Abstract
We describe the status of the COVID-19 epidemic in Vietnam, major response successes, factors that prompted implementation of certain public health actions, and the impact of these actions. In addition, information for three case studies is reported, with crucial learnings to inform future response. Findings from this study suggest that as early as 20 January 2020, Vietnam held a national risk assessment, established a national COVID-19 Response Plan and Technical Treatment and Care Guidelines, and prepared public health laboratories to accurately diagnose cases and hospitals to effectively treat patients. The first COVID-19 case was detected on 23 January. As of 30 September, there had been three waves of the COVID-19 epidemic totalling 1095 cases, and resulting in 35 deaths all among people with underlying health conditions. Evidence of potential transmission of SARS-CoV-2 from a commercial passenger flight inbound to Vietnam was reported. This study also highlights the importance of early technical preparedness, strong political commitment, multisectoral and multilevel efforts, increased resourcing and coordination towards an effective COVID-19 response. Controlling outbreaks in settings, such as crowded public places (bars and hospitals), within certain villages and over cities, required early detection, aggressive trace-test-quarantine efforts, a geographically extensive lockdown area and an adoption of several non-pharmaceutical interventions. Many low-income and middle-income countries have experienced their second or third wave of the COVID-19 epidemic, and they can learn from Vietnam’s response across the three epidemic waves. Swift governmental action, strict border control measures, effective communication of health promotion measures, widespread community engagement, expanded testing capacity and effective social measures to slow the spread of SARS-CoV-2, are highly important in these locations.
Keywords: public health, SARS, epidemiology
Summary box.
We present the COVID-19 epidemic in Vietnam and the country’s major response successes, factors that prompted implementation and impacts of public health actions.
Transmission of SARS-CoV-2 remains low in Vietnam, with a total of 1095 cases and 35 deaths by 30 September 2020, identified over three waves of the epidemic over the last 8 months.
Recommendations from this study are for the government to act rapidly, to enforce strict border control measures, to extensively engage the community, and to expand testing capacity.
Effective social protection measures have contributed to the success in halting the spread of SARS-CoV-2 in Vietnam.
With the possibility of epidemic resurgence, further enhanced preparedness and response efforts, increased resources and strengthened political will be required to end the epidemic.
Introduction
The emergence of SARS-CoV-2, the causative agent of COVID-19, is presenting unprecedented challenges.1 2 There have been significant successes to date in the development process of effective COVID-19 vaccines,3–5 drugs to treat symptoms6 and availability of neutralising antibodies.7 Nevertheless, strategies for preventing and controlling viral transmission still relies heavily on the practices of isolating cases, mandating quarantine for exposed persons, promoting physical distancing, improving handwashing measures and increasing use of masks in the community.8
Vietnam has been recognised as a country with extensively documented successes of SARS-CoV-2 control.9 Its early successes provide lessons that may be useful, particularly for low-income and middle-income countries to improve their COVID-19 response. The main aims of this study were to provide a summary of the status of the COVID-19 epidemic in Vietnam, highlight key response successes, examine factors that prompted implementation of certain public health actions and describe the impact of these actions. An additional aim was to describe responses of three case study outbreaks in crowded public places (a bar and a referral hospital), a village of Son Loi in northern Vietnam and the Da Nang region in central Vietnam. As the COVID-19 pandemic continues to grow, these lessons are essential to inform better preparedness, prevention and response in Vietnam and other settings.
The COVID-19 epidemic in Vietnam
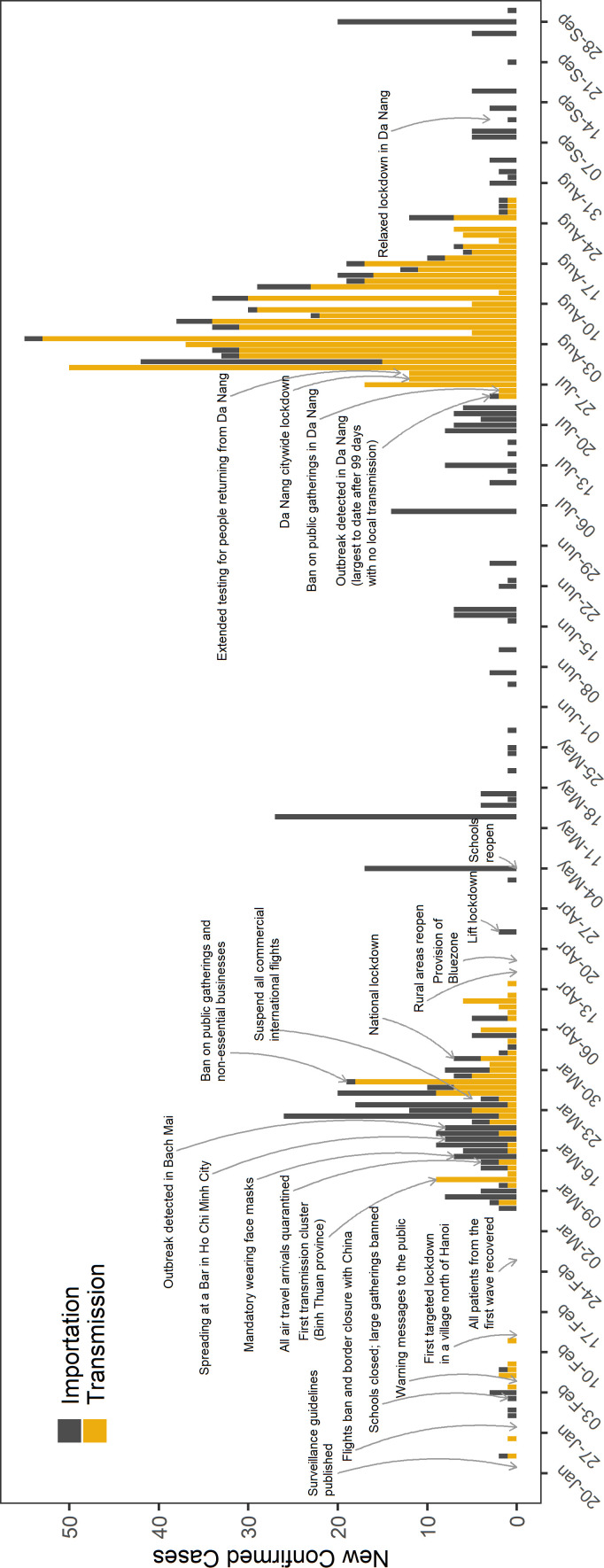
Vietnam’s first COVID-19 case was detected on 23 January 2020.10 As of 30 September, there were 1095 cases that resulted in 35 deaths all among people with underlying health conditions. There have been three waves of the COVID-19 epidemic in Vietnam, with increasing rates of transmission over time (figure 1). Early in the epidemic, transmission occurred following importation of cases through international commercial air travel. For instance, in early March, a Boeing 787–9 carrying 217 passengers and crew members flew for over 10 hours from London to Hanoi. A 26-year-old female passenger infected with SARS-CoV-2, having symptoms that lasted approximately 1 day before departure, likely transmitted first to twelve other passengers in the same business class cabin, two other passengers and a crew member in economic cabin, then three household contacts after arriving in Hanoi.11 Available data suggest that strains of SARS-CoV-2 isolated from seven other passengers and three household contacts showed a 99.98%–100.00% sequence similarity to the index case (analysis available on request). This demonstrates the extensive transmission potential for viral spread on airline travel.12 13 Another instance was of a 51-year-old female tourist who flew from Washington, District of Columbia, USA to Binh Thuan province located on the central coast of Vietnam, and who was later confirmed on landing to be infected with SARS-CoV-2. She was believed to be the source of infection of eight second-generation and two third-generation community cases. Over the course of the epidemic, the largest outbreak was seen in Da Nang, a tourist attraction city in central Vietnam. A total of 550 locally transmitted cases linked to this outbreak were detected from 23 July to 2 September.
Figure 1.
Trend of COVID-19 cases showing key response measures in Vietnam, January–September 2020. Cases are indicated by diagnosis data (n=1095).
Successes in the COVID-19 response in Vietnam
Health system preparedness
On 31 December 2019, WHO announced that a series of patients with pneumonia of unknown aetiology were reported in Wuhan, China.14 Vietnamese officials suspected that this abnormal pneumonia from China that was occurring around the Lunar New Year was similar to the 2003–2004 SARS outbreak. As a result, officials sensed a potential for emergence of a highly infectious and lethal disease. Therefore, only 7 days after this announcement, health system preparedness efforts were launched in Vietnam starting with a national risk assessment done on 7 January 2020. From this assessment, it was concluded that given the large volume of daily movement of populations between China and Vietnam that there was a high risk of this unknown disease being imported into Vietnam.
Based on lessons learnt from the outbreaks of SARS in 2003–2004,15 avian influenza in 2004–2005,16 and Zika virus17 in 2016, Vietnam coordinated a rapid response to address (unknown at the time) the novel epidemic caused by SARS-CoV-2. On 16 January, Vietnam’s health system managers and other associated ministries developed and widely disseminated a national COVID-19 Response Plan and Technical Treatment and Care Guidelines. From 20 January, hospitals across the country prepared to provide proper isolation, treatment and care for suspected and confirmed COVID-19 cases.18 Hospitals and satellite health centres in the northern, central and southern regions were selected by the Ministry of Health (MoH) to manage severe cases. Regional COVID-19 therapeutic task forces were established, and these groups were prepared for deployment by the MoH to provincial treatment sites. In view of an assumed increased infection risk among frontline medical staff as had been seen during the SARS outbreak,15 19personal protective equipment was stockpiled, and infection control measures were reinforced at hospitals. On 22 January, 1 day after the interim COVID-19 surveillance guidelines were published, a cluster of SARS-CoV-2 cases was identified within a familial group. A cascade of interventions, including proper isolation, prompt identification of movements and contacts of people from this family, and timely reporting and sharing of information was implemented to contain onward transmission.
COVID-19 prevention and control policies and strategies
One week after the first COVID-19 case was detected in Vietnam, the prime minister declared war on COVID-19 and mandated full implementation measures for the COVID-19 response. The statement, ‘saving lives is prioritised above consideration of the economic loss’, was released early by the Government of Vietnam. This implies that the government viewed the COVID-19 epidemic as a national emergency. Such a strategic perspective helped to illuminate the role of the political, governmental and social systems in the response.
The response to the crisis, overviewed by the prime minister, received strong support from political elites, including the general secretary of the Communist Party and the Chairwoman of the National Assembly. Of note, a clear strategic response structure was overlaid on the foundation of a one-party government, and the major response strategies and policies were made at the central level and executed through a top-down process. Specifically, governmental organisations at all three administrative tiers (central, provincial and district level) had already effectively worked together on joint health emergency response committees. These committees presented a unified executing and coordinating body at each geographical response level. Local government groups implemented the ‘Four onsites’ principle for onsite leadership, onsite human resources, onsite materials and supplies, and onsite logistics20 to control and prevent the COVID-19 spread in their geographical jurisdiction.
Border control measures
In early January, the MoH began enhancing border control measures to prevent importation of COVID-19 cases. Vietnam implemented a policy for taking passenger temperatures with non-contact thermometers at all international airports and at official land border crossings between China and Vietnam. All inbound passengers from China were required to complete a medical declaration form. From 21 March, electronic medical declaration forms were made mandatory for all passengers entering Vietnam to aid identification of suspected cases for testing and quarantine.
At border crossings, health officers assessed, identified, and separated passengers either with fever or those who disclosed a history of either fever, cough or shortness of breath or were exposed to a known COVID-19 patient in the past 2 weeks before arriving in Vietnam. At-risk passengers were transferred to a given designated hospital for a 14-day compulsory quarantine period, and nasopharyngeal and throat swabs were collected and tested for SARS-CoV-2. By the end of August, of the 710 arriving at-risk passengers, only one tested positive for SARS-CoV-2. Passengers without symptoms or exposure who arrived in Vietnam before 14 March received an information leaflet for reporting signs and symptoms of infection. These passengers were granted entry into the country, but were quarantined at their home or in their hotel and monitored daily for 14 days by health staff from local commune health stations. Those arriving in Vietnam after 14 March were subject to mandatory quarantine for 14 days in centralised facilities. The change in the quarantine policy was to limit the risk of case importations to Vietnam from a large volume of people returning to Vietnam from countries where the outbreaks were occurring. Until the end of August, the government of Vietnam covered the cost of quarantine for all passengers arriving in Vietnam. From September, passengers were accountable to cover costs associated with quarantine.
Effective 28 January, the prime minister banned all international flights to and from Wuhan and other affected areas in China, and closed all border crossings and transport lines between China and Vietnam (figure 1). Vietnam is the first Southeast Asian country to deny entry to new arrivals from China.21 As a result, substantial importation of cases through air travel was halted, greatly reducing onward transmission of SARS-CoV-2. Early travel restrictions that were implemented by mid-February helped slow the spread from other countries.22 In mid-March, visas were suspended for all foreigners for a period of 30 days. Hence, the number of incoming and outgoing international commercial flights were rapidly reduced, and from late March all international flights were suspended. Flight permits were only granted for diplomatic, official, repatriation and cargo purposes. From April to August, approximately 110 chartered flights had been operated to repatriate over 28 500 Vietnamese nationality, who were stranded in 75 countries and territories due to COVID-19 travel restrictions. In late September, international travel restrictions were lifted for countries with a low prevalence of COVID-19, namely Taiwan, Japan, Korea, China, Cambodia and Lao People’s Democratic Republic. Apart from air travel, train service between Vietnam and China was cancelled in early February. All land border crossings and transport lines with Lao People’s Democratic Republic and Cambodia were closed for 15 days in April to halt much of the cross-border movement. Given the occurrence of outbreaks on cruise ship voyages, since mid-March international seaports have not granted cruise ships permission to dock.23
COVID-19 testing
Samples have been collected from people at risk for SARS-CoV-2 infection. They are people who arrived in Vietnam and were suspected of SARS-CoV-2 infection, resided in outbreak areas, were close contacts of laboratory-confirmed cases, were exposed to persons from community-based or hospital-based outbreaks, and from passengers under quarantine in centralised facilities. Nasopharyngeal and throat swabs made up 85.8% of these samples and were tested for the presence of SARS-CoV-2 using real-time reverse transcription-PCR (RT-PCR). To ensure local testing supply needs, Vietnam produced a SARS-CoV-2 RT-PCR diagnostic kit, which received Conformité Européene certification in April. Other domestically developed diagnostic testing products, including primers and probes, and antibody tests, were also stockpiled. Staff training and technical assistance were provided to extend the testing laboratory network. By the end of September, over 120 laboratories across the country had SARS-CoV-2 testing capacity, up from only two laboratories as of late January.
Social measures
Isolation, contact tracing, and quarantine
In Vietnam, all people with laboratory-confirmed SARS-CoV-2 infection were immediately isolated in hospital. This practice is protected by law, as COVID-19 is classified as a group A infectious disease in Vietnam. This group includes diseases that are highly contagious, can cause outbreaks, and can be life threatening. For domestic cases, anyone who they were in contact with over the last 14 days were identified and interviewed by field investigation teams from provincial centres for disease control, district health centres and local governmental authorities. To improve the comprehensiveness of contact tracing, mobile phone numbers from all people who were infected were provided to public security officers to identify all places visited by these people over the past 14 days. There were two rounds of contract tracing per person (F1 and F2) with different testing and quarantine strategies (see box 1 and case study 1 for more details).
Box 1. Contact tracing, quarantine and testing of contacts.
The interim COVID-19 surveillance guidelines came into effect on 21 January 2020. Two rounds of contract tracing per person are described as follows.
Group F1—Close contacts of a case (F0). Defined as being close to a laboratory-confirmed case or a suspected case in an incubation period within 2 m (approximately 6 ft).
Close contacts are (1) household members; (2) colleagues from the same office; (3) contacts from a meeting, workshop or conference; contacts from tourist travel; (4) any passenger seated in the same row of seats or within two rows of a case for any form of public transportation (flights, trains and buses); (5) hospital staff who takes care of a confirmed infection.
These close contacts are subject to mandatory quarantine for 14 days at hospital or centralised quarantine facilities.
Two sets of swabs on day 1 and day 14 of quarantine are obtained from the nasopharynx and throat for SARS-CoV-2 testing, regardless of symptoms.
Group F2—Close contacts of group F1.
Required to self-monitor for symptoms and to home quarantine. If person they contacted from group F1 tested positive, this person is subsequently classified as group F1. Otherwise, the self-quarantine period is just completed.
In outbreaks of COVID-19 in the community and hospitals, in which local transmission occurred, nasopharyngeal and throat swabs were collected from group 2 for SARS-CoV-2 testing.
During the first 6 weeks of the epidemic, the MoH was primarily responsible for ensuring measures for case isolation and quarantine in hospital of close contacts. Military personnel were then deployed and facilities across the country were also used to quarantine all people entering Vietnam. Infected people remained in isolation until two consecutive nasopharyngeal and throat swabs collected 24-hours apart tested negative for SARS-CoV-2, and they were deemed clinically stable; the time lag between the two follow-up swabs during isolation was usually within a range of 1–2 days based on clinical conditions. All patients received free treatment, as the cost of treatment was covered by the National Health Insurance for Vietnamese citizens and through private insurance held by foreigners. Uninfected people in quarantine were tested twice for SARS-CoV-2 on days 1 and 14. They were released from quarantine if their nasopharyngeal and throat swabs remained negative on day 14.
Recommendations for masks usage and hand washing
Wearing masks, which was already normalised in many settings in Asia, has the potential to limit the spread of respiratory viruses, as shown in previous outbreaks.24 25 On 15 January, the MoH began recommending masks be worn for people coming in contact with a person having a respiratory illness. Initial studies suggest that SARS-CoV-2 is primarily transmitted through respiratory droplets, and the role of asymptomatic and pre-symptomatic viral transmission is important.26 27 Wearing a mask became mandatory in public places in Vietnam on 16 March. The public was further encouraged to wash their hands frequently and disinfect surfaces and objects to avoid fomite transmission of the virus.
In early August, following reports of an outbreak in Da Nang, mask usage was reported at levels of 90%. This was a significant increase from the 35% usage observed in late July. To enforce mask wearing in public, from November, the government fined those non-compliant 1–3 million Vietnam Dong (approximately US$43–US$129).
School closures and bans on public gatherings
SARS-CoV-2 was introduced into Vietnam just before the Tet or Vietnamese Lunar New Year holiday lasting from 23 January to 29 January, when schools and universities were closed across the country for holiday observance. During the period from February to March, academic lessons were broadcasted on television for high school students, first in Ho Chi Minh City (HCMC) and then in Hanoi. In late March, educational facilities turned to remote online learning platforms, with participation increasing over the academic year. Educational facilities remained closed until May 4, similar to measures taken in other Asian countries.28–30
With the increasing spread of outbreaks detected in the large cities of Hanoi and HCMC, a ban on indoor gatherings of 20 people or more and of 10 people or more in public places was issued in late March. Entertainment, cultural and sporting events held in public places were banned and non-essential businesses, including restaurants, bars, beauty salons, barbershops, hair salons, massage parlours, spas and gyms, were closed. A 2 m physical distancing was also recommended.
National lockdown
A prediction that widespread SARS-CoV-2 transmission could occur, would threaten individual and population health, and could subsequently exhaust Vietnam’s societal and economic systems led to implementation of nationwide lockdown recommendations from 1 April to 15 April. During the national lockdown, there was a stricter ban on public gatherings of more than two people outside of schools, hospitals or governmental agencies. A stay-home-order was issued, and people were only allowed to go outside for essential needs, such as buying groceries and medications or going to the emergency room. Employees of state agencies were recommended to work from home, except those providing essential services. A 1-week extension of the lockdown period was applied to 12 high-risk cities and provinces, such as Hanoi, Da Nang and HCMC. During that period, domestic travel by all modes of transport was banned, and non-essential services were shuttered. This strategy had a considerable negative impact on the economy and on the lives of citizens in Vietnam.31–33 To address this, the government offered a social protection package containing severance pay for workers who lost their jobs as result of the COVID-19 epidemic, allowance for individuals on social allowance and those from poor/near poor households, incentives for domestic business households, and tax breaks and interest rate cuts for companies affected by the epidemic. It was reported by the Ministry of Finance that by late-September 2020, about 12.65 million people received the social protection support, and the total expenditure for this programme was approximately US$540 million.
Other environmental factors
Vietnam has a typical tropical climate, with the average relative humidity of 65%–90% and the average annual temperature of 22–27°C (General Statistics Office of Vietnam, 2019). In Vietnam, motorbikes are the primary mode of transportation (88.5%), and approximately 0.4% of people used public transport (buses or taxis).34 A large proportion of the population (65%) in Vietnam live in rural areas and are thus rarely exposed to in crowded, poorly ventilated indoor environments (General Statistics Office of Vietnam, 2019). The meteorological, physiological, travel requirements and working conditions, together with implementation of the national lockdown in Vietnam, is not preferable for the intercommunity transmission of SARS-CoV-2.35 36
Roles of the media during the epidemic
Recognising the key role of the media during the epidemic, Vietnam disseminated their mid-term plan for communicating health risks for the 2020–2025 period, in January 2020. The plan includes a section for communicating strategies during a public health crisis, which has been used as the foundation for communication during the COVID-19 epidemic in Vietnam.
On 5 February, warning messages about the dangers and modes of transmission of COVID-19, as well as information on prevention measures were made publicly available through all media platforms. The national risk communication strategy has a focus on timeliness, transparency, precision and reliability of COVID-19 information to gain community involvement. The MoH, with support of leading telecoms and informatics technology companies, developed and launched a website (https://ncov.moh.gov.vn/) and applications to dissemination public health information around the epidemic. Two crucial applications were the electronic medical declaration application ‘NCOVI’ (https://ncovi.vnpt.vn/) and the contact tracing application ‘Bluezone’ (https://www.bluezone.gov.vn). A report of the Ministry of Information and Communication showed that as of August 2020, the Bluezone application was download by approximately 14.9 (14%) of 96.2 million people. By matching the movements of a user to that of all index (F0) individuals, Bluezone showed a risk notification as being in an F1 or F2 group, and suggested general technical guidance for the user.
The MoH sent information on the COVID-19 situation and key prevention measures to its citizens via mass text messaging (>27 billion) using major mobile service providers (Viettel, MobiFone, Vinaphone, etc) and several applications (Zalo, Viber, Lotus, TikTok, etc). In addition to the aforementioned website and applications, various communication campaigns were also disseminated on social media, television, the radio and in newspapers to educate the public on prevention measures. Messages were tailored to encourage people to adopt prevention behaviours, to define people at substantial risk of infection, and to guide people with symptoms or a history of exposure to access health services and to declare their status and get tested. Messaging was posted online in other languages, including English, French, Chinese and Korean, for non-Vietnamese speaking populations. Misleading online information around the COVID-19 outbreak was traced and retracted, and fines of 5–10 million Vietnam Dong (US$215–US$430) were issued.
Over the course of the epidemic, of note, medical record privacy was suspended for the benefit of improving population health in Vietnam. In most cases, only deidentified information on patient demographics and travel history were made publicly available on the MoH website, various newspapers and television. Ultimately, the goal of posting and broadcasting this information was to alert people of any potential case contact and of locations for testing. In a few circumstances, in early March, names of some COVID-19 cases were unintendedly posted, and this caused substantial social distress for those affected. Therefore, there is a need for a procedure securing personal data of cases developed and maintained during the response.
COVID-19 case studies
Case study 1: outbreaks in crowded public places
In mid-March, two outbreaks of COVID-19 occurred, one in a bar in HCMC37 and another in Bach Mai hospital in Hanoi.38 People from both facilities were promptly quarantined after domestic infections were confirmed.
Outbreak in a bar in HCMC
There was a citywide effort from health and security sectors to identify, and trace two rounds of contacts associated with this bar and to collect nasopharyngeal and throat swabs for testing. City officials identified suspected cases via direct contact tracing and mobile phone tracking, quarantined them in a government facility, and tested them for SARS-CoV-2. Of the 298 people who entered in this bar between 13 March and 17 March, most (256 people, 85.9%) were non-Vietnamese. At diagnosis, the index case, a British man, was critically ill, so his movements for the period 14 days prior to onset of the disease were publicised via several media platforms. The bar owner and city officials promptly posted information on the potential transmission event, a St. Patrick’s Day celebration held at bar on 14 March, on their websites. The contacts of the index case and bar attendees were encouraged to contact health facilities and to use the contract tracing application for completing their health declarations. Mobile phones of people who entered the bar over the outbreak period but did not contact local authorities were traced and sent a mobile text message through short message service requesting a prompt health declaration. In addition to the index case, 18 laboratory-confirmed cases, including four Vietnamese citizens and 14 foreigners with British, Brazil, Canadian and South African nationalities, were identified. Of the 18 cases, 12 people were believed to have acquired SARS-CoV-2 at the bar, and 6 of the 502 people from the F1 group with no visit to the bar were from onward transmission.37 A total of 4483 people within the F2 group were identified and quarantined at home.
There was a fear that public gatherings in HCMC would lead to rapid spread of SARS-CoV-2. Therefore, officials mandated closure of local entertainment facilities for approximately 3 weeks, from 24 March to 15 April. No new cases were identified after 6 April in HCMC and the outbreak was deemed under control. The HCMC’s response to this outbreak is consistent with findings from modelling studies showing the feasibility of controlling COVID-19 outbreaks through isolation, testing, contact tracing and physical distancing.39 40
This outbreak from this bar showed that several aspects were essential for a successful response to an outbreak of COVID-19 among non-Vietnamese speakers. These included the availability of online information with appropriate language on testing and treatment locations, effective contact tracing with assistance of interpreters and participation of local authorities. Establishment of bilingual hotlines in both Vietnamese and English can be an effective way to assess risk, to provide a forum for foreigners to request information on testing, and to prevent overcrowding at hospitals during an outbreak.
Outbreak in a referral hospital in Hanoi
The outbreak in Bach Mai hospital was publicised through various media channels. All citizens who had visited the hospital from 10 March to 20 March were requested to contact local health authorities to disclose their history of exposure and symptoms, for specimen collection for SARS-CoV-2 testing, and to quarantine at centralised centres for 14 days where indicated.38 More than 6200 health professionals and other staff members, 5900 hospital inpatients and 28 000 people who visited the affected hospital over this period were quarantined and tested. Health staff and inpatients were quarantined in hospitals. To meet testing needs, blood drawn from people in quarantine was tested for SARS-CoV-2 antibodies using rapid tests, while routine and monitoring swabs obtained from the nasopharynx and throat of suspected and confirmed cases were tested using RT-PCR. Contract tracing revealed two other epidemiologically linked outbreaks with 58 SARS-CoV-2 cases identified. Of these, 46 people were likely infected in hospital and 12 were from onward transmission. Of concern, however, was the high rate of failure to trace contacts linked to these cases (36 of 58 cases).
In late August, a student from Hai Duong (located in a neighbouring province of Hanoi) who had visited Hanoi for about 1 month, but had no symptoms and tested negative 1 day before departing for Tokyo, then tested positive for SARS-CoV-2 at Narita Airport. Taken together, this suggests that there had been a potential for community transmission in Hanoi.41 Further investigation is ongoing.
Additional response was that the affected hospital reduced overcrowding in their departments to limit a secondary transmission between hospital staff, patients and visitors. Specifically, the hospital transferred inpatients with stable conditions to other hospitals, suspended admissions of new patients to departments with COVID-19 patients, and limited patient admission to all other departments.38 People suffering from chronic diseases were prescribed therapeutic drugs for longer periods of time to reduce the number of hospital visits that had to be made to collect refills. Only patients with a severe illness or those needing emergency care were admitted to hospital. Field hospitals were also set up in HCMC in February and Hanoi in March to treat patients and prepare for and cope with COVID-19 patient overflow situations.
Case study 2: outbreaks in a village
In early February, a cluster of six secondary COVID-19 cases was identified from Son Loi commune, a rural community with 2774 households 40 km northwest of the capital Hanoi. This commune was promptly quarantined for 21 days. The response included house-to-house daily proactive searches to identify cases and their close contacts, expropriation of existing health facilities for isolation and quarantine, and dissemination of educational COVID-19 messages through health facility loudspeakers. A total of 422 epidemiological links to the six confirmed cases were identified.42 This localised outbreak was declared over after 3 weeks without any new cases identified. This targeted lockdown for houses, tower blocks or villages was consequently adopted in several provinces to contain communal spread of SARS-CoV-2.9 This suggests that along with conventional approaches for outbreak control, a targeted lockdown may be a promising intervention to prevent and control COVID-19 in areas with evidence of domestic infection in the community in the early wave of the outbreak. However, further research is warranted to confirm whether this was an effective approach.
Case study 3: outbreaks in the Da Nang region
Through existing systems to surveil patients with severe viral pneumonia, a domestic COVID-19 case was detected on 23 July at a hospital in Da Nang.43 General measures including bans on public gatherings, citywide physical distancing, restrictions on all travel and recommendations to wear masks, were promptly implemented in this city. Based on experience from the previous outbreak in Bach Mai hospital, the hospital was immediately locked down, and field hospitals were setup to take over service delivery. The difference in this city’s response was the extended contact tracing and testing at citywide level, with expert and equipment assistance from national agencies and other provinces. Influenced by the effective use of testing as an outbreak control strategy for South Korea,44 Da Nang extended its testing coverage and methods to maximise its yield for people at risk with or without signs and symptoms. Commune-level task forces were established to identify all residents who had experienced either fever, cough or dyspnoea. Pharmacies were requested to notify people with influenza-like illness or those who purchased fever medication. Suspected persons could quarantine at home, and their blood and nasopharyngeal samples collected were tested accordingly using domestically produced ELISA and RT-PCR diagnostic kits.
Another target population included 1.4 million travellers who visited Da Nang between 1 July and 28 July. Measures to triage this group required cooperation of health and governmental services to allocate appropriate resources, establish testing capacity and compel certain groups of people to undergo testing in all 62 other provinces. The travellers were encouraged to declare their health status using the NCOVI or Bluezone applications. Local governmental authorities further searched and identified travellers with no health declaration. People with respiratory illness were quarantined at health facilities, and their specimens were collected and tested for SARS-CoV-2. Healthy people could quarantine at home, and they were guided to visit a designated health facility for specimen collection and SARS-CoV-2 testing.
As of 2 September, more than 552 000 SARS-CoV-2 tests were conducted. A total of 389 cases were identified from Da Nang and 161 cases from 14 other provinces. Da Nang enrolled one person per household and tested nasopharyngeal and throat swabs of over 70 000 enrolees. No confirmed cases were found, and the outbreak was deemed over on 12 September.
Conclusion
Despite the absence of definite evidence that relatively low levels of transmission of SARS-CoV-2 in Vietnam can be attributed to interventions implemented, this study provides a summary of valuable success stories from Vietnam’s COVID-19 response for use by policy-makers and practitioners towards improving the response worldwide. Swift governmental action, strict border control measures, large community involvement, expanded testing capacity and effective social measures would have attributed to the success in halting the spread of SARS-CoV-2 in Vietnam. It is worth noting that differences in sociocultural environments, political structures and legal frameworks between Vietnam and other countries may pose a challenge to a widespread applicability of the measures reported herein. However, specific challenges for a given country should be identified in a timely manner and properly addressed to successfully promote health, prevent transmission and best respond to the COVID-19 pandemic.
With low local transmission of SARS-CoV-2, relaxation of the response has been observed in Vietnam, and society has moved to a ‘new normal’ status. This is seen as the way forward to balance between controlling measures and civil liberties during such epidemics. As a result of lifting social restrictions, several countries have faced the return of domestic transmission.45 46 This will be no exception for Vietnam, as new COVID-19 cases may continue to be detected. This reality demands a real-time passive COVID-19 surveillance system and new approaches to interventions to better cover large populations, enhanced preparedness and response efforts, increased resources, and strengthened political will to end the epidemic, to reduce pressure on healthcare systems until an effective vaccine is fully developed and administrated globally. Tackling the COVID-19 epidemic is a challenge for all countries. For many communities, countries and regions where the second or third wave of COVID-19 cases has just re-emerged, a rapid response is urgently needed.
Acknowledgments
We acknowledge those who have been involved in the COVID-19 response in every corner of the country of Vietnam. Without their dedication and hard work, this work could not have been completed. We would like to express our sincere thanks to our colleagues for their tremendous support and encouragement. We also thank Dr Assaf Oron with the Institute for Disease Modelling for assistance with a figure and Dr Sherrie Kelly with the Burnet Institute for valuable comments and assistance with English language editing prior to submission.
Footnotes
Handling editor: Seye Abimbola
TVN and QDT contributed equally.
Contributors: TN, QDT and QDP conceived the study, collected data, interpreted the data and wrote the first draft of the manuscript. QDT and LNV collected and interpreted policies and epidemiological data. DTTT, HCT, LDKV, TNL and TVN collected and managed data about policies and responses. PTL and QCL assisted in the interpretation of findings, reviewed the manuscript, and contributed critical revision of the manuscript. PTL sought the research grant. All authors have approved the final version.
Funding: This work was granted by Vietnam’s Ministry of Science and Technology (grant number: 32/20-ĐTĐL.CN-CNN).
Disclaimer: The findings and conclusions in this publication are those of the authors and do not necessarily represent the official position of the Government of Vietnam, the Ministry of Health, the General Department of Preventive Medicine, and the Pasteur Institute of Ho Chi Minh City.
Competing interests: None declared.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data are available from the corresponding author by request.
References
- 1.Zhu N, Zhang D, Wang W, et al. . A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med 2020;382:727–33. 10.1056/NEJMoa2001017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization WHO Director-General’s opening remarks at the media briefing on COVID-19, 2020. Available: https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19-11-march-2020 [Accessed 10 Sept 2020].
- 3.Mahase E. Covid-19: Moderna vaccine is nearly 95% effective, trial involving high risk and elderly people shows. BMJ 2020;371:m4471 10.1136/bmj.m4471 [DOI] [Google Scholar]
- 4.Mahase E. Covid-19: Vaccine candidate may be more than 90% effective, interim results indicate. BMJ 2020;371:m4347. 10.1136/bmj.m4347 [DOI] [PubMed] [Google Scholar]
- 5.Kemp A. AZD1222 vaccine met primary efficacy endpoint in preventing COVID-19. Available: https://www.astrazeneca.com/media-centre/press-releases/2020/azd1222hlr.html [Accessed 26 Nov 2020].
- 6.Beigel JH, Tomashek KM, Dodd LE, et al. . Remdesivir for the Treatment of Covid-19 - Final Report. N Engl J Med 2020;383:1813–26. 10.1056/NEJMoa2007764 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chen P, Nirula A, Heller B, et al. . SARS-CoV-2 neutralizing antibody LY-CoV555 in outpatients with Covid-19. N Engl J Med 2020:NEJMoa2029849. 10.1056/NEJMoa2029849 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wilder-Smith A, Freedman DO. Isolation, quarantine, social distancing and community containment: pivotal role for old-style public health measures in the novel coronavirus (2019-nCoV) outbreak. J Travel Med 2020;27:taaa020. 10.1093/jtm/taaa020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pollack P, Thwaites G, Rabaa M. Emerging COVID-19 success story: Vietnam’s commitment to containment, 2020. Available: https://ourworldindata.org/covid-exemplar-vietnam [Accessed 10 Sept 2020].
- 10.Phan LT, Nguyen TV, Luong QC, et al. . Importation and human-to-human transmission of a novel coronavirus in Vietnam. N Engl J Med 2020;382:872–4. 10.1056/NEJMc2001272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Khanh NC, Thai PQ, Quach H-L, et al. . Transmission of SARS-CoV 2 during long-haul flight. Emerg Infect Dis 2020;26:2617–24. 10.3201/eid2611.203299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bae SH, Shin H, Koo H-Y, et al. . Asymptomatic transmission of SARS-CoV-2 on evacuation flight. Emerg Infect Dis 2020;26:2705–8. 10.3201/eid2611.203353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hoehl S, Karaca O, Kohmer N, et al. . Assessment of SARS-CoV-2 transmission on an international flight and among a tourist group. JAMA Netw Open 2020;3:e2018044 10.1001/jamanetworkopen.2020.18044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.World Health Organization Pneumonia of unknown cause – China. Available: https://www.who.int/csr/don/05-january-2020-pneumonia-of-unkown-cause-china/en/ [Accessed 8 Apr 2020].
- 15.Ohara H. Experience and review of SARS control in Vietnam and China. Trop Med Health 2004;32:235–40. 10.2149/tmh.32.235 [DOI] [Google Scholar]
- 16.Hien TT, de Jong M, Farrar J. Avian influenza--a challenge to global health care structures. N Engl J Med 2004;351:2363–5. 10.1056/NEJMp048267 [DOI] [PubMed] [Google Scholar]
- 17.Nguyen DT, Do HT, Le HX, et al. . Zika preparedness and response in Viet Nam. Western Pac Surveill Response J 2018;9:1–3. 10.5365/wpsar.2018.9.1.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pham QT, Rabaa MA, Duong HL, et al. . The first 100 days of SARS-CoV-2 control in Vietnam. Clin Infect Dis 2020:ciaa1130. 10.1093/cid/ciaa1130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nishiyama A, Wakasugi N, Kirikae T, et al. . Risk factors for SARS infection within hospitals in Hanoi, Vietnam. Jpn J Infect Dis 2008;61:388–90. [PubMed] [Google Scholar]
- 20.Joint Advocacy Network Initiative (JANI) Four on-the-spot motto in disaster management. Available: https://www.preventionweb.net/files/13235_13235FouronthespotMotto1.pdf [Accessed 26 Nov 2020].
- 21.Singapore Ministry of Health Extension of precautionary measures to minimise risk of community spread in Singapore:. Available: https://www.moh.gov.sg/news-highlights/details/extension-of-precautionary-measures-to-minimise-risk-of-community-spread-in-singapore [Accessed 13 Sept 2020].
- 22.Chinazzi M, Davis JT, Ajelli M, et al. . The effect of travel restrictions on the spread of the 2019 novel coronavirus (COVID-19) outbreak. Science 2020;368:395–400. 10.1126/science.aba9757 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Moriarty LF, Plucinski MM, Marston BJ, et al. . Public health responses to COVID-19 outbreaks on cruise ships - Worldwide, February-March 2020. MMWR Morb Mortal Wkly Rep 2020;69:347–52. 10.15585/mmwr.mm6912e3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Leung NHL, Chu DKW, Shiu EYC, et al. . Respiratory virus shedding in exhaled breath and efficacy of face masks. Nat Med 2020;26:676–80. 10.1038/s41591-020-0843-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lau JTF, Tsui H, Lau M, et al. . Sars transmission, risk factors, and prevention in Hong Kong. Emerg Infect Dis 2004;10:587–92. 10.3201/eid1004.030628 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tong Z-D, Tang A, Li K-F, et al. . Potential presymptomatic transmission of SARS-CoV-2, Zhejiang Province, China, 2020. Emerg Infect Dis 2020;26:1052–4. 10.3201/eid2605.200198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pan X, Chen D, Xia Y, et al. . Asymptomatic cases in a family cluster with SARS-CoV-2 infection. Lancet Infect Dis 2020;20:410–1. 10.1016/S1473-3099(20)30114-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wu Z. Outbreak of COVID-19 in China and the country’s responses. Retroviruses and Opportunistic Infections (CROI) 2020: special session SS-1: International Antiviral Society–USA, 2020. [Google Scholar]
- 29.Kwok KO, Li KK, Chan HHH, et al. . Community responses during early phase of COVID-19 epidemic, Hong Kong. Emerg Infect Dis 2020;26:1575–9. 10.3201/eid2607.200500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Government of Korea COVID-19, testing time for resilience: in recovering from COVID-19: Korean experience. Available: https://www.preventionweb.net/publications/view/71638 [Accessed 10 Sept 2020].
- 31.Hamadani JD, Hasan MI, Baldi AJ, et al. . Immediate impact of stay-at-home orders to control COVID-19 transmission on socioeconomic conditions, food insecurity, mental health, and intimate partner violence in Bangladeshi women and their families: an interrupted time series. Lancet Glob Health 2020;8:e1380–9. 10.1016/S2214-109X(20)30366-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ahmed SAKS, Ajisola M, Azeem K, et al. . Impact of the societal response to COVID-19 on access to healthcare for non-COVID-19 health issues in slum communities of Bangladesh, Kenya, Nigeria and Pakistan: results of pre-COVID and COVID-19 lockdown stakeholder engagements. BMJ Glob Health 2020;5:e003042. 10.1136/bmjgh-2020-003042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Fezzi C, Fanghella V. Real-time estimation of the short-run impact of COVID-19 on economic activity using electricity market data. Environ Resour Econ 2020:1–16. 10.1007/s10640-020-00467-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chu MC, Nguyen LX, Ton TT, et al. . Assessment of motorcycle ownership, use, and potential changes due to transportation policies in Ho Chi Minh City, Vietnam. J Transp Eng A Syst 2019;145:05019007. 10.1061/JTEPBS.0000273 [DOI] [Google Scholar]
- 35.Sajadi MM, Habibzadeh P, Vintzileos A, et al. . Temperature, humidity, and latitude analysis to estimate potential spread and seasonality of coronavirus disease 2019 (COVID-19). JAMA Netw Open 2020;3:e2011834. 10.1001/jamanetworkopen.2020.11834 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Nishiura H, Oshitani H, Kobayashi T. Closed environments facilitate secondary transmission of coronavirus disease 2019 (COVID-19). medRxiv 2020. [Google Scholar]
- 37.Chau NVV, Hong NTT, Ngoc NM, et al. . Superspreading event of SARS-CoV-2 infection at a bar, Ho Chi Minh City, Vietnam. Emerg Infect Dis 2021;27:310–4. 10.3201/eid2701.203480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Duy C, Nong VM, Van Ngo A, et al. . Nosocomial coronavirus disease outbreak containment, Hanoi, Vietnam, March-April 2020. Emerg Infect Dis 2021;27:10–17. 10.3201/eid2701.202656 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hellewell J, Abbott S, Gimma A, et al. . Feasibility of controlling COVID-19 outbreaks by isolation of cases and contacts. Lancet Glob Health 2020;8:e488–96. 10.1016/S2214-109X(20)30074-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kucharski AJ, Klepac P, Conlan AJK, et al. . Effectiveness of isolation, testing, contact tracing, and physical distancing on reducing transmission of SARS-CoV-2 in different settings: a mathematical modelling study. Lancet Infect Dis 2020;20:1151–60. 10.1016/S1473-3099(20)30457-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.University of Sydney National Hospital for Tropical Diseases, Woolcock Institute of Medical Research, Indo-Pacific Center for Health Security. COVID-19 sero-prevalence survey. Available: https://infogram.com/eng-covid-19-serology-survey-1h0r6rppzxpll2e?live [Accessed 25 Dec 2020].
- 42.Thanh HN, Van TN, Thu HNT, et al. . Outbreak investigation for COVID-19 in northern Vietnam. Lancet Infect Dis 2020;20:535–6. 10.1016/S1473-3099(20)30159-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Vuong NM, Le Quyen NT, Tra DT, Nong VM, Le Thi Nguyen Q, Doan TT, et al. . The second wave of COVID-19 in a tourist hotspot in Vietnam. J Travel Med 2020:taaa174. 10.1093/jtm/taaa174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kim YJ, Sung H, Ki C-S, et al. . COVID-19 testing in South Korea: current status and the need for faster diagnostics. Ann Lab Med 2020;40:349–50. 10.3343/alm.2020.40.5.349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Xu S, Li Y. Beware of the second wave of COVID-19. Lancet 2020;395:1321–2. 10.1016/S0140-6736(20)30845-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Strzelecki A. The second worldwide wave of interest in coronavirus since the COVID-19 outbreaks in South Korea, Italy and Iran: a Google trends study. Brain Behav Immun 2020;88:950–1. 10.1016/j.bbi.2020.04.042 [DOI] [PMC free article] [PubMed] [Google Scholar]