Abstract
Purpose
This study aimed to examine the initial efficacy of a parent-assisted blended intervention combining components of Structured TEACCHing and Social Thinking, designed to increase social communication and self-regulation concept knowledge in 1st and 2nd graders (n = 17) diagnosed with autism spectrum disorder (ASD) and their parents.
Method
A randomized delayed treatment control group design with pre- and postintervention assessments of both parents and children was implemented within a community practice setting. Two follow-up assessments at 3 and 6 months postintervention were also completed.
Results
Overall, results indicate that the intervention is efficacious in teaching social communication and self-regulation concept knowledge to children with ASD and their parents. Both parents and children demonstrated an increase in social communication and self-regulation knowledge after participating in the Growing, Learning, and Living With Autism Group as compared to a delayed treatment control group. The effects of the intervention did not extend to parent–child interactions coded from video recordings. Child treatment effects were maintained at the 3- and 6-month follow-up assessments.
Conclusions
Preliminary efficacy of the Growing, Learning, and Living With Autism Group was established. Based on parent report at the conclusion of the intervention, this is a socially valid intervention for teaching social communication and self-regulation skills to school-age children with ASD.
Supplemental Material
In the United States, current prevalence rates of autism spectrum disorder (ASD) are reported between one in 40 and one in 59 children (Baio et al., 2018; Kogan et al., 2018). Nearly half of children with ASD have average to above average cognitive ability (Christensen, 2016); yet, their adult outcomes are poor when compared to peers with typical development (Dijkhuis, Ziermans, Van Rijn, Staal, & Swaab, 2016; Howlin, Moss, Savage, & Rutter, 2013) and peers with ASD who have below average cognitive ability (Mordre et al., 2012). Autism symptom severity, adaptive functioning, and exposure to early intervention are all more predictive of positive adult outcomes in ASD than cognitive ability alone (Anderson, Liang, & Lord, 2014; Gray et al., 2014). Though average to above average cognition increases the chances that an individual with ASD will be employed, these individuals are less likely to be involved in activities outside their homes than their peers with lower cognitive skills (Taylor & Seltzer, 2011). Social communication and self-regulation are skill areas in which individuals with ASD struggle. Social communication deficits have been shown to negatively affect academic performance (Welsh, Parke, Widaman, & O'Neil, 2001), be associated with psychiatric conditions like anxiety and depression (Barnhill, 2001), and affect friendship and employment outcomes in adulthood (Howlin et al., 2013). Self-regulation deficits, specifically emotion regulation and executive functioning difficulties, negatively impact engagement in academic and social settings for children (Jahromi, Bryce, & Swanson, 2013) and are correlated with self-reports of lower quality of life compared to non-ASD peers in young adulthood (Dijkhuis et al., 2016). Thus, there is a need for interventions targeting social communication and self-regulation in school-age children with ASD with average or above average cognitive skills with the long-term goal of improving adult quality of life outcomes.
Group interventions are common practice for targeting social communication goals in children with “high-functioning” ASD (i.e., those with average to above average cognitive abilities, including structural language skills in the average range, but varying levels of autism symptomatology), but evidence for the efficacy of these groups has been mixed (Rao, Beidel, & Murray, 2008). In 2010, Reichow and Volkmar completed a review of social skills group intervention studies for school-age children with ASD and concluded that social skills groups met criteria (based on Reichow, Volkmar, & Cicchetti, 2008) to be considered an evidence-based practice for ASD.
It has been argued that cognitive behavioral therapy approaches to teaching social communication skills, commonly referred to as social cognitive interventions, are more effective than behavioral approaches for children with high-functioning ASD because they teach social problem-solving skills that can be used to change behavior flexibly across contexts, rather than learning fixed social rules (Crooke, Winner, & Olswang, 2016). For instance, head nodding is a prosocial behavior that indicates that one is listening to a communication partner. However, it is socially appropriate to stop nodding and even look away from a communication partner if they talk for too long or say something with which one does not agree. A behavioral approach may simply reward the child for nodding while someone else is talking (note that this may be an appropriate approach for a child with less social communication competence), whereas a social cognitive approach that teaches why and how to use prosocial behaviors such as nodding may be best for a high-functioning child who is held to the same social standards as typically developing peers. Bauminger (2007) conducted a 7-month school-based social cognitive intervention with a group of children with high-functioning ASD. Though the intervention effectively improved the children's social cognition skills (i.e., ability to define and recognize emotions, social situations, and constructs; better understanding of others; and improved awareness of others), these effects did not generalize to peer interactions. A major limitation of this study was that it did not include a control group. In a randomized controlled trial of a social cognitive intervention in a clinic setting with children with high-functioning ASD, Lopata et al. (2010) found treatment effects on social skills knowledge and understanding of nonliteral language. Furthermore, parent report measures indicated an increase in social skills and a decrease is withdrawal behaviors. Thus, there seems to be preliminary evidence for social cognitive approaches to teaching social communication skills to school-age children with high-functioning ASD. Moreover, there are several evidence-based practices that are used consistently by clinicians during social cognitive interventions to improve social communication skills, including visual supports, modeling, reinforcement, scripting, social skills training, structured play groups, social narratives, and video modeling (Wong et al., 2015). A blend of these practices or key ingredients may be essential to the success of social cognitive interventions.
Interventions targeting self-regulation have been found to be efficacious for children with attention-deficit/hyperactivity disorder (Reid, Trout, & Schartz, 2005) and learning disabilities (Reid, 1996) and have shown emerging evidence for groups of children with ASD (e.g., Stoesz, Montgomery, & MacKenzie, 2013). Though both social communication and self-regulation are skill areas that predict outcomes for children with high-functioning ASD and interventions targeting these skills have a promising evidence base, we have identified no research on interventions addressing both of these skill areas in high-functioning school-age children. The purpose of this study is to examine the initial efficacy of an existing parent-assisted community intervention for school-age children with ASD that targets both self-regulation and social communication skills.
When establishing efficacy for an intervention program, it is important to remember that the extent to which participants are satisfied with their intervention experience has a significant impact on whether or not that intervention is adopted and implemented (Kazdin, 1977). Just because an intervention demonstrates efficacy on outcome measures does not mean that it is appropriate or feasible in “real-world” contexts (S. L. Carter, 2010). Social validity is broadly defined as participant satisfaction with intervention procedures, goals, and outcomes (Wolf, 1978). It has been argued that autism treatments cannot be considered truly evidence based without establishing social validity (Callahan et al., 2016), and therefore, this was an additional aim of the study.
The Growing, Learning, and Living With Autism Group
The purpose of the Growing, Learning, and Living With Autism (GoriLLA) Group at the Chapel Hill TEACCH Autism Center is to equip children diagnosed with ASD and their parents with self-regulation and social communication concept knowledge that can be applied throughout their daily routines. The GoriLLA Group intervention package is a blend of two widely used and complementary approaches: (a) Structured TEACCHing (Klinger, Klinger, & Pohlig, 2007; Mesibov, Shea, & Schopler, 2005; Schopler, Lansing, & Waters, 1983) and (b) components from the Social Thinking methodology (Hendrix, Palmer, Tarshis, & Winner, 2013; Winner & Crooke, 2009), specifically the five Social Thinking concepts from We Thinkers! Volume 1: Social Explorers (Hendrix et al., 2013; formerly named The Incredible Flexible You) curriculum and components from the Zones of Regulation curriculum (Kuypers, 2011). This small group intervention is parent assisted, meaning that parents are active participants in the groups, and complete weekly homework activities with their children to increase generalization of skills. Parents who have participated in previous GoriLLA Groups anecdotally report increased use and effectiveness of the intervention strategies at home, and the demand for the program is high. However, the efficacy of this intervention has yet to be studied within the context of a controlled trial.
The essential elements of Structured TEACCHing are as follows: (a) structure the environment to make activities understandable, (b) use strengths in visual skills to supplement weaker skills, (c) use special interests to promote engagement in learning, and (d) support self-initiated meaningful communication (Mesibov & Shea, 2010). These four Structured TEACCHing elements provide the framework on which the GoriLLA Group is built. Activities are environmentally structured such that tasks flow from left to right and the duration of the task, end of the task, and next task are always clear to participants. All activities include visual supports. For example, pictures of a flower and a candle are used to visually support inhalation and exhalation during deep breathing exercises and chair yoga practice. Special interests are incorporated into activities, when appropriate, to increase engagement. For instance, the clinician may use an example from a child's favorite TV show if that child is not paying attention. Finally, spontaneous social communication skills such as asking questions of others and head nodding are formally and informally supported throughout the sessions. For example, the children formally identify these skills in themselves using video feedback, but the clinician may also informally label a spontaneous comment that a parent made during the group.
The TEACCH model encourages parent-assisted intervention to support generalization of clinic-taught skills to daily routines across natural environments (Van Bourgondien & Coonrod, 2013); therefore, parents are active participants in the GoriLLA Group intervention. Though early behavioral interventions for children with ASD often employ parent coaching or parent-mediated approaches (see Nevill, Lecavalier, & Stratis, 2018, for meta-analysis), the literature on parent involvement in interventions for older children with ASD is sparse. Frankel et al. (2010) tested a social cognitive intervention called the parent-assisted children's friendship training program with children with high-functioning ASD using a randomized delayed treatment control group design. They found significant time by group effects on parent measures of social skills and play date behavior and child measures of popularity and loneliness after the 12-week intervention. The same research group (Laugeson, Frankel, Gantman, Dillon, & Mogil, 2012; Laugeson, Frankel, Mogil, & Dillon, 2009) used a parent-assisted model called PEERS to teach social competence skills to adolescents with high-functioning ASD and found improvements on parent report measures. The parent-assisted nature of their PEERS treatment was hypothesized to contribute to the maintenance of adolescents' treatment gains seen on social measures 1–5 years after the intervention (Mandelberg, Frankel, Cunningham, Gorospe, & Laugeson, 2014). In a home-based observational study of emotion self-regulation in 30- to 48-month-old children with ASD, Laurent and Gorman (2018) found that parents matched their behavior to their child's developmental level and used more behaviors consistent with parents of typically developing 2-year-olds; greater use of these parent behaviors (i.e., physical engagement, helping, redirection, and physical comfort) was then associated with better child social communication competence, but not child sensory processing competence. Considering prior positive treatment outcomes found in parent-mediated interventions for toddlers with ASD (Gulsrud, Jahromi, & Kasari, 2010), implementing an intervention of this type for elementary school–age children with ASD should improve their social communication and self-regulation concept knowledge in these areas.
Social Thinking is a therapeutic, cognitive-based methodology composed of several curricula, frameworks, and strategies. The focus of the methodology is to build social concepts and social cognitive knowledge for competencies in understanding and using social behaviors (Crooke et al., 2016; Winner, 2013). This methodology establishes the awareness needed to adapt behavior and flexibly meet social expectations across contexts and communication partners (Crooke et al., 2016). Social Thinking components are blended into the Structured TEACCHing framework to create the GoriLLA Group program because they provide a way to make abstract social concepts concrete for those learners who may not infer meaning in language easily. In this way, the visual and environmental supports of Structured TEACCHing lend themselves easily to the concrete elements of Social Thinking (e.g., holding up drawings of thought bubbles to make the thoughts of others more salient). The We Thinkers! Volume 1 curriculum is designed for high-functioning social learners from preschool to early elementary school, and therefore, the vocabulary and activities are appropriate for the young school-age children served by the GoriLLA Group. Furthermore, the Social Thinking vocabulary is “portable” in that it uses language-based strategies that can travel with the child and the parent across social environments, which promotes generalization. Emotion vocabulary and self-regulation are known to be challenging for children with ASD (Laurent & Rubin, 2004). For this reason, sections of the widely used self-regulation curriculum from Social Thinking, the Zones of Regulation (Kuypers, 2011), are embedded in the GoriLLA Group intervention. Components of the Social Thinking methodology, including the Zones of Regulation, are popular and widely used for children with ASD but do not have an established evidence base. Moreover, there is a need for parent-assisted interventions that tackle social cognitive concepts and self-regulation in community settings for children with ASD. In fact, very few randomized controlled trials have been conducted with this type of social cognitive intervention package for young children and even fewer examining the role of parents. This efficacy study aimed to answer the following research questions:
-
Is the GoriLLA Group intervention efficacious in teaching self-regulation and social communication concept knowledge to first and second graders with ASD and their parents?
a. Do first and second graders with ASD or their parents who participate in the GoriLLA Group intervention gain more self-regulation and social communication concept knowledge during the 12-week intervention period compared to a delayed treatment control group?
Do gains in concept knowledge by parents or children associated with the GoriLLA Group generalize to parent–child interactions after completing the group?
Is the GoriLLA Group a socially valid intervention for teaching self-regulation and social communication strategies to first and second graders with ASD and their parents?
Are gains in child and parent self-regulation and social communication concept knowledge maintained 3 and 6 months postintervention?
Method
Participants in this study were 17 children diagnosed with ASD and their parents (see participant demographics in Table 1). To be included, the children had to (a) have a medical diagnosis of ASD documented from The University of North Carolina TEACCH Autism Program or another clinic based on Diagnostic and Statistical Manual of Mental Disorders, 5th Edition criteria (American Psychiatric Association, 2013) supported by an Autism Diagnostic Observation Schedule (ADOS; Lord et al., 2012) and clinical parent interview, (b) be included 80%–100% of the time in a first- or second-grade regular education classroom, (c) read on a first-grade level or above (based on parent report and/or Individualized Education Plan), and (d) be able to tolerate separation from their parents for up to 30 min. In addition, parents and children had to be fluent English speakers. Inclusion in 80%–100% of the school day was used as a proxy of (a) readiness to participate in a group treatment program and (b) cognitive ability to comprehend program material. Reading on grade level was a necessary inclusion criterion because concepts and vocabulary are presented at a first-grade level and worksheets and visuals for the group require first-grade literacy skills. Four families were bilingual, but all parents reported that English was their child's strongest language. Though all children had a documented diagnosis of ASD, only five children in this sample met the ASD cutoff score of ≥ 15 on the Social Communication Questionnaire (SCQ; Rutter, Bailey, & Lord, 2003) at the preintervention assessment. Validation studies of the SCQ found that this cut-point is less valid for use with children under the age of 7.5 years than for older individuals (Barnard-Brak, Brewer, Chesnut, Richman, & Schaeffer, 2016; Lee, David, Rusyniak, Landa, & Newschaffer, 2007) and that the SCQ is more sensitive to children with lower cognitive and adaptive skills than high-functioning children (Snow & Lecavalier, 2008). Furthermore, the SCQ is a screening tool and is not meant for diagnostic purposes like the ADOS. For these reasons, the child's original diagnosis using the ADOS was considered more valid than the SCQ, and children who did not meet SCQ criteria were still included in the study.
Table 1.
Demographic characteristics of participants enrolled in intervention versus delayed treatment control groups.
| Characteristic | Intervention group (n = 8) | Delayed treatment group (n = 9) |
|---|---|---|
| Child age at study enrollment in years | ||
| Range | 6–8 | 6–8 |
| M (SD) | 6.75 (0.89) | 6.89 (0.78) |
| Child sex—girls, n (%) | 2 (25) | 2 (22) |
| Child race, n (%) | ||
| White | 7 (88) | 6 (67) |
| African American | 1 (12) | — |
| Asian | — | 2 (22) |
| Mixed/other | — | 1 (11) |
| Child ethnicity, n (%) | ||
| Non-Hispanic | 6 (75) | 9 (100) |
| Hispanic | 2 (25) | — |
| Child's age at ASD diagnosis in years | ||
| Range | 2–5 | 1.5–7 |
| M (SD) | 4.06 (1.21) | 3.83 (1.70) |
| Child's SCQ total score at study enrollment | ||
| Range | 9–20 | 9–18 |
| M (SD) | 14.5 (4.17) | 9.78 (5.07) |
| Mother's education, n (%) | ||
| Vocational/associate degree/some college | — | 1 (11) |
| College—4-year degree | 6 (75) | 2 (22) |
| Graduate/professional degree | 2 (25) | 6 (66) |
| Father's education, n (%) | ||
| Not reported | 1 (12.5) | — |
| Vocational/associate degree/some college | 1 (12.5) | — |
| College—4 year degree | 2 (25) | 2 (22) |
| Graduate/professional degree | 4 (50) | 7 (78) |
Note. Em dashes indicate "0" or no participants in the sample with that characteristic. ASD = autism spectrum disorder; SCQ = Social Communication Questionnaire.
After randomization, the study groups (intervention: n = 8; control: n = 10) were evenly matched on age, t(16) = 0.62, p ≤ .73, and sex, χ2(1, 18) = 0.06, p ≤ .80. Parents of children randomized to the delayed treatment control group reported significantly fewer symptoms of ASD on the SCQ, t(15) = –2.08, p ≤ .03, than parents of the children in the intervention group. Race, ethnicity, and parent education levels were not significantly different between the groups.
Parents were asked to report interventions that their child was currently receiving and had received from birth to the start of the study. Children's current treatment goals overwhelmingly focused on social communication skills and pragmatic language. Some children were also receiving occupational therapy for handwriting or additional speech-language therapy for fluency disorders. All of the children had prestudy exposure to “social skills” instruction either in a group or individual setting, most often with a speech-language pathologist but occasionally with an occupational therapist or psychologist. Parents reported that seven of the children had been exposed to the Zones of Regulation curriculum and eight of the children had previous or current exposure to other components of the Social Thinking methodology; in all but one case, if a child was exposed to one of these curricula, he was also exposed to the other. Twenty-five percent of the intervention group and 60% of the delayed treatment control group had previous exposure to these curricula. Intervention dosage of Social Thinking and the Zones of Regulation was highly variable as reported by parents. Some parents reported that Social Thinking concepts like “Whole Body Listening” along with non–Social Thinking concepts were used in an intervention, while other parents reported using vocabulary or following weekly lessons from one or more components of the Social Thinking methodology. Furthermore, some parents did not provide an Individualized Education Plan or report details of their child's school intervention, so it is possible that some of the school interventions also used these curricula.
Procedure
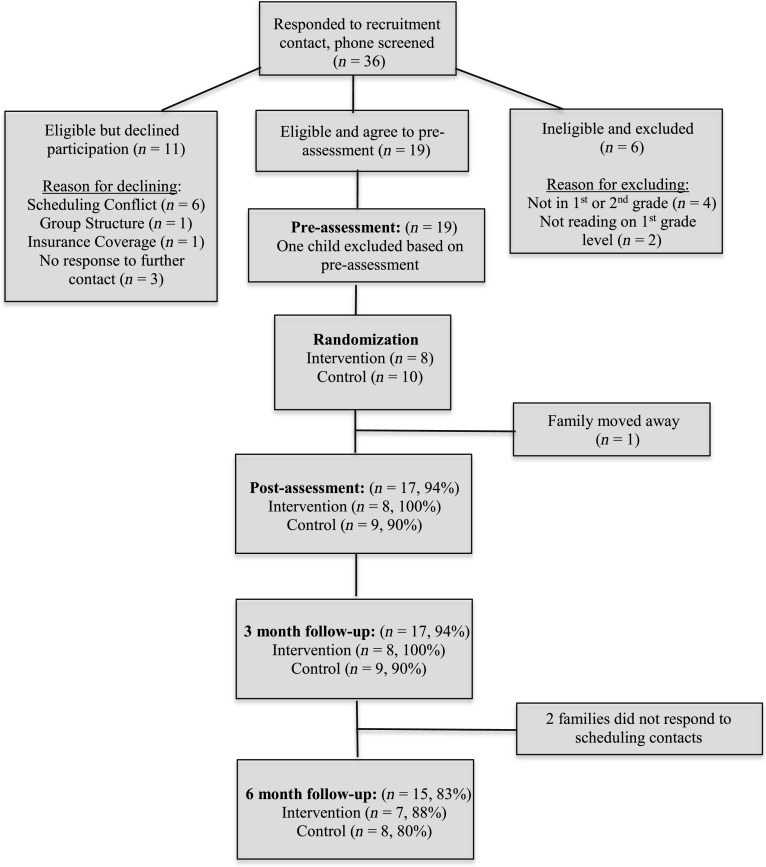
A randomized delayed treatment control group design was used to address the study aims. A recruitment letter was mailed to parents of children on the clinic waitlist for the GoriLLA Group (n = 37). Families from the waitlist were given 2 weeks to respond to the letter or a follow-up phone call before an e-mail announcing study recruitment was sent to the clinic listserv of the Chapel Hill TEACCH Center to fill the remaining participant openings (approximately 2,800 e-mail addresses). The first author screened parents by phone (n = 36) to see if they and their children met minimum study inclusion criteria before inviting them for an assessment. See Figure 1 for a flow chart of study recruitment and retention.
Figure 1.
Flow diagram for the Growing, Learning, and Living With Autism Group Study.
Assessments took place at pre- and postintervention and two follow-up visits, 3 and 6 months postintervention, at the Chapel Hill TEACCH Center. At each 60- to 90-min assessment, parent and child intervention strategy knowledge was tested and a 15-min parent–child play interaction, assessing application of strategies, was completed. Participants were given $25 for each assessment; thus, they were compensated up to $100 for this study. The first author and the GoriLLA Group clinicians administered all of the preintervention assessments prior to randomization. Assessors for the postintervention and follow-up assessments came from a pool of five master's students in speech-language pathology who were blind to the family's group allocation.
Our recruitment goal was to have 16 families participate in the study, as four families per group was considered optimal by the clinicians; however, to account for possible attrition during the delayed treatment period, two additional families were overrecruited to the delayed treatment control group. A sample size of 18 families was the largest sample size deemed feasible for the study, given the constraints of the clinical program. A total of 19 families completed pretreatment assessments. Eighteen of the 19 families met study inclusion criteria based on the preintervention assessment. These 18 families were randomized in blocks of nine to ensure equal chance of group membership in either the intervention GoriLLA Groups or the delayed treatment control groups (eight families randomized to the intervention group; 10 to the control group). Two groups of four families ran concurrently in the spring with the delayed treatment groups receiving their services as usual in the community while waiting to participate in the GoriLLA Group in the fall. The 3- and 6-month follow-up visits for the intervention groups in the fall served as the pre- and postintervention assessments for the delayed treatment groups who received the GoriLLA intervention between these assessment time points.
Participants were seen for the study using the same HIPAA-compliant clinical procedures used at the Chapel Hill TEACCH Center. Intervention sessions were billed as psychotherapy groups as part of standard clinic practices. GoriLLA Groups met for 90 min weekly, and sessions consisted of parent–child large and small group activities targeting social communication and self-regulation (see session content summaries in Table 2). Weekly 20- to 30-min parent breakout sessions consisted of (a) review of the previous week's homework, (b) discussion of the current week's concept and brainstorming how to practice at home, (c) group behavior problem solving for one family, (d) discussion of what the children are doing and how to support them in the upcoming parent–child activity, and (e) assignment of “homework” for the week.
Table 2.
Growing, Learning, and Living With Autism (GoriLLA) Group session sequence and content summary.
| Session | Session title | Session content summary |
|---|---|---|
| Parent Session 1 | Introduction to GoriLLA Group and Structured TEACCHing | Presentation and parent discussion about the purpose of the GoriLLA Group, how groups will be structured, what a parent-assisted intervention means, and the objectives of the group. |
| Introduction to Structured TEACCHing and how environmental structure and visual supports will be used in sessions. | ||
| Parent Session 2 | Introduction to Social Thinking and the Zones of Regulation | Presentation and parent discussion of child social communication and self-regulation characteristics and how the group aims to address those issues. |
| Introduction to The Incredible Flexible You and Zones of Regulation curricula and vocabulary that will be used in the groups. | ||
| Parent–Child Session 1 | Thinking Thoughts and Feeling Feelings | Introductions and purpose of the GoriLLA Group |
| • Introduce “expected and unexpected behaviors” (Kuypers, 2011, pp. 48–53) introduction, sorting expectations for the group using this vocabulary | ||
| • Deep breathing and chair yoga introduction (adapted from Living Words of Wisdom, 2014) | ||
| Introduce “Thinking Thoughts and Feeling Feelings” (Hendrix et al., 2013, pp. 49–70) | ||
| • Read Book 1 with guided lesson plan (pp. 53–56) | ||
| • Song “Where you think a thought” (p. 159) | ||
| • “I’m thinking of” activity (adapted from pp. 56–57) | ||
| • Block building dramatic play activity (pp. 58–59) | ||
| • Social Smarts Booklet (adapted from Winner & Crooke, 2010) | ||
| • Thinking Thoughts and Feeling Feelings review worksheet (adapted from Hendrix et al., 2013) | ||
| Prizes (behavioral reinforcement) | ||
| Parent–Child Session 2 | Self-regulation and Me | Chair yoga and deep breathing |
| Introduction to the Zones of Regulation (Kuypers, 2011, pp. 23–36) | ||
| • Sort emotion face cards onto Zones poster (adapted from pp. 27–36) | ||
| Vocabulary review from previous week (“feed” vocabulary words written on bananas to a gorilla poster) | ||
| • Read book The Way I Feel (Cain, 2005) with lesson based on Kuypers (2011) pp. 82–84 | ||
| • Play Twister with Zones of Regulation questions | ||
| • Make stress balls (fill balloons with rice or flour) | ||
| • Build LEGO creations while parents are coached using paper thought bubbles (visual support for thinking a thought) and pause card (visual support for stopping an activity and finishing it later) | ||
| • Review “Get to Green GoriLLA Plan” (relaxation activity system with visuals that includes chair yoga, progressive relaxation, positive visualization, deep breathing, and stress balls) and practice with parent coaching | ||
| • Introduce “Zones check-in” (adapted from Kuypers, 2011, pp. 99) | ||
| • “Spotlight friend” (show and tell activity with children coached by parents to ask questions about another person’s interest or experience) | ||
| • Prizes | ||
| Parent–Child Session 3a | The Group Plan, Part 1 | Introduce “The Group Plan” (Hendrix et al., 2013, pp. 71–88) |
| • Read Book 2 with guided lesson plan (p. 73–75) | ||
| • Milk Pail Obstacle Course (p. 76) | ||
| • Egg Pass (p. 77) | ||
| • “Our family and the group plan” worksheet with parents adapted from The Group Plan concept | ||
| • The Group Plan review worksheet adapted from Hendrix et al., 2013 materials | ||
| Parent–Child Session 4 | The Group Plan, Part 2 | Review “The Group Plan” (Hendrix et al., 2013, pp. 71–88) |
| • Plant a garden activity (follow the group plan for making tissue paper flowers and coloring in a garden for a group art project) | ||
| • Make trail mix (adapted from p. 78) | ||
| • Play Richard Scarry’s Busytown Game, practice following the group plan | ||
| • Group plan review worksheet (adapted from Hendrix et al., 2013, content) | ||
| • Good thoughts time (positive visualization time using thought bubbles, p. 65) | ||
| Parent–Child Session 5 | Thinking With Your Eyes, Part 1 | Introduce “Thinking With Your Eyes” (Hendrix et al., 2013, pp. 89–107) |
| • Read Book 3 with guided lesson plan (pp. 92–93) | ||
| • Astronaut Dress Up (p. 95) | ||
| • Space Walk (p. 96) | ||
| • Practice following parent’s gaze using arrows as visual supports (adapted from p. 94) | ||
| • Time to Relax book (clinic created visual supports for relaxation strategies) | ||
| Parent–Child Session 6 | Thinking With Your Eyes, Part 2 | Review “Thinking With Your Eyes” (Hendrix et al., 2013, pp. 89–107) |
| • Thinking With Your Eyes high fives (p. 95) | ||
| • Thinking With Your Eyes music activity (p. 95) | ||
| • Introduce SENSE (McAfee, 2002, pp. 102–108) | ||
| • Video modeling (Cox and AFIRM team, 2018) conversations with SENSE | ||
| • SENSE review worksheet (adapted from McAfee, 2002) | ||
| • Time to Relax book | ||
| Parent–Child Session 7 | Body in the Group, Part 1 | Introduce “Body in the Group” (Hendrix et al., 2013, pp. 109–123) |
| • Read Book 4 with guided lesson plan (pp. 111–112) | ||
| • Islands activity (pp. 113–114) | ||
| • Obstacle course (pp. 114–115) | ||
| • Review worksheet based on “Body in the Group” concept | ||
| Parent–Child Session 8 | Body in the Group, Part 2 | Review “Body in the Group” (Hendrix et al., 2013, pp. 109–123) |
| • Read “Personal Space Camp” (Cook, 2007) | ||
| • Music activity (p. 113) | ||
| • Trace and decorate bodies | ||
| • Group walk to practice staying in the group | ||
| • “Report to parents” review worksheet based on Body in the Group concept | ||
| Parent–Child Session 9 | Whole Body Listening | Introduce “Whole Body Listening” (Hendrix et al., 2013, pp. 125–139) |
| • Read Book 5 with guided lesson plan (pp. 127–129) | ||
| • Whole body listening poster activity | ||
| • Zoo adventure (p. 131) | ||
| • Music activity (p. 130) | ||
| • Rhyming fill-in-the-blank worksheet based on Whole Body Listening concept | ||
| • Review worksheet based on Whole Body Listening concept | ||
| Parent–Child Session 10 | Putting It All Together | Review games adapted to include group concepts and vocabulary |
| • Headbanz | ||
| • Jeopardy | ||
| • Bingo | ||
| • True or False hallway “trek” | ||
| Celebration and award ceremony |
Starting with Session #3, all sessions begin with snack and arrival worksheet (e.g., word search of group concepts), Get to Green GoriLLA Plan, Zones Check-In, and vocabulary review. All sessions end with Get to Green GoriLLA Plan, Zones Check-In, Spotlight Friend, and Prizes. These activities are described where they are introduced in Sessions 1 and 2 above.
The intervention was delivered by teams of two trained clinicians with master's degrees, assisted by a clinical psychology doctoral student or postdoctoral research fellow. Fidelity was monitored via video recordings of each session; adherence checklists were monitored by the principal investigator, and deviations were discussed with the clinical team at weekly meetings. Overall, clinician quality and behavior management ratings were recorded by research assistants to obtain an objective measure of the quality of intervention implementation and behavior management in each session. These ratings were assigned from video recordings once the intervention was completed. Parents completed homework exercises and maintained a log of strategies that they used each week. The core GoriLLA Group strategies and concepts that were tested at pre- and postassessments and logged each week by parents can be viewed in Table 3.
Table 3.
Growing, Learning, and Living With Autism Group core strategies and concepts.
| Strategy/concept |
Definition |
|---|---|
| Self-regulation | |
| Zones of regulation | Using concrete terminology and visuals (colors) to make abstract emotion identification and regulation concepts comprehensible to young children |
| Stress balls | Releasing negative feelings and energy by squeezing a ball |
| Deep breathing | Visual support for diaphragmatic breathing |
| Progressive relaxation | Step-by-step visual exercise to tense and relax each body part to release tension. |
| Chair yoga | Six simple yoga poses with visual instructions (adapted from Living Words of Wisdom, 2014) |
| Drawing/journaling | A method of expressing thoughts/feelings/experiences through writing and drawing |
| Visualization | Using positive imagery to shift thoughts from negative to positive. Thought bubbles held above a child's head used as visual supports (see Hendrix et al., 2013, p. 50) to encourage “thinking a happy thought” |
|
Social communication | |
| Expected vs. unexpected behaviors | Concrete terminology to describe behaviors that give others comfortable/uncomfortable thoughts in various social scenarios (Palmer et al., 2016, pp. 33–60) |
| The group plan | Terminology to describe the benefits of working on what the group is doing rather than following “your own plan” (Hendrix et al., 2013, pp. 71–88) |
| Thinking with your eyes | Method of describing the social information conveyed by social eye gaze shifts, using the visual support of arrows to indicate that “eyes are like arrows” and how kids can use this information to learn about what others are thinking (Hendrix et al., 2013, pp. 89–108) |
| SENSE | Nonverbal conversation skills—space, eye contact, nodding (gestures), statements, and expressions (McAfee, 2002, pp. 102–108) |
| Body in the group | Method of teaching the physical boundaries of group participation (Hendrix et al., 2013, pp. 109–124) |
| Whole body listening | Children learn to identify all of the clues their bodies provide to show they are listening (Hendrix et al., 2013, pp. 125–142) |
| Social narratives | Writing personal narratives from the child's perspective about behavioral expectations in a particular setting (taught only in parent breakout sessions) |
|
Structured TEACCHing | |
| Pause cards | Visual reminder to pause an activity and come back to it later |
| Visual countdowns | Physically removing numbers from a countdown to demonstrate when a transition is approaching |
| Schedules/checklists | Use of schedules and activity checklists to inform children about what is expected now, when it will be finished, and what is coming in the future |
All study procedures were reviewed and approved by the institutional review board at the The University of North Carolina at Chapel Hill. Informed parental consent was obtained for all participants in the study. If children were over the age of 7 years, they assented to their participation in the study.
Instrumentation
Intervention Efficacy Outcome Measures
The Child Observation Protocol (COP; C. V. Carter, Varblow, Brady, & Woods, 2016) is a 22-item semistructured measure of the 12 core social communication and self-regulation concepts and vocabulary taught in the GoriLLA Group (see Supplemental Material S1 for item descriptions; full measure available upon request). The COP was developed by the GoriLLA Group clinicians to assess GoriLLA Group concept and vocabulary knowledge, and it was administered at all assessment time points. Children were seated across from an examiner and asked to follow a visual schedule as they progressed through materials for each task. Items were scored on a 0–3 scale, with 3 indicating mastery of the concept; total scores ranged from 0 to 66. A total score was used as the primary outcome measure for children in the study.
To elucidate the effectiveness of the three major intervention components of the GoriLLA Group, COP items were divided into three theoretically based subscales: Social Thinking, Self-Regulation, and Social Communication. The Social Thinking subscale included core concepts and vocabulary from one component of the Social Thinking methodology, We Thinkers! Volume 1 (Hendrix et al., 2013). One additional Social Thinking vocabulary–concept pair (i.e., expected and unexpected behaviors) from the We Thinkers! Volume 2: Social Explorers curriculum guide (Hendrix, Palmer, Tarshis, & Winner, 2016) was introduced in Session 1. Items included in the Social Thinking subscale were Expected Versus Unexpected Behavior, the Group Plan, Body in the Group, Thinking With Your Eyes, Whole Body Listening, and Labeling Thoughts/Feelings of Others. The Self-Regulation subscale included select concepts and vocabulary from the Zones of Regulation curriculum (Kuypers, 2011): identifying zone colors, stating body states for each zone, sorting scenarios into reasonable zones, demonstration of calming techniques, and coping with two unexpected events during the assessment (e.g., skipping a scheduled fun activity and waiting to complete a LEGO building task until the end of the assessment). Finally, the Social Communication subscale included verbal and nonverbal conversation skills taught in the GoriLLA Group, which were coded across the entirety of the assessment interaction with the examiner: sharing information with others, taking turns in conversation, commenting on topics unrelated to own interests, asking questions, using appropriate body language (SENSE concept from McAfee, 2002, pp. 102–108), and recognizing emotion in others.
COP tasks were the same at all assessment time points, but some stimuli (e.g., the particular social situations depicted in photographs, the fun activity that needed to be skipped) were changed to minimize memory effects. Assessors at Time Points 2, 3, and 4 were master's students in speech-language pathology who were blind to the child's group allocation and established reliability with the test creators by having over 80% scoring agreement on two sequential assessment observations, either live or via video recording, prior to administering and scoring the protocol independently. Internal consistency of the COP was fair to good (Cronbach's alpha at pretest = .76, Cronbach's alpha at posttest = .81). Interrater reliability data were collected live with a second research assistant independently scoring seven (41%) of the postintervention assessments. The intraclass correlation coefficient (ICC) for the total COP score was .97, which is in the “excellent” range. ICCs for COP items were in the “good” to “excellent” range (based on Cicchetti & Sparrow, 1990), with a few exceptions; Item B5 (eye contact/gestures/body language; ICC = .16) and Item K1 (following eye gaze; ICC = .42) seemed to be particularly challenging social interaction skills to code when observing rather than administering the assessment.
The Parent Report of Group Outcomes (PROGO; C. V. Carter & Brady, 2016) consists of 12 multiple-choice questions tapping general ASD knowledge as well as concepts and vocabulary from GoriLLA Group sessions (see Supplemental Material S2 for sample questions from the PROGO; full measure available upon request). It includes three open-ended hypothetical scenarios, and parents are asked to describe the strategies they would use with their child in that scenario. All parents completed this measure at all assessment time points. Scenarios and the order of the multiple-choice questions were changed to minimize memory effects from pre- to posttest. Internal consistency was fair for the multiple-choice questions on this measure (Cronbach's alpha at Time 1 = .55, Cronbach's alpha at Time 2 = .66). The open-ended scenario questions were transcribed and coded for the number of times in each scenario the parent reported that they would use a GoriLLA Group strategy or vocabulary word. The total number of strategies/vocabulary words reported in each scenario at each time point was used in the analyses.
Generalization to Parent–Child Interaction Outcome Measure
The 3-Box Task (Brady-Smith et al., 1999; Howard, Martin, Berlin, & Brooks-Gunn, 2011; NICHD Early Child Care Research Network, 1999; Vandell, 1979) is a semistructured parent–child play observation of parent and child social interaction skills (e.g., Parental Sensitivity, Child Engagement of Parent, Mutuality/Connectedness; see Table 4 for a full list of subscales measured). This task served as a measure of the generalization of strategies practiced in the GoriLLA Group to parent–child interaction occurring outside the intervention context. Dyads are given three numbered containers and asked to play with the box contents in sequence over the course of 15 min. The exact contents of the boxes changed at each assessment, but they always included (a) a turn-taking game like Jenga, (b) a set of pretend play figures and their accessories, and (c) a picture book. ICCs during a parent–child interaction with 36-month-olds from a previous research group (Early Head Start Project) ranged from .54 to .69, with 89%–98% exact coder agreement (Love et al., 2005). Ten child and parent behaviors were rated from video on a 1–7 scale by a master's student research assistant who was blind to the family's study group allocation. A bachelor's-level research assistant was trained to independently score 20% of the videos as a reliability check (i.e., one of every five recordings was selected using a random number generator). Average rater agreement for the 10 ratings was good (mean exact kappa = .81). For this sample, Parent Intrusiveness (exact kappa = .18) and Parent Engagement (exact kappa = .36) had very low rater agreement compared to the other scales.
Table 4.
Results by measure.
| Measure | Subscale | Time 1 M (SD) |
Time 2 M (SD) |
Time 3 M (SD) |
Time 4 M (SD) |
Time × Group interaction |
Effect |
|||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Intervention | DT | Intervention | DT | Intervention | DT | Intervention | DT | F | p | η2 | ||
| COP | ||||||||||||
| Total | 20.09 (4.43) | 21.18 (4.59) | 24.61 (4.26) | 20.86 (5.87) | 24.56 (4.26) | 20.41 (3.83) | 25.84 (4.56) | 23.29 (5.34) | 6.90 | .02* | .32 | |
| Social Thinking | 9.44 (3.16) | 10.55 (3.54) | 11.38 (2.13) | 9.89 (3.66) | 11.44 (2.58) | 9.31 (3.41) | 12.07 (3.67) | 9.71 (3.60) | 4.78 | .05* | .24 | |
| Self-Regulation | 4.13 (1.22) | 4.35 (0.97) | 6.19 (1.36) | 4.3 (1.07) | 5.88 (1.13) | 4.63 (0.99) | 6.5 (0.41) | 6.14 (1.41) | 4.14 | .06 | .22 | |
| Social Communication | 3.78 (0.77) | 3.48 (1.19) | 4.56 (1.45) | 3.69 (1.28) | 4.5 (0.73) | 3.73 (0.96) | 4.49 (1.07) | 4.57 (1.03) | 4.14 | .06 | .22 | |
| PROGO | ||||||||||||
| Total | 9.04 (0.85) | 9.92 (0.99) | 10.38 (1.18) | 10.06 (0.94) | 10.01 (0.63) | 10.00 (1.00) | 10.49 (0.49) | 10.85 (0.69) | 7.06 | .02* | .32 | |
| Social Thinking | 2.44 (0.32 | 2.73 (0.34) | 2.56 (0.37) | 2.69 (0.30) | 2.5 (0.30) | 2.69 (0.40) | 2.75 (0.29) | 2.82 (0.28) | 1.29 | .27 | .08 | |
| Self-Regulation | 2.66 (0.57) | 2.8 (0.80) | 3.56 (0.65) | 2.89 (0.57) | 3.13 (0.35) | 2.94 (0.48) | 3.39 (0.38) | 3.43 (0.55) | 6.10 | .03* | .29 | |
| Autism Spectrum Disorder | 3.94 (0.45) | 4.40 (0.47) | 4.25 (0.58) | 4.47 (0.37) | 4.39 (0.33) | 4.37 (0.61) | 4.35 (0.22) | 4.60 (0.48) | 1.91 | .19 | .11 | |
| Self-Regulation Scenario | 0.38 (1.06) | 0.67 (0.71) | 1.5 (1.41) | 0.78 (0.83) | 1.29 (0.70) | 0.50 (0.76) | 1 (0) | 2.5 (0.71) | 2.75 | .12 | .15 | |
| Social Thinking Scenario | 0.13 (0.35) | 0.67 (0.71) | 0.63 (0.74) | 0.56 (0.53) | 0.50 (0.55) | 0.75 (0.71) | 0.67 (0.58) | 0.50 (0.58) | 3.44 | .08 | .19 | |
| Structured TEACCHing Scenario | 0 (0) | 1 (1) | 0.88 (0.64) | 1.33 (0.71) | 0.75 (0.50) | 1 (0.53) | 0.50 (0.71) | 2 (0) | .90 | .28 | .08 | |
| 3-Box Task | ||||||||||||
| Parent Sensitivity | 5.56 (1.24) | 6.36 (0.92) | 5.78 (1.20) | 6 (1) | .43 | .53 | .03 | |||||
| Parent Intrusiveness | 2.78 (1.48) | 1.82 (1.17) | 2.44 (1.33) | 2 (1.55) | .15 | .71 | .01 | |||||
| Parent Cognitive Stimulation | 5 (1) | 4.91 (1.64) | 4.56 (1.01) | 4.64 (1.80) | .32 | .58 | .02 | |||||
| Parent Positive Regard | 4.67 (0.5) | 5.09 (0.94) | 4.56 (0.73) | 5.27 (1.10) | 1.50 | .24 | .09 | |||||
| Parent Negative Regard | 1.56 (0.53) | 1.27 (0.65) | 1.56 (0.53) | 1.36 (0.81) | 2.01 | .18 | .12 | |||||
| Parent Detachment | 1.33 (0.5) | 1.27 (0.47) | 1.89 (0.60) | 1.18 (0.4) | 4.85 | .04* | −.24 | |||||
| Child Engagement | 5.56 (1.01) | 5.55 (1.37) | 5.22 (0.97) | 5.36 (1.63) | 2.13 | .17 | .12 | |||||
| Child Attention to Objects | 6.22 (0.67) | 6.36 (0.67) | 6 (1) | 6.18 (0.98) | .27 | .61 | .02 | |||||
| Child Negativity | 1.67 (0.5) | 1.45 (1.04) | 1.89 (0.93) | 1.82 (0.75) | .004 | .95 | .00 | |||||
| Mutuality/ Connectedness |
5.44 (0.73) | 5.72 (1.10) | 5.22 (0.67) | 5.45 (1.04) | .72 | .41 | .05 | |||||
| Auditory Press | ||||||||||||
| Attention to Alarm | 2.63 (1.19) | 2.44 (1.24) | .75 (0.71) | 1.11 (1.45) | .99 | .34 | .06 | |||||
| Attention to Other | 1.88 (0.83) | 2 (1.41) | 1.75 (1.04) | 2.11 (1.27) | .15 | .70 | .01 | |||||
| Attention to Parent | 1.38 (0.92) | 0.89 (1.27) | 0.75 (1.04) | 0.56 (0.73) | .25 | .63 | .02 | |||||
| Self-Comforting | 0.38 (0.52) | 0.33 (0.71) | 0 (0) | 0 (0) | .02 | .89 | .00 | |||||
| Physical Action Toward Alarm |
0.13 (0.35) | 0.11 (0.33) | 0 (0) | 0 (0) | .01 | .93 | .00 | |||||
Note. 3-Box Task and Auditory Press not collected at Time 3 and Time 4. Time by group interaction and effects reported are for Time 1 to Time 2. Intervention for the delayed treatment control group occurred between Time 3 and Time 4. DT = delayed treatment control group; COP = Child Observation Protocol, Unweighted subscale scores; PROGO = Parent Report of Group Outcomes, Unweighted subscale scores.
p ≤ .05.
Two self-regulation presses were added to the 3-Box Task for this study in order to directly assess generalization of the self-regulation concepts learned in the group to parent–child interactions: (a) an auditory interruption that occurred during the play session when a clock alarmed for 30 s and (b) a delayed gratification task wherein the child was given a mini cupcake at the start of the play time and told that they would receive a second cupcake if they delayed eating the first cupcake until the examiner returned. The alarm task was coded for child self-regulatory behaviors (e.g., covering ears, asking parent to turn it off) and attention shifts (e.g., looking at alarm, looking at parent for assistance) during the 30-s period that the alarm is sounding. The delayed gratification task was coded for parent (e.g., distracting the child from the cupcake) and child (e.g., touching the cupcake) behaviors in 30-s intervals across the entire 15-min play period. See Table 4 for complete list of the parent and child behaviors coded.
Social Validity Outcome Measure
The GoriLLA Group Social Validity Measure, based on the Social Validity Questionnaire for Parents (Barrett, 2005), is an 11-item tool designed to tap parent satisfaction with the goals, procedures, and effects of the intervention. Items are coded from a scale of 1 (not at all) to 4 (always). Parents in the intervention group completed this measure at posttest.
ASD Symptom Measure
The SCQ (Rutter et al., 2003) was completed by parents at the preintervention assessment to describe the child's current clinical symptom levels of ASD.
Fidelity Measure
The GoriLLA Group Fidelity Tool was developed to assess fidelity of the GoriLLA Group curriculum implementation (see Supplemental Material S3 for sample session fidelity form; full fidelity form available upon request). It includes documentation of attendance, an adherence checklist of session activities and materials, and 5-point ratings for overall Quality and Behavior Management skills used by clinicians throughout the session (higher scores indicate better skills; see Supplemental Material S4 for the quality and behavior ratings used). Clinicians were asked to aim for between 80% and 100% adherence to their session curriculum. They codeveloped the adherence checklists with the principal investigator and had access to them during each session. Two master's student research assistants in speech-language pathology were trained to reliability on the Quality and Behavior Management ratings and monitored fidelity of the intervention from video recordings. They were also trained in the core treatment components of the GoriLLA Group and reviewed the manual and materials lists before coding each session. Interrater reliability for Quality and Behavior Management ratings was established by coding videos of the pilot group sessions until there was greater than 80% agreement on ratings for three consecutive videos. Each activity was rated for Quality and Behavior Management by the raters, and an overall mean of all the activity ratings in the session was used in the analyses. Twenty percent of the recordings were randomly selected for fidelity coding using a random number generator. Exact rater agreement on mean session quality ratings was high at 91%. Monday and Thursday groups had nearly identical mean quality ratings (Monday = 3.06, Thursday = 3.07), indicating consistency of Quality during the study. Rater agreement for Behavior Management ratings was 100%. Mean behavior ratings were the same (4.76) for Monday and Thursday groups, indicating consistency of Behavior Management during the study.
Results
All analyses were conducted using JMP 13 Pro (JMP Pro, 2014). Although multiple statistical tests were performed within each outcome to address the research questions, in this preliminary efficacy study project with a modest sample size, we judged it more important to avoid overlooking statistical signals of effectiveness of the GoriLLA Group intervention (Type II errors), rather than to avoid false assertions of effectiveness (Type I errors). Therefore, conservative adjustments to the Type I error rates were not employed. Table 4 summarizes results from all study measures at pre- and postintervention related to Research Questions 1 and 2.
Efficacy of the GoriLLA Group in Increasing Self-Regulation and Social Communication Concept Knowledge
Time × Group interactions on the COP were tested using repeated-measures analysis of variance (ANOVA). Significant time by group effects were found for the total COP score, F(1, 15) = 6.90, p ≤.02, η2 = .32, indicating that the intervention group improved their self-regulation and social communication knowledge and skills during the intervention period significantly more than the delayed treatment group. When analyzed by subscale, a significant Time × Group interaction was found for the Social Thinking subscale, F(1, 15) = 4.78, p ≤ .05, η2 = .24. Time by group effects were not statistically significant for the Self-Regulation subscale, F(1, 15) = 4.14, p ≤ .06, η2 = .22, or the Social Communication subscale, F(1, 15) = 4.14, p ≤ .06, η2 = .22, though effect sizes were large and favored the intervention group in each case. When controlling for the significant group differences in preintervention autism symptoms on the SCQ, these effects were no longer significant, though effect sizes were medium, favoring the intervention group: Total COP score, F(1, 14) = 2.73, p ≤ .12, η2 = .11; Social Thinking subscale, F(1, 14) = 2.34, p ≤ .15, η2 = .12.
Since nearly half of the children had been reportedly exposed to Social Thinking and the Zones of Regulation (in seven of eight cases, children were exposed to both), COP performance differences between the children with previous exposure to these curricula (n = 8) versus those without previous exposure (n = 9) were examined. There were no significant differences in preintervention COP scores between children with previous Social Thinking and Zones of Regulation exposure and children without that exposure: Total COP score: F(2, 15) = 0.06, p ≤ .94; Social Thinking subscale: F(2, 15) = 0.01, p ≤ .99; Self-Regulation subscale: F(2, 15) = 2.10, p ≤ .16.
Repeated-measures ANOVA were used to test for Time × Group interactions on the multiple-choice section of the PROGO. A significant time by group effect was found for the total score on the PROGO, F(1, 15) = 7.06, p ≤ .02, η2 = .32, favoring the intervention group. When analyzed separately by subscale, the Self-Regulation subscale of the PROGO demonstrated a significant time by group effect, F(1, 15) = 6.10, p ≤ .03, η2 = .29, but the Social Thinking, F(1, 15) = 1.29, p ≤ .27, η2 = .08, and ASD Knowledge, F(1, 15) = 1.91, p ≤ .19, η2 = .11, subscales did not, though they had medium effect sizes.
Frequency counts of the number of GoriLLA Group strategies and concepts reported in the three applied scenarios from the PROGO were analyzed using repeated-measures ANOVA to test for Time × Group interactions for each scenario. In the first scenario, targeting self-regulation strategies, parents in the intervention group showed a pattern of slightly increased GoriLLA Group strategies reported from Time 1 to Time 2, but the Time × Group interaction was nonsignificant, F(1, 15) = 2.75, p ≤ .12, η2 = .15. Similarly, the second scenario, targeting Social Thinking concepts, showed an increase from Time 1 to Time 2 in the intervention group as compared to the delayed treatment control group (mean at Time 1 = 0.6, mean at Time 2 = 0.4), but there was not a significant Time × Group interaction, F(1, 15) = 3.44, p ≤ .08, η2 = .19. Finally, the third scenario, targeting Structured TEACCHing strategies, showed significant time effects, F(1, 15) = 6.25, p ≤ .02, indicating that both groups improved from pre- to posttest, but there were no significant time by group effects, F(1, 15) = 0.90, p ≤ .28, η2 = .08. However, in the case of all three scenarios, medium to medium–large effect sizes favored the intervention group.
Generalization of Self-Regulation and Social Communication Concept Knowledge to Parent–Child Interactions
No GoriLLA Group treatment effects were found to generalize to parent–child social interaction behaviors coded on the 3-Box Task. No Time × Group interactions were found for parent, child, or mutuality/connectedness behaviors coded during this task. One unanticipated exception was that Parent Detachment increased significantly for parents who participated in the GoriLLA Group as compared to the waitlist control group, F(1, 15) = 4.85, p ≤ .04, η2 = .24. The Auditory Press during the 3-Box Task did not show any Time × Group interaction effects. Finally, the Delayed Gratification Press during the 3-Box Task interaction did not demonstrate any significant time or time by group effects in the sample. In fact, more than half of the children in the sample were “noneaters,” meaning that they made an immediate decision to wait for the examiner to return in order to receive a second cupcake and did not demonstrate any behaviors counter to that decision during the 15-min play period with their parent. This restricted the number of parent and child behaviors that occurred during the interactions. In contrast, about a third (n = 5) of the sample were classified as “eaters,” meaning that, upon hearing the instructions, they immediately decided to eat the cupcake and did so within minutes. This behavior also restricted the number of codable behaviors, as there was no longer a temptation in the room to elicit behaviors once the child finished eating the cupcake. There were more “eaters” in the delayed treatment control group (n = 4) than the intervention group (n = 1) at the preintervention assessment, so a treatment effect was not possible to detect; however, it was noted that “noneaters” were consistent with their decision across time points and only one “eater” became a “noneater” from the pre- to postassessment. Data from the 3-Box Task at Time 3 and Time 4 were not analyzed due to lack of effects between Time 1 and Time 2.
Social Validity
Seven of the eight intervention group parents who received the GoriLLA Group intervention completed the social validity measure. Items were rated on a 1–4 scale with “1” indicating not useful at all and “4” indicating very useful. Overall, parents rated the GoriLLA Group as mostly useful to very useful for teaching social communication and self-regulation skills to their child, helping them to support their child's development in these areas, and advocating for their child in community settings. Parents unanimously felt that it was helpful for them to participate in the group with other parents of children with ASD. They also enjoyed attending the group and felt that their child enjoyed the group experience most of the time to all of the time. t Tests were used to examine differences in the two GoriLLA Groups, which met on different days of the week with slightly different clinician teams. Parents in one of the groups felt that self-regulation skills were significantly less useful for children with ASD in general compared to the other group. These parents started the intervention with slightly less self-regulation knowledge than the other group, but these differences were not statistically significant: pretest, t(6) = 1.45, p ≤ .20; posttest, t(6) = 0.87, p ≤ .42. Interestingly, their children started and ended the groups with slightly more knowledge and skills on the COP in this area, but these were also not significant differences: pretest, t(6) = –1.20, p ≤ .28; posttest, t(6) = –0.52, p ≤ .62. It is plausible that, because their children had more knowledge and skills in this area, parents did not feel that these skills were as important areas of need for children with ASD as did parents of children in the other GoriLLA Group. Otherwise, there were no significant differences in social validity responses between GoriLLA Groups that met on different days. Parents whose children had participated previously in group interventions with strategies and concepts from Social Thinking and the Zones of Regulation tended to rate the usefulness of the GoriLLA Group lower than those who were new to the concepts. For example, one parent noted, “This felt more like nice reinforcement of what we already know.”
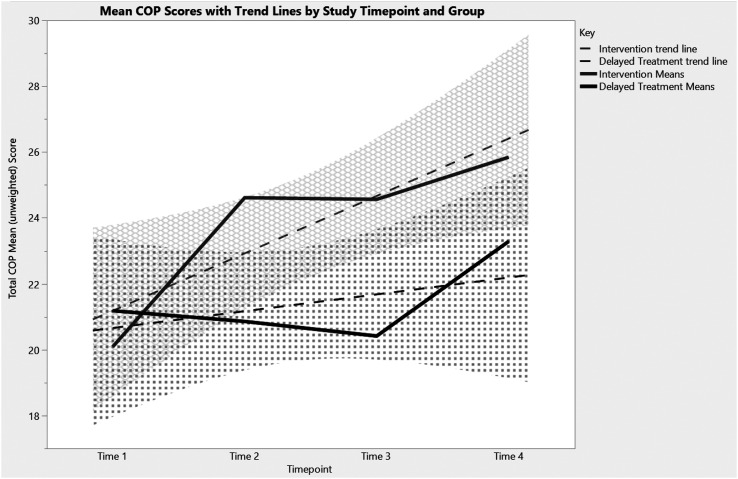
Maintenance of Concept Knowledge at 3 and 6 Months Follow-Up
Families in both study groups participated in follow-up assessments at 3 and 6 months postintervention. These assessments also served as pre- and postintervention assessments for the delayed treatment group who received the intervention between these time points. At the 3-month follow-up assessment, just before the control group started intervention, time by group differences were stable, with the intervention group children performing significantly better on the COP than the delayed treatment group children, F(2, 13) = 4.81, p ≤ .03. This time by group difference remained significant even after the control group completed intervention at 6 months follow-up, F(3, 10) = 3.40, p ≤ .04, because the intervention group continued to gain knowledge (see Figure 2). ANOVAs from the 3- to 6-month follow-up assessments showed significant gains in the intervention group, F(1, 6) = 10.46, p ≤.02, but not in the delayed treatment group, F(1, 8) = 4.10, p ≤ .10; however, there was a trend toward replication of the effects of the GoriLLA Group intervention on the COP for the delayed treatment group. Furthermore, time by group effects on the Social Thinking subscale, F(3, 10) = 3.29, p ≥ .07, approached significance, and the Self-Regulation subscale was significant, F(3, 10) = 6.54, p ≥ .01, when examined across all four time points. The Social Communication subscale did not demonstrate time by group effects over time. Time by group effects on the PROGO were not statistically significant at either the 3-month or the 6 month follow-up assessments.
Figure 2.
Mean Child Observation Protocol (COP) total score with trend lines by group across all four study time points.
Treatment Fidelity
Attendance
Most families attended between 10 and 11 (M = 10.75, SD = 1.49) of the 12 sessions; the number of absences ranged from none to four. Parents reported the reasons for absences were due to family and situational factors and events (e.g., vacation, illness, school program), not the intervention itself.
Adherence
With 100% rater agreement, the coded sessions adhered to the lesson plan with 95% accuracy. In addition, there was 100% compliance with the materials lists during the coded sessions. There were no significant differences found in mean adherence ratings between the two intervention groups, suggesting that, despite differing clinician teams, adherence to the curriculum was similar for both groups.
Clinician Quality
Quality ratings of “3” on the 5-point scale indicated a high level of clinician knowledge and implementation of the curriculum. Ratings higher than “3” indicated specific instances of going above and beyond this level of quality during the session. The mean quality rating across all rated sessions was 3.07 (SD = 0.13). Considering that this mean also reflects a mean quality rating over all activities within a session, this overall quality rating suggests a consistently high level of clinician knowledge and implementation of the GoriLLA Group curriculum during the study.
Clinician Behavior Management
Group member Behavior Management by the clinicians was rated on a 5-point scale. For this rating, a “5” indicates that either no undesirable behaviors occurred during the session or that behaviors were managed quickly and without any ongoing issue (e.g., needing to try more than one strategy or reminding the child of the strategy multiple times to manage the behavior). A “4” indicates a high level of Behavior Management wherein use of strategies by the clinician is effective for keeping the session going, but multiple efforts or strategies to manage those behaviors are needed. The overall mean behavior rating across all activities within the coded sessions was high at 4.76 (SD = 0.11), indicating a high level of Behavior Management on the part of clinicians when it was necessary during the rated sessions.
Discussion
This study examined the efficacy of a parent-assisted blended intervention program using components from Social Thinking and Structured TEACCHing to increase social communication and self-regulation concept knowledge in first and second graders diagnosed with ASD and their parents. Overall, the results of this study indicate that the GoriLLA Group intervention package demonstrates preliminary efficacy for teaching social communication and self-regulation concept knowledge to children with ASD and their parents. Both parents and children demonstrated an increase in social communication and self-regulation concept knowledge after participating in the GoriLLA Group as compared to a delayed treatment control group. Even when controlling for preintervention group differences in autism symptoms reported on the SCQ, effects of the child measure remained moderate, though they were not statistically significant. Furthermore, in applied written scenario responses, parents' use of intervention strategies and vocabulary increased from pre- to posttest, though results were not statistically significant.
The key ingredients of this blended intervention package included (a) the use of the Structured TEACCHing framework (environmental structure, visual supports), (b) the concrete social vocabulary and strategies of We Thinkers! Volume 1, (c) the self-regulation vocabulary and strategies from the Zones of Regulation, and (d) the use of parent assistance during activities. These ingredients combined to form a blended intervention package that is not only effective in increasing concept knowledge but also socially valid for those with ASD and their parents. Though the Social Thinking subscale was the only child measure (COP subscale) to reach statistical significance, both the Self-Regulation and Social Communication subscales had large effect sizes and approached statistical significance (ps = .06). Only the Self-Regulation subscale was statistically significant for the parent (PROGO) measure; yet, the effect sizes for the other subscales were moderate. These effects show promise for the key GoriLLA Group intervention package ingredients.
The effects of the GoriLLA Group intervention did not generalize to parent–child interactions during the semistructured set of activities that were part of the pre- and posttest assessment protocol. This is consistent with the lack of generalizability to peer interactions found in other social cognitive intervention studies (e.g., Bauminger, 2007). It is possible that the dosage of this 12-week intervention was inadequate to show generalization effects immediately following intervention. Considering that the significant changes seen on the COP and PROGO were primarily in the area of concept knowledge, rather than application of strategies, it is unlikely that application of strategies would generalize beyond the clinic setting after a 12-week intervention. An unanticipated finding from the coded parent–child interactions on the 3-Box Task was that Parent Detachment increased significantly from pre- to postassessments in the dyads that participated in the GoriLLA Group. One interpretation of this finding may be that parents who participated in the GoriLLA Group were more confident about their child's ability to regulate themselves while playing with toys and, as a result, demonstrated more detached parenting characteristics at posttest. Intervention group parents were also more comfortable in the building from attending weekly GoriLLA Group sessions and may have demonstrated more of their typical detached parenting behaviors (e.g., answering e-mails on their phone while their child played) than they would have at pretest or as compared to the control group parents who may have had the social motivation to impress the research team so that their child would receive intervention.
The time by group effects seen on the COP were consistent at the 3- and 6-month follow-up assessments, as were subscale results for Self-Regulation. Due to the parent-assisted nature of the intervention, we assume that parents continued to use the strategies and vocabulary from the GoriLLA Group at home, which allowed their children to continue to make gains relative to the control group, even after the control group received the intervention. The control group's gains on the COP were not significant from pre- (Time 3) to postintervention (Time 4); their mean unweighted total score change during intervention was 2.88 compared to 4.52 in the intervention group. It is possible that, since the control group demonstrated significantly fewer autism symptoms at the start of the study compared to the intervention group, they had less room for growth and made comparatively modest progress during the intervention. The time by group effects for the PROGO were not maintained at the follow-up assessments. Considering the small sample size, it is challenging to interpret these insignificant results, but further testing of this intervention with a larger sample size is warranted.
Results indicate that the GoriLLA Group is a socially valid blended intervention package for teaching social communication and self-regulation skills to early elementary school–age children with ASD. Overall, intervention group parents reported that they enjoyed the groups, found the content effective, and appreciated the opportunity to learn alongside other parents of children with ASD. Furthermore, fidelity data show that the GoriLLA Group was feasible for clinicians to implement each week at a high level of quality and behavior management, even with different clinical teams and practicum students working with each group.
Limitations
There were some limitations to this study. In order to complete the study in a community setting, some decisions that affected the rigor of the research protocol were made. First, the sample size, though it was the largest possible given the resources at the Chapel Hill TEACCH Center, was small and underpowered the analyses to detect effect sizes that were less than large. Though the clinical sample was representative of a “real-world” community sample at the Chapel Hill TEACCH Center and included some racial and ethnic diversity as well as four females with ASD, the small sample size prevented examination of racial, ethnic, or sex differences in treatment outcome. Some children in this study met the clinical ASD cutoff on the SCQ, and some did not, meaning that this sample may not be representative of other research samples of children with ASD. Moreover, all children in this study were mainstreamed in their school setting and reading on grade level. These were important research inclusion criteria to make sure that all children could understand the manualized treatment content; however, it is possible that minor modifications could be made for lower functioning children to benefit from the program. Ensuring that this intervention benefits as many individuals with ASD as possible and that modifications are made, when necessary, for various subpopulations within ASD is an important next research step.
Assessments were also affected by the community setting in which this study took place. Space, time, and clinic policies at the Chapel Hill TEACCH Center all had to be taken into consideration and limited the number of measures that could be included in the protocol (e.g., using the ADOS to confirm community diagnosis could not be accommodated). Although there was plenty of clinical space and time allotted for the usual four to five families seen for pre–post GoriLLA Group assessments clinically, tripling the number of assessments for the study put a strain on those resources. In order to get families in for assessments within a 3-week window at each time point, the majority of the research assessments took place during evenings and weekends.
Furthermore, the GoriLLA Group interventionists created both the parent and child measures based on their years of experience implementing the groups. Alternate measures of social communication and self-regulation were considered for use in this study, but no standardized measures that were likely to detect the changes in the core targets of the GoriLLA Group after a low-dosage, 12-week intervention period were available. The clinically developed measures were revised with pilot data to be more objective for research purposes, detect change over time, and establish reliable administration and scoring procedures, but strong psychometric properties were not established prior to use of these measures for research purposes. Though all of the psychometric data possible were collected and reported to aid in interpreting results of these measures, the use of validated measures as primary outcomes would strengthen the results of this study. Further research is needed with larger samples of children to further determine the psychometric properties of the COP and the PROGO.
Since the GoriLLA Group is a blended treatment model composed of two widely used curricula (Structured TEACCHing and two components of the Social Thinking Methodology: We Thinkers! Volume 1 vocabulary/concepts and the Zones of Regulation vocabulary/concepts), treatment contamination was another limitation of this study. Over half of the participants had some previous or current exposure to one of these curricula, although this is also a reflection of what happens in real-world clinical practice where children are often exposed to multiple interventions. Despite asking parents about their child's exposure to these curricula, it was difficult to ascertain the extent to which children had been exposed. Based on parent report in this sample, it seems that there is considerable variation both in services that claim to implement each of these curricula and in the extent to which what is taught in these curricula is communicated to parents. Therefore, controlling for previous exposure to these curricula was a challenge. Comparing the pretest COP scores of children whose parents reported previous exposure to Social Thinking and the Zones of Regulation to children whose parents did not report previous exposure yielded no significant differences; however, it is certainly possible that other children in the study had previous exposure to the GoriLLA Group concepts and vocabulary at school and in private therapy sessions of which their parents were not aware. In future studies, communicating with school and private interventionists may more accurately elucidate pretreatment exposure to these curricula.
Conclusions
In summary, this initial efficacy study suggests that significant changes in social communication and self-regulation knowledge in first and second graders with high-functioning ASD can be made and sustained in a low-intensity social cognitive community-based treatment.
Supplementary Material
Acknowledgments
This study was funded by a University of North Carolina Chapel Hill Community Engagement Fellowship awarded to Sallie Nowell. The work reported here was partially supported by the Institute of Education Sciences, U.S. Department of Education (Grants R324A100305 and R324B160038 awarded to The University of North Carolina at Chapel Hill). The opinions expressed represent those of the authors and do not represent views of the Institute or the U.S. Department of Education. We gratefully acknowledge the staff at the Chapel Hill TEACCH Center, especially our clinical research partners Katie Brady, Celeste Carter, and Linda Varblow, who created the GoriLLA Group; the graduate students who volunteered their time; and the families who participated in this research. We would also like to acknowledge Pamela Crooke and Michelle Garcia Winner for their generous collaboration and consultation regarding use of the Social Thinking methodology in this project.
Funding Statement
This study was funded by a University of North Carolina Chapel Hill Community Engagement Fellowship awarded to Sallie Nowell. The work reported here was partially supported by the Institute of Education Sciences, U.S. Department of Education (Grants R324A100305 and R324B160038 awarded to The University of North Carolina at Chapel Hill).
References
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed., DSM-5). Washington, DC: Author. [Google Scholar]
- Anderson D. K., Liang J. W., & Lord C. (2014). Predicting young adult outcome among more and less cognitively able individuals with autism spectrum disorders. The Journal of Child Psychology and Psychiatry, 55, 485–494. https://doi.org/10.1111/jcpp.12178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baio J., Wiggins L., Christensen D. L., Maenner M. J., Daniels J., Warren Z., … Dowling N. F. (2018). Prevalence of autism spectrum disorder among children aged 8 years—Autism and developmental disabilities monitoring network, 11 sites, United States, 2014. MMWR Surveillance Summaries, 67, 1–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnard-Brak L., Brewer A., Chesnut S., Richman D., & Schaeffer A. M. (2016). The sensitivity and specificity of the Social Communication Questionnaire for autism spectrum with respect to age. Autism Research, 9(8), 838–845. [DOI] [PubMed] [Google Scholar]
- Barnhill G. P. (2001). Social attributions and depression in adolescents with Asperger syndrome. Focus on Autism and Other Developmental Disabilities, 16(1), 46–53. [Google Scholar]
- Barrett P. (2005). Support materials for the FRIENDS program. Brisbane, Australia: Pathways Health and Research Centre. [Google Scholar]
- Bauminger N. (2007). Brief report: Group social-multimodal intervention for HFASD. Journal of Autism and Developmental Disorders, 37(8), 1605–1615. [DOI] [PubMed] [Google Scholar]
- Brady-Smith C., O'Brien C., Berlin L., Ware A., Fauth R. C., & Brooks-Gunn J. (1999). Early head start research and evaluation project: Child–parent interaction rating scales for the Three-Bag Assessment. New York, NY: National Center for Children and Families. [Google Scholar]
- Cain J. (2005). The way I feel. Seattle, WA: Parenting Press. [Google Scholar]
- Callahan K., Hughes H. L., Mehta S., Toussaint K. A., Nichols S. M., Ma P. S., … Wang H.-T. (2016). Social validity of evidence-based practices and emerging interventions in autism. Focus on Autism and Other Developmental Disabilities, 32(3), 188–197. https://doi.org/10.1177/1088357616632446 [Google Scholar]
- Carter C. V., & Brady K. (2016). Parent report of group outcomes (PROGO). Unpublished manuscript.
- Carter C. V., Varblow L., Brady K. & Woods (2016). Child Observation Protocol (COP). Unpublished manuscript.
- Carter S. L. (2010). The social validity manual: A guide to subjective evaluation of behavioral interventions. Boston, MA: Academic Press. [Google Scholar]
- Christensen D. L. (2016). Prevalence and characteristics of autism spectrum disorder among children aged 8 years—Autism and developmental disabilities monitoring network, 11 sites, United States, 2012. MMWR Surveillance Summaries, 65, 1–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cicchetti D. V., & Sparrow S. S. (1990). Assessment of adaptive behavior in young children.
- Cook J. (2007). Personal space camp. Chattanooga, TN: National Center for Youth Issues. [Google Scholar]
- Cox A., & AFIRM Team. (2018). Video modeling. Chapel Hill, NC: National Professional Development Center on Autism Spectrum Disorder, FPG Child Development Center, University of North Carolina; Retrieved from http://afirm.fpg.unc.edu/video-modeling [Google Scholar]
- Crooke P. J., Winner M. G., & Olswang L. B. (2016). Thinking socially: Teaching social knowledge to foster social behavioral change. Topics in Language Disorders, 36(3), 284–298. [Google Scholar]
- Dijkhuis R. R., Ziermans T. B., Van Rijn S., Staal W. G., & Swaab H. (2016). Self-regulation and quality of life in high-functioning young adults with autism. Autism, 21(7), 896–906. https://doi.org/10.1177/1362361316655525 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frankel F., Myatt R., Sugar C., Whitham C., Gorospe C. M., & Laugeson E. (2010). A randomized controlled study of parent-assisted children's friendship training with children having autism spectrum disorders. Journal of Autism and Developmental Disorders, 40(7), 827–842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gray K. M., Keating C. M., Taffe J. R., Brereton A. V., Einfeld S. L., Reardon T. C., & Tonge B. J. (2014). Adult outcomes in autism: Community inclusion and living skills. Journal of Autism and Developmental Disorders, 44(12), 3006–3015. [DOI] [PubMed] [Google Scholar]
- Gulsrud A. C., Jahromi L. B., & Kasari C. (2010). The co-regulation of emotions between mothers and their children with autism. Journal of Autism and Developmental Disorders, 40(2), 227–237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hendrix R., Palmer K., Tarshis N., & Winner M. (2013). The incredible flexible you: A social thinking curriculum for the preschool and early elementary years. Santa Clara, CA: Think Social Publishing. [Google Scholar]
- Hendrix R., Palmer K. Z., Tarshis N., & Winner M. G. (2016). We thinkers! Volume 2: Social problem solvers. Social Thinking Publishing. [Google Scholar]
- Howard K., Martin A., Berlin L. J., & Brooks-Gunn J. (2011). Early mother–child separation, parenting, and child well-being in Early Head Start families. Attachment & Human Development, 13(1), 5–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howlin P., Moss P., Savage S., & Rutter M. (2013). Social outcomes in mid-to later adulthood among individuals diagnosed with autism and average nonverbal IQ as children. Journal of the American Academy of Child & Adolescent Psychiatry, 52(6), 572–581. [DOI] [PubMed] [Google Scholar]
- Jahromi L. B., Bryce C. I., & Swanson J. (2013). The importance of self-regulation for the school and peer engagement of children with high-functioning autism. Research in Autism Spectrum Disorders, 7(2), 235–246. [Google Scholar]
- JMP Pro. (2014). Version 13.1. 0. SAS Institute: Cary, NC. [Google Scholar]
- Kazdin A. E. (1977). Assessing the clinical or applied significance of behavior change through social validation. Behavior Modification, 1, 427–452. [Google Scholar]
- Klinger L. G., Klinger M. R., & Pohlig R. L. (2007). Implicit learning impairments in autism spectrum disorders. In Pérez J. M., González P. M., Comí M. L., & Nieto C. (Eds.), . New developments in autism: The future is today (pp. 76–103). Philadelphia, PA: Jessica Kingsley Publishers. [Google Scholar]
- Kogan M. D., Vladutiu C. J., Schieve L. A., Ghandour R. M., Blumberg S. J., Zablotsky B., … Lu M. C. (2018). The prevalence of parent-reported autism spectrum disorder among US children. Pediatrics, 142(6), e20174161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuypers L. (2011). The zones of regulation. Santa Clara, CA: Think Social Publishing. [Google Scholar]
- Laugeson E. A., Frankel F., Gantman A., Dillon A. R., & Mogil C. (2012). Evidence-based social skills training for adolescents with autism spectrum disorders: The UCLA PEERS program. Journal of Autism and Developmental Disorders, 42(6), 1025–1036. [DOI] [PubMed] [Google Scholar]
- Laugeson E. A., Frankel F., Mogil C., & Dillon A. R. (2009). Parent-assisted social skills training to improve friendships in teens with autism spectrum disorders. Journal of Autism and Developmental Disorders, 39(4), 596–606. [DOI] [PubMed] [Google Scholar]
- Laurent A. C., & Gorman K. (2018). Development of emotion self-regulation among young children with autism spectrum disorders: The role of parents. Journal of Autism and Developmental Disorders, 48(4), 1249–1260. [DOI] [PubMed] [Google Scholar]
- Laurent A. C., & Rubin E. (2004). Challenges in emotional regulation in Asperger syndrome and high-functioning autism. Topics in Language Disorders, 24(4), 286–297. [Google Scholar]
- Lee L. C., David A. B., Rusyniak J., Landa R., & Newschaffer C. J. (2007). Performance of the Social Communication Questionnaire in children receiving preschool special education services. Research in Autism Spectrum Disorders, 1(2), 126–138. [Google Scholar]
- Living Words of Wisdom. (2014). Chair yoga. Retrieved from http://www.livingwordsofwisdom.com/chair-yoga.html
- Lopata C., Thomeer M. L., Volker M. A., Toomey J. A., Nida R. E., Lee G. K., … Rodgers J. D. (2010). RCT of a manualized social treatment for high-functioning autism spectrum disorders. Journal of Autism and Developmental Disorders, 40(11), 1297–1310. [DOI] [PubMed] [Google Scholar]
- Lord C., Rutter M., DiLavore P. C., Risi S., Gotham K., & Bishop S. (2012). Autism diagnostic observation schedule: ADOS. Los Angeles, CA: Western Psychological Services. [Google Scholar]
- Love J. M., Kisker E. E., Ross C., Raikes H., Constantine J., Boller K., … Vogel C. (2005). The effectiveness of early head start for 3-year-old children and their parents: Lessons for policy and programs. Developmental Psychology, 41(6), 885–901. [DOI] [PubMed] [Google Scholar]
- Mandelberg J., Frankel F., Cunningham T., Gorospe C., & Laugeson E. A. (2014). Long-term outcomes of parent-assisted social skills intervention for high-functioning children with autism spectrum disorders. Autism, 18(3), 255–263. [DOI] [PubMed] [Google Scholar]
- McAfee J. (2002). Navigating the social world. Arlington, TX: Future Horizons. [Google Scholar]
- Mesibov G. B., & Shea V. (2010). The TEACCH program in the era of evidence-based practice. Journal of Autism and Developmental Disorders, 40(5), 570–579. [DOI] [PubMed] [Google Scholar]
- Mesibov G. B., Shea V., & Schopler E. (2005). The TEACCH approach to autism spectrum disorders. New York, NY: Springer Science & Business Media. [Google Scholar]
- Mordre M., Groholt B., Knudsen A. K., Sponheim E., Mykletun A., & Myhre A. M. (2012). Is long-term prognosis for pervasive developmental disorder not otherwise specified different from prognosis for autistic disorder? Findings from a 30-year follow-up study. Journal of Autism and Developmental Disorders, 42(6), 920–928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nevill R. E., Lecavalier L., & Stratis E. A. (2018). Meta-analysis of parent-mediated interventions for young children with autism spectrum disorder. Autism, 22(2), 84–98. https://doi.org/10.1177/1362361316677838 [DOI] [PubMed] [Google Scholar]
- NICHD Early Child Care Research Network. (1999). Chronicity of maternal depressive symptoms, maternal sensitivity, and child functioning at 36 months. Developmental Psychology, 35, 1297–1310. [DOI] [PubMed] [Google Scholar]
- Palmer K. Z., Tarshis N., Hendrix R., & Winner M. G. (2016). We thinkers! Volume 2: Social problem solvers curriculum. Santa Clara, CA: Think Social Publishing. [Google Scholar]
- Rao P. A., Beidel D. C., & Murray M. J. (2008). Social skills interventions for children with Asperger's syndrome or high-functioning autism: A review and recommendations. Journal of Autism and Developmental Disorders, 38(2), 353–361. [DOI] [PubMed] [Google Scholar]
- Reichow B., & Volkmar F. R. (2010). Social skills interventions for individuals with autism: Evaluation for evidence-based practices within a best evidence synthesis framework. Journal of Autism and Developmental Disorders, 40(2), 149–166. [DOI] [PubMed] [Google Scholar]
- Reichow B., Volkmar F. R., & Cicchetti D. V. (2008). Development of an evaluative method for determining the strength of research evidence in autism. Journal of Autism and Developmental Disorders, 38, 1311–1318. [DOI] [PubMed] [Google Scholar]
- Reid R. (1996). Research in self-monitoring with students with learning disabilities: The present, the prospects, the pitfalls. Journal of Learning Disabilities, 29(3), 317–331. [DOI] [PubMed] [Google Scholar]
- Reid R., Trout A. L., & Schartz M. (2005). Self-regulation interventions for children with attention deficit/hyperactivity disorder. Exceptional Children, 71(4), 361–377. [Google Scholar]
- Rutter M., Bailey A., & Lord C. (2003). The Social Communication Questionnaire: Manual. Los Angeles, CA: Western Psychological Services. [Google Scholar]
- Schopler E., Lansing M., & Waters L. (Eds.). (1983). Teaching activities for autistic children. Austin, TX: Pro-Ed. [Google Scholar]
- Snow A. V., & Lecavalier L. (2008). Sensitivity and specificity of the Modified Checklist for Autism in Toddlers and the Social Communication Questionnaire in preschoolers suspected of having pervasive developmental disorders. Autism, 12(6), 627–644. [DOI] [PubMed] [Google Scholar]
- Stoesz B. M., Montgomery J. M., & MacKenzie H. (2013, May). Evaluation of executive function and autism characteristics in children with ASD participating in spark*. Poster presented at the International Meeting for Autism Research (IMFAR), Spain. [Google Scholar]
- Taylor J. L., & Seltzer M. M. (2011). Employment and post-secondary educational activities for young adults with autism spectrum disorders during the transition to adulthood. Journal of Autism and Developmental Disorders, 41(5), 566–574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Bourgondien M. E., & Coonrod E. (2013). TEACCH: An intervention approach for children and adults with autism spectrum disorders and their families. In Interventions for autism spectrum disorders (pp. 75–105). New York, NY: Springer. [Google Scholar]
- Vandell D. L. (1979). A microanalysis of toddlers' social interaction with mothers and fathers. The Journal of Genetic Psychology, 134(2), 299–312. [Google Scholar]
- Welsh M., Parke R. D., Widaman K., & O'Neil R. (2001). Linkages between children's social and academic competence: A longitudinal analysis. Journal of School Psychology, 39, 463–481. [Google Scholar]
- Winner M. G. (2013). Why teach social thinking? Questioning our assumptions about what it means to learn social skills. San Jose, CA: Think Social Publishing. [Google Scholar]
- Winner M. G., & Crooke P. (2009). Social thinking: A developmental treatment approach for students with social learning/social pragmatic challenges. SIG 1 Perspectives on Language Learning and Education, 16(2), 62–69. [Google Scholar]
- Winner M. G., & Crooke P. (2010). You are a social detective: Explaining social thinking to kids. Santa Clara, CA: Think Social Publishing. [Google Scholar]
- Wolf M. M. (1978). Social validity: The case for subjective measurement or how applied behavior analysis is finding its heart. Journal of Applied Behavior Analysis, 11, 203–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong C., Odom S. L., Hume K. A., Cox A. W., Fettig A., Kucharczyk S., … Schultz T. R. (2015). Evidence-based practices for children, youth, and young adults with autism spectrum disorder: A comprehensive review. Journal of Autism and Developmental Disorders, 45(7), 1951–1966. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.