect model.
The results of this study suggest that early tracheotomy does not have significant beneficial effects on short-term clinical endpoints, whereas it can reduce the ICU stay and mechanical ventilation duration. Further large-scale RCTs should be conducted to verify the results of this study and evaluate the long-term clinical endpoints between early and late tracheotomy for critically ill patients undergoing mechanical ventilation. Future meta-analyses should specifically examine the advantages of early termination of sedation when using early tracheotomy.
Author contributions
Conceptualization: Kun Chen.
Data curation: Hongsheng Deng, Qiang Fang.
Formal analysis: Hongsheng Deng, Qiang Fang, Kun Chen.
Methodology: Kun Chen.
Writing – original draft: Hongsheng Deng, Qiang Fang, Xiaoling Zhang.
Writing – review & editing: Hongsheng Deng, Qiang Fang, Kun Chen, Xiaoling Zhang.
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Footnotes
Abbreviations: CIs = confidence intervals, ICU = intensive care unit, RCTs = randomized controlled trials, RRs = relative risks, SMDs = standardized mean differences.
How to cite this article: Deng H, Fang Q, Chen K, Zhang X. Early versus late tracheotomy in ICU patients: A meta-analysis of randomized controlled trials. Medicine. 2021;100:3(e24329).
This study was supported by the Science and Technology Social Development Key Projects of Jinhua Municipal Bureau (No. 2018–3–012).
The authors have no conflicts of interest to disclose.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
APACHE = acute physiology and chronic health evaluation; GCS = Glasgow Coma Score; ISS = injury severity score; SAPS = simplified acute physiologic score.
RRs = relative risks.
CI = confidence interval; RR = relative risk.
References
- [1].Scales DC, Ferguson ND. Tracheostomy: it's time to move from art to science. Crit Care Med 2006;34:3039–40. [DOI] [PubMed] [Google Scholar]
- [2].Esteban A, Anzueto A, Alía I, et al. How is mechanical ventilation employed in the intensive care unit? An international utilization review. Am J Respir Crit Care Med 2000;161:1450–8. [DOI] [PubMed] [Google Scholar]
- [3].Pryor JP, Reilly PM, Shapiro MB. Surgical airway management in the intensive care unit. Crit Care Clin 2000;16:473–88. [DOI] [PubMed] [Google Scholar]
- [4].Diehl JL, El Atrous S, Touchard D, et al. Changes in the work of breathing induced by tracheotomy in ventilator-dependent patients. Am J Respir Crit Care Med 1999;159:383–8. [DOI] [PubMed] [Google Scholar]
- [5].Durbin CG, Jr, Perkins MP, Moores LK. Should tracheostomy be performed as early as 72 hours in patients requiring prolonged mechanical ventilation? Respir Care 2010;55:76–87. [PubMed] [Google Scholar]
- [6].De Leyn P, Bedert L, Delcroix M, et al. Tracheotomy: clinical review and guidelines. Eur J Cardiothorac Surg 2007;32:412–21. [DOI] [PubMed] [Google Scholar]
- [7].Ryan DW, Kilner AJ. Another death after percutaneous dilational tracheostomy. Br J Anaesth 2003;91:925–6. [DOI] [PubMed] [Google Scholar]
- [8].Shlugman D, Satya-Krishna R, Loh L. Acute fatal haemorrhage during percutaneous dilatational tracheostomy. Br J Anaesth 2003;90:517–20. [DOI] [PubMed] [Google Scholar]
- [9].McWhorter AJ. Tracheotomy: timing and techniques. Curr Opin Otolaryngol Head Neck Surg 2003;11:473–9. [DOI] [PubMed] [Google Scholar]
- [10].Plummer AL, Gracey DR. Consensus conference on artificial airways in patients receiving mechanical ventilation. Chest 1989;96:178–80. [DOI] [PubMed] [Google Scholar]
- [11].Wang F, Wu Y, Bo L, et al. The timing of tracheotomy in critically ill patients undergoing mechanical ventilation: a systematic review and meta-analysis of randomized controlled trials. Chest 2011;140:1456–65. [DOI] [PubMed] [Google Scholar]
- [12].Shan L, Zhang R, Li LD. Effect of timing of tracheotomy on clinical outcomes: an update meta-analysis including 11 trials. Chin Med Sci J 2013;28:159–66. [DOI] [PubMed] [Google Scholar]
- [13].Liu CC, Livingstone D, Dixon E, et al. Early versus late tracheostomy: a systematic review and meta-analysis. Otolaryngol Head Neck Surg 2015;152:219–27. [DOI] [PubMed] [Google Scholar]
- [14].Liu X, Wang HC, Xing YW, et al. The effect of early and late tracheotomy on outcomes in patients: a systematic review and cumulative meta-analysis. Otolaryngol Head Neck Surg 2014;151:916–22. [DOI] [PubMed] [Google Scholar]
- [15].Meng L, Wang C, Li J, et al. Early vs late tracheostomy in critically ill patients: a systematic review and meta-analysis. Clin Respir J 2016;10:684–92. [DOI] [PubMed] [Google Scholar]
- [16].Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009;6:e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Jadad AR, Moore RA, Carroll D, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials 1996;17:1–2. [DOI] [PubMed] [Google Scholar]
- [18].DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials 1986;7:177–88. [DOI] [PubMed] [Google Scholar]
- [19].Ades AE, Lu G, Higgins JP. The interpretation of random-effects meta-analysis in decision models. Med Decis Making 2005;25:646–54. [DOI] [PubMed] [Google Scholar]
- [20].Deeks JJ, Higgins JPT, Altman DG. Higgins J, Green S. Analyzing data and undertaking meta-analyses. The Cochrane Collaboration, Cochrane Handbook for Systematic Reviews of Interventions 5.0.1. Oxford, UK: 2008. [Google Scholar]
- [21].Higgins JP, Thompson SG, Deeks JJ, et al. Measuring inconsistency in meta-analyses. BMJ 2003;327:557–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Tobias A. Assessing the influence of a single study in the meta-anyalysis estimate. Stata Technical Bull 1999;8:15–7. [Google Scholar]
- [23].Altman DG, Bland JM. Interaction revisited: the difference between two estimates. BMJ 2003;326:219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Egger M, Davey Smith G, Schneider M, et al. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997;315:629–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics 1994;50:1088–101. [PubMed] [Google Scholar]
- [26].Dunham CM, LaMonica C. Prolonged tracheal intubation in the trauma patient. J Trauma 1984;24:120–4. [DOI] [PubMed] [Google Scholar]
- [27].Rodriguez JL, Steinberg SM, Luchetti FA, et al. Early tracheostomy for primary airway management in the surgical critical care setting. Surgery 1990;108:655–9. [PubMed] [Google Scholar]
- [28].Sugerman HJ, Wolfe L, Pasquale MD, et al. Multicenter, randomized, prospective trial of early tracheostomy. J Trauma 1997;43:741–7. [DOI] [PubMed] [Google Scholar]
- [29].Saffle JR, Morris SE, Edelman L. Early tracheostomy does not improve outcome in burn patients. J Burn Care Rehabil 2002;23:431–8. [DOI] [PubMed] [Google Scholar]
- [30].Bouderka MA, Fakhir B, Bouaggad A, et al. Early tracheostomy versus prolonged endotracheal intubation in severe head injury. J Trauma 2004;57:251–4. [DOI] [PubMed] [Google Scholar]
- [31].Rumbak MJ, Newton M, Truncale T, et al. A prospective, randomized, study comparing early percutaneous dilational tracheotomy to prolonged translaryngeal intubation (delayed tracheotomy) in critically ill medical patients. Crit Care Med 2004;32:1689–94. [DOI] [PubMed] [Google Scholar]
- [32].Barquist ES, Amortegui J, Hallal A, et al. Tracheostomy in ventilator dependent trauma patients: a prospective, randomized intention-to-treat study. J Trauma 2006;60:91–7. [DOI] [PubMed] [Google Scholar]
- [33].Blot F, Similowski T, Trouillet JL, et al. Early tracheotomy versus prolonged endotracheal intubation in unselected severely ill ICU patients. Intensive Care Med 2008;34:1779–87. [DOI] [PubMed] [Google Scholar]
- [34].Terragni PP, Antonelli M, Fumagalli R, et al. Early vs late tracheotomy for prevention of pneumonia in mechanically ventilated adult ICU patients: a randomized controlled trial. JAMA 2010;303:1483–9. [DOI] [PubMed] [Google Scholar]
- [35].Trouillet JL, Luyt CE, Guiguet M, et al. Early percutaneous tracheotomy versus prolonged intubation of mechanically ventilated patients after cardiac surgery: a randomized trial. Ann Intern Med 2011;154:373–83. [DOI] [PubMed] [Google Scholar]
- [36].Koch T, Hecker B, Hecker A, et al. Early tracheostomy decreases ventilation time but has no impact on mortality of intensive care patients: a randomized study. Langenbecks Arch Surg 2012;397:1001–8. [DOI] [PubMed] [Google Scholar]
- [37].Zheng Y, Sui F, Chen XK, et al. Early versus late percutaneous dilational tracheostomy in critically ill patients anticipated requiring prolonged mechanical ventilation. Chin Med J (Engl) 2012;125:1925–30. [PubMed] [Google Scholar]
- [38].Bösel J, Schiller P, Hook Y, et al. Stroke-related early tracheostomy versus prolonged orotracheal intubation in neurocritical care trial (SETPOINT): a randomized pilot trial. Stroke 2013;44:21–8. [DOI] [PubMed] [Google Scholar]
- [39].Young D, Harrison DA, Cuthbertson BH, et al. Effect of early vs late tracheostomy placement on survival in patients receiving mechanical ventilation: the TracMan randomized trial. JAMA 2013;309:2121–9. [DOI] [PubMed] [Google Scholar]
- [40].Diaz-Prieto A, Mateu A, Gorriz M, et al. A randomized clinical trial for the timing of tracheotomy in critically ill patients: factors precluding inclusion in a single center study. Crit Care 2014;18:585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Buonopane CE, Pasta V, Sottile D, et al. Cricothyrotomy performed with the Melker™ set or the QuickTrach™ kit: procedure times, learning curves and operators’ preference. G Chir 2014;35:165–70. [PMC free article] [PubMed] [Google Scholar]
- [42].Shirawi N, Arabi Y. Bench-to-bedside review: early tracheostomy in critically ill trauma patients. Crit Care 2006;10:201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Pierson DJ. Tracheostomy and weaning. Respir Care 2005;50:526–33. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


