Key Points
Question
What is the incidence of first transient ischemic attack (TIA) and how is TIA associated with subsequent stroke risk?
Findings
In this population-based cohort study from 1948-2017, the estimated crude TIA incidence was 1.19/1000 person-years, the risk of stroke was significantly greater after TIA compared with matched control participants who did not have a TIA (adjusted hazard ratio, 4.37), and the risk of stroke within 90 days after TIA was significantly lower in the most recent epoch from 2000-2017 compared with an earlier period from 1948-1985 (hazard ratio, 0.32).
Meaning
Among participants in the Framingham Heart Study from 1948-2017, TIA was associated with greater risk of subsequent stroke compared with matched control participants without TIA, and the risk of stroke after a TIA was lower in more recent periods.
Abstract
Importance
Accurate estimation of the association between transient ischemic attack (TIA) and risk of subsequent stroke can help to improve preventive efforts and limit the burden of stroke in the population.
Objective
To determine population-based incidence of TIA and the timing and long-term trends of stroke risk after TIA.
Design, Setting, and Participants
Retrospective cohort study (Framingham Heart Study) of prospectively collected data of 14 059 participants with no history of TIA or stroke at baseline, followed up from 1948-December 31, 2017. A sample of TIA-free participants was matched to participants with first incident TIA on age and sex (ratio, 5:1).
Exposures
Calendar time (TIA incidence calculation, time-trends analyses), TIA (matched longitudinal cohort).
Main Outcomes and Measures
The main outcomes were TIA incidence rates; proportion of stroke occurring after TIA in the short term (7, 30, and 90 days) vs the long term (>1-10 years); stroke after TIA vs stroke among matched control participants without TIA; and time trends of stroke risk at 90 days after TIA assessed in 3 epochs: 1954-1985, 1986-1999, and 2000-2017.
Results
Among 14 059 participants during 66 years of follow-up (366 209 person-years), 435 experienced TIA (229 women; mean age, 73.47 [SD, 11.48] years and 206 men; mean age, 70.10 [SD, 10.64] years) and were matched to 2175 control participants without TIA. The estimated incidence rate of TIA was 1.19/1000 person-years. Over a median of 8.86 years of follow-up after TIA, 130 participants (29.5%) had a stroke; 28 strokes (21.5%) occurred within 7 days, 40 (30.8%) occurred within 30 days, 51 (39.2%) occurred within 90 days, and 63 (48.5%) occurred more than 1 year after the index TIA; median time to stroke was 1.64 (interquartile range, 0.07-6.6) years. The age- and sex-adjusted cumulative 10-year hazard of incident stroke for patients with TIA (130 strokes among 435 cases) was 0.46 (95% CI, 0.39-0.55) and for matched control participants without TIA (165 strokes among 2175) was 0.09 (95% CI, 0.08-0.11); fully adjusted hazard ratio [HR], 4.37 (95% CI, 3.30-5.71; P < .001). Compared with the 90-day stroke risk after TIA in 1948-1985 (16.7%; 26 strokes among 155 patients with TIA), the risk between 1986-1999 was 11.1% (18 strokes among 162 patients) and between 2000-2017 was 5.9% (7 strokes among 118 patients). Compared with the first epoch, the HR for 90-day risk of stroke in the second epoch was 0.60 (95% CI, 0.33-1.12) and in the third epoch was 0.32 (95% CI, 0.14-0.75) (P = .005 for trend).
Conclusions and Relevance
In this population-based cohort study from 1948-2017, the estimated crude TIA incidence was 1.19/1000 person-years, the risk of stroke was significantly greater after TIA compared with matched control participants who did not have TIA, and the risk of stroke after TIA was significantly lower in the most recent epoch from 2000-2017 compared with an earlier period from 1948-1985.
This cohort study uses Framingham Heart Study (FHS) data to assess population-based incidence of transient ischemic attack (TIA), and the timing and long-term trends of stroke risk after TIA, among participants in the FHS Original, Offspring, and Third Generation cohorts from 1948 to 2017.
Introduction
Transient ischemic attack (TIA) is a major herald of impending stroke.1,2 Heightened awareness, identification of persons at high risk, and timely management can significantly mitigate this risk.3 As secondary prevention interventions have evolved including rapid and complete evaluation and commencement of appropriate preventive therapies, decrease in short- and long-term stroke risk after TIA over time is expected but has not been documented. While the elevated early risk of stroke after a TIA has been well-described,4,5 the long-term risk is incompletely characterized. Early stroke risk stratification schemes are widely used,6 but less is known regarding clinical and demographic factors that determine the long-term risk of stroke after TIA. In a large multicenter TIA registry study, it was found that the risk of stroke and cardiovascular events continues to rise steadily in the long term, suggesting that patients with TIA remain at high risk beyond the early phase.7 The study included patients evaluated in organized centers staffed by stroke specialists, which limits generalization of the findings to the general population that might not have ready access to specialized services and in whom the risk might be even higher.
This study used systematically gathered longitudinal data from Framingham Heart Study participants, with follow-up spanning more than 6 decades, to investigate the incidence of first TIA. The short- and long-term risk of stroke after first-ever TIA were assessed, and the clinical and demographic characteristics related to this risk were described. In addition, time trends in stroke risk after TIA were explored.
Methods
Written informed consent was obtained at each visit from study participants, and the study protocol was approved by the institutional review board of the Boston University School of Medicine.
The Framingham Heart Study is a longitudinal, population-based cohort study. The Original Cohort was enrolled in 1948 (5209 persons, aged 28-62 years). The Offspring Cohort was enrolled in 1971 (5124 persons, aged 5-70 years). The Third Generation Cohort (4095 persons, aged 19-74 years) began enrollment in 2002.
The cohorts are predominantly White, of European descent (≈99%). From a sociodemographic standpoint, the participants are considered middle-class and well-educated (≈70% high school graduate, ≈18% college degree). Detailed descriptions of the study have been published.8
The incidence cohort comprised participants from the Original, Offspring, and Third Generation cohorts who were free of stroke and TIA.
Cohort Surveillance and Follow-up Procedures
Original Cohort participants have been examined biennially since enrollment; Offspring Cohort participants are reexamined approximately every 4 years and Third Generation Cohort participants every 6 years.9,10 These scheduled in-person visits include, among other things, a detailed medical and family history with special emphasis on cerebrovascular and cardiac symptoms, cardiovascular-oriented physical examination, medications used, and a neurocognitive battery. For those who cannot attend the examination on the study premises, visits by study staff are conducted. In addition to scheduled in-person visits and self-reporting of symptoms by patients, family members, or primary care physicians, all participants are contacted annually for a structured health review (eMethods in the Supplement), including review of focal neurologic symptoms suggestive of stroke or TIA.11 Furthermore, the main local hospital in Framingham is surveyed daily for admissions of study participants.
Any concerning symptoms trigger a review by a neurologist with stroke expertise to adjudicate the nature of the symptoms. If the symptoms are suspicious for stroke or TIA, an in-person visit is conducted by a study neurologist, either on study premises or by visiting the participant at the hospital or rehabilitation facility. The visit includes a detailed history of the event, neurologic examination, and review of medical records, including brain and vascular imaging data. These event-triggered in-person visits are in addition to the scheduled in-person visits described above. Study staff collects all available information, including hospitalization notes and discharge summaries and imaging and laboratory data. Ultimately, all relevant information is brought before a panel including at least 2 neurologists with stroke expertise who adjudicate the TIA or stroke event and subtype.
Outcomes
Two primary outcomes of interest were TIA in the incidence cohort and stroke after TIA (or stroke after matching for control participants) in the matched longitudinal cohort analysis. For stroke after TIA we followed up patients for up to 10 years after TIA.
TIA Definition
TIA was defined as an episode of rapid-onset focal neurologic dysfunction attributed to focal cerebral ischemia, with resolution within 24 hours. Transient visual disturbances associated with retinal ischemia were defined as transient monocular blindness and considered TIAs. Isolated transient symptoms such as altered consciousness, syncope, dizziness, amnesia, confusion, vertigo, dysarthria, dysphagia, or diplopia were not considered TIAs unless associated with other symptoms of brainstem ischemia. Focal symptoms associated with migraines were also excluded. Participants with a clinical diagnosis of TIA who were later found to have evidence of cerebral infarct in appropriate vascular distribution on computed tomography or magnetic resonance imaging were considered to have had a TIA. We characterized the duration, symptoms (motor, sensory, speech, and visual), and probable location (ocular, hemispheric, or brainstem) of the TIA. Further details regarding TIA subtyping are provided in the eMethods in the Supplement.
Stroke Definition
Stroke was defined as an acute-onset focal neurologic deficit of vascular etiology, persisting for more than 24 hours. Events with global neurologic dysfunction such as stupor or coma in the case of brainstem ischemia or subarachnoid hemorrhage were also considered strokes after review of the ancillary data and adjudication in the review process. Both ischemic and hemorrhagic stroke subtypes were included. Stroke subtypes were categorized based on preestablished criteria that include clinical features, imaging studies, and other laboratory criteria; noninvasive vascular studies; cardiac evaluations for a source of embolus; and, when available, information from autopsy studies. Ischemic stroke was diagnosed if a focal neurologic deficit was documented and the imaging showed no hemorrhage, the imaging showed an ischemic infarct that correlated with the clinical deficit, or an ischemic infarct was documented at autopsy.
A stroke was classified as cardioembolic if a cardiac source of embolus was found. All other ischemic infarcts were historically classified as atherosclerotic brain infarctions. This broad category initially included large-artery infarcts, lacunar infarcts, and infarcts of unknown origin. With the evolution in stroke phenotyping, more subcategories have been added. For the purpose of this analysis we have made a further distinction between lacunar and nonlacunar atherosclerotic brain infarctions outlined in detail in the eMethods in the Supplement. Other defined etiologies (eg, fibromuscular dysplasia, arterial dissection) are classified separately.
Risk Factors Definition
The study spans 70 years, during which some of the cardiovascular risk factor definitions have changed; presence or absence of a cardiovascular risk factor is in accordance with the accepted definition at the time of data recording. Blood pressure was recorded in each visit and used as a continuous variable. Hypertension was defined as systolic blood pressure greater than 140 mm Hg or diastolic blood pressure greater than 90 mm Hg, or use of an antihypertensive medication.12 Age was used both as continuous variable and dichotomized as younger than 65 years and 65 years or older, and education status as with and without high school degree. We also recorded current smoking, diagnosis of diabetes, atrial fibrillation, and coronary heart disease as binary variables.
Statistical Analyses
Participants were followed up until they developed the first-ever TIA or were censored (at death or their latest study evaluation before December 2014). Follow-up for stroke after TIA was extended until December 31, 2017. We examined the annual age- and sex- specific incidence rates of TIA per 1000 person-years. We also used direct standardization to the overall age distribution to obtain age-adjusted 1-year incidence rates per 1000 person-years.
We used a nested matched longitudinal cohort study design to investigate the risk of subsequent stroke after the first TIA. The matched cohort design was used only to select control participants without TIA matched to each participant with TIA at the time of the TIA. Each participant with TIA was randomly assigned 5 age- and sex-matched controls who were alive, stroke-free, and TIA-free prior to the date of TIA in their assigned case participant.
We constructed Cox proportional-hazards regression models to examine the crude and adjusted risk of stroke after a first TIA. To compute hazard ratios (HRs), we constructed 3 models: model 1 was adjusted for age and sex; model 2 added education level; and model 3 added hypertension, diabetes, atrial fibrillation, coronary heart disease, and current smoking. Participants with missing data on any of these variables were excluded from the adjusted analyses. To assess the potential effect of excluding individuals with missing variables on estimated associations we present 2 additional iterations of model 3 excluding the variables that resulted in data missingness (diabetes and current smoking) as well as an iteration of model 2 on the modified sample that resulted from excluding participants with missing data. In addition, we provide age-, sex-, and confounders-adjusted cumulative hazards for participants with TIA and control participants without TIA separately. To test the proportionality assumption, we generated time-dependent covariates by creating interactions of the predictors and a function of survival time and included it in the model.
We performed stratified analyses within subgroups defined by the above-mentioned clinicodemographic variables as well as TIA characteristics. We used a series of Cox proportional hazards models adjusted for age and sex, including interaction terms.
We also present findings focused on the last epoch (2000-2017), which informs on contemporary conditions and helps to contextualize the findings.
We further performed bivariable exploratory comparisons within the participants who experienced a TIA, to establish factors associated with subsequent stroke risk over the entire follow-up period, and further stratified by timing of stroke at 7 days (0-7 vs >7), 30 days (0-30 vs >30), 90 days (0-90 vs >90), and 1 year (0-365 vs >365 days).
We analyzed trends in stroke incidence after TIA by epoch (1945-1985, 1986-1999, and 2000-2017), further stratified by stroke timing and adjusted for age and sex. The 1986 cutoff point was chosen to reflect changes in primary and secondary prevention practices, especially with regard to blood pressure control.13,14 The 2000 cutoff was chosen to reflect further changes in secondary prevention practices, especially the widespread use of statins and anticoagulants and introduction of non–vitamin K antagonists.
For each epoch, we reported 90-day, 1-year, 5-year, and 10-year HRs, which represent the incidence (hazards) of stroke during each epoch relative to incidence (hazards) during the first epoch, respectively. We estimated linear trends using the elapsed mean time.
We used a 2-sided α level of .05 for all tests. There was no adjustment for multiple comparisons, and study findings should be interpreted as exploratory; post hoc false discovery rate–adjusted P values remained unchanged (<.001). All statistical analyses were performed using SAS version 9.4 (SAS Institute Inc).
Results
Baseline Demographic and Risk Factor Characteristics, Clinical Characteristics, and Incidence of TIAs
The incidence cohort comprised 14 059 participants (5125 from the Original Cohort, 5070 from the Offspring Cohort, and 3864 from the Third Generation Cohort). None of the time-dependent covariates was found to be significant; therefore, the proportionality assumption holds.
Over 66 years of follow-up (366 209 person-years), 435 participants were identified with a first TIA (229 women; mean age, 73.47 [SD, 11.48] years and 206 men; mean age, 70.10 [SD, 10.64] years). The matched longitudinal cohort sample totaled 2610 participants (435 with TIA and 2175 without TIA) (1145 women; mean age, 72.87 [SD, 11.59] years and 1030 men; with mean age, 69.6 [SD, 10.67] years).
Baseline characteristics of participants with TIA and matched controls are reported in Table 1. Patients with TIA had significantly higher prevalence of hypertension, diabetes, atrial fibrillation, and coronary artery disease and smoking. With the exception of smoking, these differences remained statistically significant between participants with TIA and matched controls in the third epoch. Clinical characteristics of incident TIAs are summarized in eTable 1 in the Supplement. Weakness was the most frequent symptom, reported in 47% of participants, and 59% of participants reported 1 symptom. Eighty-one percent of TIAs were referable to the anterior circulation and 66% of participants had symptoms lasting less than 1 hour, with only 9% reporting symptoms lasting 12 or more hours.
Table 1. Baseline Characteristics of Participants With TIA and Control Participants Without TIA.
| Entire follow-up period (1948-2017) | Current epoch (2000-2017) | |||||||
|---|---|---|---|---|---|---|---|---|
| With TIA (n = 435)a | Without TIA (n = 2175) | Absolute difference (95% CI) | P value | With TIA (n = 118) | Without TIA (n = 590) | Absolute difference (95% CI) | P value | |
| Age, mean (SD), y | 71.9 (11.2) | 71.3 (11.3) | 0.55 (−0.61 to 1.71) | .35 | 73.2 (13.4) | 72.8 (13.3) | 0.39 (−2.25 to 3.03) | .77 |
| Sex, No. (%) | ||||||||
| Women | 229 (53) | 1145 (53) | 0.00 (−0.05 to 0.05) | >.99 | 65 (55) | 325 (55) | 0.00 (0.10 to 0.10) | >.99 |
| Men | 206 (47) | 1030 (47) | 0.00 (−0.05 to 0.05) | 53 (45) | 265 (45) | 0.00 (0.10 to 0.10) | ||
| Blood pressure, mean (SD), mm Hg | ||||||||
| Systolic | 144 (23) | 136 (21) | 7.17 (4.80 to 9.53)a | <.001 | 135 (21) | 130 (20) | 4.20 (0.22 to 8.19)a | .04 |
| Diastolic | 78 (13) | 77 (11) | 1.00 (0.29 to 2.29)a | .13 | 73 (11) | 73 (11) | 0.25 (−1.88 to 2.37)a | .82 |
| Hypertension treatment, No./total (%) | 198/422 (47) | 700/2075 (34) | 13.2 (8.0 to 18.4) | <.001 | 67/115 (58) | 248/584 (42) | 15.8 (5.9 to 25.6) | .002 |
| Stage I hypertension, No./total (%) | 315/430 (73) | 1223/2156 (57) | 16.5 (2.1 to 11.9) | <.001 | 76/117 (65) | 318/587 (54) | 10.8 (1.2 to 20.3) | .03 |
| Diabetes mellitus, No./total (%) | 59/346 (17) | 198/1729 (11) | 5.6 (1.4 to 9.8) | .004 | 27/101 (27) | 71/512 (14) | 12.8 (3.7 to 22.0) | .001 |
| Atrial fibrillation, No. (%) | 42 (10) | 115 (5) | 4.4 (1.4.32 to 7.3) | .001 | 19 (16) | 41 (7) | 9.1 (2.2 to 16.1) | .001 |
| Current smoking, No./total (%) | 100/409 (24) | 397/1994 (20) | 4.5 (0.2 to 9.0) | .04 | 16 (14) | 75/586 (13) | 0.8 (−7.5 to 6.0) | .82 |
| Coronary heart disease, No. (%) | 103 (24) | 330 (15) | 8.5 (4.2 to 12.8) | <.001 | 23 (19) | 71 (12) | 7.5 (−0.2 to 15.1) | .03 |
Abbreviation: TIA, transient ischemic attack.
For the continuous variables systolic and diastolic blood pressure, data are reported as absolute mean difference and corresponding 95% CI.
The crude and age- and sex-specific incidence of TIA are reported in Table 2. Overall crude incidence rate was 1.19/1000 person-years and increased with age; incidence in the age group 85 to 94 years was 4.88/1000 person-years, while for participants in the age group 45 to 54 years it was 0.22/1000 person-years. In the most recent epoch (2000-2014), the incidence rate was 1.29/1000 person-years (Table 2).
Table 2. Annual Age- and Sex-Specific Incidence Rates of Transient Ischemic Attack.
| Incidence | No./person-years (rate per 1000 person-years) | |||||
|---|---|---|---|---|---|---|
| Entire follow-up period (1948-2017) | Current epoch (2000-2017) | |||||
| Women | Men | Women and men combined | Women | Men | Women and men combined | |
| Crude | 229/204 983 (1.12) | 206/161 455 (1.28) | 435/366 209 (1.19) | 65/50 739 (1.28) | 53/40 692 (1.30) | 118/91 313 (1.29) |
| Age-standardized rate | 1.04 | 1.41 | NA | 1.21 | 1.39 | NA |
| By age group, y | ||||||
| 35-44 | 2/33 393 (0.06) | 5/28 504 (0.18) | 7/61 897 (0.11) | 1/7525 (0.13) | 4/6395 (0.63) | 5/13 920 (0.36) |
| 45-54 | 12/50 188 (0.24) | 8/43 218 (0.19) | 20/93 406 (0.22) | 5/10 973 (0.46) | 1/9478 (0.11) | 6/20 451 (0.29) |
| 55-64 | 33/51 364 (0.64) | 49/42 818 (1.14) | 82/94 182 (0.87) | 9/12 376 (0.73) | 8/10 039 (0.80) | 17/22 415 (0.76) |
| 65-74 | 66/38 972 (1.69) | 66/29 729 (2.22) | 132/68 701 (1.92) | 12/10 106 (1.19) | 13/8387 (1.55) | 25/18 493 (1.35) |
| 75-84 | 74/22 910 (3.23) | 64/14 070 (4.55) | 138/36 980 (3.73) | 19/6423 (2.96) | 18/4747 (3.79) | 37/11 170 (3.31) |
| 85-94 | 42/8158 (5.15) | 14/3322 (4.21) | 56/11 480 (4.88) | 19/33 376 (5.69) | 9/1647 (5.46) | 28/4983 (5.62) |
Stroke Risk After TIA
The etiologic classification and timing of subsequent strokes are summarized in eTable 2 and the eFigure in the Supplement. No participant was lost to follow-up. Over a median of 8.86 (interquartile range [IQR], 3.98-10.00) years of follow-up, 130 participants (29.8%) experienced a stroke; of those strokes, 121 were ischemic. Eighty-nine (68.5% of all ischemic strokes) were classified as nonlacunar atherosclerotic infarctions and ischemic strokes of unknown etiology and 20 (15.4% of all ischemic strokes) as cardioembolic. Among the 130 participants who had a stroke, 28 strokes (21.5%) occurred within 7 days; 40 (30.8%) occurred within 30 days; 51 (39.2%) occurred within 90 days; and 63 (48.5%) occurred more than 1 year after the index TIA (eFigure in the Supplement). Median time to stroke was 601 (IQR, 24-2414) days (1.64 [IQR, 0.07-6.6] years).
Factors Associated With Subsequent Stroke Within TIA Cases
Comparisons of baseline demographics and clinical characteristics between patients with TIA and subsequent stroke vs patients with TIA but without a stroke on 7 and 90 days are presented in eTables 3A and 3B in the Supplement. Stroke risk was mainly associated with hypertension (odds ratio for 7-day stroke, 5.83 [95% CI, 1.35-25.11]). A statistically significant linear association between both systolic and diastolic blood pressure was noted for both early and late risk of stroke. With regard to TIA features, only presence of language symptoms was significantly associated with early stroke risk after TIA (odds ratio, 2.74 [95% CI, 1.21-6.21]).
Stroke Risk After TIA
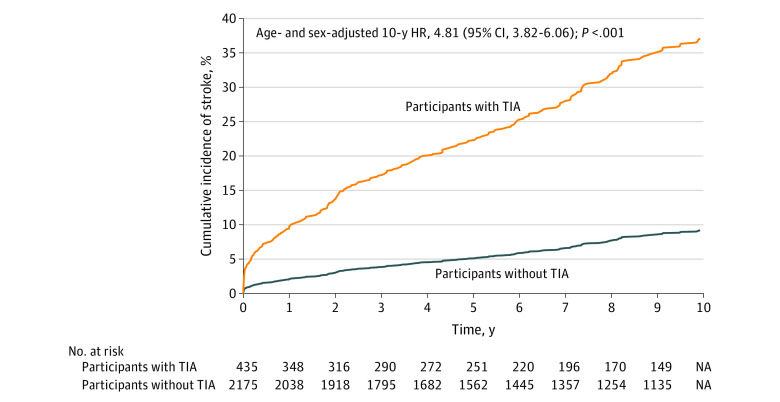
There were 130 stroke events after TIA among 435 participants with TIA compared with 165 strokes among 2175 matched control participants without TIA (age- and sex-adjusted HR, 4.81 [95% CI, 3.82-6.06]; P < .001) (Table 3). The age- and sex-adjusted cumulative 10-year hazard was 0.46 (95% CI, 0.39-0.55) in cases and 0.09 (95% CI, 0.08-0.11) in controls. A significant association between TIA and subsequent stroke was observed in fully adjusted models taking into account common stroke risk factors, with an HR for up to 10 years of follow-up (median, 8.86 years) of 4.37 (95% CI, 3.31-5.78); P < .001) (Table 3). The adjusted 5-year HR was 6.24 (95% CI, 4.44-8.75) (eTable 4 in the Supplement). These associations were unaltered in analyses limited to the last epoch (2000-2017) (eTable 5 in the Supplement): the adjusted HR of stroke was 4.67 (95% CI, 2.49-8.76; P < .001). Iterations of the adjusted models without adjustments for the variables with high rates of data missingness yield similar results (Table 3; eTable 6 in the Supplement): the adjusted HR without adjustment for diabetes was 4.50 (95% CI, 3.52-5.75; P < .001). Stroke incidence in participants with TIA was higher over time, diverging from stroke risk in participants without TIA throughout the entire follow-up period (Figure).
Table 3. 10-Year Hazard Ratio of Stroke in Participants With Transient Ischemic Attack Compared With Control Participants Without TIA (Entire Follow-up Period [1948-2017])a.
| Model adjustments | With TIA | Without TIA | With TIA absolute [cumulative] hazard (95% CI) | Without TIA absolute [cumulative] hazard (95% CI) | HR (95% CI) | P value | |||
|---|---|---|---|---|---|---|---|---|---|
| Cases, stroke/No. | Person-years of follow up | Controls, stroke/No. | Person-years of follow up | ||||||
| Crude risk | None | 130/435 | 2480 | 165/2175 | 15 781 | 0.48 (0.40-0.57) | 0.10 (0.08-0.11) | 4.84 (3.84-6.09) | <.001 |
| Model 1 | Age and sex | 130/435 | 2480 | 165/2175 | 15 781 | 0.46 (0.39-0.55) | 0.09 (0.08-0.11) | 4.81 (3.82-6.06) | <.001 |
| Model 2 | Model 1 + education | 128/425 | 2411 | 160/2079 | 15 167 | 0.46 (0.39-0.56) | 0.10 (0.08-0.11) | 4.88 (3.86-6.16) | <.001 |
| Model 3 | Model 2 + stroke risk factorsb,c | 95/319 | 1886 | 113/1513 | 11 307 | 0.40 (0.32-0.50) | 0.09 (0.08-0.11) | 4.37 (3.31-5.78) | <.001 |
| Model 3a | Model 2 + risk factorsd | 122/396 | 2226 | 145/1898 | 13 858 | 0.40 (0.33-0.50) | 0.09 (0.08-0.11) | 4.50 (3.52-5.75) | <.001 |
Abbreviation: HR, hazard ratio.
Over median 8.86 (interquartile range, 3.98-10.00) years of follow-up.
Stroke risk factors included hypertension, diabetes, atrial fibrillation, coronary heart disease, current smoking.
Participants with missing data on stroke risk factors have been excluded from this model.
This iteration of model 3 stroke risk factors includes hypertension, atrial fibrillation, coronary heart disease, and current smoking. Diabetes has been excluded because of high rate of missingness.
Figure. Kaplan-Meier Curves of 10-Year Cumulative Incidence of Stroke in Patients With TIA vs Matched Control Participants Without TIA.
Median follow-up for participants with transient ischemic attack (TIA), 8.63 (interquartile range, 8.22-8.86) years; for control participants without TIA, 8.50 (interquartile range, 8.22-8.72) years. NA indicates not available.
Prespecified subgroup analyses are presented in eTable 7 in the Supplement. A significant interaction was found with age, driven by a significantly higher HR in participants younger than 65 years (13.1 [95% CI, 6.94-24.73] vs 4.38 [95% CI, 3.37-5.70] for those ≥65 years; P = .002 for interaction); significant interactions were also found with atrial fibrillation and coronary heart disease. There was no significant difference in stroke risk between participants with TIA and those without TIA in the subgroup of participants with atrial fibrillation (HR, 1.16 [95% CI, 0.53-2.54] vs 6.05 [95% CI, 4.70-7.78] in those without atrial fibrillation; P < .001 for interaction) and coronary heart disease (HR, 3.18 [95% CI, 1.95-5.17] vs 5.87 [95% CI, 4.47-7.71] in those without coronary heart disease; P = .02 for interaction).
Trend in Stroke Risk After TIA
Temporal trends in stroke risk after TIA are summarized in Table 4. There was a significant decrease in both short- and long-term stroke risk across the 3 epochs. Compared with the first epoch, the HR for 90-day risk of stroke in the second epoch was 0.60 (95% CI, 0.33-1.12) and in the third epoch was 0.32 (95% CI, 0.14-0.75) (P = .005 for trend). Similarly lower risk was observed for 1-, 5-, and 10-year risks of stroke (Table 4).
Table 4. Temporal Trends of Stroke After Transient Ischemic Attack.
| Time horizon for stroke risk | Total No. of events | Epoch 1 (1948-1985) | Epoch 2 (1986-1999) | Epoch 3 (2000-2017) | P value for trend |
|---|---|---|---|---|---|
| 90 d | |||||
| No. of events, No./total | 51/435 | 26/155 | 18/162 | 7/118 | |
| Proportion of cases with subsequent stroke, % | 11.7 | 16.7 | 11.1 | 5.9 | |
| Hazard ratio (95% CI)a,b | 1 [Reference] | 0.60 (0.33-1.12) | 0.32 (0.14-0.75) | .005 | |
| 1 y | |||||
| No. of events, No./total | 67/435 | 37/155 | 21/162 | 9/118 | |
| Proportion of cases with subsequent stroke, % | 15.4 | 23.9 | 12.9 | 7.6 | |
| Hazard ratio (95% CI)a,b | 1 [Reference] | 0.49 (0.28-0.84) | 0.29 (0.14-0.60) | <.001 | |
| 5 y | |||||
| No. of events, No./total | 107/435 | 55/155 | 33/162 | 19/118 | |
| Proportion of cases with subsequent stroke, % | 24.6 | 35.5 | 20.4 | 16.1 | |
| Hazard ratio (95% CI)a,b | 1 [Reference] | 0.48 (0.31-0.74) | 0.37 (0.22-0.63) | <.001 | |
| 10 y | |||||
| No. of events, No./total | 130/435 | 64/155 | 42/162 | 24/118 | |
| Proportion of cases with subsequent stroke, % | 29.9 | 41.3 | 25.9 | 20.3 | |
| Duration of follow up, median (range)c | 6.49 (0.74-10) | 6.85 (1.88-10) | 5.39 (2.19-8.62) | ||
| Hazard ratio (95% CI)a,b | 1 [Reference] | 0.52 (0.35-0.78) | 0.43 (0.27-0.69) | <.001 |
Each row represents a separate Cox regression analysis with a different time horizon; hence, the number at risk (n = 435) is the same in all analyses.
Age- and sex-adjusted.
Only median duration of follow-up for the 10-year time horizon is reported. In all other time strata (90 days, 1 year, 5 years), all participants have complete follow-up and the median follow-up time coincides with the maximum duration of these time windows.
Discussion
In this population-based cohort study from 1948-2017, the estimated crude TIA incidence was 1.19/1000 person-years and remained unchanged in the most recent epoch after 2000. The risk of stroke was significantly greater after TIA compared with risk among matched participants who did not have TIA, and this association did not change in contemporary analyses focused on the years after 2000 only. However, the short- and long-term risk of stroke after TIA was significantly lower in the most recent epoch from 2000-2017, compared with an earlier period from 1948-1985.
The observed TIA incidence rate was higher than rates in previously reported population-based cohorts, ranging from 0.42/100 person-years to 0.83/1000 person-years2,15,16; there was no significant difference in a focused analysis of the most recent epoch after 2000. A more recent population study in Sweden also provided a lower estimate,17 although the estimated incidence rate in a recent population-based study in the US was comparable to that observed in the current study.18 Given the rigorous diagnostic approach for TIA in the study, it is unlikely that TIA mimics accounted for this observation. TIAs tend to be poorly recognized19 and prone to underreporting by patients20 and are often diagnosed in retrospect only if followed by a stroke. A National Stroke Association–sponsored survey conducted in 2000 estimated that about 1.2 million US residents older than 45 years experienced 1 or more symptoms of TIA, and most likely experienced a TIA without realizing it.21 Therefore, this study’s mode of active surveillance is advantageous, ensuring capture of more TIAs than a passive surveillance mode. This study spanned more than 6 decades of follow-up, during which advances in cardiovascular risk prevention have decreased the risk of cerebrovascular disease, likely including TIAs, and it is possible that the calculation including participants from past decades is mildly inflated. However, analysis of the most contemporary era after the year 2000 did not show a notable difference in the incidence rate. Taking all of the above competing factors into account, it is likely that this study’s estimation is a relatively accurate representation of contemporary TIA incidence in the general population.
The rate of subsequent stroke in the studied cohort was high; 30% of participants with TIA experienced a stroke over a median of 8.9 years of follow-up. This rate is higher than those from previously reported TIA cohorts with long-term follow-up, ranging from 6% after 1 year of follow-up22 to 9% in 5 years of follow-up.7 Active surveillance monitoring methods used in this study may account for this difference to some extent. However, access to specialized care and advances in secondary preventive practices are more likely contributors. The present cohort is community-based, and it cannot be ensured that all participants had access to specialists and received optimal secondary preventive care. In contrast, a recent large longitudinal TIA registry recruited patients from specialized centers and clinics with access to vascular neurologists and generally receiving a comprehensive stroke workup and preventive care.7,22 In addition, this very high risk does not reflect the substantial decreases in both short- and long-term stroke risk after TIA over time, despite the overall population aging: 1- and 5-year risks of post TIA stroke in the 2000-2017 era are 7.6% and 16.1%, respectively, considerably lower than the respective cumulative risks over the entire observation period and closer to modern era estimates. These decreases most likely reflect the effectiveness of secondary prevention interventions such as stricter blood pressure control and administration of antithrombotic medications; a recent study in Australia23 documented a similar trend in the first decade of 2000.
Despite advances in secondary prevention, stroke risk after TIA remains higher compared with risk among TIA-free participants, even after accounting for confounding cardiovascular risk factors; the risk remained generally unchanged across most subgroups. Although early stroke risk is often highlighted,4,6 the subsequent stroke incidence continued to increase and diverge from that of TIA-free participants over the entire follow-up period in this study; 49% of strokes occurred more than 12 months from the index TIA, a finding in line with recent large longitudinal studies with similarly long follow-up periods, despite general adherence to prescribed preventive practices.7 With the exception of higher blood pressure and language symptoms on presentation, none of the traditionally recognized prognostic factors of higher early stroke risk6,24 were associated with subsequent early or delayed stroke. Taken together, these findings suggest that patients with TIA represent a particularly high-risk group in need of vigorous surveillance beyond the early, high-risk period and with special attention to hypertension monitoring and treatment.
The study has several strengths. To our knowledge, it has a longer observation period than any other TIA incidence study. The long median follow-up period exceeding 5 years allowed characterization of the natural history of post-TIA stroke in both its early and delayed phases. The current study included a cohort of matched control participants who provide a comparator group highlighting the importance of TIA as a herald of future stroke. The cohort is phenotyped in detail, with more than 98% retention and follow-up of participants ensuring data completeness. Longitudinal follow-up, active surveillance methods, and the rigor of case ascertainment have already been discussed in detail.
Limitations
This study has several limitations. First, the analyzed cohort included a population of overwhelmingly White European ancestry. It is likely that the TIA incidence rates found in predominantly White populations are underestimates of the TIA incidence in the US population, as it has been demonstrated that Black and Mexican American individuals have higher incidence rates than non-Hispanic White individuals2,25; a similar pattern is true for risk of stroke after TIA.
Second, there are limitations inherent to the nature of the main end point of interest (TIA), which is prone to recall and misclassification bias. However, the study design, surveillance, and case ascertainment methods mitigate many of these shortcomings to the degree that is practically feasible in the context of an epidemiologic study.
Third, information on medical and surgical treatments after TIA is incomplete, and their effect could not be accounted for. Although it could be assumed that participants received the standard of care for secondary prevention, it is impossible to adjudicate individual physician prescription practices or participant adherence to medical care and their association with subsequent stroke risk.
Fourth, the current study used the classic, time-based definition of TIA (symptoms lasting <24 hours) to maintain uniform consistency of case ascertainment across all study epochs. Under the newer, recently introduced tissue-and-time definition of TIA (symptoms lasting less than 24 hours and not associated with new visible infarction), some of the TIA cases would now be classified as transient symptoms associated with infarction.26,27Accordingly, in practice settings where availability of magnetic resonance imaging permits use of the modern tissue definition, the current study delineates changes in incidence of the composite of TIAs and transient symptoms associated with infarction.
Fifth, risk factors at pre-TIA baseline were used, several of which are very likely to have changed in the interval between baseline assessment and the event of interest. This did not allow examination of performance of stratification schemes for stroke risk after TIA that use certain values obtained at the time of presentation.
Conclusions
In this population-based cohort study from 1948-2017, the estimated crude TIA incidence was 1.19/1000 person-years, the risk of stroke was significantly greater after TIA compared with matched control participants who did not have TIA, and the risk of stroke after TIA was significantly lower in the most recent epoch from 2000-2017 compared with an earlier period from 1948-1985.
eMethods. Definition of Assumed TIA Localization and Definition of Stroke
eTable 1. Clinical Characteristics of Transient Ischemic Attacks (TIAs)
eTable 2. Etiologic Classification of Strokes Post-TIA
eTable 3a. Comparison of Risk Factors and TIA Characteristics Between TIA Cases With Early Stroke vs Not (0-7 Days)
eTable 3b. Comparison of Risk Factors and TIA Characteristics Between TIA Cases With Early Stroke vs Not (0-90 Days)
eTable 4. 5-Year Hazard Ratio of Stroke in Subjects With TIA as Compared to Controls
eTable 5. 10-Year Hazard Ratio of Stroke in Subjects With TIA as Compared to Controls for the Last Epoch 2000-2017
eTable 6. 10-Year Hazard Ratio of Stroke in Subjects With TIA as Compared to Controls, Alternative Models Excluding Variables With High Rates of Data Missingness
eTable 7. Hazard Ratio of Stroke in Subjects With TIA as Compared to Controls Within Predefined Subgroups
eFigure. Time to Stroke After TIA
References
- 1.Dennis M, Bamford J, Sandercock P, Warlow C. Prognosis of transient ischemic attacks in the Oxfordshire Community Stroke Project. Stroke. 1990;21(6):848-853. doi: 10.1161/01.STR.21.6.848 [DOI] [PubMed] [Google Scholar]
- 2.Kleindorfer D, Panagos P, Pancioli A, et al. . Incidence and short-term prognosis of transient ischemic attack in a population-based study. Stroke. 2005;36(4):720-723. doi: 10.1161/01.STR.0000158917.59233.b7 [DOI] [PubMed] [Google Scholar]
- 3.Johnston SC, Easton JD, Farrant M, et al. ; Clinical Research Collaboration, Neurological Emergencies Treatment Trials Network, and the POINT Investigators . Clopidogrel and aspirin in acute ischemic stroke and high-risk TIA. N Engl J Med. 2018;379(3):215-225. doi: 10.1056/NEJMoa1800410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Johnston SC, Gress DR, Browner WS, Sidney S. Short-term prognosis after emergency department diagnosis of TIA. JAMA. 2000;284(22):2901-2906. doi: 10.1001/jama.284.22.2901 [DOI] [PubMed] [Google Scholar]
- 5.Hill MD, Yiannakoulias N, Jeerakathil T, Tu JV, Svenson LW, Schopflocher DP. The high risk of stroke immediately after transient ischemic attack: a population-based study. Neurology. 2004;62(11):2015-2020. doi: 10.1212/01.WNL.0000129482.70315.2F [DOI] [PubMed] [Google Scholar]
- 6.Johnston SC, Rothwell PM, Nguyen-Huynh MN, et al. . Validation and refinement of scores to predict very early stroke risk after transient ischaemic attack. Lancet. 2007;369(9558):283-292. doi: 10.1016/S0140-6736(07)60150-0 [DOI] [PubMed] [Google Scholar]
- 7.Amarenco P, Lavallée PC, Monteiro Tavares L, et al. ; TIAregistry.org Investigators . Five-year risk of stroke after TIA or minor ischemic stroke. N Engl J Med. 2018;378(23):2182-2190. doi: 10.1056/NEJMoa1802712 [DOI] [PubMed] [Google Scholar]
- 8.Tsao CW, Vasan RS. Cohort profile: the Framingham Heart Study (FHS): overview of milestones in cardiovascular epidemiology. Int J Epidemiol. 2015;44(6):1800-1813. doi: 10.1093/ije/dyv337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kannel WB, Feinleib M, McNamara PM, Garrison RJ, Castelli WP. An investigation of coronary heart disease in families: the Framingham Offspring Study. Am J Epidemiol. 1979;110(3):281-290. doi: 10.1093/oxfordjournals.aje.a112813 [DOI] [PubMed] [Google Scholar]
- 10.An investigation of coronary heart disease in families: the Framingham Offspring Study. Am J Epidemiol. 2017;185(11):1093-1102. doi: 10.1093/aje/kwx110 [DOI] [PubMed] [Google Scholar]
- 11.Andersson C, Johnson AD, Benjamin EJ, Levy D, Vasan RS. 70-year legacy of the Framingham Heart Study. Nat Rev Cardiol. 2019;16(11):687-698. doi: 10.1038/s41569-019-0202-5 [DOI] [PubMed] [Google Scholar]
- 12.The fifth report of the Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure (JNC V). Arch Intern Med. 1993;153(2):154-183. doi: 10.1001/archinte.1993.00410020010002 [DOI] [PubMed] [Google Scholar]
- 13.IPPPSH Collaborative Group Cardiovascular risk and risk factors in a randomized trial of treatment based on the beta-blocker oxprenolol: the International Prospective Primary Prevention Study in Hypertension (IPPPSH). J Hypertens. 1985;3(4):379-392. doi: 10.1097/00004872-198508000-00011 [DOI] [PubMed] [Google Scholar]
- 14.Medical Research Council Working Party MRC trial of treatment of mild hypertension: principal results. Br Med J (Clin Res Ed). 1985;291(6488):97-104. doi: 10.1136/bmj.291.6488.97 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dennis MS, Bamford JM, Sandercock PA, Warlow CP. Incidence of transient ischemic attacks in Oxfordshire, England. Stroke. 1989;20(3):333-339. doi: 10.1161/01.STR.20.3.333 [DOI] [PubMed] [Google Scholar]
- 16.Brown RD Jr, Petty GW, O’Fallon WM, Wiebers DO, Whisnant JP. Incidence of transient ischemic attack in Rochester, Minnesota, 1985-1989. Stroke. 1998;29(10):2109-2113. doi: 10.1161/01.STR.29.10.2109 [DOI] [PubMed] [Google Scholar]
- 17.Tavosian A, Ström JO, Appelros P. Incidence of transient ischemic attacks in Sweden. Neuroepidemiology. 2016;47(1):20-25. doi: 10.1159/000447240 [DOI] [PubMed] [Google Scholar]
- 18.Madsen TE, Khoury JC, Alwell K, et al. . Temporal trends of sex differences in transient ischemic attack incidence within a population. J Stroke Cerebrovasc Dis. 2019;28(9):2468-2474. doi: 10.1016/j.jstrokecerebrovasdis.2019.06.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Howard VJ, McClure LA, Meschia JF, Pulley L, Orr SC, Friday GH. High prevalence of stroke symptoms among persons without a diagnosis of stroke or transient ischemic attack in a general population: the REasons for Geographic And Racial Differences in Stroke (REGARDS) study. Arch Intern Med. 2006;166(18):1952-1958. doi: 10.1001/archinte.166.18.1952 [DOI] [PubMed] [Google Scholar]
- 20.Chandratheva A, Lasserson DS, Geraghty OC, Rothwell PM; Oxford Vascular Study . Population-based study of behavior immediately after transient ischemic attack and minor stroke in 1000 consecutive patients: lessons for public education. Stroke. 2010;41(6):1108-1114. doi: 10.1161/STROKEAHA.109.576611 [DOI] [PubMed] [Google Scholar]
- 21.TIA/Mini Strokes: Public Knowledge and Experience—Roper Starch Worldwide Survey. National Stroke Association, 2000. [Google Scholar]
- 22.Amarenco P, Lavallée PC, Labreuche J, et al. ; TIAregistry.org Investigators . One-year risk of stroke after transient ischemic attack or minor stroke. N Engl J Med. 2016;374(16):1533-1542. doi: 10.1056/NEJMoa1412981 [DOI] [PubMed] [Google Scholar]
- 23.Sundararajan V, Thrift AG, Phan TG, Choi PM, Clissold B, Srikanth VK. Trends over time in the risk of stroke after an incident transient ischemic attack. Stroke. 2014;45(11):3214-3218. doi: 10.1161/STROKEAHA.114.006575 [DOI] [PubMed] [Google Scholar]
- 24.Rothwell PM, Giles MF, Flossmann E, et al. . A simple score (ABCD) to identify individuals at high early risk of stroke after transient ischaemic attack. Lancet. 2005;366(9479):29-36. doi: 10.1016/S0140-6736(05)66702-5 [DOI] [PubMed] [Google Scholar]
- 25.Morgenstern LB, Smith MA, Lisabeth LD, et al. . Excess stroke in Mexican Americans compared with non-Hispanic Whites: the Brain Attack Surveillance in Corpus Christi Project. Am J Epidemiol. 2004;160(4):376-383. doi: 10.1093/aje/kwh225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Prabhakaran S, Chong JY, Sacco RL. Impact of abnormal diffusion-weighted imaging results on short-term outcome following transient ischemic attack. Arch Neurol. 2007;64(8):1105-1109. doi: 10.1001/archneur.64.8.1105 [DOI] [PubMed] [Google Scholar]
- 27.Arsava EM, Furie KL, Schwamm LH, Sorensen AG, Ay H. Prediction of early stroke risk in transient symptoms with infarction: relevance to the new tissue-based definition. Stroke. 2011;42(8):2186-2190. doi: 10.1161/STROKEAHA.110.604280 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMethods. Definition of Assumed TIA Localization and Definition of Stroke
eTable 1. Clinical Characteristics of Transient Ischemic Attacks (TIAs)
eTable 2. Etiologic Classification of Strokes Post-TIA
eTable 3a. Comparison of Risk Factors and TIA Characteristics Between TIA Cases With Early Stroke vs Not (0-7 Days)
eTable 3b. Comparison of Risk Factors and TIA Characteristics Between TIA Cases With Early Stroke vs Not (0-90 Days)
eTable 4. 5-Year Hazard Ratio of Stroke in Subjects With TIA as Compared to Controls
eTable 5. 10-Year Hazard Ratio of Stroke in Subjects With TIA as Compared to Controls for the Last Epoch 2000-2017
eTable 6. 10-Year Hazard Ratio of Stroke in Subjects With TIA as Compared to Controls, Alternative Models Excluding Variables With High Rates of Data Missingness
eTable 7. Hazard Ratio of Stroke in Subjects With TIA as Compared to Controls Within Predefined Subgroups
eFigure. Time to Stroke After TIA