Abstract
Wound healing is a dynamic biological process achieved through four sequential, overlapping phases; hemostasis, inflammation, tissue proliferation and remodeling. For effective wound healing, all four phases must occur in the appropriate order and time frame. It is well accepted that the wound healing process becomes disrupted in the elderly, increasing the propensity of non-healing wound states that can lead to substantial patient morbidity and an enormous financial burden on healthcare systems. Estrogen deprivation in the elderly has been identified as the key driver of age-related delayed wound healing in both genders, with topical and systemic estrogen replacement reversing the detrimental effects of aging on wound repair. Evidence suggests estrogen deprivation may contribute to the development of chronic wound healing states in the elderly but research in this area is somewhat limited, warranting further investigations. Moreover, although the beneficial effects of estrogen on cutaneous healing have been widely explored, the development of estrogen-based treatments to enhance wound repair in the elderly have yet to be widely exploited. This review explores the critical role of estrogen in reversing age-related impaired healing and evaluates the prospect of developing more focused novel therapeutic strategies that enhance wound repair in the elderly via activation of specific estrogen signaling pathways in regenerating tissues, whilst leaving non-target tissues largely unaffected.
Keywords: wound healing, aging, age-related impaired healing, estrogen, estrogen receptors
Background
Declining levels of estrogen in both genders with increasing age suggests that age-related impaired wound healing may result in part from the loss of protection that was once afforded by estrogen during youth. Indeed, estrogen treatments appear to reverse the detrimental effects of age-related impaired healing, resulting in accelerated wound repair in both genders. Despite these findings, the use of estrogen-based treatments to reverse delayed healing in the elderly has not been widely adopted outside research settings. Moreover, the potential role of the sex steroid hormones in chronic wounds remains unclear but evidence suggests that being male is a risk factor for venous ulceration, whilst the use of hormone replacement therapy (HRT) by post-menopausal women appears to reduce the risk of venous ulceration (Bérard et al., 2001[22]; Margolis et al., 2002[82]). Furthermore, polymorphisms in the estrogen receptor-beta (ER-β) gene are associated with venous ulceration (Ashworth et al., 2005[16], 2008[15]). Thus, it is feasible that estrogen deprivation may contribute to the development of chronic wound healing states in the elderly. The lack of extensive research in this area highlights the need for further investigations to explore the precise mechanisms by which estrogen deficiency may contribute to the development or progression of chronic wounds in the elderly. This review explores current knowledge in this field, highlighting the critical role of estrogen in reversing age-related impaired healing and prospects for developing more focused therapies in the form of local dressings that promote healing in the elderly via activation of specific estrogen signaling pathways in regenerating tissues, whilst leaving other non-target tissues in the body largely unaffected.
Acute Wound Healing
Acute wound healing is a complex and dynamic biological process divided into four sequential, overlapping phases; hemostasis, inflammation, tissue proliferation and remodeling of the tissue scar (Figure 1(Fig. 1); Reference in Figure 1: El Mohtadi, 2019[41]). Immediately after trauma, degranulating platelets adhere to damaged blood vessels and start a hemostatic reaction, increasing the coagulation cascade and producing a fibrin clot to prevent extreme blood loss and provide a temporary protection for the wound against foreign bodies (Vaughan et al., 2000[147]; Weyrich and Zimmerman, 2004[152]; Gilliver et al., 2007[50]). Platelets in the clot release a variety of pro-inflammatory cytokines and growth factors including platelet-derived growth factor (PDGF), transforming growth factor-beta (TGF-β), fibroblast growth factor-2 (FGF-2), vascular endothelial growth factor (VEGF) and epidermal growth factor (EGF) (Bauer et al., 1985[19]; Guo and DiPietro, 2010[54]). These cytokines, chemokines and growth factors attract inflammatory cells from circulation to the wound site, initiating the inflammatory phase. Neutrophils are the first inflammatory cells recruited from circulation (Ley et al., 2007[77]). They peak in numbers at 24 to 36 hours post-injury (Dovi et al., 2004[39]). Neutrophils remove foreign materials and invading microorganisms, such as bacteria, via the release of reactive oxygen species (ROS) and lysosomal enzymes, and degrade damaged matrix tissues by collagenases and proteinases (Mosser and Edwards, 2010[95]). The majority of neutrophils are enclosed in the wound clot and are either eliminated with the eschar or by macrophages via phagocytosis (Newman et al., 1982[100]; Kondo and Ishida, 2010[70]).
Figure 1. Typical timescale and phases of acute wound healing stages in young adult humans. Immediately after injury, healing initiates with hemostasis. This results in the formation of a fibrin clot within minutes following injury. The inflammatory phase overlaps with hemostasis and occurs within minutes after injury, with neutrophils being recruited from circulation, followed by monocytes. Monocytes undergo a series of changes to differentiate into tissue macrophages, which carry out phagocytosis and release cytokines that encourage the recruitment and activation of further leukocytes to the injury site and initiation of the proliferation phase. Three to ten days after injury, the proliferation phase starts enabling granulation tissue formation, re-epithelialization and angiogenesis. The final phase is the remodeling of a mature tissue scar, which can take several months or, in some cases, up to a year post-injury. 0 = day of wounding/injury (El Mohtadi, 2019).
In response to chemoattractants such as TGF-β, macrophage chemoattractant protein 1 (MCP-1), and macrophage inflammatory protein (MIP), monocytes from the bloodstream subsequently arrive at the wound area and differentiate into tissue macrophages, peaking in numbers around day 5 to day 7 post-injury (Lorenz and Longaker, 2008[79]; Sen and Roy, 2008[125]). Macrophages replace neutrophils as the predominant inflammatory cells at the wound site and carry out the process of phagocytosis of invading microorganisms, removal of damaged tissues and dead neutrophils, and the release of growth factors such as PDGF and TGF-β (Beanes et al., 2003[20]; El Mohtadi et al., 2020[42]). Damaged extracellular matrix is degraded by the action of macrophage-derived proteolytic enzymes such as metalloproteases. Macrophages also release growth factors that induce the proliferative phase including insulin-like growth factor-1 (IGF-1), keratinocyte growth factor (KGF), epidermal growth factor (EGF) and vascular endothelial growth factor (VEGF) (Shaw et al., 1990[128]). Three to ten days after injury, tissue proliferation starts. It is characterized by the creation of new extracellular matrix (ECM) by fibroblasts, re-epithelialization (the restoration of an intact epidermis) by keratinocytes and angiogenesis (revascularization) by endothelial cells. The final phase is remodeling of the tissue scar, which can take several months or, in some cases, up to a year post-injury. It is characterized by the remodeling of collagen and the vascular maturation of newly formed capillaries, allowing vascular density to return to normal within the wound (Guo and DiPietro, 2010[54]). For successful healing, wound repair requires progression through all four phases in the correct order and time frame (Singer and Clark, 1999[130]; Guo and DiPietro, 2010[54]).
Aging and Wound Healing
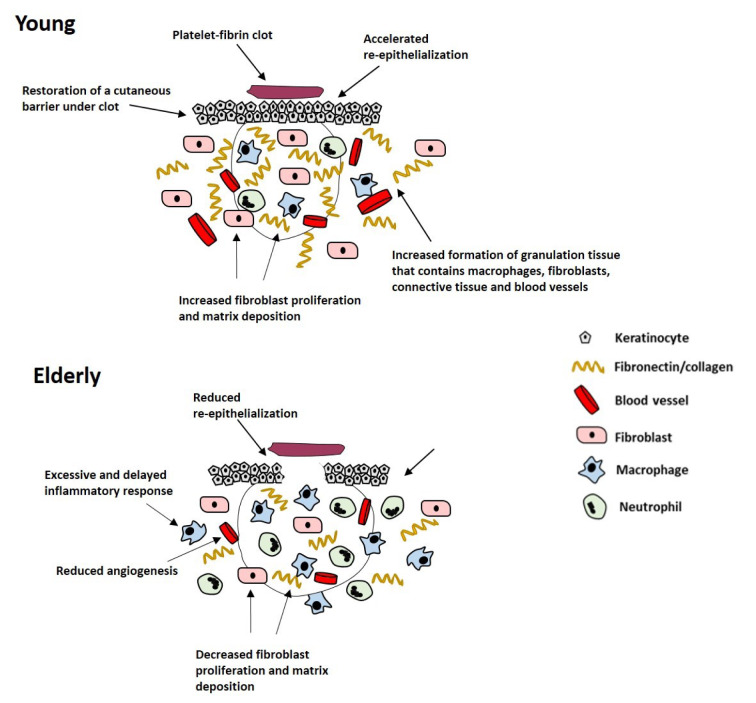
With increasing age, acute wound healing proceeds but becomes delayed. This detrimental change in acute wound healing in the elderly is called age-related impaired healing and is linked with intrinsic cellular aging processes, including an elevated but delayed inflammatory response, reduced cell proliferation and migration, decreased extracellular matrix (ECM) production and increased enzymatic degradation of tissues leading to skin fragility (Thomas, 2001[144]). Delayed wound healing in the elderly is associated with delayed hemostasis (Ashcroft et al., 1999[9]), prolonged and excessive inflammation, delayed re-epithelialization, impaired angiogenesis and reduced matrix deposition (Figure 2(Fig. 2); Reference in Figure 2: El Mohtadi, 2019[41]) (Ashcroft et al., 1997[8], 2002[10]). Although the inflammatory response becomes more pronounced with increasing age, the propensity for wounds to become infected increases in the elderly (Ashcroft et al., 2002[10]; Cooper et al., 2015[37]), due to the delay in wound repair and the impaired ability of inflammatory cells to eliminate bacteria from the wound site (Emori et al., 1991[46]; Thomas, 2001[144]).
Figure 2. Schematic representation of the effect of age on acute wound healing. Age-related impaired healing is linked to delayed but excessive inflammation, delayed re-epithelialization, reduced angiogenesis and decreased fibroblast proliferation and matrix deposition (El Mohtadi, 2019).
In contrast, chronic wounds are characterized by failure of tissue repair processes to proceed through an orderly set of wound healing phases within an expected time frame. Wounds are deemed chronic if they do not heal within three months and in many cases they can take several months or even years to heal (if they heal at all) (Mustoe, 2005[97]; Adeyi et al., 2009[1]). Chronic wounds typically affect the elderly (over 65 years of age) and arise from one or more underlying pathologies, with more than 90 % of chronic wounds being venous, diabetic or pressure ulcers (Boulton et al., 2005[24]). Chronic wounds have major clinical implications and cause an enormous burden on healthcare services, in terms of medical effort and cost (Harding et al., 2002[55]; Boulton et al., 2005[24]). Chronic wound treatment costs the UK National Health Service (NHS) about £5 billion per annum (Guest et al., 2015[52]).
At present, effective therapies/treatments for chronic wounds are somewhat limited, making this an area of research that needs urgent attention. Chronic wounds become trapped within the inflammatory phase of wound repair and are characterized by an excessive, unabated inflammatory response that leads to tissue breakdown (Snyder, 2005[133]; Taylor et al., 2005[143]; Fazli et al., 2009[47]). A shift in the balance between the formation and degradation of ECM occurs, leading to ECM breakdown by destructive inflammatory mediators such as proteases (Edwards et al., 2004[40]; Schönfelder et al., 2005[124]). Chronic wounds also have defective macrophage function that leads to increased propensity of bacterial infection, decreased growth factor secretion, impaired angiogenesis and delayed re-epithelialization (Hohn et al., 1976[60]; Harding et al., 2002[55]; Frykberg and Banks, 2015[48]).
Estrogen and Aging
Endogenous estrogens are produced from cholesterol, initially by several enzymes to create androgens, such as testosterone and androstenedione, which are then converted to estrogens through the action of the P450 enzyme aromatase, in the endoplasmic reticulum of estrogen-producing cells (Payne and Hales, 2004[106]). In adipose tissues, androstenedione is converted to estrone whilst in ovarian granulosa cells testosterone is converted into estradiol. Aromatase is found in many peripheral tissues such as skin, bone, adipose tissue, brain and vascular smooth muscle (Nawata et al., 1995[98]; Simpson, 2000[129]; Azcoitia et al., 2001[17]; Ling et al., 2004[78]). In females at the age of reproduction, systemic estrogen is produced mainly by the ovary. It is predominantly biosynthesized in granulose cells of the ovarian follicles and the corpora lutea. In males, the gonad is the principle producer of systemic estrogen. However, a substantial amount of estrogen is also produced locally in peripheral tissues in both genders, acting in an autocrine and paracrine manner (Labrie et al., 1998[73]). A significant amount of inactive steroid precursors including dehydroepiandrosterone (DHEA), its sulphate (DHEA-S), and androstenedione (4-dione) are produced by the adrenals and converted into active steroid hormones in peripheral tissues (Labrie et al., 1998[73]). Several peripheral human tissues, such as adipose tissue, bone and skin can produce active estrogens and androgens locally from conversion of adrenal-derived inactive precursors (Nelson and Bulun, 2001[99]). Plasma DHEA-S is the major adrenal-derived steroid precursor and levels in adult men and women are around 100 to 500 times higher than those of testosterone and as much as 1000 to 10 000 times higher than those of estradiol (Labrie et al., 2000[74]). Thus, inactive adrenal-derived steroid precursors provide a large circulating reservoir for conversion into potent sex steroid hormones in peripheral tissues. However, the sharp decline in DHEA and DHEA-S production by the adrenals during aging in both genders results in a dramatic fall in the synthesis of active androgens and estrogens in peripheral tissues, a phenomenon which could be associated with several age-related diseases (Labrie et al., 1998[73]). Estrogen synthesized locally in peripheral tissues becomes progressively more important after the menopause in women, when systemic levels are lost (Picard et al., 2000[109]). However, the rapid decline in local production of active estrogens with increasing age means peripheral estrogen production is insufficient to compensate for the loss in systemic estrogen levels in elderly women.
Estrogen Receptors
Over the past decades, the existence of two nuclear estrogen receptor (ER) proteins have been identified, ER-alpha (ER-α) and ER-beta (ER-β), that are part of the nuclear receptor (NR) family. ER-α was first discovered in 1958 (Jensen and Jacobson, 1960[65]) and is known to be predominant in reproductive tissues (Kuiper et al., 1997[71]; Ali and Coombes, 2000[4]; Campbell et al., 2010[33]) whereas ER-β was first identified in rat prostate and ovary in 1996 (Mosselman et al., 1996[94]) and predominates in peripheral, non-reproductive tissues (Kuiper et al., 1997[71]; Ali and Coombes, 2000[4]; Campbell et al., 2010[33]). The biological effects of estrogens are largely mediated by the binding of estrogen to nuclear ER homodimers or heterodimers (Matthews and Gustafsson, 2003[84]), and subsequent activation or repression of gene transcription (Paige et al., 1999[103]). However, rapid, non-genomic estrogen signaling involving membrane-bound ER proteins has also been described (Gruber et al., 2002[51]; Ascenzi et al., 2006[6]). Recent research suggests estrogen can have direct effects on inflammatory cells, such as monocytes and macrophages, and skin-associated cells such as keratinocytes, due to the presence of nuclear and membrane-bound ER proteins (Weusten et al., 1986[151]; Stimson, 1988[137]; Cocchiara et al., 1990[36]). The response of particular inflammatory cells depends on the local levels of estrogen and the maturity (stage of differentiation) of the cells (Ashcroft and Ashworth, 2003[7]).
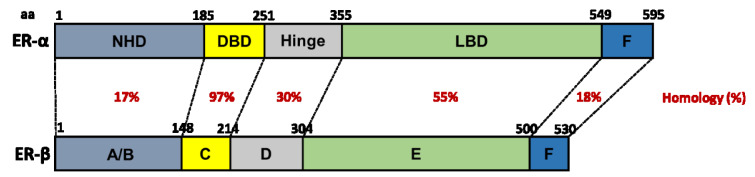
Estrogen signals predominantly by binding to inactive ER proteins in the nucleus of the cell (Klinge, 2000[69]). ER proteins share a structure (Figure 3(Fig. 3); References in Figure 3: Webb et al., 1999[149]; Klinge, 2000[69]; Begam et al., 2017[21]; El Mohtadi, 2019[41]) that is typical of the NR family, consisting of six domains (A-F) (Kuiper et al., 1998[72]; Klinge, 2000[69]; Begam et al., 2017[21]). ER proteins are expressed in skin, suggesting estrogen regulates skin function, maintenance and/or turnover (Ashworth, 2005[14]). While ER-α and ER-β have 97 % homology in the C domain that acts as a DNA-binding domain (DBD), they only have 55 % homology in the E domain which forms the ligand-binding domain (LBD) (Barkhem et al., 1998[18]; Webb et al., 1999[149]; Klinge, 2000[69]), enabling targeted ER activation using artificial ligands with ER-specific binding affinity.
Figure 3. The structure of human ER-α and ER-β. Homology between domains (A-F) is represented as percentage (%) similarity. NHD = N-terminal homology domain, DBD = DNA-binding domain, LBD = ligand-binding domain (Webb et al., 1999; Klinge, 2000; Begam et al., 2017; El Mohtadi, 2019).
When estrogen binds to ER proteins, they become activated and dimerize (Klinge, 2000[69]). The DBD of each activated ER then binds to an estrogen response element (ERE) in the DNA of target genes and induces gene transcription (Kuiper et al., 1998[72]; Klinge, 2000[69]). In cells expressing a single ER subtype, homodimers of ER-α or ER-β are formed (Kuiper et al., 1998[72]). In cells that express both ER subtypes, a heterodimer containing one ER-α and one ER-β may form (Kuiper et al., 1998[72]). ER heterodimers and ER-α homodimers bind to DNA with a similar affinity. However, ER-β homodimers bind to DNA with a lower affinity (Kuiper et al., 1998[72]).
Both ER-α and ER-β enhance aspects of acute wound repair but their roles are somewhat different; although ER-α regulates inflammatory cell activity, ER-β appears to modulate the overall wound healing response (Emmerson and Hardman, 2012[45]). The delayed wound repair observed in ovariectomized mice can be reversed by stimulation of ER-β alone, whilst ER-α activation alone fails to enhance murine wound repair (Campbell et al., 2010[33]). Moreover, estrogen replacement therapy in ovariectomized mice lacking functional ER-β retards wound healing, suggesting ER-β may be critical to establishing prompt tissue formation during wound repair (Campbell et al., 2010[33]). In addition, a human study conducted by Ashworth (2005[14]) indicates that polymorphisms in the 0N promoter region of the human ER-β gene are significantly associated with chronic venous ulceration in the British Caucasian population.
Effect of Estrogen on Skin Maintenance
It is commonly accepted that the age-related reduction in estrogen levels is linked with skin degeneration. However, most evidence in humans comes from studies performed in pre- and/or post-menopausal women. During pregnancy, skin syndromes such as psoriasis have been shown to improve, an effect that is directly linked to increased estrogen levels in the circulation (Boyd et al., 1996[25]). Moreover, oral contraceptive pills are frequently used to treat severe acne. During the menopause, estrogen deficiency results in detrimental changes in skin appearance including sagging, wrinkling, dryness and fragility (Ashcroft et al., 1999[9]; Shah and Maibach, 2001[127]). These changes can often be reversed during the first 6 months of topical or systemic estrogen replacement therapy (Brincat et al., 1987[27]).
There is a reduction in mainly collagen type III, but also type I to some degree, in the skin of post-menopausal women compared to pre-menopausal women, resulting in a decrease in the ratio of type III/type I collagen within the dermis that is associated with estrogen deficiency (Affinito et al., 1999[2]; Horng et al., 2017[62]). When applied locally to the skin of post-menopausal women, estradiol significantly increases the production of hydroxyproline, reflecting elevated collagen synthesis in the dermis (Albright et al., 1941[3]; Affinito et al., 1999[2]; Sator et al., 2001[120]; Horng et al., 2017[62]). Indeed, topical estrogen improves the external facial appearance of post-menopausal women by reducing skin sagging and wrinkling (Schmidt et al., 1994[123]). Not only topical but also systemic estrogen supplementation conserves skin thickness by promoting dermal collagen deposition in post-menopausal women (Savvas et al., 1993[122]; Sauerbronn et al., 2000[121]).
It has also been reported that estrogen replacement therapy can improve skin elasticity by 5 % per year (Brincat et al., 1987[27]). In line with this finding, topical estrogen supplementation improves the elasticity of ECM fibres in the dermis (Albright et al., 1941[3]; Sator et al., 2001[120]). Topical estrogen ointments notably increase the number and thickness of elastin fibres in the ECM, with histological examination demonstrating improved orientation and reduced fibre fragmentation in the dermis (Punnonen et al., 1987[112]). Estrogen also promotes the synthesis of glycosaminoglycans in the ECM, restoring skin turgor and moisture levels (Brincat, 2000[26]).
Topical estrogen application enhances stratum corneum barrier function of skin in post-menopausal women and increases the rate of mitosis and turnover of epidermal cells (Stumpf et al., 1974[139]). Estrogen also enhances the vascularization of dermis and in terms of skin appendages, estrogen extends the life cycle of human hair follicles but retards hair growth and sebum secretion by sebaceous glands (Stumpf et al., 1974[139]).
In summary, the age-related fall in the levels of estrogen detrimentally affects the maintenance and turnover of intact skin, whilst estrogen supplementation reverses these effects in the elderly by stimulating keratinocyte proliferation, increasing ECM deposition and quality, and enhancing skin turgor and moisture retention.
Estrogen and Wound Healing
The influence of estrogen on wound healing was first studied in animals in 1947 (Sjövall, 1947[132]; Horng et al., 2017[62]) and then in humans in 1953 (Sjöstedt, 1953[131]; Horng et al., 2017[62]). Subsequently, there has been an accumulating body of evidence supporting estrogen as a global regulator of wound healing (Brincat et al., 1987[27]; Varila et al., 1995[146]; Affinito et al., 1999[2]; Sauerbronn et al., 2000[121]; Mills et al., 2005[89]; Hardman and Ashcroft, 2008[56]; Brufani et al., 2009[28]; Lee et al., 2013[76]; Midgley et al., 2016[87]; Mukai et al., 2016[96]; Chenu et al., 2017[34]; Leblanc et al., 2017[75]; Horng et al., 2017[62]; Pepe et al., 2017[107]; Wilkinson and Hardman, 2017[154]).
Research has demonstrated the key role of sex-steroid hormones in inflammation and the wound healing process (Guo and DiPietro, 2010[54]; Gilliver et al., 2007[50]). Estrogen has protective, anti-inflammatory properties in several tissues (Straub, 2007[138]). Estrogen has also been reported to stimulate wound repair processes such as re-epithelialization and ECM production independently from its anti-inflammatory effects in elderly subjects of both genders (Ashcroft et al., 1997[8]). HRT-treated post-menopausal women heal acute wounds faster than their age-matched control counterparts, who have taken no estrogen supplementation (Ashcroft et al., 1997[8]). Other reports indicate that topical estrogen supplementation enhances wound healing in elderly male and female patients, connected with a reduced inflammatory response (Ashcroft et al., 1997[8], 1999[9]).
Variances in the human immune system between male and female subjects have been identified in several epidemiological and medical studies (McGowan et al., 1975[85]; Bone, 1992[23]), with evidence indicating that women have a superior immune system compared to men (Gulshan et al., 1990[53]; Wichmann et al., 1996[153]). Other experiments have indicated that estrogen has immune-enhancing properties during stress, including increased resistance to several pathogenic infections (Yamamoto, 1999[157]).
Since systemic and peripheral estrogens decline with age, it is suggested that estrogen deprivation in the elderly could increase the propensity for chronic wounds. Margolis et al. (2002[82]) performed a case-cohort study to investigate the protective effects of estrogen against chronic wounds. Patients aged oved 65 years receiving HRT treatment were shown to be 30-40 % less likely to develop a venous leg ulcer than age-matched patients lacking HRT supplementation (Margolis et al., 2002[82]).
Chronic wounds are characterized by an excessive and chronic prolonged inflammation. High levels of inflammatory mediators, including tumor necrosis factor alpha (TNF-α), interleukin-1 beta (IL-1β), IL-6, IGF-1 and matrix metalloproteinases (MMPs), that are present in chronic wound exudate (Ashcroft et al., 1997[8], 1999[9]) are downregulated via the action of estrogen (Vural et al., 2006[148]; Straub, 2007[138]; Wira et al., 2015[155]). In particular, TNF-α is elevated in humans that are predisposed to chronic wounds and has been identified as a therapeutic target for impaired wound healing in the elderly (Ashcroft et al., 2012[13]). Both systemic and topical estrogen treatments enhance wound healing in elderly men and women by stimulating re-epithelialization, angiogenesis, matrix deposition and wound contraction whilst dampening the inflammatory response and expression of pro-inflammatory cytokines and proteolytic mediators (Ashcroft et al., 1997[8]; Ashcroft and Ashworth, 2003[7]; Thornton, 2013[145]; Archer, 2012[5]; Stevenson and Thornton, 2007[136]).
Effect of estrogen on the inflammatory phase of wound healing
It is commonly known that age-related impaired healing is associated with an excessive and prolonged inflammatory response, linked with increased but delayed inflammatory cell recruitment, and increased secretion of pro-inflammatory cytokines such as TNF-α (Ralston et al., 1990[115]; Pottratz et al., 1994[111]). Moreover, TNF-α is elevated in elderly patients with venous ulcers compared to age-matched healthy controls, with the highest levels of TNF-α typically found in patients carrying polymorphisms of the promoter region of the ER-β gene that predispose to venous ulceration (Ashworth et al., 2008[15]).
Recent research has indicated that chronic wounds are associated with elevated levels of elastase and MMPs, which are released by macrophages, keratinocytes and fibroblasts, and linked with excessive tissue destruction (Wysocki et al., 1993[156]). Estrogen has been described to control and dampen the early inflammatory response during acute wound healing by inhibiting neutrophil infiltration to the wound via a reduction in the expression of cell adhesion molecules (Ashcroft et al., 1999[9]; Sproston et al., 2018[134]). Furthermore, estrogen increases the oxidative metabolism of neutrophils, suggesting estrogen deprivation could lead to diminished phagocytic capability of neutrophils, an increased risk of infection and a postponement in healing (Magnusson and Einarsson, 1990[81]). Estrogen has been shown to have a direct influence on monocytes and macrophages, due to their possession of both nuclear and membrane-bound estrogen receptor (ER) proteins (Weusten et al., 1986[151]; Suenaga et al., 1996[141], 1998[140]). In addition, 17β-estradiol has been reported to reverse the substantial delay in cutaneous murine wound healing induced by bacterial lipopolysaccharide (Crompton et al., 2016[38]).
Increased levels of epidermal pro-matrix metalloproteinase-2 (pro-MMP-2) have been observed in intact aging skin and is immediately activated following cutaneous injury, explaining the reported rise in MMP-2 and ECM degeneration observed in the wounds of the elderly (Ashcroft et al., 1997[12]). In addition, research suggests that estrogen deficiency inhibits the differentiation of monocytes into tissue macrophages during the inflammatory phase of wound healing, leading to an increase in protease expression (Calvin et al., 1998[32]). Estrogen decreases tissue-damaging protease levels, including elastase and MMP secretion, leading to an overall increase in the content of collagen and fibronectin in the dermis (Ashcroft et al., 1999[9]).
In skin, the anti-inflammatory effect of estrogen is predominantly mediated through inhibition of the pro-inflammatory cytokine, macrophage migration inhibitory factor (MIF) (Hardman et al., 2005[57]). Macrophage migration inhibitory factor (MIF) has been identified as a global regulator of wound healing mediated by estrogen and released by monocytes, macrophages, neutrophils, endothelial cells and keratinocytes (Hardman et al., 2005[57]; Emmerson et al., 2009[44]). Ashcroft et al. (2003[11]) reported that mice with estrogen deficiency have higher MIF levels, resulting in an elevated inflammatory response and delayed wound healing, whereas MIF null-mice displayed enhanced wound healing, with lower inflammation and greater matrix formation. Estrogen downregulates MIF expression leading to a decline in inflammation, enhanced matrix deposition, increased re-epithelialization and an overall accelerated wound repair (Hardman et al., 2005[57]).
Effect of estrogen on the proliferative phase of wound healing
Age-related impaired healing is linked with reduced growth factor expression, reduced keratinocyte proliferation and increased response to inhibitory cytokines, causing a delayed re-epithelialization in vivo (Butcher and Klingsberg, 1963[30]; Rattan and Derventzi, 1991[116]; Holt et al., 1992[61]). Estrogen enhances the mitogenesis of keratinocytes and increases re-epithelialization in post-menopausal women (Ashcroft et al., 1997[8]). It has been reported that the rate of wound re-epithelialization of post-menopausal women treated with HRT for more than 3 months was similar to levels of re-epithelialization in pre-menopausal females, whereas a non-HRT post-menopausal group showed diminished re-epithelialization. This improved re-epithelialization following estrogen supplementation is due to increased proliferation of epidermal keratinocytes (Raja et al., 2007[114]).
In addition to its effect on epithelial migration and proliferation, estrogen indirectly effects matrix deposition by mesenchymal cells. Various in vivo animal studies report that estrogen increases fibroblast infiltration and collagen deposition. In contrast, a small number of studies report a decrease in fibroblast infiltration and collagen deposition following treatment with estrogen in mice (Lundgren, 1973[80]; Pallin et al., 1975[104]). A possible explanation for these contradictions include differences in the wound models, hormone concentrations and intervals of administration used. Furthermore, the duration of estrogen insufficiency results in distinct effects on several healing parameters; for instance, wound contraction becomes reduced after 4 months of estrogen deprivation whereas matrix deposition becomes reduced after only 1 month (Calvin et al., 1998[31]). In humans, topical estrogen supplementation in elderly men and women results in reduced wound size via stimulation of wound contraction (Ashcroft et al., 1999[9]). Estrogen promotes PDGF expression by monocytes and macrophages (Mendelsohn and Karas, 1999[86]), leading to mitogenesis and chemotaxis of fibroblasts and a subsequent increase in wound contraction and ECM deposition (Seppä et al., 1982[126]). Estrogen also enhances the secretion of TGF-β1 by dermal fibroblasts in vivo (Ashcroft et al., 1997[8], 1999[9]), resulting in enhanced formation of ECM, particularly collagen deposition (Ashcroft and Ashworth, 2003[7]).
Estrogen promotes angiogenesis, leading to increased granulation tissue (Iyer et al., 2012[64]) through a direct stimulation of endothelial cells (Rubanyi et al., 2002[118]). Estrogen modulates the synthesis of IL-1 by tissue macrophages, a key protein implicated in the creation of a new granulation tissue (Hu et al., 1988[63]). Estrogen increases endothelial cell attachment to laminin, fibronectin and collagens I and IV in vitro. In addition, estrogen enhances the creation of capillary-like structures by endothelial cells, when positioned on a reconstructed basement membrane (Morales et al., 1995[92]). Paradoxically, other in vitro studies report a reduction in vascularity following stimulation with estrogen (Nyman, 1971[102]; Lundgren, 1973[80]). The precise effect of estrogen on angiogenesis remains unknown, and additional investigations are needed to define the impact of estrogen on vascularzsation in acute and impaired wound healing.
In summary, despite some contradictions in the literature, estrogen appears on balance to enhance most tissue formation occurring in the proliferative phase of wound healing, particularly re-epitheliazation and ECM formation.
Effect of estrogen on the remodeling phase of wound healing
The age-related decline in estrogen levels causes a decrease in wound collagen and fibronectin in vivo. This has been associated with elevated levels of inflammatory cell-derived elastase, MMP-2 and MMP-9 (Herrick et al., 1997[59]; Ashcroft et al., 1997[12]). Estrogen supplementation reverses the degradation of ECM by inhibiting the synthesis of wound proteases such as MMPs during wound remodeling (Ashcroft and Ashworth, 2003[7]; Brincat, 2000[26]).
Topical estrogen supplementation increases the deposition of collagen during the remodeling phase of wound repair in elderly patients (Ashcroft et al., 1997[8], 1999[9]). Previous animal studies report that 17β-estradiol increases the production of tissue inhibitor of metalloproteinases (TIMPs) by rabbit uterine fibroblasts, but reduces the production of pro-collagenase and pro-stromelysin (Sato et al., 1991[119]). Another in vivo study reports that topical estrogen treatment increases collagen deposition in elderly males and females after 7 and 80 days post-injury (Ashcroft et al., 1999[9]). It was also noticed in other in vivo studies that matrix collagen deposition at 7 and 84 days post-wounding decreased in post-menopausal women lacking HRT treatment. In contrast, post-menopausal females who took HRT for more than 3 months had similar levels of matrix collagen deposition and wound remodeling as younger pre-menopausal females (Ashcroft et al., 1997b, 1999[9]).
Estrogen stimulates the expression of TGF-β1 in vivo. This results in improving collagen deposition in the dermis (Ashcroft et al., 1997[8]). Reports suggest a decreased wound collagen deposition associated with MMP-mediated collagenolysis in ovarectomized rats (Pirila et al., 2001[110]). These effects were reversed by estrogen replacement, implicating estrogen as a pivotal mediator involved in shifting the balance from matrix degradation to matrix synthesis (Pirila et al., 2001[110]). Interestingly, an in vivo study indicated that the quality of mature tissue scars was greater in post-menopausal women in comparison with pre-menopausal women. This suggests that estrogen enhances wound repair at the expense of scar quality (Ashcroft et al., 1997[8]).
Future Perspectives for Estrogen Therapies
Although many known effects of estrogen on wound healing have been established in the past two decades, fewer recent developments have been made and there remain substantial areas for further investigation. It has been established that estrogen plays a fundamental beneficial role in skin maintenance and acute wound healing processes. Moreover, the systemic and peripheral decline in estrogen with increasing age suggests estrogen deprivation could be linked with chronic wounds in the elderly. However, systemic estrogen replacement therapy is an unfocused, biological sledgehammer rather than a targeted treatment strategy. Although estrogen is protective against photoaging, an extrinsic aging process that correlates with higher mortality rates from skin cancers in men than women (Weinstock, 1994[150]; Miller and Neil, 1997[88]), unopposed systemic estrogen replacement therapy is a risk factor for breast and endometrial cancer development (Nuttall et al., 2001[101]), thereby restricting its exploitation in clinical practice. The widespread distribution of estrogen-responsive tissues exposes non-target cells to the potential hyper-proliferative and neoplastic effects of systemic estrogen therapies, suggesting either local estrogen or targeted therapies are needed. Interestingly, studies performed in vitro have shown that ER-β is the dominant partner in heterodimers, resulting in an ER-β-predominant effect with repressed ER-α transcriptional activity (Pettersson and Gustafsson, 2001[108]). Thus, by modulating ER-α-mediated gene transcription, ER-β may decrease the overall cellular sensitivity to estrogen and provide protection against the hyper-proliferative and neoplastic effects of ER-α (Rollerova and Urbancikova, 2000[117]). Thus, a clear understanding of tissue-specific regulation of ER expression and downstream cellular and molecular mechanisms of estrogen action might enable controlled manipulation of estrogen signaling pathways during wound repair, potentially leading to the development of more targeted therapies with fewer side effects on non-target tissues.
Selective estrogen receptor modulators (SERMs) are ER-interacting molecules that have the ability to bind ER proteins and act as agonists in some tissues whilst acting as antagonists in different tissues (Brzozowski et al., 1997[29]; Cho and Nuttall, 2001[35]). SERMs have been used clinically to promote the beneficial effects of estrogen in target tissues whilst reducing the detrimental effects of estrogen (e.g. increased risk of breast cancer) in non-target tissues (Mirkin and Pickar, 2015[90]). Tamoxifen, raloxifene and the dietary phytoestrogen genistein are the most frequently documented SERMs in the literature. They are known to have estrogenic effects in numerous peripheral tissues, but are anti-estrogenic in the breast tissue and are therefore used extensively in breast cancer research (Furr and Jordan, 1984[49]; Morris and Wakeling, 2002[93]; Park and Jordan, 2002[105]; Mirkin and Pickar, 2015[90]). Tamoxifen was discovered and reported by the Food and Drug Administration (FDA) in 1977 (Park and Jordan, 2002[105]; Jordan, 2006[66]; Mirkin and Pickar, 2015[90]; Quirke, 2017[113]). Tamoxifen binds to both ER proteins and its effect depends on the cell and tissue type, being anti-estrogenic in breast tissue and therefore commonly used to prevent and/or treat breast cancer in both post- and pre-menopausal females (Zidan et al., 2004[158]; Quirke, 2017[113]). Tamoxifen has also been reported to maintain the density of bone in rats and humans (Jordan et al., 1987[67]; Zidan et al., 2004[158]). However, it has multiple side effects and is frequently linked with endometrial cancer due to its estrogenic effects in the uterus (Kedar et al., 1994[68]).
There have been some investigations on the effect of SERMs on skin and wound healing processes. Tamoxifen and raloxifene have been shown to stimulate fibroblast proliferation in vitro (Stevenson et al., 2009[135]). While raloxifene improves skin elasticity and collagen deposition in post-menopausal females (Sumino et al., 2009[142]), genistein has been reported to improve the vascularization of the dermis and augment the loss of epidermal thickness typically observed in post-menopausal females (Moraes et al., 2009[91]). Another study on mice indicated genistein stimulates wound healing via synthesis of TGF-β1 (Marini et al., 2010[83]). Moreover, tamoxifen, raloxifene and genistein all significantly enhance wound healing in ovariectomized mice by stimulating re-epithelialization and dampening inflammation via activation of ER-β (Hardman et al., 2008[58]; Emmerson et al., 2010[43]). However, the use of existing SERMs have not yet been exploited in the treatment of chronic wound states.
The repurposing of existing pharmaceutical drugs or the development of novel therapies that act as ER-specific ligands or exhibit tissue-specific estrogenic effects, delivered locally within specialized wound dressings may have potential clinical applications in the treatment of chronic wound states in the elderly. Understanding the differential effects on downstream gene transcription or repression in various tissue/cell types may help develop more focused treatments for impaired wounds that can mediate specific estrogen-responsive signaling pathways in injured tissues whilst reducing unwanted side effects in non-target tissues.
Conclusion
The literature indicates estrogen deficiency is a central paradigm of age-related impaired wound healing in both genders, with topical and systemic estrogen replacement reversing the detrimental effects of aging on both wound repair and skin maintenance. There is growing evidence indicating estrogen deprivation may also contribute to the development of chronic wounds in the elderly but further research is needed in this area. Interestingly, although the beneficial effects of estrogen on wound repair have been widely explored, the development of estrogen-based treatments to promote healing has failed to gain traction to date, most likely due to undesired cellular activity (including hyper-proliferative/neoplastic effects) in non-target tissues. However, a rekindled interest may be stimulated by prospects of developing targeted therapeutic strategies that might promote healing through selective activation of estrogen-responsive signaling pathways in regenerating peripheral tissues, whilst leaving non-target tissues largely unaffected.
Conflict of interest
The authors declare no conflict of interest.
Acknowledgement
The authors wish to acknowledge that this review article includes some aspects of the introductory chapters of the PhD thesis submitted by the lead author (Mohamed El Mohtadi).
References
- 1.Adeyi A, Muzerengi S, Adeyi IGA, Gupta I. Leg ulcers in older people: A review of management. Br J Med Practit. 2009;2(3):21–28. [Google Scholar]
- 2.Affinito P, Palomba S, Sorrentino C, Di Carlo C, Bifulco G, Arienzo MP, et al. Effects of postmenopausal hypoestrogenism on skin collagen. Maturitas. 1999;33:239–247. doi: 10.1016/s0378-5122(99)00077-8. [DOI] [PubMed] [Google Scholar]
- 3.Albright F, Smith PH, Richardson AM. Postmenopausal osteoporosis: Its clinical features. J Am Med Assoc. 1941;116:2465–2474. [Google Scholar]
- 4.Ali S, Coombes RC. Estrogen receptor alpha in human breast cancer: Occurrence and significance. J Mammary Gland Biol Neoplasia. 2000;5:271–281. doi: 10.1023/a:1009594727358. [DOI] [PubMed] [Google Scholar]
- 5.Archer DF. Postmenopausal skin and estrogen. Gynecol Endocrinol. 2012;28(Suppl 2):2–6. doi: 10.3109/09513590.2012.705392. [DOI] [PubMed] [Google Scholar]
- 6.Ascenzi P, Bocedi A, Marino M. Structure–function relationship of estrogen receptor α and β: Impact on human health. Mol Aspects Med. 2006;27:299–402. doi: 10.1016/j.mam.2006.07.001. [DOI] [PubMed] [Google Scholar]
- 7.Ashcroft GS, Ashworth JJ. Potential role of estrogens in wound healing. Am J Clin Dermatol. 2003;4:737–743. doi: 10.2165/00128071-200304110-00002. [DOI] [PubMed] [Google Scholar]
- 8.Ashcroft GS, Dodsworth J, Van Boxtel E, Tarnuzzer R, Horan MA, Schultz GS, et al. Estrogen accelerates cutaneous wound healing associated with an increase in TGF-b1 levels. Nat Med. 1997;3(11):1209–1215. doi: 10.1038/nm1197-1209. [DOI] [PubMed] [Google Scholar]
- 9.Ashcroft GS, Greenwell-Wild T, Horan MA, Wahl SM, Ferguson MW. Topical estrogen accelerates cutaneous wound healing in aged humans associated with an altered inflammatory response. Am J Pathol. 1999;155:1137–1146. doi: 10.1016/S0002-9440(10)65217-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ashcroft GS, Mills SJ, Ashworth JJ. Ageing and wound healing. Biogerontology. 2002;3:337–345. doi: 10.1023/a:1021399228395. [DOI] [PubMed] [Google Scholar]
- 11.Ashcroft GS, Mills SJ, Lei K, Gibbons L, Jeong M-J, Taniguchi M, et al. Estrogen modulates cutaneous wound healing by downregulating macrophage migration inhibitory factor. J Clin Invest. 2003;111:1309–1318. doi: 10.1172/JCI16288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ashcroft, Horan MA, Herrick SE, Tarnuzzer RW, Schultz GS, Ferguson MWJ. Age-related differences in the temporal and spatial regulation of matrix metalloproteinases (MMPs) in normal skin and acute cutaneous wounds of healthy humans. Cell Tissue Res. 1997;290:581–591. doi: 10.1007/s004410050963. [DOI] [PubMed] [Google Scholar]
- 13.Ashcroft, Jeong MJ, Ashworth JJ, Hardman M, Jin W, Moutsopoulos N, et al. Tumor necrosis factor‐alpha (TNF‐α) is a therapeutic target for impaired cutaneous wound healing. Wound Repair Regen. 2012;20:38–49. doi: 10.1111/j.1524-475X.2011.00748.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ashworth JJ. Estrogen receptor polymorphisms and wound healing. Manchester, UK: The University of Manchester, Faculty of Life Sciences; 2005. [Google Scholar]
- 15.Ashworth JJ, Smyth JV, Pendleton N, Horan M, Payton A, Worthington J, et al. Polymorphisms spanning the 0N exon and promoter of the estrogen receptor‐beta (ERβ) gene ESR2 are associated with venous ulceration. Clin Genet. 2008;73:55–61. doi: 10.1111/j.1399-0004.2007.00927.x. [DOI] [PubMed] [Google Scholar]
- 16.Ashworth JJ, Smyth JV, Pendleton N, Horan M, Payton A, Worthington J, et al. The dinucleotide (CA) repeat polymorphism of estrogen receptor beta but not the dinucleotide (TA) repeat polymorphism of estrogen receptor alpha is associated with venous ulceration. J Steroid Biochem Mol Biol. 2005;97:266–270. doi: 10.1016/j.jsbmb.2005.05.012. [DOI] [PubMed] [Google Scholar]
- 17.Azcoitia I, Sierra A, Veiga S, Honda Si, Harada N, Garcia‐Segura LM. Brain aromatase is neuroprotective. J Neurobiol. 2001;47:318–329. doi: 10.1002/neu.1038. [DOI] [PubMed] [Google Scholar]
- 18.Barkhem T, Carlsson B, Nilsson Y, Enmark E, Gustafsson J-Å, Nilsson S. Differential response of estrogen receptor α and estrogen receptor β to partial estrogen agonists/antagonists. Mol Pharmacol. 1998;54:105–112. doi: 10.1124/mol.54.1.105. [DOI] [PubMed] [Google Scholar]
- 19.Bauer E, Cooper T, Huang J, Altman J, Deuel T. Stimulation of in vitro human skin collagenase expression by platelet-derived growth factor. Proc Natl Acad Sci U S A. 1985;82:4132–4136. doi: 10.1073/pnas.82.12.4132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Beanes SR, Dang C, Soo C, Ting K. Skin repair and scar formation: The central role of TGF-[beta] Expert Rev Mol Med. 2003;5(08):1–22. doi: 10.1017/S1462399403005817. [DOI] [PubMed] [Google Scholar]
- 21.Begam AJ, Jubie S, Nanjan M. Estrogen receptor agonists/antagonists in breast cancer therapy: A critical review. Bioorg Chem. 2017;71:257–274. doi: 10.1016/j.bioorg.2017.02.011. [DOI] [PubMed] [Google Scholar]
- 22.Bérard A, Kahn SR, Abenhaim L. Is hormone replacement therapy protective for venous ulcer of the lower limbs? Pharmacoepidemiol Drug Saf. 2001;10:245–251. doi: 10.1002/pds.582. [DOI] [PubMed] [Google Scholar]
- 23.Bone RC. Toward an epidemiology and natural history of SIRS (systemic inflammatory response syndrome) JAMA. 1992;268:3452–3455. [PubMed] [Google Scholar]
- 24.Boulton AJM, Vileikyte L, Ragnarson-Tennvall G, Apelqvist J. The global burden of diabetic foot disease. Lancet. 2005;366(9498):1719–1724. doi: 10.1016/S0140-6736(05)67698-2. [DOI] [PubMed] [Google Scholar]
- 25.Boyd AS, Morris LF, Phillips CM, Menter MA. Psoriasis and pregnancy: Hormone and immune system interaction. Int J Dermatol. 1996;35:169–172. doi: 10.1111/j.1365-4362.1996.tb01632.x. [DOI] [PubMed] [Google Scholar]
- 26.Brincat MP. Hormone replacement therapy and the skin. Maturitas. 2000;35:107–117. doi: 10.1016/s0378-5122(00)00097-9. [DOI] [PubMed] [Google Scholar]
- 27.Brincat MP, Versi E, Moniz CF, Magos A, de Trafford J, Studd JW. Skin collagen changes in postmenopausal women receiving different regimens of estrogen therapy. Obstet Gynecol. 1987;70:123–127. [PubMed] [Google Scholar]
- 28.Brufani M, Ceccacci F, Filocamo L, Garofalo B, Joudioux R, La Bella A, et al. Novel locally active estrogens accelerate cutaneous wound healing. A preliminary study. Mol Pharm. 2009;6:543–556. doi: 10.1021/mp800206b. [DOI] [PubMed] [Google Scholar]
- 29.Brzozowski AM, Pike AC, Dauter Z, Hubbard RE, Bonn T, Engström O, et al. Molecular basis of agonism and antagonism in the oestrogen receptor. Nature. 1997;389(6652):753. doi: 10.1038/39645. [DOI] [PubMed] [Google Scholar]
- 30.Butcher EO, Klingsberg J. Age, gonadectomy, and wound healing in the palatal mucosa of the rat. Oral Surg Oral Med Oral Pathol. 1963;16:484–493. doi: 10.1016/0030-4220(63)90178-6. [DOI] [PubMed] [Google Scholar]
- 31.Calvin M, Dyson M, Rymer J, Young SR. The effect of ovarian hormone deficiency on macrophage infiltration during the inflammatory phase of wound healing in a rat model. Wounds: A compendium of clinical research and practice. 1998;10(5):158–163. [Google Scholar]
- 32.Calvin M, Dyson M, Rymer J, Young SR. The effects of ovarian hormone deficiency on wound contraction in a rat model. Br J Obstet Gynaecol. 1998;105:223–227. doi: 10.1111/j.1471-0528.1998.tb10057.x. [DOI] [PubMed] [Google Scholar]
- 33.Campbell L, Emmerson E, Davies F, Gilliver SC, Krust A, Chambon P, et al. Estrogen promotes cutaneous wound healing via estrogen receptor β independent of its antiinflammatory activities. J Exp Med. 2010;207:1825–1833. doi: 10.1084/jem.20100500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chenu C, Adlanmerini M, Boudou F, Chantalat E, Guihot A-L, Toutain C, et al. Testosterone prevents cutaneous ischemia and necrosis in males through complementary estrogenic and androgenic actions. Arterioscler Thromb Vasc Biol. 2017;37:909–919. doi: 10.1161/ATVBAHA.117.309219. [DOI] [PubMed] [Google Scholar]
- 35.Cho CH, Nuttall ME. Therapeutic potential of oestrogen receptor ligands in development for osteoporosis. Emerg Drugs. 2001;6(1):137–154. doi: 10.1517/14728214.6.1.137. [DOI] [PubMed] [Google Scholar]
- 36.Cocchiara R, Albeggiani G, Di Trapani G, Azzolina A, Lampiasi N, Rizzo F, et al. Modulation of rat peritoneal mast cell and human basophil histamine release by estrogens. Int Arch Allergy Immunol. 1990;93:192–197. doi: 10.1159/000235300. [DOI] [PubMed] [Google Scholar]
- 37.Cooper RL, Segal RA, Diegelmann RF, Reynolds AM. Modeling the effects of systemic mediators on the inflammatory phase of wound healing. J Theor Biol. 2015;367:86–99. doi: 10.1016/j.jtbi.2014.11.008. [DOI] [PubMed] [Google Scholar]
- 38.Crompton R, Williams H, Ansell D, Campbell L, Holden K, Cruickshank S, et al. Oestrogen promotes healing in a bacterial LPS model of delayed cutaneous wound repair. Lab Invest. 2016;96:439–449. doi: 10.1038/labinvest.2015.160. [DOI] [PubMed] [Google Scholar]
- 39.Dovi JV, Szpaderska AM, DiPietro LA. Neutrophil function in the healing wound: Adding insult to injury? Thromb Haemost. 2004;92:275–280. doi: 10.1160/TH03-11-0720. [DOI] [PubMed] [Google Scholar]
- 40.Edwards JV, Howley P, Cohen IK. In vitro inhibition of human neutrophil elastase by oleic acid albumin formulations from derivatized cotton wound dressings. Int J Pharm. 2004;284(1-2):1–12. doi: 10.1016/j.ijpharm.2004.06.003. [DOI] [PubMed] [Google Scholar]
- 41.El Mohtadi M. Effect of estrogen on host-pathogen interactions in ex vivo and in vitro models of the inflammatory phase of age-related impaired healing. Manchester, UK: Manchester Metropolitan University, Department of Life Sciences; 2019. [Google Scholar]
- 42.El Mohtadi M, Pilkington L, Liauw CM, Ashworth JJ, Dempsey-Hibbert N, Belboul A, et al. Differential engulfment of Staphylococcus aureus and Pseudomonas aeruginosa by monocyte-derived macrophages is associated with altered phagocyte biochemistry and morphology. EXCLI J. 2020;19:1372–1384. doi: 10.17179/excli2020-2766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Emmerson E, Campbell L, Ashcroft GS, Hardman MJ. The phytoestrogen genistein promotes wound healing by multiple independent mechanisms. Mol Cell Endocrinol. 2010;321:184–193. doi: 10.1016/j.mce.2010.02.026. [DOI] [PubMed] [Google Scholar]
- 44.Emmerson E, Campbell L, Ashcroft GS, Hardman MJ. Unique and synergistic roles for 17β-estradiol and macrophage migration inhibitory factor during cutaneous wound closure are cell type specific. Endocrinology. 2009;150:2749–2757. doi: 10.1210/en.2008-1569. [DOI] [PubMed] [Google Scholar]
- 45.Emmerson E, Hardman MJ. The role of estrogen deficiency in skin ageing and wound healing. Biogerontology. 2012;13(1):3–20. doi: 10.1007/s10522-011-9322-y. [DOI] [PubMed] [Google Scholar]
- 46.Emori TG, Banerjee SN, Culver DH, Gaynes RP, Horan TC, Edwards JR, et al. Nosocomial infections in elderly patients in the United States, 1986–1990. Am J Med. 1991;91:S289–SS93. doi: 10.1016/0002-9343(91)90384-a. [DOI] [PubMed] [Google Scholar]
- 47.Fazli M, Bjarnsholt T, Kirketerp-Møller K, Jørgensen B, Andersen AS, Krogfelt KA, et al. Nonrandom distribution of Pseudomonas aeruginosa and Staphylococcus aureus in chronic wounds. J Clin Microbiol. 2009;47:4084–4089. doi: 10.1128/JCM.01395-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Frykberg RG, Banks J. Challenges in the treatment of chronic wounds. Adv Wound Care. 2015;4:560–582. doi: 10.1089/wound.2015.0635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Furr B, Jordan V. The pharmacology and clinical uses of tamoxifen. Pharmacol Ther. 1984;25:127–205. doi: 10.1016/0163-7258(84)90043-3. [DOI] [PubMed] [Google Scholar]
- 50.Gilliver SC, Ashworth JJ, Ashcroft GS. The hormonal regulation of cutaneous wound healing. Clin Dermatol. 2007;25(1):56–62. doi: 10.1016/j.clindermatol.2006.09.012. [DOI] [PubMed] [Google Scholar]
- 51.Gruber CJ, Tschugguel W, Schneeberger C, Huber JC. Production and actions of estrogens. N Engl J Med. 2002;346:340–352. doi: 10.1056/NEJMra000471. [DOI] [PubMed] [Google Scholar]
- 52.Guest JF, Ayoub N, McIlwraith T, Uchegbu I, Gerrish A, Weidlich D, et al. Health economic burden that wounds impose on the National Health Service in the UK. BMJ Open. 2015;5(12):e009283. doi: 10.1136/bmjopen-2015-009283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Gulshan S, McCruden A, Stimson W. Oestrogen receptors in macrophages. Scand J Immunol. 1990;31:691–697. doi: 10.1111/j.1365-3083.1990.tb02820.x. [DOI] [PubMed] [Google Scholar]
- 54.Guo Sa, DiPietro LA. Factors affecting wound healing. J Dental Res. 2010;89:219–229. doi: 10.1177/0022034509359125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Harding KG, Morris HL, Patel GK. Science, medicine and the future: Healing chronic wounds. BMJ. 2002;324(7330):160–163. doi: 10.1136/bmj.324.7330.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hardman M, Ashcroft GS. Estrogen, not intrinsic aging, is the major regulator of delayed human wound healing in the elderly. Genome Biol. 2008;9(5):R80. doi: 10.1186/gb-2008-9-5-r80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Hardman M, Waite A, Zeef L, Burow M, Nakayama T, Ashcroft GS. Macrophage migration inhibitory factor: A central regulator of wound healing. Am J Pathol. 2005;167:1561–1574. doi: 10.1016/S0002-9440(10)61241-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Hardman MJ, Emmerson E, Campbell L, Ashcroft GS. Selective estrogen receptor modulators accelerate cutaneous wound healing in ovariectomized female mice. Endocrinology. 2008;149:551–557. doi: 10.1210/en.2007-1042. [DOI] [PubMed] [Google Scholar]
- 59.Herrick S, Ashcroft G, Ireland G, Horan M, McCollum C, Ferguson M. Up-regulation of elastase in acute wounds of healthy aged humans and chronic venous leg ulcers are associated with matrix degradation. Lab Invest. 1997;77:281–288. [PubMed] [Google Scholar]
- 60.Hohn DC, MacKay RD, Halliday B, Hunt TK. Effect of O2 tension on microbicidal function of leukocytes in wounds and in vitro. Surg Forum. 1976;27(62):18–20. [PubMed] [Google Scholar]
- 61.Holt DR, Kirk SJ, Regan MC, Hurson M, Lindblad WJ, Barbul A. Effect of age on wound healing in healthy human beings. Surgery. 1992;112:293–298. [PubMed] [Google Scholar]
- 62.Horng HC, Chang WH, Yeh CC, Huang BS, Chang CP, Chen YJ, et al. Estrogen effects on wound healing. Int J Mol Sci. 2017;18(11):2325. doi: 10.3390/ijms18112325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Hu S-K, Mitcho YL, Rath NC. Effect of estradiol on interleukin 1 synthesis by macrophages. Int J Immunopharmacol. 1988;10:247–252. doi: 10.1016/0192-0561(88)90055-0. [DOI] [PubMed] [Google Scholar]
- 64.Iyer V, Klebba I, McCready J, Arendt LM, Betancur-Boissel M, Wu M-F, et al. Estrogen promotes ER-Negative tumor growth and angiogenesis through mobilization of bone marrow–derived monocytes. Cancer Res. 2012;72:2705–2713. doi: 10.1158/0008-5472.CAN-11-3287. [DOI] [PubMed] [Google Scholar]
- 65.Jensen EV, Jacobson HI. Fate of steroid estrogens in target tissues. In: Pincus G, Vollmer EP, editors. Biological activities of steroids in relation to cancer. New York: Academic Press; 1960. pp. 161–178. [Google Scholar]
- 66.Jordan VC. Tamoxifen (ICI46, 474) as a targeted therapy to treat and prevent breast cancer. Br J Pharmacol. 2006;147(S1):S269–SS76. doi: 10.1038/sj.bjp.0706399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Jordan VC, Phelps E, Lindgren JU. Effects of anti-estrogens on bone in castrated and intact female rats. Breast Cancer Res Treat. 1987;10(1):31–35. doi: 10.1007/BF01806132. [DOI] [PubMed] [Google Scholar]
- 68.Kedar R, Bourne TH, Collins W, Campbell S, Powles T, Ashley S, et al. Effects of tamoxifen on uterus and ovaries of postmenopausal women in a randomised breast cancer prevention trial. Lancet. 1994;343(8909):1318–1321. doi: 10.1016/s0140-6736(94)92466-x. [DOI] [PubMed] [Google Scholar]
- 69.Klinge CM. Estrogen receptor interaction with co-activators and co-repressors. Steroids. 2000;65:227–251. doi: 10.1016/s0039-128x(99)00107-5. [DOI] [PubMed] [Google Scholar]
- 70.Kondo T, Ishida Y. Molecular pathology of wound healing. Forensic Sci Int. 2010;203:93–98. doi: 10.1016/j.forsciint.2010.07.004. [DOI] [PubMed] [Google Scholar]
- 71.Kuiper GG, Carlsson B, Grandien K, Enmark E, Häggblad J, Nilsson S, et al. Comparison of the ligand binding specificity and transcript tissue distribution of estrogen receptors α and β. Endocrinology. 1997;138:863–870. doi: 10.1210/endo.138.3.4979. [DOI] [PubMed] [Google Scholar]
- 72.Kuiper GG, Shughrue PJ, Merchenthaler I, Gustafsson J-Å. The estrogen receptor β subtype: A novel mediator of estrogen action in neuroendocrine systems. Front Neuroendocrinol. 1998;19:253–286. doi: 10.1006/frne.1998.0170. [DOI] [PubMed] [Google Scholar]
- 73.Labrie F, Bélanger A, Luu-The V, Labrie C, Simard J, Cusan L, et al. DHEA and the intracrine formation of androgens and estrogens in peripheral target tissues: Its role during aging. Steroids. 1998;63:322–328. doi: 10.1016/s0039-128x(98)00007-5. [DOI] [PubMed] [Google Scholar]
- 74.Labrie F, Luu-The V, Lin S-X, Simard J, Labrie C. Role of 17β-hydroxysteroid dehydrogenases in sex steroid formation in peripheral intracrine tissues. Trends Endocrinol Metab. 2000;11:421–427. doi: 10.1016/s1043-2760(00)00342-8. [DOI] [PubMed] [Google Scholar]
- 75.Leblanc D, Schneider M, Angele P, Vollmer G, Docheva D. The effect of estrogen on tendon and ligament metabolism and function. J Steroid Biochem Mol Biol. 2017;172:106–116. doi: 10.1016/j.jsbmb.2017.06.008. [DOI] [PubMed] [Google Scholar]
- 76.Lee W-L, Cheng M-H, Tarng D-C, Yang W-C, Lee F-K, Wang P-H. The benefits of estrogen or selective estrogen receptor modulator on kidney and its related disease - chronic kidney disease - mineral and bone disorder: Osteoporosis. J Chin Med Assoc. 2013;76:365–371. doi: 10.1016/j.jcma.2013.03.010. [DOI] [PubMed] [Google Scholar]
- 77.Ley K, Laudanna C, Cybulsky MI, Nourshargh S. Getting to the site of inflammation: the leukocyte adhesion cascade updated. Nat Rev Immunol. 2007;7:678. doi: 10.1038/nri2156. [DOI] [PubMed] [Google Scholar]
- 78.Ling S, Dai A, Dilley RJ, Jones M, Simpson E, Komesaroff PA, et al. Endogenous estrogen deficiency reduces proliferation and enhances apoptosis-related death in vascular smooth muscle cells: insights from the aromatase-knockout mouse. Circulation. 2004;109:537–543. doi: 10.1161/01.CIR.0000109699.45186.30. [DOI] [PubMed] [Google Scholar]
- 79.Lorenz HP, Longaker MT. Wounds: Biology, pathology, and management. In: Norton JA, et al., editors. Surgery. NewYork: Springer; 2008. pp. 77–88. [Google Scholar]
- 80.Lundgren D. Influence of estrogen and progesterone on exudation, inflammatory cell migration and granulation tissue formation in preformed cavities. Scand J Plastic Reconstruct Surg. 1973;7(1):10–14. doi: 10.3109/02844317309072412. [DOI] [PubMed] [Google Scholar]
- 81.Magnusson U, Einarsson S. Effects of exogenous oestradiol on the number and functional capacity of circulating mononuclear and polymorphonuclear leukocytes in the sow. Vet Immunol Immunopathol. 1990;25:235–247. doi: 10.1016/0165-2427(90)90047-v. [DOI] [PubMed] [Google Scholar]
- 82.Margolis DJ, Bilker W, Knauss J, Baumgarten M, Strom BL. The incidence and prevalence of pressure ulcers among elderly patients in general medical practice. Ann Epidemiol. 2002;12:321–325. doi: 10.1016/s1047-2797(01)00255-1. [DOI] [PubMed] [Google Scholar]
- 83.Marini H, Polito F, Altavilla D, Irrera N, Minutoli L, Calo M, et al. Genistein aglycone improves skin repair in an incisional model of wound healing: a comparison with raloxifene and oestradiol in ovariectomized rats. Br J Pharmacol. 2010;160:1185–1194. doi: 10.1111/j.1476-5381.2010.00758.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Matthews J, Gustafsson J-Å. Estrogen signaling: A subtle balance between ERα and ERβ. Mol Intervent. 2003;3(5):281. doi: 10.1124/mi.3.5.281. [DOI] [PubMed] [Google Scholar]
- 85.McGowan JE, Barnes MW, Finland M. Bacteremia at Boston City Hospital: Occurrence and mortality during 12 selected years (1935-1972), with special reference to hospital-acquired cases. J Infect Dis. 1975;132:316–335. doi: 10.1093/infdis/132.3.316. [DOI] [PubMed] [Google Scholar]
- 86.Mendelsohn ME, Karas RH. The protective effects of estrogen on the cardiovascular system. N Engl J Med. 1999;340:1801–1811. doi: 10.1056/NEJM199906103402306. [DOI] [PubMed] [Google Scholar]
- 87.Midgley AC, Morris G, Phillips AO, Steadman R. 17β‐estradiol ameliorates age‐associated loss of fibroblast function by attenuating IFN‐γ/STAT 1‐dependent miR‐7 upregulation. Aging Cell. 2016;15:531–541. doi: 10.1111/acel.12462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Miller JG, Neil SM. Gender and cutaneous melanoma. Br J Dermatol. 1997;136:657–665. [PubMed] [Google Scholar]
- 89.Mills SJ, Ashworth JJ, Gilliver SC, Hardman MJ, Ashcroft GS. The sex steroid precursor DHEA accelerates cutaneous wound healing via the estrogen receptors. J Invest Dermatol. 2005;125:1053–1062. doi: 10.1111/j.0022-202X.2005.23926.x. [DOI] [PubMed] [Google Scholar]
- 90.Mirkin S, Pickar JH. Selective estrogen receptor modulators (SERMs): A review of clinical data. Maturitas. 2015;80:52–57. doi: 10.1016/j.maturitas.2014.10.010. [DOI] [PubMed] [Google Scholar]
- 91.Moraes AB, Haidar MA, Júnior JMS, Simões MJ, Baracat EC, Patriarca MT. The effects of topical isoflavones on postmenopausal skin: Double-blind and randomized clinical trial of efficacy. Eur J Obstet Gynecol Reprod Biol. 2009;146:188–192. doi: 10.1016/j.ejogrb.2009.04.007. [DOI] [PubMed] [Google Scholar]
- 92.Morales DE, McGowan KA, Grant DS, Maheshwari S, Bhartiya D, Cid MC, et al. Estrogen promotes angiogenic activity in human umbilical vein endothelial cells in vitro and in a murine model. Circulation. 1995;91:755–763. doi: 10.1161/01.cir.91.3.755. [DOI] [PubMed] [Google Scholar]
- 93.Morris C, Wakeling A. Fulvestrant ('Faslodex') - a new treatment option for patients progressing on prior endocrine therapy. Endocr Relat Cancer. 2002;9:267–276. doi: 10.1677/erc.0.0090267. [DOI] [PubMed] [Google Scholar]
- 94.Mosselman S, Polman J, Dijkema R. ERβ: Identification and characterization of a novel human estrogen receptor. FEBS Lett. 1996;392:49–53. doi: 10.1016/0014-5793(96)00782-x. [DOI] [PubMed] [Google Scholar]
- 95.Mosser DM, Edwards JP. Exploring the full spectrum of macrophage activation. Nat Rev Immunol. 2008;8:958-69. Erratum in: Nat Rev Immunol. 2010;10:460. doi: 10.1038/nri2448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Mukai K, Urai T, Asano K, Nakajima Y, Nakatani T. Evaluation of effects of topical estradiol benzoate application on cutaneous wound healing in ovariectomized female mice. PloS One. 2016;11(9):e0163560. doi: 10.1371/journal.pone.0163560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Mustoe T. Dermal ulcer healing: Advances in understanding. Euroconference on tissue repair and ulcer/woundhealing: molecular mechanisms, therapeutictargets and future directions. Paris, France, March 17 – 18, 2005; Paris: Institut Pasteur; 2005. [Google Scholar]
- 98.Nawata H, Tanaka S, Tanaka S, Takayanagi R, Sakai Y, Yanase T, et al. Aromatase in bone cell: Association with osteoporosis in postmenopausal women. J Steroid Biochem Mol Biol. 1995;53:165–174. doi: 10.1016/0960-0760(95)00031-t. [DOI] [PubMed] [Google Scholar]
- 99.Nelson LR, Bulun SE. Estrogen production and action. J Am Acad Dermatol. 2001;45:S116–SS24. doi: 10.1067/mjd.2001.117432. [DOI] [PubMed] [Google Scholar]
- 100.Newman SL, Henson JE, Henson PM. Phagocytosis of senescent neutrophils by human monocyte-derived macrophages and rabbit inflammatory macrophages. J Exp Med. 1982;156:430–442. doi: 10.1084/jem.156.2.430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Nuttall ME, Pendrak I, Emery JG, Nadeau DP, Fisher PW, Nicholson TA, et al. Antagonism of oestrogen action in human breast and endometrial cells in vitro: potential novel antitumour agents. Cancer Chemother Pharmacol. 2001;47:437–443. doi: 10.1007/s002800000259. [DOI] [PubMed] [Google Scholar]
- 102.Nyman S. Studies on the influence of estradiol and progesterone on granulation tissue. J Periodontal Res. 1971;6:5–24. [PubMed] [Google Scholar]
- 103.Paige LA, Christensen DJ, Grøn H, Norris JD, Gottlin EB, Padilla KM, et al. Estrogen receptor (ER) modulators each induce distinct conformational changes in ER α and ER β. Proc Natl Acad Sci U S A. 1999;96:3999–4004. doi: 10.1073/pnas.96.7.3999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Pallin B, Ahonen J, Zederfeldt B. Granulation tissue formation in oophorectomized rats treated with female sex hormones. II. Studies on the amount of collagen and on tensile strength. Acta Chir Scand. 1975;141:710–714. [PubMed] [Google Scholar]
- 105.Park W-C, Jordan VC. Selective estrogen receptor modulators (SERMS) and their roles in breast cancer prevention. Trends Mol Med. 2002;8(2):82–88. doi: 10.1016/s1471-4914(02)02282-7. [DOI] [PubMed] [Google Scholar]
- 106.Payne AH, Hales DB. Overview of steroidogenic enzymes in the pathway from cholesterol to active steroid hormones. Endocr Rev. 2004;25:947–970. doi: 10.1210/er.2003-0030. [DOI] [PubMed] [Google Scholar]
- 107.Pepe G, Braga D, Renzi TA, Villa A, Bolego C, D’Avila F, et al. Self-renewal and phenotypic conversion are the main physiological responses of macrophages to the endogenous estrogen surge. Sci Rep. 2017;7:44270. doi: 10.1038/srep44270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Pettersson K, Gustafsson J-Å. Role of estrogen receptor beta in estrogen action. Annu Rev Physiol. 2001;63:165–192. doi: 10.1146/annurev.physiol.63.1.165. [DOI] [PubMed] [Google Scholar]
- 109.Picard F, Deshaies Y, Lalonde J, Samson P, Labrie C, Bélanger A, et al. Effects of the estrogen antagonist EM-652. HCl on energy balance and lipid metabolism in ovariectomized rats. Int J Obesity. 2000;24(7):830. doi: 10.1038/sj.ijo.0801240. [DOI] [PubMed] [Google Scholar]
- 110.Pirila E, Ramamurthy N, Maisi P, McClain S, Kucine A, Wahlgren J, et al. Wound healing in ovariectomized rats effects of chemically modified tetracycline (CMT-8) and estrogen on matrix metalloproteinases-8,-13 and type I collagen expression. Curr Med Chem. 2001;8:281–294. doi: 10.2174/0929867013373552. [DOI] [PubMed] [Google Scholar]
- 111.Pottratz ST, Bellido T, Mocharla H, Crabb D, Manolagas SC. 17 beta-Estradiol inhibits expression of human interleukin-6 promoter-reporter constructs by a receptor-dependent mechanism. J Clin Invest. 1994;93:944–950. doi: 10.1172/JCI117100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Punnonen R, Vaajalahti P, Teisala K. Local oestriol treatment improves the structure of elastic fibers in the skin of postmenopausal women. Ann Chir Gynaecol Suppl. 1987;202:39–41. [PubMed] [Google Scholar]
- 113.Quirke VM. Tamoxifen from failed contraceptive pill to best-selling breast cancer medicine: a case-study in pharmaceutical innovation. Front Pharmacol. 2017;8:620. doi: 10.3389/fphar.2017.00620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Raja SK, Garcia MS, Isseroff RR. Wound re-epithelialization: Modulating keratinocyte migration in wound healing. Front Biosci. 2007;12(3):2849–2868. doi: 10.2741/2277. [DOI] [PubMed] [Google Scholar]
- 115.Ralston SH, Russell RGG, Gowen M. Estrogen inhibits release of tumor necrosis factor from peripheral blood mononuclear cells in postmenopausal women. J Bone Mineral Res. 1990;5:983–988. doi: 10.1002/jbmr.5650050912. [DOI] [PubMed] [Google Scholar]
- 116.Rattan SIS, Derventzi A. Altered cellular responsiveness during ageing. Bioessays. 1991;13:601–606. doi: 10.1002/bies.950131111. [DOI] [PubMed] [Google Scholar]
- 117.Rollerova E, Urbancikova M. Intracellular estrogen receptors, their characterization and function. Endocr Regul. 2000;34:203–218. [PubMed] [Google Scholar]
- 118.Rubanyi GM, Johns A, Kauser K. Effect of estrogen on endothelial function and angiogenesis. Vasc Pharmacol. 2002;38:89–98. doi: 10.1016/s0306-3623(02)00131-3. [DOI] [PubMed] [Google Scholar]
- 119.Sato T, Ito A, Mori Y, Yamashita K, Hayakawa T, Nagase H. Hormonal regulation of collagenolysis in uterine cervical fibroblasts. Modulation of synthesis of procollagenase, prostromelysin and tissue inhibitor of metalloproteinases (TIMP) by progesterone and oestradiol-17 β. Biochem J. 1991;275:645–650. doi: 10.1042/bj2750645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Sator P-G, Schmidt J, Sator M, Huber J, Hönigsmann H. The influence of hormone replacement therapy on skin ageing: a pilot study. Maturitas. 2001;39:43–55. doi: 10.1016/s0378-5122(00)00225-5. [DOI] [PubMed] [Google Scholar]
- 121.Sauerbronn A, Fonseca A, Bagnoli V, Saldiva P, Pinotti J. The effects of systemic hormonal replacement therapy on the skin of postmenopausal women. Int J Gynecol Obstet. 2000;68:35–41. doi: 10.1016/s0020-7292(99)00166-6. [DOI] [PubMed] [Google Scholar]
- 122.Savvas M, Bishop J, Laurent G, Watson N, Studd J. Type III collagen content in the skin of postmenopausal women receiving oestradiol and testosterone implants. Br J Obstet Gynaecol. 1993;100:154–156. doi: 10.1111/j.1471-0528.1993.tb15212.x. [DOI] [PubMed] [Google Scholar]
- 123.Schmidt JB, Binder M, Macheiner W, Kainz CH, Gitsch G, Bieglmayer C. Treatment of skin ageing symptoms in perimenopausal females with estrogen compounds. A pilot study. Maturitas. 1994;20:25–30. doi: 10.1016/0378-5122(94)90097-3. [DOI] [PubMed] [Google Scholar]
- 124.Schönfelder U, Abel M, Wiegand C, Klemm D, Elsner P, Hipler U-C. Influence of selected wound dressings on PMN elastase in chronic wound fluid and their antioxidative potential in vitro. Biomaterials. 2005;26:6664–6673. doi: 10.1016/j.biomaterials.2005.04.030. [DOI] [PubMed] [Google Scholar]
- 125.Sen CK, Roy S. Redox signals in wound healing. Biochim Biophys Acta. 2008;1780:1348–1361. doi: 10.1016/j.bbagen.2008.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Seppä H, Grotendorst G, Seppä S, Schiffmann E, Martin GR. Platelet-derived growth factor in chemotactic for fibroblasts. J Cell Biol. 1982;92:584–588. doi: 10.1083/jcb.92.2.584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Shah MG, Maibach HI. Estrogen and skin. Am J Clin Dermatol. 2001;2:143–150. doi: 10.2165/00128071-200102030-00003. [DOI] [PubMed] [Google Scholar]
- 128.Shaw LM, Messier JM, Mercurio AM. The activation dependent adhesion of macrophages to laminin involves cytoskeletal anchoring and phosphorylation of the alpha 6 beta 1 integrin. J Cell Biol. 1990;110:2167–2174. doi: 10.1083/jcb.110.6.2167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Simpson E. Role of aromatase in sex steroid action. J Mol Endocrinol. 2000;25:149–156. doi: 10.1677/jme.0.0250149. [DOI] [PubMed] [Google Scholar]
- 130.Singer AJ, Clark RA. Cutaneous wound healing. N Engl J Med. 1999;341:738–746. doi: 10.1056/NEJM199909023411006. [DOI] [PubMed] [Google Scholar]
- 131.Sjöstedt S. The effect of diethylstilbenediol on the healing of wounds in the human vagina. Acta Endocrinol. 1953;12:260–263. doi: 10.1530/acta.0.0120260. [DOI] [PubMed] [Google Scholar]
- 132.Sjövall A. The influence of oestrogen upon the healing of vaginal wounds in rats. Acta Obstet Gynecol Scand. 1947;27(1):1–10. doi: 10.3109/00016344709159873. [DOI] [PubMed] [Google Scholar]
- 133.Snyder RJ. Treatment of nonhealing ulcers with allografts. Clin Dermatol. 2005;23:388–395. doi: 10.1016/j.clindermatol.2004.07.020. [DOI] [PubMed] [Google Scholar]
- 134.Sproston NR, El Mohtadi M, Slevin M, Gilmore W, Ashworth JJ. The effect of C-reactive protein isoforms on nitric oxide production by U937 monocytes/macrophages. Front Immunol. 2018;9:1500. doi: 10.3389/fimmu.2018.01500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Stevenson S, Sharpe DT, Thornton MJ. Effects of oestrogen agonists on human dermal fibroblasts in an in vitro wounding assay. Exp Dermatol. 2009;18:988–990. doi: 10.1111/j.1600-0625.2009.00864.x. [DOI] [PubMed] [Google Scholar]
- 136.Stevenson S, Thornton J. Effect of estrogens on skin aging and the potential role of SERMs. Clin Interv Aging. 2007;2(3):283–297. doi: 10.2147/cia.s798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Stimson W. Oestrogen and human T lymphocytes: presence of specific receptors in the T‐suppressor/cytotoxic subset. Scand J Immunol. 1988;28:345–350. doi: 10.1111/j.1365-3083.1988.tb01459.x. [DOI] [PubMed] [Google Scholar]
- 138.Straub RH. The complex role of estrogens in inflammation. Endocr Rev. 2007;28:521–574. doi: 10.1210/er.2007-0001. [DOI] [PubMed] [Google Scholar]
- 139.Stumpf WE, Sar M, Joshi SG. Estrogen target cells in the skin. Experientia. 1974;30:196–198. doi: 10.1007/BF01927732. [DOI] [PubMed] [Google Scholar]
- 140.Suenaga R, Evans M, Mitamura K, Rider V, Abdou N. Peripheral blood T cells and monocytes and B cell lines derived from patients with lupus express estrogen receptor transcripts similar to those of normal cells. J Rheumatol. 1998;25:1305–1312. [PubMed] [Google Scholar]
- 141.Suenaga R, Mitamura K, Evans M, Abdou N. Binding affinity and quantity of estrogen receptor in peripheral blood monocytes of patients with systemic lupus erythematosus. Lupus. 1996;5:227–231. doi: 10.1177/096120339600500311. [DOI] [PubMed] [Google Scholar]
- 142.Sumino H, Ichikawa S, Kasama S, Takahashi T, Kumakura H, Takayama Y, et al. Effects of raloxifene and hormone replacement therapy on forearm skin elasticity in postmenopausal women. Maturitas. 2009;62:53–57. doi: 10.1016/j.maturitas.2008.10.005. [DOI] [PubMed] [Google Scholar]
- 143.Taylor JE, Laity PR, Hicks J, Wong SS, Norris K, Khunkamchoo P, et al. Extent of iron pick-up in deforoxamine-coupled polyurethane materials for therapy of chronic wounds. Biomaterials. 2005;26:6024–6033. doi: 10.1016/j.biomaterials.2005.03.015. [DOI] [PubMed] [Google Scholar]
- 144.Thomas DR. Age-related changes in wound healing. Drugs Aging. 2001;18:607–620. doi: 10.2165/00002512-200118080-00005. [DOI] [PubMed] [Google Scholar]
- 145.Thornton MJ. Estrogens and aging skin. Dermatoendocrinology. 2013;5(2):264–270. doi: 10.4161/derm.23872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Varila E, Rantala I, Oikarinen A, Risteli J, Reunala T, Oksanen H, et al. The effect of topical oestradiol on skin collagen of postmenopausal women. Br J Obstet Gynaecol. 1995;102:985–989. doi: 10.1111/j.1471-0528.1995.tb10906.x. [DOI] [PubMed] [Google Scholar]
- 147.Vaughan MB, Howard EW, Tomasek JJ. Transforming growth factor-β1 promotes the morphological and functional differentiation of the myofibroblast. Exp Cell Res. 2000;257:180–189. doi: 10.1006/excr.2000.4869. [DOI] [PubMed] [Google Scholar]
- 148.Vural P, Akgul C, Canbaz M. Effects of hormone replacement therapy on plasma pro-inflammatory and anti-inflammatory cytokines and some bone turnover markers in postmenopausal women. Pharmacol Res. 2006;54:298–302. doi: 10.1016/j.phrs.2006.06.006. [DOI] [PubMed] [Google Scholar]
- 149.Webb P, Nguyen P, Valentine C, Lopez GN, Kwok GR, McInerney E, et al. The estrogen receptor enhances AP-1 activity by two distinct mechanisms with different requirements for receptor transactivation functions. Mol Endocrinol. 1999;13:1672–1685. doi: 10.1210/mend.13.10.0357. [DOI] [PubMed] [Google Scholar]
- 150.Weinstock MA. Epidemiologic investigation of nonmelanoma skin cancer mortality: The Rhode Island Follow-Back Study. J Invest Dermatol. 1994;102(6):6S–9S. doi: 10.1111/1523-1747.ep12385735. [DOI] [PubMed] [Google Scholar]
- 151.Weusten J, Blankenstein MA, Gmelig-Meyling F, Schuurman H, Kater L, Thijssen J. Presence of oestrogen receptors in human blood mononuclear cells and thymocytes. Eur J Endocrinol. 1986;112:409–414. doi: 10.1530/acta.0.1120409. [DOI] [PubMed] [Google Scholar]
- 152.Weyrich AS, Zimmerman GA. Platelets: signaling cells in the immune continuum. Trends Immunol. 2004;25:489–495. doi: 10.1016/j.it.2004.07.003. [DOI] [PubMed] [Google Scholar]
- 153.Wichmann MW, Zellweger R, DeMaso CM, Ayala A, Chaudry IH. Enhanced immune responses in females, as opposed to decreased responses in males following haemorrhagic shock and resuscitation. Cytokine. 1996;8:853–863. doi: 10.1006/cyto.1996.0114. [DOI] [PubMed] [Google Scholar]
- 154.Wilkinson HN, Hardman MJ. The role of estrogen in cutaneous ageing and repair. Maturitas. 2017;103:60–64. doi: 10.1016/j.maturitas.2017.06.026. [DOI] [PubMed] [Google Scholar]
- 155.Wira CR, Rodriguez-Garcia M, Patel MV. The role of sex hormones in immune protection of the female reproductive tract. Nat Rev Immunol. 2015;15:217–230. doi: 10.1038/nri3819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Wysocki AB, Staiano-Coico L, Grinneill F. Wound fluid from chronic leg ulcers contains elevated levels of metalloproteinases MMP-2 and MMP-9. J Invest Dermatol. 1993;101(1):64–68. doi: 10.1111/1523-1747.ep12359590. [DOI] [PubMed] [Google Scholar]
- 157.Yamamoto E. Studies on sex-manipulation and production of cloned populations in hirame, Paralichthys olivaceus (Temminck et Schlegel) Aquaculture. 1999;173:235–246. [Google Scholar]
- 158.Zidan J, Keidar Z, Basher W, Israel O. Effects of tamoxifen on bone mineral density and metabolism in postmenopausal women with early-stage breast cancer. Med Oncol. 2004;21:117–121. doi: 10.1385/MO:21:2:117. [DOI] [PubMed] [Google Scholar]