Abstract
Retroperitoneal lipomas are extremely rare with few cases reported so far in the literature. They can reach different sizes and present with a variety of symptoms. The differential diagnosis is mainly with well-differentiated liposarcoma (WDLPS). We present a 34-year-old woman with a retroperitoneal lipoma herniating through the inguinal canal into the proximal thigh. The patient underwent complete oncological resection using a Karakousis’s abdominoinguinal incision. Retroperitoneal lipomas are a very rare condition and sometimes require resections technically challenging. MDM2 amplification is critical for its differential diagnosis with WDLPS.
Keywords: surgical oncology, pathology
Background
Lipomas are the most frequent soft tissue tumour in adults. They frequently arise from the subdermal tissue of trunk and extremities and are very rare in the retroperitoneum.1 They are well-circumscribed, lobulated lesions and demarcated from surrounding tissues by a thin fibrous capsule.2 On the other hand, primary retroperitoneal tumours represent less than 1% of all body tumours and majority of them are malignant. We present a case of a retroperitoneal lipoma herniating through the inguinal foramen.
Case presentation
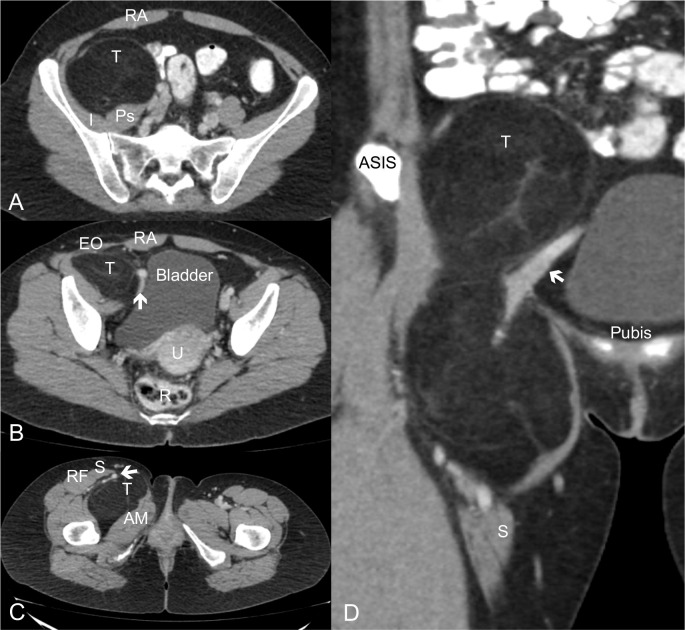
A 34-year-old woman was referred to our surgical unit because of a retroperitoneal mass found on abdominal CT scan performed due to distension and mild unspecific abdominal pain. Her medical history accounted for insulin-resistance, open right inguinal hernioplasty at age 4 and pilonidal cyst resection. Physical examination showed a large lump in the proximal right thigh, but with normal neurological and functional tests. CT-scan showed a retroperitoneal hypodense soft-tissue mass measuring 218×67×53 mm. The tumour was in contact with the right psoas muscle and medially displaced the ipsilateral iliac right vessels. Moreover, it herniated through the inguinal canal into the proximal thigh (figure 1).
Figure 1.
CT scan. (A) Axial view showing a right retroperitoneal soft-tissue tumour in contact with the iliopsoas muscle and medially displacing ipsilateral iliac vessels. (B, C) Axial view showing herniation through inguinal canal into the thigh and displacing forwards the femoral vessels. (D) Coronal view of the tumour with a ‘dumbbell appearance’. AM, adductor magnus; Arrows, iliofemoral vessels; ASIS, anterosuperior iliac spine; EO, external oblique; R, rectum, RA, rectus abdominis; RF, rectus femoris; S, sartorium muscle; T, tumour; U, uterus.
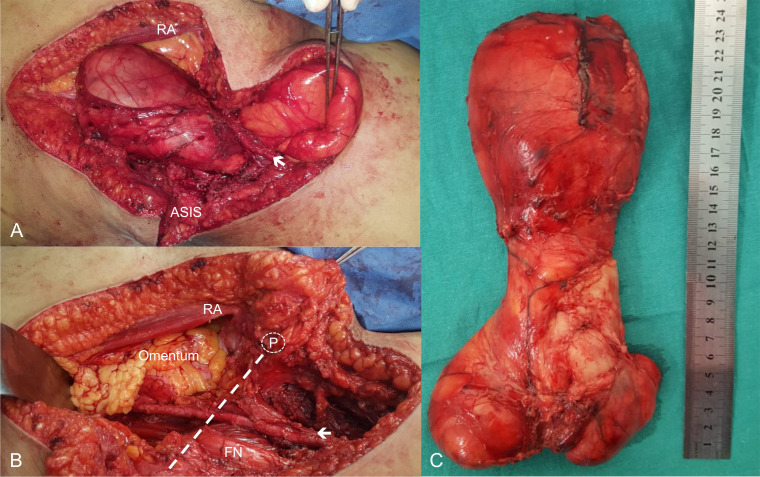
An incisional biopsy was performed before referral to our department. Histopathology study of the sample revealed a lipomatous tumour but in that moment MDM2 amplification on the fluorescent in situ hybridisation (FISH) could not be done. After discussing the case in a multidisciplinary tumour board, the resection was made with negative margins (figure 2A, B).
Figure 2.
(A, B) Dumbbell lipomatous tumour herniating through the inguinal canal. (C) Gross macroscopic specimen. Arrows, iliofemoral vessels; Dashed line, inguinal ligament; FN, femoral nerve; P, pubic tubercle; RA, rectus abdominis.
The patient underwent en bloc resection of the tumour using a Karakousis’s abdominoinguinal approach. Margins of the tumour lodge were marked with clips. She was discharged on postoperative day 2 without pain and normal extremity functions. Final histopathological examination confirmed a 14×13×7 cm lipoma (636 g) without MDM2 amplification on FISH (figure 2C). After 20 months of follow-up, the patient remains without symptoms and no evidence of local recurrence.
Differential diagnosis
Due to the impossibility to establish a definitive diagnosis on an imaging basis only, pathological assessment remains the gold standard of diagnosis. Despite the lack of complete histopathological diagnosis at initial evaluation the final diagnosis was made with the complete surgical specimen using standard techniques and FISH (MDM2 amplification analysis).
Treatment
Complete surgical resection is the cornerstone of the treatment of soft tissue tumours.
Outcome and follow-up
After 20 months of follow-up, the patient remains without symptoms and no evidence of local recurrence.
Discussion
Benign retroperitoneal lipomas in adults are exceedingly rare with less than 20 cases reported in the literature since 1980 and the first one with these anatomical characteristics to our awareness. The retroperitoneum has a wide potential space and tumours tend to grow to large sizes before becoming symptomatic. Hence, clinical presentation of retroperitoneal lipomas and soft-tissue sarcoma (STS) in general varies in different reports. The differential diagnosis is mainly with well-differentiated liposarcoma (WDLPS) which is—by far—the most frequent histotype in this anatomical site (along with dedifferentiated liposarcoma).1 3 Of note, WDLPS has high tendency to recur locally and does not metastasise.
CT-scan and MRI are the modalities of choice to assess a retroperitoneal mass. Radiological findings are very similar to those of a simple lipoma making not possible to exclude a WDLPS only by imaging assessment in most cases.4 Smooth margins with lobular contours and a fatty component with low contrast enhancement are usually present in both. Due to this, pathological assessment is the mainstay of diagnosis. Any lipomatous tumour in retroperitoneum should be suspected as malignant unless genetically proven otherwise.5 Only some WDLPS and DDLPS (de-differentiated liposarcoma) with unequivocal radiological findings can be certainly diagnosed without sample analysis.1 Therefore, core-needle biopsy, especially decided after a multidisciplinary tumour board evaluation, is the standard diagnostic procedure even though biopsies often remain inconclusive.4
In the case presented, we could not reliably rule out the diagnosis of a WDLPS, and, moreover, the tumour had a prominent pelvic extension herniating through the inguinal notch. It had been described that some pelvic soft tissue tumours can extend through the foramina of the pelvis. Furthermore, WDLPS is the histological subtype more propense to do it through the sciatic notch—referred as ‘dumbbell tumours’.6 In our case, because of the foramen involved, we choose to make an abdominoinguinal incision. This approach, along with others, is commonly used for tumours herniating through the obturator foramen.7 8 Finally, we believe a critical preoperative and intraoperative judgement of tumour’s anatomic and histological characteristics are of utmost importance in these scenarios in order to make the best decision. In the case presented, the tumour was encapsulated not showing an infiltrating growth and sole tumour resection was performed. So, surgical planning is critical in retroperitoneal and pelvic STS surgery, especially if malignancy cannot be ruled out. Complete surgical resection is the mainstay treatment1 9 and the best chance of resection with curative intent is the primary presentation.10 Since data on retroperitoneal lipomas are scarce, a close and periodic follow-up is advised.
Learning points.
Retroperitoneal lipomas in adults are very rare and differential diagnosis is mainly with well-differentiated liposarcoma.
MDM2 amplification is critical for its final diagnosis.
Surgical planning is critical in retroperitoneal and pelvic STS surgery; all cases should be discussed in a specialised Multidisciplinary Tumor Board Meeting.
Footnotes
Contributors: Study concept and design: SDQ, WSN. Acquisition of data: WSN, HDS, EAP, SDQ. Drafting of the manuscript: WSN, HDS. Critical revision of the manuscript for important intellectual content: SDQ. Final revision and final approval for publication: SDQ. All authors read and approved the final manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Quagliuolo V, Gronchi A. Current treatments of retroperitoneal sarcomas. Updates Surg, 2019. [Google Scholar]
- 2.Dalal KM, Antonescu CR, Singer S. Diagnosis and management of lipomatous tumors. J Surg Oncol 2008;97:298–313. 10.1002/jso.20975 [DOI] [PubMed] [Google Scholar]
- 3.Gronchi A, Strauss DC, Miceli R, et al. Variability in patterns of recurrence after resection of primary retroperitoneal sarcoma (Rps): a report on 1007 patients from the multi-institutional collaborative Rps Working group. Ann Surg 2016;263:1002–9. 10.1097/SLA.0000000000001447 [DOI] [PubMed] [Google Scholar]
- 4.Weniger M, D'Haese JG, Kunz W, et al. En-bloc resection of a giant retroperitoneal lipoma: a case report and review of the literature. BMC Res Notes 2015;8:75. 10.1186/s13104-015-1038-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Clay MR, Martinez AP, Weiss SW, et al. Mdm2 and CDK4 immunohistochemistry: should it be used in problematic differentiated lipomatous tumors?: a new perspective. Am J Surg Pathol 2016;40:1647–52. 10.1097/PAS.0000000000000713 [DOI] [PubMed] [Google Scholar]
- 6.Mullen JT, van Houdt W. Soft tissue tumors of the pelvis: technical and histological considerations. J Surg Oncol 2018;117:48–55. 10.1002/jso.24943 [DOI] [PubMed] [Google Scholar]
- 7.Karakousis CP. Abdominoinguinal incision and other incisions in the resection of pelvic tumors. Surg Oncol 2000;9:83–90. 10.1016/S0960-7404(00)00028-1 [DOI] [PubMed] [Google Scholar]
- 8.Bonvalot S, Raut CP, Pollock RE, et al. Technical considerations in surgery for retroperitoneal sarcomas: position paper from E-Surge, a master class in sarcoma surgery, and EORTC-STBSG. Ann Surg Oncol 2012;19:2981–91. 10.1245/s10434-012-2342-2 [DOI] [PubMed] [Google Scholar]
- 9.Bonvalot S, Rivoire M, Castaing M, et al. Primary retroperitoneal sarcomas: a multivariate analysis of surgical factors associated with local control. J Clin Oncol 2009;27:31–7. 10.1200/JCO.2008.18.0802 [DOI] [PubMed] [Google Scholar]
- 10.Trans-Atlantic RPS Working Group Management of primary retroperitoneal sarcoma (Rps) in the adult: a consensus approach from the Trans-Atlantic Rps Working group. Ann Surg Oncol 2015;22:256–63. 10.1245/s10434-014-3965-2 [DOI] [PubMed] [Google Scholar]