Abstract
Hydrogen peroxide is a liquid that functions in mechanical removal of the necrotic tissue via the elimination of tissue debris.
In this study, we aimed to evaluate the effectiveness of the use of hydrogen peroxide in necrosectomy treatment of walled-off pancreatic necrosis.
Records of 24 patients who were diagnosed with pancreatic necrosis or walled-off pancreatic necrosis and underwent endoscopic necrosectomy (EN) were retrospectively assessed. Patients were divided into 2 groups; hydrogen peroxide used for treatment or not used, and these 2 groups were compared.
A total of 24 patients underwent endoscopic intervention for walled-off pancreatic necrosis. Procedural success was comparable between the 2 groups. During the post-procedural follow-up, the duration of the hospital stay, recurrence, and complication rates were found to be similar in both groups. The mean number of the endoscopic interventions was significantly lower in the hydrogen peroxide group (4.2 ± 1.4 vs 6.1 ± 4.2; P = .01).
The use of hydrogen peroxide for EN in walled-off pancreatic necrosis patients seems to have similar efficiency and safety. However, it can be said that the use of hydrogen peroxide could reduce the number of endoscopic procedures.
Keywords: hydrogen peroxide, pancreatic necrosis, walled-off pancreatic necrosis
1. Introduction
Pancreatic necrosis (PN) and walled-off pancreatic necrosis (WOPN) are important local complications observed during the course of acute pancreatitis. They are seen approximately in 10% to 15% of the patients.[1] Endoscopic ultrasonography (EUS) and cross-sectional imaging modalities have been used more frequently in acute pancreatitis management. Therefore, awareness of these complications has increased recently.
Previous pancreatitis management guidelines recommended primarily surgical treatment methods for PN and WOPN. However, treatment approaches and disease management have changed in recent years, especially because of EUS-guided metal stenting and endoscopic necrosectomy (EN) was associated with lower mortality and morbidity compared with the surgery.[2–5]
Hydrogen peroxide (H2O2) is a liquid that functions in mechanical removal of the necrotic tissue via the elimination of tissue debris and can help close the necrotic cavity by stimulating granulation and fibrosis in healthy tissue.[6,7] Hydrogen peroxide was used in 2013 for the first time by Abdelhafez et al. during transluminal retroperitoneal EN treatment in pancreatic wall of necrosis, and its efficacy and safety was demonstrated.[8] Similar results were obtained in various studies performed afterwards. Besides, it has a favorable impact on the success of EUS-guided necrosectomy treatment.[9,10]
In this study, we aimed to evaluate the effectiveness of the use of H2O2 and whether it provides additional contribution to the procedure in necrosectomy treatment of PN/WOPN.
2. Methods
2.1. Patient selection
Records of 24 patients who were diagnosed with PN or WOPN and underwent EN between June 2010 and July 2019 were retrospectively assessed.
2.1.1. Exclusion Criteria
Peripancreatic fluids other than WOPN, patients with malignant fluid collections, and patients who had missing data during the follow-up period were excluded from the study.
The study was conducted in accordance with the Declaration of Helsinki, and the protocol was approved by the Ethics Committee of Izmir Katip Çelebi University Hospital. (ethic comittee number=2020 GOKAE 0412).
2.2. Study design
The data assessed in the study were retrieved from Katip Çelebi University Faculty of Medicine Gastroenterology Department of Izmir Training and Research Hospital's electronic database system (Probel). Demographic characteristics, cause of pancreatitis, the size and the location of the necrosis, the method of endoscopic intervention (EUS or duodenoscopy), features of the endoscopic intervention, the total number of interventions, the duration of the hospital stay and complications, the need for surgical intervention (if present), and mortality were evaluated. Patients were divided into 2 groups; H2O2 used for treatment or not used, and these 2 groups were compared with respect to the parameters mentioned above. Descriptions, classifications, and severity indices of PN/WOPN were based on the revised Atlanta criteria.[1]
EN technique: Endoscopy procedure was performed by a linear EUS (Olympus Exera II CLV-180 linear EUS) or a duodenoscope (Fujinon VP-4450HD). An anesthesiologist participated in each procedure to apply anesthesia.
A 19-G aspiration needle (Expect, Boston Scientific, Boston, Massachusetts, USA) or needle knife (Micro-Tech, Nanjing, China), a 0.035-inch (0.89 mm) guidewire (Jagwire; Boston Scientific, Boston, Massachusetts) were used for the drainage of collections. Pancreatic SEMS (self-expandable metallic stent) (Micro-Tech, Nanjing, China) was used for stenting. After the collection was punctured, biliary bougie dilator and CRE balloon dilation catheter (12 mm) were used for the dilation.
Abdominal computerized tomography (CT) was performed in all patients before the procedure, by which the anatomical relation of the necrosis cavity with the stomach and its wall maturation were evaluated. CT images showed that the gastric wall and the wall of the necrosis cavity were adjacent in all cases. In 7 of the patients, the procedure was continued with the duodenoscopy after marking the intervention site with the linear EUS probe. After the 19-G needle or the needle-knife was inserted through the linear EUS or the duodenoscope and the lesion was punctured, the 0.35-inch guidewire was inserted. By means of C-arm scopy (X-Ray), it was ascertained that the guidewire made 2 rounds in the lesion. The puncture site was dilated with the biliary bougie dilator through the guidewire, and then dilation was continued with the 12 mm CRE balloon dilation catheter. The pancreatic SEMS was placed through the guidewire. After that, the necrosis cavity was accessed by the endoscope, and the necrosis was drained by the polypectomy snare, the netting snare, the stone extraction basket or the foreign body forceps every 3 days. After the necrosis evacuation, the cavity was washed with approximately 500 ml of water, followed by additional washing with 250 mL of 50% diluted H2O2. One week after the stenting and before the removal of it, a control abdominal CT was performed. The stents were removed endoscopically after the cavity was completely cleared of the necrosis.
2.3. Statistical analysis
All programs were performed using SPSS 25.0 package program. Frequency and percentages of categorical variables, mean, and standard deviation or median and minimum-maximum values of continuous variables were calculated as descriptive statistics. The relationship between categorical variables was tested by Chi-square or Fisher's precision test, and the relationship between continuous variables was tested by Spearman correlation analysis. The Mann Whitney-U Test was used to compare the 2 independent sample mean, and Kruskal Wallis Test was used to compare the mean of more than 2 independent samples. The confidence level of the study was 95% (P < .05 was considered statistically significant).
3. Results
A total of 24 patients underwent endoscopic intervention for WOPN (12 males and 12 females, median age 61.5 years) (Fig. 1). The causes of pancreatitis in which H2O2 was used for treatment were gallstones in 9 patients and alcohol use in 2 patients. Gallstones were the etiologic factor for the rest of the patients in whom H2O2 was not used. The baseline characteristics of the patients are shown in Table 1.
Figure 1.
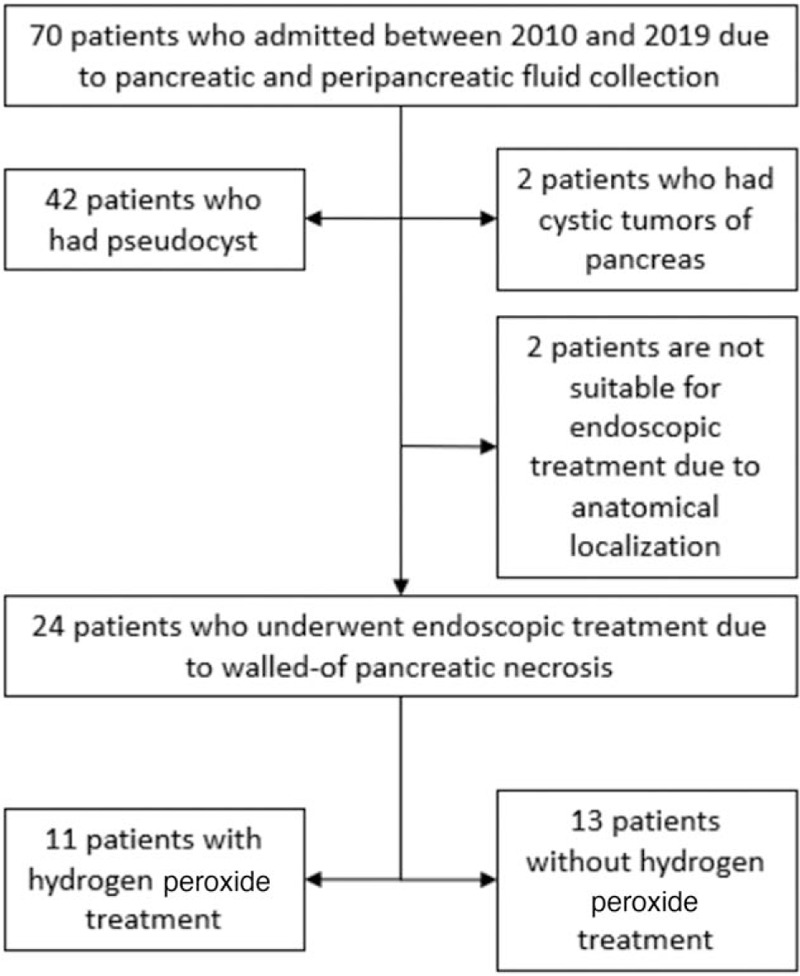
Flow chart of patient selection for the study.
Table 1.
The baseline characteristics of the patients.
| H2O2 used | H2O2 not used | P | |
| WOPN, n | 11 | 13 | |
| Sex, n (%) | |||
| Female | 5 (58.3%) | 7 (41.7%) | .688 |
| Male | 6 (50%) | 6 (50%) | |
| Mean age (SD), year | 64.9 ± 11.8 | 62.4 ± 9.7 | .58 |
| Pancreatitis etiology, n (%) | |||
| Gallstone | 9 (40.9%) | 13 (59.1%) | .10 |
| Alcohol | 2 (100%) | 0 | |
| Cyst long axis measurement (SD), mm | 118.6 ± 74.2 | 125.3 ± 47.7 | .79 |
| Site of PFC | |||
| Pancreatic head, n | 4 (33.3%) | 8 (66.7%) | .21 |
| Pancreatic body/tail, n | 7 (58.3%) | 5 (41.7%) | |
EUS was used in 17 (70.8%) of the endoscopic necrosectomies, whereas duodenoscope was preferred in only 7 (29.2%) of them. In all patients, the gastric wall and the wall of the necrosis cavity were adjacent. There was no statistically significant difference between the H2O2 and non- H2O2 groups with respect to the procedure used. The site of endoscopic intervention, stent type, 19-G needle, or needle knife use was similar between the study groups. Procedural success was comparable between the 2 groups. Characteristics of the endoscopic intervention of the whole study cohort are presented in Table 2.
Table 2.
Characteristics of the endoscopic intervention.
| H2O2 used | H2O2 not used | ||
| n (%) | n (%) | P | |
| Endoscopy type | |||
| EUS | 6 (35.3%) | 11 (64.7%) | .10 |
| Duodenoscopy | 5 (71.4%) | 2 (28.6%) | |
| Site of necrosectomy | |||
| Stomach body or antrum | 8 (44.4%) | 10 (55.6%) | .531 |
| Duodenal bulb | 2 (40%) | 3 (60%) | |
| Transpapiller | 0 | 1 | |
| Puncture | |||
| Needle knife | 7 (63.6%) | 9 (69.2%) | .10 |
| 19G | 4 (30.8%) | 9 (69.2%) | |
| Stent type | |||
| SEMS | 10 | 12 | .72 |
| Double pigtail+SEMS | 1 | 1 | |
| Procedural technical success | 10 (92.3%) | 12 (90.9%) | .90 |
During the post-procedural follow-up, the duration of the hospital stay, recurrence, and complication rates were found to be similar in both groups. The mean number of the endoscopic interventions was significantly lower in the H2O2 group (4.2 ± 1.4 vs 6.1 ± 4.2; P = .01). The follow-up features of the patients who underwent EN due to WOPN are shown in Table 3.
Table 3.
The follow-up features of the patients who underwent endoscopic necrosectomy due to WOPN.
| H2O2 used | H2O2 not used | P | |
| Mean of endoscopic sessions | 4.2 ± 1.4 | 6.1 ± 4.2 | .01 |
| The duration of the hospital stay (day) | 23.2 ± 10.2 | 27.4 ± 14.5 | .43 |
| Recurrence | 0 | 0 | |
| Procedure adeverse events | |||
| Self-limited bleeding | 0 | 1 | .19 |
| Perforation | 0 | 0 | |
| Stent maldeployment | 2 | 0 | |
| Infection of PFC cavity | 0 | 0 | |
The appearance of the WPON cavity before and after the use of H2O2 were shown in Figures 2 and 3. Necrosectomy procedure by using H2O2 in a WPON patient was showed in the video.
Figure 2.
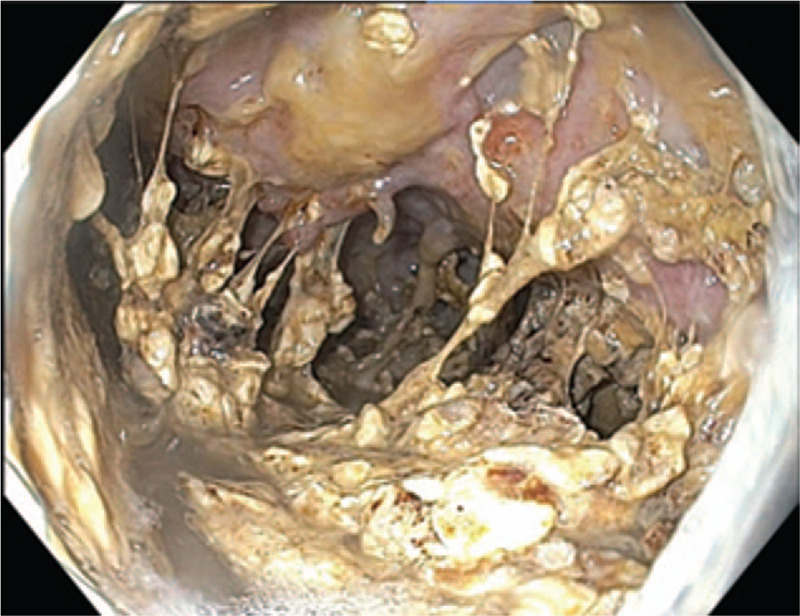
The appearance of the WOPN cavity before the use of H2O2.
Figure 3.

The appearance of the WOPN cavity after the use of H2O2.
4. Discussion
With the progress of endoscopic methods and particularly with the increasing use of EUS for therapeutic purposes, EN has become the treatment modality of choice in necrotic tissue drainage in WOPN. Especially by using LAMS stents for this purpose, technical and clinical success rates have increased, and the need for repeat procedure has reduced.[11] EN is a safe technique, yet complications may occur. The frequency of complications such as bleeding, perforation, stent migration, and stent infection has been reported as 4% to 26%.[12,13] The amount of necrotic material in the abscess cavity is an important factor determining the success of endoscopic drainage.[6] Clogging of the stents with the necrotic material and the need for re-endoscopy reduce clinical success rate; therefore, more effective techniques are being developed. It was suggested that a chemical substance put into the necrosis cavity would facilitate the mechanical debridement of the necrosis; hence, contribute favorably to the success of the treatment.[2]
H2O2 is a chemical agent known for its effect on mechanical cleaning of wounds. It contributes to remove necrotic tissue and may help close the necrotic cavity by stimulating the granulation and the fibrosis in the healthy tissue.[6,7] For this purpose, Abdelhafez et al used H2O2 for the debridement of the PN in ten patients. They reported a 100% clinical and technical success rate along with minor bleeding in only 3 patients. The authors did not report any recurrence or need for surgery during the course of follow-up. However, EUS was not used in that study.[8] In our study, we aimed to evaluate the effect of H2O2 use in EN on the treatment outcome and the number of endoscopic interventions. We used H2O2 in WOPN patients with intense debris regardless of cyst size and localization. For this purpose, we compared the EN procedures with and without the use of H2O2.
In studies conducted after the Abdelhafez et al, H2O2 was used for EN in WOPN patients. SEMS was placed by an endoscopic method, and necrosectomy was performed with H2O2. In the case series of Siddiqui et al., the necrosectomy with H2O2 was reported to be effective and has similar risks to EN without H2O2. Other similar studies had reported clinical success rates between 90.6% to 95% and the technical success rates reaching 100%.[6,14] In studies that used EN without H2O2, the clinical success rates were reported between 80% to 91%.[12,15] In our study, the technical success rate was 92.3% in the H2O2 group and 90.9% in the non- H2O2 group, and the difference was not statistically significant.
Repeated interventions may be needed in patients with WOPN because of stent occlusion by the necrotic material. In our study, the mean number of the intervention per patient was in line with the figures reported in the literature in the non- H2O2 group.[12] The mean number of interventions per patient was between 2.0 to 3.2 in patients receiving H2O2 treatment.[6,9,14] In our study, the mean number of endoscopic interventions per patient was 4.2 in the H2O2 group, and it was significantly lower than that of the non- H2O2 group. However, the mean number of endoscopic interventions in our study was higher than reported by similar studies in the literature. While the number of interventions was higher in the first cases due to insufficient experience of the endoscopist, this number gradually decreased as our competency increased. We found that the mean number of interventions per patient was high in the first cases because of insufficient experience.
Recurrence rates after the debridement with H2O2 had been reported between 0% to 5.2% in EN procedure.[6,9,14] In our study, it was not possible to conclude the effect of H2O2 on recurrence rate because no recurrence was detected in EN patients.
In previous studies, complication frequency was reported between 4% to 26% in patients whom H2O2 was not used, whereas this rate was reported between 12.5–28% in patients whom H2O2 was used.[6,12,13,15] In a study by Bansal et al., 4.7% of patients had life-threatening bleeding.[14] The mortality rate was reported between 4.7% to 7%.[6] In studies conducted without the use of H2O2, the mortality rate was reported between 0% to 26%.[11,16] In this study, the complication rate was similar in both H2O2 and non- H2O2 groups (9.1% vs 7.69%, P > .05). Stent migration was detected in 2 patients in the H2O2 group, and self-limited bleeding was seen in 1 patient in the non- H2O2 group. None of the patients died.
Except EN related complications, there were cases of embolism developing after some surgical procedures that used H2O2 in the literature.[17,18] Complications such as pneumoperitoneum, perforation and bleeding have been reported in the abdominal cavity after H2O2 use. In most of these cases, H2O2 was given into closed cavities with high pressure and entered into the blood vessels.[19]
There are some limitations to our study. First, it is a retrospective study. The study was not done according to any protocol. In a multicenter, prospective study with a larger number of patients, intergroup comparisons would give more accurate results. The lack of long-term results of the patients and the use of different instruments for the procedures are other limitations that deserve mention.
In conclusion, the use of H2O2 for EN in WOPN patients seems to have similar efficiency and safety in our study to the previous literature. However, it can be said that the use of H2O2 could reduce the number of endoscopic procedures.
Author contributions
Conceptualization: Suleyman Gunay, Emrah Alper.
Data curation: Suleyman Gunay, Betül Paköz, Hakan Çamyar, Elif Saritaş Yüksel.
Formal analysis: Suleyman Gunay.
Investigation: Cem Çekiç, Hakan Çamyar.
Methodology: Suleyman Gunay, Betül Paköz, Firdevs Topal.
Project administration: Firdevs Topal.
Software: Suleyman Gunay, Elif Saritaş Yüksel.
Supervision: Emrah Alper, Ömer Burcak Binicier.
Validation: Suleyman Gunay, Ömer Burcak Binicier.
Visualization: Cem Çekiç, Ömer Burcak Binicier.
Footnotes
Abbreviations: CT = computerized tomography, EN = endoscopic necrosectomy, EUS = endoscopic ultrasonography, H2O2 = hydrogen peroxide, PN = pancreatic necrosis, SEMS = self-expandable metallic stent, WOPN = walled-off pancreatic necrosis.
How to cite this article: Günay S, Paköz B, Çekiç C, Çamyar H, Alper E, Yüksel ES, Topal F, Binicier ÖB. Evaluation of hydrogen peroxide-assisted endoscopic ultrasonography-guided necrosectomy in walled-off pancreatic necrosis: a single-center experience. Medicine. 2021;100:3(e23175).
The authors have no conflicts of interest to disclose.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
H2O2 = hydrogen peroxide, PFC = pancreatic fluid collection, SD = standard deviation, WOPN = walled-off pancreatic necrosis.
EUS = Endoscopic ultrasonography, H2O2 = hydrogen peroxide, SEMS = self-expandable metallic stent.
H2O2 = hydrogen peroxide, PFC = pancreatic fluid collection, WOPN = walled-off pancreatic necrosis.
References
- [1].Banks PA, Bollen TL, Dervenis C, et al. Classification of acute pancreatitis–2012: revision of the Atlanta classification and definitions by international consensus. Gut 2013;62:102–11. [DOI] [PubMed] [Google Scholar]
- [2].Yachimski P. Can we now recommend hydrogen peroxide for pancreatic necrosectomy? Time for controlled data. Endosc Int Open 2017;5:E854–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Besselink MG, Verwer TJ, Schoenmaeckers EJ, et al. Timing of surgical intervention in necrotizing pancreatitis. Arch Surg 2007;142:1194–201. [DOI] [PubMed] [Google Scholar]
- [4].Bakker OJ, van Santvoort HC, van Brunschot S, et al. Endoscopic transgastric vs surgical necrosectomy for infected necrotizing pancreatitis: a randomized trial. JAMA 2012;307:1053–61. [DOI] [PubMed] [Google Scholar]
- [5].Seifert H, Wehrmann T, Schmitt T, et al. Retroperitoneal endoscopic debridement for infected peripancreatic necrosis. Lancet 2000;356:653–5. [DOI] [PubMed] [Google Scholar]
- [6].Mohamed O Othman, Sherif Elhanafi, Mohammed Saadi, et al. Extended cystogastrostomy with hydrogen peroxide irrigation facilitates endoscopic pancreatic necrosectomy. Diagn Ther Endosc 2017;2017:7145803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Krasner D, Kane D. Chronic wound care: a clinical sourcebook for healthcare professionals. health management publications. Incorporated 1997. [Google Scholar]
- [8].Abdelhafez M, Elnegouly M, Hasab Allah MS, et al. Transluminal retroperitoneal endoscopic necrosectomy with the use of hydrogen peroxide and without external irrigation: a novel approach for the treatment of walledoff pancreatic necrosis. Surg Endosc 2013;27:3911–20. [DOI] [PubMed] [Google Scholar]
- [9].Siddiqui AA, Easler J, Strongin A, et al. Hydrogen peroxide assisted endoscopic necrosectomy for walled-off pancreatic necrosis: a dual center pilot experience. Dig Dis Sci 2014;59:687–90. [DOI] [PubMed] [Google Scholar]
- [10].Galasso D, Baron TH, Attili F, et al. Endoscopic ultrasound-guided drainage and necrosectomy of walled-off pancreatic necrosis using a metal stent with an electrocautery-enhanced delivery system and hydrogen peroxide. Endoscopy 2015;47: Suppl 1 UCTN: E68. [DOI] [PubMed] [Google Scholar]
- [11].Sharaiha RZ, Tyberg A, Khashab MA, et al. Endoscopic therapy with lumen-apposing metal stents is safe and effective for patients with pancreatic walled-off necrosis. Clin Gastroenterol Hepatol 2016;14:1797–803. [DOI] [PubMed] [Google Scholar]
- [12].Seifert H, Biermer M, Schmitt W, et al. Transluminal endoscopic necrosectomy after acute pancreatitis: a multicentre Study with long-term follow-up (the GEPARD Study). Gut 2009;58:1260–6. [DOI] [PubMed] [Google Scholar]
- [13].Lakhtakia S, Basha J, Talukdar R, et al. Endoscopic “step-up approach” using a dedicated biflanged metal stent reduces the need for direct necrosectomy in walled-off necrosis (with videos). Gastrointest Endosc 2017;85:1243–52. [DOI] [PubMed] [Google Scholar]
- [14].Bansal RK, Puri R, Choudhary NS, et al. Endoscopic pancreatic necrosectomy: why scuff when you can flush themuck – make it an easy row to hoe. Endosc Int Open 2017;05:847–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Gardner TB, Coelho-Prabhu N, Gordon SR, et al. Direct endoscopic necrosectomy for the treatment of walled-off pancreatic necrosis: results from a multicenter U.S. series. Gastrointest Endosc 2011;73:718–26. [DOI] [PubMed] [Google Scholar]
- [16].Huggett MT, Oppong KW, Pereira SP, et al. Endoscopic drainage of walled-off pancreatic necrosis using a novel self-expanding metal stent. Endoscopy 2015;47:929–32. [DOI] [PubMed] [Google Scholar]
- [17].Zhang J, Zhang C, Yan J. Massive cerebral gas embolism under discectomy due to hydrogen peroxide irrigation. Case Rep Neurol Med 2015;2015:497340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Beattie C, Harry LE, Hamilton SA, et al. Cardiac arrest following hydrogen peroxide irrigation of a breast wound. J Plast Reconstr Aesthet Surg 2010;63:e253–4. [DOI] [PubMed] [Google Scholar]
- [19].Jones PM, Segal GH, Gelb AW. Venous oxygen embolism produced by injection of hydrogen peroxide into an enterocutaneous fistula. Anesth Analg 2004;99:1861–3. [DOI] [PubMed] [Google Scholar]


