Abstract
Aim
To compare marginal bone level changes around immediately placed and immediately provisionalized implants with immediately placed and delayed provisionalized implants in the aesthetic region after five years of function.
Materials and Methods
Forty patients with a failing tooth in the maxillary anterior region were randomly assigned immediate implant placement with immediate (Group A: n = 20) or delayed (Group B: n = 20) provisionalization. Definitive crown placement occurred three months after provisionalization. The primary outcomes were changes in marginal bone level. In addition, survival rates, buccal bone thickness, soft peri‐implant tissues, aesthetics and patient‐reported outcomes were assessed.
Results
After 5 years, the mean mesial and distal marginal bone level changes were 0.71 ± 0.68 mm and 0.71 ± 0.71 mm, respectively, in group A and 0.49 ± 0.52 mm and 0.54 ± 0.64 mm, respectively, in group B; the difference between the groups was not significant (p = .305 and p = .477, respectively). Implant and restoration survivals were 100%. No clinically relevant differences in buccal bone thickness or in mid‐facial peri‐implant mucosal level, aesthetic and patient outcomes were observed.
Conclusions
The mean marginal bone level changes following immediate implant placement and provisionalization were comparable with immediate implant placement and delayed provisionalization. (www.isrctn.com: ISRCTN57251089 and www.trialregister.nl: NL8255).
Keywords: aesthetic region, dental implants, immediate placement
Clinical Relevance.
Scientific rationale for the study: No 5‐year comparative studies, assessing the complete panel of outcome measures including changes in the hard‐ and soft‐tissue dimensions, buccal bone thickness, implant and restoration survival, aesthetic evaluation and patient‐reported outcome of immediate placement and provisionalization of dental implants in the maxillary aesthetic zone, have been published thus far.
Principal findings: There were no significant differences in marginal bone levels between immediate implant placement with immediate provisionalization and immediate placement with delayed provisionalization at the 5‐year follow‐up.
Practical implications: Immediate provisionalization of dental implants in post‐extraction sites in the maxillary aesthetic zone is a reliable alternative for delayed provisionalization.
1. INTRODUCTION
There is a growing tendency to place single‐tooth implants in the aesthetic zone immediately after extracting a failing tooth, preferably combined with immediate provisionalization (Tonetti et al., 2019; Slagter et al., 2014). Slagter et al. (2014) published a systematic review with a pooled analysis and demonstrated that immediate placement and provisionalization of dental implants in the aesthetic zone resulted in slightly less peri‐implant bone loss compared with immediate placement and delayed provisionalization, probably due to the extra surgical procedure. Other systematic reviews reporting short‐term results indicate that there is a slightly higher risk of implant loss with immediate placement in post‐extraction sockets compared with delayed placement in healed sites (Cosyn et al., 2019; Gallucci et al., 2018; Mello et al., 2017). However, one systematic review noted that immediately placed implants were accompanied by a better preservation of peri‐implant bone levels (Canellas et al., 2019). Furthermore, immediate implant placement seems to be well appreciated by patients (Huynh‐Ba et al., 2018) probably because the accompanying minimal invasive flapless surgery has less an impact on the hard and soft tissues than with delayed procedures (Weigl & Strangio, 2016). The common factor of these systematic reviews is that the patients for immediate implant placement, whether or not in combination with immediate provisionalization, should be carefully selected to minimize risks. They also mention that the data are still very limited, with too short evaluation periods and lack full‐scale evaluation parameters, including the stability of the labial mucosa and bone levels in the aesthetic region (Buser et al., 2017; Cosyn et al., 2019; Gallucci et al., 2018; Huynh‐Ba et al., 2018; Mello et al., 2017; Weigl & Strangio, 2016). This statement was also confirmed in a Consensus report and clinical recommendations of the XV European Workshop in Periodontology (Tonetti et al., 2019).
It has been shown that immediate provisionalization of implants in healed sites in the maxillary aesthetic region has a comparable 5‐year outcome with delayed provisionalization of implants (Cooper et al., 2014a; Den Hartog et al., 2016; Donos et al., 2019).
Prospective studies with a follow‐up of at least 5 years on immediate dental implant placement in the maxillary aesthetic region, in combination with immediate provisionalization studies are scarce and limited to Cooper et al., (2014b), Cosyn et al., (2016), Noelken et al. (2018), Raes, Cosyn, et al. (2018) and Raes, Eghbali, et al. (2018). Stability of buccal bone and mid‐facial mucosa level are critical outcome parameters in this field and should be part of follow‐up studies with a baseline pre‐operative status (Cosyn et al., 2019). Only Noelken et al. (2018) and Raes, Eghbali, et al. (2018) used both cone beam computed tomography (CBCT) to analyse buccal bone thickness and linear mid‐facial mucosa level measurements as part of the evaluation.
It can be concluded that full‐scale evaluation of immediate implant placement combined with immediate or delayed provisionalization with a follow‐up of at least 5 years is underreported in this field of implant dentistry. Therefore, the aim of this 5‐year comparative study was to compare peri‐implant bone changes, buccal bone thickness, mucosa levels, aesthetic ratings by professionals and patient‐reported satisfaction with the maxillary aesthetic region following immediate implant placement and provisionalization with immediate implant placement and delayed provisionalization.
2. MATERIALS AND METHODS
2.1. Study design
The study was designed as a comparative study with a follow‐up of 5 years. Recruitment of patients, implant treatment and follow‐up took place at the Department of Oral and Maxillofacial Surgery of the University Medical Center Groningen (UMCG), the Netherlands. The study was approved by the local medical ethical committee (NL32240.042.10) and registered in a trial register (www.isrctn.com: ISRCTN57251089 and www.trialregister.nl: NL8255). The follow‐up study, since it took part at regular routine control visits, without collection of extra data, is not a clinical research with test subjects as meant in the Medical Research Involving Human Subjects Act (WMO). Patients, however, gave oral informed consent for using their research data. This study was conducted in accordance with the requirements of the Helsinki Declaration of 1975 and revised in 2008 and CONSORT Guidelines. Written informed consent was obtained from all eligible patients before enrolment.
Eligible patients, aged >18 years, presented with a failing tooth in the maxillary aesthetic zone (incisor, canine or first pre‐molar) referred for single‐tooth implant treatment were asked to join this randomized clinical trial. Pre‐operatively, cone beam computed tomography (CBCT) was used to assess whether there was sufficient bone on the palatal side to place an implant, since for primary stability of the implant, sufficient palatal bone is necessary. Patients were excluded from participation in this study if they met ≥1 of the following criteria: (a) inadequate oral hygiene, (b) insufficient mesiodistal width for implant placement, (c) periodontal disease, (d) smoking, (e) general health does not permit a surgical procedure or (f) a vertical bony defect of ≥5 mm of the labial socket wall after removal of the tooth. The size of the bone defect was assessed after extraction of the failing tooth. The size was checked by a bone sounding technique with a periodontal probe at the labial side of the socket.
Details of the study design, sample size calculation and results of the one‐year follow‐up were described by Slagter et al. (2015). Informed consent was obtained from patients before surgical treatment was scheduled. A computerized random number generator (without specific criteria for randomization) was used for allocating patients to:
Group A: immediate implant placement (NobelActive, Nobel Biocare AB, Goteborg, Sweden) and immediate provisionalization
Group B: immediate implant placement (NobelActive, Nobel Biocare AB, Goteborg, Sweden) and delayed provisionalization
2.2. Surgical and prosthetic protocol
Pre‐operatively, patients started prophylactic antibiotic therapy (amoxicillin 500 mg t.i.d. for 7 days or clindamycin 300 mg q.i.d. in case of amoxicillin allergy). All surgeries were performed under local anaesthesia. The failing tooth was removed atraumatically, without raising a mucoperiosteal flap. The implant site was prepared on the palatal side of the alveolus using a surgical template based on the ideal position of the prospective restoration. The last used implant drill was placed as a space maintainer for the implant to be placed and to prevent that augmentation material fills the implant site. Subsequently, autogenous bone was gathered as grafting material from the retromolar–ramus area using a bonescraper (Bonescraper, Biomet 3i, Warsaw, Indiana, USA) and mixed 1:1 with anorganic bone (Geistlich Bio‐Oss, Geistlich Pharma AG, Wolhusen, Switzerland). After this, the gap between the drill and the alveolar walls was augmented with the mixture of autogenous bone and bone substitute. Subsequently, the implant drill was removed and the implant (NobelActive) was placed at a depth of 3 mm apical to the most apical aspect of the prospective clinical crown, guided by the surgical template. To facilitate positioning the depth of the implant, the surgical template was provided with an example of the prospective clinical crown in an ideal position as would going to be seen above the mucosal margin. The insertion torque of the implants in both groups was at least 45 Ncm, achieving primary stability.
In group A, an implant‐level impression was made immediately after implant placement and a screw‐retained provisional restoration was fabricated in the dental laboratory. The provisional restoration was screwed directly onto the implant with 20 Ncm by a manual torque wrench (Manual Torque Wrench Prosthetic; Nobel Biocare AB), within 24 hours after implant placement.
In group B, a corresponding cover screw was placed immediately after implant placement. To facilitate closure and healing of the grafted area, a free oval soft‐tissue graft, harvested from the palatal mucosa, was sutured on top of the reconstructed socket. The diameter of the punch was 2 mm larger than the socket access. That 2 mm of epithelium was removed from soft‐tissue graft. The 2 mm zone of the soft‐tissue graft denuded from epithelium was located beneath the mucosa at the recipient site. The graft was sutured with Ethilon 5‐0 (Johnson & Johnson, Amersfoort, the Netherlands) on top of the reconstructed socket. After three months, the implant was uncovered by a small incision at the cover screw site, followed by an implant‐level impression and placement of a provisional restoration, according to the procedure described for group A.
After a provisional phase of 3 months, a definitive zirconia‐based and porcelain‐veneered restoration was placed in both groups. Depending on the location of the screw access hole, the final crown was either a cemented‐retained or screw‐retained zirconia crown (Procera, NobelBiocare AB). Abutment screws were torqued with 32 Ncm. Cement‐retained crowns were cemented with glass ionomer cement (Fuji Plus, GC Europe, Leuven, Belgium).
2.3. Outcome measures
The primary outcome measure of this study was the change in marginal peri‐implant bone level (MBL) proximal to the implant, 5 years after placing the definitive crown.
Secondary outcome measures included implant and restoration survival and changes in interproximal peri‐implant mucosa (IML), mid‐facial peri‐implant mucosal level (MML) and buccal bone thickness (BBT). Furthermore, papilla volume, peri‐implant mucosa health, amount of plaque, amount of bleeding and pocket probing depth were assessed. Aesthetic outcome was assessed by means of an objective index, and patients' satisfaction was measured using a visual analogue scale (VAS).
2.4. Survival rate
The implants' survival rate was defined as the percentage of functional implants five years after definitive crown placement in both groups, following the Smith and Zarb (1989) criteria for successful osseointegration. The definitive restorations' survival rate was defined as the percentage of functional initial restorations still in situ.
2.5. Radiographic assessments
Standardized digital peri‐apical radiographs were taken with a custom‐made aiming device, with extensions for stability on the occlusal and palatal surface of neighbouring teeth (Meijndert et al., 2004), immediately after implant placement (baseline = T0), and one (T1), and sixty (T60) months after definitive crown placement. The vertical distance from the shoulder of the implant to the first‐bone‐to‐implant contact was measured at the distal and mesial site of the implant. Changes in MBL, in relation to peri‐implant bone level at baseline, were calculated at T1 and T60.
To define the presence and thickness of buccal bone at the time of tooth extraction and to measure changes in the BBT over time, CBCTs (iCAT 3D exam scanner, KaVo Dental GmbH, Biberach, Germany) were made before extraction and 1 month and 5 years after placing the final restoration. First, the CBCT Digital Imaging and Communications in Medicine (DICOM) files were imported into a medical image computing program (Maxilim, version 2.3, Medicim, Sint‐Niklaas, Belgium). Second, the exact position of the implant was then determined with Multimodality Image Registration using Information Theory (Maes et al., 1997) and a Maxilim file with the exact coordinates of the implant in the particular patient was created. Third, the planning software used these coordinates to align a planning implant onto the exact same position (NobelClinician, version 2.1, Nobel Biocare‐Guided Surgery Center, Mechelen, Belgium). Fourth, measurements of the buccal bone (in mm) could be done. The area of interest was the upper 5 mm section of the implant starting at the implant neck towards the apical point (location M1, M2, M3, M4, M5). The distance of the buccal bone outline to the centre of the implant was measured for each location. The radius of the interior contour of the implant, as provided by the manufacturer for each location, was then subtracted from this measurement to determine the distance of the outline of the implant to the buccal bone outline. This measuring method prevented measurements at the interface between implant and bone which are disturbed by scattering. The method applied results in measurements made at the most outer buccal contour of the implant relative to the dental arch.
Due to this method, the actual thickness of the bone wall buccally of the failing tooth is not measured, but the distance from the future implant to the outer contour of the buccal bone wall. These values can be used for comparison with the after implant placement follow‐up period.
More details of the methods for measuring buccal bone thickness and the results of the one‐year follow‐up were described by Slagter, Raghoebar, et al. (2015), Slagter et al. (2017) and Meijer et al. (2019).
Radiographs are made routinely to monitor peri‐implant bone levels at start of loading and at least at 1‐year follow‐up and thereafter at 5 years, 10 years, etc. This is done with intra‐oral radiographs for approximal bone levels. In case of anterior implants, additional CBCT scans are advised for monitoring the buccal bone level.
2.6. Photographic assessments
Standardized digital photographs (Nikon D300 s, Nikon Corporation, Yurakucho, Tokyo, Japan) were taken before implant placement (Tpre) and after definitive crown placement, at T1 and T60, using the technique described earlier (Meijndert et al., 2004). The IML and MML changes were compared with the original gingival level of the failing tooth.
2.7. Clinical assessments
The following clinical variables were assessed at Tpre, T1 and T60:
Papilla volume: assessing the mesial and distal papilla adjacent to the implant using the papilla index (Jemt, 1997)
Amount of plaque: assessed at four sites per implant/adjacent tooth (mesial, buccal, distal and palatal) using the modified plaque index (Mombelli, van Oosten, Schurch Jr, & Land, 1987)
Amount of bleeding: using the modified sulcus bleeding index (Mombelli et al., 1987)
Gingiva: using the Gingival Index (Löe & Silness, 1963)
Probing pocket depth: assessed at four sites per implant/adjacent tooth (mesial, buccal, distal and palatal), measured to the nearest 1 mm
2.8. Peri‐implant mucositis and peri‐implantitis
Incidence of peri‐implant mucositis and peri‐implantitis was calculated. As definition for peri‐implant mucositis and peri‐implantitis, the consensus reached at the 2017 World Workshop on the Classification of Periodontal and Peri‐Implant Diseases and Conditions (Berglundh et al., 2018) has been used, being:
peri‐implant mucositis (radiographic bone loss <2 mm): BoP+ and/or suppuration and
peri‐implantitis: BoP+ and/or suppuration in combination with increased probing depth compared with previous examinations and in combination with marginal bone loss beyond crestal bone level changes resulting from initial bone remodelling (≥2 mm)
2.9. Aesthetic assessment
The aesthetic outcome was assessed from standardized digital photographs (Nikon D300s, Nikon Corporation) taken at Tpre, T1 and T60 in both groups. Peri‐implant mucosa and implant restoration aesthetic outcomes were determined using the Pink Esthetic score/ White Esthetic Score (PES/WES) (Belser et al., 2009).
2.10. Patients' satisfaction
Overall patient satisfaction was assessed at T1 and T60 with a VAS and scores ranging from 0 to 10 (0 = completely dissatisfied to 10 = completely satisfied).
2.11. Statistical analysis
Group differences were evaluated by one‐way analyses of variance (ANOVA) for continuous data and by Fisher's exact test for categorical data. The Mann–Whitney U test was used to calculate possible significant differences between the groups' BBT medians. The normal distributed data, shown by means ± standard deviation (SD), were analysed using ANCOVA to test the effect of the pre‐operative bone defect on change in BBT. A p‐value of .05 was considered to indicate statistical significance. All analyses were performed using SPSS (PASW Statistics 20.0, SPSS Inc.; IBM Corporation, Chicago, IL, USA).
3. RESULTS
3.1. Patients
Twenty patients (male/female: 5/15) were included in group A with a mean age of 39 ± 16.9 years and with either central incisor (n = 7), lateral incisor (n = 8) and cuspid (n = 5) failing teeth. Twenty patients (male/female: 8/12) were included in group B with a mean age of 42 ± 14.2 years and with either central incisor (n = 13), lateral incisor (n = 6) and cuspid (n = 1) failing teeth. The division of 4.3 mm diameter implants with a regular platform and 3.5 mm diameter implants with a narrow platform was 12/8 and 15/5 in, respectively, group A and group B. All patients had bony defects of the socket wall in the vertical direction after removing the failing tooth, but always <5 mm. The mean size of the defect was 3.4 ± 1.2 mm and 4.2 ± 1.1 mm in, respectively, group A and group B.
All the patients received their assigned treatment. The 5‐year follow‐up analysis consisted of 18 group A patients (1 patient moved abroad and 1 patient moved without leaving an address) and 17 group B patients (1 patient died, 1 patient moved too far to participate and 1 patient moved without leaving an address; Figure 1).
Figure 1.
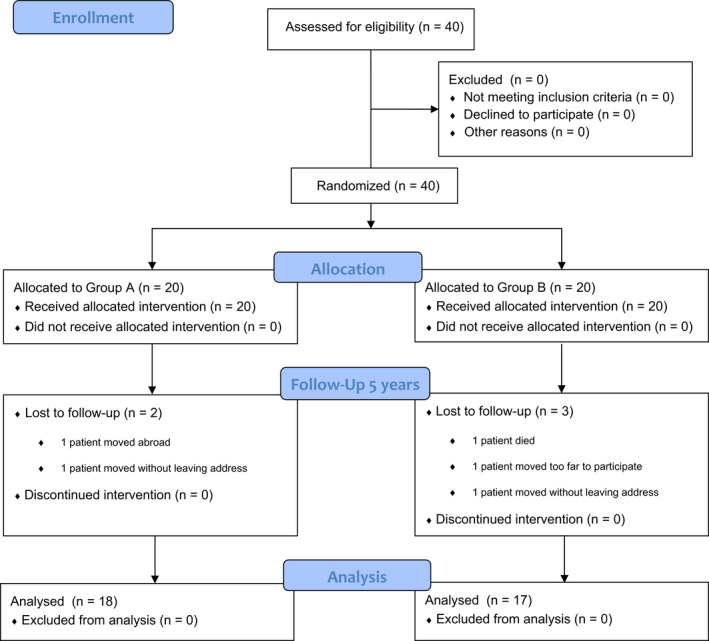
Consort flow diagram
3.2. Survival rate
No implants were lost during the study resulting in an implant survival rate of 100% in both groups five years after definitive restoration placement. Restoration survival was 88.9% in group A (2 patients needed new restorations due to porcelain chipping) and 88.2% in group B (1 patient needed 2 new restorations due to a zirconia abutment fracture).
3.3. Marginal bone level and buccal bone thickness changes
Table 1 shows the mean MBL changes at the mesial and distal site after 1 month and 60 months in relation to the condition at implant placement. The greatest MBL change was observed from implant placement until T1 in both groups. Thereafter, only minor changes were observed in both groups until T60, without a significant difference (Group A: 0.71 ± 0.68 mm mesially and 0.71 ± 0.71 mm distally vs. group B: 0.49 ± 0.52 mm mesially and 0.54 ± 0.64 mm distally; p = .305 and p = .477 for the mesial and distal sides, respectively, Figure 2).
Table 1.
Changes in marginal bone level from implant placement (baseline) to 1 month (T1) and to 60 months (T60) and changes in marginal soft‐tissue level from pre‐operative (Tpre) to 1 month (T1) and to 60 months (T60) after definitive crown placement
| Variable | Mean (SD) | Mean (SD) | p‐value* | Mean (SD) | Mean (SD) | p‐value* |
|---|---|---|---|---|---|---|
| Group A | Group B | Group A | Group B | |||
| Marginal bone level changes in mm (±SD) | Baseline‐T1 | Baseline‐T1 | Baseline‐T60 | Baseline‐T60 | ||
| Mesial of implant | −0.70 (0.67) | −0.68 (0.64) | .921 | −0.71 (0.68) | −0.49 (0.52) | .305 |
| Distal of implant | −0.69 (0.71) | −0.64 (0.63) | .802 | −0.71 (0.71) | −0.54 (0.64) | .477 |
| Marginal soft‐tissue level changes in mm (±SD) | Tpre‐T1 | Tpre‐T1 | Tpre‐T60 | Tpre‐T60 | ||
| Mesial of implant | −0.90 (0.45) | −0.44 (0.45) | .003 | −1.19 (0.93) | −0.65 (0.66) | .066 |
| Distal of implant | −0.44 (0.45) | −0.78 (0.67) | .543 | −1.18 (0.84) | −1.20 (0.95) | .935 |
| Mid‐facial of implant | −1.15 (0.81) | −0.78 (0.86) | .184 | −1.44 (0.98) | −0.81 (1.01) | .082 |
One‐way analysis of variance (ANOVA).
Figure 2.
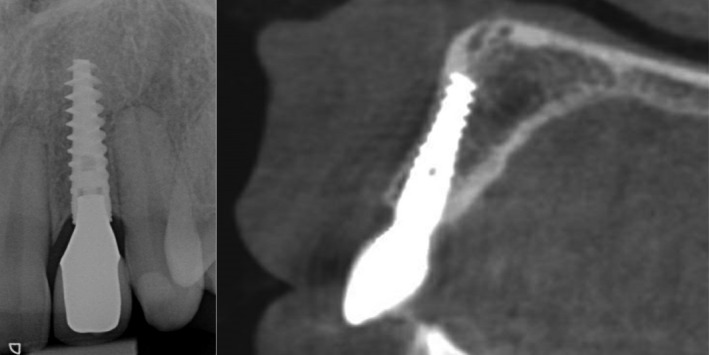
Intra‐oral radiograph and cone beam computed tomography of implant of group A (immediate implant placement/immediate provisionalization) in position 22 after 5 years in function
Table 2 depicts the BBT medians and interquartile ranges for the various levels (M0 to M5) at Tpre, T1 and T60. Analysing pre‐operative CBCT scans, there are no significant differences in the distance from the future implant to the outer contour of the buccal bone wall between the groups at all 6 positions. At the 5‐year evaluation, there was significantly less BBT in group B in 4 out of 6 positions along the implant axis (Figure 2). In both groups, the pre‐operative bone defect showed no significant correlation with the change in BBT between Tpre and T60 (p = .63).
Table 2.
Buccal bone thickness pre‐extraction, 1 month and 5 years after dental implant surgery in group A (immediate placement/immediate provisionalization) and group B (immediate placement/delayed provisionalization), expressed as medians and significant differences between the groups
| Group A | Group B | Significance* (p) | |
|---|---|---|---|
| Median (interquartile range) in mm | Median (interquartile range) in mm | ||
| Buccal bone thickness pre‐extraction | |||
| M0 (at neck) | 2.23 [1.84;2.74] | 2.14 [1.64;2.59] | .639 |
| M1 | 2.26 [1.56;2.56] | 2.16 [1.74;2.54] | 1.000 |
| M2 | 2.43 [2.08;2.78] | 2.23 [1.60;2.48] | .175 |
| M3 | 2.33 [1.93;2.45] | 2.23 [1.54;2.34] | .165 |
| M4 | 2.15 [1.65;2.35] | 1.95 [1.54;2.35] | .415 |
| M5 | 1.64 [1.36;2.15] | 1.94 [1.50;2.45] | .552 |
| Buccal bone thickness 1 month | |||
| M0 (at neck) | 2.04 [0.73;2.54] | 0.94 [0.54;1.98] | .125 |
| M1 | 2.26 [1.73;2.46] | 1.06 [0.51;2.36] | .071 |
| M2 | 2.23 [1.78;2.73] | 1.48 [0.60;2.25] | .026 |
| M3 | 2.23 [1.75;2.45] | 1.34 [0.57;2.01] | .009 |
| M4 | 1.93 [1.63;2.25] | 1.45 [0.45;1.91] | .022 |
| M5 | 1.54 [1.26;2.04] | 1.21 [0.38;1.62] | .088 |
| Buccal bone thickness 5 years | |||
| M0 (at neck) | 1.24 [0.73;2.34] | 0.88 [0.64;2.13] | .381 |
| M1 | 2.05 [1.23;2.44] | 1.53 [0.66;2.16] | .145 |
| M2 | 2.11 [1.64;2.48] | 1.48 [0.98;2.08] | .027 |
| M3 | 2.19 [1.82;2.38] | 1.43 [0.85;1.65] | <.001 |
| M4 | 1.94 [1.43;2.14] | 1.05 [0.65;1.45] | .001 |
| M5 | 1.65 [1.13;1.91] | 1.06 [0.56;1.36] | .001 |
Mann–Whitney U test for significant differences between medians of groups at three time points.
3.4. Interproximal and mid‐facial peri‐implant mucosal level changes
Table 1 shows the soft‐tissue level changes from the pre‐operative situation up to 60 months after placing the definitive restorations at the mesial, distal and mid‐facial sites. The 5‐year mid‐facial follow‐up soft‐tissue level change was 1.44 ± 0.98 mm and 0.81 ± 1.01 mm in group A and group B, respectively, without a significant difference (p = .082).
3.5. Clinical outcome
A healthy mucosa and low plaque and bleeding indexes could be seen at all evaluation periods for both groups, without significant differences (Table 3). Pocket probing depth remained stable for both groups in all four measured sites, without significant differences between the groups (Table 3).
Table 3.
Clinical outcome measures (papilla index, gingival index, plaque index, bleeding index and pocket probing depth) in means (with standard deviations) at pre‐operative and 1 month (T1) and 60 months (T60) after definitive crown placement
| Variable | Tpre | p‐value* | T1 | p‐value* | T60 | p‐value* | |||
|---|---|---|---|---|---|---|---|---|---|
| Group A | Group B | Group A | Group B | Group A | Group B | ||||
| Papilla volume (papilla index) | |||||||||
| Mesial | 1.95 (1.10) | 1.95 (0.85) | .99 | 2.16 (0.83) | 2.37 (0.60) | .38 | 2.56 (0.78) | 2.60 (0.74) | 1.000 |
| Distal | 2.05 (0.99) | 1.68 (0.67) | .19 | 2.37 (0.76) | 2.00 (0.67) | .12 | 2.50 (0.79) | 2.40 (0.64) | .239 |
| Health of gingiva (gingival index) | 0.00 (0.00) | 0.00 (0.00) | NA | 0.90 (0.31) | 0.79 (0.42) | .35 | 0.00 (0.00) | 0.00 (0.00) | NA |
| Amount of plaque (plaque index) | 0.10 (0.31) | 0.05 (0.23) | .59 | 0.00 (0.00) | 0.05 (0.23) | .31 | 0.00 (0.00) | 0.00 (0.00) | NA |
| Bleeding after probing (bleeding index) | 0.75 (0.55) | 0.68 (0.58) | .71 | 0.60 (0.60) | 0.47 (0.61) | .52 | 0.39 (0.70) | 0.20 (0.41) | .678 |
| Pocket probing depth (mm) | |||||||||
| Mesial | 2.70 (0.80) | 2.44 (0.71) | .31 | 3.50 (0.83) | 3.21 (0.71) | .25 | 3.61 (1.24) | 3.00 (0.38) | .077 |
| Distal | 2.85 (1.09) | 2.61 (0.70) | .43 | 3.15 (0.49) | 3.21 (0.92) | .80 | 3.06 (0.94) | 3.13 (0.83) | .805 |
| Buccal | 1.60 (0.75) | 1.89 (0.96) | .31 | 2.65 (1.42) | 2.79 (0.86) | .72 | 2.44 (1.04) | 2.80 (0.68) | .265 |
| Palatal | 1.65 (0.81) | 2.06 (0.80) | .13 | 2.30 (0.66) | 2.79 (0.42) | .18 | 2.72 (0.58) | 2.67 (0.49) | .769 |
Abbreviation: NA, not applicable.
Fisher's exact test for the indices of papilla, gingiva, plaque and bleeding; one‐way analysis of variance (ANOVA) for pocket probing depth.
3.6. Peri‐implant mucositis and peri‐implantitis
Incidence of peri‐implant mucositis was 22.4% and 17.6%, and of peri‐implantitis 5.6% and 0% in group A and group B, respectively.
3.7. Aesthetic assessment
Both groups' PES/WES scores were acceptable after five years, as shown in Table 4. The total aesthetic outcome was 15.44 ± 2.64 in group A and 15.73 ± 2.15 in group B (p = .736) (Figure 3).
Table 4.
Mean values (SD) of aesthetic evaluation and overall patient satisfaction at pre‐operative (Tpre) and 1 month (T1) and 60 months (T60) after definitive crown placement
| Variable | Tpre | p‐value* | T1 | p‐value* | T60 | p‐value* | |||
|---|---|---|---|---|---|---|---|---|---|
| Group A | Group B | Group A | Group B | Group A | Group B | ||||
| PES | 7.00 (2.05) | 6.90 (1.32) | .631 | 7.80 (1.66) | 7.40 (1.59) | .711 | 7.83 (1.69) | 7.07 (1.79) | .216 |
| WES | 5.00 (2.33) | 5.40 (1.65) | .702 | 7.99 (1.73) | 7.60 (1.09) | .682 | 7.50 (2.12) | 8.27 (1.53) | .252 |
| PES/WES | 11.60 (3.33) | 11.10 (3.46) | .433 | 16.20 (2.20) | 15.10 (1.71) | .383 | 15.44 (2.64) | 15.73 (2.15) | .736 |
| Overall patient satisfaction (score 0–10) | 7.9 (1.8) | 8.1 (1.7) | .634 | 8.4 (1.1) | 8.7 (1.8) | .654 | |||
PES, Pink Esthetic score; WES, White Esthetic Score.
One‐way analysis of variance (ANOVA).
Figure 3.

Photograph of implant restoration of patient of group A (immediate implant placement/immediate provisionalization) in position 22 after 5 years in function (same patient as in Figure 2)
3.8. Patients' satisfaction
The overall patient satisfaction was high in both groups, whereby the 5‐year follow‐up VAS‐scores were 8.4 ± 1.1 and 8.7 ± 1.8 for groups A and B, respectively (p = .654).
4. DISCUSSION
Both immediate implant placement with immediate provisionalization and immediate implant placement with delayed provisionalization were accompanied by minor peri‐implant bone loss. At the 5‐year evaluation, the only significant, although clinically irrelevant, difference between both procedures was that the implants of the immediate provisionalization group were buccally covered with a slightly thicker layer of bone.
Buser et al., (2017) recommended that immediate implant placement can be used in ideal clinical situations, being a fully intact facial bone wall with a thick wall phenotype (>1 mm) and a thick gingival biotype). At the same time, they mention that a thick wall phenotype is rarely present in the anterior maxilla. Possible risks would be recession of the facial mucosa and orofacial flattening of the soft‐tissue profile. The results of the present study do not support these recommendations. In the present study, there was not always an intact facial wall, patients were not selected having a thick facial bone wall and also thin gingival biotypes were present. Notwithstanding the presence of those risk factors, results after a midterm follow‐up period were good.
Prospective studies with a follow‐up of at least 5 years after immediate dental implant placement in the maxillary aesthetic region, in combination with immediate provisionalization, are limited to Cooper et al. (2014b), Cosyn et al. (2016), Noelken et al. (2018) and Raes, Cosyn, et al. (2018), Raes, Eghbali, et al. (2018). The two Raes, Cosyn, et al. (2018) manuscripts evaluated the same study group over a period of 8 years. However, a comparative study with immediate implant placement and delayed provisionalization has not been done before.
4.1. Survival rate
The implant survival rate in the above‐mentioned studies varied from 93.8% to 100%, which is comparable with the present study's survival rate of 100%. The same holds on comparing the 5‐year results in a systematic review on the survival rate of implant‐supported single‐tooth replacement in general where the calculated percentage was high at 97.2 (Jung et al., 2012). Of the immediate placement and immediate provisionalization studies with a 5‐year follow‐up, only Cosyn et al. (2016) mentioned a restoration survival rate, being 94.1%. A 96.3% survival rate was calculated for implant‐supported restorations in general (Jung et al., 2012). The present study found 88.9% in group A and 88.2% in group B. This lower restoration survival rate could have been due to the use of porcelain as veneering material and zirconia as abutment material, which materials are known for their higher complication rates (Pjetursson et al., 2018; Rabel et al., 2018).
4.2. Peri‐implant hard tissue dimensions
Cosyn et al. (2016) mentioned an approximal bone loss of 0.12 mm after 1 year and 0.19 mm after 5 years. Raes, Cosyn, et al. (2018) reported a bone gain of 1.01 mm 1 year and 0.98 mm 8 years after implant placement. In our study, group A received the same treatment as the aforementioned studies and had an approximal bone loss of 0.70 mm and 0.71 mm after 1 and 5 years, respectively. These numbers differ among the three studies. This could be because of different surgical procedures, for instance in the study of Raes, Cosyn, et al. (2018) no bone grafts were used. But probably also because of the difficulty in interpreting bone‐to‐implant contact at baseline, the implant does not fit exactly in the extraction socket and therefore measurements are difficult and might differ among studies. Nevertheless, it is striking that the changes are minimal between 1 and 5 years in all three studies, meaning that peri‐implant bone levels remain rather stable after healing and maturation. In all three studies, an implant design with an implant‐abutment conical connection with platform‐switching was used. In the review of Romanos and Javed (2014), control of micromotion between implant and abutment is stated to be an important factor that influences stability of crestal bone levels. Also in the clinical study of Romanos et al. (2015), it appeared that conical connections, probably because of its stability, results in limited peri‐implant bone loss during a long‐term follow‐up period. Next to this, also the feature of platform‐switching contributes to preservation of peri‐implant bone levels (De Medeiros et al., 2016). A stable connection between abutment and implant, together with platform‐switching, indisputable contributes to less peri‐implant bone level changes, but it must be said that good oral hygiene and a strict maintenance protocol is absolutely mandatory for these stable bone levels.
Only the Noelken et al. (2018) and Raes, Eghbali, et al. (2018) studies used cone beam computed tomography (CBCT) to analyse buccal bone thickness. Noelken et al. (2018) had a BBT of 1.18, 1.28 and 1.11 mm, respectively, at 1, 3 and 6 mm along the implant axis measured from the neck of the implant. Raes, Eghbali, et al. (2018) calculated a BBT of 1.12, 1.32 and 0.95 mm, respectively, at 1, 3 and 5 mm along the implant axis. The BBT of group A of the present study varied from 1.24 to 2.19 mm in the first 5 mm along the implant axis, starting at the neck of the implant. The thickness of the buccal bone was also 1–2 mm at the end of the other three studies' evaluation periods. Group B's BBTs varied, in this study, along the implant axis at T1 and were significantly less at T60. Pre‐existent bone volume can be excluded as a possible reason, because there were no significant differences with the buccal bone thickness before extracting the failing tooth. It seems that immediate provisionalization preserves the buccal bone layer better than delayed provisionalization. Perhaps the presence of a provisional restoration appears to trigger, together with some oral function, the conservation of newly augmented buccal bone. In both groups, there is small buccal bone thickness gain between T1 and T60 at some positions, but also at some positions there is a small loss in thickness. One could say that buccal bone thickness is more or less stable at most positions between T1 and T60.
4.3. Interproximal and mid‐facial peri‐implant mucosal level changes
A systematic review reported that immediate implant placement is associated with an increased risk of peri‐implant soft‐tissue recession (Cosyn et al., 2012). This study's soft‐tissue level change mid‐facially, compared with the pre‐operative situation, was −1.44 ± 0.98 mm and −0.81 ± 1.01 mm in group A and group B, respectively. It must be mentioned that most of recession occurred in the first follow‐up period and remained more or less stable thereafter. A comparison of mid‐facial soft tissues after 5 years is only possible with the Cosyn et al. (2016) study. They reported a recession of 0.53 mm, which is less than in the present study. Prosthetic procedures, as well as the implant system, appear to be similar, but it must be mentioned that in a number of cases in the study of Cosyn et al. (2016) connective tissue grafts were applied to compensate for recession. Other studies did not take the pre‐operative soft‐tissue level as a starting point, thus missing the possible effect in the first months after extraction, or did not mention soft‐tissue changes at all. Nevertheless, it must be mentioned that mid‐facial soft‐tissue recession takes place and must be considered before treatment.
In group A, the surgical site with the implant and augmented bone was closed with the provisional restoration. In group B, this surgical site was closed with a free soft‐tissue graft. This is a difference in treatment and could have had an impact of soft‐tissue outcome. Although not significantly different, there is a trend of less recession of mid‐facial soft tissue in group B, which might be caused by the extra surgery with a soft‐tissue graft. Further research with a sufficient group size should be carried out to unveil this.
4.4. Clinical outcome
A healthy peri‐implant situation existed at the 5‐year evaluation. Papilla volume, pocket probing depths and the health of the peri‐implant soft tissues remained stable throughout the study period, while the plaque and bleeding indexes remained low in both groups. Other studies with a follow‐up of at least 5 years also mentioned positive clinical outcomes (Cooper et al., 2014b; Cosyn et al., 2016; Noelken et al., 2018 and Raes, Cosyn, et al., 2018).
4.5. Peri‐implant mucositis and peri‐implantitis
Derks and Tomasi (2015) reported in a systematic review with meta‐analysis a prevalence of 43% for peri‐implant mucositis and 22% for peri‐implantitis. In the present study, much lower values were reported, but it must be kept in mind that the systematic review included groups with a high heterogeneity in population and treatment.
4.6. Aesthetic assessments
The high PES/WES scores did not differ statistically between both groups and are comparable with the aesthetic results published in the literature regarding single‐tooth implants in the aesthetic zone of healed sites (Meijndert et al., 2020). However, none of the other 5‐year studies of immediate placement used the modified PES/WES scoring.
4.7. Patients' satisfaction
Immediate placement and provisionalization are known to be associated with high subjective satisfaction rates (Hartlev et al., 2014). This is in line with the satisfaction perceived by the patients in our study. Only Raes, Cosyn, et al. (2018) reported high patient satisfaction scores for a number of parameters.
4.8. Limitations
Some limitations have to be addressed. First, when determining the group size at the start of the study, it was calculated that 19 patients would be needed per group to detect a possible difference in marginal bone level change (Slagter, Meijer, et al., 2015). After 5 years, 18 patients could be analysed in group A and 17 patients in group B, meaning that the conclusions on marginal bone level change have lost some power. Second, this was a university‐based study with experienced professionals and dedicated patients to a strict hygiene protocol, consisting of information, checking and reinstruction of dental hygiene procedures at every visit. The patients were carefully selected to fit in the research protocol. Thus, the results of the present study may deviate from those achieved by a general practice.
The gap between the labial bony plate and the implant was in the present study augmented with a mixture of autologous bone and a bone substitute. At the time of defining the study protocol, it was thought to have the best predictable result. Being aware that this also induces an extra surgical site, with extra morbidity in the retromolar–ramus area, one could argue that perhaps only using a bone substitute would give the same result. Further research is needed to explore this idea.
In both groups, implant placement was taken as baseline measurement for intraoral radiographs. However, there is a different situation at start in both groups: in case of immediate provisionalization changes in peri‐implant bone level can be caused by healing and maturation after implant placement together with changes caused by loading and exposure to the oral cavity, whereas in the delayed provisionalization group changes in peri‐implant bone level can only be caused by healing and maturation after implant placement. This could lead to differences in interpretation of outcomes.
Another limitation is that the level of smile line was not included in the study. Smile line could have influenced the patient's opinion on the final result as expressed in the outcome Overall patient satisfaction.
Here, the bony defect should not have been larger than 5 mm. Given this study's seemingly favourable immediate placement outcomes, immediate placement in a larger bony defect should certainly be considered.
5. CONCLUSION
Within the limitations of this study, one can conclude that mean marginal bone level changes following immediate implant placement and provisionalization were comparable with immediate implant placement and delayed provisionalization. Hard‐ and soft‐tissue outcomes were favourable and professionals and patients were satisfied with the aesthetic result.
CONFLICT OF INTEREST
The authors declare that there are no conflicts of interest.
AUTHOR CONTRIBUTIONS
KWS, GMR and HJAM made substantial contributions to conception and design of the study. KWS, HJAM, DFMH and AV contributed to acquisition, analysis and interpretation of data. KWS, GMR, AV and HJAM contributed to drafting the article and revised it critically for important intellectual content. All authors approved the final version of the article to be published.
Funding informationThe study was supported by an unrestricted grant from Nobel Biocare Services AG: implant materials were provided (materials grant: 2009‐851).
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- Belser, U. C. , Grutter, L. , Vailati, F. , Bornstein, M. M. , Weber, H. P. , & Buser, D. (2009). Outcome evaluation of early placed maxillary anterior single‐tooth implants using objective esthetic criteria: A cross‐sectional, retrospective study in 45 patients with a 2‐ to 4‐year follow‐up using pink and white esthetic scores. Journal of Periodontology, 80(1), 140–151. 10.1902/jop.2009.080435 [DOI] [PubMed] [Google Scholar]
- Berglundh, T. , Armitage, G. , Araujo, M. G. , Avila‐Ortiz, G. , Blanco, J. , Camargo, P. M. , Chen, S. , Cochran, D. , Derks, J. , Figuero, E. , Hämmerle, C. H. F. , Heitz‐Mayfield, L. J. A. , Huynh‐Ba, G. , Iacono, V. , Koo, K. T. , Lambert, F. , McCauley, L. , Quirynen, M. , Renvert, S. , Salvi, G. E. , & Zitzmann, N. (2018). Peri‐implant diseases and conditions: Consensus report of workgroup 4 of the 2017 World Workshop on the Classification of Periodontal and Peri‐Implant Diseases and Conditions. Journal of Clinical Periodontology, 45(Suppl 20), S286–S291. 10.1111/jcpe.12957 [DOI] [PubMed] [Google Scholar]
- Buser, D. , Chappuis, V. , Belser, U. C. , & Chen, S. (2017). Implant placement post extraction in esthetic single tooth sites: When immediate, when early, when late? Periodontology 2000, 73(1), 84–102. 10.1111/prd.12170 [DOI] [PubMed] [Google Scholar]
- Canellas, J. V. D. S. , Medeiros, P. J. D. , Figueredo, C. M. D. S. , Fischer, R. G. , & Ritto, F. G. (2019). Which is the best choice after tooth extraction, immediate implant placement or delayed placement with alveolar ridge preservation? A systematic review and meta‐analysis. Journal of Craniomaxillofacial Surgery, 47(11), 1793–1802. 10.1016/j.jcms.2019.08.004 [DOI] [PubMed] [Google Scholar]
- Cooper, L. F. , Reside, G. , Raes, F. , Garriga, J. S. , Tarrida, L. G. , Wiltfang, J. , Kern, M. , & De Bruyn, H. (2014a). Immediate provisionalization of dental implants in grafted alveolar ridges in the esthetic zone: A 5‐year evaluation. International Journal of Periodontics & Restorative Dentistry, 34(4), 477–486. 10.11607/prd.2022 [DOI] [PubMed] [Google Scholar]
- Cooper, L. F. , Reside, G. J. , Raes, F. , Garriga, J. S. , Tarrida, L. G. , Wiltfang, J. , Kern, M. , & De Bruyn, H. (2014b). Immediate provisionalization of dental implants placed in healed alveolar ridges and extraction sockets: A 5‐year prospective evaluation. International Journal of Oral and Maxillofacial Implants, 29(3), 709–717. 10.11607/jomi.3617 [DOI] [PubMed] [Google Scholar]
- Cosyn, J. , De Lat, L. , Seyssens, L. , Doornewaard, R. , Deschepper, E. , & Vervaeke, S. (2019). The effectiveness of immediate implant placement for single tooth replacement compared to delayed implant placement: A systematic review and meta‐analysis. Journal of Clinical Periodontology, 46(Suppl 21), 224–241. 10.1111/jcpe.13054 [DOI] [PubMed] [Google Scholar]
- Cosyn, J. , Eghbali, A. , Hermans, A. , Vervaeke, S. , De Bruyn, H. , & Cleymaet, R. (2016). A 5‐year prospective study on single immediate implants in the aesthetic zone. Journal of Clinical Periodontology, 43(8), 702–709. 10.1111/jcpe.12571 [DOI] [PubMed] [Google Scholar]
- Cosyn, J. , Hooghe, N. , & De Bruyn, H. (2012). A systematic review on the frequency of advanced recession following single immediate implant treatment. Journal of Clinical Periodontology, 39(6), 582–589. 10.1111/j.1600-051X.2012.01888.x [DOI] [PubMed] [Google Scholar]
- De Medeiros, R. A. , Pellizzer, E. P. , Vechiato Filho, A. J. , Dos Santos, D. M. , Da Silva, E. V. , & Goiato, M. C. (2016). Evaluation of marginal bone loss of dental implants with internal or external connections and its association with other variables: A systematic review. Journal of Prosthetic Dentistry, 116(4), 501–506.e5. 10.1016/j.prosdent.2016.03.027 [DOI] [PubMed] [Google Scholar]
- Den Hartog, L. , Raghoebar, G. M. , Stellingsma, K. , Vissink, A. , & Meijer, H. J. A. (2016). Immediate loading of anterior single‐tooth implants placed in healed sites: Five‐year results of a randomized clinical trial. International Journal of Prosthodontics, 29(6), 584–591. 10.11607/ijp.4993 [DOI] [PubMed] [Google Scholar]
- Derks, J. , & Tomasi, C. (2015). Peri‐implant health and disease. A systematic review of current epidemiology. Journal of Clinical Periodontology, 42(Suppl 16), S158–S171. 10.1111/jcpe.12334 [DOI] [PubMed] [Google Scholar]
- Donos, N. , Horvath, A. , Calciolari, E. , & Mardas, N. (2019). Immediate provisionalization of bone level implants with a hydrophilic surface. A five‐year follow‐up of a randomized controlled clinical trial. Clinical Oral Implants Research, 30(2), 139–149. 10.1111/clr.13400 [DOI] [PubMed] [Google Scholar]
- Gallucci, G. O. , Hamilton, A. , Zhou, W. , Buser, D. , & Chen, S. (2018). Implant placement and loading protocols in partially edentulous patients: A systematic review. Clinical Oral Implants Research, 29(Suppl 16), 106–134. 10.1111/clr.13276 [DOI] [PubMed] [Google Scholar]
- Hartlev, J. , Kohberg, P. , Ahlmann, S. , Andersen, N. T. , Schou, S. , & Isidor, F. (2014). Patient satisfaction and esthetic outcome after immediate placement and provisionalization of single‐tooth implants involving a definitive individual abutment. Clinical Oral Implants Research, 25(11), 1245–1250. 10.1111/clr.12260 [DOI] [PubMed] [Google Scholar]
- Huynh‐Ba, G. , Oates, T. W. , & Williams, M. A. H. (2018). Immediate loading vs. early/conventional loading of immediately placed implants in partially edentulous patients from the patients' perspective: A systematic review. Clinical Oral Implants Research, 29(Suppl 16), 255–269. 10.1111/clr.13278 [DOI] [PubMed] [Google Scholar]
- Jemt, T. (1997). Regeneration of gingival papillae after single‐implant treatment. International Journal of Periodontics & Restorative Dentistry, 17(4), 326–333. [PubMed] [Google Scholar]
- Jung, R. E. , Zembic, A. , Pjetursson, B. E. , Zwahlen, M. , & Thoma, D. S. (2012). Systematic review of the survival rate and the incidence of biological, technical, and aesthetic complications of single crowns on implants reported in longitudinal studies with a mean follow‐up of 5 years. Clinical Oral Implants Research, 23(Suppl 6), 2–21. 10.1111/j.1600-0501.2012.02547.x [DOI] [PubMed] [Google Scholar]
- Löe, H. , & Silness, J. L. (1963). Periodontal disease in pregnancy. I. Prevalence and severity. Acta Odontologica Scandinavica, 21(12), 533–551. 10.3109/00016356309011240 [DOI] [PubMed] [Google Scholar]
- Maes, F. , Collignon, A. , Vandermeulen, D. , Marchal, G. , & Suetens, P. (1997). Multimodality image registration by maximization of mutual information. IEEE Transactions on Medical Imaging, 16, 187–198. 10.1109/42.563664 [DOI] [PubMed] [Google Scholar]
- Meijer, H. J. A. , Slagter, K. W. , Vissink, A. , & Raghoebar, G. M. (2019). Buccal bone thickness at dental implants in the maxillary anterior region with large bony defects at time of immediate implant placement: A 1‐year cohort study. Clinical Implant Dentistry and Related Research, 21(1), 73–79. 10.1111/cid.12701 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meijndert, C. M. , Raghoebar, G. M. , Santing, H. J. , Vissink, A. , & Meijer, H. J. A. (2020). Performance of bone‐level implants with conical connections in the anterior maxilla: A 5‐year prospective cohort study. Clinical Oral Implants Research, 31(2), 173–180. 10.1111/clr.13553 [DOI] [PubMed] [Google Scholar]
- Meijndert, L. , Meijer, H. J. A. , Raghoebar, G. M. , & Vissink, A. (2004). A technique for standardized evaluation of soft and hard peri‐implant tissues in partially edentulous patients. Journal of Periodontology, 75(5), 646–651. 10.1902/jop.2004.75.5.646 [DOI] [PubMed] [Google Scholar]
- Mello, C. C. , Lemos, C. A. A. , Verri, F. R. , Dos Santos, D. M. , Goiato, M. C. , & Pellizzer, E. P. (2017). Immediate implant placement into fresh extraction sockets versus delayed implants into healed sockets: A systematic review and meta‐analysis. International Journal of Oral and Maxillofacial Surgery, 46(9), 1162–1177. 10.1016/j.ijom.2017.03.016 [DOI] [PubMed] [Google Scholar]
- Mombelli, A. , van Oosten, M. A. , Schurch, E. Jr , & Land, N. P. (1987). The microbiota associated with successful or failing osseointegrated titanium implants. Oral Microbiology and Immunology, 2(4), 145–151. 10.1111/j.1399-302x.1987.tb00298.x [DOI] [PubMed] [Google Scholar]
- Noelken, R. , Moergel, M. , Kunkel, M. , & Wagner, W. (2018). Immediate and flapless implant insertion and provisionalization using autogenous bone grafts in the esthetic zone: 5‐year results. Clinical Oral Implants Research, 29(3), 320–327. 10.1111/clr.13119 [DOI] [PubMed] [Google Scholar]
- Pjetursson, B. E. , Zarauz, C. , Strasding, M. , Sailer, I. , Zwahlen, M. , & Zembic, A. (2018). A systematic review of the influence of the implant‐abutment connection on the clinical outcomes of ceramic and metal implant abutments supporting fixed implant reconstructions. Clinical Oral Implants Research, 29(Suppl 18), 160–183. 10.1111/clr.13362 [DOI] [PubMed] [Google Scholar]
- Rabel, K. , Spies, B. C. , Pieralli, S. , Vach, K. , & Kohal, R. J. (2018). The clinical performance of all‐ceramic implant‐supported single crowns: A systematic review and meta‐analysis. Clinical Oral Implants Research, 29(Suppl 18), 196–223. 10.1111/clr.13337 [DOI] [PubMed] [Google Scholar]
- Raes, S. , Cosyn, J. , Noyelle, A. , Raes, F. , & De Bruyn, H. (2018). Clinical outcome after 8 to 10 years of immediately restored single implants placed in extraction sockets and healed ridges. International Journal of Periodontics & Restorative Dentistry, 38(3), 337–345. 10.11607/prd.3478 [DOI] [PubMed] [Google Scholar]
- Raes, S. , Eghbali, A. , Chappuis, V. , Raes, F. , De Bruyn, H. , & Cosyn, J. (2018). A long‐term prospective cohort study on immediately restored single tooth implants inserted in extraction sockets and healed ridges: CBCT analyses, soft tissue alterations, aesthetic ratings, and patient‐reported outcomes. Clinical Implant Dentistry and Related Research, 20(4), 522–530. 10.1111/cid.12613 [DOI] [PubMed] [Google Scholar]
- Romanos, G. E. , Aydin, E. , Gaertner, K. , Nentwig, G. H. (2015). Long‐term results after subcrestal or crestal placement of delayed loaded implants. Clinical Implant Dentistry and Related Research, 17(1), 133–141. 10.1111/cid.12084 [DOI] [PubMed] [Google Scholar]
- Romanos, G. E. , & Javed, F. (2014). Platform switching minimises crestal bone loss around dental implants: Truth or myth? Journal of Oral Rehabilitation, 41(9), 700–708. 10.1111/joor.12189 [DOI] [PubMed] [Google Scholar]
- Slagter, K. W. , den Hartog, L. , Bakker, N. A. , Vissink, A. , Meijer, H. J. A. , & Raghoebar, G. M. (2014). Immediate placement of dental implants in the esthetic zone: A systematic review and pooled analysis. Journal of Periodontology, 85(7), e241–e250. 10.1902/jop.2014.130632 [DOI] [PubMed] [Google Scholar]
- Slagter, K. W. , Meijer, H. J. A. , Bakker, N. A. , Vissink, A. , & Raghoebar, G. M. (2015). Feasibility of immediate placement of single‐tooth implants in the aesthetic zone: A 1‐year randomized controlled trial. Journal of Clinical Periodontology, 42(8), 773–782. 10.1111/jcpe.12429 [DOI] [PubMed] [Google Scholar]
- Slagter, K. W. , Raghoebar, G. M. , Bakker, N. A. , Vissink, A. , & Meijer, H. J. A. (2017). Buccal bone thickness at dental implants in the aesthetic zone: A 1‐year follow‐up cone beam computed tomography study. Journal of Craniomaxillofacial Surgery, 45(1), 13–19. 10.1016/j.jcms.2016.11.004 [DOI] [PubMed] [Google Scholar]
- Slagter, K. W. , Raghoebar, G. M. , Vissink, A. , & Meijer, H. J. A. (2015). Inter‐ and intraobserver reproducibility of buccal bone measurements at dental implants with cone beam computed tomography in the esthetic region. International Journal of Implant Dentistry, 1(1), 8 10.1186/s40729-015-0007-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith, D. E. , & Zarb, G. A. (1989). Criteria for success of osseointegrated endosseous implants. Journal of Prosthetic Dentistry, 62(5), 567–572. 10.1016/0022-3913(89)90081-4 [DOI] [PubMed] [Google Scholar]
- Tonetti, M. S. , Jung, R. E. , Avila‐Ortiz, G. , Blanco, J. , Cosyn, J. , Fickl, S. , Figuero, E. , Goldstein, M. , Graziani, F. , Madianos, P. , Molina, A. , Nart, J. , Salvi, G. E. , Sanz‐Martin, I. , Thoma, D. , Van Assche, N. , & Vignoletti, F. (2019). Management of the extraction socket and timing of implant placement: Consensus report and clinical recommendations of group 3 of the XV European Workshop in Periodontology. Journal of Clinical Periodontology, 46(Suppl 21), 183–194. 10.1111/jcpe.13131 [DOI] [PubMed] [Google Scholar]
- Weigl, P. , & Strangio, A. (2016). The impact of immediately placed and restored single‐tooth implants on hard and soft tissues in the anterior maxilla. European Journal of Oral Implantology, 9(Suppl 1), S89–S106. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


