Abstract
Aim
To establish the effect of a single‐brushing exercise on dental plaque removal using an oscillating‐rotating power toothbrush (OR‐PTB) as compared to a high‐frequency sonic power toothbrush (HFS‐PTB).
Materials and Methods
The MEDLINE‐PubMed and Cochrane‐CENTRAL databases were searched up to September 2019. The inclusion criteria contained (randomized) controlled clinical trials involving healthy adult participants brushing with an OR‐PTB as compared to an HFS‐PTB. Plaque index (PI) scores were evaluated after a single‐brushing exercise.
Results
A total of 15 publications were included, representing 34 comparisons, of which 8 were professional brushing exercises and 26 participant brushing exercises. The potential risk of bias was estimated to be low. In the overall descriptive analysis of 34 comparisons, 19 comparisons showed a statistically significant difference in favour of the OR‐PTB and 4 in favour of the HFS‐PTB. The meta‐analysis using the professional brushing study design showed a significant difference of means (DiffM) in favour of the OR‐PTB (PI score) (DiffM 0.19; P < .0001) (95% CI [013; 0.25]). In those studies where the participants brushed themselves, the data were inconclusive. PI scores showed no difference between the two brushes (P = .15), while one plaque index (the Rustogi Modified Navy plaque index) indicated significant favour for the OR‐PTB (DiffM 0.06; P = .002) (95% CI [0.02; 0.09]).
Conclusion
Based on the estimated evidence profile, there is moderate certainty of evidence of a very small but significant beneficial effect on plaque removal after a single‐brushing exercise with the OR‐PTB over the HFS‐PTB.
Keywords: dental plaque, oscillating‐rotating toothbrush, power toothbrush, power toothbrush, single brushing, sonic toothbrush, systematic review
1. INTRODUCTION
Dental plaque biofilm‐induced gingival inflammation is defined as “an inflammatory lesion resulting from interactions between the dental plaque biofilm and the host's immune‐inflammatory response.” 1 Management of gingival inflammation is both a primary prevention strategy for periodontitis and a secondary prevention strategy for recurrent periodontitis. Prevention has become the cornerstone of the modern dental practice, and plaque control through effective personal oral hygiene is the key to preventive dentistry. 2 Therefore, professional oral hygiene instruction results in reducing dental plaque and gingival inflammation. Toothbrushing is universally recommended as a primary means of personal oral care. 2 Effective removal of plaque from the tooth surfaces by brushing is well known to have a significant impact on the prevention of oral diseases. 3 However, the effect of toothbrushing depends on a number of factors, including motivation, understanding and manual dexterity. Different types of toothbrushes are available and can be distinguished between manual (MTB) and power (PTB) toothbrushes. When the electric toothbrush was introduced, it had at a brush head comparable to a regular MTB capable of a variety of motions and driven by a power source. Over time, new technologies have improved their efficacy, and PTBs have become established as a valuable alternative to a manual toothbrush (MTBs). 4 Since the 1990s, PTBs have become a common household device for oral hygiene 5 in Western society. Due to their cleaning performance and user‐friendly practicability, PTBs are becoming more and more widely distributed. 6
A previously published systematic review has determined the efficacy of plaque removal following a single‐brushing exercise using a PTB 7 to be on average 46%. The available evidence indicated that the power supply was a rechargeable or replaceable battery. The modes of action, as well as brushing duration and type of instructions, were factors which contributed to the variation in the observed efficacy. 7 A more recent systematic review evaluated direct comparisons of MTBs vs PTBs in single‐brushing exercises and showed that there is a moderate certainty that the PTB was more effective independent of the plaque index score used. 8
A recently published study assessed the 11‐year longitudinal effects of PTBs on periodontal clinical parameters in an adult population. 9 Over the longer term, significant benefits were seen in both mild and moderate periodontitis for PTBs as compared to MTBs. However, there was no differentiation 12 and based on the PTB mode of action, for instance oscillating‐rotating power toothbrushes (OR‐PTB) or high‐frequency sonic power toothbrushes (HFS‐PTB). From the sub‐analysis in the recent systematic review, 8 it appeared that both OR‐PTB and HFS‐PTB modes of action are more effective than MTB. These two PTBs are globally the most frequently sold and researched PTBs. A direct comparison concerning the efficacy of plaque removal by these PTB systems is of interest and often discussed. A Cochrane systematic review from almost a decade ago evaluated the direct comparison between the different modes of action of PTBs for plaque reduction, as well as the health condition of the tissue surrounding the teeth. 10 No definitive conclusions could be drawn regarding the superiority of one type over another. The authors found some evidence that OR‐PTBs reduce plaque and gingivitis more than HFS‐PTBs in the short term. However, this difference was small, and the clinical importance is unclear. 10
Recently, two systematic reviews 11 , 12 have been published on the effect of PTBs with an OR vs a HFS mode of action. However, one review was based on data published from 2007 to 2017 and limited to RCTs involving OR toothbrushes from a single manufacturer. 11 The other review only included RCTs published from January 2009 through March 2019. 12 Currently, no systematic review has included data from the days of the development of the PTBs till the present, which prompted the need for a systematic review of the literature to evaluate the effect of single brushing studies of PTBs with an OR‐PTB vs an HFS‐PTB mode of action on plaque removal.
2. MATERIALS AND METHODS
This systematic review and meta‐analysis were prepared and reported in accordance with the Cochrane Handbook for Systematic Reviews of Interventions, which provides guidance for the preparations. In addition, the guidelines of Transparent Reporting of Systematic Reviews and Meta‐analyses 13 , 14 , 15 and Assessing the Methodology Quality of Systematic Reviews 16 , 17 were followed. The protocol for this systematic review was developed “a priori” and registered with the International Prospective Register of Systematic reviews 18 under registration number CRD42020160957.
2.1. Focused question
What is the effect of an OR‐PTB as compared to a HFS‐PTB on dental plaque removal after a single‐brushing exercise in healthy participants?
2.2. Search strategy
A structured search strategy was designed to include any relevant publications that evaluated the effect of the two PTBs on dental plaque removal after a single‐brushing exercise in a direct comparison. For the comprehensive search strategy, electronic databases were queried to search for appropriate papers that satisfied the study purpose. The National Library of Medicine, Washington, DC (MEDLINE‐PubMed), EMBASE and the Cochrane Central Register of Controlled Trials (CENTRAL) were used to detect appropriate publications. A systematic electronic search was conducted up to September 2019. The search strategy, including the employed search terms, is presented in Table 1. All references cited in the papers that were selected for this review were checked for additional studies. Hand searching was performed as part of the Cochrane Worldwide Hand Searching Program and uploaded to CENTRAL.
Table 1.
Search terms used for the search strategy
| The following strategy was used in the search: {(intervention) AND (specification)} |
|
{(<Intervention:> Toothbrush* OR "Toothbrushing"[Mesh]) AND (<specification:> power* OR electric*)} |
The asterisk (*) was used as a truncation symbol.
2.3. Screening and selection
Titles and abstracts of studies obtained from the searches conducted were screened by two independent reviewers (NLHH and EVDS) using the Rayyan 19 , 20 web application. Possible duplicates were indicated and checked by two reviewers to eliminate those that were identical. Disagreements in the screening and selection process were resolved by consensus or if a disagreement persisted, by arbitration through a third reviewer (DES). Titles and abstracts were read in detail to screen for suitability. The reviewers worked independently and were blinded from each other's results during the screening process. Titles and abstracts were categorized as included, excluded or undecided. Once the list of included titles and abstracts was obtained, full‐text versions were retrieved and screened for suitability. After the independent screening process, the search was unblinded, and the conflicts that were identified by Rayyan 19 were resolved by the reviewers.
The eligibility criteria were as follows:
Publications written in the English language
(Randomized) controlled clinical trials (CCT or RCT)
-
Studies conducted in humans
≥18 years old
In good general health, which means no systemic disorders
Without orthodontic fixed appliances
Intervention: a high‐frequency sonic power toothbrush (HFS‐PTB)
Comparison: an oscillating‐rotating power toothbrush (OR‐PTB)
single‐brushing exercise (pre‐ and post‐measurements)
Brushed by the participant or by a professional
Clinical evaluation parameter: plaque index scores
2.4. Heterogeneity assessment
The heterogeneity of the plaque index scores across studies was detailed according to the following factors:
Study design and participants’ characteristics
Study procedures and study products
Plaque indices and modifications
To evaluate methodological heterogeneity, the study design and toothbrushing regimens were evaluated. When clinical or methodological heterogeneity was considered as high across studies, sources of heterogeneity were explored by performing subgroup analyses and sensitivity analyses.
2.5. Risk of bias assessment
Two reviewers (NLHH and DES) individually scored the methodological qualities of the included studies according to the method described by Van der Weijden et al (2009) 4 and in further detail by Keukenmeester et al (2012). 21 The study was classified as having an estimated low risk of bias when random allocation, defined eligibility criteria, masking of examiners, masking of patients, balanced experimental groups, identical treatment between groups (except for the intervention) and reporting of follow‐up were present. When one of these seven criteria was missing, the study was considered to have an estimated moderate risk of bias. 21 When two or more of these criteria were missing, the study was estimated to have a high risk of bias. Additionally, five ethical aspects were introduced to estimate the potential conflict of interest, for example reported funding or a declared (or absent) conflict of interest. The potential risk of bias was estimated, and the acquired evidence was graded. Disagreements in the quality assessments were resolved by consensus or if disagreement persisted, by arbitration through a third reviewer (GAW).
2.6. Statistical analysis
2.6.1. Data extraction
The data from the publications that met the selection criteria were extracted and processed for further analysis. Two reviewers (EVDS and NLHH) evaluated the selected publications for mean baseline, end and difference scores, and standard deviation (SD). To ensure an accurate estimate, any data approximation in figures was avoided. Some of the studies provided a standard error (SE) of the mean. These values were converted to standard deviations (SD) based on the sample size (SE = SD/√N). Numbers with three digits were rounded to two digits. In the case of missing data or undetermined information, attempts were made to contact the first or corresponding author of the included publications for clarification or to retrieve additional data. For studies that had multiple treatment arms and those in which data from the control group were compared with more than one other group, the number of participants (N) in the control group was divided by the number of comparisons. Disagreements in the data extraction were resolved by consensus or if disagreement persisted, by arbitration through a third reviewer (DES) data extraction.
2.6.2. Data analysis
Descriptive analysis
The data were summarized and analysed using vote counting. 22 A descriptive data presentation was used for the included studies to give an overview of the results. The clinical parameter of interest was plaque index (PI).
Meta‐analysis
When appropriate, a meta‐analysis was performed, and the difference of means (DiffM) was calculated using an inverse variance method in Review Manager (RevMan [Computer program] Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014), 23 with either the fixed or random effects model, as appropriate. For the analysis, the assumption was made that summary data were missing at random; thus, all available data were included. Data were separated per index being the Modified Silness and Löe plaque index, 24 , 25 , 26 the Modified Quigley and Hein plaque index, 27 , 28 , 29 and the Rustogi Modified Navy plaque index. 30 Subgroup analyses were performed based on professional brushing and participant brushing. Heterogeneity was tested using the chi‐square test and the I 2 statistic. 31 A chi‐square test resulting in a P‐value < .1 was considered to be an indication of significant statistical heterogeneity. As an approximate guide for assessing the degree of inconsistency across studies, an I 2 statistic of 0%‐40% was interpreted as might not be important, a statistic of 40%‐60%% as possibly representing moderate heterogeneity, 60%‐80% as possibly representing substantial heterogeneity and 80%‐100% as possibly representing considerable heterogeneity. 32
Publication bias
If the meta‐analysis comprised sufficient trials to make visual inspection of the plot meaningful (10 trials minimum), funnel plots were used as a formal detection for assessment of publication bias. The presence of asymmetry in the inverted funnel may suggest a systematic difference between large and small trials in their estimates of treatment effects as a potential bias. 33
Additional analysis
Trial sequential analysis (TSA) is a cumulative random effects meta‐analysis method that estimates a required information size (RIS) (ie required meta‐analysis sample size) using the same framework as sample size calculation for an individual RCT but additionally accounting for heterogeneity and multiple comparisons when new RCTs are added. The Lan‐DeMets version 34 of the O’Brien‐Fleming function 35 was used for calculating the trial sequential monitoring boundaries (TSMBs). TSA software version 0.9.5.10 Beta (Copenhagen Trial Unit) was used. 36 , 37 , 38 , 39
Distribution‐based methods were used in order to determine the clinical relevance of study results. 40 , 41 , 42 , 43 , 44 Using the distribution‐based method, the clinical relevance was scored as not clinically relevant, potentially clinically relevant or clinically relevant based on the relationship among the mean difference of the variable, minimal important difference (MID) and effect size (ES). 44 An effect size of 0.20 (0.0‐0.39) was interpreted as small, 0.50 (0.40‐0.79) as medium and ≥0.80 as large. The MID was determined by multiplying the effect size of the difference between groups by the pooled baseline standard deviation of the two groups. 40 The MID was calculated by multiplying either 0.2 or 0.5 with the pooled baseline standard deviation. 42
2.7. Grading the body of evidence
The Grading of Recommendations Assessment, Development and Evaluation system, as proposed by the GRADE working group, was used to rank and grade the evidence emerging from this review. 45 , 46 Two reviewers (GAW and DES) rated the certainty of the evidence, as well as the strength and direction of the recommendations, according to the following aspects: risk of bias of the individual studies, consistency and precision among the study outcomes, directness of the study results and detection of publication bias. Any disagreement between the two reviewers was resolved after an additional discussion with the third reviewer (EVDS).
3. RESULTS
3.1. Search and selection results
Figure 1 shows the search and selection of the included publications. Out of the unique titles and abstracts, there were 14 conflicts (<2%) scored by the two reviewers. The comprehensive search of the databases resulted in 16 publications that were selected for full‐text reading. Finally, 15 publications 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 , 61 were selected that described 34 comparisons.
Figure 1.
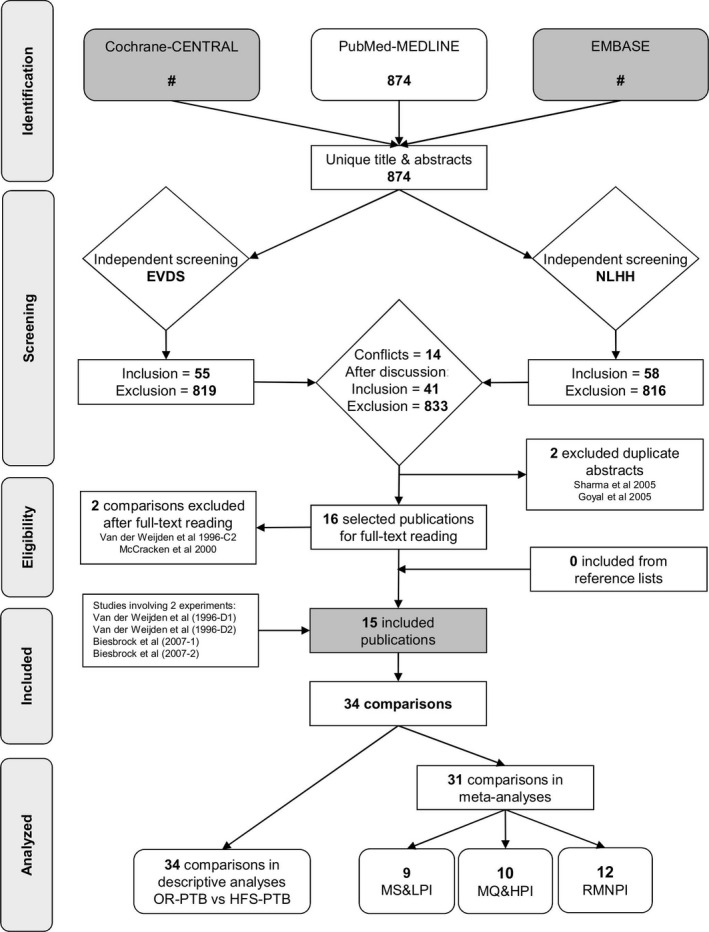
Search and selection results. OR‐PTB= Oscillating‐rotating power toothbrush; HFS‐PTB= High‐frequency sonic power toothbrush; MS&LPI= modified Silness and Löe plaque index; MQ&HPI= modified Quigley and Hein plaque index; RMNPI= Rustogi modified Navy plaque index
3.2. Study characteristics and heterogeneity assessment
Considerable heterogeneity was observed in the 15 publications with respect to study design aspects, study population, number of participants, gender, age of participants, conflicts of interest and reported funding. Information regarding the study characteristics is displayed in detail in Appendix S1A and described in Appendix S1B. All included studies were RCTs. Nine experiments used a crossover design 45 , 50 , 51 , 52 , 53 , 54 , 55 , 56 of which one 45 had a split‐mouth design, testing different brushing times in four quadrants. Eight experiments had a parallel design. 45 , 46 , 47 , 48 , 49 , 57 , 58 , 59 The total study duration varied from single experiments (1‐4 per study) to 6 months with several appointments assessing pre‐ and post‐brushing plaque removal efficacy. The mean age of the total 1,303 participants was approximately 40, which varied from 18 to 69 years.
3.3. Risk of bias assessment
To estimate the potential risk of bias of the included studies, the quality assessment aspects of internal validity, external validity and statistical validity, as well as clinical and ethical aspects, are presented in the Appendix S2. The potential risk of bias is estimated to be low for all included studies. The ethical aspects are reported more often in the recent publications.
3.4. Results of study outcomes
The Appendix S3 shows the results from the data extraction of plaque index scores of the selected studies.
3.4.1. Descriptive analysis
Table 2A and B present the descriptive analysis of the 34 comparisons indicating either OR‐PTB or HFS‐PTB. Overall plaque removal in 19 comparisons was statistically, significantly different in favour of the OR‐PTB (56%) as compared to the HFS‐PTB. The sub‐analysis based on professional brushing showed all but one comparison in favour of the OR‐PTB (89%). When participants’ brushing exercises were analysed, 12 out of 26 comparisons were significantly in favour of the OR‐PTB (46%) and 4 out of 26 in favour of the HFS‐PTB (15%).
Table 2A.
Descriptive summary of the comparisons (N = 8) and intervention indicating significances for the professional brushing
| Experiments | Comparisons | ||
|---|---|---|---|
| Authors (year) | Intervention | Plaque score reduction | Comparison |
| Van der Weijden et al (1996‐D1) 45 | HFS‐PTB | < |
OR‐PTB D7 1‐min brushing |
| HFS‐PTB | < |
OR‐PTB D9 1‐min brushing |
|
| HFS‐PTB | < |
OR‐PTB D7 2‐min brushing |
|
| HFS‐PTB | < |
OR‐PTB D9 2‐min brushing |
|
| HFS‐PTB | < |
OR‐PTB D7 3‐min brushing |
|
| HFS‐PTB | < |
OR‐PTB D9 3‐min brushing |
|
| HFS‐PTB | = |
OR‐PTB D7 4‐min brushing |
|
| HFS‐PTB | < |
OR‐PTB D9 4‐min brushing |
|
| Summary professional brushing |
7/8 in favour of OR‐PTB = 89% 0 in favour of HFS‐PTB 1/8 no difference = 11% 0 unclear |
||
Abbreviations: ?, unknown; <, significant difference in favour of the comparison (OR‐PTB); =, no significant difference; >, significant difference in favour of the intervention (HFS‐PTB); D1, duration study part I; D7 (type of brush), Plak Remover; D9 (type of brush), Plak Remover with EB9 brush head; HFS‐PTB, high‐frequency sonic power toothbrush; OR‐PTB; oscillating‐rotating power toothbrush.
Table 2B.
Descriptive summary of the comparisons (N = 26) and intervention indicating significances for the participant brushing
| Experiments | Comparisons | ||
|---|---|---|---|
| #Authors (year) | Intervention | Plaque score reduction | Comparison |
| Van der Weijden et al (1996‐D2) 45 | HFS‐PTB | = |
OR‐PTB D7 1‐min brushing |
| HFS‐PTB | = |
OR‐PTB D9 1‐min brushing |
|
| HFS‐PTB | < |
OR‐PTB D7 2‐min brushing |
|
| HFS‐PTB | < |
OR‐PTB D9 2‐min brushing |
|
| HFS‐PTB | = |
OR‐PTB D7 3‐min brushing |
|
| HFS‐PTB | = |
OR‐PTB D9 3‐min brushing |
|
| HFS‐PTB | = |
OR‐PTB D7 4‐min brushing |
|
| HFS‐PTB | = |
OR‐PTB D9 4‐min brushing |
|
| Van der Weijden et al (1996‐C1) 46 | HFS‐PTB | < | OR‐PTB |
| Robinson et al (1997) 47 | HFS‐PTB | ? | OR‐PTB |
| Yankell & Emling (1997) 48 | HFS‐PTB | ? | OR‐PTB |
| Sharma et al (1998) 49 | HFS‐PTB | < | OR‐PTB |
| Hanato et al (2005) 50 | HFS‐PTB TST | > | OR‐PTB |
| HFS‐PTB CST | > | OR‐PTB | |
| Sharma et al (2005) 51 | HFS‐PTB | < | OR‐PTB PC |
| HFS‐PTB | < | OR‐PTB 3DE | |
| Strate et al (2005) 52 | HFS‐PTB | < | OR‐PTB |
| Biesbrock et al (2007‐1) 53 |
HFS‐PTB Standard brush |
< | OR‐PTB |
| Biesbrock et al (2007‐2) 53 |
HFS‐PTB Compact brush |
< | OR‐PTB |
| Biesbrock et al (2008) 54 | HFS‐PTB | < | OR‐PTB |
| Putt et al (2008) 55 | HFS‐PTB | > | OR‐PTB |
| Williams et al (2008) 56 | HFS‐PTB | < | OR‐PTB |
| Goyal et al (2009) 57 | HFS‐PTB | < | OR‐PTB |
| Williams et al (2009) 58 | HFS‐PTB | = | OR‐PTB |
| Ayad et al (2012) 59 |
HFS‐PTB Side to side |
= | OR‐PTB |
| HFS‐PTB Colgate | > | OR‐PTB | |
| Summary participant brushing |
12/26 in favour OR‐PTB = 46% 4/26 in favour of HFS‐PTB = 15% 8/26 no difference = 31% 2/26 unclear = 8% |
||
Abbreviations: ?, unknown; <, significant difference in favour of the comparison (OR‐PTB); =, no significant difference; >, significant difference in favour of the intervention (HFS‐PTB); 3DE, Professional Care which has been developed as an upgrade to the 3D Excel 3DE; C1, comparison study part I; D2, duration study part II; D7 (type of brush), Plak Remover; D9 (type of brush), Plak Remover with EB9 brush head; HFS‐PTB, high‐frequency sonic power toothbrush; OR‐PTB, oscillating‐rotating power toothbrush; PC, Professional Care 7000.
3.4.2. Meta‐analysis
Overall
Table 3A, 3B, 3C, 4 presents an overview of the outcomes of the performed meta‐analysis, which included 31 out of the 34 comparisons. The subsequent forest plots are displayed per index used and per subgroup in the Appendices S4‐S6. The related funnel plot for the Rustogi Modified Navy plaque index 30 (RMNPI) difference scores is presented in the Appendix S6D.
Table 3A.
Meta‐analysis for single‐brushing design studies for the Modified Silness and Löe plaque index 24 , 25 , 26 using a random model
|
Single‐brushing design |
Number of studies | Number of comparisons | Comparison | Effect size | Heterogeneity | Online appendix number | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| DiffM | 95% CI | P‐value | I 2 | P‐value | Forrest plot | Funnel plot | Trial sequential analysis | ||||
|
Professional brushing Van der Weijden et al (1996) 45 1 min Van der Weijden et al (1996) 45 2 min Van der Weijden et al (1996) 45 3 min Van der Weijden et al (1996) 45 4 min Van der Weijden et al (1996) 46 |
1 | 9 | Baseline | −0.01 | (−0.05; 0.03) | .61 | 0% | .99 | S4C | NA | NA |
| End | 0.19 | (0.13; 0.25) | <.0001 | 0% | .94 | S4B | NA | S4C | |||
| Difference | ? | ||||||||||
|
Participant brushing Van der Weijden et al (1996) 45 1 min Van der Weijden et al (1996) 45 2 min Van der Weijden et al (1996) 45 3 min Van der Weijden et al (1996) 45 4 min |
1 | 8 | Baseline | 0.02 | (−0.01; 0.05) | .32 | 0% | .98 | S4A | NA | NA |
| End | 0.06 | (−0.02; 0.14) | .15 | 0% | .97 | S4B | NA | S4D | |||
| Difference | ? | ||||||||||
P‐values are presented in bold if P ≤ .05.
Abbreviations: ?, unclear; NA, not applicable.
Table 3B.
Meta‐analysis for single‐brushing design studies for the Modified Quigley and Hein plaque index 27 , 28 , 29 using a random model
|
Single‐brushing design |
Number of studies | Number of comparisons | Comparison | Effect size | Heterogeneity | Online appendix number | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| DiffM | 95% CI | P‐value | I 2 | P‐value | Forrest plot | Funnel plot | Trial sequential analysis | ||||
|
Participant brushing Robinson et al (1997) 47 Yankell & Emling (1997) 48 Williams et al (2008) 56 Williams et al (2009) 58 |
4 | 10 | Baseline | 0.01 | (−0.09; 0.10) | .92 | 55% | .02 | S5A | NA | NA |
| End | −0.00 | (−0.07; 0.07) | .93 | 12% | .34 | S5B | NA | S5D | |||
|
Participant brushing Williams et al (2008) 56 Williams et al (2009) 58 |
2 | 4 | Difference | 0.03 | (−0.03; 0.08) | .32 | 0% | .41 | S5C | NA | S5E |
P‐values are presented in bold if P ≤ .05.
Abbreviation: NA, not applicable.
Table 3C.
Meta‐analysis for single‐brushing design studies for the Rustogi Modified Navy plaque index 30 using a random model
|
Single‐brushing design Rustogi Modified Navy plaque index 30 |
Number of studies | Number of comparisons | Comparison | Effect size | Heterogeneity | Online appendix number | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| DiffM | 95% CI | P‐value | I 2 | P‐value | Forrest plot | Funnel plot | Trial sequential analysis | ||||
|
Participant brushing Sharma et al (1998) 49 Sharma et al (2005) 51 Strate et al (2005) 52 Goyal et al (2009) 57 Ayad et al (2012) 59 |
5 | 9 | Baseline | −0.00 | (−0.01; 0.00) | .14 | 52% | .03 | S6A | NA | NA |
| End | 0.06 | (0.02; 0.09) | .002 | 96% | <.00001 | S6B | NA | S6E | |||
|
Participant brushing Sharma et al (1998) 49 Sharma et al (2005) 51 Strate et al (2005) 52 Biesbrock et al (2007) 53 Biesbrock et al (2008) 54 Goyal et al (2009) 57 Ayad et al (2012) 59 |
7 | 12 | Difference | 0.06 | (0.04; 0.09) | <.00001 | 96% | <.00001 | S6C | S6D | S6F |
P‐values are presented in bold if P ≤ .05. According to Sälzer et al 2015. 30
Abbreviation: NA, not applicable.
Table 4.
| Interpretation of the heterogeneity | |
|---|---|
| Overview | Percentage % |
| Potentially not important | 0%‐40% |
| Moderate heterogeneity | 40%‐60% |
| Substantial heterogeneity | 60%‐80% |
| Considerable heterogeneity | 80%‐100% |
3.4.3. Subgroup analysis
Professional brushing
Table 3A shows the analysis from professional brushing evaluating the Modified Silness and Löe plaque index 24 , 25 , 26 (MS&LPI). In total, eight comparisons from one publication were included. 47 The end scores showed a significant effect in favour of the OR‐PTB with a DiffM of 0.19 (95% CI [0.13; 0.25]; P < .0001). For details on professional brushing, see Appendices S4A,B.
Participant brushing
There was no significant difference regarding the end scores using the MS&LPI 22 , 23 , 24 , 25 , 26 with a DiffM of 0.06 (95% CI [−0.02; 0.14]; P = .15) (see Table 3A, 3B, 3C, 4). For details on participant brushing, see Table 3A, 3B, 3C, 4, and Appendix S4A, B, S5A,B, S6A,B.
For the Modified Quigley and Hein plaque index 27 , 28 , 29 (MQ&HPI), the difference of means for baseline, end scores and incremental scores were not significant (95% CI [−0.07; 0.07] P = .93 and 95% CI [−0.03; 0.08] P = .32) (see Table 3B). Meta‐analysis of those comparisons that evaluated plaque scores according to the RMN plaque index 30 showed a significant difference of means in end scores (DiffM = 0.06 95% CI [0.02; 0.09] P < .002) and incremental scores (DiffM = 0.06 95% CI [0.04; 0.09] P < .00001) both in favour of the OR‐PTB (see Table 3C, 4).
Publication bias
The funnel plot was only possible for the RMN plaque index. Appendix S6D shows an asymmetry in the inverted funnel which suggests 33 , 35 that publication bias is likely. The presence of asymmetry may suggest a systematic difference between large and small trials in their estimates of treatment effects publication bias. 31 , 33
3.5. Additional analysis
The related TSA graph per index is presented in Appendix S4C,D,E, S5D,E,andS6E,F. The TSA suggested that for the RMN plaque index, the statistical evidence was firm for this meta‐analysis and shows that the effect was robust. Additional data will not likely alter the summary effect.
Evaluation of the clinical relevance of the results of the variable plaque indices was performed according to the distribution‐based method using the effect size, 62 minimal important difference (MID) 42 , 45 and the clinical judgement. 43 The statistical results of the clinical relevance assessments indicated that the difference between the OR‐PTB and the HFS‐PTB was potentially, clinically relevant (see Appendix S7). In total, 77% of the included experiments showed a potentially clinical relevance.
No (serious) adverse events were reported (see Appendix S9).
3.6. Evidence profile
Table 4 shows a summary of the various factors used to rate the quality and strength of evidence and the direction of recommendations according to GRADE, 45 , 46 including the level of certainty. 63 The magnitude of difference in effect of the OR‐PTB as compared to the HFS‐PTB was rated as “very small.” Based on the quality and body of evidence, the strength of the recommendation that emerges from this review is estimated to be moderate.
Table 4.
Estimated evidence profile appraisal of the strength of the recommendation and the direction regarding the single‐use efficacy of oscillating‐rotating compared with high‐frequency power toothbrushes on dental plaque removal
| Determinants of quality | Plaque index score |
|---|---|
| Study design (Appendix S1A,B) | RCTs crossover and parallel designs |
|
#studies N = 15 #experiments N = 17 #comparisons N = 34 (Figure 1) |
34 |
| Risk of bias (Appendix S2) | Low |
| Consistency (Tables 2 and 3) | Rather inconsistent |
| Directness (single‐brushing exercise) | Rather generalizable |
| Precision (Table 3A, 3B, 3C, 4) | Precise |
| Reporting bias (Appendix S6D) | Possible to likely |
| Magnitude of the effect (Table 3A, 3B, 3C, 4) | Very small |
| Strength of the recommendation based on the quality and body of evidence | Moderate |
| Direction of recommendation | There is moderate certainty of evidence of a very small but significant beneficial effect with the OR‐PTB over the HFS‐PTB. However, there is uncertainty that the clinical impact of this in long term is beneficial. |
Abbreviations: HFS‐PTB, high‐frequency sonic power toothbrush; OR‐PTB, oscillating‐rotating power toothbrush.
4. DISCUSSION
It has been shown that the use of a PTB is more effective than a MTB for plaque and gingivitis reduction. 64 , 65 A recent evaluation of brushing studies also showed that a PTB is more effective than a MTB with respect to plaque removal. 8 The aim of the present review was to evaluate the effect of oscillating‐rotating (OR‐PTB) power toothbrushes as compared to high‐frequency sonic (HFS‐PTB) power toothbrushes on dental plaque removal after a single‐brushing exercise. From this review, it can be concluded that there is moderate certainty of a very small difference in plaque removal after a single‐brushing exercise between an OR‐PTB vs an HFS‐PTB. This is in line with the former findings of the Cochrane systematic review on different powered toothbrushes. 10 These authors have concluded that there is some evidence that OR‐PTBs reduce plaque and gingivitis more than side‐to‐side brushes in the short term. Two recent systematic reviews corroborate these findings. A subject‐level meta‐analysis of studies up to 3 months provided support for the use of OR‐PTB over HFS‐PTB to improve plaque control and gingival health. 11 The other review provided some evidence that OR‐PTB might remove more plaque and reduce the number of bleedings sites better than other PTB, specifically, HSF‐PTB. 12 Taken all this evidence together, the recommendation from the present review is that when given a choice between an OR‐PTB and an HFS‐PTB, the OR‐PTB should at first be considered. The recommendations that emerge from this review can help guide the dental care professional in providing evidence‐based advice to their patients concerning PTB use.
4.1. Variables
Worldwide, a variety of PTBs are currently available in the marketplace 5 (eg counter oscillation, circular, ultrasonic and multidimensional). Apart from brush head movement, many other factors can influence the effectiveness on plaque removal, such as filament arrangement and orientation, and brush head size and shape. Other user aspects, such as instruction method, technique of use and duration, can also contribute to the variation in the observed effect. The extracted data of the present systematic review did not allow for a further sub‐analysis on any of these variables nor could a distinction be made based on the type of OR‐PTB. The reason is that these details were often absent or insufficiently reported (see Table 1). To overcome this issue in future studies, it is suggested to use the Template for Intervention Description and Replication (TIDieR). 66 , 67 The checklist and guide should improve the reporting of interventions and facilitate authors structuring accounts of their interventions. It should also benefit reviewers and editors assessing the descriptions and readers using the information. The TIDieR checklist, however, was developed in 2014; while in the present systematic review, the most recent included study was published in 2012 and therefore unfortunately did not benefit from this checklist.
4.2. Study design of interest
In the literature, there are different definitions of short‐term studies regarding plaque removal. The earlier reviews on toothbrushes excluded single‐use and clinician‐supervised studies as these were not considered to be representative of everyday use. 10 , 64 It has even been suggested that studies evaluating PTBs on the basis of a single brushing are particularly vulnerable to errors due to the novelty effect. 68 In addition, toothbrush efficacy is shown to be more effective in single‐use studies than conventional designs. 69 single‐brushing exercise studies are considered to provide limited information because they do not take into account the benefits of gingival health. 69 Nonetheless, this type of study design has been found to be very appropriate for assessing plaque removal as it facilitates the control of confounding variables such as patient compliance. 70 A single‐brushing exercise can be seen as a short‐term study on the efficacy of plaque removal and considered as the proof of principal. Generally, observations of plaque removal efficacy in single‐use brushing studies have proven to be relatively consistent with longer‐term measures of plaque removal efficacy. 71 Previously published systematic reviews have determined the efficacy, following single‐brushing exercises, on plaque removal of a MTB 72 and a PTB 7 separately and also compared with each other. 8 Obviously, this type of study design is a common design of interest for both researchers and clinicians.
4.3. Plaque score indexes
Difference in effect size and significance level was found between studies using different plaque scores (for details, see Table 3A, 3B, 3C, 4). An explanation for the result of different plaque score reductions in the present systematic review could be by the use of different plaque scores indexes. Both the Q&H index 27 , 28 , 29 and the Navy 30 plaque index assess plaque in a descriptive manner. The Q&H index is recommended by Fischman (1986) 73 for the evaluation of antiplaque procedures such as tooth brushing. This index emphasizes differences in plaque accumulation in the gingival third of the tooth, the most important region in relation to periodontal infections. 74 However, the 1‐unit reduction in the Q&H index (0‐5) 27 , 28 , 29 from 4 to 3 does not represent the same clinical effect as a reduction from 2 to 1. 7 The Navy plaque index 30 offers the advantage to emphasize approximal plaque score which makes this index very valuable in clinical practice. However, for plaque formation studies this index seems less suitable because of its low discriminating power and because it soon reaches a maximum score. 74 The phenomenon that the effect size with the Navy index 30 is larger than with Q&H index 27 , 28 , 29 has been observed in previous analysis. A systematic review that evaluated manual toothbrushes found plaque score reductions of 52% with the Navy index as compared to 30% with the Q&H index. 72 Similarly, in a review concerning PTBs these figures were 65% and 36%, respectively. 7 The origin of the difference between both indices may in part be explained by the fact that the Q&H plaque index 27 , 28 , 29 tends to overestimate the incisal half of the crown at the expense of the gingival margin. In contrast, the Navy plaque index 30 gives greater weight to plaque along the gingival margin and approximal area.
Clear distinction has to be made between plaque index scores and percentage plaque scores. Both the Q&H index and the Navy index assess plaque in a descriptive manner; therefore, plaque index scores may reflect the actual amount of plaque in a more accurate way than percentages do. However, the 1‐unit reduction on the Q&H index (0‐5) from 4 to 3 does not represent the same clinical effect as a reduction from 2 to 1. Therefore, percentages may be a more appropriate way to report the efficacy of a brushing episode because the effect depends on the amount of plaque present prior to the brushing exercise. The reader should be cautious when interpreting percentage outcomes. One needs to clearly distinguish between ‘percentage point reduction’ as being the absolute difference between prebrushing and post‐brushing percentage plaque scores as used in the present review, and the npercentage change reduction’ as the relative difference between the prebrushing and post‐brushing plaque scores.
4.4. Bias
From the current descriptive analysis (Table 2A and B), professional brushing showed a positive effect in favour of the OR‐PTB in 7 out of 8 (89%) comparisons, while for participant brushing this was 12 out of 26 (46%) in favour of the OR‐PTB. The difference is illustrated in the meta‐analysis of the MS&L plaque index, 24 , 25 , 26 where for the professional brushers, there was a significant effect that was not confirmed in participant brushing (Table 3A). All included professional brushing exercises, however, originate from the same research group 47 , 48 and may therefore introduce performance bias with an overestimation of the results. Conversely, in the professional brushing study design, the variable of the subject participating in the study will be avoided. Therefore, the potential ability of each toothbrush regarding plaque removing effectiveness can be studied without being biased or influenced, for example, by manual dexterity or the brushing experience of the participant. The funnel plot of the meta‐analysis as presented in Appendix S6D is suggestive of publication bias, as included studies are spread mostly at the top of the funnel with a lack of studies located at the bottom. Also funding publication bias may play a role as 10 studies report either sponsorship, funding or involvement of authors related to industry. However, the effect of funding source on publication bias is not clear, when trials that are just financially supported the responsibility for the conduct and reporting of the trial lies primarily with the research group. 75 When a study is performed in an academic setting, the researchers need to comply with the university and national codes of ethics for research. Besides, if a trial is supported by industry or sponsored by industry, this sponsorship has been defined in good practice guidelines. 75 , 76 As discussed above, different plaque score indexes may result in a different effect sizes. 7 , 72 As companies show a preference for a certain index, this may also introduce a reporting bias. Seven of the nine studies with involvement of the OR‐PTB Company used the Rustogi Modified Navy plaque index, 30 whereas studies with involvement of the HFS‐PTB Company toothbrush evaluated the PTBs with the Modified Quigley and Hein plaque index 27 , 28 , 29 (see Appendix S11). The impact of this preference for a specific index on the outcome of the present review could not be substantiated but meta‐analysis with the Modified Quigley and Hein plaque index 29 does not show a difference between an OR‐PTB and the HFS‐PTB, whereas with the Rustogi Modified Navy plaque index 30 a significant difference was observed. Therefore, a potential effect of the choice of plaque score index cannot be ruled out.
4.5. Ethical aspects
Including ethical aspects as an integral part of the quality assessment is under debate. The Cochrane Handbook 14 states that measures of quality alone are often strongly associated with aspects that could introduce bias. More focus is needed on the mechanisms that lead to bias. Cochrane presents examples of quality indicators that should not be assessed within this domain, including criteria related to applicability, generalizability or external validity, and criteria related to precision, reporting standards and ethical aspects. These factors may be important and should be presented in the table of characteristics of included studies. The present systematic review includes ethical aspects for the quality assessment, which are presented in the risk of bias table (see Appendix S2). However, these were not taken into consideration for the rating of the actual risk of bias as proposed by the Cochrane Handbook. 14 There is considerable heterogeneity with respect to reporting ethical aspects of the included studies. Appendix S2 provides transparency regarding adherence to ICH guideline E6, good clinical practice. This guideline is an international ethical and scientific quality standard for designing, conducting, recording and reporting trials that involve the participation of human subjects. This was not commonly reported and thus deserves attention in future studies.
4.6. Limitation and recommendation
PTBs over the past decades have undergone technological improvements. 5 The original technologies of the oscillation‐rotating movements or sonic vibrations are the same, but the movements or sonic vibrations themselves have been optimized, as well as the brush head designs. Furthermore, digital software has been developed to optimize a patient's oral hygiene performance. This systematic review included publications dated from 1996, and the latest included study dated from 2012. 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 , 61 The developmental changes in the intermediate 16 years could not be evaluated as such but could possibly affect the outcome. For future studies, the true impact of these specific novel digital features should be evaluated. Another limitation may be the use of only published research papers. The authors of this review did not have the resources to obtain data that are kept on file by the various power toothbrush manufacturers. This is known as the “file drawer,” a form of publication bias.
5. CONCLUSION
There is moderate certainty of evidence of a very small but significant beneficial effect on plaque removal after a single‐brushing exercise for the OR‐PTB vs HFS‐PTB.
6. CLINICAL RELEVANCE
6.1. Scientific rationale for the study
A systematic synthesis of the available data concerning the direct comparison of the two most commonly sold power toothbrush designs worldwide with respect to plaque removal is currently lacking.
6.2. Principal findings
Based on single‐brushing exercises, there is a moderate certainty of a very small but significant difference in favour of the OR‐PTB compared with the HFS‐PTB.
6.3. Practical Implications
Both types of power toothbrushes appear to be effective according to plaque score reduction. There is a moderate certainty in recommending the OR‐PTB over the HFS‐PTB. However, the clinical relevance of the observed very small difference needs to be established in longer‐term studies.
CONFLICT OF INTEREST
The authors declare that they have no conflicts of interest.
AUTHOR CONTRIBUTIONS
All authors have given final approval and agreed to be accountable for all aspects of the work, ensuring integrity and accuracy. EVDS drafted the manuscript and contributed to design, search and selection, and analysis and interpretation. DES critically revised the manuscript and contributed to conception and design, search and selection, and analysis and interpretation. NLHH drafted the manuscript and contributed to design, search and selection, and analysis and interpretation. CV critically revised the manuscript and contributed to analysis and interpretation. GAW critically revised the manuscript and contributed to conception and design, and analysis and interpretation.
ETHICAL APPROVAL
Ethical approval was not required.
Supporting information
Appendix S1‐S12
ACKNOWLEDGEMENTS
This study was sponsored by an unrestricted educational grant by Procter and Gamble Company Worldwide Clinical Investigations—Oral Care. This company had no say in the design or conduct of this review nor did they influence the reporting and publishing of the findings.
van der Sluijs E, Slot DE, Hennequin‐Hoenderdos NL, Valkenburg C, van der Weijden GA. Dental plaque score reduction with an oscillating‐rotating power toothbrush and a high‐frequency sonic power toothbrush: a systematic review and meta‐analysis of single‐brushing exercises. Int. J. Dent. Hygiene.2021;19:78–92. 10.1111/idh.12463
Funding information
For this research, GA van der Weijden received an unrestricted educational grant from Procter & Gamble Worldwide Clinical Investigations—Oral Care. The authors have previously received either external advisor fees, lecturer fees or research grants from toothbrush manufacturers. Those manufacturers included Colgate, Dentaid, GABA, Lactona, Oral‐B, Procter & Gamble, Philips, Sara Lee, Sunstar, Waterpik and Unilever.
Contributor Information
Eveline van der Sluijs, Email: e.vd.sluijs@acta.nl.
Dagmar Else Slot, Email: e.vd.sluijs@acta.nl.
REFERENCES
*Included publications in this systematic review
- 1. Chapple ILC, Mealey BL, Van Dyke TE, et al. Periodontal health and gingival diseases and conditions on an intact and a reduced periodontium: consensus report of workgroup 1 of the 2017 world workshop on the classification of periodontal and peri‐implant diseases and conditions. J Periodontol. 2018;89(Suppl 1):S74‐S84. [DOI] [PubMed] [Google Scholar]
- 2. Chapple IL, Van der Weijden F, Doerfer C, et al. Primary prevention of periodontitis: managing gingivitis. J Clin Periodontol. 2015;42:S71‐S76. [DOI] [PubMed] [Google Scholar]
- 3. Loe H, Theilade E, Jensen SB. Experimental gingivitis in man. J Periodontol. 1965;36:177‐187. [DOI] [PubMed] [Google Scholar]
- 4. Van der Weijden F, Dell'Acqua F, Slot DE. Alveolar bone dimensional changes of post‐extraction sockets in humans: a systematic review. J Clin Periodontol. 2009;36:1048‐1058. [DOI] [PubMed] [Google Scholar]
- 5. Penick C. Power toothbrushes: a critical review. Int J Dent Hyg. 2004;2:40‐44. [DOI] [PubMed] [Google Scholar]
- 6. Sälzer S, Van der Weijden GA, Dorfer CE, Slot DE. Current evidence on prevention of gingivitis: oral hygiene devices and dentifrices. Int J Evidence‐Based Practice Dent Hygienist. 2017;3:118‐127. [Google Scholar]
- 7. Rosema N, Slot DE, van Palenstein Helderman WH, Wiggelinkhuizen L, Van der Weijden GA. The efficacy of powered toothbrushes following a brushing exercise: a systematic review. Int J Dental Hygiene. 2016;14:29‐41. [DOI] [PubMed] [Google Scholar]
- 8. Elkerbout TA, Slot DE, Rosema NAM, Van der Weijden GA. How effective is a powered toothbrush as compared to a manual toothbrush? A systematic review and meta‐analysis of single‐brushing exercises. Int J Dent Hyg. 2020;18:17‐26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Pitchika V, Pink C, Völzke H, Welk A, Kocher T, Holtfreter B. Long‐term impact of powered toothbrush on oral health: 11‐year cohort study. J Clin Periodontol. 2019;46:713‐722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Deacon SA, Glenny AM, Deery C, et al. Different powered toothbrushes for plaque control and gingival health. Cochrane Database Syst Rev. 2010;12:CD004971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Grender J, Adam R, Zou Y. The effects of oscillating‐rotating electric toothbrushes on plaque and gingival health: a meta‐analysis. Am J Dent. 2020;33:3‐11. [PubMed] [Google Scholar]
- 12. Clark‐Perry D, Levin L. Systematic review and meta‐analysis of randomized controlled studies comparing oscillating‐rotating and other powered toothbrushes. J Am Dent Assoc. 2020;151:265‐275. [DOI] [PubMed] [Google Scholar]
- 13. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta‐analyses: the PRISMA statement. J Clin Epidemiol. 2009;62:1006‐1012. [DOI] [PubMed] [Google Scholar]
- 14. Higgins JPT, Thomas J, Chandler J, et al. (eds). Cochrane handbook for systematic reviews of interventions version 6.0 (updated July 2019). Cochrane, 2019. www.training.cochrane.org/handbook. Assessed on August 10, 2020.
- 15. PRISMA statement, Preferred reporting items for systematic reviews and meta‐analysis. http://prisma‐statement.org/. Accessed on August 10, 2020.
- 16. AMSTAR . A measurement tool to assess systematic reviews. http://amstar.ca/index.php. Accessed on August 10, 2020.
- 17. Shea BJ, Grimshaw JM, Wells GA, et al. Development of AMSTAR: a measurement tool to assess the methodological quality of systematic reviews. BMC Med Res Methodol. 2007;7:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. PROSPERO . International prospective register of systematic reviews. 2014. http://www.crd.york.ac.uk/PROSPERO. Accessed on: 5 December 2019.
- 19. Ryan R,Cochrane Consumers and Communication Review Group . Cochrane consumers and communication review group: data synthesis and analysis. 2013. http://cccrg.cochrane.org. Accessed on: August 10, 2020.
- 20. Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan—a web and mobile app for systematic reviews. Syst Rev. 2016;5:210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Keukenmeester RS, Slot DE, Rosema NA, Van der Weijden GA. Determination of a comfortable volume of mouthwash for rinsing. Int J Dental Hygiene. 2012;10:169‐174. [DOI] [PubMed] [Google Scholar]
- 22. Light RJ, Smith PV. Accumulating evidence: procedures for resolving contradictions among research studies. Harv Educ Rev. 1971;41:429‐471. [Google Scholar]
- 23. Review Manager (RevMan). Version 5.3 ed. Copenhagen: The Nordic Cochrane Centre The Cochrane Collaboration; 2014.
- 24. Silness J, Löe H. Periodontal disease in pregnancy (II). Correlation between oral hygiene and periodontal condition. Acta odontol Scand. 1964;22:121‐135. [DOI] [PubMed] [Google Scholar]
- 25. Van der Weijden GA, Danser MM, Nijboer A, Timmerman MF, Van der Velden U. The plaque‐removing efficacy of an oscillating/rotating toothbrush. A short term study. J Clin Periodontol. 1993;20(4):273‐278. [DOI] [PubMed] [Google Scholar]
- 26. Danser MM, Timmerman MF, Jzerman Y, Piscaer MI, Van Der Velden U, Van Der Weijden GA. Plaque removal with a novel manual toothbrush (X‐Active) and the Braun Oral‐B 3D Plaque Remover. J Clin Periodontol. 2003;30:138‐144. [DOI] [PubMed] [Google Scholar]
- 27. Quigley GA, Hein JW. Comparative cleansing efficiency of manual and power brushing. J Am Dent Assoc. 1962;65:26‐29. [DOI] [PubMed] [Google Scholar]
- 28. Turesky S, Gilmore ND, Glickman L. Reduced formation by chloromethyl analogue of vitamin C. J Periodontol. 1970;41:41‐43. [DOI] [PubMed] [Google Scholar]
- 29. Lobene RR, Soparker PM, Newman BS. Use of dental floss. Effect of plaque and gingivitis. Clin Prev Dent. 1982;4:5‐8. [PubMed] [Google Scholar]
- 30. Rustogi KN, Curtis JP, Volpe AR, Kemp JH, McCool JJ, Korn LR. Refinement of the modified navy plaque index to increase plaque scoring efficiency in gumline and interproximal tooth areas. J Clin Dent. 1992;3:C9‐C12. [PubMed] [Google Scholar]
- 31. Higgins JP, Green S. Cochrane Handbook for Systematic Reviews of Interventions. Chichester: Wiley‐Blackwell; 2011. [Google Scholar]
- 32. Sälzer S, Slot DE, Van der Weijden FA, Dörfer CE. Efficacy of inter‐dental mechanical plaque control in managing gingivitis–a meta‐review. J Clin Periodontol. 2015;42:S92‐S105. [DOI] [PubMed] [Google Scholar]
- 33. Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta‐analysis detected by a simple, graphical test. BMJ. 1997;315:629‐634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. DeMets DL, Lan KK. Interim analysis: the alpha spending function approach. Stat Med. 1994;13:1341‐1352; discussion 53–56. [DOI] [PubMed] [Google Scholar]
- 35. O'Brien PC, Fleming TR. A multiple testing procedure for clinical trials. Biometrics. 1979;35:549‐556. [PubMed] [Google Scholar]
- 36. Wetterslev J, Thorlund K, Brok J, Gluud C. Trial sequential analysis may establish when firm evidence is reached in cumulative meta‐analysis. J Clin Epidemiol. 2008;61:64‐75. [DOI] [PubMed] [Google Scholar]
- 37. Brok J, Thorlund K, Wetterslev J, Gluud C. Apparently conclusive meta‐analyses may be inconclusive–Trial sequential analysis adjustment of random error risk due to repetitive testing of accumulating data in apparently conclusive neonatal meta‐analyses. Int J Epidemiol. 2009;38:287‐298. [DOI] [PubMed] [Google Scholar]
- 38. Thorlund K, Anema A, Mills E. Interpreting meta‐analysis according to the adequacy of sample size. An example using isoniazid chemoprophylaxis for tuberculosis in purified protein derivative negative HIV‐infected individuals. Clin Epidemiol. 2010;2:57‐66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Thorlund K, Engstrøm J, Wetterslev J, Imberger G, Gluud C. User manual for Trial Sequential Analysis (TSA). Copenhagen Trial Unit, 2011. Copenhagen, Denmark: Centre for Clinical Intervention Research; 2017: 1‐115. [Google Scholar]
- 40. Cohen J. A power primer. Psychol Bull. 1992;112:155‐159. [DOI] [PubMed] [Google Scholar]
- 41. Guyatt GH, Osoba D, Wu AW, Wyrwich KW, Norman GR, Clinical Significance Consensus Meeting G . Methods to explain the clinical significance of health status measures. Mayo Clin Proc. 2002;77:371‐383. [DOI] [PubMed] [Google Scholar]
- 42. Lemieux J, Beaton DE, Hogg‐Johnson S, Bordeleau LJ, Goodwin PJ. Three methods for minimally important difference: no relationship was found with the net proportion of patients improving. J Clin Epidemiol. 2007;60:448‐455. [DOI] [PubMed] [Google Scholar]
- 43. Musselman KE. Clinical significance testing in rehabilitation research: what, why, and how? Phys Ther Rev. 2007;12:287‐296. [Google Scholar]
- 44. Armijo‐Olivo S, Warren S, Fuentes J, Magee DJ. Clinical relevance vs. statistical significance: using neck outcomes in patients with temporomandibular disorders as an example. Man Ther. 2011;16:563‐572. [DOI] [PubMed] [Google Scholar]
- 45. Guyatt GH, Oxman AD, Kunz R, et al. Incorporating considerations of resources use into grading recommendations. BMJ. 2008;336:1170‐1173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. GRADE . Grading of Recommendations Assessment, Development and Evaluation (GRADE) working group. 2016. http://www.gradeworkinggroup.org/. Assessed on August 10, 2020.
- 47.* Van der Weijden FA, Timmerman MF, Snoek IM, Reijerse E, Van der Velden U. Toothbrushing duration and plaque removing efficacy of electric toothbrushes. Am J Dent. 1996;9:S31‐S36. [PubMed] [Google Scholar]
- 48.* Van der Weijden GA, Timmerman MF, Reijerse E, Snoek CM, Van der Velden U. Comparison of an oscillating/rotating electric toothbrush and a 'sonic' toothbrush in plaque‐removing ability. A professional toothbrushing and supervised brushing study. J Clin Periodontol. 1996;23:407‐411. [DOI] [PubMed] [Google Scholar]
- 49.* Robinson PJ, Maddalozzo D, Breslin S. A six‐month clinical comparison of the efficacy of the Sonicare and the Braun Oral‐B electric toothbrushes on improving periodontal health in adult periodontitis patients. J Clin Dent. 1997;8:4‐9. [PubMed] [Google Scholar]
- 50.* Yankell SL, Emling RC. A thirty‐day safety and efficacy evaluation of the rowenta, braun and sonicare powered toothbrushes and a manual toothbrush. J Clin Dent. 1997;8:120‐123. [PubMed] [Google Scholar]
- 51.* Sharma NC, Galustians J, Qaqish J, Cugini M. A comparison of two electric toothbrushes with respect to plaque removal and subject preference. Am J Dent. 1998;11:S29‐S33. [PubMed] [Google Scholar]
- 52.* Hanato Y, Kishimoto T, Ojima M, et al. Comparative study of plaque removal efficacy of twin‐motor sonic toothbrush with floating bristles and conventional powered toothbrushes in posterior teeth. Am J Dent. 2005;18:237‐240. [PubMed] [Google Scholar]
- 53.* Sharma NC, Goyal CR, Qaqish JG, Cugini MA, Thompson MC, Warren PR. Single‐use plaque removal efficacy of three power toothbrushes. J Dent. 2005;33:11‐15. [PubMed] [Google Scholar]
- 54.* Strate J, Cugini MA, Warren PR, Qaqish JG, Galustians HJ, Sharma NC. A comparison of the plaque removal efficacy of two power toothbrushes: oral‐b professional care series versus sonicare elite. Int Dent J. 2005;55:151‐156. [DOI] [PubMed] [Google Scholar]
- 55.* Biesbrock AR, Bartizek RD, Walters PA, et al. Clinical evaluations of plaque removal efficacy: an advanced rotating‐oscillating power toothbrush versus a sonic toothbrush. J Clin Dent. 2007;18:106‐111. [PubMed] [Google Scholar]
- 56.* Biesbrock AR, Walters PA, Bartizek RD, Goyal CR, Qaqish JG. Plaque removal efficacy of an advanced rotation‐oscillation power toothbrush versus a new sonic toothbrush. Am J Dent. 2008;21:185‐188. [PubMed] [Google Scholar]
- 57.* Putt MS, Milleman JL, Jenkins W, Schmitt P, Master AS, Strate J. A randomized crossover‐design study to investigate the plaque removal efficacy of two power toothbrushes: Philips Sonicare Flexcare and Oral‐B Triumph. Compend Contin Educ Dent. 2008;29(56):58‐64. [PubMed] [Google Scholar]
- 58.* Williams K, Rapley K, Huan J, et al. A study comparing the plaque removal efficacy of an advanced rotation‐oscillation power toothbrush to a new sonic toothbrush. J Clin Dent. 2008;19:154‐158. [PubMed] [Google Scholar]
- 59.* Goyal CR, Qaqish J, He T, Grender J, Walters P, Biesbrock AR. A randomized 12‐week study to compare the gingivitis and plaque reduction benefits of a rotation‐oscillation power toothbrush and a sonic power toothbrush. J Clin Dent. 2009;20:93‐98. [PubMed] [Google Scholar]
- 60.* Williams K, Rapley K, Haun J, et al. Comparison of rotation/oscillation and sonic power toothbrushes on plaque and gingivitis for 10 weeks. Am J Dent. 2009;22:345‐349. [PubMed] [Google Scholar]
- 61.* Ayad F, Petrone DM, Wachs GN, Mateo LR, Chaknis P, Panagakos F. Comparative efficacy of a specially engineered sonic powered toothbrush with unique sensing and control technologies to two commercially available power toothbrushes on established plaque and gingivitis. J Clin Dent. 2012;23:A5‐A10. [PubMed] [Google Scholar]
- 62. Cohen J. Statistical Power Analysis for the Behavioral Sciences, (2nd edn). Hillsdale, NJ: Erlbaum Associates; 1988. [Google Scholar]
- 63. Smiley CJ, Tracy SL, Abt E, et al. Evidence‐based clinical practice guideline on the nonsurgical treatment of chronic periodontitis by means of scaling and root planing with or without adjuncts. J Am Dent Assoc. 2015;146:525‐535. [DOI] [PubMed] [Google Scholar]
- 64. De Jager M, Rmaile A, Darch O, Bikker JW. The effectiveness of manual versus high‐frequency, high‐amplitude sonic powered toothbrushes for oral health: a meta‐analysis. J Clin Dent. 2017;28:A13‐A28. [PubMed] [Google Scholar]
- 65. Yaacob M, Worthington HV, Deacon SA, et al. Powered versus manual toothbrushing for oral health. Cochrane Database Syst Rev. 2014;17:CD002281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Hoffmann T, Glasziou P, Boutron I, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ. 2014;348:g1687. [DOI] [PubMed] [Google Scholar]
- 67. http://www.equator‐network.org/reporting‐guidelines/tidier/. Assessed on August 10, 2020.
- 68. Ash MM. A review of the problems and results of studies on manual and power toothbrushes. J Periodontol. 1964;35:202‐213. [Google Scholar]
- 69. Claydon N, Addy M. Comparison single‐use plaque removal by toothbrushes of different designs. J Clin Periodontol. 1996;23:1112‐1116. [DOI] [PubMed] [Google Scholar]
- 70. Egelberg L, Claffey N. Role of mechanical dental plaque removal in prevention and therapy of caries and periodontal diseases. Consensus report of Group B In: Lang NP, Attström R, Löe H, eds. Proceedings of European Workshop on Mechanical Plaque Control – Status of the Art and Science of Dental Plaque Control. Chicago, Berlin; London; Tokyo; Paris: Quintessence; 1998:169‐172. [Google Scholar]
- 71. Haun J, Williams K, Friesen L, et al. Plaque removal efficacy of a new experimental battery‐powered toothbrush relative to two advanced‐design manual toothbrushes. J Clin Dent. 2002;13:191‐197. [PubMed] [Google Scholar]
- 72. Slot DE, Wiggelinkhuizen L, Rosema NA, Van der Weijden GA. The efficacy of manual toothbrushes following a brushing exercise: a systematic review. Int J Dent Hyg. 2012;10:187‐197. [DOI] [PubMed] [Google Scholar]
- 73. Fischman SL. Current status of indices of plaque. J Clin Periodontol. 1986;13: 371‐374, 379‐380. [DOI] [PubMed] [Google Scholar]
- 74. Quirynen M, Dekeyser C, van Steenberghe D. Discriminating power of five plaque indices. J Periodontol. 1991;62:100‐105. [DOI] [PubMed] [Google Scholar]
- 75. Van Lent M, Out HJ. Effect of funding source on publication bias is not so clear cut. BMJ. 2013;347:f7582. [DOI] [PubMed] [Google Scholar]
- 76. International conference on harmonisation of technical requirements for registration of pharmaceuticals for human use . ICH harmonised tripartite guideline. Guideline for good clinical practice E6. 1996. www.ich.org/fileadmin/Public_Web_Site/ICH_Products/Guidelines/Efficacy/E6_R1/Step4/E6_R1__Guideline.pdf. Assessed on August 27, 2020.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1‐S12


