Abstract
Aging is a physiological process mediated by numerous biological and genetic pathways, which are directly linked to lifespan and are a driving force for all age-related diseases. Human life expectancy has greatly increased in the past few decades, but this has not been accompanied by a similar increase in their healthspan. At present, research on aging biology has focused on elucidating the biochemical and genetic pathways that contribute to aging over time. Several aging mechanisms have been identified, primarily including genomic instability, telomere shortening, and cellular senescence. Aging is a driving factor of various age-related diseases, including neurodegenerative diseases, cardiovascular diseases, cancer, immune system disorders, and musculoskeletal disorders. Efforts to find drugs that improve the healthspan by targeting the pathogenesis of aging have now become a hot topic in this field. In the present review, the status of aging research and the development of potential drugs for aging-related diseases, such as metformin, rapamycin, resveratrol, senolytics, as well as caloric restriction, are summarized. The feasibility, side effects, and future potential of these treatments are also discussed, which will provide a basis to develop novel anti-aging therapeutics for improving the healthspan and preventing aging-related diseases.
Keywords: Aging, Hallmarks of aging, Age‐related diseases, Anti‐aging drugs
Introduction
Since the dawn of human civilization, the desire for immortality has been a common pursuit. Due to improvements in living conditions and the continuous development of medical technology, human lifespan has increased dramatically over the last century (Campisi et al. 2019). Aging is the irreversibly progressive decline of physiological function, which eventually leads to age-related diseases, such as cardiovascular diseases, musculoskeletal disorders and arthritis, neurodegenerative diseases, and cancer. These age-related diseases produce a heavy economic and psychological burden for patients, their families, and society as a whole (de Magalhães et al. 2017). The primary feature of aging is the accumulation of cellular senescence (López-Otín et al. 2013) induced by destructive stimuli from inside and outside the cell (Hernandez-Segura et al. 2018). Cellular senescence affects the body in two ways. Firstly, excessive accumulation of senescent cells inevitably affects tissue regeneration. Secondly, senescent cells secrete a large number of inflammatory factors and present with the senescence-associated secretory phenotype (SASP), which has negative effects on the surrounding environment (López-Otín et al. 2013; Baker et al. 2016) found that although AP20187, a synthetic drug that activates FK506-binding protein-fused Casp8, effectively cleared senescent cells with high expression of p16 (Ink4a) and prolonged the lifespan of mice, some of the mice had elevated urea levels and exhibited severe thrombocytopenia (Baker et al. 2016). Bael et al. (2018) found that WM-1119, an inhibitor of the histone acetyltransferases KAT6A and KAT6B, could induce cellular senescence and arrest tumor growth in mice with lymphoma. Silva-Álvarez et al. (2020) found that the removal of senescent cells from adult zebrafish with limb amputation injuries was harmful to tissue regeneration (Da Silva-Álvarez et al. 2020). Thus, blocking cellular senescence may cause other complications. Therefore, cellular senescence is a double-edged sword when it comes to maintaining cellular balance.
Many strategies for ameliorating age-related diseases have been extensively studied, including calorie restriction through the control of diet and exercise and pharmaceutical treatments targeting specific cells and molecules (Di Daniele et al. 2017; Leong 2018). Although these treatments have achieved significant effects in various models, medication for the elderly is still a challenging issue that needs careful attention. This is because insufficient clinical data indicate that these drugs have a positive effect. On the other hand, careful consideration must also be given to the possible negative effects of these drugs. In this review, the mechanisms of aging will be described, several aging-related diseases will be identified to demonstrate the possible consequences of aging, and an analysis of the feasibility of targeted aging therapies will be performed to pave the way for future research on aging biology.
Hallmarks of aging
In order to illuminate the mechanisms and effects of anti-aging therapies on aging-related diseases, the cellular and molecular markers for aging must first be clarified. Based on the study of many different types of organisms, especially mammals, nine factors and related candidate markers are usually considered when determining the aging phenotype (López-Otín et al. 2013).
Genomic instability
One commonly accepted cause of aging is the accumulation of genetic damage, which could disrupt cell homeostasis and result in genome instability (Kubben and Misteli 2017). Somatic mutations, chromosomal aneuploidy, and copy mutations all contribute to exacerbating damage to the DNA (Tiwari and Wilson 2019). As humans age, defects appear in the DNA repair mechanism, which affects the expression of essential genes and the transcription pathways, leading to cell dysfunction. A large number of preclinical studies indicate that damaged DNA repair capability can lead to the occurrence of premature aging syndromes, such as Werner syndrome and Bloom syndrome (Foo et al. 2019). In addition, mutations in aged mitochondrial DNA and deficits in the nuclear lamina can also cause genome instability (Kauppila et al. 2018). Genome damage is closely related to aging, so interventions that can stabilize the genome and restore DNA repair capabilities should be explored to define its impact on aging.
Reduced telomere length
Telomeres are repetitive sequences at the distal ends of chromosomes. If telomeres reach a critically short length during cell division, known as the Hayflick limit, it triggers DNA damage and cellular senescence (Hayflick and Moorhead 1961; Herrmann et al. 2018). Importantly, telomere shortening also shows during natural aging in both humans and mice (Zhu et al. 2019). Also, numerous epidemiological studies have indicated that telomere depletion was significantly correlated to aging, biological morbidity, and mortality (Mensà et al. 2019). Telomerase, which is highly expressed in embryonic stem cells to extend telomeres, cannot be detected in most normal human cells (Saretzki 2018). Ullah et al. (2019) found that impaired telomerase activity accelerated senescence of stem cells (Ullah and Sun 2019). Jesus et al. (2012) reported that activation of telomerase activity through viral transduction could extend the survival time and reduce the incidence of cancer in wild-type mice (de Jesus et al. 2012). Notably, cells with short telomeres may escape senescence and become immortalized, usually by activating or upregulating telomerase. However, most human cancers have shorter telomeres and increased activity of telomerase (Shay 2016). Or it can be thought of in another way that the senescence caused by the shorter telomeres and limited telomerase activity may be the mechanism that prevents tumorigenesis in some large and long-lived mammals. There are several telomerase inhibitors in clinical phase II trials for the treatment of various cancers (Shay 2016). Telomere shortening can cause mammalian aging, while telomerase can reverse this phenomenon. Therefore, telomerase and its regulation of telomere length are important therapeutic targets for cancer and age-related diseases. Therefore, targeting telomeres or telomerase may be a strategy for developing innovative drug therapies to delay aging.
Epigenetic alterations
Modifications of chromatin include alterations in DNA methylation, histone modifications, and chromatin remodeling, which are related to cell aging (Kane and Sinclair 2019). Sirtuin families have been studied extensively as potential anti-aging factors. Ravi et al. (2019) reported that SIRT6 gene deletion severely affects cardiac function in mice and that inhibition of mTOR or Sp1 can eliminate the negative effects of SIRT6 gene deletion (Ravi et al. 2019). In addition, SIRT1 and SIRT3 genes all contribute to the improvement of healthy aging in mammals (Morigi et al. 2018). With aging, mammalian cells undergo global and local DNA hypomethylation (Kane and Sinclair 2019). Maierhofer et al. (2019) confirmed that DNA methylation and histone modifications were increased in mouse models of the premature aging syndrome (Maierhofer et al. 2019). However, there is still no evidence that DNA methylation can be changed to prolong life. It was shown that epigenetic changes could be reversed to some extent (Chen and Kerr 2019). Azacitidine and decitabine are epigenetic modifiers that have been approved by the FDA for treating myelodysplastic syndromes (MDS) and acute myeloid leukemia (AML). In clinical trials, both compounds have been shown to improve patients’ pathology results while extending their average life expectancy (Kantarjian et al. 2012). Overall, understanding and manipulating the epigenome holds promise for improving age-related pathologies and extending a healthy lifespan.
Loss of proteostasis
The occurrence of aging and most aging-related diseases are related to the impairment of protein homeostasis. Protein aggregation, post-translational modification, and altered protein turnover are hallmarks of aging (Basisty et al. 2018). Autophagy and the ubiquitin-proteasome system are the primary protein degradation systems of the cells (Kaushik and Cuervo 2015; Klaips et al. 2018), and their activity declines with aging. Studies showed that the autophagy activators, such as rapamycin and spermidine, could extend the lifespan of yeast, nematodes, fruit flies, and mice (Wong et al. 2020). In addition, reducing protein synthesis by inhibiting the mTOR signaling pathway and calorie restriction also prolongs the lifespan (Basisty et al. 2018). Sorrentino et al. (2017) reported that maintaining protein homeostasis could reduce the aggregation of amyloid protein in Alzheimer’s disease (AD) transgenic nematodes and mice and increased the lifespan of the test animals to a certain extent (Sorrentino et al. 2017). Collectively, studies on protein synthesis, quality control, and degradation pathways strongly suggest that maintenance of proteostasis is essential for health and longevity.
Deregulated nutrient sensing
Nutrient sensing through insulin/IGF-1 (IIS) was the first pathway demonstrated to regulate aging and age-related diseases in organisms. Pharmacological or caloric restriction (CR) targeting nutrient signaling pathways have been shown to attenuate aging in many organisms (Santos et al. 2016). Attenuating the signaling activity of the IIS pathway consistently extended the lifespan (Mathew et al. 2017). Bitto et al. (2016) stated that transient rapamycin treatment could inhibit the mTOR signaling pathway, thereby extending the lifespan of middle-aged mice (Bitto et al. 2016). Downregulation of mTORC1 expression also improved the average lifespan of yeast, elegans, and fruit flies (Arriola Apelo and Lamming 2016). The other two sensors in the IIS axis are AMPK and sirtuins. Emerging studies have demonstrated that metformin could activate the AMPK signaling pathway to extend the lifespan. Salminen et al. (2017) found that fibroblast growth factor 21 (FGF21) could extend the lifespan of mammals by activating AMPK signaling (Salminen et al. 2017). Studies also showed that CR could extend the lifespan of these model organisms by regulating the sirtuin family (Kapahi et al. 2017). Therefore, the synthesis and decomposition pathways of nutrient metabolism should be considered for targeted anti-aging therapies. Meanwhile, the complexity of certain signal pathways should also be deliberated. For example, the inhibition of mTOR will cause slow wound healing, insulin resistance, and other adverse reactions such as induced cataracts (Zaza et al. 2018).
Cellular senescence
Cellular senescence is a state of cell cycle arrest (Hernandez-Segura et al. 2018). The general view holds that aging is caused by a large accumulation of senescent cells in the tissue. The senescence-related secreted phenotype (SASP) and DNA damage are the main factors leading to senescence (Hernandez-Segura et al. 2017). In addition, mitochondrial dysfunction-associated senescence (MiDAS) is associated with mild or no transcriptional induction of several SASP factors (Wiley et al. 2016). For instance, inhibition of the IL-1 receptor reduced the expression of SASP and partially prevented oncogene-induced senescence (OIS) (Acosta et al. 2013). At the same time, many SASP factors exert non-cell-autonomous function and cause neighboring cells to age (Acosta et al. 2008; Ritschka et al. 2017). The critical role of p16INK4a and p53 in the induction of cell senescence has favored the hypothesis that they contribute to physiological aging (López-Otín et al. 2013). Cao et al. (2003) showed that the aging status of premature mutant mice can be significantly reduced by eliminating p16INK4a or p53, which was consistence with the findings of other groups (Baker et al. 2011; Cao et al. 2003). However, mice with a mild and systemic increase in p16INK4a, p19ARF, or p53 tumor suppressors exhibited an extended lifespan (Matheu et al. 2007). However, it is worth noting that cellular senescence can also be beneficial. In fact, senescence is a potent anti-cancer mechanism that, as mentioned earlier, can prevent malignancy by limiting the replication of preneoplastic cells in the early stage. Several drugs, such as docetaxel, bleomycin, cyclophosphamide, doxorubicin, that are used in the clinical treatment of cancer are formally based on this feature of cellular aging known as therapy-induced senescence (TIS) (Calcinotto et al. 2019). In summary, cell senescence is a double-edged sword, which can either present a beneficial compensatory response to damage, or accelerate aging by exhausting tissue regeneration. Therefore, it is necessary to consider these two processes when developing new interventions.
Stem cell exhaustion
The loss of regenerative ability in tissues and organs is also one of the important features that cause aging. For example, with advancing age, the activity of hematopoietic stem cells decreases, which can lead to a series of pathological manifestations, such as a reduced adaptive immune response, an increased risk of anemia, and a decreased number of lymphoid cells (Goodell and Rando 2015). The same problem occurs in intestinal stem cells (ISCs). Compared with young mice, the number of ISCs in older mice is maintained at a lower level, resulting in a breakdown in intestinal structure and function (Keyes and Fuchs 2018). An important debate regarding the decline in stem cell function is the relative role of cell-intrinsic compared to cell-extrinsic pathways (Conboy and Rando 2012). Transplantation of muscle-derived stem cells from young mice to progeroid mice extended their lifespan and improved tissue function even though donor cells were not detected, suggesting that their therapeutic benefit may derive from systemic effects caused by secreted factors (Lavasani et al. 2012). Furthermore, using a parabiosis model, it has been demonstrated that the decline in neural and muscle stem cell function in old mice can be reversed by systemic factors from young mice (Xiong et al. 2018). Overall, targeting the senescence of stem cells has become a challenging problem that may provide novel concepts for therapeutic intervention.
Mitochondrial dysfunction
Mitochondria dysfunction could cause a deficit in the respiratory chain, increased reactive oxygen species (ROS) production, reduced ATP levels (Green et al. 2011; Harman 1965), promote apoptosis and trigger inflammation, which causes a variety of age-related diseases. However, numerous studies have shown that increased mitochondrial ROS production and oxidative damage cannot reduce the lifespan of model organisms (Kauppila et al. 2017). This is because it is only when the ROS level exceeds a certain threshold that age-related damage is aggravated (Hekimi et al. 2011). Hood et al. (2019) pointed out that an imbalance in the mitochondrial network and impaired mitochondrial function will lead to an imbalance in the metabolic state of skeletal muscle and a decrease in muscle mass. Exercise can slow the aging process caused by mitochondrial imbalance (Hood et al. 2019). However, it is still uncertain whether improving mitochondrial function can delay aging and prevent or treat age-related diseases.
Altered intercellular communication
Cellular communication also plays an important role in the aging process by regulating neuroendocrine, endocrine, and neuronal levels (Diamanti-Kandarakis et al. 2017). Neurohormonal signalings (e.g., renin-angiotensin, adrenergic, and insulin-IGF1 signaling) tend to mediate aging as inflammatory reactions increase, and the immunosurveillance environment changes (Salminen et al. 2012). Inflammation could be caused by the accumulation of proinflammatory cytokine secretion in senescent cells, an altered autophagy response, and increased NF-κB signaling (Green et al. 2011; Salminen et al. 2012; Senovilla et al. 2012). Genetic and pharmacological inhibition of NF-κB signaling could prevent age-related features in aging mouse models (Osorio et al. 2012). Inflammation and stress can activate the NF-κB signaling pathway in the hypothalamus, resulting in reduced GnRH. GnRH treatment can prevent impaired neurogenesis and slow down the aging process in mice (Zhang et al. 2013). Similar results also occurred in sirtuins. Pharmacological activation of SIRT1 may prevent inflammation in mice (Gillum et al. 2011). SIRT2 and SIRT6 also down-regulate inflammation through deacetylating NF-κB subunits and suppressing the downstream target genes (Kawahara et al. 2009; Yuan et al. 2016). In addition, cellular senescence influences neighboring cells via gap-junction contacts, growth factors, interleukins, and ROS, highlighting the importance of the microenvironment in modulating aging at different levels (Nelson et al. 2018). A large number of studies have shown that the change in intercellular communication is closely related to senescence. In a recent follow-up study, metformin significantly inhibited the expression of pro-inflammatory cytokines and reduced the associated risk of death in elderly diabetic patients (Tizazu et al. 2019). In primary hepatocytes, metformin inhibits TNF-α-dependent NF-κB signaling and the expression of IL-6 and IL-1β by its unique anti-hyperglycemic mechanism (Cameron et al. 2016; Moiseeva et al. 2013). Resveratrol could also significantly reduce the peripheral secretion of inflammatory factors in patients with grade one hypertension by improving intercellular communication (Li et al. 2018). As such, cellular senescence interferes with tissue homeostasis and regeneration and is responsible for aging-related diseases (van Deursen 2014). On the other hand, senescent cells can also play an active role in embryogenesis and tissue remodeling. For example, senescence is an effective barrier against tumorigenesis (Calcinotto et al. 2019). In the following, age-related diseases associated with cellular senescence and the potential targets of anti-aging drugs, from a theoretical basis of the mechanisms behind aging-related diseases, will be discussed.
Age‐related diseases
Aging is the driving factor of various age-related diseases, and it causes a significant burden on social and economic stability. Based on the study of the Global Burden of Disease in 2017(GBD 2017), 92 of 293 (31.4%) diseases were determined to be age-related (Lublóy 2020). The most common aging-related diseases included neurodegenerative diseases, cancer, cardiovascular diseases, and metabolic diseases.
Neurodegenerative diseases
Aging is the most common risk factor for the development of neurodegenerative diseases. Alzheimer’s disease (AD) is the most common neurodegenerative disease in the world, and its incidence increases with advancing age (Trevisan et al. 2019). The characteristics of AD include extracellular amyloid plaques, intracellular neurofibrillary tangles (NFTs), and hyperphosphorylation of Tau protein (Xia et al. 2018; Janczura et al. 2018). Janczura et al. (2018) and Graff et al. (2012) found that histone acetylation was significantly reduced in the brains of AD patients and mice. Indirectly enhancing histone acetylation by chronic inhibition of histone deacetylases (HDACs) was able to reverse the cognitive deficits in a mouse model of AD (Kilgore et al. 2010). Aged mice and humans have a reduction in the number of neurons compared to their younger counterparts (Donev et al. 2009; Fabricius et al. 2013). Also, brain aging is mainly manifested by a large panel of pro-inflammatory factors characterized by SASP, altered signaling, and the accumulation of senescent glia (Harry 2013). The role of microglia in AD pathogenesis is complex (Wyss-Coray and Rogers 2012). Normally, microglia plays the role of a “scavenger”, which is the main phagocytic cell in the brain, and performing a central role in the clearance of Aβ. However, the effectiveness of this clearance decreases with the development of AD (Njie et al. 2012; Olah et al. 2018) reported elderly microglia to have a more inflammatory phenotype (Olah et al. 2018). These findings showed that aged microglia presented both impaired neuroprotective abilities and low-grade neuroinflammation, but sustained secretion of the SASPs that drive inflammation in neurodegeneration. Additionally, reactive astrocytes are induced in various human neurodegenerative diseases, including AD (Liddelow and Barres 2017). Also, the number and the neurogenesis capability of neural stem cells (NSCs) decreases with age (Apple et al. 2017; Fan et al. 2017). Conversely, transplantation of NSCs slows the progression and restores spatial memory ability in AD mice (Zhang et al. 2017).
Parkinson’s disease (PD) is also a neurodegenerative disease (Jankovic and Kapadia 2001). The prevalence of PD increases significantly, by approximately ten times, between 50 and 80 years of age (Pringsheim et al. 2014). The loss of dopaminergic neurons in the substantia nigra (SN) is considered a hallmark of PD (Kanaan et al. 2007). Several studies have shown that PD has the same cell function impairment seen in the aging process. The ubiquitin-proteasome system and lysosome in the brains of people with PD were mutated and showed histological signs of impaired function (Jankovic and Kapadia 2001). In addition, microglia cells showed increased staining intensity and transformation to activate phagocytic morphology during senescence, which occurs preferentially in the vulnerable vtSN region in PD. Compared to other sub-regions, the vtSN in elderly monkeys showed an excessively large microglia response, suggesting that the vtSN is more prone to neuroinflammation after being injured (Kanaan et al. 2008).
Cardiovascular disease
Aging has a significant effect on the heart and arterial system, leading to an increased prevalence of cardiovascular diseases (CVD), such as atherosclerosis, hypertension, myocardial infarction, and stroke (Donato et al. 2018). By 2030, about 20% of the population will be over 65 years old, and CVD will cause 40% of all deaths (Heidenreich et al. 2011). Aging cardiovascular tissues demonstrate pathological alterations, including hypertrophy, altered left ventricular (LV) diastolic function, diminished LV systolic reserve capacity, increased arterial stiffness, and impaired endothelial function (Lakatta and Levy 2003). Telomere shortening is related to the occurrence of CVD, vascular cell aging, aortic valve stenosis, cardiovascular risk factors (i.e., hypertension, type 2 diabetes, obesity, and smoking), and arterial thrombotic events. However, the causality of these associations remains uncertain (Kurz et al. 2006). The age-dependent deficiency of adrenergic signal transduction and calcium treatment, which are associated with cell aging, can also cause incompetence and reduced muscle strength of the LV, and affects exercise endurance (Paneni et al. 2017). The age-dependent changes to mitochondrial adaptor p66Shc profoundly affect the steady-state of the cardiovascular system. Clinical studies have shown that p66 Shc expression is significantly increased in stroke patients (Spescha et al. 2013, 2015) also confirmed that the production of ROS in the brain of p66 Shc-deficient mice was reduced, and the size of stroke was reduced after ischemia-reperfusion brain injury (Spescha et al. 2013). Genome instability is also a risk factor for CVD. Hutchinson–Gilford progeria syndrome, characterized by massive nuclear DNA damage, is associated with premature atherosclerosis and CVD, which leads to fatal myocardial infarction (MI) or stroke by age 13 on average (Capell et al. 2007). In addition, abnormal epigenetic modifications also affect the incidence of CVD. SIRT6 can prevent endothelial dysfunction and atherosclerosis (Xu et al. 2016). SIRT1 overexpression improves the metabolic efficiency and endothelial function of aged mice (Winnik et al. 2015). The dysregulation of angiogenic pathways is associated with age-dependent reductions in the number and functionality of stem, and progenitor cells, including circulating angiogenic cells (CACs) and bone marrow (BM) derived cells (Lähteenvuo and Rosenzweig 2012).
Cancer
From 2010 to 2030, the aging of the US population will lead to a 67% increase in the incidence of cancer among Americans over 65 years of age (Smith et al. 2009). With the accumulation of senescent cells, the expression of SASP will increase and promote an inflammatory state, enhancing the invasive capabilities and accelerating the progression of cancer (Faget et al. 2019; Hartley et al. 2017). NF-κB and p38MAPK signaling pathways play important roles in the release of SASPs, which promote epithelial-mesenchymal transition (EMT) in cancer cells (Coppé et al. 2010). Epigenetic modification is an important link between aging and cancer. Aberrant methylation patterns are observed in almost all neoplasms. For example, p21WAF1 / CIP1, p16INK4a, and the hypermethylation of these genes could drive carcinogenesis (Baylin and Ohm 2006; Li and Tollefsbol 2010). Fraga et al. (2005) found that cancer cells often exhibit losses in both histone acetylation and methylation, especially in H4 at the acetylated Lys16 and trimethylated Lys20 residues (Fraga et al. 2005). Histone acetyl dehydrogenase (HDAC) is closely related to the progression and prognosis of certain types of cancer, such as urogenital, reproductive, and gastrointestinal cancers (Li and Seto 2016). Histone deacetylase inhibitors (HDACi), such as MS-275 and SAHA, could trigger the apoptosis of advanced thyroid cancer by inhibiting HDAC1 and HDAC2 (Lin et al. 2019; Ma et al. 2019).
Immune system diseases
The immune system also undergoes dramatic aging-related changes, which could cause the body to lose its ability to fight against infection and cancer and increase the risk of autoimmune diseases (Sadighi Akha 2018). The decline of the immune system is characterized by a shift in T-cell phenotype from native to memory, fewer early progenitor B cells, an increased proportion of mature T-cells, as well as chronic low-grade inflammation (Ray and Yung 2018). Naïve CD4+ T cells isolated from older humans and mice showed lower responsiveness to T-cell receptor stimulation and altered cytokine secretion profiles compared with Naïve CD4+ T cells isolated from young hosts. Also, the function of naïve CD4+ T cells to produce antibodies against B cells was reduced (Pereira et al. 2020; Raphael et al. 2020). However, age-dependent changes in the composition of memory CD4+ T cell subsets also imply a weakened immune response to viral infections (e.g., influenza virus and vaccines) (Gustafson et al. 2020). One of the hallmarks of age-related changes in the human immune system is the accumulation of CD28− CD8+ T cells, which are absent in neonates and constitute the majority (80–90%) of circulating CD8+ T cells in the elderly. Accumulation of CD28- CD8 + T cells has also been found in viral infections such as COVID-19, which explains why the majority of patients with severe cases of COVID-19 are elderly (Pietrobon et al. 2020). In addition, naive CD4 + T cells had longer telomeres than memory CD4+T cells, and the difference in telomere length may reflect the number of cell divisions experienced by memory cells in vivo (Patrick and Weng 2019). Rufer et al. (1999) reported that telomere shortening was also found to occur during the transition from naïve to memory CD8 + T cells (Rufer et al. 1999). The aging lung is not only less functional, but it also has a reduced ability to prevent infections from environmental stresses and injuries. The aging of immune cells may lead to the development of disease. Th17 cells are predominantly observed in elderly asthmatics, in contrast to the Th2 inflammatory milieu presented in most young patients. Since Th17 cells can develop from the same lineage as anti-inflammatory regulatory T cells (Tregs), a preferential shift toward a Th17 response may reduce Tregs and promote the development of a pro-inflammatory environment in the elderly (Bullone and Lavoie 2017; Diller et al. 2016; Doe et al. 2010).
Musculoskeletal disorders
The elderly are prone to injuries and degenerative musculoskeletal disorders. Sarcopenia and osteoarthritis (OA) are among the most common aging-related musculoskeletal disorders and have a significant economic impact (Grote et al. 2019). Sarcopenia is defined as the loss of muscle mass and function with age. Skeletal muscle mass and function decline by 30–50% by age 80, with the degree of muscle mass loss being worse in the elderly who are inactive. Increased inflammation leads to further ROS generation in skeletal muscles, which increases cell apoptosis and affects skeletal muscle catabolism (Musci et al. 2020). Impaired mitochondrial function and weakened antioxidant defenses have also been found to be associated with the development of sarcopenia (Gaffney et al. 2018). In addition, a growing number of studies have linked neuromuscular remodeling to muscle atrophy. Sheth et al. (2018) found that a decline in the number of motor units occurs before the loss of muscle function, which is due to reduced muscle size and contractility (Sheth et al. 2018). IL-6 inhibition is an approved and clinically effective therapy for rheumatoid arthritis (Favalli 2020). However, Costa et al. found that IL-6 knockout mice developed more severe symptoms of OA in old age, which suggests that OA is mediated by a combination of pro- and anti-inflammatory factors (da Costa et al. 2016). Spectral tracing experiments in mice have shown that the loss of chondrocytes proliferation activities due to aging may contribute to the progression of OA (Kozhemyakina et al. 2015). Accumulated DNA damage and oxidative stress also accelerate OA, and Didier et al. found that miR-24 inhibition of p16INK4A expression prevented chondrocyte senescence (Philipot et al. 2014). In addition, OA-associated reductions in AMPK activity have been observed in aged mice, and this reduced activity indicated a significant reduction in mitochondrial biogenesis (Wang et al. 2015; Caramés et al. 2015) demonstrated a significant decrease in autophagy protein expression due to decreased AMPK activity, resulting in increased levels of apoptosis and cartilage deficit in OA mice (Caramés et al. 2015). In summary, interventions to remove senescent cells and slow down cellular senescence can be considered for treating musculoskeletal disorders such as sarcopenia and OA in the elderly.
Anti‐aging drugs
Anti-aging is a very promising and yet challenging field, which is complicated by the mechanisms of aging. Some FDA approved drugs target one or more molecules to reduce cellular damage and prolong the healthspan. Next, this review will examine examples of the data obtained for these drugs in different model organisms and clinical trials to promote future directions for the continued study of aging biology. In addition, some of the possible side effects of these drugs in humans and animal models will be discussed.
Metformin
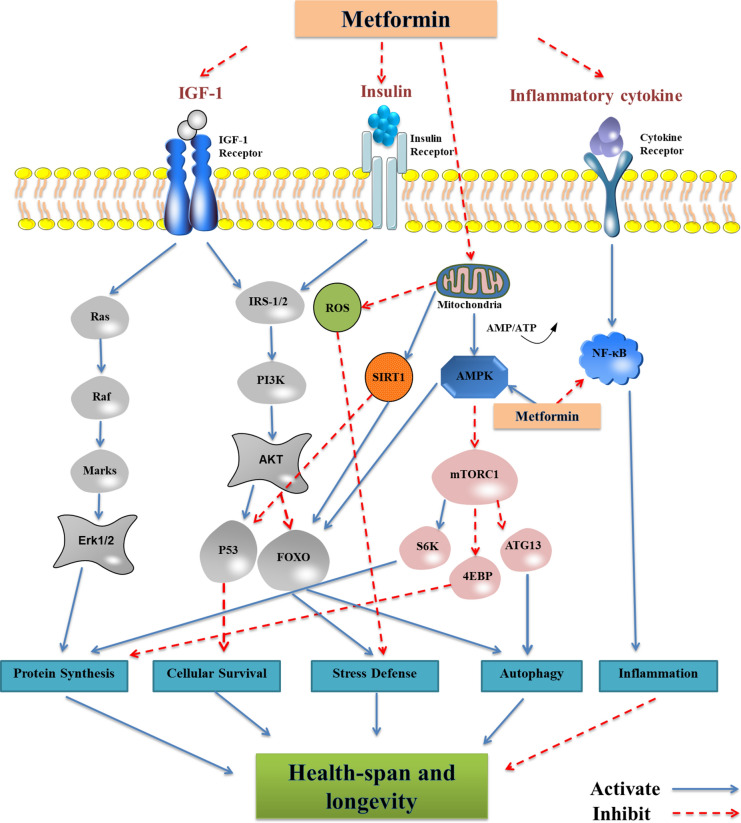
Metformin is a widely prescribed medication, which has been used to treat type 2 diabetes (T2D) in the past century (Pryor and Cabreiro 2015). At the same time, metformin has been shown to effectively reduce the pathogenesis and mortality of cardiovascular diseases (Palmer et al. 2016). Compared with other hypoglycemic drugs, elderly patients taking metformin have a lower risk of death due to cardiovascular disease (Schlender et al. 2017). In addition, recent studies have found that metformin has a positive effect on cancer, neurodegenerative diseases, and polycystic ovary syndrome (Barzilai et al. 2016). For example, metformin leads to decreased insulin levels and IGF-1 signaling (Liu et al. 2011), activation of AMPK (Cho et al. 2015), inhibition of mTOR (Nair et al. 2014; Pérez-Revuelta et al. 2014), a reduction in ROS (Batandier et al. 2006), and DNA damage (Shown in Fig. 1) (Algire et al. 2012; Cabreiro et al. 2013) found that metformin extended the lifespan of Caenorhabditis elegans by changing microbial folate and methionine metabolism (Cabreiro et al. 2013). Metformin also has positive prevention and treatment effects on aging-related diseases. After continuous injection of metformin in SAMP8 mice for eight weeks, the expression of APPc99 and pTau in the mice brain was significantly reduced, and the learning and memory abilities of the mice were significantly improved (Farr et al. 2019). Ou et al. (2018) found that metformin exerted a neuroprotective effect on APP/PS1 mice via triggering neurogenesis and anti-inflammation by regulating AMPK/mTOR/S6K/Bace1 and AMPK/P65 NF-κB signaling in the hippocampus (Ou et al. 2018). In addition, metformin inhibited SNCA phosphorylation and aggregation, reduced oxidative stress, and improved MPTP-induced motor and cognitive dysfunction in mice with PD (Lu et al. 2016; Patil et al. 2014). A survey of older adults with diabetes in Singapore also found that long-term treatment with metformin in patients with T2D may reduce the risk of dementia and cognitive impairment (Ng et al. 2014).
Fig. 1.
Metformin targets the major pathways of aging. Extracellularly, metformin decreases insulin levels and IGF-1 signaling while influencing multiple cytokines to participate in anti-aging processes. Intracellularly, metformin reduces ROS production by inhibiting mitochondrial complex I in the electron transport chain generation and AMPK activation, simultaneous increase in mTOR signal inhibition and SIRT1 activation, which resulting in a longer life-span; Metformin affects inflammatory responses, cellular stress responses and autophagy responses, etc. by acting both inside and outside the cell. These cellular processes are the primary biological responses associated with aging
In addition to glucose homeostasis, the involvement of the tumor suppressor pathway is another target for metformin’s action. A growing number of studies have shown that metformin has an inhibitory effect on some cancer cells in vivo and in vitro, such as rectal cancer and p53 mutant colon cancer (Algire et al. 2010; Buzzai et al. 2007; Gwinn et al. 2008; Hirsch et al. 2009; Hosono et al. 2010). In clinical trials, metformin also exerted excellent anti-cancer effects. A meta-analysis of diabetic patients treated with metformin and other drugs demonstrated a 30% lower incidence of cancers in metformin-allocated patients, such as breast cancer, gastric cancer, and prostate cancer (Col et al. 2012; Decensi et al. 2010; Tseng 2016). The survival rate was significantly improved for patients with pancreatic cancer who were treated with metformin (Li et al. 2017).
Although the therapeutic effect of metformin is well known for diabetes, there is evidence that long-term use of metformin may cause vitamin B12 deficiency in T2D patients and cause lactic acid accumulation in mice and humans (Aroda et al. 2016; Langan and Goodbred 2017; Marathe et al. 2017). In addition, the side effects of metformin also include irritation of the gastrointestinal tract, including diarrhea, nausea, flatulence, dyspepsia, vomiting, and abdominal discomfort, but in most cases, these symptoms are not obvious (McCreight et al. 2018). Stynen et al. (2018) reported that there are 745 proteins that are regulated by metformin treatment (Stynen et al. 2018). There is still uncertainty about whether these proteins demonstrate beneficial or potentially detrimental off-target effects when metformin is taken across the lifespan. Therefore, before providing metformin as a targeted aging drug, further research is needed to determine its broader effects, the molecular mechanism of action, and its safety implications.
Rapamycin
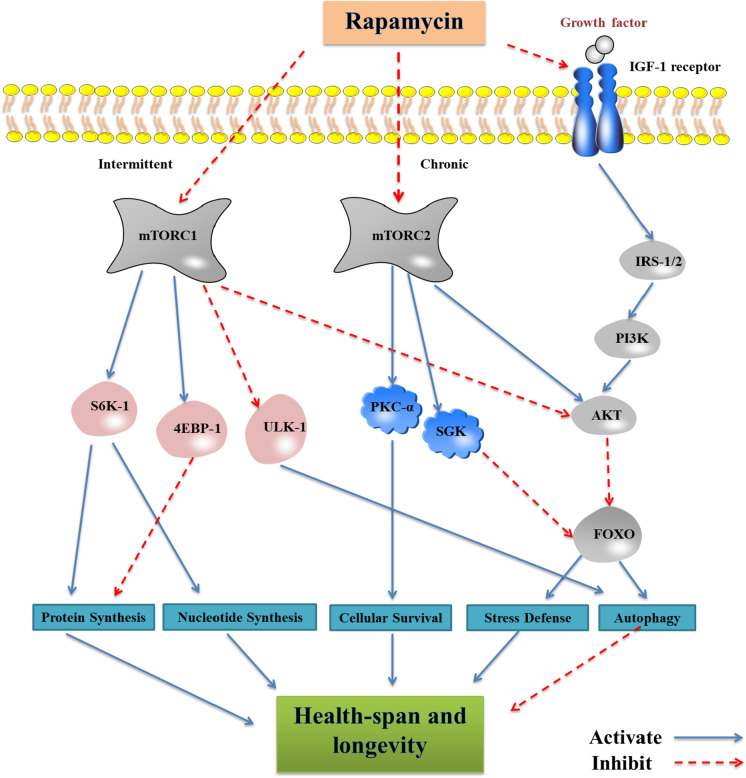
Rapamycin is a macrolide produced by Streptomyces hygroscopicus and was initially discovered as an antifungal agent. Recent studies have found that rapamycin can inhibit the mechanistic target of rapamycin (mTOR) protein kinase and extend the average lifespan of yeast, C. elegans, and fruit flies, but the role in mammals needs to be explored further (Johnson et al. 2013). Several other studies have shown that rapamycin could effectively extend the average and maximum lifespans of mice, such as C57BL/6, 129/SV, and UM-HET3 mice (Harrison et al. 2009; Anisimov et al. 2011; Chen et al. 2009; Neff et al. 2013). In addition, rapamycin has been found to inhibit tumorigenesis and extend the lifespan of many genetic early-onset models, such as p53 mutant mice, Apc mutant animals, Rb mutant mice, and HER-2/neu transgenic mice (Anisimov et al. 2010; Comas et al. 2012; Hasty et al. 2014). In addition, studies have found that rapamycin also has a neuroprotective effect. Oral rapamycin treatment could effectively improve cognitive function in elderly mice (Neff et al. 2013), reduce the pathological features of AD, and maintain the integrity of the blood-brain barrier by preventing neuronal loss and improving cognitive function (Carosi and Sargeant 2019). In addition to exhibiting excellent anti-aging effects in animal models, rapamycin has also shown unexpected results in clinical trials. A recent meta-analysis showed that rapamycin has a positive effect on tuberous sclerosis – a rare multisystem disease with the formation of benign tumors and neurological disorders (Sasongko et al. 2016). A clinical trial conducted by Chung et al. showed that topical treatment with rapamycin significantly increased p16INKA4A and collagen IV protein levels and improved the histological appearance of the subjects’ skin tissues, which suggests that rapamycin can be used to some extent as an anti-aging therapy in human beings (Chung et al. 2019). The mechanisms of the effects of rapamycin on lifespan are shown in Fig. 2.
Fig. 2.
Rapamycin regulates lifespan primarily through the mTOR signaling pathway. mTOR exists mainly in two functionally distinct complexes termed mTORC1 and mTORC2. Rapamycin inhibits mTORC1 on an intermittent basis, while long-term administration also inhibits mTORC2 in most tissues. Inhibition of mTORC1 promotes protein and nucleotide synthesis as well as autophagy responses, while also reducing cellular stress responses. These effects of rapamycin may promote longevity. In contrast, inhibition of mTORC2 leads to metabolic dysfunction and reduced lifespan, but the exact mechanism is unclear
As an FDA-approved drug, rapamycin has been used in humans as a post-transplant immunosuppressant and for the treatment of renal cell carcinoma, coronary artery stent coating, lymphovascular smooth muscle tumor, and autoimmune diseases (McCormack et al. 2011). However, various and serious negative effects limit its use. As a typical mTOR inhibitor, rapamycin acutely inhibits mTORC1, which could promote longevity partially through the inhibition of S6K1, protein translation, and increased autophagy. Conversely, a long-term overdose of rapamycin will inhibit the expression of mTORC2, which can result in metabolic dysfunction and a decrease in the lifespan of male mice through an as yet undetermined mechanism (Arriola Apelo and Lamming 2016). Therefore, further experiments are needed to determine the beneficial effects of rapamycin on mTORC1 inhibition-mediated aging and age-related diseases while minimizing the side effects associated with mTORC2.
Resveratrol
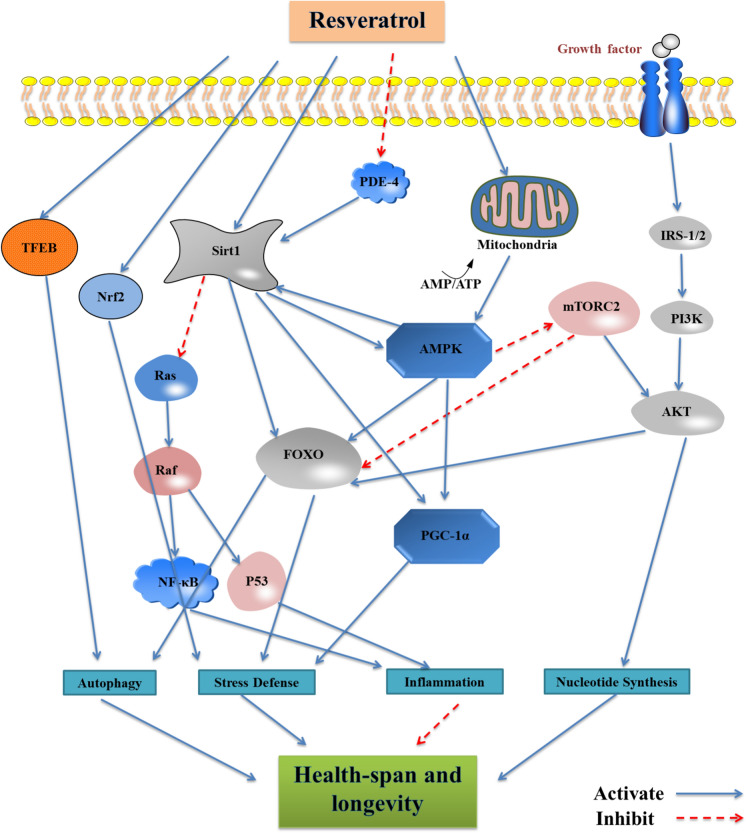
Resveratrol (3,5,4′-trihydroxystilbene) is a phytoalexin found in many plant species, such as grapes, peanuts, and berries, which could respond to mechanical injury, fungal infection, and UV radiation (Silva et al. 2019). Resveratrol mainly promotes health and lifespan in yeast and C. elegans by activating the sirtuin family (Cao et al. 2018; Howitz et al. 2003; Price et al. 2012; Wood et al. 2004). Resveratrol can promote the viability and proliferation of human umbilical cord mesenchymal stem cells (hUC-MSCs) in a dose-response manner, mitigating senescence and inducing the expression of SIRT1, while inhibiting the expression of p53 and p16 (Wang et al. 2016). Although resveratrol has not been reported to extend the lifespan of wild-type mammals, studies have shown that resveratrol supplementation can extend the lifespan of mammals with impaired metabolism. Resveratrol can reverse the physiological indicators of mice on a high-calorie diet to reduce the risk of death by about 31% (Baur et al. 2006; Gocmez et al. 2016) suggested that resveratrol was effective in preventing a cognitive deficit in AD rats by inhibiting the production of inflammatory cytokines (Gocmez et al. 2016). Resveratrol combined with hUC-MSCs transplantation could improve the learning and memory functions of AD mice and enhance neurogenesis (Wang et al. 2018). In addition, resveratrol can pass through the blood-brain barrier and act on the brain of elderly patients with AD, prevent amyloid deposition, and reduce the formation of plaque (Sawda et al. 2017) Zhang et al. (2018) showed that resveratrol alleviated motor and cognitive deficits in PD model mice in a dose-dependent manner (Zhang et al. 2018). Emerging studies have shown that resveratrol can significantly reduce overall tumor development by promoting apoptosis, regulating the cell cycle, and inhibiting Cyclooxygenase (COX) activity and prostaglandin production (Kalra et al. 2008). Resveratrol has also been found to mediate the protective effects against inflammatory diseases and cardiovascular diseases through various mechanisms (Park et al. 2012; Tsai et al. 2014; Xia et al. 2017; Zhu et al. 2018). The mechanisms of the effects of resveratrol on lifespan are shown in Fig. 3.
Fig. 3.
Resveratrol is involved in anti-aging as an activator of the sirtuin family and the Nrf2 pathway. Inhibition of mitochondrial ATP production by resveratrol leads to activation of AMPK, which enhances NAD + availability thereby overcoming the rate limitation imposed by this cofactor on SIRT1 enzyme activity. In turn, resveratrol directly activates SIRT1 thereby positively controlling AMPK activity. Together, AMPK and SIRT1 form a positive feedback pathway to prolong life by modulating multiple downstream factors. In addition, resveratrol can act directly on transcriptional regulators thus acting as an anti-inflammatory and antioxidant effect
Resveratrol has shown great promise in multiple animal models. However, its role in human clinical trials is still controversial. A 26-week intervention trial performed with 23 overweight elderly patients concluded that resveratrol supplementation might improve glucose metabolism, hippocampal functional connectivity, and memory function (Witte et al. 2014). But a recent meta-analysis showed the opposite result. A follow-up study on 225 patients showed that resveratrol did not have a positive effect on memory and cognition (Farzaei et al. 2018). In addition, Gliemann et al. (2013) showed that resveratrol supplementation reduced the positive effect of exercise training on blood pressure, blood cholesterol, and maximal oxygen uptake but did not affect the retardation of atherosclerosis (Gliemann et al. 2013). This phenomenon implies trying not to consume foods containing resveratrol during exercise. Resveratrol has been tolerated in animal experiments, but when administered in high doses, resveratrol may cause serious side effects such as diarrhea and local allergies (la Porte et al. 2010; Popat et al. 2013). In addition, resveratrol has a low bioavailability, which may limit its clinical application. A further challenge is that resveratrol is difficult to use in large-scale clinical trials at this stage.
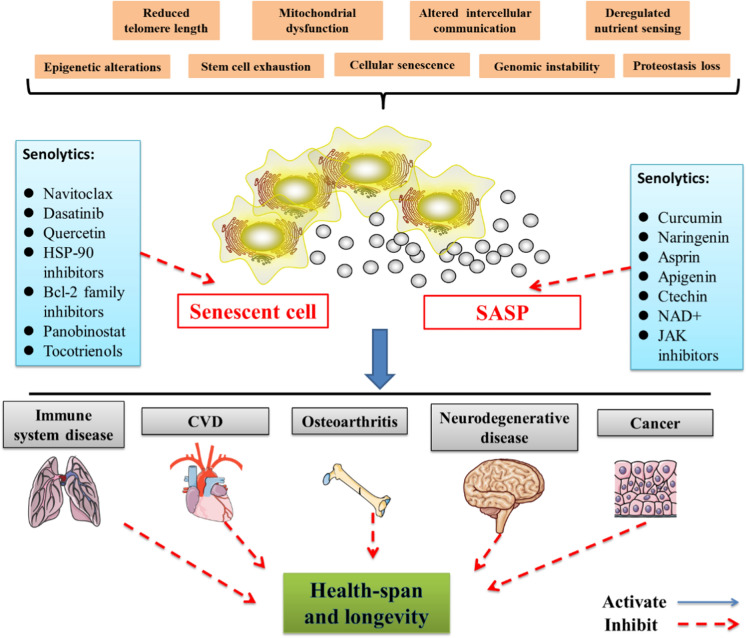
Senolytics
Senolytics, drugs that selectively clear senescent cells, have been developed recently and may be a novel strategy for extending the healthspan and lifespan. Senescent cells increase several anti-apoptotic regulators, including dependence receptors, PI3K/Akt and BCL-2, which can jointly regulate the ability of cells to resist apoptosis (Zhu et al. 2015). Dasatinib (D) and quercetin (Q) could induce apoptosis in senescent fat progenitor cells and alleviate several aging-related phenotypes in premature aging and natural aging mice induced by injury (Zhu et al. 2015). Navitoclax, a BCL-2 family inhibitor, could reduce the viability of senescent human umbilical vein epithelial cells (HUVEC) and IMR90, but it has no effects on human primary preadipocytes (Zhu et al. 2016). Other senolytics, such as ABT-737, A1331852 and A1155463 can also inhibit BCL-2 (Zhu et al. 2017) and clear senescent cells. Navitoclax could remove SASP-targeted senescent cells (SNC) during the formation of atherosclerosis (Childs et al. 2016) and prevent hematopoietic SNC from rejuvenating (Chang et al. 2016). ATB263 clears a series of senescent cancer cells and eliminates chemotherapy-induced senescent cells, reducing cancer relapse and metastasis in mouse models (Demaria et al. 2017; Wang et al. 2017). Senolytic (D + Q) treatment reduced the abundance of senescent cells in the brains of obese mice, restored neurogenesis, and reduced neuropsychiatric dysfunction (Musi et al. 2018; Ogrodnik et al. 2019; Zhang et al. 2019). In addition, senolytics may be effective for a variety of age-related diseases, such as idiopathic pulmonary fibrosis, sarcopenia, osteoarthritis, and glomerulosclerosis (Kim and Kim 2019). As research has progressed, senolytics have also shown promising results in clinical trials. Cox et al. (2015) conducted acute and chronic interventions using curcumin to treat elderly patients respectively and showed that both treatment regimens significantly improved their learning and memory abilities (Cox et al. 2015). Justice et al. (2019) found that senolytics (D + Q) significantly improved the clinical performance of 14 patients with idiopathic pulmonary fibrosis (IPF) (Justice et al. 2019). It can also effectively eliminate p16 INK4a-positive cells, reduce SA-β-gal activity, and decrease the release of inflammatory factors in diabetic nephropathy (Hickson et al. 2019; Rossman et al. 2018).
Although senolytic therapy exhibits exciting anti-aging effects, the current understanding of senolytics has its own limitations. Navitoclax has been reported to cause severe thrombocytopenia and neutropenia, and these side effects limit its application (Niedernhofer and Robbins 2018). Another potential problem is tissue atrophy, which is caused by senescent cells being largely eliminated. In addition, senolytics eliminate not only the harmful effects of senescent cells but also their beneficial effects. Although cellular senescence is the cause of aging and aging-related diseases, senescent cells can also play a positive role. For example, senescence is an effective barrier against tumorigenesis in the early stages of cancer (Calcinotto et al. 2019). Therefore, the dual biological function of senolytics must be evaluated. Furthermore, it is necessary to advance the current version of senolytics by improving its targeting capability and selectively inhibiting its harmful effects on cells and tissues. Precise clinical trials of senolytics therapy have not yet been performed. More translational studies should also be considered.
Caloric restriction
Recently, progressively more research has recommended caloric restriction (CR) to reduce obesity-induced aging-related diseases (Salvestrini et al. 2019). The aim of CR is to reduce calorie intake without malnutrition and to improve the viability of organisms (Broskey et al. 2019). An accumulating number of studies have reported that CR has a positive effect on DNA repair and telomere mechanisms. The incidence of tumors in TERT transgenic (TgTERT) mice was significantly reduced with CR, which also prolonged their lifespan compared to wild-type (WT) controls under the same diet (Vera et al. 2013). Reducing calorie intake can increase metabolic efficiency and prevent cell damage (Picca et al. 2017). It can also extend the lifespan of rodents and humans by reducing insulin, glucose, and the IGF-1 signaling pathway (Hwangbo et al. 2020; Pifferi and Aujard 2019a). In mammals, it is clear that CR induces the expression and activity of sirtuins in many tissues, which are closely related to aging (Imai and Guarente 2010). The positive effects of CR on inflammation and insulin resistance have been demonstrated in a rat model of age-associated inflammation by regulating GSH redox status and NF-κB, SIRT1, and FoxOs (Chung et al. 2011; Horrillo et al. 2011). Important improvements were shown in the onset and development of CVD and diabetes. The incidence of CVD is reduced with CR by controlling the mechanisms of maintaining cardiac activity, such as autophagy, proteasome-mediated turnover, apoptosis, and mitochondrial quality, to control its effects during aging (Rattan 2014). PGC-1α expression and mitochondrial biogenesis stimulated by AMPK and SIRT1 in muscle have been associated with the reduction of insulin resistance, and the use of CR or CR mimickers, such as resveratrol or metformin, contribute to preventing the onset and the progression of the diseases (Gerhart-Hines et al. 2007). Human clinical trials have also demonstrated positive effects of CR (Lorenzini 2014). A survey by Most et al. (2018) showed that continuous CR in healthy, nonobese individuals could reduce the incidence of cardiovascular disease by 30% (Most et al. 2018). Redman and Simin found that long-term CR without malnutrition could enhance the efficiency of resting energy expenditure, thereby reducing oxidative damage to tissues and organs (Redman et al. 2018), and inducing significant suppression of inflammation, as shown by a two-year CR dietary intervention (Meydani et al. 2016).
Despite the positive effects of moderate CR on human aging, some of the possible negative effects of CR should also be considered. As people get older, physiological reserves diminish, leading to reduced resistance to various stressors. In the case of malnutrition, these adverse factors can be magnified-a problem that faces many older people. Therefore, CR should not be used as a potential intervention for treating diseases in this specific population (Pifferi and Aujard 2019b). Also, people with a low body mass index (BMI, less than 21 kg/m2) should also be cautious of utilizing CR, as this could lead to rapid weight loss and thus increase the risk of further health problems (Le Bourg and Redman 2018). In addition, a study by McGrath et al. found that exercise could cause bone loss and appeared to be harmful to the bones of mice in the CR group compared to the control group (McGrath et al. 2020). Clinical studies have also found that CR could decrease bone mineral density as well as increase the risk of osteoporotic fractures compared to a control group (Villareal et al. 2016). Therefore, before engaging in CR as a therapy to slow down the aging process, many factors, such as the patient’s physical condition, mental state, and BMI, should be taken into consideration. Blindly engaging in dieting or CR should not be promoted (Fig. 4).
Fig. 4.
Senolytic therapies target aging. During the aging process, senescent cells accumulate in large amounts in tissues and are associated with the development of various age-related diseases. Senolytics can help slow down the aging process by eliminating the accumulation of senescent cells, reducing age-related diseases and prolonging healthspan. Uncontrolled activation of SASP can cause chronic inflammation, leading to tissue dysfunction, this ultimately leads to aging and age-related diseases. Senolytics also can positively impact aging-related diseases by modulating the regulatory network of SASP in senescent cells and by inhibiting SASP from exerting its deleterious effects
Conclusions
Medicine has undergone a gradual shift in its underlying concept, from “sick care” to “health care”.That is to say, medicine is moving away from focusing on treatments after the occurrence of a disease towards intervening before the recognized risk factors progress to disease onset. Defining the hallmarks of aging helps to establish a framework of aging-related mechanisms and thus provides theoretical support for improving human health and extending the lifespan. Due to the continuously growing trend of an aging population, the anti-aging strategy is undoubtedly an increasingly important area for the pharmaceutical industry and public health organizations. However, considering the limitations and side effects of anti-aging drugs, there are presently too many concerns that need further clarification. Therefore, collaborative efforts from multidisciplinary researchers are required to advance these potential treatment strategies.
Funding
This study was supported by National Natural Science Foundation of China (U2004201), Central Plains Thousand People Plan of Henan Province (204200510013), and Training plan for young excellent teachers in Colleges and Universities of Henan (2020GGJS008).
Compliance with ethical standards
Conflict of interest
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Shanshan Ma, Email: mashanshan84@163.com.
Fangxia Guan, Email: guanfangxia@126.com.
References
- Acosta JC, et al. Chemokine signaling via the CXCR2 receptor reinforces senescence. Cell. 2008;133:1006–1018. doi: 10.1016/j.cell.2008.03.038. [DOI] [PubMed] [Google Scholar]
- Acosta JC, et al. A complex secretory program orchestrated by the inflammasome controls paracrine senescence. Nat Cell Biol. 2013;15:978–990. doi: 10.1038/ncb2784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Algire C, Amrein L, Zakikhani M, Panasci L, Pollak M. Metformin blocks the stimulative effect of a high-energy diet on colon carcinoma growth in vivo and is associated with reduced expression of fatty acid synthase . Endocr Relat Cancer. 2010;17:351–360. doi: 10.1677/erc-09-0252. [DOI] [PubMed] [Google Scholar]
- Algire C, et al. Metformin reduces endogenous reactive oxygen species and associated DNA damage. Cancer Prev Res. 2012;5:536–543. doi: 10.1158/1940-6207.capr-11-0536. [DOI] [PubMed] [Google Scholar]
- Anisimov VN, et al. Rapamycin extends maximal lifespan in cancer-prone mice. Am J Pathol. 2010;176:2092–2097. doi: 10.2353/ajpath.2010.091050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anisimov VN, et al. Rapamycin increases lifespan and inhibits spontaneous tumorigenesis in inbred female mice. Cell Cycle. 2011;10:4230–4236. doi: 10.4161/cc.10.24.18486. [DOI] [PubMed] [Google Scholar]
- Apple DM, Solano-Fonseca R, Kokovay E. Neurogenesis in the aging brain. Biochem Pharmacol. 2017;141:77–85. doi: 10.1016/j.bcp.2017.06.116. [DOI] [PubMed] [Google Scholar]
- Aroda VR, et al. Long-term metformin use and vitamin B12 deficiency in the diabetes prevention program outcomes study. J Clin Endocrinol Metab. 2016;101:1754–1761. doi: 10.1210/jc.2015-3754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arriola Apelo SI, Lamming DW. Rapamycin: an inhibiTOR of aging emerges from the soil of Easter Island. J Geront Ser A. 2016;71:841–849. doi: 10.1093/gerona/glw090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker DJ, et al. Clearance of p16Ink4a-positive senescent cells delays ageing-associated disorders. Nature. 2011;479:232–236. doi: 10.1038/nature10600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker DJ, et al. Naturally occurring p16(Ink4a)-positive cells shorten healthy lifespan. Nature. 2016;530:184–189. doi: 10.1038/nature16932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barzilai N, Crandall JP, Kritchevsky SB, Espeland MA. Metformin as a tool to target aging. Cell Metab. 2016;23:1060–1065. doi: 10.1016/j.cmet.2016.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Basisty N, Meyer JG, Schilling B. Protein turnover in aging longevity. Proteomics. 2018;18:e1700108. doi: 10.1002/pmic.201700108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Batandier C, Guigas B, Detaille D, El-Mir MY, Fontaine E, Rigoulet M, Leverve XM. The ROS production induced by a reverse-electron flux at respiratory-chain complex 1 is hampered by metformin. J Bioenerg Biomembr. 2006;38:33–42. doi: 10.1007/s10863-006-9003-8. [DOI] [PubMed] [Google Scholar]
- Baur JA, et al. Resveratrol improves health and survival of mice on a high-calorie diet. Nature. 2006;444:337–342. doi: 10.1038/nature05354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baylin SB, Ohm JE. Epigenetic gene silencing in cancer: a mechanism for early oncogenic pathway addiction? Nat Rev Cancer. 2006;6:107–116. doi: 10.1038/nrc1799. [DOI] [PubMed] [Google Scholar]
- Bitto A, et al. Transient rapamycin treatment can increase lifespan and healthspan in middle-aged mice. eLife. 2016 doi: 10.7554/eLife.16351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Broskey NT, Marlatt KL, Most J, Erickson ML, Irving BA, Redman LM. The panacea of human aging: calorie restriction versus exercise. Exer Sport Sci Rev. 2019;47:169–175. doi: 10.1249/jes.0000000000000193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bullone M, Lavoie JP. The contribution of oxidative stress and inflamm-aging in human and equine asthma. Int J Mol Sci. 2017 doi: 10.3390/ijms18122612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buzzai M, et al. Systemic treatment with the antidiabetic drug metformin selectively impairs p53-deficient tumor cell growth. Cancer Res. 2007;67:6745–6752. doi: 10.1158/0008-5472.can-06-4447. [DOI] [PubMed] [Google Scholar]
- Cabreiro F, et al. Metformin retards aging in C. elegans by altering microbial folate and methionine metabolism. Cell. 2013;153:228–239. doi: 10.1016/j.cell.2013.02.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calcinotto A, Kohli J, Zagato E, Pellegrini L, Demaria M, Alimonti A. Cellular senescence: aging, cancer, and injury. Physiol Rev. 2019;99:1047–1078. doi: 10.1152/physrev.00020.2018. [DOI] [PubMed] [Google Scholar]
- Cameron AR, et al. Anti-inflammatory effects of metformin irrespective of diabetes status. Circ Res. 2016;119:652–665. doi: 10.1161/circresaha.116.308445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campisi J, Kapahi P, Lithgow GJ, Melov S, Newman JC, Verdin E. From discoveries in ageing research to therapeutics for healthy ageing. Nature. 2019;571:183–192. doi: 10.1038/s41586-019-1365-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cao L, Li W, Kim S, Brodie SG, Deng CX. Senescence, aging, and malignant transformation mediated by p53 in mice lacking the Brca1 full-length isoform. Genes Dev. 2003;17:201–213. doi: 10.1101/gad.1050003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cao W, Dou Y, Li A. Resveratrol boosts cognitive function by targeting SIRT1. Neurochem Res. 2018;43:1705–1713. doi: 10.1007/s11064-018-2586-8. [DOI] [PubMed] [Google Scholar]
- Capell BC, Collins FS, Nabel EG. Mechanisms of cardiovascular disease in accelerated aging syndromes. Circ Res. 2007;101:13–26. doi: 10.1161/circresaha.107.153692. [DOI] [PubMed] [Google Scholar]
- Caramés B, Olmer M, Kiosses WB, Lotz MK. The relationship of autophagy defects to cartilage damage during joint aging in a mouse model. Arthrit Rheumatol. 2015;67:1568–1576. doi: 10.1002/art.39073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carosi JM, Sargeant TJ. Rapamycin and Alzheimer disease: a double-edged sword? Autophagy. 2019;15:1460–1462. doi: 10.1080/15548627.2019.1615823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang J, et al. Clearance of senescent cells by ABT263 rejuvenates aged hematopoietic stem cells in mice. Nat Med. 2016;22:78–83. doi: 10.1038/nm.4010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen C, Liu Y, Liu Y, Zheng P. mTOR regulation and therapeutic rejuvenation of aging hematopoietic stem cells. Sci Signal. 2009;2:75. doi: 10.1126/scisignal.2000559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen D, Kerr C. The epigenetics of stem cell aging comes of age. Trends Cell Biol. 2019;29:563–568. doi: 10.1016/j.tcb.2019.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Childs BG, Baker DJ, Wijshake T, Conover CA, Campisi J, van Deursen JM. Senescent intimal foam cells are deleterious at all stages of atherosclerosis . Science. 2016;354:472–477. doi: 10.1126/science.aaf6659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cho K, et al. Antihyperglycemic mechanism of metformin occurs via the AMPK/LXRα/POMC pathway. Sci Rep. 2015;5:8145. doi: 10.1038/srep08145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chung HY, et al. Molecular inflammation as an underlying mechanism of the aging process and age-related diseases. J Dent Res. 2011;90:830–840. doi: 10.1177/0022034510387794. [DOI] [PubMed] [Google Scholar]
- Chung CL, et al. Topical rapamycin reduces markers of senescence and aging in human skin: an exploratory, prospective, randomized trial. GeroScience. 2019;41:861–869. doi: 10.1007/s11357-019-00113-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Col NF, Ochs L, Springmann V, Aragaki AK, Chlebowski RT. Metformin and breast cancer risk: a meta-analysis and critical literature review. Breast Cancer Res Treatm. 2012;135:639–646. doi: 10.1007/s10549-012-2170-x. [DOI] [PubMed] [Google Scholar]
- Comas M, et al. New nanoformulation of rapamycin Rapatar extends lifespan in homozygous p53-/- mice by delaying carcinogenesis. Aging. 2012;4:715–722. doi: 10.18632/aging.100496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conboy IM, Rando TA. Heterochronic parabiosis for the study of the effects of aging on stem cells and their niches. Cell Cycle. 2012;11:2260–2267. doi: 10.4161/cc.20437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coppé JP, Desprez PY, Krtolica A, Campisi J. The senescence-associated secretory phenotype: the dark side of tumor suppression. Ann Rev Pathol. 2010;5:99–118. doi: 10.1146/annurev-pathol-121808-102144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cox KH, Pipingas A, Scholey AB. Investigation of the effects of solid lipid curcumin on cognition and mood in a healthy older population. J Psychopharmacol. 2015;29:642–651. doi: 10.1177/0269881114552744. [DOI] [PubMed] [Google Scholar]
- da Costa JP, Vitorino R, Silva GM, Vogel C, Duarte AC, Rocha-Santos T. A synopsis on aging-theories, mechanisms and future prospects. Ageing Res Rev. 2016;29:90–112. doi: 10.1016/j.arr.2016.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Da Silva-Álvarez S, Guerra-Varela J, Sobrido-Cameán D, Q uelle A, Barreiro-Iglesias A, Sánchez L, Collado M. Cell senescence contributes to tissue regeneration in zebrafish. Aging Cell. 2020;19:e13052. doi: 10.1111/acel.13052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Jesus BB, Vera E, Schneeberger K, Tejera AM, Ayuso E, Bosch F, Blasco MA. Telomerase gene therapy in adult and old mice delays aging and increases longevity without increasing cancer. EMBO Mol Med. 2012;4:691–704. doi: 10.1002/emmm.201200245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Magalhães JP, Stevens M, Thornton D. The business of anti-aging. Sci Trends Biotechnol. 2017;35:1062–1073. doi: 10.1016/j.tibtech.2017.07.004. [DOI] [PubMed] [Google Scholar]
- Decensi A, Puntoni M, Goodwin P, Cazzaniga M, Gennari A, Bonanni B, Gandini S. Metformin and cancer risk in diabetic patients: a systematic review and meta-analysis. Cancer Prevent Res. 2010;3:1451–1461. doi: 10.1158/1940-6207.capr-10-0157. [DOI] [PubMed] [Google Scholar]
- Demaria M, et al. Cellular senescence promotes adverse effects of chemotherapy and cancer relapse. Cancer Discov. 2017;7:165–176. doi: 10.1158/2159-8290.cd-16-0241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Daniele N, et al. Impact of Mediterranean diet on metabolic syndrome cancer longevity. Oncotarget. 2017;8:8947–8979. doi: 10.18632/oncotarget.13553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diamanti-Kandarakis E, et al. Mechanisms in endocrinology: aging and anti-aging: a combo-endocrinology overview. Eur J Endocrinol. 2017;176:R283–Rr308. doi: 10.1530/eje-16-1061. [DOI] [PubMed] [Google Scholar]
- Diller ML, Kudchadkar RR, Delman KA, Lawson DH, Ford ML. Balancing inflammation: the link between Th17 and regulatory T cells. Mediat Inflamm. 2016;2016:6309219. doi: 10.1155/2016/6309219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doe C, et al. Expression of the T helper 17-associated cytokines IL-17A and IL-17F in asthma and COPD. Chest. 2010;138:1140–1147. doi: 10.1378/chest.09-3058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donato AJ, Machin DR, Lesniewski LA. Mechanisms of dysfunction in the aging vasculature and role in age-related. Dis Circ Res. 2018;123:825–848. doi: 10.1161/circresaha.118.312563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donev R, Kolev M, Millet B, Thome J. Neuronal death in Alzheimer’s disease and therapeutic opportunities. J Cell Mol Med. 2009;13:4329–4348. doi: 10.1111/j.1582-4934.2009.00889.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fabricius K, Jacobsen JS, Pakkenberg B. Effect of age on neocortical brain cells in 90+ year old human females: a cell counting study. Neurobiol Aging. 2013;34:91–99. doi: 10.1016/j.neurobiolaging.2012.06.009. [DOI] [PubMed] [Google Scholar]
- Faget DV, Ren Q, Stewart SA. Unmasking senescence: context-dependent effects of SASP in cancer. Nat Rev Cancer. 2019;19:439–453. doi: 10.1038/s41568-019-0156-2. [DOI] [PubMed] [Google Scholar]
- Fan X, Wheatley EG, Villeda SA. Mechanisms of hippocampal aging and the potential for rejuvenation. Annu Rev Neurosci. 2017;40:251–272. doi: 10.1146/annurev-neuro-072116-031357. [DOI] [PubMed] [Google Scholar]
- Farr SA, Roesler E, Niehoff ML, Roby DA, McKee A, Morley JE. Metformin improves learning and memory in the SAMP8 mouse model of Alzheimer’s disease. J Alzheimer’s Dis. 2019;68:1699–1710. doi: 10.3233/jad-181240. [DOI] [PubMed] [Google Scholar]
- Farzaei MH, Rahimi R, Nikfar S, Abdollahi M. Effect of resveratrol on cognitive and memory performance and mood: a meta-analysis of 225 patients. Pharmacol Res. 2018;128:338–344. doi: 10.1016/j.phrs.2017.08.009. [DOI] [PubMed] [Google Scholar]
- Favalli EG. Understanding the role of interleukin-6 (IL-6) in the joint and beyond: a comprehensive review of IL-6 inhibition for the management of rheumatoid. Arthritis Rheumatol Therapy. 2020;7:473–516. doi: 10.1007/s40744-020-00219-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foo MXR, Ong PF, Dreesen O. Premature aging syndromes: from patients to mechanism. J Dermatol Sci. 2019;96:58–65. doi: 10.1016/j.jdermsci.2019.10.003. [DOI] [PubMed] [Google Scholar]
- Fraga MF, et al. Loss of acetylation at Lys16 and trimethylation at Lys20 of histone H4 is a common hallmark of human cancer. Nat Genet. 2005;37:391–400. doi: 10.1038/ng1531. [DOI] [PubMed] [Google Scholar]
- Gaffney CJ, Pollard A, Barratt TF, Constantin-Teodosiu D, Greenhaff PL, Szewczyk NJ. Greater loss of mitochondrial function with ageing is associated with earlier onset of sarcopenia in C. elegans. Aging. 2018;10:3382–3396. doi: 10.18632/aging.101654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerhart-Hines Z, et al. Metabolic control of muscle mitochondrial function and fatty acid oxidation through SIRT1/PGC-1alpha. EMBO J. 2007;26:1913–1923. doi: 10.1038/sj.emboj.7601633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gillum MP, et al. SirT1 regulates adipose tissue inflammation. Diabetes. 2011;60:3235–3245. doi: 10.2337/db11-0616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gliemann L, et al. Resveratrol blunts the positive effects of exercise training on cardiovascular health in aged men. J Physiol. 2013;591:5047–5059. doi: 10.1113/jphysiol.2013.258061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gocmez SS, Gacar N, Utkan T, Gacar G, Scarpace PJ, Tumer N. Protective effects of resveratrol on aging-induced cognitive impairment in rats. Neurobiol Learn Mem. 2016;131:131–136. doi: 10.1016/j.nlm.2016.03.022. [DOI] [PubMed] [Google Scholar]
- Goodell MA, Rando TA. Stem cells and healthy aging. Science. 2015;350:1199–1204. doi: 10.1126/science.aab3388. [DOI] [PubMed] [Google Scholar]
- Gräff J, et al. An epigenetic blockade of cognitive functions in the neurodegenerating brain. Nature. 2012;483:222–226. doi: 10.1038/nature10849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green DR, Galluzzi L, Kroemer G. Mitochondria and the autophagy-inflammation-cell death axis in organismal aging . Science. 2011;333:1109–1112. doi: 10.1126/science.1201940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grote C, Reinhardt D, Zhang M, Wang J. Regulatory mechanisms and clinical manifestations of musculoskeletal aging. J Orthopaed Res. 2019;37:1475–1488. doi: 10.1002/jor.24292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gustafson CE, Kim C, Weyand CM, Goronzy JJ. Influence of immune aging on vaccine responses. J Allergy Clin Immunol. 2020;145:1309–1321. doi: 10.1016/j.jaci.2020.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gwinn DM, et al. AMPK phosphorylation of raptor mediates a metabolic checkpoint. Mol Cell. 2008;30:214–226. doi: 10.1016/j.molcel.2008.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harman D. The free radical theory of aging: effect of age on serum copper levels. J Gerontol. 1965;20:151–153. doi: 10.1093/geronj/20.2.151. [DOI] [PubMed] [Google Scholar]
- Harrison DE, et al. Rapamycin fed late in life extends lifespan in genetically heterogeneous mice. Nature. 2009;460:392–395. doi: 10.1038/nature08221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harry GJ. Microglia during development and aging. Pharmacol Ther. 2013;139:313–326. doi: 10.1016/j.pharmthera.2013.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartley AV, Martin M, Lu T. Aging: cancer-an unlikely couple. Aging. 2017;9:1949–1950. doi: 10.18632/aging.101295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasty P, et al. eRapa restores a normal life span in a FAP mouse model. Cancer Prevent Res. 2014;7:169–178. doi: 10.1158/1940-6207.capr-13-0299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayflick L, Moorhead PS. The serial cultivation of human diploid cell strains. Exp Cell Res. 1961;25:585–621. doi: 10.1016/0014-4827(61)90192-6. [DOI] [PubMed] [Google Scholar]
- Heidenreich PA, et al. Forecasting the future of cardiovascular disease in the United States: a policy statement from the American. Heart Assoc Circ. 2011;123:933–944. doi: 10.1161/CIR.0b013e31820a55f5. [DOI] [PubMed] [Google Scholar]
- Hekimi S, Lapointe J, Wen Y. Taking a “good” look at free radicals in the aging process. Trends Cell Biol. 2011;21:569–576. doi: 10.1016/j.tcb.2011.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hernandez-Segura A, de Jong TV, Melov S, Guryev V, Campisi J, Demaria M. Unmasking transcriptional heterogeneity in senescent cells. Curr Biol. 2017;27:2652–2660.e2654. doi: 10.1016/j.cub.2017.07.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hernandez-Segura A, Nehme J, Demaria M. Hallmarks of cellular senescence. Trends Cell Biol. 2018;28:436–453. doi: 10.1016/j.tcb.2018.02.001. [DOI] [PubMed] [Google Scholar]
- Herrmann M, Pusceddu I, März W, Herrmann W. Telomere biology and age-related diseases. Clin Chem Lab Med. 2018;56:1210–1222. doi: 10.1515/cclm-2017-0870. [DOI] [PubMed] [Google Scholar]
- Hickson LJ, et al. Senolytics decrease senescent cells in humans: preliminary report from a clinical trial of Dasatinib plus Quercetin in individuals with diabetic kidney disease. EBioMedicine. 2019;47:446–456. doi: 10.1016/j.ebiom.2019.08.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirsch HA, Iliopoulos D, Tsichlis PN, Struhl K. Metformin selectively targets cancer stem cells, and acts together with chemotherapy to block tumor growth and prolong remission. Cancer Res. 2009;69:7507–7511. doi: 10.1158/0008-5472.can-09-2994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hood DA, Memme JM, Oliveira AN, Triolo M. Maintenance of skeletal muscle mitochondria in health. Exer Aging Annu Rev Physiol. 2019;81:19–41. doi: 10.1146/annurev-physiol-020518-114310. [DOI] [PubMed] [Google Scholar]
- Horrillo D, et al. Age-associated development of inflammation in Wistar rats: effects of caloric restriction. Arch Physiol Biochem. 2011;117:140–150. doi: 10.3109/13813455.2011.577435. [DOI] [PubMed] [Google Scholar]
- Hosono K, et al. Metformin suppresses azoxymethane-induced colorectal aberrant crypt foci by activating AMP-activated protein kinase. Mol Carcinogen. 2010;49:662–671. doi: 10.1002/mc.20637. [DOI] [PubMed] [Google Scholar]
- Howitz KT, et al. Small molecule activators of sirtuins extend Saccharomyces cerevisiae lifespan. Nature. 2003;425:191–196. doi: 10.1038/nature01960. [DOI] [PubMed] [Google Scholar]
- Hwangbo DS, Lee HY, Abozaid LS, Min KJ (2020) Mechanisms of lifespan regulation by calorie restriction and intermittent fasting in model organisms. Nutrients. 10.3390/nu12041194 [DOI] [PMC free article] [PubMed]
- Imai S, Guarente L. Ten years of NAD-dependent SIR2 family deacetylases: implications for metabolic diseases. Trends Pharmacological Sci. 2010;31:212–220. doi: 10.1016/j.tips.2010.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Janczura KJ, et al. Inhibition of HDAC3 reverses Alzheimer’s disease-related pathologies in vitro and in the 3xTg-AD mouse model. Proc Natl Acad Sci USA. 2018;115:E11148–E11157. doi: 10.1073/pnas.1805436115. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- Jankovic J, Kapadia AS. Functional decline in Parkinson disease. Arch Neurol. 2001;58:1611–1615. doi: 10.1001/archneur.58.10.1611. [DOI] [PubMed] [Google Scholar]
- Johnson SC, Rabinovitch PS, Kaeberlein M. mTOR is a key modulator of ageing and age-related disease. Nature. 2013;493:338–345. doi: 10.1038/nature11861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Justice JN, et al. Senolytics in idiopathic pulmonary fibrosis: results from a first-in-human, open-label pilot study. EBioMedicine. 2019;40:554–563. doi: 10.1016/j.ebiom.2018.12.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalra N, Roy P, Prasad S, Shukla Y. RETRACTED: Resveratrol induces apoptosis involving mitochondrial pathways in mouse skin tumorigenesis. Life Sci. 2008;82:348–358. doi: 10.1016/j.lfs.2007.11.006. [DOI] [PubMed] [Google Scholar]
- Kanaan NM, Kordower JH, Collier TJ. Age-related accumulation of Marinesco bodies and lipofuscin in rhesus monkey midbrain dopamine neurons: relevance to selective neuronal vulnerability. J Comp Neurol. 2007;502:683–700. doi: 10.1002/cne.21333. [DOI] [PubMed] [Google Scholar]
- Kanaan NM, Kordower JH, Collier TJ. Age and region-specific responses of microglia, but not astrocytes, suggest a role in selective vulnerability of dopamine neurons after 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine exposure in monkeys. Glia. 2008;56:1199–1214. doi: 10.1002/glia.20690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kane AE, Sinclair DA. Epigenetic changes during aging and their reprogramming potential. Crit Rev Biochem Mol Biol. 2019;54:61–83. doi: 10.1080/10409238.2019.1570075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kantarjian HM, et al. Multicenter, randomized, open-label, phase III trial of decitabine versus patient choice, with physician advice, of either supportive care or low-dose cytarabine for the treatment of older patients with newly diagnosed acute myeloid leukemia. J Clin Oncol. 2012;30:2670–2677. doi: 10.1200/jco.2011.38.9429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kapahi P, Kaeberlein M, Hansen M. Dietary restriction and lifespan: lessons from invertebrate models. Ageing Res Rev. 2017;39:3–14. doi: 10.1016/j.arr.2016.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kauppila TES, Kauppila JHK, Larsson NG. Mammalian mitochondria and aging. An update. Cell Metab. 2017;25:57–71. doi: 10.1016/j.cmet.2016.09.017. [DOI] [PubMed] [Google Scholar]
- Kauppila TES, et al. Mutations of mitochondrial DNA are not major contributors to aging of fruit flies. Proc Natl Acad Sci USA. 2018;115:E9620–E9629. doi: 10.1073/pnas.1721683115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaushik S, Cuervo AM. Proteostasis and aging. Nat Med. 2015;21:1406–1415. doi: 10.1038/nm.4001. [DOI] [PubMed] [Google Scholar]
- Kawahara TL, et al. SIRT6 links histone H3 lysine 9 deacetylation to NF-kappaB-dependent gene expression and organismal life span. Cell. 2009;136:62–74. doi: 10.1016/j.cell.2008.10.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keyes BE, Fuchs E. Stem cells: aging and transcriptional fingerprints. J Cell Biol. 2018;217:79–92. doi: 10.1083/jcb.201708099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kilgore M, Miller CA, Fass DM, Hennig KM, Haggarty SJ, Sweatt JD, Rumbaugh G. Inhibitors of class 1 histone deacetylases reverse contextual memory deficits in a mouse model of Alzheimer’s disease. Neuropsychopharmacology. 2010;35:870–880. doi: 10.1038/npp.2009.197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim EC, Kim JR. Senotherapeutics: emerging strategy for healthy aging and age-related disease. BMB Rep. 2019;52:47–55. doi: 10.5483/BMBRep.2019.52.1.293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klaips CL, Jayaraj GG, Hartl FU. Pathways of cellular proteostasis in aging and disease. J Cell Biol. 2018;217:51–63. doi: 10.1083/jcb.201709072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kozhemyakina E, et al. Identification of a Prg4-expressing articular cartilage progenitor cell population in mice. Arthrit Rheumatol. 2015;67:1261–1273. doi: 10.1002/art.39030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kubben N, Misteli T. Shared molecular and cellular mechanisms of premature ageing and ageing-associated diseases. Nat Rev Mol Cell Biol. 2017;18:595–609. doi: 10.1038/nrm.2017.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurz DJ, et al. Degenerative aortic valve stenosis, but not coronary disease, is associated with shorter telomere length in the elderly. Arterioscler Thromb Vasc Biol. 2006;26:e114–117. doi: 10.1161/01.atv.0000222961.24912.69. [DOI] [PubMed] [Google Scholar]
- la Porte C, Voduc N, Zhang G, Seguin I, Tardiff D, Singhal N, Cameron DW. Steady-state pharmacokinetics and tolerability of trans-resveratrol 2000 mg twice daily with food, quercetin and alcohol (ethanol) in healthy human subjects. Clin Pharmacokinet. 2010;49:449–454. doi: 10.2165/11531820-000000000-00000. [DOI] [PubMed] [Google Scholar]
- Lähteenvuo J, Rosenzweig A. Effects of aging on angiogenesis. Circ Res. 2012;110:1252–1264. doi: 10.1161/circresaha.111.246116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lakatta EG, Levy D. Arterial and cardiac aging: major shareholders in cardiovascular disease enterprises: Part II: the aging heart in health: links to heart disease. Circulation. 2003;107:346–354. doi: 10.1161/01.cir.0000048893.62841.f7. [DOI] [PubMed] [Google Scholar]
- Langan RC, Goodbred AJ. Vitamin B12 deficiency: recognition and management. Am Fam Phys. 2017;96:384–389. [PubMed] [Google Scholar]
- Lavasani M, et al. Muscle-derived stem/progenitor cell dysfunction limits healthspan and lifespan in a murine progeria model. Nat Commun. 2012;3:608. doi: 10.1038/ncomms1611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le Bourg E, Redman LM. Do-it-yourself calorie restriction: the risks of simplistically translating findings in animal models to humans. BioEssays. 2018;40:e1800087. doi: 10.1002/bies.201800087. [DOI] [PubMed] [Google Scholar]
- Leong I. Sustained caloric restriction in health. Nat Rev Endocrinol. 2018;14:322. doi: 10.1038/s41574-018-0008-2. [DOI] [PubMed] [Google Scholar]
- Li Y, Seto E (2016) HDACs and HDAC inhibitors in cancer development and therapy. Cold Spring Harbor Perspect Med. 10.1101/cshperspect.a026831 [DOI] [PMC free article] [PubMed]
- Li Y, Tollefsbol TO. Impact on DNA methylation in cancer prevention and therapy by bioactive dietary components. Curr Med Chem. 2010;17:2141–2151. doi: 10.2174/092986710791299966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li X, Li T, Liu Z, Gou S, Wang C. The effect of metformin on survival of patients with pancreatic cancer: a meta-analysis. Sci Rep. 2017;7:5825. doi: 10.1038/s41598-017-06207-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li YR, Li S, Lin CC. Effect of resveratrol and pterostilbene on aging and longevity . BioFactors. 2018;44:69–82. doi: 10.1002/biof.1400. [DOI] [PubMed] [Google Scholar]
- Liddelow SA, Barres BA. Reactive astrocytes: production, function, and therapeutic potential. Immunity. 2017;46:957–967. doi: 10.1016/j.immuni.2017.06.006. [DOI] [PubMed] [Google Scholar]
- Lin CL, et al. HDAC1 and HDAC2 double knockout triggers cell apoptosis in advanced thyroid cancer. Int J Mol Sci. 2019 doi: 10.3390/ijms20020454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu B, Fan Z, Edgerton SM, Yang X, Lind SE, Thor AD. Potent anti-proliferative effects of metformin on trastuzumab-resistant breast cancer cells via inhibition of erbB2/IGF-1 receptor interactions. Cell Cycle. 2011;10:2959–2966. doi: 10.4161/cc.10.17.16359. [DOI] [PubMed] [Google Scholar]
- López-Otín C, Blasco MA, Partridge L, Serrano M, Kroemer G. The hallmarks of aging. Cell. 2013;153:1194–1217. doi: 10.1016/j.cell.2013.05.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lorenzini A. How much should we weigh for a long and healthy life span? The need to reconcile caloric restriction versus longevity with body mass index versus mortality data . Front Endocrinol. 2014;5:121. doi: 10.3389/fendo.2014.00121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu M, Su C, Qiao C, Bian Y, Ding J, Hu G. Metformin prevents dopaminergic neuron death in MPTP/P-induced mouse model of Parkinson’s disease via autophagy and mitochondrial ROS clearance. Int J Neuropsychopharmacol. 2016 doi: 10.1093/ijnp/pyw047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lublóy Á. Medical crowdfunding in a healthcare system with universal coverage: an exploratory study. BMC Public Health. 2020;20:1672. doi: 10.1186/s12889-020-09693-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma S, et al. Histone deacetylases inhibitor MS-275 suppresses human esophageal squamous cell carcinoma cell growth and progression via the PI3K/Akt/mTOR pathway. J Cell Physiol. 2019;234:22400–22410. doi: 10.1002/jcp.28805. [DOI] [PubMed] [Google Scholar]
- Maierhofer A, et al. Epigenetic signatures of Werner syndrome occur early in life and are distinct from normal epigenetic aging processes. Aging Cell. 2019;18:e12995. doi: 10.1111/acel.12995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marathe PH, Gao HX, Close KL. American Diabetes Association Standards of Medical Care in Diabetes 2017. J Diabet. 2017;9:320–324. doi: 10.1111/1753-0407.12524. [DOI] [PubMed] [Google Scholar]
- Matheu A, et al. Delayed ageing through damage protection by the Arf/p53 pathway. Nature. 2007;448:375–379. doi: 10.1038/nature05949. [DOI] [PubMed] [Google Scholar]
- Mathew R, Pal Bhadra M, Bhadra U. Insulin/insulin-like growth factor-1 signalling (IIS) based regulation of lifespan across species. Biogerontology. 2017;18:35–53. doi: 10.1007/s10522-016-9670-8. [DOI] [PubMed] [Google Scholar]
- McCormack FX, et al. Efficacy and safety of sirolimus in lymphangioleiomyomatosis. N Engl J Med. 2011;364:1595–1606. doi: 10.1056/NEJMoa1100391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCreight LJ, et al. Pharmacokinetics of metformin in patients with gastrointestinal intolerance. Diabet Obes Metab. 2018;20:1593–1601. doi: 10.1111/dom.13264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGrath C, et al. Exercise degrades bone in caloric restriction, despite suppression of marrow adipose tissue (MAT) J Bone Miner Res. 2020;35:106–115. doi: 10.1002/jbmr.3872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mensà E, Latini S, Ramini D, Storci G, Bonafè M, Olivieri F. The telomere world and aging: analytical challenges and future perspectives. Ageing Res Rev. 2019;50:27–42. doi: 10.1016/j.arr.2019.01.004. [DOI] [PubMed] [Google Scholar]
- Meydani SN, et al. Long-term moderate calorie restriction inhibits inflammation without impairing cell-mediated immunity: a randomized controlled trial in non-obese humans. Aging. 2016;8:1416–1431. doi: 10.18632/aging.100994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moiseeva O, et al. Metformin inhibits the senescence-associated secretory phenotype by interfering with IKK/NF-κB activation. Aging Cell. 2013;12:489–498. doi: 10.1111/acel.12075. [DOI] [PubMed] [Google Scholar]
- Morigi M, Perico L, Benigni A. Sirtuins in renal health and disease. J Am Soc Nephrol. 2018;29:1799–1809. doi: 10.1681/asn.2017111218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Most J, Gilmore LA, Smith SR, Han H, Ravussin E, Redman LM. Significant improvement in cardiometabolic health in healthy nonobese individuals during caloric restriction-induced weight loss and weight loss maintenance. Am J Physiol Endocrinology Metab. 2018;314:E396–E405. doi: 10.1152/ajpendo.00261.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Musci RV, et al. The Dunkin Hartley Guinea pig is a model of primary osteoarthritis that also exhibits early onset myofiber remodeling that resembles human musculoskeletal aging. Front Physiol. 2020;11:571372. doi: 10.3389/fphys.2020.571372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Musi N, Valentine JM, Sickora KR, Baeuerle E, Thompson CS, Shen Q, Orr ME. Tau protein aggregation is associated with cellular senescence in the brain. Aging Cell. 2018;17:e12840. doi: 10.1111/acel.12840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nair V, Sreevalsan S, Basha R, Abdelrahim M, Abudayyeh A, Rodrigues Hoffman A, Safe S. Mechanism of metformin-dependent inhibition of mammalian target of rapamycin (mTOR) and Ras activity in pancreatic cancer: role of specificity protein (Sp) transcription factors. J Biol Chem. 2014;289:27692–27701. doi: 10.1074/jbc.M114.592576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neff F, et al. Rapamycin extends murine lifespan but has limited effects on aging. J Clin Investig. 2013;123:3272–3291. doi: 10.1172/jci67674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson G, Kucheryavenko O, Wordsworth J, von Zglinicki T. The senescent bystander effect is caused by ROS-activated NF-κB signalling. Mech Ageing Dev. 2018;170:30–36. doi: 10.1016/j.mad.2017.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ng TP, Feng L, Yap KB, Lee TS, Tan CH, Winblad B. Long-term metformin usage and cognitive function among older adults with diabetes. J Alzheimer’s Dis. 2014;41:61–68. doi: 10.3233/jad-131901. [DOI] [PubMed] [Google Scholar]
- Niedernhofer LJ, Robbins PD. Senotherapeutics for healthy ageing. Nat Rev Drug Discov. 2018;17:377. doi: 10.1038/nrd.2018.44. [DOI] [PubMed] [Google Scholar]
- Njie EG, Boelen E, Stassen FR, Steinbusch HW, Borchelt DR, Streit WJ. Ex vivo cultures of microglia from young and aged rodent brain reveal age-related changes in microglial function. Neurobiol Aging. 2012;33:195.e191–112. doi: 10.1016/j.neurobiolaging.2010.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogrodnik M, et al. Obesity-induced cellular senescence drives anxiety and impairs. Neurogen Cell Metab. 2019;29:1233. doi: 10.1016/j.cmet.2019.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olah M, et al. A transcriptomic atlas of aged human microglia. Nat Commun. 2018;9:539. doi: 10.1038/s41467-018-02926-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osorio FG, et al. Nuclear lamina defects cause ATM-dependent NF-κB activation and link accelerated aging to a systemic inflammatory response. Genes Dev. 2012;26:2311–2324. doi: 10.1101/gad.197954.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ou Z, et al. Metformin treatment prevents amyloid plaque deposition and memory impairment in APP/PS1 mice. Brain Behav Immun. 2018;69:351–363. doi: 10.1016/j.bbi.2017.12.009. [DOI] [PubMed] [Google Scholar]
- Palmer SC, et al. Comparison of clinical outcomes and adverse events associated with glucose-lowering drugs in patients with type 2 diabetes: a meta-analysis. Jama. 2016;316:313–324. doi: 10.1001/jama.2016.9400. [DOI] [PubMed] [Google Scholar]
- Paneni F, Diaz Cañestro C, Libby P, Lüscher TF, Camici GG. The aging cardiovascular system: understanding it at the cellular and clinical levels. J Am Coll Cardiol. 2017;69:1952–1967. doi: 10.1016/j.jacc.2017.01.064. [DOI] [PubMed] [Google Scholar]
- Park DW, Kim JS, Chin BR, Baek SH. Resveratrol inhibits inflammation induced by heat-killed Listeria monocytogenes. J Med Food. 2012;15:788–794. doi: 10.1089/jmf.2012.2194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patil SP, Jain PD, Ghumatkar PJ, Tambe R, Sathaye S. Neuroprotective effect of metformin in MPTP-induced Parkinson’s disease in mice. Neuroscience. 2014;277:747–754. doi: 10.1016/j.neuroscience.2014.07.046. [DOI] [PubMed] [Google Scholar]
- Patrick M, Weng NP. Expression and regulation of telomerase in human T cell differentiation, activation, aging and diseases. Cell Immunol. 2019;345:103989. doi: 10.1016/j.cellimm.2019.103989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pereira B, Xu XN, Akbar AN. Targeting inflammation and immunosenescence to improve vaccine responses in the elderly. Front Immunol. 2020;11:583019. doi: 10.3389/fimmu.2020.583019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pérez-Revuelta BI, Hettich MM, Ciociaro A, Rotermund C, Kahle PJ, Krauss S, Di Monte DA. Metformin lowers Ser-129 phosphorylated α-synuclein levels via mTOR-dependent protein phosphatase 2A activation. Cell Death Dis. 2014;5:e1209. doi: 10.1038/cddis.2014.175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Philipot D, et al. p16INK4a and its regulator miR-24 link senescence and chondrocyte terminal differentiation-associated matrix remodeling in osteoarthritis. Arthritis Res Therapy. 2014;16:R58. doi: 10.1186/ar4494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Picca A, Pesce V, Lezza AMS. Does eating less make you live longer and better? An update on calorie restriction. Clin Interv Aging. 2017;12:1887–1902. doi: 10.2147/cia.s126458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pietrobon AJ, Teixeira FME, Sato MN. Immunosenescence and inflammaging: risk factors of severe COVID-19 in older people. Front Immunol. 2020;11:579220. doi: 10.3389/fimmu.2020.579220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pifferi F, Aujard F. Caloric restriction, longevity and aging: recent contributions from human and non-human primate studies. Prog Neuro-Psychopharmacol Biol Psychiatry. 2019;95:109702. doi: 10.1016/j.pnpbp.2019.109702. [DOI] [PubMed] [Google Scholar]
- Pifferi F, Aujard F. Caloric restriction, longevity and aging: Recent contributions from human and non-human primate studies. Prog Neuro-Psychopharmacol Biol Psychiatry. 2019;95:109702. doi: 10.1016/j.pnpbp.2019.109702. [DOI] [PubMed] [Google Scholar]
- Popat R, et al. A phase 2 study of SRT501 (resveratrol) with bortezomib for patients with relapsed and or refractory multiple myeloma. Br J Haematol. 2013;160:714–717. doi: 10.1111/bjh.12154. [DOI] [PubMed] [Google Scholar]
- Price NL, et al. SIRT1 is required for AMPK activation and the beneficial effects of resveratrol on mitochondrial function. Cell Metabol. 2012;15:675–690. doi: 10.1016/j.cmet.2012.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pringsheim T, Jette N, Frolkis A, Steeves TD. The prevalence of Parkinson’s disease: a systematic review and meta-analysis. J Movement Disord Soc. 2014;29:1583–1590. doi: 10.1002/mds.25945. [DOI] [PubMed] [Google Scholar]
- Pryor R, Cabreiro F. Repurposing metformin: an old drug with new tricks in its binding pockets. Biochem J. 2015;471:307–322. doi: 10.1042/bj20150497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raphael I, Joern RR, Forsthuber TG. Memory CD4(+) T cells in immunity and autoimmune diseases. Cells. 2020;7:8. doi: 10.3390/cells9030531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rattan SI. Aging is not a disease: implications for intervention. Aging Dis. 2014;5:196–202. doi: 10.14336/ad.2014.0500196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ravi V, et al. SIRT6 transcriptionally regulates global protein synthesis through transcription factor Sp1 independent of its deacetylase activity. Nucleic Acids Res. 2019;47:9115–9131. doi: 10.1093/nar/gkz648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ray D, Yung R. Immune senescence, epigenetics and autoimmunity. Clin Immunol. 2018;196:59–63. doi: 10.1016/j.clim.2018.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Redman LM, Smith SR, Burton JH, Martin CK, Il’yasova D, Ravussin E. Metabolic slowing and reduced oxidative damage with sustained caloric restriction support the rate of living and oxidative damage theories of aging. Aging Cell Metab. 2018;27:805–815.e804. doi: 10.1016/j.cmet.2018.02.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ritschka B, et al. The senescence-associated secretory phenotype induces cellular plasticity and tissue regeneration. Genes Dev. 2017;31:172–183. doi: 10.1101/gad.290635.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rossman MJ, et al. Chronic supplementation with a mitochondrial antioxidant (mitoq) improves vascular function in healthy older adults. Hypertension. 2018;71:1056–1063. doi: 10.1161/hypertensionaha.117.10787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rufer N, et al. Telomere fluorescence measurements in granulocytes and T lymphocyte subsets point to a high turnover of hematopoietic stem cells and memory T cells in early childhood. J Exp Med. 1999;190:157–167. doi: 10.1084/jem.190.2.157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sadighi Akha AA. Aging and the immune system: an overview. J Immunol Methods. 2018;463:21–26. doi: 10.1016/j.jim.2018.08.005. [DOI] [PubMed] [Google Scholar]
- Salminen A, Kaarniranta K, Kauppinen A. Inflammaging: disturbed interplay between autophagy and inflammasomes. Aging. 2012;4:166–175. doi: 10.18632/aging.100444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salminen A, Kauppinen A, Kaarniranta K. FGF21 activates AMPK signaling: impact on metabolic regulation and the aging process. J Mol Med. 2017;95:123–131. doi: 10.1007/s00109-016-1477-1. [DOI] [PubMed] [Google Scholar]
- Salvestrini V, Sell C, Lorenzini A. Obesity may accelerate the aging process . Front Endocrinol. 2019;10:266. doi: 10.3389/fendo.2019.00266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santos J, Leitão-Correia F, Sousa MJ, Leão C (2016) Dietary restriction and nutrient balance in aging. Oxid Med Cell Longev 2016:4010357. 10.1155/2016/4010357 [DOI] [PMC free article] [PubMed]
- Saretzki G. Telomeres, telomerase and ageing. Sub-cell Biochem. 2018;90:221–308. doi: 10.1007/978-981-13-2835-0_9. [DOI] [PubMed] [Google Scholar]
- Sasongko TH, Ismail NF, Zabidi-Hussin Z. Rapamycin and rapalogs for tuberous sclerosis complex. Cochrane Database Syst Rev. 2016;7:011272. doi: 10.1002/14651858.CD011272.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sawda C, Moussa C, Turner RS. Resveratrol for Alzheimer’s disease. Ann N Y Acad Sci. 2017;1403:142–149. doi: 10.1111/nyas.13431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schlender L, et al. Efficacy and safety of metformin in the management of type 2 diabetes mellitus in older adults: a systematic review for the development of recommendations to reduce potentially inappropriate prescribing. BMC Geriatr. 2017;17:227. doi: 10.1186/s12877-017-0574-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Senovilla L, et al. An immunosurveillance mechanism controls cancer cell ploidy . Science. 2012;337:1678–1684. doi: 10.1126/science.1224922. [DOI] [PubMed] [Google Scholar]
- Shay JW. Role of telomeres and telomerase in aging and cancer. Cancer Discov. 2016;6:584–593. doi: 10.1158/2159-8290.cd-16-0062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheth KA, et al. Muscle strength and size are associated with motor unit connectivity in aged mice. Neurobiol Aging. 2018;67:128–136. doi: 10.1016/j.neurobiolaging.2018.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silva P, Sureda A, Tur JA, Andreoletti P, Cherkaoui-Malki M, Latruffe N. How efficient is resveratrol as an antioxidant of the Mediterranean diet, towards alterations during the aging process? Free Radic Res. 2019;53:1101–1112. doi: 10.1080/10715762.2019.1614176. [DOI] [PubMed] [Google Scholar]
- Smith BD, Smith GL, Hurria A, Hortobagyi GN, Buchholz TA. Future of cancer incidence in the United States: burdens upon an aging changing nation. J Clin Oncol. 2009;27:2758–2765. doi: 10.1200/jco.2008.20.8983. [DOI] [PubMed] [Google Scholar]
- Sorrentino V, et al. Enhancing mitochondrial proteostasis reduces amyloid-β proteotoxicity. Nature. 2017;552:187–193. doi: 10.1038/nature25143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spescha RD, et al. Deletion of the ageing gene p66(Shc) reduces early stroke size following ischaemia/reperfusion brain injury. Eur Heart J. 2013;34:96–103. doi: 10.1093/eurheartj/ehs331. [DOI] [PubMed] [Google Scholar]
- Spescha RD, et al. Post-ischaemic silencing of p66Shc reduces ischaemia/reperfusion brain injury and its expression correlates to clinical outcome in stroke. Eur Heart J. 2015;36:1590–1600. doi: 10.1093/eurheartj/ehv140. [DOI] [PubMed] [Google Scholar]
- Stynen B, et al. Changes of cell biochemical states are revealed in protein homomeric. Complex Dyn Cell. 2018;175:1418–1429.e1419. doi: 10.1016/j.cell.2018.09.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tiwari V, Wilson DM. DNA damage and associated DNA repair defects in disease and premature. Aging Am J Hum Genet. 2019;105:237–257. doi: 10.1016/j.ajhg.2019.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tizazu AM, et al. Metformin monotherapy downregulates diabetes-associated inflammatory status and impacts on mortality. Front Physiol. 2019;10:572. doi: 10.3389/fphys.2019.00572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trevisan K, Cristina-Pereira R, Silva-Amaral D, Aversi-Ferreira TA. Theories of aging and the prevalence of Alzheimer’s disease. BioMed Res Int. 2019;2019:9171424. doi: 10.1155/2019/9171424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai CF, Wang KT, Chen LG, Lee CJ, Tseng SH, Wang CC. Anti-inflammatory effects of Vitis thunbergii var. taiwaniana on knee damage associated with arthritis. J Med Food. 2014;17:479–486. doi: 10.1089/jmf.2013.2914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tseng CH. Metformin reduces gastric cancer risk in patients with type 2 diabetes mellitus. Aging. 2016;8:1636–1649. doi: 10.18632/aging.101019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ullah M, Sun Z. Klotho deficiency accelerates stem cells aging by impairing telomerase activity. J Gerontol Ser A. 2019;74:1396–1407. doi: 10.1093/gerona/gly261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Deursen JM. The role of senescent cells in ageing. Nature. 2014;509:439–446. doi: 10.1038/nature13193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vera E, Bernardes de Jesus B, Foronda M, Flores JM, Blasco MA. Telomerase reverse transcriptase synergizes with calorie restriction to increase health span and extend mouse longevity. PLoS ONE. 2013;8:e53760. doi: 10.1371/journal.pone.0053760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Villareal DT, et al. Effect of two-year caloric restriction on bone metabolism and bone mineral density in non-obese younger adults: a randomized clinical trial. J Bone Miner Res. 2016;31:40–51. doi: 10.1002/jbmr.2701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y, Zhao X, Lotz M, Terkeltaub R, Liu-Bryan R. Mitochondrial biogenesis is impaired in osteoarthritis chondrocytes but reversible via peroxisome proliferator-activated receptor γ coactivator 1α Arthrit Rheumatol. 2015;67:2141–2153. doi: 10.1002/art.39182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang X, et al. Resveratrol exerts dosage-dependent effects on the self-renewal and neural differentiation of hUC-MSCs. Mol Cells. 2016;39:418–425. doi: 10.14348/molcells.2016.2345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang L, et al. High-throughput functional genetic and compound screens identify targets for senescence induction in cancer. Cell Rep. 2017;21:773–783. doi: 10.1016/j.celrep.2017.09.085. [DOI] [PubMed] [Google Scholar]
- Wang X, et al. Resveratrol promotes hUC-MSCs engraftment and neural repair in a mouse model of Alzheimer’s disease. Behav Brain Res. 2018;339:297–304. doi: 10.1016/j.bbr.2017.10.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiley CD, et al. Mitochondrial dysfunction induces senescence with a distinct secretory. Phenotype Cell Metab. 2016;23:303–314. doi: 10.1016/j.cmet.2015.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winnik S, Auwerx J, Sinclair DA, Matter CM. Protective effects of sirtuins in cardiovascular diseases: from bench to bedside. Eur Heart J. 2015;36:3404–3412. doi: 10.1093/eurheartj/ehv290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witte AV, Kerti L, Margulies DS, Flöel A. Effects of resveratrol on memory performance, hippocampal functional connectivity, and glucose metabolism in healthy older adults. J Neurosci. 2014;34:7862–7870. doi: 10.1523/jneurosci.0385-14.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong SQ, Kumar AV, Mills J, Lapierre LR. Autophagy in aging and longevity. Hum Genet. 2020;139:277–290. doi: 10.1007/s00439-019-02031-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wood JG, Rogina B, Lavu S, Howitz K, Helfand SL, Tatar M, Sinclair D. Sirtuin activators mimic caloric restriction and delay ageing in metazoans. Nature. 2004;430:686–689. doi: 10.1038/nature02789. [DOI] [PubMed] [Google Scholar]
- Wyss-Coray T, Rogers J. Inflammation in Alzheimer disease: a brief review of the basic science and clinical literature. Cold Spring Harbor Perspect Med. 2012;2:a006346. doi: 10.1101/cshperspect.a006346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xia N, Förstermann U, Li H. Effects of resveratrol on eNOS in the endothelium and the perivascular adipose tissue . Ann N Y Acad Sci. 2017;1403:132–141. doi: 10.1111/nyas.13397. [DOI] [PubMed] [Google Scholar]
- Xia X, Jiang Q, McDermott J, Han JJ. Aging and Alzheimer’s disease: comparison and associations from molecular to system level. Aging Cell. 2018;17:e12802. doi: 10.1111/acel.12802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiong C, Zhang Z, Baht GS, Terrando N. A mouse model of orthopedic surgery to study postoperative cognitive dysfunction and tissue regeneration. J Visualiz Exp. 2018 doi: 10.3791/56701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu S, et al. SIRT6 protects against endothelial dysfunction and atherosclerosis in mice. Aging. 2016;8:1064–1082. doi: 10.18632/aging.100975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuan F, Xu ZM, Lu LY, Nie H, Ding J, Ying WH, Tian HL. SIRT2 inhibition exacerbates neuroinflammation and blood-brain barrier disruption in experimental traumatic brain injury by enhancing NF-κB p65 acetylation and activation. J Neurochem. 2016;136:581–593. doi: 10.1111/jnc.13423. [DOI] [PubMed] [Google Scholar]
- Zaza G, Granata S, Caletti C, Signorini L, Stallone G, Lupo A. mTOR inhibition role in cellular mechanisms. Transplantation. 2018;102:S3–Ss16. doi: 10.1097/tp.0000000000001806. [DOI] [PubMed] [Google Scholar]
- Zhang G, et al. Hypothalamic programming of systemic ageing involving IKK-β, NF-κB and GnRH. Nature. 2013;497:211–216. doi: 10.1038/nature12143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang W, et al. NSCs promote hippocampal neurogenesis, metabolic changes and synaptogenesis in APP/PS1 transgenic mice . Hippocampus. 2017;27:1250–1263. doi: 10.1002/hipo.22794. [DOI] [PubMed] [Google Scholar]
- Zhang LF, Yu XL, Ji M, Liu SY, Wu XL, Wang YJ, Liu RT. Resveratrol alleviates motor and cognitive deficits and neuropathology in the A53T α-synuclein mouse model of Parkinson’s disease. Food Funct. 2018;9:6414–6426. doi: 10.1039/c8fo00964c. [DOI] [PubMed] [Google Scholar]
- Zhang P, et al. Senolytic therapy alleviates Aβ-associated oligodendrocyte progenitor cell senescence and cognitive deficits in an Alzheimer’s disease model. Nat Neurosci. 2019;22:719–728. doi: 10.1038/s41593-019-0372-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu Y, et al. The Achilles’ heel of senescent cells: from transcriptome to senolytic drugs. Aging Cell. 2015;14:644–658. doi: 10.1111/acel.12344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu Y, et al. Identification of a novel senolytic agent, navitoclax, targeting the Bcl-2 family of anti-apoptotic factors. Aging Cell. 2016;15:428–435. doi: 10.1111/acel.12445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu Y, et al. New agents that target senescent cells: the flavone, fisetin, and the BCL-X(L) inhibitors, A1331852 and A1155463. Aging. 2017;9:955–963. doi: 10.18632/aging.101202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu X, Yang J, Zhu W, Yin X, Yang B, Wei Y, Guo X. Combination of berberine with resveratrol improves the lipid-lowering efficacy. Int J Mol Sci. 2018 doi: 10.3390/ijms19123903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu Y, Liu X, Ding X, Wang F, Geng X. Telomere and its role in the aging pathways: telomere shortening cell senescence mitochondria dysfunction. Biogerontology. 2019;20:1–16. doi: 10.1007/s10522-018-9769-1. [DOI] [PubMed] [Google Scholar]