Supplemental Digital Content is available in the text
Keywords: amputation, lower limb, participation., prognosis, walking
Abstract
Lower limb amputation (LLA) is still a health issue requiring rehabilitation and long-term care even in industrial societies. Several studies on subjects with LLA have been focused on the efficacy of rehabilitation and factors influencing the use of prosthesis. However, literature data on the recovery of ability to walk outdoors, and thus to participate in social life in this population is limited.
To investigate potential correlations between socio-demographic and clinical factors, and the use of the prosthesis for indoor and/or outdoor walking referred to as community ambulation (CA) in subjects with LLA.
An observational cohort study on 687 LLA subjects was conducted. Socio-demographic and clinical characteristics of 302 subjects who received similar rehabilitative treatment with respect to the standard protocol were collected by a telephone survey with a structured questionnaire. The CA recovery, in terms of patient's autonomy and participation, assessed by Walking Handicap Scale, was considered as the main outcome.
The univariate analysis demonstrated statistical significant positive correlation between CA and gender (χ2 = 3.901, P = .048); amputation level (χ2 = 24.657, P < .001); pre-LLA (χ2 = 6.338, P = .012) and current work activity (χ2 = 25.192, P < .001); prosthesis use (χ2 = 187.037, P < .01); and time from LLA (r = 0.183, P < .001); increasing age was negatively correlated with the outcome (r = –0.329, P < .001), while pain intensity was not significant. Being male (75.4%); trans-tibial (TT) amputation level (9.79%); working before (3.81%) and after LLA (7.68%); and the prosthesis use (24.63%) increased the probability of CA recovery. Multivariate binary logistic regression analysis confirmed that the prosthesis use (P < .001) and TT amputation level (P = .042) are predictors of a positive outcome (Walking Handicap Scale 4–6).
These findings highlight the importance of the use of prosthesis in people with LLA for the restoration of a good capacity of participation (CA), especially in subjects with TT amputation level. The identification of predictive factors may help tailor-made rehabilitation approaches addressing an earlier reintegration to social life.
1. Introduction
Lower limb amputation (LLA) is still a health issue requiring rehabilitation and long-term care,[1] despite the great advances in medicine and prevention of accidents in high welfare industrial societies with significant reductions in the incidence of LLA in specific at-risk populations.[2]
Several systematic reviews and epidemiologic data on LLA have been focused on the efficacy of rehabilitation in terms of the use of prosthesis[1–4] in order to compensate for the functional loss[5,6] within a rehabilitation program aimed at recovery of standing and walking ability while wearing a prosthesis.[7] Literature reports dissimilar data on percentages of amputees who successfully use the artificial limb after rehabilitation, ranging from 5%[8] to 100%[9,10] possibly related to what is meant as successful rehabilitation outcome: that is, living at home autonomously,[11] having a good level of independence,[12] Activities of daily living,[13,14] mobility,[15] and participation.[11] However, the gold standard of the rehabilitation process remains the restoration of an adequate level of functioning and participation in an indoor and/or outdoor activity, referred to as community ambulation (CA). Literature data has not sufficiently addressed this aspect in individuals with LLA.
Moreover, differences in surgical procedures, postoperative care, prosthesis manufacture, rehabilitation strategies, and geographic origin in these studies, lead to a vast heterogeneity of the samples and, as a result, difficult comparison among various observational studies on large samples of LLA[16–18] as well as in epidemiological studies.[4,19,20] Indeed, studies on return to work or social activity in people with LLA include many confounding factors which reduce the identification of the rehabilitation outcome predictors. Therefore, studies on pivotal socio-demographic (gender, age, working status) and clinical parameters (such as side, pain, and amputation level) should be carried out by minimizing the effect of confounding variables such as different rehabilitation programs and/or prosthesis manufacture, which could influence the outcome of LLA rehabilitation. To our best knowledge, few population-based studies have been conducted in a well-defined geographical area, while minimizing these factors.[21]
Due to the lack of data on the CA in subjects with LLA after prosthesis and the several confounding factors generated by the vast heterogeneity of the samples in the studies so far published, there is a need for well-conducted and large-sample studies on this topic. Therefore, the aim of this study was to investigate potential correlations between socio-demographic and clinical factors and the use of the prosthesis for indoor and/or outdoor walking, in terms of participation, referred to as CA in subjects with LLA,[22] while minimizing confounding factors. This outcome could present a picture of the global status of activities and participation in LLA subjects, since the loss of functional mobility directly impact the reduction of participation in these subjects.[23] As a result, it could provide further indications on the usefulness of CA as a predictive factor and to identify subgroups of subjects that may better respond to a tailored rehabilitation to walk independently.
2. Methods
An observational study was conducted on a database of 687 LLA subjects who received the same prosthesis manufacture and underwent homogeneous clinical prosthesis optimization and treatment with respect to a standard rehabilitation protocol.[25] The database was applied in this study compatibly with the norms of the privacy guarantee according to the regulations of the national law (G.U. n. 190 of 14/08/2008).
Subjects were selected based on the following inclusion criteria: patients referred to the same Orthotic Prosthetic Centre for LLA prosthesis; prosthesis clinical optimization in the last decades to 2017; age between 18 and 80 years; unilateral amputation; LLA at the trans-tibial (TT) or trans-femoral (TF) level; neoplastic, traumatic or vascular origin; informed consent to participate to the project and to answer to a telephone interview.
Exclusion criteria considered for subjects selection were: upper limb amputation; bilateral amputations; foot or hip amputations; incomplete data available in the database; postsurgery wound-related clinical implications in the first year after the last intervention; lack of informed consent.
Out of 687 records, 302 subjects satisfied the inclusion/exclusion criteria (Fig. 1 Consort diagram). The subjects were interviewed via telephone by a trained operator, not aware of the purpose of the study and not involved in data processing.
Figure 1.
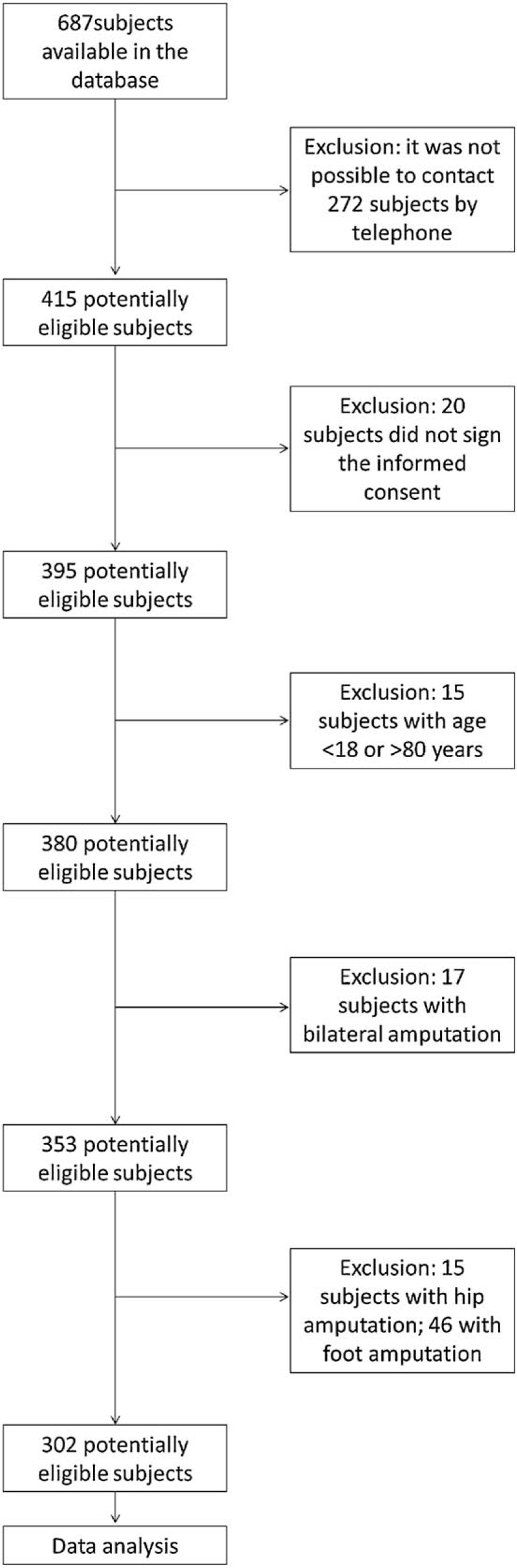
Flowchart of the study procedure.
The telephone survey was based on a questionnaire “Supplemental Digital Content (Appendix 1)” exploring the following data:
-
(1)
socio-demographic status before and after amputation;
-
(2)
clinical aspects related to amputation;
-
(3)
autonomy and participation according to the criteria of the Walking Handicap Scale (WHS).[26]
The WHS is a simple tool that could be administered also through a brief telephone interview, thus assessing the participation as recommended by the International Classification of Functioning, disability and health (ICF).[27] Specifically, CA was defined as “independent mobility outside home, which includes the ability to confidently deal with uneven terrain, private streets, rural roads, shopping centers, and public transport.”[22] The WHS identifies 6 functional categories and 3 community walk performance groups, graduated from most-limited community walkers to community walkers. The scale includes ecological tasks such as going to a medical appointment, visiting friends, shopping, going to church or to a restaurant, and traveling.[28,29] Outcomes were considered positive if the WHS scores between 4 and 6, thus indicating the ability to walk autonomously (or with assistance) outdoor and/or in the community. Outcomes were considered negative with a WHS score between 1 and 3.
The following factors were identified as independent variables, so as prognostic indicators: age; gender; amputation level; amputation side; cause of amputation; time from last surgery; pre-LLA working status (yes/no); current working status (yes/no); pain intensity, assessed by Numeric Rating Scale (NRS); use of the prosthesis (yes/no).
In this study, the etiology (vascular or traumatic) was not taken into account, since recent literature suggests that etiology does not affect the return to work after LLA.[30]
The study was approved by the local Ethics Committee on July 08, 2018 with the number 07/2018.
2.1. Statistical analysis
The statistical analysis was conducted using SPSS Statistics for Windows, Version 26.0. The univariate analysis was executed considering mean and standard deviation values for continuous variables, and all categorical variables were presented by %. Bivariate correlations were evaluated with Pearson's correlation for continuous variables, while the chi-square test χ2 was applied for categorical variables.
In order to investigate how dependent variables may influence changes in the independent variable, a linear multiple regression model was applied, with the following formula:
Community Ambulation (CA)=β0 + β1∗age + β2∗gender + β3∗amputation level + β4∗time from amputation + β5∗side of amputation + β6∗pre amputation activity + β7∗post amputation activity + β∗pain intensity + β∗prosthesis use + −ε
Multivariable binary logistic regression analysis and multilinear regression were performed to determine the relation between WHS and socio-demographic and clinical characteristics. The multivariable binary logistic regression shows the results in odds ratio (OR) of the predictive model considering the positive outcome of CA (WHS 4–6). Consequently, the relation between CA and every single independent variable was analyzed to understand the potential positive or negative effect of each variable on the recovery of CA capacity.
A 2-sided significance level at 0.05 was used for all statistical tests.
3. Results
Data from 302 people with LLA were analyzed (Table 1). The sample's mean age was 60.6 ± 14.2 years old, of which 240 (79.5%) males (59.8 ± 14.2 years old) and 62 (20.5%) females (63.4 ± 18.9 years old), while the mean values of the time from the last LLA surgery was 2.04 ± 1.68 years.
Table 1.
Demographic and clinical profile of the sample (n = 302).
| Total sample n = 302 | |
| Age (yrs), mean ± d | 60.6 ± 14.2 |
| Gender Male, n (%) | 240 (79.5) |
| Amputationlevel, n (%) | |
| -TF | 148 (49) |
| -TT | 154 (51) |
| Time from the last LLA (years), mean ± d | 2.04 ± 1.68 |
| Amputation side dx, n (%) | 136 (45) |
| Working status | |
| -declared to work before LLA, n (%) | 150 (49.7) |
| -declared to work currently, n (%) | 77 (25.5) |
| Presence of pain (Yes), n (%) | 205 (67.9) |
| Pain intensity (NRS), mean ± d | 6.78 ± 2.13 |
| Use of prosthesis (Yes), n (%) | 241 (79.8) |
| WHS - Community ambulation (unable to walk), n (%) | 82 (27.2) |
From the whole sample, 49% of subjects presented TT-amputation level and 51% TF-amputation level; 55% left side amputation; 27.2% declared to be unable to walk in the community; 49.7% stated they had worked before LLA, whereas only 25.5% were employed also after amputation. The 79.8% of subjects confirmed to use regularly the prosthesis. The pain was reported by 67.9% of the subjects and the mean pain intensity (NRS) perceived by amputees was 6.78 ± 2.13: of which 40.5% associated with phantom limb; and 14.6% with stump pain; whereas 44.9% declared to suffer both phantom limb and stump pain (Table 1).
The bivariate correlation analysis revealed that increasing age negatively (r = –0.329, P < .001), and increasing time from last LLA surgery (r = 0.183, P < .001) positively affected the CA recovery, while pain intensity (r = –0.120, P = .086) had no significant effect on the outcome. Being male, the TT rather than TF amputation level, the pre and post LLA working activity, and the regular use of prosthesis had a significant positive impact on CA recovery, but there is no significant correlation between the amputation side and the outcome (Table 2).
Table 2.
Association between categorical independent variables and community ambulation.
| Community ambulation | ||
| χ2 | P value | |
| Gender | 3.901 | .048∗ |
| Amputation level | 24.657 | <.01∗∗ |
| Amputation side | 1.122 | .290 |
| Pre-LLA working status | 6.338 | .012∗ |
| Current working status | 25.192 | <.01∗∗ |
| Use of prosthesis | 187.037 | <.01∗∗ |
The multiple linear regression model, confirmed by statistical significance, represented a good estimate (R-squared adj = 0.657, P = .014) of the relationship between the dependent variable and independent variables (Table 3). The multiple regression model (stepwise method) as set up explained about 66% of the variability of CA, and the goodness of fit explained by the model (F = 80.052, P < .001) was significant. The standardized regression coefficients showed that the CA, in correspondence to the continuous variables, increased by a unit for each year of time since the last surgery (β = 0.106,P = .014); while decreased by 0.115 for each year of age (β = –0.115, P = .014). About the dichotomized variables, the relation results highly significant for subjects who use regularly the prosthesis (β = 0.683, P < .001); for those who currently work (β = 0.125 P = .009), and for subjects with TT amputation level (β = 0.101 P = .017). Gender (P = .608), amputee side (P = .757), presurgery activity (P = .271), and pain intensity (measured by NRS; P = .338) were not significant.
Table 3.
Results by multiple linear regression model for the Walking Handicap Scale∗.
| Community ambulation | [R2adj = 65.7%] | ||
| Independent variables | Coefficient β | 95% CI | P value |
| Age (yrs) | −0.115 | −0.03, −0.003 | .014 |
| Gender (female reference) | 0.022 | — | .608 |
| Amputation level (TF reference) | 0.101 | 0.073–0.728 | .017 |
| Time from the last LLA | 0.106 | 0.028–0.243 | .014 |
| Amputation side (right reference) | −0.013 | .757 | |
| Pre-LLA working status | 0.046 | — | .271 |
| Current working status | 0.125 | 0.153–1.059 | .009 |
| Pain intensity (NRS) | 0.041 | — | .338 |
| Use of prosthesis | 0.683 | 2.721–3.516 | <.001 |
| Constant | 1.984 | 1.030–2.937 | <.001 |
The results by Logistic regression model (χ2 = 156.672 P < .001) are shown in Table 4. The OR further confirmed a positive influence of the following independent variables (ie, WHS: 4–6): amputation level, meaning that subjects with TT level of amputation level are 3.213 (P = .042) times more likely to walk than those with TF level; and prosthesis users (ie, who use regularly the prosthesis) are 440 (P < .001) times more likely to walk than prosthesis nonusers.
Table 4.
Results by the multivariable binary logistic regression analysis∗: Coefficient, standard error (SE), odds ratios (OR), P-values and 95% confidence intervals (CI).
| Independent variables | Coefficien† | SE | OR‡ | P-value | 95% CI |
| Age§ | −0.015 | 0.02 | 0.98 | .487 | 0.94–1.03 |
| Gender (Male) | −0.18 | 0.69 | 0.83 | .790 | 0.21–3.22 |
| Amputation level (TT) | 1.17 | 0.57 | 3.21 | .042 | 1.04–9.91 |
| Time from the last LLA§ | 0.34 | 0.22 | 1.41 | .118 | 0.92–2.16 |
| Amputation side (Left) | −0.03 | 0.54 | 0.97 | .949 | 0.33–2.80 |
| Pre-LLA working status | 0.99 | 0.57 | 2.70 | .082 | 0.88–8.28 |
| Current working status | 0.62 | 0.88 | 1.86 | .480 | 0.33–10.34 |
| Pain intensity|| | 0.07 | 0.13 | 1.07 | .585 | 0.83–1.38 |
| Use of prosthesis | 6.08 | 1.11 | 440.16 | <.001 | 50.01–3873.45 |
| Constant | −5.03 | 2.20 | 0.007 | .023 |
Figure 2 was reported in order to explicitly show the difference of CA recovery rate (%) in subjects with TT amputation with respect to their peers with TF amputation by the use of prosthesis.
Figure 2.
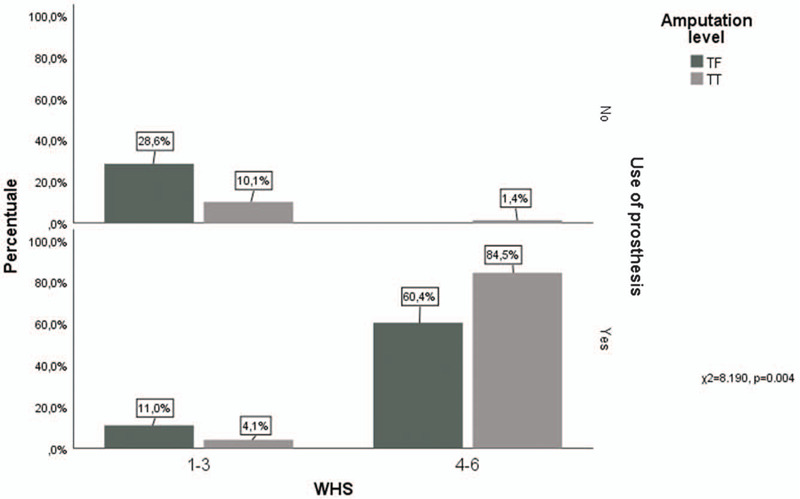
Effect of amputation level associated with the use of prosthesis on community ambulation.
4. Discussion
This observational study was designed to analyze the socio-demographic and clinical characteristics of subjects with LLA, who received a standardized rehabilitation treatment, in order to identify potential inferences of these characteristics on indoor and/or outdoor walking.
To this aim, a database of 302 subjects was analyzed by a linear and logistic regression model to explore all potential relation between the dependent variable (WHS) and every independent variable as predictive factors for CA recovery.[32]
Systematic reviews and epidemiologic data on LLA showed controversial outcomes related to the efficacy of rehabilitation in terms of wearing and use of the prosthesis. This matter may be due to the different definitions of the terms “rehabilitation goals” and quality of life (QoL).[1–4,33] In this study, rehabilitation is defined as “successful” when persons with LLA regain the ability to walk with a prosthesis, being independent in activities of daily living. In other words, rehabilitation is considered “successful,” when subjects are able to walk autonomously, so as to participate in social activities. Furthermore, regaining the walking ability is critical in order to prevent metabolic bone disease which can be elicited by immobility.[34] Thus, CA can be considered as a reliable indicator of successful rehabilitation since it requires not only fine motor control skills but also the cognitive ability to regulate motor control with various auditory and visual environmental stimuli. The CA is also influenced by several environmental factors (ie, the type of terrain, the presence of sudden obstacles) and by the ability to manage multiple attention tasks.[22,30]
Another possible bias in the data so far presented in the literature, is the extreme variability in postoperative care, prosthesis manufacture, rehabilitation strategies, and geographic origin.[4,19,20] The data observed in this study, refined from variables such as different prosthesis manufacture, rehabilitation strategies, optimization of the prosthesis, and geographic origin, confirmed data represented in existing literature relating to age, gender, and level of amputation.[33,35]
The most relevant and interesting data emerging from the present study is related to the neutral effect of pain and the amputation side on the rehabilitation outcome. These data are partly not in accordance with the literature since these factors may appear to be negative indicators of the walking ability restoration.[36,37] Conversely, from our findings, they were not revealed as determining factors in the recovery of the ability to walk outdoors (WHS:4–6). Alternatively, the TT level of amputation, rather than TF, as well as the regular use of the prosthesis was found highly protective for a positive outcome according to previous studies.[36–38]
Indeed, the presence of pain and its intensity per se does not seem to influence the recovery of CA. In this context, pain intensity has been shown by other authors to be critical only in association with other variables such as the level of amputation and age.[38] Moreover, in the amputee, phenomena such as the phantom limb and the associated phantom limb pain are related to the extension of the cortical area involved in the differentiation:[36] therefore a TF amputation has a cortical area more exposed to a reorganization than a TT one, and consequently to the development of the prosthesis. It is also been ascertain that, possibly with the same cortical reorganizing mechanism, pain tends to decrease over time and therefore long-term amputees tend to suffer less from the impact of pain on walking ability.[36]
The correlation between the amputation side and the outdoor walking was understudied in the literature. However, our results did not find it as an influencing factor for the recovery of CA. This finding is in contrast with a study by Kerstein et al[37]: they showed that subjects who lost the left lower extremity tended to make better progress in walking ability recovery, than those who required a prosthesis for the right leg, achieving maximum benefits from rehabilitation in less time.[38] More recently, in a selected population of Paralympics amputees short track sprinters, no differences were noted in their performances relating to the amputation side.[39] Although this fact could be linked to their athletic preparation, it is consistent with our findings. A very recent study found an asymmetrical reorganization of the motor cortex in patients with phantom limb following a unilateral traumatic LLA, showing no association with pain intensity nor differences regarding the amputation side.[40] Our data however extend this concept to a general population with LLA, pointing out the need for further studies on the neurophysiologic possible changes related to the amputation side after the LLA.
Our data show that while increasing time from amputation has a positive impact on the CA recovery, increasing age negatively affects this outcome. Recently, the cosmetic prosthesis was considered part of a “successful rehabilitation” in elderly amputees.[35] Although age independently is not determinant for the possibility of prosthetic rehabilitation, it turns important if a “successful rehabilitation” means an improvement of outdoor walking in terms of QoL and participation.[41] As assumed by Burger et al, the ability to engage in community activities is age-related. Hence, persons who underwent an LLA need much longer time to regain a discrete functional capacity compared to their younger peers. While the independence level achieved is related not only to the age but also to the time span since amputation.[42] In fact, the mobility limitations could occur later in the life of people who were younger at the amputation time.
Despite the literature did not indicate gender difference among amputees, some gender differences emerge in terms of age (eg, men were younger than women at the amputation time) and the amputation level (eg, men were significantly more likely to have a foot amputation whereas the incidence of thigh amputation was higher in women).[43] This could justify the slight difference observed by our study in favor of males for a better recovery of CA. However, this has been associated with the difficulty of readaptation to changes in role, often in relationship to the responsibilities in the family, especially with the partner and also in terms of body image.[23,44]
Although the worldwide statistics on exact amputation level incidence are very difficult to establish, the results of the present study confirmed that persons with TT amputation had a better prognosis compared to ones with TF, as stated also by Esquenazi et al.[45] The surgical technique with revascularization procedures allows preservation of the knee, which decreases energy demand and can give to elderly the opportunity to better benefit from gait rehabilitation. The more proximal the amputation, the more energy is required from the cardiovascular and pulmonary systems for prosthetic gait.[36] In accordance with these findings, a recent retrospective study showed that amputation aetiology did not impact on return to work whereas TF amputation level had a negative prognostic effect on return to work after LLA, which in turn has been detected by our results to have a direct positive effect on CA recovery.[31]
People who worked before and/or returned to work after LLA have a higher probability of recovering CA since they have a higher tendency to return to participation in social activities. These two factors could be also considered as age-related factors. In our sample, young age is a positive indicator for CA recovery and, consequently, the work activity both before and/or after LLA has a positive effect on CA restoration. Though it is assumable that the younger a person is, the more likely she/he is to have worked before and/or more motivated is to return to work after LLA, thus having a better chance to recover the CA. In a recent study on the prevalence of anxiety and depression among lower limb amputees, the authors showed how these factors were related to employment, supporting our data related to the importance of pre-LLA working status.[46] Indeed, this disclosure is quite critical as most authors found that among those who returned to work a range of 22% to 67% of subjects retained the same occupation as before amputation, while the rest had to change the type of job activity and/or employment form to part-time. Despite the return to work depends on general factors relating to the type of work activity and organizational policies, it remains directly dependent on the ability to walk outdoors after LLA, as well as confirmed by our data.
4.1. Study limitations
This study has been conducted on a selected large sample of persons with unilateral LLA, thus the findings must not be generalized. However, a selected sample (standard rehabilitation protocols) and minimizing confounding factors by considering similar prosthesis manufacture kept down the influence of such factors on the outcome, thus providing more homogenous information. A recent trial in TT amputees demonstrated how kinematic and kinetic measures during the over-ground gait required an increased functionality, in terms of energy return, after changing the prosthesis.[47] As a result, the data from this study suggests future prospective and even better international multicentre studies in order to confirm these findings on larger samples with different cultural aspects.
5. Conclusions
The findings of this observational cohort study confirm the positive correlation between the recovery of Community Ambulation capacity and the amputation techniques aimed at preserving the knee level (TT amputation), with a physiological Q angle (an index of the vector for the combined pull of extensor mechanisms and patellar tendon),[48] compared to Trans-Femoral amputations. Our data highlight the importance of the regular use of prosthesis in people with LLA in order to have a better chance to restore a good level of participation in terms of ability to walk indoors and outdoors. These indicators are considerable in order to predict a targeted prognosis and better provide a tailored rehabilitation program.
Identification of subgroups of subjects with LLA who may have a better chance to recover the CA and return to participate autonomously in social contexts, based on specific socio-demographic and clinical characteristics could lead clinicians to plan a more effective rehabilitative program.
Special attention should be paid to subject with fewer opportunities to recover the walking ability in terms of participation, offering psychological supports, and ensuring a QoL supported by social services. This approach may reduce the economic and social burden of LLA subjects’ management.[24,31]
Author contributions
Conceptualization: Carlo Damiani, Sanaz Pournajaf, Marco Franceschini, Roberto Casale.
Data curation: Sanaz Pournajaf, Michela Goffredo, Gabriele Denza, Benedetta Rosa.
Formal analysis: Michela Goffredo, Stefania Proietti, Benedetta Rosa.
Investigation: Sanaz Pournajaf, Gabriele Denza, Marco Franceschini.
Methodology: Sanaz Pournajaf, Stefania Proietti, Marco Franceschini, Roberto Casale.
Project administration: Marco Franceschini.
Software: Stefania Proietti.
Supervision: Carlo Damiani, Marco Franceschini, Roberto Casale.
Validation: Marco Franceschini.
Visualization: Carlo Damiani, Sanaz Pournajaf, Michela Goffredo, Stefania Proietti, Gabriele Denza, Benedetta Rosa, Marco Franceschini, Roberto Casale.
Writing – original draft: Sanaz Pournajaf, Marco Franceschini, Roberto Casale.
Writing – review & editing: Sanaz Pournajaf, Michela Goffredo, Marco Franceschini, Roberto Casale.
Supplementary Material
Footnotes
Abbreviations: ADL = activities of daily living, CA = community ambulation, LLA = lower limb amputation, NRS = Numeric Rating Scale, OR = odds ratio, QoL = quality of life, TF = trans-femoral, TT = trans-tibial, WHS = Walking Handicap Scale.
How to cite this article: Damiani C, Pournajaf S, Goffredo M, Proietti S, Denza G, Rosa B, Franceschini M, Casale R. Community ambulation in people with lower limb amputation: an observational cohort study. Medicine. 2021;100:3(e24364).
This project was partially funded by the Italian Ministry of Health [Ricerca Corrente].
The authors have no conflicts of interest to disclose.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
NRS = Numeric Rating Scale, TF = Amputation level Trans-Femoral, TT = Trans-Tibial, WHS = Walking Handicap Scale.
P < .05.
P < .01.
Number of observations = 302; ANOVA P < .001; The statistical significant results are highlighted with bold character.
The statistical significant results are highlighted with bold character.
Number of observations: 205; likelihood ratio test statistics P < .001.
The coefficient in this table gives the chance in the log odds of the outcome for a 1-unit increase in the predictor variable.
Odds ratio (OR) is defined as the ratio of the odds of an event occurring in 1 group to the odds of it occurring in another group. Odds are defined as the ratio of the probability of an “event” and the probability of a “non-event.”
For 1 year increase.
For 1 unit increase.
References
- [1].Willey J, Mentias A, Vaughan-Sarrazin M, et al. Epidemiology of lower extremity peripheral artery disease in veterans. J Vasc Surg 2018;68:527–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Jeffcoate W, Young B. Reducing amputation in diabetes: work from the West Country provides both evidence and a tool-kit. Diabetic Med 2018;35:8–9. [DOI] [PubMed] [Google Scholar]
- [3].Moxey PW, Gogalniceanu P, Hinchliffe RJ, et al. Lower extremity amputations—a review of global variability in incidence. Diabetic Med 2011;28:1144–53. [DOI] [PubMed] [Google Scholar]
- [4].Moxey PW, Hofman D, Hinchliffe RJ, et al. Epidemiological study of lower limb amputation in England between 2003 and 2008. Br J Surg 2010;97:1348–53. [DOI] [PubMed] [Google Scholar]
- [5].Blumentritt S, Schmalz T, Jarasch R. Significance of static prosthesis alignment for standing and walking of patients with lower limb amputation. Der Orthopade 2001;30:161–8. [DOI] [PubMed] [Google Scholar]
- [6].Culham EG, Peat M, Newell E. Below-knee amputation: a comparison of the effect of the SACH foot and single axis foot on electromyographic patterns during locomotion. Prosthet Orthot Int 1986;10:15–22. [DOI] [PubMed] [Google Scholar]
- [7].Nadollek H, Brauer S, Isles R. Outcomes after trans-tibial amputation: the relationship between quiet stance ability, strength of hip abductor muscles and gait. Physiother Res Int 2002;7:203–14. [DOI] [PubMed] [Google Scholar]
- [8].Houghton AD, Taylor PR, Thurlow S, et al. Success rates for rehabilitation of vascular amputees: implications for preoperative assessment and amputation level. Br J Surg 1992;79:753–5. [DOI] [PubMed] [Google Scholar]
- [9].Brunelli S, Averna T, Porcacchia P, et al. Functional status and factors influencing the rehabilitation outcome of people affected by above-knee amputation and hemiparesis. Arch Phys Med Rehabilit 2006;87:995–1000. [DOI] [PubMed] [Google Scholar]
- [10].Gailey RS. Predictive outcome measures versus functional outcome measures in the lower limb amputee. J Prosthet Orthot 2006;18:51–60. [Google Scholar]
- [11].Davie-Smith F, Coulter E, Kennon B, et al. Factors influencing quality of life following lower limb amputation for peripheral arterial occlusive disease: A systematic review of the literature. Prosthet Orthot Int 2017;41:537–47. [DOI] [PubMed] [Google Scholar]
- [12].De-Rosende Celeiro I, Simón Sanjuán L, Santos-del-Riego S. Activities of daily living in people with lower limb amputation: outcomes of an intervention to reduce dependence in pre-prosthetic phase. Disabil Rehabil 2017;39:1799–806. [DOI] [PubMed] [Google Scholar]
- [13].Collin C, Wade DT, Cochrane GM. Functional outcome of lower limb amputees with peripheral vascular disease. Clin Rehabil 1992;6:13–21. [Google Scholar]
- [14].Gerhards F, Florin I, Knapp T. The impact of medical, reeducational, and psychological variables on rehabilitation outcome in amputees. Int J Rehabil Res 1984;7:379–88. [DOI] [PubMed] [Google Scholar]
- [15].Datta D, Nair PN, Payne J. Outcome of prosthetic management of bilateral lower-limb amputees. Disabil Rehabil 1992;14:98–102. [DOI] [PubMed] [Google Scholar]
- [16].McWhinnie DL, Gordon AC, Collin J, et al. Rehabilitation outcome 5 years after 100 lower-limb amputations. Br J Surg 1994;81:1596–9. [DOI] [PubMed] [Google Scholar]
- [17].Munin MC, Espejo-De Guzman MC, Boninger ML, et al. Predictive factors for successful early prosthetic ambulation among lower-limb amputees. J Rehabil Res Dev 2001;38:379–84. [PubMed] [Google Scholar]
- [18].Leung ECC, Rush PJ, Devlin M. Predicting prosthetic rehabilitation outcome in lower limb amputee patients with the functional independence measure. Arch Phys Med Rehabil 1996;77:605–8. [DOI] [PubMed] [Google Scholar]
- [19].Dillingham TR, Pezzin LE, MacKenzie EJ. Limb amputation and limb deficiency: epidemiology and recent trends in the United States. South Med J 2002;95:875–84. [DOI] [PubMed] [Google Scholar]
- [20].Rommers GM, Vos LDW, Groothoff JW, et al. Epidemiology of lower limb amputees in the north of The Netherlands: aetiology, discharge destination and prosthetic use. Prosthet Orthot Int 1997;21:92–9. [DOI] [PubMed] [Google Scholar]
- [21].Heikkinen M, Saarinen J, Suominen VP, et al. Lower limb amputations: differences between the genders and long-term survival. Prosthet Orthot Int 2007;31:277–86. [DOI] [PubMed] [Google Scholar]
- [22].Pournajaf S, Goffredo M, Agosti M, et al. Community ambulation of stroke survivors at 6 months follow-up: an observational study on sociodemographic and sub-acute clinical indicators. Eur J Phys Rehabil Med 2019;55:433–41. [DOI] [PubMed] [Google Scholar]
- [23].Desrochers J, Frengopoulos C, Payne MW, et al. Relationship between body image and physical functioning following rehabilitation for lower-limb amputation. Int J Rehabil Res 2019;42:85–8. [DOI] [PubMed] [Google Scholar]
- [24].Damiani C. Amputee rehabilitation: taking charge, functional assessment and goal setting. Giornale italiano di medicina del lavoro ed ergonomia. G Ital Med Lav Ergon 2015;37:16–21. Italian. [PubMed] [Google Scholar]
- [25].Casale R, Maini M, Bettinardi O, et al. Motor and sensory rehabilitation after lower limb amputation: state of art and perspective of change. G Ital Med Lav Ergon 2013;35:51–60. [PubMed] [Google Scholar]
- [26].Perry J, Garrett M, Gronley JK, et al. Classification of walking handicap in the stroke population. Stroke 1995;26:982–9. [DOI] [PubMed] [Google Scholar]
- [27].Organisation mondiale de la santé, World Health Organization. International classification of functioning, disability and health: ICF. World Health Organization. 2001. [Google Scholar]
- [28].Lord SE, Rochester L. Measurement of community ambulation after stroke: current status and future developments. Stroke 2005;6:1457–61. [DOI] [PubMed] [Google Scholar]
- [29].Franceschini M, Rampello A, Agosti M, et al. Walking performance: correlation between energy cost of walking and walking participation. New statistical approach concerning outcome measurement. PloS One 2013;8:e56669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Journeay WS, Pauley T, Kowgier M, et al. Return to work after occupational and non-occupational lower extremity amputation. Occup Med 2018;68:438–43. [DOI] [PubMed] [Google Scholar]
- [31].CAVALLI-SFORZA, LL. Analisi statistica per medici e biologi: una introduzione elementare. Bollati Boringhieri. 1992. Italian. [Google Scholar]
- [32].Dancey CP, Reidy J. Statistics Without Maths for Psychology. Harlow, UK: Pearson Education; 2007. [Google Scholar]
- [33].Sinha R, Van Den Heuvel WJ. A systematic literature review of quality of life in lower limb amputees. Disabil Rehabil 2011;33:883–99. [DOI] [PubMed] [Google Scholar]
- [34].Ehnert S, Linnemann C, Aspera-Werz RH, et al. Feasibility of cell lines for in vitro co-cultures models for bone metabolism. SciMed J 2020;2:157–81. [Google Scholar]
- [35].Cutson TM, Bongiorni DR. Rehabilitation of the older lower limb amputee: a brief review. J Am Geriatr Soc 1996;44:1388–93. [DOI] [PubMed] [Google Scholar]
- [36].Hirsh AT, Dillworth TM, Ehde DM, et al. Sex differences in pain and psychological functioning in persons with limb loss. J Pain 2010;11:79–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Bramati IE, Rodrigues EC, Simões EL, et al. Lower limb amputees undergo long-distance plasticity in sensorimotor functional connectivity. Sci Rep 2019;9:2518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Kerstein MD, Zimmer H, Dugdale FE, et al. Successful rehabilitation following amputation of dominant versus nondominant extremities. Am J Occup Ther 1977;31:313–5. [PubMed] [Google Scholar]
- [39].Hobara H, Potthast W, Sano Y, et al. Does amputation side influence sprint performances in athletes using running-specific prostheses? SpringerPlus 2015;4:670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Pacheco-Barrios K, Pinto CB, Velez FS, et al. Structural and functional motor cortex asymmetry in unilateral lower limb amputation with phantom limb pain. Clin Neurophysiol 2020;131:2375–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Burger H, Maver T, Marinček Č. Partial hand amputation and work. Disabil Rehabil 2007;29:1317–21. [DOI] [PubMed] [Google Scholar]
- [42].Burger H, Marinček Č, Isakov E. Mobility of persons after traumatic lower limb amputation. Disabil Rehabil 1997;19:272–7. [DOI] [PubMed] [Google Scholar]
- [43].Armstrong DG, Lavery LA, Van Houtum WH, et al. The impact of gender on amputation. J Foot Ankle Surg 1997;36:66–9. [DOI] [PubMed] [Google Scholar]
- [44].Bodenheimer AJ, Kerrigan SL, Garber TN, et al. Sexuality in persons with lower extremity amputations. Disabil Rehabil 2000;22:409–15. [DOI] [PubMed] [Google Scholar]
- [45].Esquenazi A. Amputation rehabilitation and prosthetic restoration. From surgery to community reintegration. Disabil Rehabil 2015;26:831–6. [DOI] [PubMed] [Google Scholar]
- [46].Hawamdeh ZM, Othman YS, Ibrahim AI. Assessment of anxiety and depression after lower limb amputation in Jordanian patients. Neuropsychiatr Dis Treat 2008;4:627.18830394 [Google Scholar]
- [47].Ray SF, Wurdeman SR, Takahashi KZ. Prosthetic energy return during walking increases after 3 weeks of adaptation to a new device. J Neuroeng Rehabili 2018;15:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48].Paranjape S, Singhania N. Effect of body positions on quadriceps angle measurement. SciMed J 2019;1:20–4. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


