Abstract
Background:
The aim of this systematic review and meta-analysis was to investigate the associations of community-level socioeconomic status (SES) on outcomes of patients with out-of hospital cardiac arrest (OHCA).
Methods:
A systematic literature review was conducted using PubMed, EMBASE, and the Cochrane database according to guidelines of Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA). We included literature that presented the outcomes based on community-level SES among patients with OHCA. SES indicators included economic indicators such as income, wealth, and occupation, as well as combined indicators, where any of these indicators were integrated. Outcomes were bystander cardiopulmonary resuscitation (CPR) and survival to discharge.
Results:
From 1394 titles, 10 cross-sectional observational studies fulfilled inclusion and exclusion criteria, representing 118,942 patients with OHCA. The odds ratios (ORs) of bystander CPR and survival to discharge for lower community-level SES patients were lower than those for higher community-level SES by economic SES indicators (bystander CPR OR 0.67; 95% CI 0.51–0.89, survival to discharge OR 0.60; 95% CI 0.35–1.02). Based on combined SES indicators the results showed similar patterns (bystander CPR OR 0.80; 95% CI 0.75–0.84, survival to discharge OR 0.76; 95% CI 0.63–0.92).
Conclusion:
In this meta-analysis, community-level SES was significantly associated with bystander CPR and survival among patients with OHCA.
Keywords: cardiopulmonary resuscitation, community, out-of-hospital cardiac arrest, socioeconomic status
1. Introduction
Out-of-hospital cardiac arrest (OHCA) is a major health problem in Europe, the United States (US), and Asia. The OHCA incidence rate per 100,000 persons has been reported to be 87 in Europe, 140.7 in the U.S., and 28.3 in Asia.[1,2] Due to recent multidisciplinary efforts, outcomes of patients with OHCA have begun to improve.[3,4] However, the extent of these improvements varies significantly depending on the region, sex, or socio-economic status (SES).[5,6]
SES is defined as a sociological and economic total measure based on educational attainment, income, employment variables, and alike.[7,8] SES has been linked to a number of health behaviors and outcomes, including cardiovascular disease, and OHCA.[9] We are well aware that patients with low SES are likely to have lower levels of education, poorer health literacy, and less access to timely and safe emergency health care, including out-of-hospital.[10] These might lead to poor outcomes for patients with a low SES. However, the characteristics of bystander intervention as well as the characteristics of the patient may influence the health outcome, but few studies have measured the SES of the bystander. Recently, several studies have reported associations between community-level SES and rates of bystander cardiopulmonary resuscitation (CPR) in patients with OHCA.[6,11–14] Community-level SES is a useful alternative indication in order to measure the bystander SES, because it is challenging to measure individual bystander SES's in the tremendously chaotic situation of an initial resuscitation intervention. Appendix.
In previous studies, associations between community-level SES and rates of bystander CPR intervention were inconsistent.[6,11–14] The reason for the inconsistency is unclear because community-level SES may have differing associations with either health outcomes for individual-level SES or subpopulations and different indicators maybe used in measuring community-level SES (e.g., income, education, or combined measure of deprivation). A systematic review and meta-analysis can help to clarify the pattern of associations between community-level SES and bystander CPR in patients with OHCA. The aim of this study was to examine the literature pertaining to the association of community-level SES and health outcomes of patients with OHCA.
2. Methods
This study followed the guidelines of Preferred Reporting Items for Systematic Reviews and Meta-Analyses.[15] Because this study design is systematic review and meta-analysis, the ethics committee or institutional review board permission is not needed.
2.1. Eligibility criteria
We included literature dealing with OHCA patients, and not limiting patient age, the environment of the cardiac arrest (e.g., witnessed status), or the location of the cardiac arrest. We included literature that presented results based on community-level SES. Factors indicating SES such as income, educational level, occupation, assets, and deprivation index were included. The exclusion criteria were:
-
(1)
studies that intended to describe methodologies or reviews of literature;
-
(2)
studies that did not report outcomes; and
-
(3)
studies that did not include a comparator group.
2.2. Outcomes
We investigated OHCA outcomes following the Utstein guidelines [16]:
-
(1)
bystander CPR and
-
(2)
survival to hospital discharge or 30-day survival.
We also reviewed neurological recovery, defined as a Cerebral Performance Category score of 1 or 2 at discharge.[17] A score of 1 indicates mild or no neurological deficit; 2 indicates moderate cerebral disability; 3 indicates severe cerebral disability; 4 indicates coma or vegetative state; and, lastly, 5 indicates brain death.
2.3. Search strategy
We searched PubMed, EMBASE, and the Cochrane Database for articles that were published before May 31, 2018, regardless of language, using Google Translate where needed. We searched both medical subject heading terms and any keywords for SES: socioeconomic, education, income, occupation, employment, and deprivation. We applied truncation symbols as part of the search strategy. Two reviewers conducted independent searches using a standard review protocol to identify all relevant peer-reviewed articles and also included articles in press, correspondence, and short reports. The 2 reviewers then independently screened the title and abstracts of articles, and if the inclusion criteria were met, we reviewed the entire article. Additionally, we conducted back-searching of article references. We selected the final list of articles used for this meta-analysis based on a consensus between the 2 reviewers. If a mismatch occurred, a third reviewer intervened to resolve the controversy.
2.4. Data extraction
The 2 reviewers conducted independent data extraction to identify the following characteristics: study name, study year, demographics of OHCA patients, contents of community-level SES, and crude numbers of OHCA patients according to SES groups. We also extracted the number of patients who received bystander CPR and survived. In addition to raw outcomes, we also extracted outcomes after adjusting odds ratios (ORs) and 95% confidence intervals (CIs) for each outcome using regression analysis when available. When studies did not demonstrate adjusted ORs for outcomes, we calculated ORs using data extracted from the studies. We resolved our disagreements by arbitration and ultimate consensus.
2.5. Quality of evidence
To evaluate the quality of evidence, we used the modified Newcastle-Ottawa Scale (NOS). The NOS is a representative tool developed for critical appraisal of observational studies, such as cohort and case-control studies.[18] This modified NOS has been adapted from the NOS for assessing the quality of cross-sectional studies for systematic review and meta-analysis.[19] The modified NOS system consists of the following 3 items based on the study design:
-
1.
Selection (Maximum 5 stars);
-
2.
Comparability (Maximum 2 stars); and
-
3.
Outcome (Maximum 3 stars).
Selection includes 4 sub-items:
-
(1)
Representativeness of the sample;
-
(2)
Sample size;
-
(3)
Non-respondents; and
-
(4)
Ascertainment of the exposure (risk factor).
Comparability does not have any sub-items.
Outcome includes 2 sub-items:
-
(1)
Assessment of the outcome and
-
(2)
Statistical test.
The 2 reviewers independently scored the quality of literature using the NOS star system, ranging from 0 to 10 stars. We resolved our disagreements by arbitration and ultimate consensus.
2.6. Statistical methods
We transformed the treatment effects to log ORs with 95% CIs, and we combined them for each outcome using a random-effects model. We assessed heterogeneity using Cochran Q test based on the corresponding I2, with I2 > 50%, indicating significant heterogeneity.[20] We conducted meta-analyses to compare the rate of bystander CPR and the rate of survival between low and high SES groups.
3. Results
3.1. Demographic findings of articles
The primary search strategy produced 1394 titles for review, and after we removed duplicates, we screened the titles of 1290 articles. We then assessed 41 abstracts of articles for eligibility and excluded 16 studies because no outcome variables were provided. We fully reviewed 25 articles and excluded an additional 14 studies due to a lack of outcome variables of SES. There is duplication of data in studies using CARES of the US and 1 article was excluded. Finally, 10 articles satisfied all inclusion and exclusion criteria.[6,11–14,21–25] There was no discrepancy between the reviewers for including or excluding studies (Fig. 1).
Figure 1.
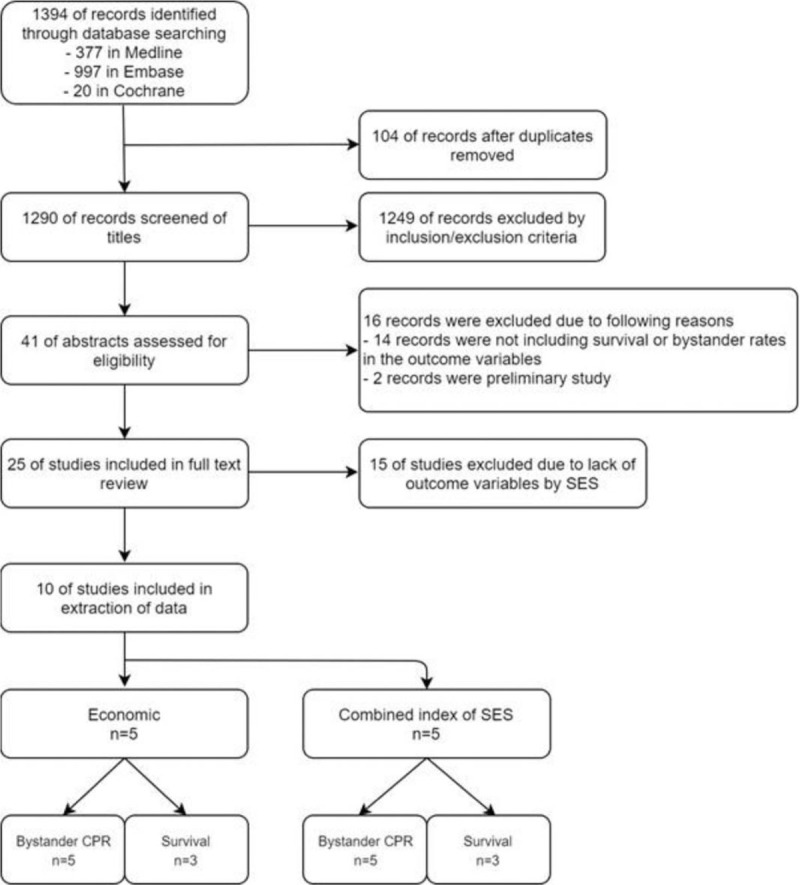
Flow of literature selection.
Table 1 summarizes the measurement of SES and results of studies in this systematic review. Although studies have been conducted in various countries, the final analysis included studies conducted in the US, Europe (England, Denmark, and France), and Asia (Republic of Korea and Taiwan). Several types of SES indicators were used in the studies included in this systematic review. Five studies used an economic indicator of community SES (such as median household income or tax-assessed property of community),[11,21,22,24,25] while 4 studies used combined indicators of communities (consisting of overcrowding, unemployment, manual occupation, and so on)[6,12,13,23] and, lastly, 1 study used the proportion of highly educated residents.[14]
Table 1.
Summary of included studies.
| Study | Region | Category of SES indicator | Measurement of SES | Summary of results |
| Clarke 2005[28] | Washington/US | Economic | Median household income of the census tract as a categorical variable with 4 values | Area-level of SES did not predict survival among patients with OHCA. |
| Sasson 2011[21] | Atlanta/US | Economic | Median household income of the census tract as a categorical variable with 5 values | Cardiac arrests in the census tracts that rank in the highest quintile of median household income were more likely to receive bystander CPR and survive than the reference group in the lowest median quintile. |
| Sasson 2012[11] | 29 sites/US | Economic | Median household income of the census tract as a categorical variable with 5 values | Patients were Less likely to receive bystander CPR if they had cardiac arrest in a neighborhood that was low-income. |
| Chiang 2014[26] | Taipei/Taiwan | Economic | Average price of real estate of the 12 administrative districts as a categorical variable with 2 values | Patients who experienced an OHCA in low-SES areas were less likely to receive bystander CPR And demonstrated worse survival outcomes. |
| Chang 2018[23] | Republic of Korea | Economic | Property tax per capita of the census tract as a categorical variable with 3 values | By property tax Per capita of the county, there were no statistical differences in their bystander CPR, survival to hospital discharge, and good neurological recovery. |
| Ahn 2011[25] | Republic of Korea | Combined | The Combined SES index was calculated using these 4 components: (1) overcrowding (more than 1.5 persons/room), (2) the percent unemployment among economically active men (between 15 and 64 yr), (3) the percent in manual occupations, (4) lack of car ownership The combined SES index of 250 administrative districts as a categorical variable with 5 values from Q1 (least deprived) to Q5 (most deprived). | Area deprivation was significantly associated with survival to hospital discharge among OHCA patients. |
| Moncur 2016[12] | North East England | Combined | The index of multiple deprivation (IMD) score is calculated from several indicators, covering economic, social and housing issues. as a categorical variable with 5 values from Q1 (least deprived) to Q5 (most deprived) | Patients in the least deprived Quintile were significantly more likely to receive bystander CPR when compared with those in the most deprived quintile. |
| Dahan 2017[13] | Paris/France | Combined | The neighborhood SES was classified in 2 categories. The neighborhood SES was calculated using 4 components: (1) median household income, (2) the percentage of blue-collar workers in the working population, (3) the unemployment rate, and (4) the percentage of adults without high school diplomas | People Collapsing with OHCA are less likely to receive bystander CPR in low SES neighborhoods. |
| Lee 2018[6] | Republic of Korea | Combined | The combined SES index was calculated using these 4 components: (1) overcrowding (more than 1.5 persons/room), (2) the percent unemployment among economically active men (between 15 and 64 yr), (3) the percent in manual occupations, (4) lack of car ownership The combined SES index of 250 administrative districts as a categorical variable with 5 values from Q1 (least deprived) to Q5 (most deprived). | The improvement of bystander CPR rate was more prominent in the highest SES communities (from 1.6% to 23.4%) than the lowest (1.6%–12.4%). Rates of survival increased in the highest communities from 3.5% to 7.8%, while smaller increases in survival were observed in the lowest communities (2.3%–5.0%). |
| Lee 2016[14] | Republic of Korea | Educational | Proportion of highly educated residents (high school graduates and higher) in a community categorized into quartile groups | OHCA patients in communities with a higher proportion of highly-educated residents were more likely to receive bystander CPR. |
∗CPR = cardiopulmonary resuscitation, NA = non applicable, OHCA = out-of hospital cardiac arrest, SES = socioeconomic status, US = United states, USD = United States Dollar.
We included 10 studies that spanned 13 years, with samples ranging from 1108 up to 34,227 patients with OHCA (Table 2). All 10 studies reported bystander CPR rates, and 6 out of 10 studies reported survival to discharge. Three out of 10 studies reported neurologic recovery. The baseline characteristics and raw outcomes of included studies are summarized in Table 2.
Table 2.
Demographic information and outcomes of included studies.
| Number of total patient | Age | Male | Witness-ed status | Shockable rhythm | Number of patient according to SES group (Low SES VS High SES) | Outcome: bystander CPR according to SES group (Low SES VS High SES) | Outcome: survival according to SES group (Low SES VS. High SES) | Outcome: good neurological recovery according to SES group (Low SES VS High SES) | ||
| Study | Region | n | Mean ± SD or Median (IQR) | (%) | (%) | (%) | n | n | n | n |
| Clarke 2005[28] | Washington/US | 1789 | 67 ± 14 | 70 | 61 | 47 | Median household income (<58,999 VS >59,000); 849 VS 853 | 324 VS 385 | 139 VS 146 | NA |
| Sasson 2011[21] | Atlanta/US | 1108 | 61.7 | 57.9 | 44.3 | 23.2 | Median household income (<42,000 VS >42,001); 687 VS 417 | 137 VS 141 | NA | NA |
| Sasson 2012[11] | 29 sites/US | 14,225 | 61.8 ± 19 | 62.7 | 42.6 | 25.4 | Median household income (<50,000 VS >50,001); 9297 VS 4,928 | 2402 VS 1666 | NA | NA |
| Chiang 2014[26] | Taipei/Taiwan | 3573 | 73.0 ± 16.0 | 62.3 | 28.3 | NA | Average price of real property (9715–6756 USD m-2 VS 5163–396 USD m-2); 1659 VS 1914 | 241 VS 376 | 69 VS 128 | 50 VS 74 |
| Chang 2018[23] | Republic of Korea | 2020 | 7 (1–16) | 66.3 | 37.2 | 6 | Property tax per capita middle & low (30–140 USD) VS high (141–700 USD); 1,334 VS 686 | 689 VS 351 | 92 VS 44 | 55 VS 20 |
| Ahn 2011[25] | Republic of Korea | 34,227 | Elderly above 65 yr old: 50.7% | 65.4 | 40.1 | 3.3 | Level of deprivation Q3–5 (most) VS Q1–2 (least); 19,860 VS. 14,367 | 245 VS 233 | 409 VS 420 | NA |
| Moncur 2016[12] | North East England | 3179 | 59.4 | 60.1 | NA | NA | Level of deprivation Q1–3 (most) VS Q4–5 (least); 1461 VS 1718 | 240 VS 383 | NA | NA |
| Dahan 2017[13] | Paris, France | 4009 | 68 ± 17 | 69.1 | 75.7 | 42.6 | SES high VS low; 3001 VS 1008 | 239 VS 538 | NA | NA |
| Lee 2018[6] | Republic of Korea | 44,118 | 69 (56–78) | 65.6 | 44.2 | 7.7 | Level of deprivation; Q5 (most) VS. Q1 (least) 19,519 VS 24,599 | 2420 VS 5756 | 976 VS 1919 | NA |
| Lee 2016[14] | Republic of Korea | 10,694 | 69 (56–78) | 67.5 | NA | 24 | Proportion of highly educated residents Q1–2 (higher) VS Q3–4 (lower); 7799 VS 2895 | 3844 VS 1268 | 915 VS 128 | 75 VS 502 |
∗All studies included are cross-sectional observation studies.
∗We extracted data from Lee 2018 study only data of 2015 year because the data duplicated with data of Ahn 2011 and Lee 2016.
∗IQR = inter-quartile range, NA = non applicable, SD = standard deviation, SES = socioeconomic status, US = United States, USD = United States Dollar, VS = versus.
3.2. Meta-analysis
Most of the included studies divided the SES into multiple (more than 3) values, while 2 studies divided the SES into only 2 values. To estimate the pool effects of SES, we rearranged the SES values in all studies dichotomously. In cases of dividing into 5 levels, the upper 3 levels were summed up as higher SES and the lower 2 levels were summed up as lower SES. In cases of dividing into 3 levels, the upper 1 level was designated as higher SES and the lower 2 levels were designated as lower SES.
We conducted meta-analysis with similar SES indicators: 5 studies using economic SES indicators and 4 studies using combined SES indicators. The remaining study used educational level as SES indicator and hence we could not conduct a meta-analysis for such.
Patients from communities with lower SES had lower odds of bystander CPR and of survival to discharge than patients in higher SES communities by economic SES indicators (bystander CPR OR: 0.67; 95% CI: 0.51–0.89; survival to discharge OR: 0.60; 95% CI: 0.35–1.02). Neurologic recovery did not have a significant association according to the economic SES indicators. We observed significant study-level heterogeneity by economic SES indicators (bystander CPR I2 = 93%; survival to discharge I2 = 94%; neurologic recovery I2 = 72%) (Fig. 2). Based on combined SES indicators, OR of bystander CPR and survival discharge in patients with lower community-level SES were lower compared with those with higher community-level SES (bystander CPR OR: 0.80; 95% CI: 0.75–0.84; survival to discharge OR: 0.76; 95% CI: 0.63–0.92). Among studies using combined SES indicators, we observed that the heterogeneity of bystander CPR was very low (I2 = 0%). The heterogeneity of survival to discharge among studies was significant (I2 = 63%) (Fig. 3).
Figure 2.
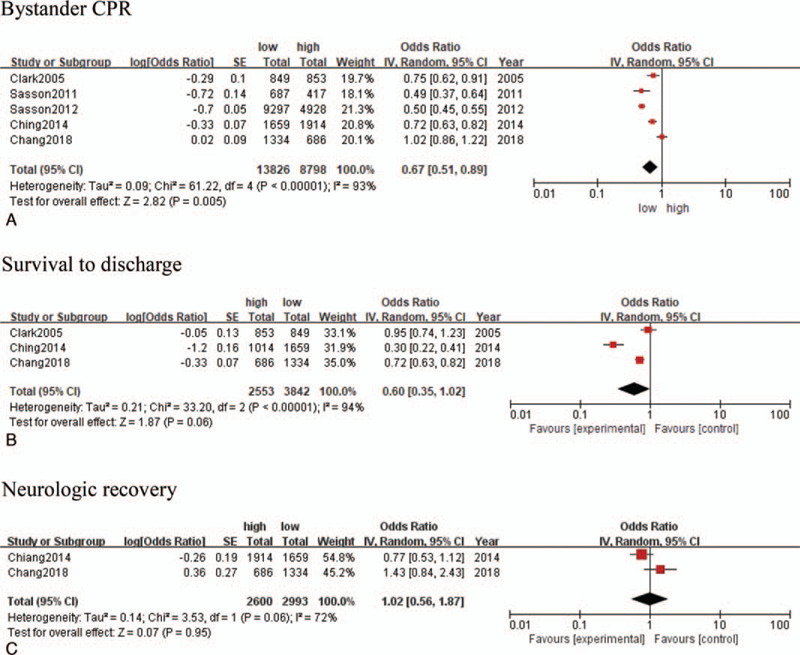
Forest plots for outcomes with low socioeconomic status (SES) communities compared with high SES communities of economic SES indicators. A: bystander CPR; B: survivals to discharge; C: neurologic recovery. CI = confidence interval, CPR = cardiopulmonary resuscitation, IV = inverse variance, SE = standard error, SES = socioeconomic status.
Figure 3.
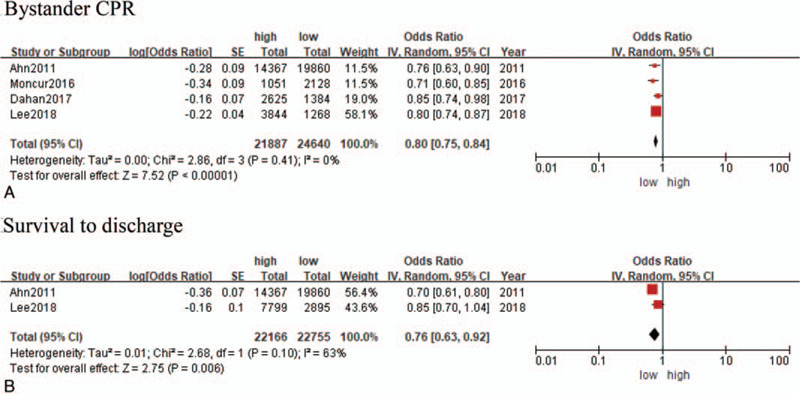
Forest plots for outcomes with low socioeconomic status (SES) communities compared with high SES communities of combined SES indicators. A: bystander CPR; B: survival to discharge. CI = confidence interval, CPR = cardiopulmonary resuscitation, IV = inverse variance, SE = standard error, SES = socioeconomic status.
3.3. Quality of evidence
Given that all 10 articles were cross-sectional observational studies, the quality of evidence— based on the modified NOS system—was high in 9 out of 10 studies (Table 3). Because all included articles were population-based studies, each earned 2 stars for representativeness of the sample. However, none of the 10 studies presented the sample size calculation. Nine of the 10 studies conducted multivariable logistic regression analysis adjusted for potential confounders (2 stars). All studies used data linkage of pre-hospital registry and hospital medical records. We regarded this data link as a blind assessment of outcome, and all studies were awarded 2 stars.
Table 3.
Quality of evidence.
| Selection | Comparability | Outcome | ||||||||
| Author/yr | Region/country | 1) Representativeness of the sample | 2) Sample size | 3) Non-respondents | 4) Ascertainment of the exposure (risk factor) | 1) Confounding factors are controlled | 1) Assessment of the outcome | 2) Statistical test | Total | Quality |
| Clarke 2005 | Washington/US | ∗∗ | – | NA | ∗ | ∗∗ | ∗∗ | ∗ | 8 | high |
| Ahn 2011 | Republic of Korea | ∗∗ | – | NA | ∗ | ∗∗ | ∗∗ | ∗ | 8 | high |
| Sasson 2011 | Atlanta/US | ∗∗ | – | NA | ∗ | ∗∗ | ∗∗ | ∗ | 8 | high |
| Sasson 2012 | 29 sites/US | ∗∗ | – | NA | ∗ | ∗∗ | ∗∗ | ∗ | 8 | high |
| Chiang 2014 | Taipei/Taiwan | ∗∗ | – | NA | ∗ | ∗∗ | ∗∗ | ∗ | 8 | high |
| Lee 2016 | Republic of Korea | ∗∗ | – | NA | ∗ | ∗∗ | ∗∗ | ∗ | 8 | high |
| Moncur 2016 | North East England/UK | ∗∗ | – | NA | ∗ | - | ∗∗ | ∗ | 6 | middle |
| Dahan 2017 | Paris/France | ∗∗ | – | NA | ∗ | ∗∗ | ∗∗ | ∗ | 8 | high |
| Chang 2018 | Republic of Korea | ∗∗ | – | NA | ∗ | ∗∗ | ∗∗ | ∗ | 8 | high |
| Lee 2018 | Republic of Korea | ∗∗ | – | NA | ∗ | ∗∗ | ∗∗ | ∗ | 8 | high |
∗NA = non applicable, UK = United Kingdom, US = United States.
∗The sample size item was not rated in all literature. When calculating the total score, it was treated as 0.
4. Discussion
In this systematic review and meta-analysis of 118,942 patients with OHCA across countries, community-level SES was associated with bystander CPR rates and the survival of patients with OHCA. We found that lower bystander CPR and survival rates were demonstrated in communities with lower SES levels compared with those communities that had higher SES levels. These results were seen not only in the meta-analysis of studies using economic SES indicators, but also in the meta-analysis of studies using combined SES indicators.
The main exposure variable in this study was community-level SES. In this systematic review and meta-analysis, 9 of the 10 studies were published since 2010, reflecting the growing interest in the disparity of bystander CPR. The mechanisms underpinning the lower bystander CPR and survival rates among lower SES communities remain speculative. One possible explanation for the disparity of bystander CPR is that there is an unequal opportunity of CPR education for those in lower SES-level communities. Previous qualitative studies reported that barriers to learning CPR in low SES residences included financial, informational, and motivational factors.[26] In our systematic review, only 1 study reported the association between level of education in community and bystander CPR.[14] This study demonstrated that OHCA patients in communities with a higher proportion of highly educated residents were more likely to receive bystander CPR. Interestingly, this disparity was widened in groups that were instructed on CPR via telephone (T-CPR). This interaction between community-level SES and T-CPR on provision of bystander CPR was revealed not only when education level was used as an indicator of community-level SES but also when it was used as an economic indicator.[23] The authors of these studies suggested tailored T-CPR programs to overcome these disparities. Additionally, it is worth noting that community-level SES reflects a disparity of access to health care resources. The studies included in our systematic review also provided results for this association. Studies in the U.S., Korea, and Taiwan showed disparities in emergency medical services (EMS) response time according to community-level SES, with higher SES communities seeing faster EMS response times.[23,24,27] In contrast, results of a study in Paris showed no association between community-level SES and time intervals from call to automated external defibrillator application. Authors suggested the standardized EMS response in Paris could attenuate SES disparity in patients with OHCA. However, it did not show any trend depending on the type of SES indicator.
Although which subpopulations may be especially vulnerable for SES disparity would be an interesting research question, there were few studies exploring different associations according to age or sex. One study in this systematic review included a pediatric patient. This study showed no association between community-level SES and provision of bystander CPR and neurologic recovery. These results are interesting because they are unique among the 10 studies included in this study. It may be controversial that these results are due to the characteristics of pediatric patients. A previous study that investigated whether bystander CPR provision differed according to the levels of education and income of parents of pediatric patients reported that the bystander CPR rate was higher in the higher SES group compared with those in the lower SES group.[28]
The main strengths of this meta-analysis were the large number of participants in the studies we included and the diversity of study populations to explore possible sources of heterogeneity. The studies included in this meta-analysis used various SES scales based on country-specific economic and educational realities. Nonetheless, we do not expect such variation to have materially influenced our meta-analysis results. In addition, 6 of the 10 studies demonstrated a dose-response association between SES level and the provision of bystander CPR and patient survival. These dose-response associations support a causal inference between SES and outcome variables.
5. Limitations
There are a few limitations to this study. First, the reviewed studies used observational data, which may include reporting bias. While we did not restrict our research to particular countries, studies included in this meta-analysis were mostly conducted in high-income countries. We cannot preclude the possibility that having more data from low- and middle-income countries may have altered our findings. Second, we calculated pooled effects using recalculated crude OR, because we rearranged SES categories and could not use adjusted OR presented in each study. Third, the heterogeneity was very high for each meta-analysis. However, we postulated that differences in EMS systems and differences of SES gradients of the regions studied could result in significant heterogeneity in the outcomes.[21] Finally, the number of studies from which the data was extracted was small. This was due to the lack of a study with minimal data for meta-analysis among the studies included in this study.
6. Future directions
In order to improve the health outcomes among patients with OHCA, further community-based interventions for narrowing the gaps in SES are warranted.
7. Conclusion
Our systematic review and meta-analysis demonstrated the pooled effects of community-level SES on the provision of bystander CPR and survival among patients with OHCA.
Author contributions
The conception and design of the study, OR analysis and interpretation of data: Dr Lee, and Dr Ahn; Drafting and critical revision for important intellectual content: Dr Lee, Dr Cha, and Dr Ahn; Final approval of the version to be submitted: all authors.
Conceptualization: Sanghun Lee, Ki Ok Ahn.
Data curation: Sanghun Lee, Ki Ok Ahn, Myeong-il Cha.
Formal analysis: Sanghun Lee, Ki Ok Ahn, Myeong-il Cha.
Investigation: Sanghun Lee, Ki Ok Ahn, Myeong-il Cha.
Methodology: Sanghun Lee, Ki Ok Ahn.
Project administration: Ki Ok Ahn.
Software: Sanghun Lee.
Supervision: Ki Ok Ahn.
Validation: Sanghun Lee, Ki Ok Ahn, Myeong-il Cha.
Visualization: Sanghun Lee.
Writing – original draft: Sanghun Lee.
Writing – review & editing: Ki Ok Ahn.
Supplementary Material
Footnotes
Abbreviations: CI = confidence interval, CPR = cardiopulmonary resuscitation, EMS = emergency medical services, NOS = Newcastle-Ottawa Scale, OHCA = out-of hospital cardiac arrest, OR = odds ratios, SES = socioeconomic status, US = United states.
How to cite this article: Lee S, Ahn KO, Cha Mi. Community-level socioeconomic status and outcomes of patients with out-of-hospital cardiac arrest: A systematic review and meta analysis. Medicine. 2021;100:3(e24170).
The authors have no funding and conflicts of interest to disclose.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Supplemental digital content is available for this article.
References
- [1].Gräsner JT, Lefering R, Koster RW, et al. EuReCa one—27 nations, one Europe, one registry: a prospective one month analysis of out-of-hospital cardiac arrest outcomes in 27 countries in Europe. Resuscitation 2016;105:188–95. [DOI] [PubMed] [Google Scholar]
- [2].Berdowski J, Berg RA, Tijssen JGP, et al. Global incidences of out-of-hospital cardiac arrest and survival rates: systematic review of 67 prospective studies. Resuscitation 2010;81:1479–87. [DOI] [PubMed] [Google Scholar]
- [3].Chan PS, McNally B, Tang F, et al. CARES Surveillance Group. Recent trends in survival from out-of-hospital cardiac arrest in the United States. Circulation 2014;130:1876–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Kim YT, Shin SD, Hong SO, et al. Effect of national implementation of Utstein recommendation from the global resuscitation alliance on ten steps to improve outcomes from out-of-hospital cardiac arrest: a ten-year observational study in Korea. BMJ Open 2017;7:e016925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Girotra S, van Diepen S, Nallamothu BK, et al. Regional variation in out-of-hospital cardiac arrest survival in the United States. Circulation 2016;133:2159–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Lee SY, Song KJ, Shin SD, et al. A disparity in outcomes of out-of-hospital cardiac arrest by community socioeconomic status: a ten-year observational study. Resuscitation 2018;126:130–6. [DOI] [PubMed] [Google Scholar]
- [7].Krieger N, Chen JT, Waterman PD, et al. Geocoding and monitoring of US socioeconomic inequalities in mortality and cancer incidence: does the choice of area-based measure and geographic level matter? The public health disparities geocoding project. Am J Epidemiol 2002;156:471–82. [DOI] [PubMed] [Google Scholar]
- [8].Cabrera-Barona P, Murphy T, Kienberger S, et al. A multi-criteria spatial deprivation index to support health inequality analyses. Int J Health Geogr 2015;14:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Kaplan GA, Keil JE. Socioeconomic factors and cardiovascular disease: a review of the literature. Circulation 1993;88:1973–98. [DOI] [PubMed] [Google Scholar]
- [10].Heo J, Oh J, Lee HY, et al. Neighborhood-level and individual-level socioeconomic status and self-reported management of ischaemic heart disease: cross-sectional results from the Korea health examinees study. BMJ Open 2019;9:e021577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Sasson C, Magid DJ, Chan P, et al. Association of neighborhood characteristics with bystander-initiated CPR. N Engl J Med 2012;367:1607–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Moncur L, Ainsborough N, Ghose R, et al. Does the level of socioeconomic deprivation at the location of cardiac arrest in an English region influence the likelihood of receiving bystander-initiated cardiopulmonary resuscitation? Emerg Med J 2016;33:105–8. [DOI] [PubMed] [Google Scholar]
- [13].Dahan B, Jabre P, Karam N, et al. CARES Surveillance Group. Impact of neighbourhood socio-economic status on bystander cardiopulmonary resuscitation in Paris. Resuscitation 2017;110:107–13. [DOI] [PubMed] [Google Scholar]
- [14].Lee SY, Ro YS, Shin SD, et al. Interaction effects between highly-educated neighborhoods and dispatcher-provided instructions on provision of bystander cardiopulmonary resuscitation. Resuscitation 2016;99:84–91. [DOI] [PubMed] [Google Scholar]
- [15].Shamseer L, Moher D, Clarke M, et al. PRISMA-P Group. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ 2015;350:g7647. [DOI] [PubMed] [Google Scholar]
- [16].Perkins GD, Jacobs IG, Nadkarni VM, et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update of the Utstein resuscitation registry templates for out-of-hospital cardiac arrest: a statement for healthcare professionals from a task force of the International Liaison Committee on resuscitation (American Heart Association, European Resuscitation Council, Australian and New Zealand Council on Resuscitation, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Council of Southern Africa, Resuscitation Council of Asia); and the American Heart Association Emergency Cardiovascular Care Committee and the Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation. Circulation 2015;132:1286–300. [DOI] [PubMed] [Google Scholar]
- [17].Edgren E, Hedstrand U, Kelsey S, et al. Assessment of neurological prognosis in comatose survivors of cardiac arrest. BRCT I study group. Lancet 1994;343:1055–9. [DOI] [PubMed] [Google Scholar]
- [18].Wells GA, Shea B, O’connell D, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Available from: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. [Google Scholar]
- [19].Herzog R, Álvarez-Pasquin MJ, Díaz C, et al. Are healthcare workers’ intentions to vaccinate related to their knowledge, beliefs and attitudes? A systematic review. BMC Public Health 2013;13:154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Cochran WG. The combination of estimates from different experiments. Biometrics 1954;10:101–29. [Google Scholar]
- [21].Sasson C, Keirns CC, Smith DM, et al. Examining the contextual effects of neighborhood on out-of-hospital cardiac arrest and the provision of bystander cardiopulmonary resuscitation. Resuscitation 2011;82:674–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Chang I, Ro YS, Shin SD, et al. Association of dispatcher-assisted bystander cardiopulmonary resuscitation with survival outcomes after pediatric out-of-hospital cardiac arrest by community property value. Resuscitation 2018;132:120–6. [DOI] [PubMed] [Google Scholar]
- [23].Ahn KO, Shin SD, Hwang SS, et al. Association between deprivation status at community level and outcomes from out-of-hospital cardiac arrest: a nationwide observational study. Resuscitation 2011;82:270–6. [DOI] [PubMed] [Google Scholar]
- [24].Chiang WC, Ko PC, Chang AM, et al. Bystander-initiated CPR in an Asian metropolitan: does the socioeconomic status matter? Resuscitation 2014;85:53–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Clarke SO, Schellenbaum GD, Rea TD. Socioeconomic status and survival from out-of-hospital cardiac arrest. Acad Emerg Med 2005;12:941–7. [DOI] [PubMed] [Google Scholar]
- [26].Sasson C, Haukoos JS, Bond C, et al. Barriers and facilitators to learning and performing cardiopulmonary resuscitation in neighborhoods with low bystander cardiopulmonary resuscitation prevalence and high rates of cardiac arrest in Columbus, OH. Circ Cardiovasc Qual Outcomes 2013;6:550–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Moon S, Bobrow BJ, Vadeboncoeur TF, et al. Disparities in bystander CPR provision and survival from out-of-hospital cardiac arrest according to neighborhood ethnicity. Am J Emerg Med 2014;32:1041–5. [DOI] [PubMed] [Google Scholar]
- [28].Rajan S, Wissenberg M, Folke F, et al. Out-of-hospital cardiac arrests in children and adolescents: incidences, outcomes, and household socioeconomic status. Resuscitation 2015;88:12–9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


