Abstract
Carbohydrate counting is an essential component of type 1 diabetes education but can be difficult for adolescents to learn. Because adolescents are avid users of technology, an Internet-based education module was compared with an in-class education session in terms of carbohydrate counting accuracy in adolescents with type 1 diabetes. Adolescent participants displayed increased carbohydrate counting accuracy after attending an in-class education session compared with an Internet-based education module. These results suggest that online education is best reserved as an adjunctive therapy to in-class teaching in this population.
Carbohydrate counting is a recommended daily practice for the self-management of type 1 diabetes, in conjunction with insulin therapy (1). This method allows for more flexibility in the timing and frequency of eating and the amount of carbohydrate consumed during meals and snacks (1). Accuracy in carbohydrate estimation is required to achieve and sustain adequate glycemic control, and differences of ≥20 g from actual carbohydrate amount have been shown to affect postprandial glucose excursions (2,3). Thus, carbohydrate counting is an essential component of conventional diabetes education, a collaborative process whereby patients gain knowledge and skills to successfully self-manage their diabetes and related conditions (4,5).
However, evidence suggests that adolescents with type 1 diabetes do not accurately count carbohydrates (6). In a previous study in adolescents with type 1 diabetes, we reported that, despite using carbohydrate counting for managing their diabetes and receiving in-class education with a dietitian, fewer than half of the sample counted carbohydrates accurately (7). Furthermore, a nutrition education intervention focused on carbohydrate counting in adolescents with type 1 diabetes found no improvement in counting accuracy and glycemic control after 3 months (8). These findings suggest a need to develop more intensive education that is cost-effective and readily available and provides the tools to empower individuals in their day-to-day diabetes management (9,10).
Multiple factors have a bearing on the delivery of diabetes care for adolescents with type 1 diabetes; these include a shift in responsibility from parents to adolescents, adolescents’ focus on social contexts and peers, developmental inclination toward risk taking, and fatigue from care of a chronic illness (11). Therefore, the approach to diabetes education needs to be engaging, developmentally appropriate, and motivating to encourage appropriate diabetes self-management.
Digital technologies are readily used among adolescents, and strategies that incorporate such technologies can potentially help adolescents enhance their skills in diabetes self-management (12,13). These strategies include online educational resources (14), short message service systems (15,16), interactive diabetes management tools (17), video games (18,19), Internet-based communication (20), Internet videoconferencing (21), and mobile device applications (22). Online education for diabetes management may help to reduce the complexity and inaccuracies associated with carbohydrate counting, as well as reduce the barrier of attending face-to-face teaching sessions by being a flexible learning option that can be reviewed at a patient’s convenience.
There is no evidence indicating the most effective type of educational platform for training adolescents in carbohydrate counting. Although studies of Internet-based educational tools for diabetes self-management have been conducted in adolescents with type 1 diabetes (23), none have focused exclusively on improving carbohydrate counting skills. Furthermore, the current literature evaluating computer-assisted diabetes education has primarily targeted adults with type 2 diabetes (24,25). Therefore, the objective of this study was to evaluate an Internet-based education module on carbohydrate-counting accuracy in adolescents with type 1 diabetes in comparison with the standard of care (in-class education session). We hypothesized that the Internet-based module would result in improved accuracy compared with the in-class session.
Research Design and Methods
Study Design
This randomized, controlled, parallel-group trial compared the effectiveness of teaching principles of carbohydrate counting to adolescents with type 1 diabetes who did not self-identify as regular carbohydrate counters (ClinicalTrials.gov Identifier: NCT02462785). As in our previous study in adolescents with type 1 diabetes who self-identified carbohydrate counting as part of their diabetes management (7), we used two methods of assessing carbohydrate estimation knowledge and accuracy: 1) carbohydrate content estimations from trays of real prepared meals and snacks and 2) a validated questionnaire to assess knowledge of carbohydrate content (the PedsCarbQuiz [PCQ]) (26). However, in the current study, we compared two educational methods: 1) an in-class session (current standard of care) and 2) an Internet-based education module.
The study was conducted at The Hospital for Sick Children (SickKids) in Toronto, Canada, a tertiary care hospital providing diabetes care to ∼950 children and adolescents annually. Dietary education is provided to all families after a diagnosis of diabetes. As children transition to adolescence, they are invited to attend an in-class session with a dietitian that offers instruction on identifying carbohydrate versus noncarbohydrate foods, portion sizes, healthy choices, carbohydrate counting, and nutrition label reading. The study was approved by the SickKids research ethics board.
Participants
Adolescents aged 12–18 years with diagnosis of type 1 diabetes were identified through chart review in consultation with the health care team and approached for participation in this study at their clinic visit. Demographic data were collected from patients, parents, and medical records and included age, sex, duration of diabetes, method of insulin administration, frequency of carbohydrate counting, and A1C levels from participants’ previous clinic visit.
Criteria for inclusion were type 1 diabetes for >1 year, access to a computer with Internet connection, and ability to communicate in English. We excluded adolescents with medication-induced diabetes and type 2 diabetes, celiac disease, and learning disabilities, as well as those who had attended a carbohydrate counting class within 6 months before recruitment and those who indicated that they count carbohydrate with all meals daily.
Written informed assent/consent was obtained from the participants and their parents. The participants were assigned to one of the study groups using a computer-generated randomization sequence with a randomization scheme of 1:1 ratio for each intervention based on the block randomization method.
General Procedures
After giving informed consent, participants completed the Youth Adolescent Questionnaire, an abbreviated version of the Food Frequency Questionnaire (FFQ) (27), to confirm regular consumption of food and snack items presented to them for carbohydrate estimation and to verify the accuracy of carbohydrate counting against familiarity with the food items. All participants were then evaluated for their knowledge of carbohydrate counting by a standardized meal and snack tray test and completed the carbohydrate knowledge section of the PCQ (26). Participants were then assigned to a dietitian-led, in-class education session or an online Internet-based session. After completion of the education sessions, all participants were asked to practice carbohydrate counting until the next clinic appointment in 3 months, at which time they repeated the tray test and PCQ.
Tray Test
One of two clusters (each cluster consisting of three meal trays and three snack items) was randomly assigned at pre- and post-intervention evaluations, covering a range of food groups and carbohydrate contents. Each participant received a different tray pre- and post-intervention, and, overall, each cluster was split so that half were presented at study visit 1 (baseline) and the other half at study visit 2 (3 months post-intervention).
The food items were selected by the study dietitian based on the knowledge of foods commonly eaten by adolescents visiting the clinic and included items used in other studies that measured carbohydrate counting accuracy. Foods identified on the FFQ that were not consumed regularly by the adolescents were not included. A combination of fresh food and some packaged food with visible nutrition labels were presented, and carbohydrate content was determined using a nutrition database (28) and information from the nutrition labels on packaged foods.
PCQ
The PCQ is an easily administered questionnaire to assess knowledge of carbohydrate counting and insulin dose calculation and has been validated in a population of North American children with type 1 diabetes and their parents (26). Scores are calculated as the percentage of questions answered correctly. Reliability analysis of the PCQ shows high internal reliability (Cronbach’s α of 0.88) and Spearman’s correlation of 0.60 (P <0.0001) on split-half reliability testing.
PCQ score correlates significantly with A1C, as well as expert assessment of participants’ proficiency for the four carbohydrate knowledge domains of the questionnaire. These domains include 1) recognition of carbohydrates, 2) carbohydrate counting for individual food items, 3) carbohydrate counting in a whole meal, and 4) nutritional label reading, which includes identifying serving size and net carbohydrates (g total carbohydrate – g fiber). The complete PCQ also includes three domains to assess insulin dosing, which were not used in this study. The first four parts of the questionnaire thoroughly evaluate participants’ knowledge of material covered in the educational modules delivered in this study.
Educational Video Development
The “Counting Carbs to Be in Charge” video can be viewed online (https://meant2prevent.ca/counting-carbs-to-be-in-charge). The video is ∼10 minutes long and includes the same concepts covered at the in-class education sessions, but was designed with an adolescent delivering the messages in short segments using techniques designed to attract and maintain attention in this age-group. These techniques include presenting visuals of foods, estimates of portion sizes, and key points using short segment highlights. Topics include the importance of carbohydrates, their function in nutrition and in diabetes, sources of carbohydrates, differences between carbohydrate and noncarbohydrate foods, common resources for carbohydrate counting, label reading, and meal planning.
The video was delivered to participants by password-protected access through the REDCap (Research Electronic Data Capture) platform (29), followed by a series of questions to test patients’ understanding after each section. Users were allowed to repeat sessions, log on and off during a session, and choose desired modules for review or repetition. The video link remained active for 1 week to allow for multiple viewings.
Study Outcomes
The primary outcome was change in individual mean differences between counted and actual carbohydrate on the tray test before and 3 months after the intervention in each group. The difference away from the actual amount (over or under) was used to calculate the individual mean difference.
The secondary outcomes were 1) the proportion of participants achieving carbohydrate counting accuracy of up to 15 g (over or under) of the actual amount of carbohydrate across the two tray groups before and after the intervention, based on literature documenting that differences of 10–20 g can affect glycemic control (2,3) and 2) the mean change in PCQ scores in each group before and 3 months after the intervention.
Statistical Analysis
Descriptive statistics (means, SDs, counts, and proportions) were calculated for demographic variables between in-class and online groups using an independent samples t test for continuous variables and a Fisher exact test for nominal variables.
Accuracy of carbohydrate counting was determined as the difference between a participant’s estimated content and the actual carbohydrate content of the meal or snack (in grams). A difference of up to 15 g over or under was classified as “accurate.” Changes in accuracy from pre- to post-intervention were compared between in-class and online groups using an unpaired t test.
The mean changes from pre- to post-intervention in PCQ scores were compared using a paired t test within the in-class group, online group, and the overall sample, and the change in PCQ scores from pre- to post-intervention were compared between in-class and online groups using an unpaired t test. Following an intention-to-treat analysis, a secondary analysis was repeated using only those participants who completed the online or in-class education session, as well as the pre- and post-intervention tray test.
Univariate and multivariate logistic regression was used to examine the associations between clinical variables and counting accuracy within 15 g (over or under) of the true content. Variables with P <0.2 on univariate analyses were entered into multivariate analyses, along with time (pre- vs. post-intervention) and group (in-class vs. online).
P <0.05 was considered statistically significant. All analyses were performed using SAS v. 9.4 software (SAS Institute, Cary, NC).
Sample Size
We previously conducted a pilot study of carbohydrate counting in eight adolescents from our clinic (aged 13–17 years, diabetes duration of 1.5–9 years, A1C 7.4–11.4%) to estimate the SD for mean difference between the counted and actual amount of carbohydrate. Each participant assessed three meal trays of commonly eaten foods varying in carbohydrate count between 68 and 76 g. Overall accuracy was variable, and 50% of this pilot sample was able to count within 15 g of the actual amount. A minimum sample size of 20 participants per group was calculated to achieve a significance level of 0.05 (α = 5%) and 80% power (β = 0.2) to detect a mean between-group difference of 7.1 g from the actual amount with estimated group SD of 9.13 g (attained from the pilot study). To allow for a 20% attrition rate, a target of 25 individuals per group was set.
Results
Demographics
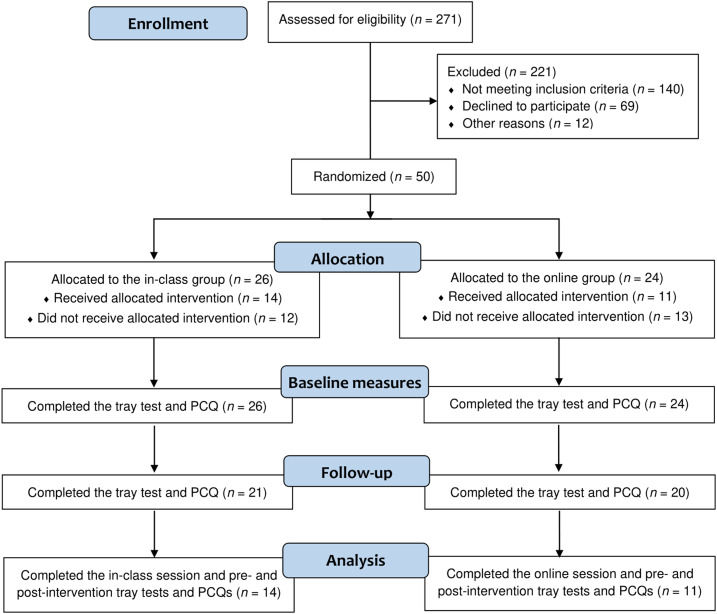
Fifty individuals participated in this study (Figure 1). A total of 26 individuals (52%) were randomized to the in-class session, and 24 individuals (48%) were randomized to the online session. Of those assigned, 14 completed the in-class education and 11 completed the online education. After carbohydrate counting education, 21 of the in-class participants and 20 of the online participants completed the tray test and PCQ at their 3-month follow-up visit.
FIGURE 1.
Consolidated Standards for Reporting of Trials (CONSORT) flow diagram.
Demographic characteristics between the in-class and online groups are presented in Table 1. There were no differences in age, ratio of males to females, duration of diabetes, type of diabetes treatment, or A1C. This sample was representative of the clinic’s adolescent population (14.4 ± 1.7 years; mean A1C 8.5 ± 1.2%) (30). Participants on regimens of two or three daily insulin injections used intermediate-acting NPH insulin and rapid-acting insulin aspart or lispro. Those taking four daily injections used insulin glargine with a rapid-acting analog insulin, and those on pump therapy used only a rapid-acting analog insulin.
TABLE 1.
Baseline Characteristics
| In-Class Group (n = 26) | Online Group (n = 24) | |
|---|---|---|
| Age, years | 15.6 ± 2.4 | 15.5 ± 2.4 |
| Sex | 14:12 | 13:11 |
| Duration of diabetes, years | ||
| 1–3 | 5 (19.2) | 5 (20.8) |
| 4–8 | 9 (34.6) | 12 (50.0) |
| >8 | 12 (46.2) | 7 (29.2) |
| Insulin treatment regimen | ||
| Injections twice daily | 1 (3.8) | 1 (4.2) |
| Injections three times daily | 13 (50.0) | 12 (50) |
| Injections four or more times daily | 7 (26.9) | 6 (25.0) |
| Insulin pump therapy | 5 (19.2) | 4 (16.7) |
| A1C, % | 9.4 ± 1.9 | 8.8 ± 1.6 |
Data are mean ± SD or n (%) except for sex, which is male:female ratio.
Tray Test Accuracy
At baseline, the absolute difference between actual carbohydrate content and estimated content for the overall sample was 20.6 ± 12.5 g for meals and 5.8 ± 6.4 g for snacks. Within each group, the absolute difference at baseline was 23.2 ± 14.6 g for meals and 6.3 ± 7.5 g for snacks in the in-class group and 17.9 ± 9.3 g for meals and 5.2 ± 5.0 g for snacks in the online group. There were no differences between groups at baseline.
The change between counted and actual carbohydrate count before and 3 months after the intervention in each group was not significant (in-class: −5.1 ± 16.9 g, P = 0.19; online: −0.1 ± 9.3 g, P = 0.96). Furthermore, there were no significant differences in the change in meal (β = −5.0 g, 95% CI −13.83 to 3.76, P = 0.25) and snack (β = 0.5 g, 95% CI −2.16 to 3.10), P = 0.72) counting accuracy between the in-class and online groups.
The proportion of participants who achieved overall counting accuracy within 15 g for each meal and snack from pre- to post-intervention was not significantly different between the in-class and online groups (44 vs. 56.1%, P = 0.59).
We performed a post hoc analysis of adolescents who completed tray tests before and 3 months after the intervention and either an in-class (n = 14) or an online (n = 11) education session. The in-class participants decreased their absolute mean tray carbohydrate counting error after education from 23.4 ± 16.0 g to 14.9 ± 11.1 g (P = 0.049). The absolute difference in carbohydrate counting error from pre- (16.7 ± 5.1 g) to post-intervention (15.1 ± 5.5 g) for the online group was not different (P = 0.52). Also, the absolute difference between actual and estimated carbohydrate content of meal trays was not significant between the in-class and the online groups (β = −7.0 g, 95% CI −17.19 to 3.13, P = 0.17).
Univariate logistic regression revealed that a higher A1C was associated with lower accuracy on the tray test (odds ratio [OR] 0.69, 95% CI 0.52–0.91, P = 0.01). No other variables were significant. Multivariate logistic regression analysis demonstrated that, for every 1% increase in A1C, participants were 32% less likely to count accurately (OR 0.68, 95% CI 0.51–0.91, P = 0.01) (Table 2). Group and time were not significant factors.
TABLE 2.
Multivariate Logistic Regression of Carbohydrate Counting Accuracy
| Parameter | OR (95% CI) | P |
|---|---|---|
| Time (pre- vs. post-intervention) | 1.59 (0.74–3.41) | 0.24 |
| Group (in-class vs. online) | 1.01 (0.39–2.61) | 0.99 |
| Most recent A1C | 0.68 (0.51–0.91) | 0.01 |
PCQ Scores
Baseline PCQ scores for the entire group were 73 ± 15%. PCQ scores pre- and post-intervention decreased significantly in both groups (in-class from 72 to 68%, P = 0.04; online from 74 to 67%, P = 0.0004). There was no significant change in PCQ scores between groups (β = 0.05, 95% CI −0.01 to 0.11, P = 0.08).
Discussion
In this study, we evaluated an online method of teaching carbohydrate counting skills to adolescents with type 1 diabetes in comparison with standard in-class education with a dietitian. Participants in this study, who did not regularly count carbohydrates, performed reasonably well on the carbohydrate counting assessments at baseline. In-class education compared with an Internet-based teaching module increased carbohydrate counting accuracy after 3 months, as assessed by the tray test. Carbohydrate counting accuracy was negatively predicted by A1C. However, both groups demonstrated a decrease in PCQ scores after 3 months.
Adolescents who completed the in-class education classes showed improved carbohydrate counting accuracy compared with the online module after 3 months. This was a surprise in light of improvements in self-management and problem-solving skills observed in adolescents with type 1 diabetes receiving usual care plus Internet support (31) and findings of a systematic review of Internet-based self-management interventions for youth with health conditions (32). However, most studies used a waitlist control or usual care as comparisons and thus were unable to conclude that online education was as effective as in-class sessions (32).
To our knowledge, no studies have focused on Internet-based education for carbohydrate counting specifically in adolescents with type 1 diabetes. A small pilot study geared to Hispanic adults showed a 25% increase in carbohydrate counting skills after completing activities and reading information on a diabetes education website (33). In another study using a computer-based, interactive diabetes education program to train adults with type 1 diabetes on estimating carbohydrate content, there was a reduction in the number of mistakes made after repeating the exercises in the program (34). However, both studies lacked in-class education sessions and, therefore, do not allow for comparison between online and in-class methods.
Increased engagement may be one potential explanation for the better outcome in the in-class group. It is possible that adolescents in our study were less engaged with the online module and preferred the interaction with their health care provider (a dietitian), which was not assessed. A review of Internet-delivered diabetes education indicated that patient engagement and usage of Internet materials waned over time and that interaction with health care providers was deemed appealing to participants (24). Internet-based education modules may be best used as an adjunctive tool to support in-class education sessions for our adolescent population, as previously suggested (34).
Having a higher A1C was associated with a lower likelihood of carbohydrate counting accuracy. This finding is consistent with evidence suggesting that carbohydrate counting may have beneficial effects on A1C in youth (35) and with our previous study showing that higher A1C was associated with lower accuracy on the tray test (7). Our findings suggest that greater ability to count carbohydrates over the preceding 3 months may affect mean blood glucose measures through adjustments in premeal insulin doses, leading to lower A1C. However, future studies assessing the long-term impact of carbohydrate counting accuracy on A1C are warranted.
PCQ scores decreased for adolescents receiving in-class and online education. Baseline PCQ scores were relatively high for adolescents who did not regularly count carbohydrates, but lower than previously reported in self-identified regular carbohydrate counters (81 ± 10%) (7). It is possible that decreased study engagement with a repeated questionnaire may have led to increased errors. Surprisingly, those who improved on the tray test did not show improved PCQ scores. A study in children and adolescents with type 1 diabetes showed a significant increase in PCQ scores after 6 months of unstructured use of an educational video game (36), suggesting that a longer period of time (≥3 months) may be needed to observe an improvement in PCQ scores.
Adherence was an issue in both the in-class and online groups, with only half of the participants completing an education session. Barriers to treatment adherence may be the result of psychosocial and motivational factors as children transition into adolescence (37). One method to potentially improve adherence is to create more interactive sessions. In a trial of 320 children with type 1 diabetes comparing two interactive, Internet-based modules focused on either coping skills training or general diabetes management, both groups reported high levels of satisfaction, and ∼75% completed the modules (38). However, diabetes knowledge was not assessed. Future studies targeting diabetes education to adolescents should identify age-specific factors to improve adherence and include more engaging and interactive components to increase satisfaction and motivation.
This study has a few limitations. As previously mentioned, there were challenges with attrition and incomplete education sessions in both the in-class and online groups, decreasing our sample size. Expanding recruitment to include the pre-adolescent age-group may have improved retention. Second, we did not assess whether improvements in carbohydrate counting affected glycemic control. Despite these limitations, our study fills a critical gap in the existing pool of studies using technology-based educational tools to improve carbohydrate counting skills in this population. One strength of our study is that real food samples were used to create a more realistic carbohydrate counting approach instead of relying on food pictures or models for estimation.
In summary, adolescents with type 1 diabetes displayed increased carbohydrate counting accuracy after attending an in-class education session compared with an Internet-based teaching module. Our preliminary results indicate that online education may be best reserved for this population as an adjunctive therapy to in-class teaching, a critical component of diabetes self-management. Future studies should determine whether using Internet-based education alongside conventional teaching methods will help to optimize diabetes self-management as adolescents transition to a more autonomous role in their diabetes care routine.
Article Information
Acknowledgments
The authors acknowledge Shawna Steele and Ping Li for assistance with study coordination and thank the clinical staff at SickKids Hospital and all of the participants who took part in this research.
Funding
This work was supported by a grant from The Lawson Foundation. The SickKids University of Toronto Mead Johnson Chair in Nutritional Sciences provides unrestricted research funding support to J.K.H.
Duality of Interest
No potential conflicts of interest relevant to this article were reported.
Author Contributions
V.P and S.G. collected and interpreted data, contributed to conceptualization of study, drafted the initial manuscript, and reviewed/edited the manuscript. B.P.P. wrote the final manuscript and performed statistical analysis. J.K.H. contributed to conceptualization of the study, supervised data collection, interpreted data analysis, and reviewed/edited the manuscript. J.K.H. is the guarantor of this work as, as such had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
V.P. and B.P.P. contributed equally to this work.
References
- 1.Kawamura T. The importance of carbohydrate counting in the treatment of children with diabetes. Pediatr Diabetes 2007;8(Suppl. 6):57–62 [DOI] [PubMed] [Google Scholar]
- 2.Smart CE, Ross K, Edge JA, Collins CE, Colyvas K, King BR. Children and adolescents on intensive insulin therapy maintain postprandial glycaemic control without precise carbohydrate counting. Diabet Med 2009;26:279–285 [DOI] [PubMed] [Google Scholar]
- 3.Smart CE, King BR, McElduff P, Collins CE. In children using intensive insulin therapy, a 20-g variation in carbohydrate amount significantly impacts on postprandial glycaemia. Diabet Med 2012;29:e21–e24 [DOI] [PubMed] [Google Scholar]
- 4.Rabasa-Lhoret R, Garon J, Langelier H, Poisson D, Chiasson JL. Effects of meal carbohydrate content on insulin requirements in type 1 diabetic patients treated intensively with the basal-bolus (ultralente-regular) insulin regimen. Diabetes Care 1999;22:667–673 [DOI] [PubMed] [Google Scholar]
- 5.Sheard NF, Clark NG, Brand-Miller JC, et al. . Dietary carbohydrate (amount and type) in the prevention and management of diabetes: a statement by the American Diabetes Association. Diabetes Care 2004;27:2266–2271 [DOI] [PubMed] [Google Scholar]
- 6.Bishop FK, Maahs DM, Spiegel G, et al. . The Carbohydrate Counting in Adolescents with Type 1 Diabetes (CCAT) study. Diabetes Spectr 2009;22:56–62 [Google Scholar]
- 7.Gurnani M, Pais V, Cordeiro K, Steele S, Chen S, Hamilton JK. One potato, two potato,… assessing carbohydrate counting accuracy in adolescents with type 1 diabetes. Pediatr Diabetes 2018;19:1302–1308 [DOI] [PubMed] [Google Scholar]
- 8.Spiegel G, Bortsov A, Bishop FK, et al. . Randomized nutrition education intervention to improve carbohydrate counting in adolescents with type 1 diabetes study: is more intensive education needed? J Acad Nutr Diet 2012;112:1736–1746 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shah VN, Garg SK. Managing diabetes in the digital age. Clin Diabetes Endocrinol 2015;1:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.O’Brien T, Denham SA. Diabetes care and education in rural regions. Diabetes Educ 2008;34:334–347 [DOI] [PubMed] [Google Scholar]
- 11.Borus JS, Laffel L. Adherence challenges in the management of type 1 diabetes in adolescents: prevention and intervention. Curr Opin Pediatr 2010;22:405–411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vaala SE, Hood KK, Laffel L, Kumah-Crystal YA, Lybarger CK, Mulvaney SA. Use of commonly available technologies for diabetes information and self-management among adolescents with type 1 diabetes and their parents: a Web-based survey study. Interact J Med Res 2015;4:e24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Deacon AJ, Edirippulige S. Using mobile technology to motivate adolescents with type 1 diabetes mellitus: a systematic review of recent literature. J Telemed Telecare 2015;21:431–438 [DOI] [PubMed] [Google Scholar]
- 14.Graue M, Wentzel-Larsen T, Hanestad BR, Søvik O. Evaluation of a programme of group visits and computer-assisted consultations in the treatment of adolescents with type 1 diabetes. Diabet Med 2005;22:1522–1529 [DOI] [PubMed] [Google Scholar]
- 15.Frøisland DH, Arsand E, Skårderud F. Improving diabetes care for young people with type 1 diabetes through visual learning on mobile phones: mixed-methods study. J Med Internet Res 2012;14:e111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Han Y, Faulkner MS, Fritz H, et al. . A pilot randomized trial of text-messaging for symptom awareness and diabetes knowledge in adolescents with type 1 diabetes. J Pediatr Nurs 2015;30:850–861 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Horan PP, Yarborough MC, Besigel G, Carlson DR. Computer-assisted self-control of diabetes by adolescents. Diabetes Educ 1990;16:205–211 [DOI] [PubMed] [Google Scholar]
- 18.Brown SJ, Lieberman DA, Germeny BA, Fan YC, Wilson DM, Pasta DJ. Educational video game for juvenile diabetes: results of a controlled trial. Med Inform (Lond) 1997;22:77–89 [DOI] [PubMed] [Google Scholar]
- 19.Kamel Boulos MN, Gammon S, Dixon MC, et al. . Digital games for type 1 and type 2 diabetes: underpinning theory with three illustrative examples. JMIR Serious Games 2015;3:e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Razeghi S, Renner C, Schäfer S, et al. . Project D: computer-mediated communication as a tool for self-help in children and adolescents with diabetes. Diabetes Educ 1998;24:577–580 [DOI] [PubMed] [Google Scholar]
- 21.Harris MA, Freeman KA, Duke DC. Seeing is believing: using Skype to improve diabetes outcomes in youth. Diabetes Care 2015;38:1427–1434 [DOI] [PubMed] [Google Scholar]
- 22.Bellfield EJ, Sharp LK, Xia Y, Gerber BS. Use of a mobile app to facilitate blood glucose monitoring in adolescents with type 1 diabetes: single-subject nonrandomized clinical trial. JMIR Diabetes 2018;3:e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bin-Abbas B, Jabbari M, Al-Fares A, El-Dali A, Al-Orifi F. Effect of mobile phone short text messages on glycaemic control in children with type 1 diabetes. J Telemed Telecare 2014;20:153–156 [DOI] [PubMed] [Google Scholar]
- 24.Pereira K, Phillips B, Johnson C, Vorderstrasse A. Internet delivered diabetes self-management education: a review. Diabetes Technol Ther 2015;17:55–63 [DOI] [PubMed] [Google Scholar]
- 25.Boren SA, Gunlock TL, Peeples MM, Krishna S. Computerized learning technologies for diabetes: a systematic review. J Diabetes Sci Technol 2008;2:139–146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Koontz MB, Cuttler L, Palmert MR, et al. . Development and validation of a questionnaire to assess carbohydrate and insulin-dosing knowledge in youth with type 1 diabetes. Diabetes Care 2010;33:457–462 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rockett HR, Breitenbach M, Frazier AL, et al. . Validation of a youth/adolescent food frequency questionnaire. Prev Med 1997;26:808–816 [DOI] [PubMed] [Google Scholar]
- 28.Computrition Inc Food service software solutions. Available from https://www.computrition.com. Accessed 4 July 2015
- 29.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap): a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42:377–381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Inman M, Daneman D, Curtis J, et al. . Social determinants of health are associated with modifiable risk factors for cardiovascular disease and vascular function in pediatric type 1 diabetes. J Pediatr 2016;177:167–172 [DOI] [PubMed] [Google Scholar]
- 31.Mulvaney SA, Rothman RL, Wallston KA, Lybarger C, Dietrich MS. An Internet-based program to improve self-management in adolescents with type 1 diabetes. Diabetes Care 2010;33:602–604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Stinson J, Wilson R, Gill N, Yamada J, Holt J. A systematic review of Internet-based self-management interventions for youth with health conditions. J Pediatr Psychol 2009;34:495–510 [DOI] [PubMed] [Google Scholar]
- 33.Porter SJ, Chapman-Novakofski KM, Scherer JA. Your Guide to Diet and Diabetes: Web-based diabetes education tailored to Hispanics. J Nutr Educ Behav 2009;41:374–376 [DOI] [PubMed] [Google Scholar]
- 34.Nebel IT, Blüher M, Starcke U, Müller UA, Haak T, Paschke R. Evaluation of a computer based interactive diabetes education program designed to train the estimation of the energy or carbohydrate contents of foods. Patient Educ Couns 2002;46:55–59 [DOI] [PubMed] [Google Scholar]
- 35.Tascini G, Berioli MG, Cerquiglini L, et al. . Carbohydrate counting in children and adolescents with type 1 diabetes. Nutrients 2018;10:109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Joubert M, Armand C, Morera J, Tokayeva L, Guillaume A, Reznik Y. Impact of a serious videogame designed for flexible insulin therapy on the knowledge and behaviors of children with type 1 diabetes: the LUDIDIAB pilot study. Diabetes Technol Ther 2016;18:52–58 [DOI] [PubMed] [Google Scholar]
- 37.Datye KA, Moore DJ, Russell WE, Jaser SS. A review of adolescent adherence in type 1 diabetes and the untapped potential of diabetes providers to improve outcomes. Curr Diab Rep 2015;15:51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Grey M, Whittemore R, Jeon S, Murphy K, Faulkner MS, Delamater A; TeenCope Study Group . Internet psycho-education programs improve outcomes in youth with type 1 diabetes. Diabetes Care 2013;36:2475–2482 [DOI] [PMC free article] [PubMed] [Google Scholar]