Abstract
Objective
To identify and describe health literacy profiles of patients with rheumatic diseases and explore whether the identified health literacy profiles can be generalized to a broader rheumatology context.
Methods
Patients with rheumatoid arthritis, spondyloarthritis, and gout from 3 hospitals in different regions in The Netherlands completed the Health Literacy Questionnaire (HLQ). Hierarchical cluster analysis was used to identify patients’ health literacy profiles based on 9 HLQ domains. A multinomial regression model with the identified health literacy profiles as the dependent variable was fitted to assess whether patients with a given disease type or attending a given hospital were more likely to belong to a specific profile.
Results
Among 895 participating patients, the lowest mean HLQ domain scores (indicating most difficulty) were found for “critical appraisal,” “navigating the health system,” and “finding good health information.” The 10 identified profiles revealed substantial diversity in combinations of strengths and weaknesses. While 42% of patients scored moderate to high on all 9 domains (profiles 1 and 3), another 42% of patients (profiles 2, 4, 5, and 6) clearly struggled with 1 or several aspects of health literacy. Notably, 16% (profiles 7–10) exhibited difficulty across a majority of health literacy domains. The probability of belonging to one of the profiles was independent of the hospital where the patient was treated or the type of rheumatic disease.
Conclusion
Ten distinct health literacy profiles were identified among patients with rheumatic diseases, independent of disease type and treating hospital. These profiles can be used to facilitate the development of health literacy interventions in rheumatology.
Introduction
Health literacy is increasingly recognized as a critical determinant of health (1) and has been hypothesized as a potential pathway leading to socioeconomic inequity in access to and outcomes of care (2, 3, 4, 5, 6). Health literacy is a complex, multidimensional concept related to literacy (7). The International Union for Health Promotion and Education defines health literacy as “the combination of personal competencies and situational resources needed for individuals to access, understand, appraise and use information and services to make decisions about health. It includes the capacity to communicate, assert and act upon these decisions” (8). While health literacy is related to education, it is critical to note that measuring education level alone as a proxy for health literacy would lead to both underestimation and overestimation of patients’ health literacy in rheumatology (9).
Significance & Innovations.
This is the first study to identify and describe a diversity of health literacy profiles of patients with rheumatoid arthritis, spondyloarthritis, and gout.
Identified health literacy profiles are independent of the type of rheumatic disease and the treating hospital and thus potentially generalizable to a broader rheumatology context.
Health literacy profiles can be used to facilitate the development of health literacy interventions.
Limited health literacy is associated with poorer health outcomes (10) and harmful health behavior (11), caused for example by suboptimal utilization of health care, less adequate patient‐provider interactions, and less adequate self‐care (6). Moreover, patients with limited health literacy are found to have reduced knowledge and understanding of their medical condition and how it should be managed (5). Health literacy difficulties disproportionally affect vulnerable groups, including older adults, ethnic minorities, individuals with disabilities, and socioeconomically disadvantaged populations (8).
Estimations of the prevalence of limited health literacy in The Netherlands range between 29% and 36% in the general population (3, 12, 13), shedding light on the magnitude of the challenge that patient health literacy may pose to our health system, health professionals, and patients. In rheumatology specifically, limited health literacy was shown to be associated with worse functional status of patients with rheumatoid arthritis (RA) (14). Another study hypothesized health literacy as a possible pathway explaining reduced access to initial biologic disease‐modifying antirheumatic drug (bDMARD) prescriptions for individuals with lower educational levels or older age (15).
Despite increasing attention to the impact of health literacy throughout the life course of (groups of) individuals (1, 8, 16, 17, 18), limited practical action has been taken to address limited health literacy as a way of reducing inequalities in access to care and in disease outcomes. Innovative interventions, including digitalization of health, might not be tailored to vulnerable patients’ health literacy (19) or reach these individuals in a timely fashion. If interventions do not account for specific health literacy needs in the target population, these already vulnerable patients are at higher risk of being left behind, while average improvements in population health could conceal these health inequalities.
Although action to address health literacy is critical, many existing studies in rheumatology merely describe associations between health literacy and health outcomes without offering practical solutions (20, 21, 22). Identifying focal points for action and developing health literacy interventions is, therefore, imperative. However, the multidimensional nature of health literacy causes individuals to experience different challenges and limitations depending on their personal health literacy strengths and weaknesses (5). Someone who has difficulty reading and understanding written health information might face other challenges than someone who is highly educated but has difficulty engaging with health care professionals. Strengths and weaknesses can occur in different patterns, and understanding these dynamics is crucial to the success of newly developed interventions. To facilitate this, the Optimizing Health Literacy and Access (Ophelia) process offers a guide to systematic development and implementation of interventions that can improve health and equity outcomes in communities (23, 24). Ophelia was developed in Australia to inform health system strengthening through optimizing the health literacy of individuals and optimizing the way organizations respond to health literacy needs by giving a voice to individuals with particular health literacy difficulties (23). The first and key phase of this approach constitutes an assessment of the health literacy of the target population that acknowledges the multidimensional nature of health literacy. Merely categorizing patients as having high or low health literacy is not sufficient to inform development of interventions. Rather, we should consider the diversity of health literacy profiles and the resulting health literacy needs of our patient population to inform meaningful improvements in care.
With this purpose in mind, the primary aim of this study was to identify health literacy profiles of patients with rheumatic diseases that uncover patterns of strengths and weaknesses across different domains of health literacy. The secondary aim was to explore whether the identified health literacy profiles are hospital specific or disease specific, or potentially generalizable to a broader rheumatology context.
Patients and Methods
Study design
An observational cross‐sectional study was conducted. It constitutes the first phase of a health literacy intervention development project in the rheumatology setting following the Ophelia process (23).
Population and setting
To capture potential differences in health literacy between patients with different rheumatic diseases and living in regions with diverse sociodemographic and geographic backgrounds, we recruited patients with RA, spondyloarthritis (SpA), and gout attending the outpatient rheumatology clinics of 3 hospitals in The Netherlands with diverse populations, namely Maastricht University Medical Center in Maastricht, Maasstad Hospital in Rotterdam, and Medisch Spectrum Twente in Enschede. We aimed to recruit 100 patients per disease group per hospital, as suggested in Ophelia to enable cluster analysis (25). All patients ages ≥18 able to answer questions in Dutch, English, German, or Arabic were eligible for participation. Data collection took place between May 2018 and May 2019.
Procedures and measurements
Consecutive patients with RA, SpA, or gout scheduled for a consultation at the outpatient clinic were informed about the study on behalf of their health care provider by regular mail 1–2 weeks prior to their consultation. Patients with limited health literacy often opt out of research projects and do not fill out questionnaires. Therefore, several strategies were employed to encourage their participation. First, front office staff reminded patients about the study upon arrival and/or after the consultation. Second, whenever possible, the treating health care provider personally introduced the patient to a researcher (MMB) who was present in the waiting room at all times for face‐to‐face communication. Third, patients could choose their preferred way of completing the questionnaire, whether on paper or digitally, at the clinic or at home, and with assistance of a researcher or relative. It was also possible to complete the questionnaire orally in an interview with a researcher, thus allowing participation of patients who might have difficulty reading. Moreover, the data collection strategy and the questionnaire were tested with a panel of patient research partners to ensure that this study was appropriate for an audience with diverse health literacy levels. A small token of appreciation in the form of a “thank you” pen was provided to encourage participants to return the questionnaire after taking it home. Patients who opted to fill out the questionnaire at home were reminded to return the questionnaire 2–3 weeks after their consultation. For returned questionnaires containing unanswered questions, the researcher contacted the patients by telephone to inquire about the missing items.
Health literacy was assessed using the Dutch version of the Health Literacy Questionnaire (HLQ), which was translated and cross‐culturally adapted from the original English‐language version (26, 27). The original version and validated translations in German and Arabic were available to allow patients with diverse cultural backgrounds to participate. The HLQ comprises 9 distinct domains of health literacy (Table 1), providing a separate score for each domain (the higher the score, the better), as it was developed to identify strengths and weaknesses across domains that would not be uncovered by a single summary score. Missing data were treated according to the expectation maximization algorithm used in Ophelia before computing mean domain scores (28).
Table 1.
Health Literacy Questionnaire domains
| Domain | Description |
|---|---|
| Part I* | |
| 1 | Feeling understood and supported by health care providers (4 items) |
| 2 | Having sufficient information to manage my health (4 items) |
| 3 | Actively managing my health (5 items) |
| 4 | Having social support for health (5 items) |
| 5 | Critical appraisal of health information (5 items) |
| Part II† | |
| 6 | Ability to actively engage with health care providers (5 items) |
| 7 | Navigating the health care system (6 items) |
| 8 | Ability to find good health information (5 items) |
| 9 | Understanding health information well enough to know what to do (5 items) |
Part I measures level of agreement with items on a 4‐point Likert scale: strongly disagree (1), disagree (2), agree (3), and strongly agree (4).
Part II measures difficulty experienced with items on a 5‐point Likert scale: always difficult/cannot do (1), usually difficult (2), sometimes difficult (3), usually easy (4), and always easy (5).
The questionnaire included additional questions on sociodemographics, self‐reported health, mastery, and self‐reported comorbidities. Sociodemographic information included age (years), sex, migration background (native Dutch, Western migrant, non‐Western migrant [29]), marital status (married, unmarried living together, single, divorced, widower), employment status (studying, employed, unemployed, [partly] disabled for work, housewife/homemaker, retired, other [multiple answers possible]), household composition (living alone, with partner, with children under and over 18 years of age, with parents, other [multiple answers possible]), and language(s) spoken at home (Dutch, English, German, Arabic, Turkish, other [multiple answers possible]). For analysis, the following dichotomous variables were created: employed (yes/no); disabled for work (yes/no); living alone (yes/no); and speaking Dutch at home (yes/no). The highest level of completed education (using standardized Dutch category definitions) was dichotomized into low (primary or lower secondary education) versus medium/high (30).
Self‐reported health was measured using a visual analog scale (range 0–10), with higher scores indicating better health. Mastery, defined as the extent to which an individual feels like he or she has control over life opportunities, was measured using the Pearlin Mastery Scale (range 7–28) (31). The Rheumatic Disease Comorbidity Index (RDCI; range 0–7) was used for information on the presence of 10 common types of comorbidities that are known to affect daily functioning and health care utilization (32).
Statistical analysis
Descriptive statistics were used to characterize the total sample and by hospital and disease group. Next, we conducted hierarchical cluster analysis based on the 9 health literacy domains using Ward’s linkage as the clustering method and the squared Euclidean distance as distance measure (33). To account for different score ranges between domains of the HLQ, the analyses were performed using Z scores per domain. Three researchers (MMB, PP, and AB) jointly examined the upper 24 cluster solutions by seeking meaningful differences between the clusters’ HLQ domains and patient characteristics while aiming to minimize within‐cluster domain variance. Distinct, meaningful clusters were selected as health literacy profiles. Of note, each patient could be assigned to 1 profile only. Profiles were presented in a heatmap reflecting mean HLQ domain scores and further described using distinctive patterns of HLQ domain scores and sociodemographic characteristics of each cluster. In a 2‐hour session, we presented and discussed the profiles and their interpretation with our patient research partner (MdW).
A multinomial regression model with the identified health literacy profiles as the dependent categorical variable was fitted to assess whether patients with 1 of the 3 rheumatic diseases or attending 1 of the 3 participating hospitals were more likely to belong to a specific profile. The base model was always adjusted for age, sex, and education. Other factors (migration background, Dutch spoken at home, living alone, marital status, disability for work, employment, mastery, comorbidities, and self‐reported health) were first added one by one and then in combinations to assess direct and confounding effects. Factors that had a significant contribution or were confounders were retained in the model. Marginal probabilities of belonging to each profile given disease or hospital were computed from the final model. Analyses were performed in SPSS, version 25 and Stata, version 15. Significance level was assumed at α = 5%.
Ethics considerations
All respondents provided written informed consent. This study was approved by the Medical Ethics Review Committee at Maastricht UMC+ (2018‐0327) as well as by the designated committees at each participating hospital for local approval (Maastricht: 18‐4‐037; Rotterdam: L2018057; Enschede: KH18‐23). One patient research partner (MdW) was involved throughout the research process.
Results
Of the 989 patients who consented to participate, 895 completed the questionnaire (for flow chart, see Supplementary Figure 1, available on the Arthritis Care & Research website at http://onlinelibrary.wiley.com/doi/10.1002/acr.24480/abstract). The mean ± SD age of participants was 61 ± 14 years, 49% were female (n = 436), and notably, only 56% of participants of working age had a paid occupation, while 51% of all participants reported having only completed low levels of education (Table 2). Recruitment of 100 patients per disease per hospital was reached for RA and SpA patients in all 3 hospitals. Recruitment of gout patients did not reach 100 patients per hospital but was large enough to have gout patients well represented in the total sample (n = 207, 23%). No substantial differences across diseases or hospitals were observed in age, education level, mastery, or self‐reported health (Table 2 and Supplementary Table 1, available on the Arthritis Care & Research website at http://onlinelibrary.wiley.com/doi/10.1002/acr.24480/abstract). A relatively smaller proportion of non‐Western migrants was observed in Maastricht (3.2%) in comparison to Enschede and Rotterdam (8.1 and 14.4%, respectively; P < 0.001).
Table 2.
Demographic characteristics of overall sample and per treating hospital*
|
Total (n = 895) |
Maastricht (n = 317) |
Rotterdam (n = 271) |
Enschede (n = 307) |
P † | |
|---|---|---|---|---|---|
| Female sex | 436 (48.7) | 155 (48.9) | 142 (52.4) | 139 (45.3) | 0.23 |
| Age, mean ± SD (range) |
61.1 ± 13.9 (18–91) |
63.0 ± 13.2 (18–91) |
59.9 ± 13.5 (25–88) |
60.1 ± 14.8 (21–89) |
0.01 |
| Rheumatic disease | 0.22 | ||||
| RA | 369 (41.2) | 133 (42.0) | 114 (42.1) | 122 (39.7) | |
| SpA | 319 (35.6) | 107 (33.8) | 107 (39.5) | 105 (34.2) | |
| Gout | 207 (23.1) | 77 (24.3) | 50 (18.5) | 80 (26.1) | |
| Education level | 0.02 | ||||
| Low | 454 (50.7) | 149 (47.0) | 159 (58.7) | 146 (47.6) | |
| Medium | 222 (24.8) | 78 (24.6) | 62 (22.9) | 82 (26.7) | |
| High | 219 (24.5) | 90 (28.4) | 50 (18.5) | 79 (25.7) | |
| Migration background | <0.001 | ||||
| Native Dutch | 738 (82.5) | 269 (84.8) | 212 (78.2) | 257 (83.7) | |
| Western migrant | 83 (9.3) | 38 (12.0) | 20 (7.4) | 25 (8.1) | |
| Non‐Western migrant | 74 (8.3) | 10 (3.2) | 39 (14.4) | 25 (8.1) | |
| Employment | |||||
| Working | 298 (33.3) | 92 (29.0) | 91 (33.6) | 115 (37.5) | 0.08 |
| Working <65 | 280 (56.1) | 89 (55.3) | 85 (52.1) | 106 (60.6) | 0.29 |
| Work disabled <65 | 146 (29.2) | 48 (29.8) | 52 (31.9) | 46 (26.3) | 0.52 |
| Retired | 358 (40.0) | 143 (45.1) | 96 (35.4) | 119 (38.8) | 0.05 |
| Household composition | |||||
| Living alone | 220 (24.6) | 86 (27.1) | 67 (24.7) | 67 (21.8) | 0.31 |
| Patient‐reported outcomes | |||||
| Mastery, mean ± SD (range) |
20.0 ± 3.4 (9–28)‡ |
19.8 ± 3.2 (9–28) |
19.7 ± 3.3 (12–28) |
20.5 ± 3.6 (10–28)‡ |
0.01 |
| RDCI score, mean ± SD (range) |
1.2 ± 1.3 (0–7) |
1.1 ± 1.3 (0–6) |
1.1 ± 1.4 (0–6) |
1.2 ± 1.4 (0–7) |
0.91 |
| Self‐reported health score, mean ± SD (range) |
6.4 ± 1.8 (0–10) |
6.6 ± 1.6 (2–10) |
6.2 ± 1.8 (0–10) |
6.4 ± 1.8 (1–10) |
0.02 |
Values are the number (%) unless indicated otherwise. RA = rheumatoid arthritis; RDCI = Rheumatic Disease Comorbidity Index; SpA = spondyloarthritis. N = 306 for mastery in Enschede, as the Pearlin Mastery Scale was not available in Arabic.
Analysis of variance/chi‐square test was used for differences across hospitals.
One respondent did not complete the Pearlin Mastery Scale, as it was not available in Arabic.
Across the HLQ domains, notable differences were observed (Table 3). Highest mean ± SD scores were found for “health care provider support” (3.14 ± 0.45 for domain 1 [range 1–4]) and “active engagement with health care providers” (3.98 ± 0.62 for domain 6 [range 1–5]). Lowest mean scores were found for “critical appraisal” (2.71 ± 0.50 for domain 5 [range 1–4]), “navigating the health system” (3.77 ± 0.62 for domain 7 [range 1–5]), and “ability to find good health information” (3.77 ± 0.72 for domain 8 [range 1–5]).
Table 3.
Health Literacy Questionnaire scores per domain for overall sample and per treating hospital*
| Domain |
Total (n = 895) |
Maastricht (n = 317) |
Rotterdam (n = 271) |
Enschede (n = 307) |
P † |
|---|---|---|---|---|---|
| 1. Health care provider support (range 1–4) |
3.14 ± 0.45 (1.25–4.00) |
3.14 ± 0.43 (1.75–4.00) |
3.10 ± 0.46 (1.25–4.00) |
3.18 ± 0.46 (1.75–4.00) |
0.09 |
| 2. Having sufficient information (range 1–4) |
3.01 ± 0.42 (1.00–4.00) |
2.99 ± 0.40 (1.50–4.00) |
2.98 ± 0.42 (1.75–4.00) |
3.06 ± 0.44 (1.00–4.00) |
0.05 |
| 3. Actively managing health (range 1–4) |
2.90 ± 0.45 (1.00–4.00) |
2.87 ± 0.44 (1.00–4.00) |
2.93 ± 0.48 (1.40–4.00) |
2.90 ± 0.42 (1.80–4.00) |
0.21 |
| 4. Having social support for health (range 1–4) |
2.97 ± 0.50 (1.20–4.00) |
2.93 ± 0.47 (1.20–4.00) |
2.93 ± 0.55 (1.20–4.00) |
3.05 ± 0.48 (1.40–4.00) |
<0.01 |
| 5. Critically appraising information (range 1–4) |
2.71 ± 0.50 (1.00–4.00) |
2.67 ± 0.48 (1.00–4.00) |
2.76 ± 0.49 (1.60–4.00) |
2.70 ± 0.53 (1.00–4.00) |
0.07 |
| 6. Actively engaging with providers (range 1–5) |
3.98 ± 0.62 (1.00–5.00) |
3.94 ± 0.62 (1.00–5.00) |
3.89 ± 0.65 (1.80–5.00) |
4.09 ± 0.59 (1.60–5.00) |
<0.001 |
| 7. Navigating the health system (range 1–5) |
3.77 ± 0.62 (1.50–5.00) |
3.69 ± 0.64 (1.50–5.00) |
3.74 ± 0.62 (1.50–5.00) |
3.86 ± 0.58 (1.67–5.00) |
<0.01 |
| 8. Finding health information (range 1–5) |
3.77 ± 0.72 (1.00–5.00) |
3.75 ± 0.69 (1.00–5.00) |
3.77 ± 0.69 (1.00–5.00) |
3.79 ± 0.78 (1.00–5.00) |
0.75 |
| 9. Understanding health information (range 1–5) |
3.91 ± 0.64 (1.60–5.00) |
3.86 ± 0.68 (1.80–5.00) |
3.89 ± 0.61 (1.80–5.00) |
3.99 ± 0.62 (1.60–5.00) |
0.02 |
Values are the mean ± SD (range) unless indicated otherwise.
Analysis of variance was used for differences across hospitals.
Domain scores were largely independent of hospital or type of rheumatic disease, although for domains 4 (social support), 6 (engaging with providers), 7 (navigating the health care system), and 9 (understanding health information), patients in Enschede tended to score slightly higher compared with patients from the other hospitals (Table 3). Moreover, for domains 1 (feeling supported by providers), 3 (actively managing health), 8 (finding health information), and 9 (understanding health information), patients with gout tended to have lower scores (see Supplementary Table 2, available on the Arthritis Care & Research website at http://onlinelibrary.wiley.com/doi/10.1002/acr.24480/abstract).
Health literacy profiles
Cluster analysis followed by researchers’ appraisal resulted in retaining 10 distinct health literacy profiles (Figure 1). Patients in 2 profiles scored moderate to high on all 9 domains: profile 1 (all very high scores) and profile 3 (high). Other profiles showed different patterns of strengths and weaknesses across the HLQ domains. Patients in profiles 2, 4, 5, and 6 struggled with 1 or several aspects of health literacy. For example, profile 4 corresponds to patients who generally fare well in engaging with health and the health system (for domains 6–9, scores ranged from 3.91 to 4.12) and have good relations with their health care provider (2.99 for domain 1) and their social network (2.98 for domain 4). However, these patients do not take ownership of their own health (2.49 for domain 3) and lack a critical attitude toward health information (2.34 for domain 5). Patients in profiles 7–10 exhibited difficulty across a majority of health literacy domains. Detailed profile descriptions are provided in Table 4. Distribution of age, mastery, the RDCI, and proportions of patients living alone, employment status, migration background, and education level differed across profiles (see Supplementary Table 3, available on the Arthritis Care & Research website at http://onlinelibrary.wiley.com/doi/10.1002/acr.24480/abstract). Of note, patients in more problematic health literacy profiles reported poorer self‐rated health (6.8 ± 1.7 for profile 1; 5.3 ± 2.1 for profile 10; P < 0.0001 for differences across all profiles) (see Supplementary Table 3).
Figure 1.
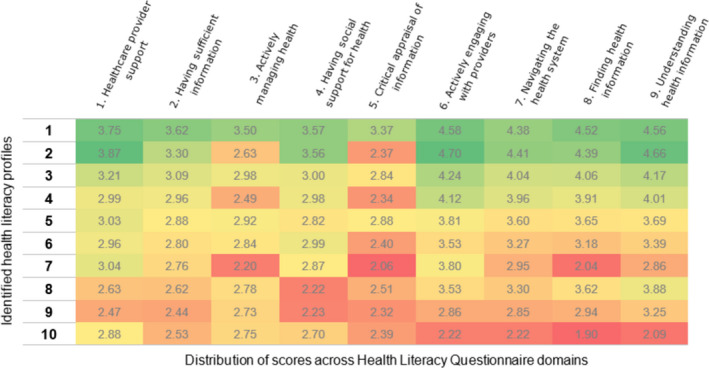
Identified health literacy profiles and mean Health Literacy Questionnaire scores per domain for each profile. Scores marked in red indicate very low scores, orange indicates low scores, yellow indicates moderate scores, and green indicates higher scores.
Table 4.
Descriptions of health literacy profiles (n = 895)*
| Profile | No. (%) | Label | Description of health literacy profile |
|---|---|---|---|
| 1 | 115 (13) | High scores; no difficulty | Patients score highly across all domains, which means that they confidently work their way through health challenges without any difficulties. |
| 2 | 32 (4) | High scores but no active role taken | Patients score low on critical attitude toward health information (domain 5 = 2.37) and take limited ownership of their own health (domain 3 = 2.63). On the other hand, these (often female [75%]) patients have a good relationship with their health care provider (domain 1 = 3.87). They engage well with their physicians (domain 6 = 4.70) to receive support and relevant information. |
| 3 | 262 (29) | Moderate to high scores; minor to no difficulty | Patients show a pattern of moderate to high scores across the spectrum. They most often have a native Dutch background (89%). Many are still working (38%) or of retirement age (42%). The profile scores suggest they are able to process health information and manage their health with little to no difficulty. |
| 4 | 110 (12) | Moderate to high scores, but no active role taken | Patients generally fare quite well. However, they have a passive attitude toward their health (domain 3 = 2.49) and are not critical toward health information (domain 5 = 2.34), which possibly indicates that health is not their main concern in life. |
| 5 | 133 (15) | Moderate scores across the spectrum | Patients report potential difficulty across multiple domains, including in particular social support for health (domain 4 = 2.82) and navigating the health system (domain 7 = 3.60) despite often living with a partner (71%). |
| 6 | 103 (12) | Lacking critical attitude and ability to acquire good information | Patients take only moderate ownership of their own health (domain 3 = 2.84), and reportedly have experienced difficulty finding health information (domain 8 = 3.18) and navigating the health system (domain 7 = 3.27). Patients in this profile often have some form of comorbidity (RDCI = 1.55) and might struggle when unexpected changes in their health status occur. |
| 7 | 25 (3) | Take no active role in their health and struggle to find and understand information | Patients struggle to manage their own health (domain 3 = 2.20) and have difficulty finding and appraising health information (domain 8 = 2.04 and 5 = 2.06), navigating the health system (domain 7 = 2.95), and understanding health information (domain 9 = 2.86). These patients are older adults (mean age 72), who often speak in local dialect at home (44%). and have low education levels (92%). They often have multiple comorbidities (mean RDCI 2.2). Their moderate to good relations with health care providers (domains 1 = 3.04 and 6 = 3.80) may partly compensate for weaknesses across other domains. |
| 8 | 62 (7) | Moderate understanding, but lack of professional and personal support | Patients generally understand health information (domain 9 = 3.88) and know how to interact with their doctor and ask the right questions (domain 6 = 3.53). However, they lack social support (one‐half reported living without a partner, domain 4 = 2.22), feel like they do not have enough information about their health (domain 2 = 2.62), and seem somewhat dissatisfied with their health care provider (domain 1 = 2.63). |
| 9 | 30 (3) | Lacks understanding, lacks support | Patients score poorly across all 9 domains. Particularly poor scores occur in domains 1–5, which mostly describe attitudes toward managing health. This profile occurs in patients of both native Dutch and immigrant backgrounds. They report being of poor health (mean 5.4 of 10) and experiencing lack of support from both their social network (domain 4 = 2.23; 47% live alone) and health care providers (domain 1 = 2.47). This implies that patients struggle to manage their health and receive little to no help. |
| 10 | 23 (3) | Low scores across all domains | Patients score poorly across all 9 domains, but particularly across domains 6–9, capturing their poor ability to perform tasks related to their health (score range 1.90–2.22). One‐third of the patients in this profile have a non‐Western background (35%). The majority of them have low education levels (96%) and are disabled for work (54% of working age subgroup). Most problematic is the severe difficulty they have finding (domain 8 = 1.90) and understanding health information (domain 9 = 2.09), which shows that they need significant assistance. |
RDCI = Rheumatic Disease Comorbidity Index.
Health literacy profiles in relation to hospital and disease
The final multinomial model assessing the distribution of profiles across diseases and hospitals was adjusted for age, sex, education, mastery, living alone, and migration background (see Supplementary Table 4, available on the Arthritis Care & Research website at http://onlinelibrary.wiley.com/doi/10.1002/acr.24480/abstract). Table 5 shows a patient’s marginal probability of belonging to 1 of the 10 identified health literacy profiles, given rheumatic disease and hospital after adjusting for covariates. There are some differences in probabilities between hospitals and disease groups for some of the health literacy profiles. However, the model showed that these differences are not statistically significant overall; having a particular health literacy profile is independent of rheumatic disease (P = 0.20) or hospital attended (P = 0.07) (see Supplementary Table 4, available at http://onlinelibrary.wiley.com/doi/10.1002/acr.24480/abstract).
Table 5.
Probabilities for fitting each of the identified profiles per rheumatic disease and treating hospital (n = 894)*
| Profile | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
|---|---|---|---|---|---|---|---|---|---|---|
| No. (%) | 115 (13) | 32 (4) | 262 (29) | 110 (12) | 133 (15) | 103 (12) | 25 (3) | 62 (7) | 30 (3) | 23 (3) |
| Rheumatic disease | ||||||||||
| RA | 0.11 | 0.05 | 0.31 | 0.15 | 0.16 | 0.11 | 0.01 | 0.05 | 0.03 | 0.03 |
| SpA | 0.16 | 0.03 | 0.26 | 0.10 | 0.15 | 0.11 | 0.04 | 0.08 | 0.05 | 0.03 |
| Gout | 0.11 | 0.03 | 0.31 | 0.12 | 0.13 | 0.14 | 0.04 | 0.08 | 0.02 | 0.02 |
| Treating hospital | ||||||||||
| Maastricht | 0.11 | 0.03 | 0.30 | 0.15 | 0.14 | 0.08 | 0.04 | 0.07 | 0.04 | 0.05 |
| Rotterdam | 0.14 | 0.03 | 0.28 | 0.10 | 0.16 | 0.13 | 0.02 | 0.09 | 0.03 | 0.01 |
| Enschede | 0.14 | 0.04 | 0.30 | 0.12 | 0.14 | 0.14 | 0.02 | 0.05 | 0.02 | 0.02 |
Estimates of marginal probabilities (between 0 and 1) of persons with a specific disease or under care in a specific hospital belonging to one of the health literacy profiles are derived from a fully adjusted multinomial model (see Supplementary Table 4, available on the Arthritis Care & Research website at http://onlinelibrary.wiley.com/doi/10.1002/acr.24480/abstract). One respondent was excluded from this analysis, as the Pearlin Mastery Scale was not available in Arabic. RA = rheumatoid arthritis; SpA = spondyloarthritis.
Discussion
The aim of this study was to identify and describe health literacy profiles of patients with RA, SpA, and gout and to explore whether the profiles are specific to a hospital or rheumatic disease type. We distinguished 10 distinct health literacy profiles, covering a range of health literacy–related strengths and weaknesses. The profiles were independent of the type of rheumatic disease or the treating hospital.
While profiles differed in the type of domains for which strengths or weaknesses were seen, common weaknesses were found for “actively managing health” (domain 3) and “critical appraisal of information” (domain 5). These aspects deserve specific attention in the majority of our patients, as only patients with profile 1 (13% of our sample) scored consistently well on these domains. Of further interest, we observed lower self‐reported health in profiles with more problematic scores across health literacy domains, hinting at the relevance of the profiles in relation to health outcomes.
The striking diversity of the identified profiles further emphasizes that health literacy does not simply range from high to low. Rather, it is an individual combination of strengths and weaknesses (either of the patient or in his or her surroundings), where strengths might function as compensation mechanisms for weaknesses. For example, a high score on social support might indicate that this patient has someone in his or her network who could help with understanding health information and making health decisions, thereby compensating for a lack of self‐reported ability in these domains. From the diverse profiles in our study, patients who score poorly across domains without clear compensation mechanisms (mostly but not exclusively reflected by profiles 6–10) likely need most attention in health care settings to ensure that they are able to receive and make use of the care they need. Notably, patients with lower education and of migrant background are overrepresented in profiles 7, 9, and 10 (8.7% of our sample). These patients reported difficulty finding good health information and navigating the health system. While for patients in profile 7 this might be mitigated by their better relationship with health care providers (domain 1), it remains a big concern for patients with profiles 9 and 10. It is both the high prevalence of limited health literacy and this diversity in patterns that professionals in clinical practice should be aware of in their communication with and treatment of patients.
In an era in which patients are invited (and even expected) to participate actively in their health and in disease management decisions, we need to tailor our approaches and interventions (related to information delivery, decision‐making, and support) to our patients’ health literacy needs (8, 19) and make sure our efforts actually reach those with limited health literacy (5). In daily practice, however, it is neither feasible nor desirable to measure the health literacy of every individual patient using the HLQ and tailor care accordingly. Rather, health literacy profiles can be used to facilitate organizational change toward health‐literate organizations in which health literacy needs are addressed by design. Key strategies emerging from Ophelia processes involve the following: 1) implementing changes that make services user friendly to individuals with limited health literacy (often called a “universal precautions approach” [34]); 2) addressing the specific barriers that patients with common health literacy profiles face; 3) improving awareness and building sensitivity to health literacy diversity among health care providers and developing skills and techniques to rapidly adapt communication approaches to the needs of different people; and 4) enhancing the ways in which families and communities support each other in acquiring and using health information.
Along these lines, this study is the first step in a care improvement process using the Ophelia process (23). In the steps to follow, health literacy profiles will be combined with qualitative information from patient interviews to create short patient stories, or “vignettes.” These vignettes will be used to facilitate group discussions with key stakeholders in patient care (including patients, physicians, nurses, management, and clinic staff) to generate ideas that could improve care. These ideas will be assessed and developed into workable packages to be implemented and evaluated in our clinics, contributing to improved and more equitable care. A recent study showed promising effects of health literacy interventions, particularly the use of teach‐back communication, on medication adherence and disease activity in a rheumatology setting (35). In addition, Ophelia studies in other settings have shown the potential for intervention development using health literacy profiles to achieve organizational change (23, 36).
When conducting this study, we did not foresee the coronavirus disease 2019 (COVID‐19) pandemic accelerating remote and digital health care delivery. An Australian survey showed that while the pandemic has left patients with rheumatic diseases concerned and in need of information, telehealth was deemed an appropriate alternative (37). However, digitalization and use of telehealth requires skills and attitudes only partially captured in the HLQ, more specifically necessitating e‐health literacy (38). While e‐health literacy was not measured in this study, challenges related to digitalization and telehealth should nevertheless be considered when developing health‐literate organizations.
This study is the first of its kind in the field of rheumatology and among the largest of studies classifying patients into health literacy profiles based on their scores across health literacy domains. While an increasing number of projects identify health literacy patterns using the HLQ (39, 40, 41) or adopt the Ophelia process in a variety of settings across the world (23, 42), much work is still in progress, and data on health literacy profiles and success of developed interventions remains scarce. Other authors have reported on health literacy profiles identified in primary care (43), hospital care (44), and cardiac rehabilitation (36). These studies also showed high diversity in the identified health literacy profiles. In this study, we observed that the distribution of patients into health literacy profiles was similar across the 3 studied rheumatic diseases and the diverse participating hospitals. While on average, patients with gout reported lower scores and patients in Enschede reported higher scores for some individual HLQ domains, these statistically significant differences did not lead to meaningful differences in the probabilities of patients having a specific health literacy profile after adjusting for covariates. We therefore suggest that the health literacy profiles identified in this study could potentially be generalized across rheumatic diseases and to other hospitals in The Netherlands.
The results of this study should be interpreted in light of a few limitations. First, despite our efforts to accommodate participation of individuals with diverse health literacy needs, we may have failed to capture some patients with the most critical levels of health literacy because they did not participate. We deployed several strategies to minimize this recruitment bias by significantly lowering the threshold to participate and encouraging responses, which resulted in inclusion of many older adults (44% age >65; 17% age >75) and 51% of patients with low education, significantly more than the 30% in the general Dutch population (45). Furthermore, we minimized missing data by contacting respondents and asking them to answer remaining items. Despite these steps, it is likely that the small number of patients in profiles with lower levels of health literacy may represent much larger and more problematic numbers in the community. Second, the selection of profiles, a dual quantitative and qualitative process based on Ward’s hierarchical cluster analysis and appraisal of results by researchers, is sensitive to subjectivity. This method does not use statistical criteria alone to determine the optimal number of clusters; rather, it involves clinical, qualitative judgments. Moreover, no evidence‐based guidelines on what constitutes a relevant difference between HLQ domain scores currently exist. However, 3 researchers (MMB, PP, and AB) jointly agreed on the most clinically meaningful cluster solution. In addition, our patient research partner (MdW) confirmed the proposed profiles as being distinct and reasonable, strengthening the face validity of our findings and contributing to our aim of identifying clinically meaningful profiles that can be used to uncover health literacy needs in our population and facilitate organizational change.
In conclusion, we identified and described a diversity of health literacy profiles of patients with rheumatic diseases. The profiles are independent of rheumatic disease and treating hospital, and thus potentially generalizable to a broader rheumatology context. These profiles can facilitate development of tailored care improvement interventions in different rheumatology settings.
Author Contributions
All authors were involved in drafting the article or revising it critically for important intellectual content, and all authors approved the final version to be submitted for publication. Mr. Bakker had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study conception and design
Bakker, Putrik, Rademakers, Ramiro, de Wit, Buchbinder, Batterham, Osborne, Boonen.
Acquisition of data
Bakker, van de Laar, Vonkeman, Kok, Voorneveld‐Nieuwenhuis, Boonen.
Analysis and interpretation of data
Bakker, Putrik, Rademakers, Ramiro, de Wit, Batterham, Osborne, Boonen.
Supporting information
Supplementary Material
Acknowledgments
We thank Mirjam Hegeman for her significant contribution to the coordination of the study in Medisch Spectrum Twente. Furthermore, we thank our panel of patient research partners for their input throughout the project and the health professionals and clinic staff at all 3 centers for their efforts in patient recruitment.
Dr. Kok has received consulting fees from Novartis (less than $10,000). Dr. Ramiro has received consulting fees and/or speaking fees from AbbVie, Eli Lilly and Company, MSD, Novartis, UCB, and Sanofi Novartis (less than $10,000 each). Dr. de Wit has received consulting fees and/or speaking fees from AbbVie, Bristol Myers Squibb, Celgene, Eli Lilly and Company, Janssen‐Cilag, Novartis, Pfizer, and Roche through the Tools2Use patient association (less than $10,000 each). Dr. Boonen has received consulting fees and/or speaking fees from UCB, Eli Lilly and Company, Novartis, and Galapagos (less than $10,000 each) and research support from AbbVie. No other disclosures relevant to this article were reported.
References
- 1. World Health Organization . Shanghai declaration on promoting health in the 2030 Agenda for Sustainable Development. Health Promot Int 2017;32:7–8. [DOI] [PubMed] [Google Scholar]
- 2. Greenhalgh T. Health literacy: towards system level solutions. BMJ 2015;350:h1026. [DOI] [PubMed] [Google Scholar]
- 3. Sørensen K, Pelikan JM, Röthlin F, Ganahl K, Slonska Z, Doyle G, et al. Health literacy in Europe: comparative results of the European health literacy survey (HLS‐EU). Eur J Public Health 2015;25:1053–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. World Health Organization . Health literacy: the solid facts. 2013. URL: https://www.euro.who.int/__data/assets/pdf_file/0008/190655/e96854.pdf?ua=1.
- 5. Batterham RW, Hawkins M, Collins PA, Buchbinder R, Osborne RH. Health literacy: applying current concepts to improve health services and reduce health inequalities. Public Health 2016;132:3–12. [DOI] [PubMed] [Google Scholar]
- 6. Paasche‐Orlow MK, Wolf MS. The causal pathways linking health literacy to health outcomes. Am J Health Behav 2007;31 Suppl 1:S19–26. [DOI] [PubMed] [Google Scholar]
- 7. Sørensen K, van den Broucke S, Fullam J, Doyle G, Pelikan J, Slonska Z, et al. Health literacy and public health: a systematic review and integration of definitions and models. BMC Public Health 2012;12:80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Bröder J, Chang P, Kickbusch I, Levin‐Zamir D, McElhinney E, Nutbeam D, et al. IUHPE position statement on health literacy: a practical vision for a health literate world. Glob Health Promot 2018;25:79–88. [Google Scholar]
- 9. Buchbinder R, Hall S, Youd JM. Functional health literacy of patients with rheumatoid arthritis attending a community‐based rheumatology practice. J Rheumatol 2006;33:879–86. [PubMed] [Google Scholar]
- 10. Berkman ND, Sheridan SL, Donahue KE, Halpern DJ, Crotty K. Low health literacy and health outcomes: an updated systematic review. Ann Intern Med 2011;155:97–107. [DOI] [PubMed] [Google Scholar]
- 11. Geboers B, Reijneveld SA, Jansen CJ, de Winter AF. Health literacy is associated with health behaviors and social factors among older adults: results from the LifeLines cohort study. J Health Commun 2016;21 Suppl 2:45–53. [DOI] [PubMed] [Google Scholar]
- 12. Heijmans M, Brabers A, Rademakers J. Health literacy in Nederland. 2018. URL: https://nivel.nl/sites/default/files/bestanden/Gezondheidsvaardigheden_in_Nederland.pdf.
- 13. Heijmans M, Brabers A, Rademakers J.Hoe gezondheidsvaardig is Nederland? Factsheet gezondheidsvaardigheden – Cijfers 2019. 2019. URL: https://nivel.nl/sites/default/files/bestanden/1003631.pdf.
- 14. Caplan L, Wolfe F, Michaud K, Quinzanos I, Hirsh JM. Strong association of health literacy with functional status among rheumatoid arthritis patients: a cross‐sectional study. Arthritis Care Res (Hoboken) 2014;66:508–14. [DOI] [PubMed] [Google Scholar]
- 15. Putrik P, Ramiro S, Lie E, Keszei AP, Kvien TK, van der Heijde D, et al. Less educated and older patients have reduced access to biologic DMARDs even in a country with highly developed social welfare (Norway): results from Norwegian cohort study NOR‐DMARD. Rheumatology (Oxford) 2016;55:1217–24. [DOI] [PubMed] [Google Scholar]
- 16. World Health Organization Regional Office for Europe . Health 2020: a European policy framework and strategy for the 21st century. Copenhagen: World Health Organization Regional Office for Europe; 2013. URL: https://www.euro.who.int/__data/assets/pdf_file/0011/199532/Health2020-Long.pdf?ua=1. [Google Scholar]
- 17. World Health Organization Regional Office for Europe . Health literacy: working together to improve health [editorial]. Public Health Panor 2019;5:133–5. [Google Scholar]
- 18. Sørensen K, Karuranga S, Denysiuk E, McLernon L. Health literacy and social change: exploring networks and interests groups shaping the rising global health literacy movement. Glob Health Promot 2018;25:89–92. [DOI] [PubMed] [Google Scholar]
- 19. Visscher BB, Steunenberg B, Heijmans M, Hofstede JM, Devillé W, van der Heide I, et al. Evidence on the effectiveness of health literacy interventions in the EU: a systematic review. BMC Public Health 2018;18:1414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Quinlan P, Price KO, Magid SK, Lyman S, Mandl LA, Stone PW. The relationship among health literacy, health knowledge, and adherence to treatment in patients with rheumatoid arthritis. HSS J 2013;9:42–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Hirsh JM, Boyle DJ, Collier DH, Oxenfeld AJ, Nash A, Quinzanos I, et al. Limited health literacy is a common finding in a public health hospital’s rheumatology clinic and is predictive of disease severity. J Clin Rheumatol 2011;17:236–41. [DOI] [PubMed] [Google Scholar]
- 22. Martin RW, McCallops K, Head AJ, Eggebeen AT, Birmingham JD, Tellinghuisen DJ. Influence of patient characteristics on perceived risks and willingness to take a proposed anti‐rheumatic drug. BMC Med Inform Decis Mak 2013;13:89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Beauchamp A, Batterham RW, Dodson S, Astbury B, Elsworth GR, McPhee C, et al. Systematic development and implementation of interventions to OPtimise Health Literacy and Access (Ophelia). BMC Public Health 2017;17:230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Batterham RW, Buchbinder R, Beauchamp A, Dodson S, Elsworth GR, Osborne RH. The OPtimising HEalth LIterAcy (Ophelia) process: study protocol for using health literacy profiling and community engagement to create and implement health reform. BMC Public Health 2014;14:694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Dodson S, Beauchamp A, Batterham R, Osborne R. Ophelia Toolkit: a step‐by-step guide for identifying and responding to health literacy needs within local communities. Swinburne: University of Technology, Melbourne, Australia; 2014. [Google Scholar]
- 26. Osborne RH, Batterham RW, Elsworth GR, Hawkins M, Buchbinder R. The grounded psychometric development and initial validation of the Health Literacy Questionnaire (HLQ). BMC Public Health 2013;13:658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Rademakers J, Waverijn G, Rijken M, Osborne R, Heijmans M. Towards a comprehensive, person‐centered assessment of health literacy: translation, cultural adaptation and psychometric test of the Dutch Health Literacy Questionnaire. BMC Public Health. Under review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Beauchamp A, Buchbinder R, Dodson S, Batterham RW, Elsworth GR, McPhee C, et al. Distribution of health literacy strengths and weaknesses across socio‐demographic groups: a cross‐sectional survey using the Health Literacy Questionnaire (HLQ). BMC Public Health 2015;15:678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Alders M. Classification of the population with a foreign background in the Netherlands. Presented at the conference The Measure and Mismeasure of Populations: the Statistical Use of Ethnic and Racial Categories in Multicultural Societies; 2001 December 17–18; Paris, France. URL: https://www.cbs.nl/-/media/imported/documents/2002/05/classification-foreign.pdf.
- 30. Statistics Netherlands . Standaard onderwijsindeling 2016.2017. URL: https://www.cbs.nl/-/media/_pdf/2017/13/pubsoi2016ed1617.pdf.
- 31. Pearlin LI, Schooler C. The structure of coping. J Health Soc Behav 1978;19:2–21. [PubMed] [Google Scholar]
- 32. England BR, Sayles H, Mikuls TR, Johnson DS, Michaud K. Validation of the rheumatic disease comorbidity index. Arthritis Care Res (Hoboken) 2015;67:865–72. [DOI] [PubMed] [Google Scholar]
- 33. Ward JH Jr. Hierarchical grouping to optimize an objective function. J Am Stat Assoc 1963;58:236–44. [Google Scholar]
- 34. DeWalt DA, Broucksou KA, Hawk V, Brach C, Hink A, Rudd R, et al. Developing and testing the health literacy universal precautions toolkit. Nurs Outlook 2011;59:85–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Hirsh J, Wood P, Keniston A, Boyle D, Quinzanos I, Caplan L, et al. Universal health literacy precautions are associated with a significant increase in medication adherence in vulnerable rheumatology patients. ACR Open Rheumatol 2020;2:110–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Aaby A, Simonsen CB, Ryom K, Maindal HT. Improving organizational health literacy responsiveness in cardiac rehabilitation using a co‐design methodology: results from the Heart Skills Study. Int J Environ Res Public Health 2020;17:1015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Antony A, Connelly K, De Silva T, Eades L, Tillett W, Ayoub S, et al. Perspectives of patients with rheumatic diseases in the early phase of COVID‐19. Arthritis Care Res (Hoboken) 2020;72:1189–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Norgaard O, Furstrand D, Klokker L, Karnoe A, Batterham R, Kayser L, et al. The e‐health literacy framework: a conceptual framework for characterizing e‐health users and their interaction with e‐health systems. Knowl Manage E Learn 2015;7:522–40. [Google Scholar]
- 39. Jessup RL, Osborne RH, Beauchamp A, Bourne A, Buchbinder R. Differences in health literacy profiles of patients admitted to a public and a private hospital in Melbourne, Australia. BMC Health Serv Res 2018;18:134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Bourne A, Peerbux S, Jessup R, Staples M, Beauchamp A, Buchbinder R. Health literacy profile of recently hospitalised patients in the private hospital setting: a cross sectional survey using the Health Literacy Questionnaire (HLQ). BMC Health Serv Res 2018;18:877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Van der Gaag M, van der Heide I, Spreeuwenberg PM, Brabers AE, Rademakers J. Health literacy and primary health care use of ethnic minorities in the Netherlands. BMC Health Serv Res 2017;17:350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Bakker MM, Putrik P, Aaby A, Debussche X, Morrissey J, Borge CR, et al. Acting together: WHO National Health Literacy Demonstration Projects (NHLDPs) address health literacy needs in the European Region. Public Health Panor 2019;5:233–43. [Google Scholar]
- 43. Aaby A, Beauchamp A, O’Hara J, Maindal HT. Large diversity in Danish health literacy profiles: perspectives for care of long‐term illness and multimorbidity. Eur J Public Health 2019;30:75–80. [DOI] [PubMed] [Google Scholar]
- 44. Jessup RL, Osborne RH, Buchbinder R, Beauchamp A. Using co‐design to develop interventions to address health literacy needs in a hospitalised population. BMC Health Serv Res 2018;18:1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Statistics Netherlands. StatLine. Bevolking; onderwijsniveau; geslacht, leeftijd en migratieachtergrond . URL: https://opendata.cbs.nl/statline/#/CBS/nl/dataset/82275NED/table?fromstatweb.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material


