Abstract
Objective
To examine county level associations between the prevalence of medical and recreational cannabis stores (referred to as dispensaries) and opioid related mortality rates.
Design
Panel regression methods.
Setting
812 counties in the United States in the 23 states that allowed legal forms of cannabis dispensaries to operate by the end of 2017.
Participants
The study used US mortality data from the Centers for Disease Control and Prevention combined with US census data and data from Weedmaps.com on storefront dispensary operations. Data were analyzed at the county level by using panel regression methods.
Main outcome measure
The main outcome measures were the log transformed, age adjusted mortality rates associated with all opioid types combined, and with subcategories of prescription opioids, heroin, and synthetic opioids other than methadone. The associations of medical dispensary and recreational dispensary counts with age adjusted mortality rates were also analyzed.
Results
County level dispensary count (natural logarithm) is negatively related to the log transformed, age adjusted mortality rate associated with all opioid types (β=−0.17, 95% confidence interval −0.23 to −0.11). According to this estimate, an increase from one to two storefront dispensaries in a county is associated with an estimated 17% reduction in all opioid related mortality rates. Dispensary count has a particularly strong negative association with deaths caused by synthetic opioids other than methadone (β=−0.21, 95% confidence interval −0.27 to −0.14), with an estimated 21% reduction in mortality rates associated with an increase from one to two dispensaries. Similar associations were found for medical versus recreational storefront dispensary counts on synthetic (non-methadone) opioid related mortality rates.
Conclusions
Higher medical and recreational storefront dispensary counts are associated with reduced opioid related death rates, particularly deaths associated with synthetic opioids such as fentanyl. While the associations documented cannot be assumed to be causal, they suggest a potential association between increased prevalence of medical and recreational cannabis dispensaries and reduced opioid related mortality rates. This study highlights the importance of considering the complex supply side of related drug markets and how this shapes opioid use and misuse.
Introduction
The epidemic of opioid misuse and drug overdose deaths in the United States constitutes a grave public health crisis. Opioid related mortality rates have increased sharply since 1999, representing over two thirds of all US drug overdose deaths in 2018.1 Researchers have estimated that altering the overall supply side of drug markets could help ameliorate the opioid crisis. In the US, this supply side has changed markedly as an increasing number of individual states have legalized the production, use, or sale of cannabis, even as the US government continues to treat cannabis possession as a federal offense. In 2008, 13 states had legalized use or sale of medical cannabis, while none allowed cannabis for recreational use. By the end of 2018, 33 states had legalized medical cannabis and 10 states had legalized recreational cannabis. In this study we examined whether the availability of legal cannabis in an increasing number of geographical areas has any implications for opioid misuse.
Several studies have explored this issue by investigating how state level medical or recreational cannabis legalization events are associated with rates of opioid related mortality. The evidence so far is mixed. Some studies found a negative association between opioid related mortality rates and medical cannabis legalization2 and recreational legalization.3 4 However, other studies have found the association between legalization events and opioid related mortality rates to be spurious or non-significant.5 6 One reason for these mixed findings could be that focusing on state level cannabis legalization events paints an incomplete picture. Several states that legalized medical cannabis use do not provide legal allowances for stores (referred to as dispensaries) to sell cannabis. Allowing for legal sale of cannabis is a key step in increasing its availability5 7 because it shifts the cost structure of supplying cannabis, making cannabis more easily and widely accessible to customers.8 Additionally, in states that have legalized recreational sale of cannabis, often a one to two year time lag exists between enactment of recreational legislation and the start of recreational dispensary operations.7 Investigating this issue at the state level is also important given that many counties within legal states have prohibited or limited retail sale of cannabis or enacted zoning and licensing laws, leading to considerable heterogeneity in the availability of legal cannabis within legalized states.9
Our study examines the association between the count of active dispensary operations (a more direct measure of legal cannabis availability than legislation events) and opioid related mortality rates at the county level over the period 2014-18. We focused on the county level because counties represent important units of analysis for population health studies. County governments provide substantial political, economic, and social structure to local populations through the administration of regulations, programmes, and services.10 More specifically, counties oversee criminal justice, social service, and health and emergency service programmes—all vital dimensions of the public infrastructure related to drug use and markets.10
We used panel regression methods to examine how the count of cannabis dispensaries relates to opioid related mortality rates. Following recent studies that have explored whether medical versus recreational legalization has differing associations with opioid use,11 12 13 we distinguished between medical and recreational cannabis dispensaries in our analyses. Medical and recreational cannabis dispensaries have different operational requirements and are subject to different licensing, regulatory, and taxation systems.9 Medical dispensaries only serve patients who have a state approved medical card or doctor’s recommendation, while recreational dispensaries sell cannabis to adults aged 21 years and older.
We also differentiated between different types of opioids. Opioids refer to a class of chemically related drugs that include the illicit drug heroin, prescription pain relievers such as oxycodone, and synthetic opioids such as fentanyl. In recent years, the rise in opioid related mortality rates has been largely driven by deaths involving fentanyl and its analogs.1 14 This finding suggests opioid overdose deaths might be composed of specific subepidemics that follow different patterns.15 In our analyses, we examined mortality rates due to all opioid types and those due to prescription opioids, heroin, and synthetic opioids other than methadone.
Methods
In our study we used secondary data on dispensary storefront locations and opioid related mortality rates over the period 2014-18. We started in 2014 when we were first able to access systematic data on dispensary locations. We ended in 2018 because this is the most recent year county level mortality data are available through the US Centers for Disease Control and Prevention. Four main types of data are included in our analysis: information on cannabis and opioid laws; dispensary location and operational information; county level demographic and economic data; and county level opioid related mortality rates.
Data collection
We collected information on state level cannabis legislation to determine the restricted set of states that allowed legal forms of dispensaries and started up dispensary operations by the end of 2017. Our sources were the Prescription Drug Abuse Policy System (PDAPS),16 cross validated with online government resources, media reports of dispensary openings by state, and information from existing studies.5 6 Eight states and the District of Columbia allowed for recreational dispensaries, while 15 allowed for medical forms only. In our models we included a control for whether a state allowed recreational sales. We also used controls for state level opioid interventions, including naloxone access, pain management oversight, and pharmacist patient identification laws (data source PDAPS).16 Figure 1 presents maps of the 23 states included in our data. Our main dataset consists of all 812 counties within these states. We also conducted supplemental analyses that replicate our main findings among all 3142 counties across the US.
Fig 1.
County level monthly counts of storefront dispensaries listed on Weedmaps.com in 23 states that allowed legal storefront dispensary operations (plus District of Columbia), averaged over calendar year, 2014-17
In the US, no centralized database exists for cannabis dispensaries at the federal level. Individual states that have legalized sale of cannabis maintain separate licensing databases for dispensaries, and the dispensary related information that has been made publicly available has varied across states and over time. To construct systematic time varying measures of dispensary counts, we collected dispensary location and operational information from Weedmaps, a major US cannabis website where dispensaries list operational information such as address, hours of operations, promotions, and contact information. Weedmaps has been used as a data source by several studies to locate cannabis dispensaries.17 18 19 20 21 Previous work suggested that Weedmaps provides higher coverage of dispensaries relative to other cannabis focused websites.9 On Weedmaps, each dispensary reports whether it is a medical or recreational dispensary and a storefront (brick and mortar) or delivery service. Our measures of dispensary counts focus on storefront operations, which have specific, known locations that local consumers can frequent. In contrast, delivery services do not have known locations. Instead, these services often span large geographical regions, listing themselves in several counties, many of which do not formally allow retail sale of cannabis.17
We collected data on dispensaries operating within each county across the US on a monthly basis from 2014 to December 2017. A subset of dispensaries (around 4%) operated under both medical and recreational licenses. If a dispensary was listed as both medical and recreational, then it was included in the county level count for each type (medical and recreational), respectively. We only counted storefront dispensaries that were listed on Weedmaps for longer than three months with specific street addresses to ensure that our dispensary measure reflected organizations that local consumers had a reasonable likelihood of finding and buying products from. We measured the average monthly count of storefront dispensaries over the 12 months in the previous calendar year because we assumed a temporal lag exists between when a dispensary initially begins operations and when it begins to sell to a sizable number of consumers. In supplementary analyses we also estimated the associations between the average monthly count of storefront dispensaries and opioid related mortality rates in the same calendar year. We estimated the natural logarithm (ln) of this count owing to skew in its distribution. Figure 1 shows changing cannabis dispensary counts across the counties in our sample during this time period.
We retrieved yearly data on prescription opioid related mortality rates in the 812 counties in our dataset from the Centers for Disease Control and Prevention multiple cause of death database; for 2018, the data were released in February 2020. Mortality rates are represented as the log transformed age adjusted death rate per 100 000 population. We first increased all values of the variable by a constant value (one) before taking the log; therefore, counties with no dispensaries have a value of zero for this log transformed variable. In our main analyses, we focused on deaths associated with people aged 21 years and older, who are eligible for recreational cannabis dispensary purchases.
We used ICD-10 (International Classification of Diseases, 10th revision) external cause of injury codes (X40-X44, X60-X64, X85, or Y10-14) and drug identification codes (T40.0-T40.4 and 40.6) to identify deaths related to opioids.14 22 23 To examine fatalities associated with more specific opioid types, we restricted drug identification codes to T40.2 (natural opioid analgesics and semisynthetic opioids) and T40.3 (methadone) to identify prescription opioid related deaths,14 code T40.1 to identify deaths due to heroin,24 and code T40.4 to identify deaths due to synthetic opioid analgesics other than methadone. Code T40.4 includes deaths caused by both pharmaceutical and illicitly sourced fentanyl. Deaths classified as involving more than one opioid type were included in the counts for each type. Figure 2 and figure 3 show age adjusted, opioid related mortality rates at the county level in states under examination in 2015 and 2018.
Fig 2.
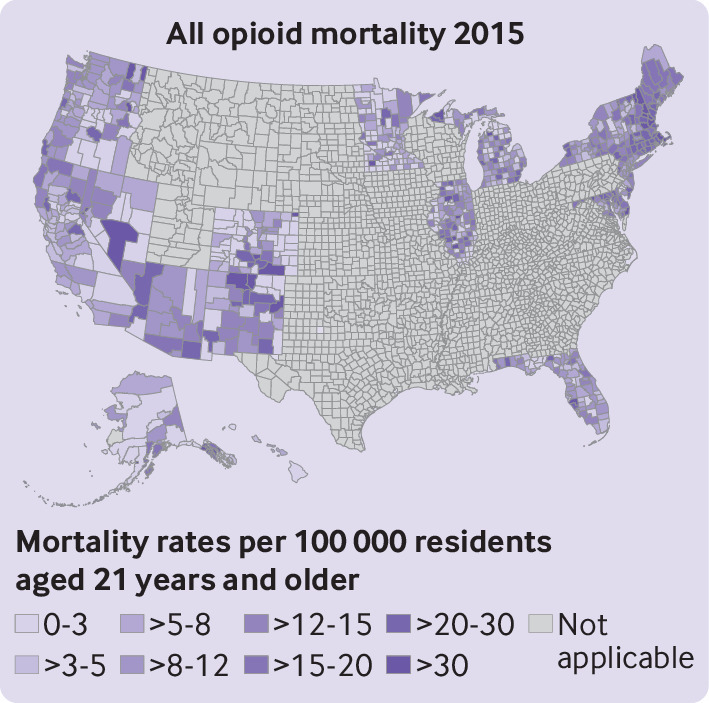
Age adjusted mortality rates related to all opioid types at county level for 23 states that allowed legal storefront dispensary operations (plus District of Columbia) for 2015. Mortality rates per 100 000 residents aged 21 years and older
Fig 3.
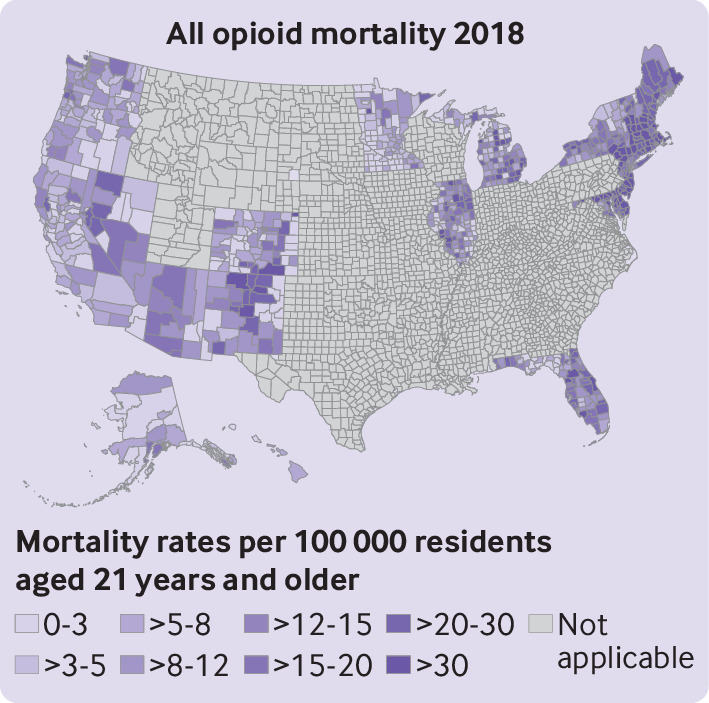
Age adjusted mortality rates related to all opioid types at county level for 23 states that allowed legal storefront dispensary operations (plus District of Columbia) for 2018. Mortality rates per 100 000 residents aged 21 years and older
We obtained demographic, socioeconomic, and labor market information at the county level from the American Community Survey. Estimates for less populated geographical areas were included by using American Community Survey five year estimates, which measure the average characteristics for all US counties over moving five year windows. Measures included data on the total population aged 21 years or older, unemployment rate, population aged 18 years or older with a disability, average per capita income (ln), proportion white (alone), proportion with bachelors degree, and proportion of men. We also included yearly gross domestic product data at the county level, rescaled to 2018, which were obtained from the US Bureau of Economic Analysis.
Statistical analyses
We used panel regression models to estimate the county level association of storefront cannabis dispensary counts with yearly age adjusted, opioid related mortality rates for 2015-18. Our models specify random effects at the county level to accommodate within county dependence in opioid related mortality outcomes. Firstly, we used models that only included county population and yearly indicator variables as control variables. Secondly, we used models will a full set of controls for county level characteristics, yearly indicators, and state cannabis and opioid related laws. Across all models, standard errors were reported to account for heteroskedasticity and within county serial correlation of errors.25
The main covariate of interest was the log transformed count of storefront dispensaries operating within each county in the previous year. One set of models estimated the effect of the log transformed count of storefront dispensaries (medical and recreational combined) on the log transformed age adjusted mortality rates associated with all opioid types combined, prescription opioids, heroin, and synthetic opioids other than methadone. A second set of models simultaneously estimated the effect of the log transformed counts of medical dispensaries and recreational dispensaries (separate terms for each) on each of the log transformed age adjusted opioid related mortality rates listed above. We also calculated the significance levels of our main independent variables by using the stepdown procedure proposed by Romano and Wolf (2005).26 This procedure is designed to adjust the probability of incorrectly identifying at least one coefficient as significant when several hypotheses are tested at once. This procedure improves upon earlier multiple testing procedures such as the Bonferroni and the Holm methods by taking into account the dependence structure of individual test statistics. Statistical analyses were performed with Stata version 16.1.
Patient and public involvement
We used secondary data and patients were not involved in setting the research question and outcome measures, nor in designing and implementing the research study.
Results
Our main analyses examined county level dynamics in the 23 states (plus the District of Columbia) that offered legal protection to dispensaries and started up dispensary operations by the end of 2017. We focused on these states because, by definition, legal dispensaries are only allowed in states that offered legal protection to dispensaries. This focus on states with legal allowances for dispensaries also enabled us to control for broader differences in the political and legal environments that differentiate states that offer legal protection to dispensaries versus those that do not. Supplemental tables 3 and 4 present analyses of the associations between dispensary counts and opioid related mortality rates among all counties in the US. We included county level random effects specifications and the same set of control variables as our main models. These supplemental analyses compared opioid related mortality rates more broadly, including a large number of counties in states that do not allow dispensary operations and therefore have a value of zero for our main measure, dispensary counts.
Table 1 and table 2 show yearly frequencies and other descriptive information about our main variables (dispensary counts and opioid related mortality rates). Table 3 presents estimated effects of average dispensary storefront count (ln) in the previous year on the current year’s log transformed age adjusted opioid related mortality rates (see supplemental tables 1 and 2 for full set of estimates). The log transformed count of storefront dispensaries in a focal county was found to be negatively related to deaths associated with all opioid types (β=−0.17, 95% confidence interval −0.23 to −0.11, P=0.002; Romano-Wolf joint test P values are reported). Because the dependent and independent variables are log transformed, the estimated coefficient can be directly interpreted as the expected percentage change in the dependent variable associated with a 1% change in the independent variable.27 According to our estimates, increasing the count of storefront dispensaries from one to two (a 100% change in dispensary count) is associated with a 17% reduction (100%×−0.17=−17%) in the age adjusted mortality rate for all opioid types. An increase from two to three dispensaries is associated with a further 8.5% reduction (50%×−0.17=−8.5%) in all opioid related mortality rates.
Table 1.
Frequencies of different classes of county level cannabis dispensary counts (averaged over 12 months of each year)
| Average count | No of counties in each frequency category | ||||
|---|---|---|---|---|---|
| 2014 | 2015 | 2016 | 2017 | 2018 | |
| All dispensary types | |||||
| 0 | 715 | 679 | 534 | 488 | 449 |
| >0-1 | 37 | 60 | 128 | 127 | 123 |
| >1-2 | 13 | 17 | 43 | 39 | 51 |
| >2-3 | 13 | 16 | 30 | 35 | 46 |
| >3-5 | 8 | 5 | 22 | 37 | 40 |
| >5-10 | 7 | 12 | 17 | 30 | 42 |
| >10 | 19 | 23 | 38 | 56 | 61 |
| Mean | 0.90 | 1.30 | 2.41 | 3.89 | 4.21 |
| Median | 0 | 0 | 0 | 0 | 0 |
| Min, max | 0, 188.9 | 0, 271.3 | 0, 372.9 | 0, 498.58 | 0, 501.8 |
| Medical dispensaries | |||||
| 0 | 720 | 687 | 565 | 526 | 491 |
| >0-1 | 33 | 58 | 127 | 147 | 148 |
| >1-2 | 19 | 17 | 37 | 42 | 55 |
| >2-3 | 11 | 15 | 26 | 29 | 43 |
| >3-5 | 3 | 6 | 14 | 32 | 30 |
| >5-10 | 10 | 7 | 14 | 8 | 18 |
| >10 | 16 | 22 | 29 | 28 | 27 |
| Mean | 0.83 | 1.14 | 1.98 | 2.47 | 2.32 |
| Median | 0 | 0 | 0 | 0 | 0 |
| Min, max | 0, 188.9 | 0, 271.3 | 0, 372.9 | 0, 498.6 | 0, 477.7 |
| Recreational dispensaries | |||||
| 0 | 786 | 774 | 722 | 703 | 662 |
| >0-1 | 14 | 13 | 33 | 14 | 28 |
| >1-2 | 6 | 7 | 23 | 10 | 16 |
| >2-3 | 2 | 5 | 8 | 17 | 19 |
| >3-5 | 3 | 9 | 12 | 14 | 17 |
| >5-10 | 0 | 3 | 7 | 28 | 29 |
| >10 | 1 | 1 | 7 | 26 | 41 |
| Mean | 0.07 | 0.16 | 0.43 | 1.42 | 2.03 |
| Median | 0 | 0 | 0 | 0 | 0 |
| Min, max | 0, 22.7 | 0, 35 | 0, 64.9 | 0, 131 | 0, 149.9 |
Classes for cannabis dispensaries are derived from averaged monthly counts of storefront dispensaries listed on Weedmaps in each county in 12 month period corresponding to each calendar year. If a dispensary was listed as both medical and recreational, then it was counted toward county level count for each type (medical and recreational), respectively.
Table 2.
Frequencies of yearly opioid related, age adjusted mortality rates at county level
| Age adjusted mortality rate | No of counties in each frequency category | |||
|---|---|---|---|---|
| 2015 | 2016 | 2017 | 2018 | |
| All opioid types | ||||
| 0 | 173 | 148 | 149 | 161 |
| >0-5 | 114 | 83 | 96 | 99 |
| >5-10 | 184 | 187 | 137 | 171 |
| >10-20 | 235 | 227 | 234 | 205 |
| >20-30 | 70 | 103 | 107 | 92 |
| >30-40 | 25 | 46 | 55 | 44 |
| >40-50 | 4 | 11 | 22 | 26 |
| >50 | 7 | 7 | 12 | 14 |
| Mean | 10.23 | 12.33 | 13.58 | 12.69 |
| Median | 8.44 | 9.66 | 10.77 | 9.08 |
| Min, max | 0, 84.47 | 0, 83.44 | 0, 105.32 | 0, 91.68 |
| Prescription | ||||
| 0 | 244 | 227 | 223 | 252 |
| >0-5 | 275 | 240 | 261 | 280 |
| >5-10 | 186 | 221 | 201 | 197 |
| >10-20 | 87 | 101 | 106 | 71 |
| >20-30 | 11 | 12 | 12 | 11 |
| >30-40 | 4 | 9 | 4 | 1 |
| >40-50 | 3 | 1 | 3 | 0 |
| >50 | 2 | 1 | 2 | 0 |
| Mean | 4.95 | 5.37 | 5.34 | 4.27 |
| Median | 3.47 | 4.06 | 3.79 | 3.46 |
| Min, max | 0, 72.59 | 0, 55.96 | 0, 75.27 | 0, 30.79 |
| Heroin | ||||
| 0 | 335 | 317 | 323 | 314 |
| >0-5 | 241 | 247 | 237 | 276 |
| >5-10 | 154 | 149 | 151 | 129 |
| >10-20 | 74 | 81 | 84 | 66 |
| >20-30 | 4 | 11 | 12 | 20 |
| >30-40 | 3 | 4 | 3 | 5 |
| >40-50 | 0 | 2 | 1 | 1 |
| >50 | 1 | 1 | 1 | 1 |
| Mean | 3.66 | 4.24 | 4.15 | 4.04 |
| Median | 1.87 | 2.14 | 2.18 | 2.06 |
| Min, max | 0, 72.59 | 0, 59.76 | 0, 50.61 | 0, 58.77 |
| Synthetic (non-methadone) | ||||
| 0 | 359 | 320 | 273 | 279 |
| >0-5 | 312 | 213 | 187 | 172 |
| >5-10 | 90 | 127 | 125 | 140 |
| >10-20 | 37 | 105 | 133 | 111 |
| >20-30 | 11 | 32 | 60 | 59 |
| >30-40 | 2 | 10 | 24 | 35 |
| >40-50 | 1 | 4 | 7 | 9 |
| >50 | 0 | 1 | 3 | 7 |
| Mean | 2.817 | 5.28 | 7.43 | 8.05 |
| Median | 0.794 | 1.805 | 3.445 | 3.509 |
| Min, max | 0, 42.24 | 0, 57.96 | 0, 96.84 | 0, 85.111 |
Classes for opioid related mortality rates are derived from age adjusted mortality rates per 100 000 residents in each year (aged 21 years and older). Rates are presented for counties in the 23 states with legal, operating storefront dispensaries by end of 2017 plus District of Columbia—812 counties in total.
Table 3.
Associations between previous year’s dispensary counts (natural logarithm) and log transformed yearly opioid related mortality rates at county level
| Log transformed opioid related mortality rate | Coefficient (95% confidence interval), Romano-Wolf P value | |||||||
|---|---|---|---|---|---|---|---|---|
| All opioid types | Prescription opioids | Heroin | Synthetic non-methadone | |||||
| Population control only | ||||||||
| All storefront dispensaries | −0.18 (−0.24 to −0.13), 0.002 | −0.10 (−0.15 to −0.06), 0.004 | −0.06 (−0.12 to −0.01), 0.07 | −0.26 (−0.32 to −0.20), 0.002 | ||||
| Medical dispensaries only | −0.18 (−0.25 to −0.11), 0.002 | −0.10 (−0.16 −0.04), 0.002 | −0.11 (−0.17 to −0.05), 0.002 | −0.20 (−0.28 to −0.13), 0.002 | ||||
| Recreational dispensaries only | −0.08 (−0.15 to −0.02), 0.04 | −0.08 (−0.15 to −0.02), 0.27 | 0.04 (−0.01 to 0.10), 0.27 | −0.21 (−0.28 to −0.13), 0.002 | ||||
| All covariates | ||||||||
| All storefront dispensaries | −0.17 (−0.23 to −0.11), 0.002 | −0.08 (−0.13 to −0.03), 0.03 | −0.08 (−0.13 to −0.02), 0.03 | −0.21 (−0.27 to −0.14), 0.002 | ||||
| Medical dispensaries only | −0.15 (−0.21 to −0.09), 0.002 | −0.06 (−0.11 to −0.00), 0.07 | −0.12 (−0.18 to −0.06), 0.002 | −0.14 (−0.21 to −0.07), 0.002 | ||||
| Recreational dispensaries only | −0.11 (−0.17 to −0.04), 0.01 | −0.05 (−0.11 to 0.02), 0.3 | 0.03 (−0.03 to 0.10), 0.30 | −0.21 (−0.29 to −0.13), 0.002 | ||||
Regression models specify random effects at county level, with yearly fixed effects. All storefront dispensaries reflects estimated effect of log transformed county level count of all storefront dispensaries (medical and recreational) on log transformed yearly age adjusted mortality rates among people aged 21 years and older for each type of opioid. Medical and recreational reflect effects of log transformed county level counts of medical storefront and recreational storefront dispensaries (estimated simultaneously) on log transformed yearly age adjusted mortality rates. Models under population control only are estimated with total population aged 21 years and older (natural logarithm (ln)) as the only control variable. Models under all covariates including county level time varying covariates for unemployment rate, average per capita income (ln), gross domestic product (ln), proportion white, total population aged 21 years and older (ln), proportion college educated, proportion men, population with disability (ln). State level time varying covariates: naloxone access law, pharmacist patient identification law, pain management clinic oversight, recreational legal. Models are estimated with robust standard errors on 812 counties in the 23 states with legal, operating storefront dispensaries by end of 2017 and District of Columbia.
We also found negative associations between storefront dispensary count and deaths associated with synthetic (non-methadone) opioids (β=−0.21, 95% confidence interval −0.27 to −0.14, P=0.002), suggesting an estimated 21% reduction in the mortality rate with an increase from one to two storefront dispensaries. Negative associations between storefront dispensary count and deaths due to prescription opioids (β=−0.08, −0.13 to −0.03) and heroin (β=−0.08, −0.13 to −0.02) are significant at the P less than 0.05 level.
Models that separate the association of medical versus recreational dispensaries with opioid related mortality rates show that both types of dispensaries have a negative association with age adjusted mortality rates due to all opioid types (medical dispensary count: β=−0.15, 95% confidence interval −0.21 to −0.09, P=0.002; recreational dispensary count: β=−0.11, −0.17 to −0.04, P=0.01). These coefficients can be interpreted as an estimated 15% reduction in mortality rate with an increase from one to two medical dispensaries, and an 11% reduction with an increase from one to two recreational dispensaries. We also found negative associations with deaths related to synthetic (non-methadone) opioids. An increase in medical dispensary count from one to two is associated with an estimated 14% reduction in mortality rates, while a similar increase in recreational dispensary count is associated with an estimated 21% reduction (medical dispensary count: β=−0.14, −0.21 to −0.07, P=0.002; recreational dispensary count: β=−0.21, −0.29 to −0.13, P=0.002). Medical dispensary count has a negative association with heroin related mortality rates (β=−0.12, −0.18 to −0.06, P=0.002), and to a weaker degree, prescription related mortality rates (β=−0.06, −0.11 to −0.00, P=0.07). Recreational dispensary count does not have a significant association with deaths related to prescription opioids or heroin (P=0.30).
Supplemental table 5 shows a consistent pattern of associations between storefront dispensaries and opioid related mortality rates when we used the current year’s (rather than the previous year’s) average counts to represent storefront dispensaries. We also found similar effects for the associations between recreational dispensaries and with all opioid related, heroin, and synthetic (non-methadone) opioid related mortality rates using contemporaneous measures (supplemental table 6).
Discussion
Principal findings
Our findings suggest that higher storefront cannabis dispensary counts are associated with reduced opioid related mortality rates at the county level. This association holds for both medical and recreational dispensaries, and appears particularly strong for deaths associated with synthetic (non-methadone) opioids, which include the highly potent synthetic opioid fentanyl and its analogs. These results were obtained after controlling for county level population characteristics, yearly effects, whether recreational dispensaries were legal or not in the focal county’s state, and opioid related state policies.
Strengths and weaknesses of the study
Our study focused on the years 2014-18, a period of considerable change in cannabis legalization across multiple states. Focusing on this period is a potential strength because we have provided relevant information about how recent changes in the cannabis landscape relate to opioid related overdose deaths; it is also a limitation in terms of the generalizability of our findings. Further, while we found a particularly strong association between the prevalence of storefront dispensaries and fentanyl related opioid deaths, it is not clear whether cannabis use and fentanyl mortality rates are more specifically linked, or if the strength of the association is owing to the rise in fentanyl use and mortality rates during the study period.
Another strength of our study is our use of a unique dataset on dispensary operations across the US over time to model how the availability of cannabis shapes opioid related mortality rates. By studying actual operations and county level dynamics, we were able to more directly model the availability of legally sold cannabis to local populations. However, our measures of storefront dispensary counts should be regarded as an approximation of all (legal and illegal) cannabis operations in the US. A previous study found that Weedmaps provided reasonable coverage of licensed dispensaries in Colorado over the period 2014-15.9 However, we do not know whether this applies to other states and for the current study period. Additionally, a number of unlicensed, illegally operating cannabis dispensaries appear to have listed themselves on Weedmaps during our period of investigation.28 Many of these illegal listings were deliveries, which we do not include in our cannabis dispensary counts owing to ambiguity in their actual operational status and geographical locations. While there appears to be a moderately high correlation (0.70) between the count of storefront and delivery based dispensaries operating within counties during the study period based on the counties cannabis deliveries claim to cover on Weedmaps, we cannot determine the extent of use of storefronts versus delivery services. Overall, our study should be regarded as a conservative examination of how the legal availability of cannabis in the US through storefront dispensaries with specific, known locations, rather than the total availability through legal and illicit markets, relates to opioid related mortality rates. Further investigation into the validity of Weedmaps and the scope of its coverage for legal and illicit markets is needed.
We have shown these associations within the subset of states that have legalized the sale of cannabis and across the complete set of counties in the US. This analysis provides a robust look at the associations between counts of dispensary storefronts and opioid related mortality rates across different geographical regions. We controlled for a number of county level factors that could affect the association between dispensary prevalence and opioid related mortality rates (such as county level unemployment rates, gross domestic product, and proportion of men). However, there might be other confounding factors that shape associations between dispensary prevalence and opioid related mortality rates. Future research is needed to evaluate how county level characteristics affect the nature of the association between cannabis dispensaries and opioid misuse outcomes. Overall, we stress that our findings are based on the ecological study of county level associations between our main variables and must be interpreted with that in mind.
Systematic data on the timing and content of county level regulations could not be gathered for all the counties examined. While we have controlled for several county level demographic and economic variables, and specify random effects at the county level, our findings cannot rule out the effects that other changes in cannabis laws and opioid control policies might have had on opioid related overdose deaths during the study period at the state and county levels. Additionally, the substances tested for and the processes for toxicological testing at the time of death investigations vary by jurisdiction in the US.14 These variations could affect reporting of substance specific death rates.
Comparisons with other studies
Several previous studies have focused on state level medical cannabis legalization events,2 5 6 with conflicting findings on the association between legalization and opioid related mortality rates. However, some studies indicate that researchers should account for legal allowances for cannabis dispensary operations rather than focusing on the mere passage of cannabis laws; this provides a better reflection of the potential availability of legal cannabis and its association with opioid use within a geographical area.4 5 8 These studies, which focus specifically on medical dispensaries, have found more consistent evidence of a negative association between statewide medical dispensary allowances and opioid related mortality rates. One study has modeled the association between medical cannabis dispensary presence and prescription opioid related death rates at the county level, and also found a negative association.29 However, these studies do not consider the presence of recreational cannabis dispensaries, which target a broader clientele (people aged 21 years or older rather than patients with medical cards or physicians’ recommendations) and have been increasingly allowed by states within the US in recent years.
In contrast to studies that focus on a single dispensary type,2 3 5 6 29 we modeled medical and recreational storefront dispensary presence separately. We also distinguished between fatalities associated with different types of opioids, including fentanyl and its analogs, which have sharply overtaken other types of opioids in number of deaths in the US in recent years.14 Another study examined the association between medical and recreational dispensaries with opioid related mortality rates, but at the state level.4 This study found a negative association between the start of both types of cannabis dispensary operations within a state and opioid related mortality rates—an association that appears most pronounced with the class of opioids that includes fentanyl and its analogs. We reported consistent findings, but at the more fine grained county level and by using the prevalence of active dispensary operations rather than a single start date. Therefore, our study complements and extends (to the county level by using active dispensary operations, and studying medical and recreational dispensary forms separately) existing studies that have found evidence of a negative association between the legal availability of cannabis in a geographical area with opioid related mortality rates.
Meaning of the study for clinicians and policy makers
Cannabis is generally thought to be a less addictive substance than opioids. Cannabis can potentially be used medically for pain management and has considerable public support. Our findings suggest that increasing availability of legal cannabis (modeled through the presence of medical and recreational dispensary operations) is associated with a decrease in deaths associated with the T40.4 class of opioids, which include the highly potent synthetic opioid fentanyl. This finding is especially important because fentanyl related deaths have become the most common opioid related cause of death, with 46 802 reported in 2018, representing 67% of all opioid related deaths in 2018.1 If consumers use cannabis and opioids for pain management, increasing the supply of legal cannabis might have implications for fentanyl demand and opioid related mortality rates overall.
However, the potential harms of cannabis, including the cognitive development of adolescents, medical conditions such as schizophrenia, and public safety risks, should not be ignored.30 31 32 Additionally, given that the efficacy of cannabis for pain management has not been well established,33 patients who turn to cannabis instead of physician prescribed opioids as a means for pain control might experience poorer symptom control. Overall, a greater understanding is needed about the impact of cannabis legalization on opioid misuse and public health outcomes before policy makers can weigh the potential benefits against the harms of promoting cannabis legalization.
Unanswered questions and future research
A key issue when considering cannabis liberalization policies is the different associations between medical and recreational legalization and health related outcomes. Arguments against recreational legalization of cannabis are that this gateway drug could exacerbate negative outcomes overall. However, evidence remains inconclusive on this key public health issue. Our research suggests that both medical and recreational dispensaries are associated with reduced opioid related mortality rates. Future research is needed investigating the association with mortality rates and other important opioid related misuse outcomes.
Conclusions
We studied county level associations between cannabis storefront dispensaries and opioid related mortality rates in the US between 2014 and 2018. Our study found that increased medical and recreational storefront dispensary counts are associated with reduced opioid related mortality rates during the study period. These associations appear particularly strong for deaths related to synthetic opioids such as fentanyl. Given the alarming rise in the fentanyl based market in the US, and the increase in deaths involving fentanyl and its analogs in recent years,14 the question of how legal cannabis availability relates to opioid related deaths is particularly pressing. Overall, our study contributes to understanding the supply side of related drug markets and how it shapes opioid use and misuse.
What is already known on this topic
In the United States, opioid related mortality rates have increased sharply in recent decades, prompting researchers to consider how changes to the overall supply side of drug markets might help ameliorate the opioid crisis
Several studies have found a negative association between opioid related mortality rates and medical cannabis and recreational cannabis legalization events; others have found this to be a spurious or non-significant association
Some studies suggest that the allowance of cannabis stores (dispensaries) legally authorized to sell cannabis, a key step in increasing access to legal cannabis, might have a stronger negative association with opioid related mortality rates at the state level
What this study adds
This study examined the association between active cannabis dispensary operations and opioid related mortality rates at the county level for medical and recreational cannabis dispensaries
Higher storefront cannabis dispensary counts were associated with reduced opioid related mortality rates
This association holds for medical and recreational cannabis dispensary counts and appears particularly strong for deaths associated with synthetic (non-methadone) opioids, including fentanyl and its analogs
Acknowledgments
We thank professors Marissa King (Yale School of Management), Airin Martinez (University of Massachusetts, Amherst) and Yuyan Shi (University of California, San Diego) for their helpful comments on early drafts of this study. We also thank Dr En Cheng (Yale School of Public Health) for statistical guidance.
Web extra.
Extra material supplied by authors
Web appendix: Supplemental tables
Contributors: GH and BK together collected and analyzed the data. GH wrote the first draft and BK commented on it. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted. Balazs Kovacs is the guarantor.
Funding: No relevant funding.
Competing interests statement: All authors have completed the ICMJE uniform disclosure form at www.icmje.org/coi_disclosure.pdf and declare: no support from any organization for the submitted work; no financial relationships with any organizations that might have an interest in the submitted work in the previous three years; no other relationships or activities that could appear to have influenced the submitted work.
Ethical approval: Ethical approval was not required.
Data sharing: Given our data agreement with the Centers for Disease Control and Prevention, the raw data will not be shared.
The lead author (the manuscript’s guarantor) affirms that the manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Dissemination to participants and related patient and public communities: The results of this study will be distributed to community members through press releases and blogs, including the use of lay summaries describing the research and its results.
Provenance and peer review: Not commissioned; externally peer reviewed.
Publisher’s note: Published maps are provided without any warranty of any kind, either express or implied. BMJ remains neutral with regard to jurisdictional claims in published maps.
References
- 1.CDC Injury Center. Drug overdose deaths. 2020. https://www.cdc.gov/drugoverdose/data/statedeaths.html.
- 2. Bachhuber MA, Saloner B, Cunningham CO, et al. Medical cannabis laws and opioid analgesic overdose mortality in the United States, 1999-2010. JAMA Intern Med 2014;174:1668 10.1001/jamainternmed.2014.4005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Livingston MD, Barnett TE, Delcher C, et al. Recreational cannabis legalization and opioid-related deaths in Colorado, 2000-2015. Am J Public Health 2017;107:1827-9. 10.2105/AJPH.2017.304059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Chan NW, Burkhardt J, Flyr M. The effects of recreational marijuana legalization and dispensing on opioid mortality. Econ Inq 2020;58:589-606. 10.1111/ecin.12819. [DOI] [Google Scholar]
- 5. Powell D, Pacula RL, Jacobson M. Do medical marijuana laws reduce addictions and deaths related to pain killers? J Health Econ 2018;58:29-42. 10.1016/j.jhealeco.2017.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Shover CL, Davis CS, Gordon SC, et al. Association between medical cannabis laws and opioid overdose mortality has reversed over time. Proc Natl Acad Sci USA 2019;116:12624-6. 10.1073/pnas.1903434116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Smart R, Pacula RL. Early evidence of the impact of cannabis legalization on cannabis use, cannabis use disorder, and the use of other substances: findings from state policy evaluations. Am J Drug Alcohol Abuse 2019;45:644-63. 10.1080/00952990.2019.1669626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Pacula RL, Sevigny EL. Marijuana liberalization policies: why we can’t learn much from policy still in motion: point/counterpoint. J Policy Anal Manage 2014;33:212-21. 10.1002/pam.21726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Hsu G, Koçak Ö, Kovács B. Co-opt or coexist? A study of medical cannabis dispensaries’ identity-based responses to recreational-use legalization in Colorado and Washington. Organ Sci 2018;29:172-90. 10.1287/orsc.2017.1167. [DOI] [Google Scholar]
- 10. Monnat SM, Peters DJ, Berg MT, et al. Using census data to understand county-level differences in overall drug mortality and opioid-related mortality by opioid type. Am J Public Health 2019;109:1084-91. 10.2105/AJPH.2019.305136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Wen H, Hockenberry JM. Association of medical and adult-use marijuana laws with opioid prescribing for medicaid enrollees. JAMA Intern Med 2018;178:673-9. 10.1001/jamainternmed.2018.1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Liang D, Wallace MS, Shi Y. Medical and non‐medical cannabis use and risk of prescription opioid use disorder: Findings from propensity score matching. Drug Alcohol Rev 2019;38:597-605. 10.1111/dar.12964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Shi Y, Liang D, Bao Y, et al. Recreational marijuana legalization and prescription opioids received by Medicaid enrollees. Drug Alcohol Depend 2019;194:13-9. 10.1016/j.drugalcdep.2018.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Wilson N. Drug and opioid-involved overdose deaths—United States, 2017-2018. MMWR Morb Mortal Wkly Rep 2020;69 10.15585/mmwr.mm6911a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Jalal H, Buchanich JM, Roberts MS, et al. Changing dynamics of the drug overdose epidemic in the United States from 1979 through 2016. Science 2018;361:eaau1184 10.1126/science.aau1184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Prescription Drug Abuse Policy System—PDAPS http://pdaps.org/. 2019.
- 17. Freisthler B, Gruenewald PJ. Examining the relationship between the physical availability of medical marijuana and marijuana use across fifty California cities. Drug Alcohol Depend 2014;143:244-50. 10.1016/j.drugalcdep.2014.07.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Shi Y. The availability of medical marijuana dispensary and adolescent marijuana use. Prev Med 2016;91:1-7. 10.1016/j.ypmed.2016.07.015. [DOI] [PubMed] [Google Scholar]
- 19. Freisthler B, Ponicki WR, Gaidus A, et al. A micro-temporal geospatial analysis of medical marijuana dispensaries and crime in Long Beach, California: medical marijuana dispensaries and crime. Addiction 2016;111:1027-35. 10.1111/add.13301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Liang D, Shi Y. The associations of neighborhood availability of marijuana dispensaries and DATA-2000 waivered providers with hospital stays related to opioids. Subst Use Misuse 2019;54:2387-99. 10.1080/10826084.2019.1650775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Hsu G, Kovács B, Koçak Ö. Experientially diverse customers and organizational adaptation in changing demand landscapes: a study of US cannabis markets, 2014-2016. Strateg Manag J 2019;40:2214-41. 10.1002/smj.3078. [DOI] [Google Scholar]
- 22. Seth P, Rudd RA, Noonan RK, et al. Quantifying the epidemic of prescription opioid overdose deaths. Am J Public Health 2018;108:500-2. 10.2105/AJPH.2017.304265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Gladden RM. Changes in opioid-involved overdose deaths by opioid type and presence of benzodiazepines, cocaine, and methamphetamine—25 states, July–December 2017 to January–June 2018. MMWR Morb Mortal Wkly Rep 2019;68 10.15585/mmwr.mm6834a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Prescription Drug Overdose Data & Statistics Guide to ICD-9-CM and ICD-10 Codes Related to Poisoning and Pain. Prescription Drug Overtose Team, Centers for Disease Control and Prevention; 2013. [Google Scholar]
- 25. Wooldridge JM. Introductory Econometrics: A Modern Approach. 5th ed Cengage Learning; 2012. [Google Scholar]
- 26. Romano JP, Wolf M. Stepwise multiple testing as formalized data snooping. Econometrica 2005;73:1237-82. 10.1111/j.1468-0262.2005.00615.x. [DOI] [Google Scholar]
- 27. Gujarati DN, Porter DC. Basic Econometrics. 5th ed McGraw-Hill Education, 2008. [Google Scholar]
- 28.Staggs B. Irvine’s Weedmaps delists 2,700 rogue marijuana stores, but bad actors find loopholes. Orange Cty. Regist. 2020.https://www.ocregister.com/weedmaps-makes-good-on-pledge-to-drop-rogue-marijuana-shops-though-bad-actors-find-loopholes.
- 29. Smith RA. The effects of medical marijuana dispensaries on adverse opioid outcomes. Econ Inq 2019;16 10.1111/ecin.12825. [DOI] [Google Scholar]
- 30. Lucas P, Baron EP, Jikomes N. Medical cannabis patterns of use and substitution for opioids & other pharmaceutical drugs, alcohol, tobacco, and illicit substances; results from a cross-sectional survey of authorized patients. Harm Reduct J 2019;16 10.1186/s12954-019-0278-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Meier MH, Caspi A, Ambler A, et al. Persistent cannabis users show neuropsychological decline from childhood to midlife. Proc Natl Acad Sci USA 2012;109:E2657-64. 10.1073/pnas.1206820109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Walsh Z, Gonzalez R, Crosby K, et al. Medical cannabis and mental health: a guided systematic review. Clin Psychol Rev 2017;51:15-29. 10.1016/j.cpr.2016.10.002. [DOI] [PubMed] [Google Scholar]
- 33. Aviram J, Samuelly-Leichtag G. Efficacy of cannabis-based medicines for pain management: a systematic review and meta-analysis of randomized controlled trials. Pain Physician 2017;20:E755-96. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Web appendix: Supplemental tables



