Abstract
Calcified lesions often result in undilatable lesions, balloon dog-boning, poor device delivery as well as underexpanded stents (UES). This leads to an increased risk of acute and chronic stent failure. A 49-year-old man was admitted with anterior wall myocardial infarction and angiogram showed a diffuse calcific left anterior descending artery/diagonal lesion, which was stented with two overlapping drug-eluting stents. Angiogram after post-dilatation showed UES. Optical coherence tomography (OCT) confirmed UES with 58% expansion, minimum stent area (MSA) of 2.91 mm2 and 360° calcium arc around the stent. This UES was dilated with a ultra high-pressure balloon (UHPB) at 40 atmosphere, that led to calcium fracture and increased MSA to 7.42 mm2 and stent expansion to 97%. While OCT-guided lesion modification prior to stenting is ideal, OCT-guided assessment and management is also invaluable post-percutaneous coronary intervention. In the event of stent underexpansion, UHPB may be used as an initial management strategy.
Keywords: cardiovascular medicine, interventional cardiology, ischaemic heart disease
Background
Calcified coronary lesions are associated with adverse clinical outcomes1 and present a major challenge for interventionists, often resulting in undilatable lesions, balloon dog-boning, poor device delivery as well as underexpanded stents (UES). Undilatable lesions and UES become more likely with increasing length, arc or thickness of coronary calcium.2 3
Coronary calcifications can be seen during angiography as radiopacities along the vessels before contrast injection, but with lower sensitivity as compared with intravascular ultrasound (IVUS). However, even with the increased accuracy for detection of calcium, IVUS does not offer information on calcium thickness and volume. This can be estimated with the use of optical coherence tomography (OCT) with a significantly higher resolution and similar sensitivity and specificity as compared with IVUS.1 Hence, coronary angiography is a poor quantifier of calcium, and its independent use to assess severely calcified lesions is associated with worst outcomes.3 This leads to an increased risk of both acute and chronic stent failure.4 OCT is the ideal method for percutaneous coronary intervention (PCI) optimisation of calcified coronary lesions so as to select the optimal management strategy.
In this case report, we describe a scenario where a severely calcified vessel resulted in suboptimal PCI and stent underexpansion as well as consequent OCT-guided management.
Case presentation
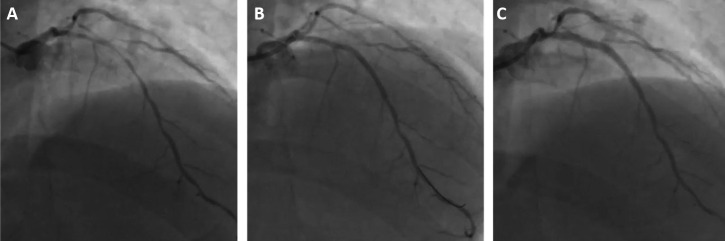
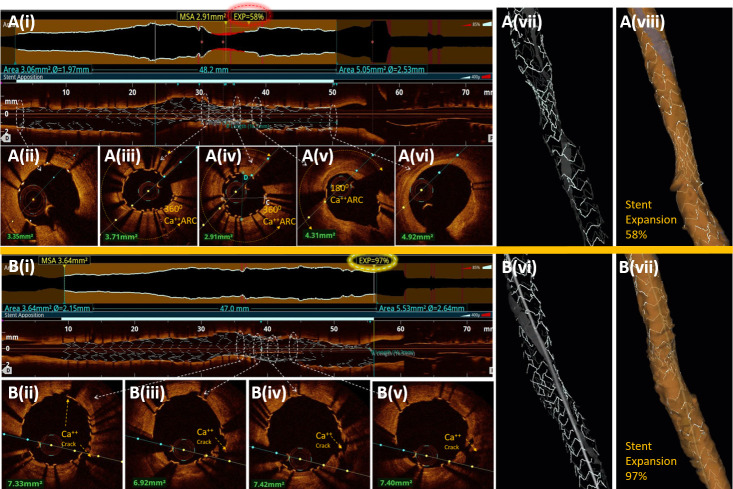
A 49-year-old man was admitted 6 days after an ST elevation anterior wall myocardial infarction, for which he was thrombolysed with tenecteplase. Coronary angiography revealed heavily calcified significant left anterior descending (LAD)/first diagonal disease (figure 1A, video 1). LAD lesion was predilated with 2.5×20 mm non-compliant balloon (NCB) at 20 atmosphere followed by two overlapping drug-eluting stents (3×18 mm and 2.75×32 mm) placement in proximal to mid-LAD, which was post-dilated with 3.25×12 mm NCB at 20 atmosphere. Angiography revealed UES in proximal LAD (figure 1B). OCT run of LAD showed UES with 58% stent expansion (figure 2A (i), (v), (vi), video 2) with 360° calcium arc around the stent (figure 2A (ii)–(iii)) and minimum stent area (MSA) of 2.91 mm2 (figure 2A (iii)). This UES was dilated with a 3.0×10 mm ultra high-pressure balloon (UHPB) (OPN NC, SIS Medical) at 40 atmosphere, that led to calcium fracture (figure 2B (ii)–(iv)), increased MSA to 7.42 mm2 and stent expansion to 97% (figure 2B (i), (iv)–(vi), video 2). Angiography showed well-expanded segment with thrombolysis in myocardial infarction III flow.
Figure 1.
Showing a case with heavily calcified LAD/D1 disease (A). PCI resulted in underexpanded stent and angiographic image as seen in image (B). Final angiography result after post-dilation with ultra high-pressure balloon shows well-expanded stent in proximal LAD and TIMI III flow (C). LAD/D1, left anterior descending/first diagonal; PCI, percutaneous coronary intervention; TIMI, thrombolysis in myocardial infarction.
Video 1.
Figure 2.
Post-PCI OCT images show UES in rendered stent view (A(i)), 3D stent only view (A(v)) and 3D lumen view (A(vi)) in proximal LAD with MSA of 2.91 mm2 (A(iii)) and 58% stent expansion. A 180°–360° calcium arc is seen around UES segment (A(ii)–A(iv)). After post-dilation with ultra high-pressure balloon at 40 atmosphere, OCT images show calcium fracture around stent (B(ii)–B(v)) resulting in increase in MSA to 7.42 mm2 and well-apposed stent with increase in stent expansion to 97%, in rendered stent view (B(i)), 3D stent only view (B(v)) and 3D lumen view (B(vi)). LAD, left anterior descending; MSA, minimum stent area; OCT, optical coherence tomography; PCI, percutaneous coronary intervention; UES, underexpanded stent.
Video 2.
Outcome and follow-up
The procedure was uneventful and the patient was discharged the next day. The patient is angina free and is under follow-up for the last 1 year.
Discussion
Calcified lesions often result in UES which leads to increased risk of acute and chronic stent failure. This occurs due to inadequate bed preparation in calcified coronary lesions, as was seen in this case. OCT is the modality of choice for the assessment of coronary calcium distribution and provides detailed information regarding calcium angle, depth and thickness prior to stent placement, thus helping in selection of appropriate strategy for plaque modification and prevention of UES.3 Fujino et al 5 recently presented an OCT-based scoring system where calcium angle, length and thickness were independent predictors of stent underexpansion, and this could be used as a modality to select appropriate lesion preparation strategies. These strategies include high-pressure balloons, scoring or cutting balloons, rotational atherectomy, orbital atherectomy, intravascular lithotripsy and laser excimer.6 The European Association of Percutaneous Coronary Interventions released a consensus document that described optimal stent expansion as relative stent expansion of >80%; or an MSA of >5.5 mm2 by IVUS and >4.5 mm2 by OCT.7 Relative stent expansion is defined as the MSA divided by the mean of proximal and distal reference lumen area. It is measured automatically by OCT machine and its value <80% is considered as UES. In this case, the dependence on coronary angiography to assess calcification resulted in suboptimal PCI results with a stent expansion of 58% and MSA of 2.91mm2. While lesion modification prior to stenting is ideal, OCT-guided assessment and management is also invaluable post-PCI, resulting in stent optimisation in at least 27% of lesions.8 Management modalities for UES include use of UHPBs, intravascular lithotripsy, laser excimer and stent ablation with rotational atherectomy. A UHPB, being double layered, has linear compliance even at 45 atmosphere, causing calcium fracture and resolution of stent underexpansion. The balloon is highly non-compliant with a nominal pressure of 10 atmosphere and a rated burst pressure of 35 atmospheres.9 It is an easy, relatively safe and effective method of calcified lesion modification. The size of the UHPB should be 0.5 mm less than the distal reference vessel diameter for predilatation and equal to the distal reference vessel diameter for post-dilating UES. Stent ablation, while effective and well accepted, is associated with several complications10 and may be more demanding in terms of procedural time, operator expertise, contrast and radiation. Intravascular lithotripsy and laser excimer are also potential treatment options for UES, but are limited by availability and cost.
Learning points.
Angiography may not be enough for identifying calcification, and intravascular imaging like optimal coherence tomography (OCT) is a must for adequate bed preparation and to prevent underexpansion of stents.
OCT is also an invaluable investigation post-percutaneous coronary intervention for optimisation of underexpanded stents.
Ultra high-pressure balloons can be the first choice in underexpanded stents and have a less learning curve requiring lesser expertise.
Footnotes
Contributors: AG and NS were involved in conceptualisation, editing the first manuscript, critical revision and final manuscript preparation. SC was involved in collection of data and preparing the first manuscript draft. KP was involved in editing the final manuscript draft.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Madhavan MV, Tarigopula M, Mintz GS, et al. Coronary artery calcification: pathogenesis and prognostic implications. J Am Coll Cardiol 2014;63:1703–14. 10.1016/j.jacc.2014.01.017 [DOI] [PubMed] [Google Scholar]
- 2. Mintz GS. Intravascular imaging of coronary calcification and its clinical implications. JACC Cardiovasc Imaging 2015;8:461–71. 10.1016/j.jcmg.2015.02.003 [DOI] [PubMed] [Google Scholar]
- 3. Mehanna E, Abbott JD, Bezerra HG. Optimizing percutaneous coronary intervention in calcified lesions: insights from optical coherence tomography of atherectomy. Circ Cardiovasc Interv 2018;11:e006813. 10.1161/CIRCINTERVENTIONS.118.006813 [DOI] [PubMed] [Google Scholar]
- 4. Généreux P, Madhavan MV, Mintz GS, et al. Ischemic outcomes after coronary intervention of calcified vessels in acute coronary syndromes. pooled analysis from the HORIZONS-AMI (Harmonizing outcomes with revascularization and stents in acute myocardial infarction) and acuity (acute catheterization and urgent intervention triage strategy) trials. J Am Coll Cardiol 2014;63:1845–54. 10.1016/j.jacc.2014.01.034 [DOI] [PubMed] [Google Scholar]
- 5. Fujino A, Mintz GS, Matsumura M, et al. A new optical coherence tomography-based calcium scoring system to predict stent underexpansion. EuroIntervention 2018;13:2182–9. 10.4244/EIJ-D-17-00962 [DOI] [PubMed] [Google Scholar]
- 6. Ueki Y, Otsuka T, Hibi K, et al. The value of intracoronary imaging and coronary physiology when treating calcified lesions. Interv Cardiol 2019;14:164–8. 10.15420/icr.2019.16.R1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Räber L, Mintz GS, Koskinas KC, et al. Clinical use of intracoronary imaging. Part 1: guidance and optimization of coronary interventions. An expert consensus document of the European association of percutaneous cardiovascular interventions. Eur Heart J 2018;39:3281–300. 10.1093/eurheartj/ehy285 [DOI] [PubMed] [Google Scholar]
- 8. Oosterveer TTM, van der Meer SM, Scherptong RWC, et al. Optical coherence tomography: current applications for the assessment of coronary artery disease and guidance of percutaneous coronary interventions. Cardiol Ther 2020;9:307–21. 10.1007/s40119-020-00185-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Secco GG, Ghione M, Mattesini A, et al. Very high-pressure dilatation for undilatable coronary lesions: indications and results with a new dedicated balloon. EuroIntervention 2016;12:359–65. 10.4244/EIJY15M06_04 [DOI] [PubMed] [Google Scholar]
- 10. Ku P-M, Huang T-Y, Chen Z-C, et al. IVUS-guided rotational atherectomy for unexpandable paclitaxel-eluting stent: a case report and review of literature. J Geriatr Cardiol 2013;10:226–9. 10.3969/j.issn.1671-5411.2013.03.014 [DOI] [PMC free article] [PubMed] [Google Scholar]